How long fever last in child
When to Worry — Children’s Fever Temperature Chart – Cleveland Clinic
Your knee-jerk reaction when your child develops a fever may be to immediately start ringing the alarms. Fevers can be scary for parents, especially first-timers. You might wonder how high is too high or if you should call the doctor immediately if your child has one. Certainly, something must be done, right?
Well, not always. It turns out that not all fevers are something to fret about. And knowing the difference between a fever that needs treatment and a fever that can be left to run its course can help your child get better faster — and with less stress on you.
“Every child will eventually experience a fever, no matter how careful you are,” says pediatrician Tracy Lim, MD. And it’s important for parents to know what to do when this happens.
We talked with Dr. Lim about how to spot a worrisome fever in children and what to do when your child has a fever.
Tips on taking your child’s temperatureFirst thing first. To know if your child is running a fever, you’ll need to take their temperature. But a look at online stores or a trip down the pharmacy aisle can leave you wondering which of those thermometer gadgets you actually need.
There’s a wide variety of thermometers available, from standard oral thermometers to temporal artery scanners.
“It is most accurate to use a rectal thermometer for infants and young children, but if you feel uneasy doing this, use whichever device makes you most comfortable,” Dr. Lim says. “In older children, an oral temperature is most accurate, if the child is able to tolerate it.”
What’s considered a fever?A “normal” body temperature is 98.6 degrees Fahrenheit, or 37 degrees Celsius, but that doesn’t mean you have to hit the panic button if your child’s temperature inches above that. Everyone’s temperature will vary a little throughout the day. It can also differ by age, activity level and other factors.
The type of thermometer you use will change the definition of what’s actually a fever for your child. Different kinds of thermometers have different levels of accuracy. This fever chart can help you understand the results you’re seeing.
Different kinds of thermometers have different levels of accuracy. This fever chart can help you understand the results you’re seeing.
Advertising Policy
Child fever temperature chart| Child’s age | Best type of thermometer | What’s considered a fever? | When to call a healthcare provider |
| 0 to 2 years | Rectal Armpit | 100.4 F (38 C) 99 F (37.22 C) | Any fever in babies under 3 months of age, or a fever over 104 F (40 C) in older kids. |
| 2 to 5 years | Rectal Ear Armpit | 100.4 F (38 C) 100.4 F (38 C) 99 F (37.22 C) | Fever over 104 F (40 C), or a fever that won’t come down with fever-reducing medication. |
| 5+ years | Ear Mouth Armpit | 100.4 F (38 C) 100 F (37.77 C) 99 F (37.22 C) | Fever over 104 F (40 C), or a fever that won’t come down with fever-reducing medication. |
It can be worrying to see your kid spike even a mild fever. We get it. But the truth is that a fever is actually a sign that your child is fighting off germs. It’s doing what it’s supposed to. And that’s a good thing.
When should you not worry about your child’s fever?
Dr. Lim says doctors tend not to worry about a fever if it’s mild, lasts fewer than five days and doesn’t affect your kid’s day-to-day activities.
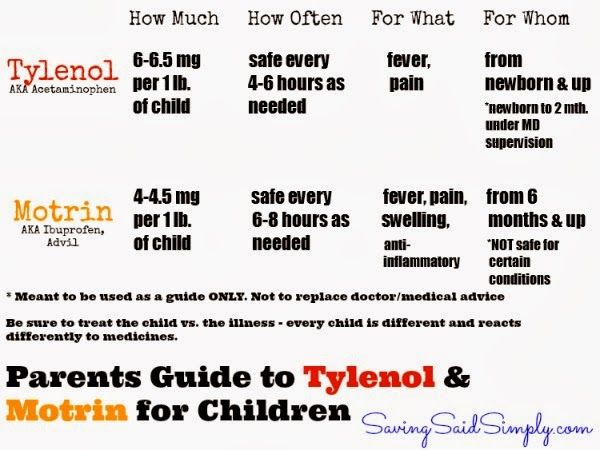
The following fevers can be monitored at home. If needed, you can also treat them with:
- Fever-reducing medication such as infant or children’s acetaminophen (Tylenol®).
- Cool compresses.
- Plenty of liquids to prevent dehydration.
- Rest.
In a child over 4 months, fevers of up to 104 F shouldn’t cause alarm. A mild fever that lasts up to five days is OK for most kids.
If your child’s behavior is relatively normal, you don’t need to be concerned. Monitor them and see if they continue to be playful and if they’re eating and drinking normally. A child with a fever may seem more tired than usual, but if they’re otherwise acting normal, there’s no reason to worry.
When to call a doctor for a feverNow for the important question: When should you be worried about a fever? Call your doctor in these cases.
Fevers in infants under 3 monthsFevers may be your infant’s only response to a serious illness. Especially in newborns, a low temperature can also be a sign of serious illness. Call a healthcare provider if your baby has any fever or if their temperature drops below 97.7 F (36.5 C) rectally.
Advertising Policy
High fever in infants and children over 3 monthsIn babies and children over 3 months, call a healthcare provider if your child’s fever is higher than 104 F (40 C), or if the fever doesn’t come down with a fever-reducing medication.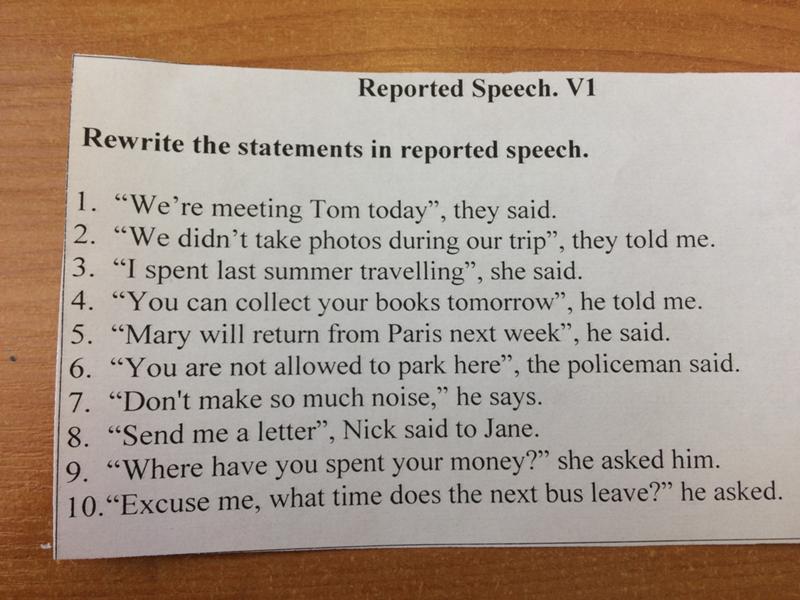
Your pediatrician may need to investigate further for underlying causes.
Your child’s fever doesn’t come down with fever reducersInfant and children’s versions of medications like acetaminophen can be used at home in babies and children if OK’d by their healthcare provider. The medications should work quickly to reduce your child’s fever. Contact a doctor if your child’s fever continues even after using a fever-reducing medication.
Your child isn’t acting like themselvesIf your child shows these signs of illness, it’s time to call a healthcare provider:
- Difficult to arouse.
- Not taking in enough liquids.
- Babies who aren’t wetting at least four diapers per day.
- Older children who aren’t urinating every eight to 12 hours.
Sometimes, parents’ instincts are meaningful. If you’re uncomfortable with your child’s temperature or illness, call a healthcare provider to discuss it.
If you’re uncomfortable with your child’s temperature or illness, call a healthcare provider to discuss it.
Seizures can be a very scary side effect of fevers in some children. Febrile seizures occur in 2% to 4% of all children under age 5. Not all seizures cause jerking movements in the body. Dr. Lim says some seizures look like “passing out.” If your child develops a seizure:
- Put your child on their side.
- Do NOT put anything in your child’s mouth.
- Call 911 if the seizure lasts more than five minutes.
If the seizure lasts fewer than five minutes, call your physician or seek immediate medical attention.
Fever facts for kids - Kids First Pediatric Partners
Fevers in kids are one of the most common issues that we see as pediatric providers, and it’s one of the biggest causes for concern for parents. No doubt, it’s scary to watch your child be sick. And it’s scary to see them get hot and be miserable.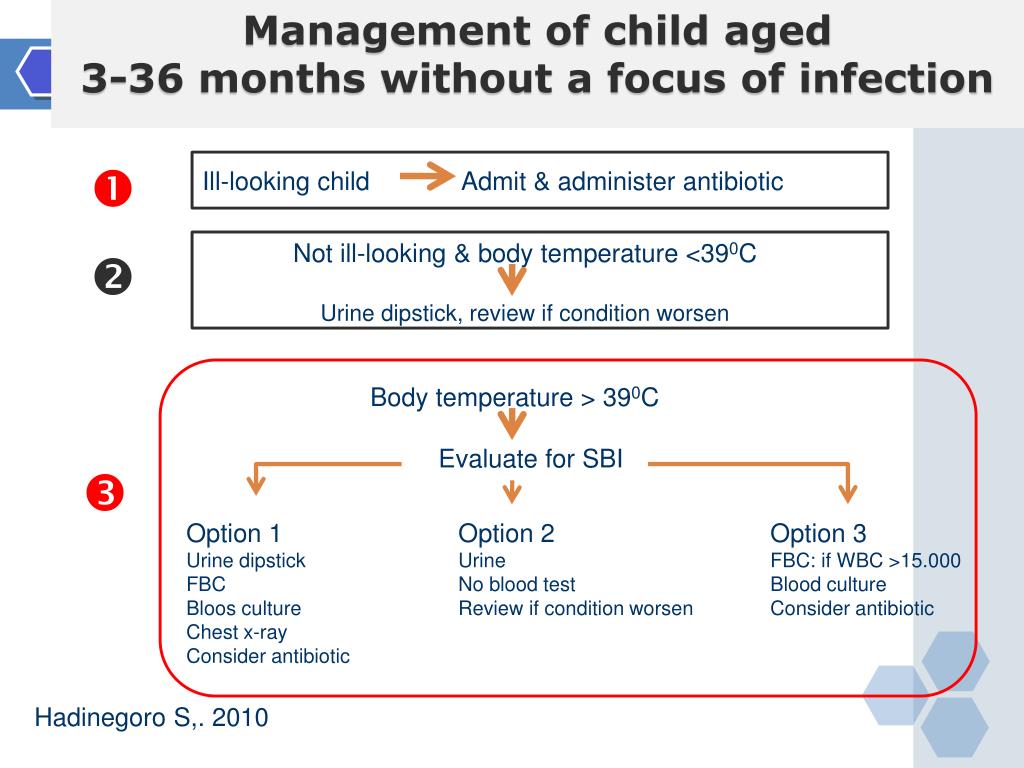
Understanding what a fever actually is might make you a little bit more comfortable with it.
Fever accounts for about a third of all the pediatric conditions we see in the office sick visits.
Here’s what parents need to know about fevers in children
The normal body temperature, as we all learned in high school biology class, 98.6 degrees Fahrenheit. In reality, 98.6 is the average of several healthy, normal, adult individuals. It’s not really a temperature that we all have to be at, and it’s certainly not a temperature that is necessarily normal for everybody.
Your normal body temperature is affected by a lot of different things.
- Age
- Time of day when you’re measuring the temperature
- Hormone levels
- Activity levels
- Menstrual cycle for women
What typically happens throughout the day is that your normal body temperature is coolest in the morning and then hottest in the evening. Your temperature can actually vary by up to one degree throughout the entire day, and that’s just when you’re feeling normal.
Babies and toddlers tend to have a higher normal body temperature than older kids and adults. Mostly this is because because they have a greater surface area to body weight ratio. They’re smaller and their weight is smaller, but they have a lot of surface area where they can give off heat. They just tend to be hotter. They also have very active growing tissues and growing tissues give off heat. They just tend to be hot.
In a newborn, which we define as a baby between the ages of zero and three months, their normal body temperature can actually be in the 99s. So 99.5 is actually normal for a lot of babies, but having said that we like our newborns to be within a certain window. So 97 to 99 tends to be more of a normal temperature for them.
What is considered a fever for adults?
The definition of fever for adults is 100.4 degrees or higher of a core body temperature. The gold standard for measuring temperature is rectally, which is not the most comfortable, obviously. We do this more for babies and for toddlers because we want to get their core body temperature, and it’s hard to do that any other way.
We do this more for babies and for toddlers because we want to get their core body temperature, and it’s hard to do that any other way.
In older kids and adults, clearly the more comfortable way to do it is through an oral thermometer. That’s another good way to measure a core body temperature, but really the best way and the gold standard is rectal.
Until what age should parents take a rectal temperature on a child?
Up to age three is actually the common recommendation. That said, parents should do what is comfortable and report the method of measurement to your pediatrician.
Is fever a sign that there’s something going wrong with a child?
A fever itself is not a problem. It’s really the sign of a problem. A lot of parents will understandably focus on the fever feeling like that’s really the big issue. For pediatricians, the fever is really more of an indication that there is something going on, something else. Usually that something else is an infection.
Most of the time infections are caused by viruses or bacteria, which are organisms that will use your healthy body to grow and sort of help themselves to survive, so they make copies inside you. It really is sort of an attack on your body.
When your body’s attacked, it activates what’s called the immune system, which is kind of the military for your body. It helps to protect you. When your body’s attacked, one of the first things it will do to sort of signal that there is this invasion is produce a fever. It produces a fever for a number of different reasons.
One of the best reasons for a fever is that the hotter body temperature can actually help slow down the growth of these viruses and bacteria, which can help of course, to reduce that infection and help you not to be as sick. That’s one reason.
It also helps increase your metabolic rate. It increases things like your heart rate, your blood pressure, your breathing rate, your muscle tone, activity, things like that in order to help you to sort of fight off whatever is infecting you.
The increased muscle tone and activity also produce the shivering and the chills. A lot of parents will worry that the child is having fevers and they’re sort of shaking and shivery. The shivering is actually a normal part of fever. It’s just your body trying to warm itself up and fight whatever’s infecting it.
Your body tries to decrease heat loss through your skin, which is why your hands and your feet tend to be very cold and clammy when you have a fever and the core part of you where your organs are, where your head is, will be much hotter.
It can produce these chemicals in your blood that induced slow wave sleep, which is why when you have fever you feel really tired. It also produces chemicals that can cause muscle aches and joint aches, which is why a lot of people feel very achy when they have fevers.
All of this activity tends to increase fluid loss. You’re breathing really hard. You’re sweating all these different things are happening. So that can make you dehydrated, which is why it’s very important anytime you have a fever to make sure that you are drinking well.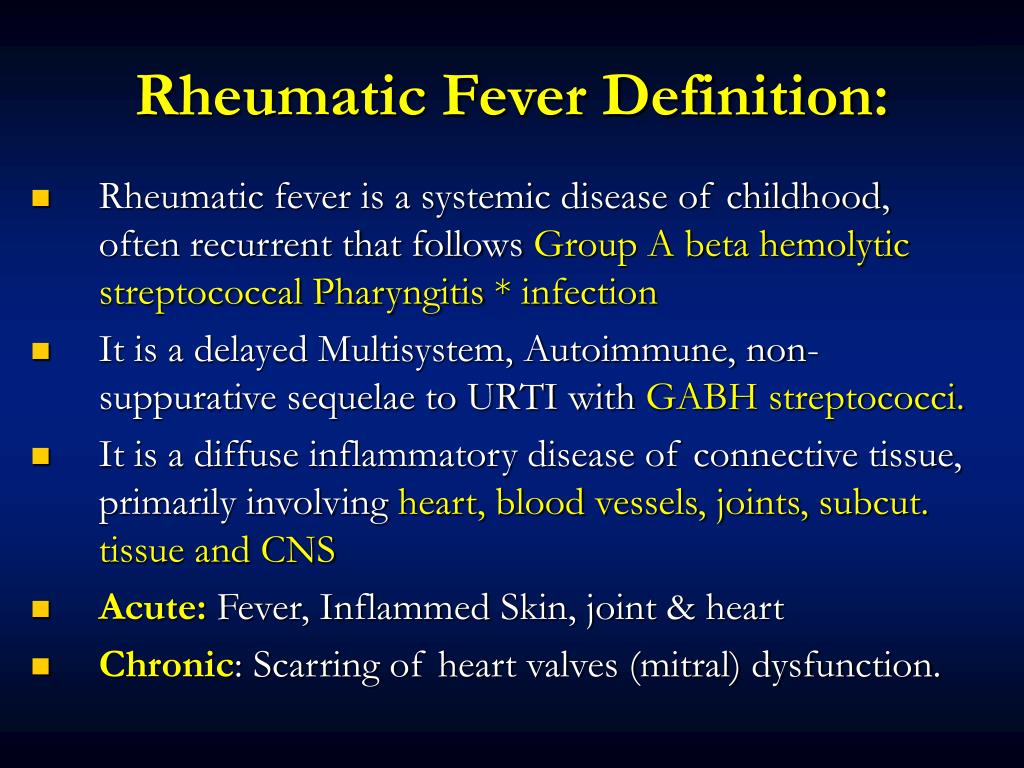
Fluid intake is part of the healing process, and it helps to recover from all of these things that your body is going during a fever.
When to call the pediatrician about a fever
In any baby, less than two months old, any fever is an emergency. Whether it’s been there for an hour or longer than that, either you need to call us or you need to just take your child to the emergency room. Although we prefer that you call us.
Newborns have a risk of serious infections, just because of their weak immunity. They tend to be a little bit more helpless when it comes to infections, and they get sick really quickly. If they have any fever, we need to know. Most of the time, what happens is we will send babies to the hospital to get tested and they need to have all of their body fluids tested.
We test blood, urine and the spinal fluid, which can be very difficult for parents to see. But it is important because those are places where serious infections can lurk. Unfortunately, a lot of times these babies do need to be hospitalized until the testing shows that they don’t have a serious infection. Even if everyone in your house has a cold and your baby seems to have the same cold, they still need to go to the emergency room and have most of the time because there can also be a serious infection.
Even if everyone in your house has a cold and your baby seems to have the same cold, they still need to go to the emergency room and have most of the time because there can also be a serious infection.
That’s one of the reasons why we don’t ever want parents to give Tylenol to a newborn less than two months old without calling us first because we don’t want to mask a fever. It’s also a reason why you want to limit visitors to really just kind of close family. Just to limit infection risk in the first two months of life until they can get those first two months shots.
In babies two months and older, it really depends on how they look. If your child is sick with a fever, but otherwise acting like him or herself, eating pretty decently, drinking pretty decently, and otherwise comfortable, and you’re comfortable with that, then it’s okay to watch them at home. We are always happy to see your child, no matter how many days of fever it’s been, if you have any concerns, but if you feel comfortable watching them generally, it’s okay to watch them and give them some Tylenol or Motrin at home.
Red flags when it comes to fevers in children
There are certain situations where we would want to see a child in the office. Most fevers are caused by viruses and viruses are benign sort of cold viruses, croup, that sort of thing. Your body can and will get rid of them on its own. Those fevers tend to last three, maybe four days. If it’s been longer than that, longer than three days certainly, we would like to see the child in the office just to make sure there’s nothing else going on. Make sure they still look really good.
Other red flags. If your child was recently sick and seemed to sort of get better, but then all of a sudden started spiking a new fever, that of course we’d want to see them for because it could be what we call a secondary infection, which is you are sick with one thing and then you get a little better and then some sort of bacteria takes advantage of you. Then you get sick with something else, like an ear infection or pneumonia.
Any fever with a strange rash, we would want to see in the office.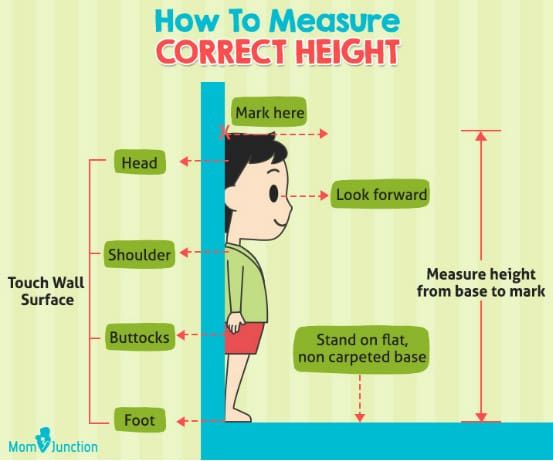
Any child who is feverish and inconsolable, meaning nothing you do makes them better. Then absolutely, we want to see them. It’s normal for them to be uncomfortable, but if they’re completely fussy and nothing you can do can make them stop crying then for sure, we want to see those kids.
If they are not making their normal number of wet diapers, we would like to see them to see if they are dehydrated.
If a child is working hard to breathe, meaning their bellies are going in and out really fast, or they seem like they’re gasping for air, we would like to see them.
If you are giving Tylenol and Motrin and they still look sick, we would like to see them.
Our main goal is to make sure the child is comfortable.
What to do when your child is comfortable because of the medicine
If your child is 104 and you give them something and it goes down to 101, but they’re more comfortable that’s perfectly fine.
Then when they’re comfortable is when they do the things that we want them to do, like drink, and eat, and sleep. Making them comfortable is the point of the medicine. You want to reduce the fever enough so they are doing those kind of normal childhood things.
Making them comfortable is the point of the medicine. You want to reduce the fever enough so they are doing those kind of normal childhood things.
What is considered a high fever in children
Most fevers never get higher than 106. That’s the highest documented. Fever brain damage happens at about 110. That temperature doesn’t happen from fever; it happens from external things. If you are working out on a really hot day, or if a child is accidentally left in a hot car. That’s the kind of thing that can make your temperature go up that high and that of course can lead to brain damage and death. That’s called hyperthermia, and that is very different.
There is no number that we would say, “Oh, for sure, you need to go to the emergency room.” The most important thing is really how does your child look? How are they acting? Are they delirious? Or are they kind of tired and achy, but otherwise themselves. That’s much more important.
Medicine that reduces fevers
Ibuprofen and acetaminophen are both very effective at reducing fever. There are no studies that show one is better than the other. Ibuprofen tends to last longer than acetaminophen. It can be dosed every six hours as opposed to every four. A lot of us tend to like it better because of that long lasting effect. It is a little bit nicer at bedtime when you can give your child something that lasts longer and helps them sleep longer.
There are no studies that show one is better than the other. Ibuprofen tends to last longer than acetaminophen. It can be dosed every six hours as opposed to every four. A lot of us tend to like it better because of that long lasting effect. It is a little bit nicer at bedtime when you can give your child something that lasts longer and helps them sleep longer.
One of the downsides of ibuprofen is that it can cause stomach irritation. It can also cause kidney problems because it is cleared from the body by the kidneys. For that reason because babies have very delicate kidneys, we don’t give babies under the age of six months ibuprofen. We would just give them acetaminophen. Ibuprofen is for six months and older only.
A lot of parents will either ask about alternating Tylenol or Motrin or ask if that should be done. We don’t recommend it. The Academy of Pediatrics also does not recommend it and there are a few reasons why.
There have been a lot of studies that have shown the combination of the two of them don’t necessarily improve patient comfort, which is really the goal. The goal is not to get temperature down, it is to improve patient comfort.
The goal is not to get temperature down, it is to improve patient comfort.
The other thing is it actually can be very dangerous. What happens is because Tylenol, or acetaminophen, is dosed every four hours and ibuprofen is dosed every six, it can be very confusing to remember what time you gave the last dose and what you’re supposed to give next. I’ve done it before. I’ve had to write it down and even then I found it very confusing. Many parents do accidentally overdose their children because they just don’t remember when the last dose was.
The other thing is it can perpetuate this whole fever phobia. It kind of makes the fever the scary thing that has to be eliminated from the child’s body. Like we said, it really is just a sign of something else going on. It doesn’t necessarily have to be completely eradicated by medications.
There is also no evidence that it reduces what are known as febrile seizures. There are some kids, a minority of kids, who will have seizures as their temperatures rise and get higher. Those seizures are called febrile seizures. They are caused just by fevers. Some practitioners think that if you alternate Tylenol and Motrin, to try to get those fevers down, that can reduce the incidents of febrile seizures. That has not been shown to be the case. A lot of people will not recommend doing that.
Those seizures are called febrile seizures. They are caused just by fevers. Some practitioners think that if you alternate Tylenol and Motrin, to try to get those fevers down, that can reduce the incidents of febrile seizures. That has not been shown to be the case. A lot of people will not recommend doing that.
The best advice I think and what I try to tell patients is stick with one. Choose either acetaminophen or ibuprofen, make that the one that you’re going to give, know how often you should be giving it, and when it’s not time for a dose, if your child is uncomfortable, sort of in between doses, then you can use the other one for breakthrough.
What about fevers with vaccinations?
A fever with a vaccination is actually a good sign. It means that the body is responding to these vaccines and creating a reaction. The point of the vaccine is to rev up your immune system so that you create these antibodies, which are your body’s way of protecting itself against these invaders that come in.
When your immune system is revved up, like we said in the beginning, you end up getting a fever and so the fevers can be normal. They’re actually a good sign that your immune system is working. Those fevers tend to last for maybe 24, 48 hours. So if your child had vaccines, but then five days later has a fever, that fever is probably not from the shots.
Again, if your child has fevers from vaccines, I would treat them with either acetaminophen or ibuprofen just to make them comfortable. Again, your goal is not necessarily to reduce the fever, but really just to help your child be more comfortable. There is actually evidence, some evidence, that if you pre-medicate with acetaminophen or ibuprofen, it can actually interfere with the immune system’s response to the vaccines. We don’t recommend that you give your child medication before they come in for their shots.
Having said that, there are some children who always have reactions and who are always miserable after fever.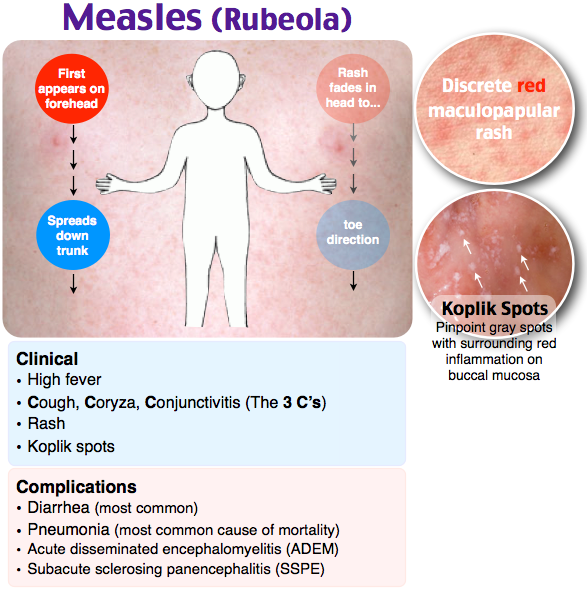 We would want them to be comfortable if you want to pre-medicate them of course you know them best so do what makes sense for them, but you don’t have to pre-medicate.
We would want them to be comfortable if you want to pre-medicate them of course you know them best so do what makes sense for them, but you don’t have to pre-medicate.
Can teething cause a fever?
Teething does not cause fevers. If we’re talking about fever as being a temperature of 100.4 or higher, teething does not cause that. Again, the vast majority of the time it’s an infection.
What usually happens is a baby is teething and so they’re putting everything in their mouths. They put a virus or something that gets them sick in their mouth, and that gives them the fever. It gets sort of miss attributed to the teething, but the teething process itself does not cause fevers.
That age group of kid also typically gets a lot of what we call viral fevers or viral syndrome with fever. Those kids in that age group typically don’t have a lot of other symptoms with these febrile illnesses. They just have a fever for a little bit, one to three days and the fever goes away.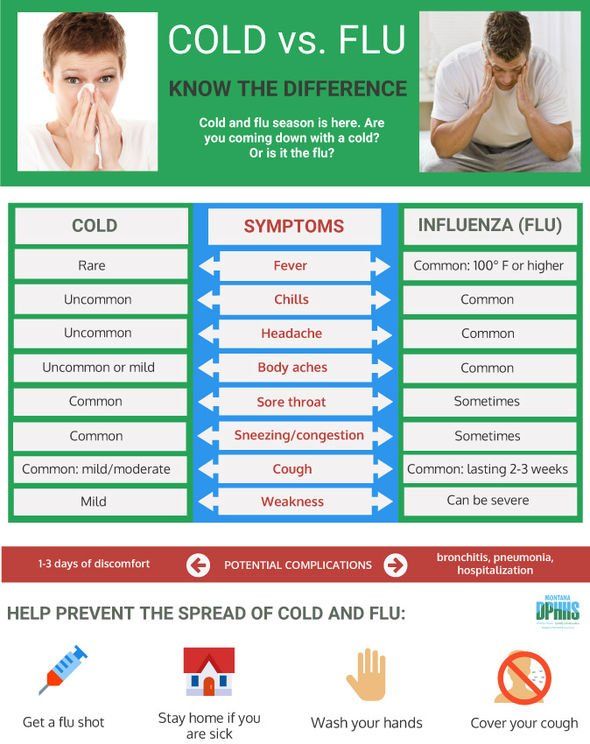 It’s very easy for parents I think to attribute that to teething because they didn’t see any big cold symptoms or other things going on.
It’s very easy for parents I think to attribute that to teething because they didn’t see any big cold symptoms or other things going on.
If you have questions about your child’s fever, give us a call at 847-676-5394, come to the morning or afternoon walk-in hours or make a telehealth appointment.
Fever
Fever and its features in children.
Promotion temperature is the most common symptom of the disease in children, each child has at least 1 time per year fever is noted. Temperature rise is also very common forces the use of medicines, all feverish children receive antipyretic means. This is facilitated by both the idea of many parents about the dangers of high temperature, and the desire of the doctor to alleviate the discomfort associated with febrile reaction or at least make appointment, the effect of which will be obvious.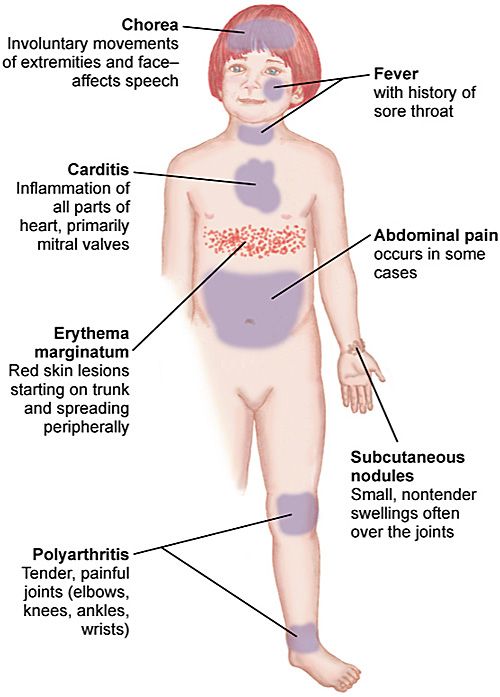 nine0003
nine0003
Wrestling with fever is an important element of treatment, but not an end in itself, since lowering the temperature in most cases does not affect the course of the disease. That's why the desire to reduce the temperature by all means and keep it at normal level indicates only about a weak acquaintance with the causes and significance of fever.
Fever- an increase in body temperature that accompanies most infectious and some non-infectious (injuries, inflammatory, autoimmune and oncological) diseases. nine0003
Normal the child's body temperature fluctuates during the day from 360C to 370C.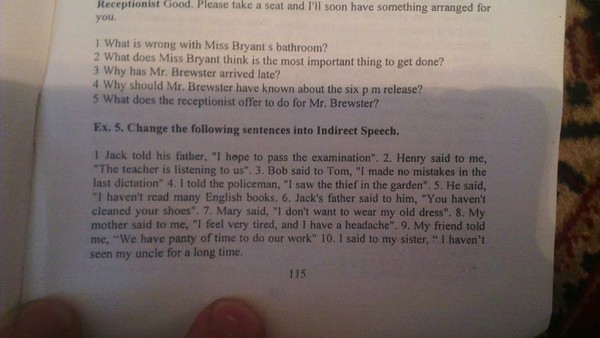
Fever - a defensive reaction directed against the causative agent of infection. At t 38.50C and above, the synthesis of interferons is enhanced, protein synthesis, leukocytosis is stimulated. All these factors reduce the ability to reproduction of many microorganisms. Fever suppression reduces intensity immune response. Fever is dangerous at temperatures closer to 410 C - mainly in children from risk groups. With a high fever, metabolism increases sharply, oxygen consumption and the release of carbon dioxide, fluid losses increase, there is extra stress on the heart and lungs. Initially healthy child tolerates these changes easily, although experiencing discomfort, but in children with pathology (often the central nervous system and congenital heart defects) can worsen the condition significantly. nine0003
There are "pink" and "white" (pale) fevers. "Pink" fever signals the correspondence of heat production to heat transfer, with it, the skin is pink, hot, moist to the touch, the child behaves normally. With "white" fever, the skin is cyanotic or marbled, often appearing "goose bumps" skin", acrocyanosis, cold extremities.
HAZARDS FEVER
Adverse phenomena caused directly by fever are extremely rare. The danger may be a disease that caused a fever that plays protective role. The main danger of fever is dehydration, which is easily prevented or corrected by the introduction of an additional amount liquids. Violation of microcirculation, the signs of which are a marble pattern skin, "goosebumps", cold extremities, are observed with "white" fever and require restoration of microcirculation. Fever is not harmful actions on the CNS. nine0003
Violation of microcirculation, the signs of which are a marble pattern skin, "goosebumps", cold extremities, are observed with "white" fever and require restoration of microcirculation. Fever is not harmful actions on the CNS. nine0003
K dangers of fever include the possibility of developing febrile seizures, which observed in 2-4% of those predisposed to children, more often at the age of 12-18 months and do not have an unfavorable influence on the central nervous system and its development.
In general, the hazards associated with fever, are largely exaggerated, with most infections the maximum temperature is set within 39.5-40.00 C, which does not threaten persistent health problems. nine0003
Fever in a child always indicates a disease, but its severity, as usually does not correlate with its severity. Many common viral (eg, rhinitis, sinusitis, pharyngitis, pneumonia) and bacterial (otitis media, urinary tract infection, impetigo) infections in immunocompetent individuals do not have a severe course, against the background of antibiotic therapy or symptomatic treatment, recovery is fast. Other infections (sepsis, meningitis, pneumonia, purulent infections of bones and joints, pyelonephritis) without treatment often lead to complications and sometimes even death. Most febrile diseases in children is associated with viral infections and those bacterial, which only briefly violate the health and do not pose a threat to the life of the child. nine0003
. Fever in a child under the age of 3 months of life requires close monitoring due to high risk of developing a serious bacterial infection.
Fever in a child under the age of 3 months of life requires close monitoring due to high risk of developing a serious bacterial infection.
"White (pale)" fever requires restoration of microcirculation.
Fever without catarrhal phenomena, rash and other visible local symptoms of infection common with urinary tract infection, in children 0-3 years of age may indicate the development bacteremia.
nine0004 Save febrile fever (more than 38.5 C) for more than 3 days, especially with rapid breathing (including in the absence of catarrhal phenomena) may indicate development of pneumonia.Hemorrhagic a rash (not blanching on pressure) with fever may indicate meningococcemia - in this case, emergency therapy is required.
Rigidity occipital muscles or their soreness, bulging of the fontanel on the background of fever indicates a CNS infection (meningitis). nine0003
Fever associated with abdominal pain and vomiting requires exclusion of appendicitis.
Fever with joint pain may be associated with bacterial arthritis, osteomyelitis.
Resistant fever with rash, changes in the oral mucosa, scleritis, an increase in lymph nodes requires the exclusion of Kawasaki disease.
Continuous (more than 2 weeks) fever requires examination to detect long-term ongoing infections, connective tissue diseases, immunodeficiency, oncological pathology. nine0003
TREATMENT FEVER
Fever is not an absolute indication for temperature reduction.
In cases where the reduction temperature is necessary, there is no need to strive to bring it to normal - enough decrease by 1-1.50С.
Indications to lower temperature:
In previously healthy children older than 3 months:
- at body temperature above 39.00C -39.50C; and/or
- in the presence of a muscular or head pain;
- in shock.
In children under 3 months of age:
- at body temperature above 380C.
In children with heart, lung, CNS:
- at body temperature above 38.50C.
Uncontrolled the use of antipyretics, especially "course", creates the illusion well-being and causes a belated appointment of etiotropic drugs. nine0003
Selection antipyretics should be founded, first of all, on their safety, and not on the strength of the effect. Ideally, an antipyretic drug for children should have the ability to quickly and effectively reduce the temperature by at least 10C, available in liquid form and as suppositories, rarely cause side effects effects at therapeutic doses and have as wide a gap as possible between therapeutic and toxic dose.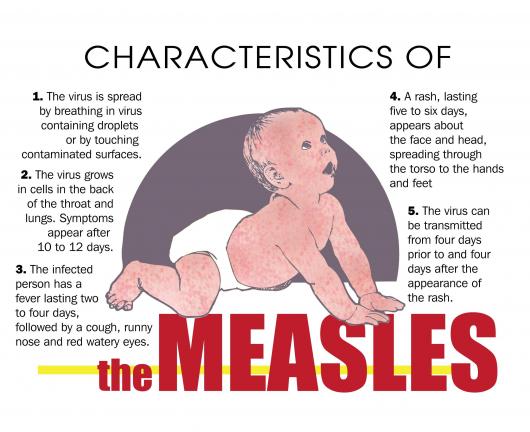
B pediatric practice prohibited the use of acetylsalicylic acid and nimesulide.
REMINDER FOR PARENTS
*temperature - protective reaction; her should be reduced only according to the indications given above;
*adequate fluid administration a feverish child is more important than a decrease in his temperature; nine0003
*not important in antipyretics "strength", but safety, to improve the patient's condition, it is enough to reduce temperature by 1-1. 50C;
50C;
* paracetamol and ibuprofen are the most safe drugs, it is important to adhere to the recommended one-time and daily their dosages;
*do not prescribe antipyretic "course" to prevent a rise in temperature, because you can see the progress bacterial infection; nine0003
* should not be used for the same reason antipyretic drugs for longer than 3 days without consulting a doctor;
*with the development of "pale" fever with spasm of the skin vessels, the introduction of an antipyretic agent should be combined with vigorously rubbing the baby's skin until redness and immediately call a doctor.
Acute respiratory viral infections
Acute respiratory viral infections are a whole group of infectious diseases characterized by similar symptoms: cough, runny nose, fever, headache, sore throat and sore throat. Depending on the pathogen, certain symptoms predominate during the course of the disease. The most pronounced clinical picture is caused by influenza viruses, parainfluenza, adenoviruses, which makes it possible to make a diagnosis without virological examination. nine0003
Depending on the pathogen, certain symptoms predominate during the course of the disease. The most pronounced clinical picture is caused by influenza viruses, parainfluenza, adenoviruses, which makes it possible to make a diagnosis without virological examination. nine0003
Influenza begins acutely against the background of full health with an increase in temperature immediately to high numbers (39-40⁰ C), often accompanied by chills. The symptoms of general intoxication come to the fore: headache, weakness, muscle and joint pain, lacrimation, pain in the eyeballs. Sometimes there is delusions, hallucinations. In young children, common symptoms are expressed: anxiety or weakness, refusal of the breast, sleep disturbance, frequent regurgitation or vomiting, frequent loose stools. Cough, runny nose, sore throat, soreness behind the sternum may be absent on the first day and join later. A favorite place for the localization of influenza viruses is the mucous membrane of the trachea, so "scratching" and pain in the chest when coughing is a constant symptom of the disease. Almost a third of patients do not have a runny nose, but dryness of the nasal mucosa is noted, which leads to repeated nosebleeds. In the first days of the disease, the cough is dry, painful, hoarseness may appear. nine0003
Almost a third of patients do not have a runny nose, but dryness of the nasal mucosa is noted, which leads to repeated nosebleeds. In the first days of the disease, the cough is dry, painful, hoarseness may appear. nine0003
In an uncomplicated course of influenza, the fever lasts 3-4 days, less often 5-6 days. If after a week the temperature does not decrease, complications may have joined. The most common complication is pneumonia. Other complications include inflammation of the paranasal sinuses and middle ear.
The main goal of health care is not the treatment of diseases, but their prevention. This fully applies to influenza, which has a pronounced winter seasonality, high contagiousness and rapid spread. nine0003
Of great importance in the prevention of influenza is the urgent isolation of patients and the separation of children at risk of infection. Epidemiologists propose to announce unscheduled holidays during the epidemic.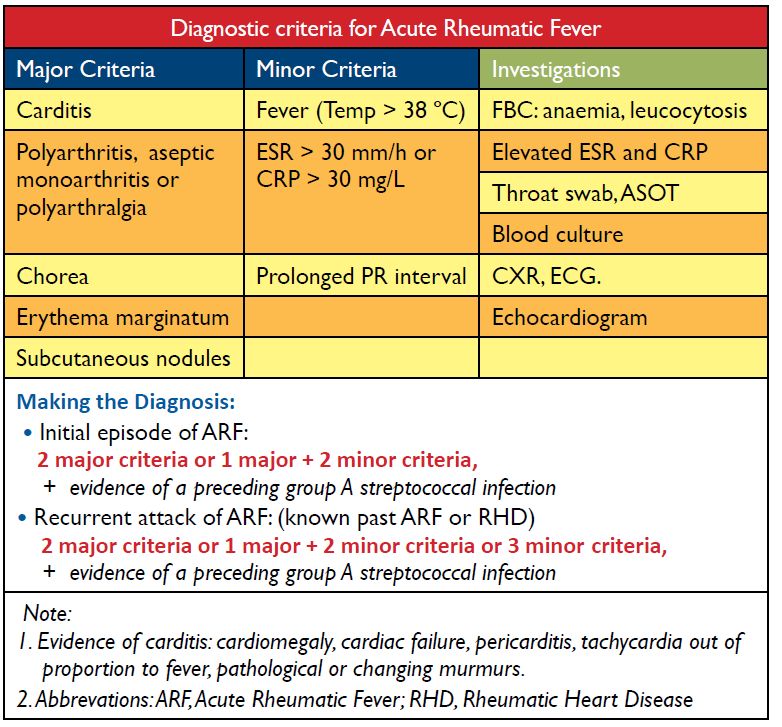 This measure significantly reduces the incidence of influenza in children's groups. Parents should also contribute to anti-epidemic measures and refuse to attend mass events, travel on excursions, go shopping and visit guests.
This measure significantly reduces the incidence of influenza in children's groups. Parents should also contribute to anti-epidemic measures and refuse to attend mass events, travel on excursions, go shopping and visit guests.
Preventive vaccinations begin in October, so that protective factors (interferon, macrophages, antibodies) are developed in the body in advance, which will prevent the development of the disease. The insidiousness of the influenza virus is manifested in its rapid variability. It is able to change the antigenic structure and acquire new properties during one epidemic. Therefore, the fight against influenza should also be aimed at strengthening nonspecific immunity, at increasing the body's ability to resist the pathogen. nine0003
If the flu is already "walking widely around the planet" and has reached your city, and even to family members, it is necessary to carry out emergency prevention for the child, which is also a preventive treatment.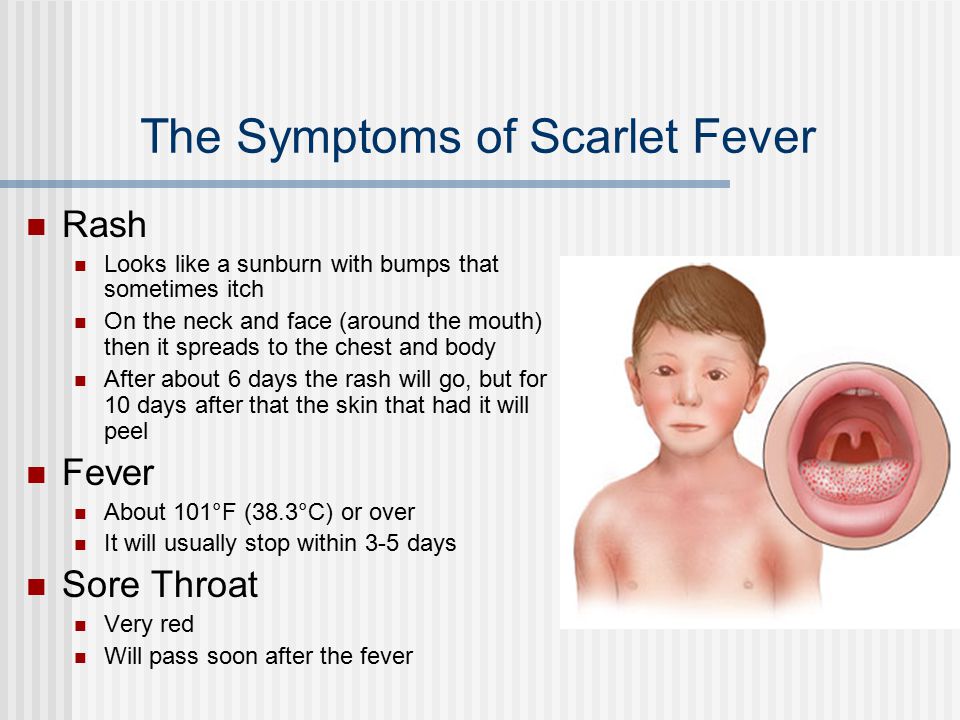 As a means for emergency prevention, interferons and drugs that enhance their production in the body (interferon inducers) are widely used.
As a means for emergency prevention, interferons and drugs that enhance their production in the body (interferon inducers) are widely used.
Human leukocyte interferon is used in the form of a solution, which is prepared from a powder, and is instilled into the nose when there is a threat of infection with influenza during the entire epidemic period, 2-3-5 drops in both nasal passages 2 times a day for children of any age. nine0003
Grippferon - nose drops of antiviral, anti-inflammatory and immunostimulating action. Recommended for children over 1 year old, 2-3 drops 2-3 times a day.
Viferon - suppositories for rectal administration, are used 2 times a day, in the morning and in the evening.
Among the interferon inducers we will name amixin, poludan, cycloferon, anaferon.
Do not forget about herbal preparations that help fight respiratory infections: onions, garlic, echinacea tincture, aralia, zamaniha, ginseng, eleutherococcus extract, etc. nine0003
nine0003
Great importance is attached to measures that enhance the nonspecific, general immunity of the body. This includes a full-fledged diet rich in proteins, vitamins and microelements, hardening procedures, a healthy lifestyle, physical education and sports.
Parainfluenza begins gradually, does not give a high temperature, does not cause severe intoxication. But its harmfulness is manifested in the fact that the virus especially often affects the larynx, causing the development of a false croup with symptoms of respiratory failure. The disease begins with a slight runny nose or cough against a background of normal or slightly elevated temperature (37.2 - 37.5 ° C). But in the middle of the night, the child wakes up from an attack of a rough "barking", "croaking" cough, shortness of breath, causing fear and anxiety, and this further intensifies the spasm. nine0003
Call an ambulance, but before the brigade arrives, try to help the suffering child. Fill the bathtub with hot water, add baking soda to it, and let the child breathe in warm, moist alkaline air while in the confined space of the bathroom. At the same time, give the child hot baths for hands and feet with a water temperature of 40 ° C. Give a warm alkaline drink: milk, in which you can add a little soda, any mineral bicarbonate water without gas. Warm, moist air helps relieve spasm of the muscles of the larynx, and alkaline steam promotes liquefaction of sputum and its discharge. The arrived ambulance team will inhale with medicines through a magic device - a nebulizer, and the child will immediately feel better. nine0003
Fill the bathtub with hot water, add baking soda to it, and let the child breathe in warm, moist alkaline air while in the confined space of the bathroom. At the same time, give the child hot baths for hands and feet with a water temperature of 40 ° C. Give a warm alkaline drink: milk, in which you can add a little soda, any mineral bicarbonate water without gas. Warm, moist air helps relieve spasm of the muscles of the larynx, and alkaline steam promotes liquefaction of sputum and its discharge. The arrived ambulance team will inhale with medicines through a magic device - a nebulizer, and the child will immediately feel better. nine0003
If the doctor insists on continuing treatment in the hospital, do not argue and do not convince him "that everything has already passed and the child is breathing well." Croup has an undulating course, and a favorable period can unexpectedly quickly give way to suffocation, requiring emergency assistance.
With croup
- do not use mustard plasters and rubbing containing essential oils and having strong odors. They are able to cause a reflex spasm of the muscles of the larynx;
They are able to cause a reflex spasm of the muscles of the larynx;
- do not use honey, raspberry jam, citrus juices - in allergy sufferers, they can increase swelling;
Do not give your child cough suppressants (sinecode). Remember that coughing has a protective function, and it should not be suppressed, but stimulated.
Adenovirus infection can be recognized by a severe runny nose, a wet cough with copious sputum, and red, festering eyes.
Adenoviruses are widely distributed throughout the world. They did not bypass our long-suffering homeland. The incidence increases in the cold season, and among all respiratory infections, it accounts for almost a third of all cases of disease. It does not disappear even in the hot summer, manifesting itself in the form of individual cases. The disease blooms especially luxuriantly in children's groups, where an outbreak can last for several months in a row, passing from one child to another. nine0003
nine0003
The disease begins with an increase in temperature, which can have two waves and last up to 12-14 days. Along with cough and runny nose, there is redness and tearing of the eyes, swelling of the eyelids and purulent discharge from the eyes. During sleep, the eyelashes stick together, and when waking up, the child cannot open his eyes, which gives him additional suffering.
The virus likes to infect adenoid tissue, lymph nodes, including the abdominal cavity. Therefore, children often complain of abdominal pain and upset stool. On the neck and in the submandibular region, you can find enlarged lymph nodes. And, looking into the throat, you will see hypertrophied edematous tonsils, often with purulent raids. nine0003
Pneumonia in adenovirus infection may be primary, caused by the virus itself. This is more commonly seen in young children. And the later development of pneumonia indicates the addition of a bacterial infection. Other complications include otitis, tonsillitis, pleurisy.
Other complications include otitis, tonsillitis, pleurisy.
For the treatment of all respiratory infections that occur with fever, it is very important to fulfill the following conditions:
• Increase heat dissipation. To do this, first of all, remove disposable diapers from the baby, which, covering almost a third of the body, prevent heat transfer and play the role of a warming compress. This is easy to see for yourself: the skin under the diaper is red, moist, with irritation in the inguinal and buttock folds. As soon as you take off the disposable diaper and dry the folds, do not be too lazy to measure the temperature, and you will be pleasantly surprised: it will drop by at least 1 degree. Do not wrap the child, do not load him with wadded blankets and downy feather beds. Take off tight tights, turtlenecks and sweaters with high tight collars. Wipe with wet wipes moistened with 1-2% vinegar or vodka. Wear light pajamas, a nightgown or T-shirt with panties.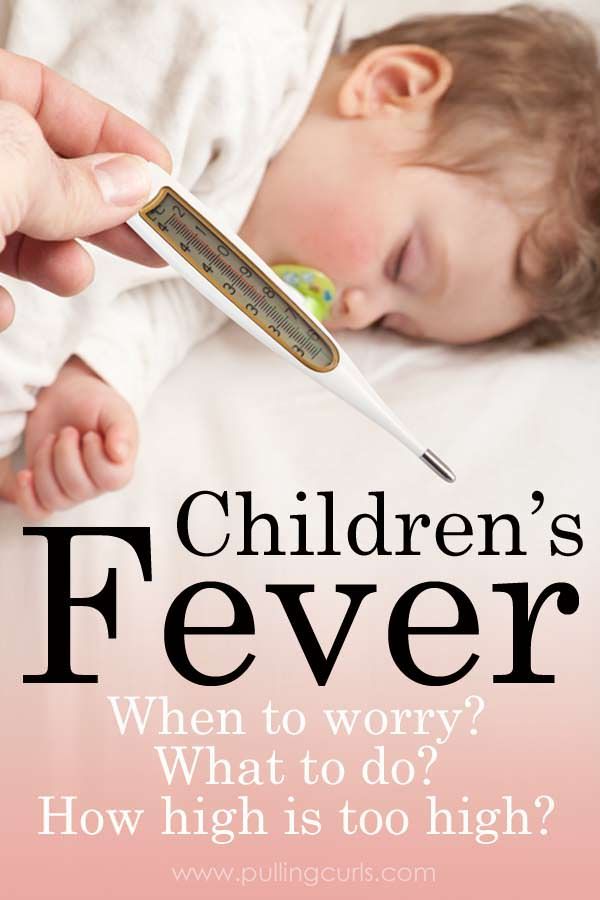 All clothing should be made of cotton fabrics that can actively absorb sweat, because the next important step is to make the child sweat. nine0003
All clothing should be made of cotton fabrics that can actively absorb sweat, because the next important step is to make the child sweat. nine0003
• Increase perspiration. It is closely adjacent to the previous one, since the evaporation of sweat from the surface of the skin willy-nilly contributes to an increase in heat transfer. In order for the child to actively sweat, it is necessary to drink him abundantly. Do not forget that sweat is not just water, but a liquid containing mineral salts. That is, sweating, the child loses vital minerals. Therefore, think about how you will make up for the deficiency of salts. It would be ideal from time to time to give the baby any glucose-salt solution (regidron, oralit, glucosolan), but not every capricious person during an illness will agree to drink tasteless water. Therefore, combine business with pleasure and prepare a decoction of raisins, dried apricots, dried fruit compote - these drinks have a lot of potassium and fructose, add a little salt (sodium and chlorine) and a little bit of baking soda (sodium bicarbonate). It will turn out a delicious and healing drink, let the baby drink with pleasure. Tired of compote? Please: mineral water, juice, herbal teas, rosehip decoction, tea with honey, lemon, raspberries (if not allergic to these products). If the child drinks willingly, do not limit him, "the water will find a hole," as the people say. It is bad when a stubborn person refuses to drink at a high temperature. The lack of fluid leads to thickening of the blood, from which all organs suffer, and especially the urinary system. If you notice that a feverish child has not urinated all day or has excreted a small amount of concentrated, darker than usual urine, then the kidneys are really thirsty and need to be provided with liquid. By any means, force the child to drink, taking into account his wishes in the choice of drinks. nine0003
It will turn out a delicious and healing drink, let the baby drink with pleasure. Tired of compote? Please: mineral water, juice, herbal teas, rosehip decoction, tea with honey, lemon, raspberries (if not allergic to these products). If the child drinks willingly, do not limit him, "the water will find a hole," as the people say. It is bad when a stubborn person refuses to drink at a high temperature. The lack of fluid leads to thickening of the blood, from which all organs suffer, and especially the urinary system. If you notice that a feverish child has not urinated all day or has excreted a small amount of concentrated, darker than usual urine, then the kidneys are really thirsty and need to be provided with liquid. By any means, force the child to drink, taking into account his wishes in the choice of drinks. nine0003
• Provide frequent ventilation of the room in which the sick child is located and maintain a cool temperature in it - ideally no higher than 18 ° C.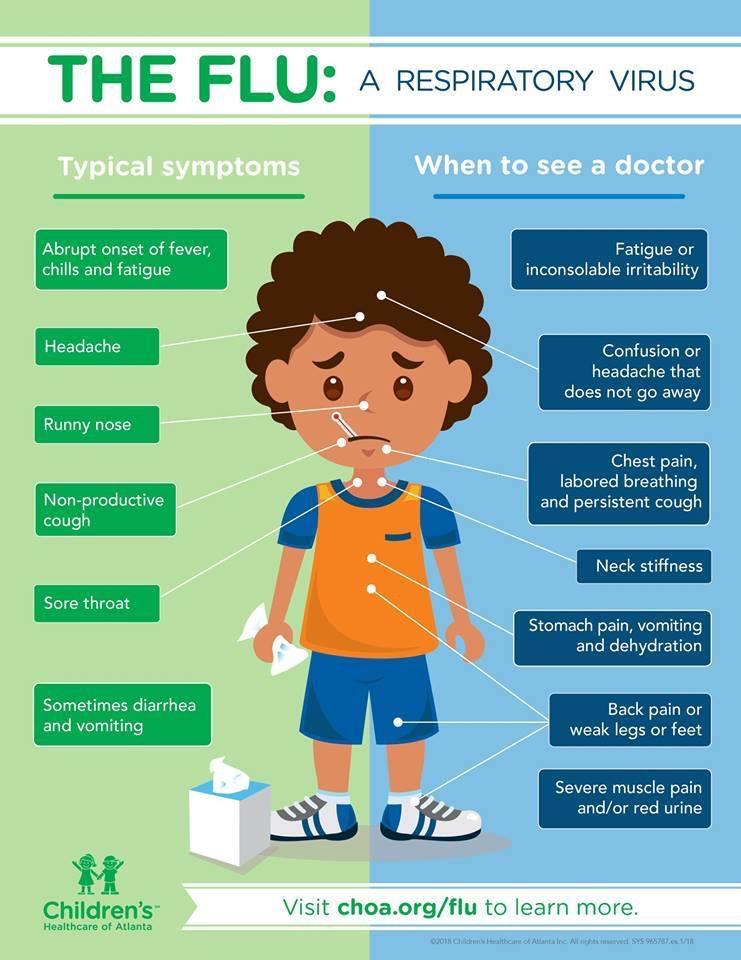 Inhalation of cool fresh air also reduces the temperature, since the body spends heat to warm it. Many mothers are terribly afraid to open the window or balcony in the nursery: "It will get even more sick." Put a hat or scarf on your head, cover it with a warm blanket and let your child breathe in fresh frosty air. As a last resort, move the patient to another room while airing. I assure you that it is impossible to “get sick even more” from clean air, but breathing stale air filled with pathogenic pathogens is difficult not only for the patient, but also for the surrounding household. nine0003
Inhalation of cool fresh air also reduces the temperature, since the body spends heat to warm it. Many mothers are terribly afraid to open the window or balcony in the nursery: "It will get even more sick." Put a hat or scarf on your head, cover it with a warm blanket and let your child breathe in fresh frosty air. As a last resort, move the patient to another room while airing. I assure you that it is impossible to “get sick even more” from clean air, but breathing stale air filled with pathogenic pathogens is difficult not only for the patient, but also for the surrounding household. nine0003
The fight against high temperature justifies itself only in those cases when it "goes off scale" beyond the mark of 39 degrees, causes a violation of the condition and behavior, the child has a tendency to seizures or a history of neurological diseases.
If the fever is accompanied by vomiting, do not force the child to take medications by mouth - they will immediately come back.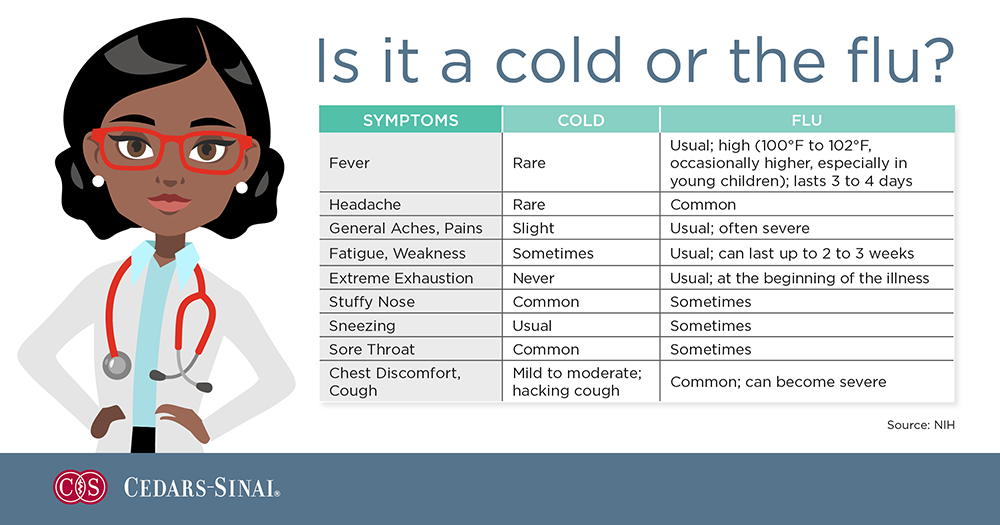 In such cases, suppositories are used, the administration of the drug with the help of an enema, and in case of emergency, injections. nine0003
In such cases, suppositories are used, the administration of the drug with the help of an enema, and in case of emergency, injections. nine0003
The intake of antipyretic drugs should be discussed with the doctor and not allowed to take initiative. Uncontrolled use and systematic excess of the dose of even the most “harmless” drug can cause a toxic or allergic effect.
Calpol, Tylenol, Panadol, Efferalgan, Cefecon - all these drugs are based on paracetamol, in fact, this is the same medicine. You need to know this in order to prevent an overdose. Exceeding the dose has a toxic effect on the liver and kidneys. Paracetamol is contraindicated in children with diseases of these organs. nine0003
In second place in terms of frequency of use is nurofen for children, produced in the form of a suspension and suppositories. The drug is prepared on the basis of ibuprofen, which is a representative of the group of non-steroidal anti-inflammatory drugs, and has not only antipyretic, but also anti-inflammatory and analgesic effects. Compared to paracetamol, Nurofen is more effective, but, unfortunately, it gives more complications. Approved for use only in children older than 3 months. The action of Nurofen begins in 30 minutes and lasts for 6-8 hours. nine0003
Compared to paracetamol, Nurofen is more effective, but, unfortunately, it gives more complications. Approved for use only in children older than 3 months. The action of Nurofen begins in 30 minutes and lasts for 6-8 hours. nine0003
A very effective drug is ibuklin, consisting of ibuprofen and paracetamol. In pediatric practice, dispersible (water-soluble) tablets are used. One tablet of children's ibuclin contains ibuprofen 100 mg and paracetamol 125 mg. Before use, dilute 1 tablet in 5 ml of chilled boiled water. The dosage of Ibuklin depends on the age and body weight of the child.
Beloved by many generations, aspirin (acetylsalicylic acid) is used only in children over 12 years of age due to the possible development of severe complications. nine0003
Often, mothers note that against the background of a high temperature, the child has cold limbs (“itself is like boiling water, but the arms and legs are icy”). This indicates a spasm of peripheral vessels.
This indicates a spasm of peripheral vessels.
Once again, the need to give a febrile patient plenty of water should be emphasized, since during this period water losses increase with sweat and rapid breathing. As a result, the excretion of fluid through the kidneys is reduced, the urine becomes concentrated, and the renal tubules can become clogged with salts, protein, cylinders, which impairs kidney function and can lead to complications. nine0003
Do not forget about the "ubiquitous and omnipotent" vitamin C. It plays an important role in increasing the body's defenses. During illness, its dose should exceed the prophylactic dose by several times and be at least 300 mg per day. Add ascorbic acid to fruit drinks, compote, juice, tea, jelly. It improves the taste of the drink and helps the body defeat the enemy.
Antibiotics and sulfa drugs are not used to treat viral infections, since the virus is not afraid of them.