Early labor pains
Ouch! Managing Labor Pains
We’ve all seen those movie scenes when a woman in a wheelchair is being rushed through the hospital doors after her water breaks. Cut to the mother-to-be screaming at the top of her lungs while pushing the baby out. Then, the money shot of the new parents staring adoringly at their newborn. But in real life, childbirth can take a lot longer than a few minutes of edited screen time, and there are a variety of ways to manage the pain that comes with bringing a baby into the world.
Erica Vu, certified nurse midwife at UC San Diego Health, talks about the stages of labor, the pain associated with the process and the interventions — both medicated and non-medicated — that are available.
How does a pregnant woman know when she is in labor?
Labor is very mysterious and one can never exactly know when it will start. Most women start to have various labor signs a few hours or weeks even before labor officially begins. These may include:
- Increased vaginal discharge — brown, pink or increased mucous discharge in general is a good sign the cervix is starting to ripen and the mucous plug, the sealed entrance to the uterus, is released.
- Many women notice more pelvis pressure as the baby’s head descends in her pelvis. Some call this “lightening” and it can happen weeks before or just as labor is starting.
- Some women start to have more nausea and loose stools or even diarrhea as the body is preparing for labor.
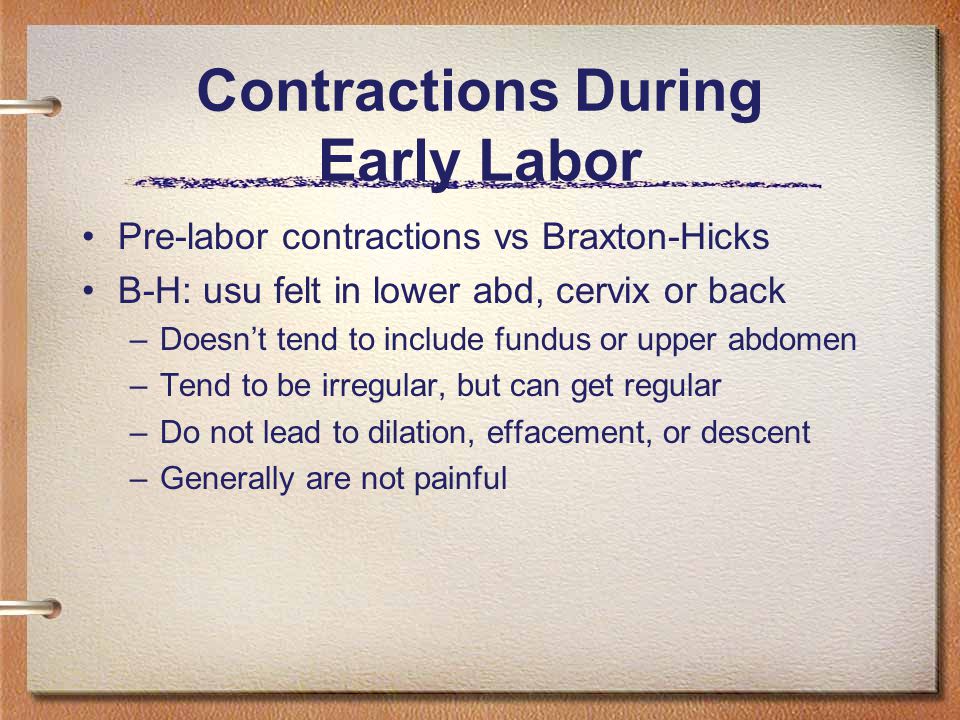
- The most common sign of labor is the increase in cramping associated with abdomen tightening or Braxton hicks. These early contractions usually start in the lower abdomen/pubic area and radiate towards the lower back. The frequency and duration of these start to increase and become more regular and rhythmic. At times, these contractions can start and increase rapidly, but for most, this can take several hours or even several days. We time the contractions from the start of one to the start of the next contraction. When they are still irregular and more than five minutes apart, most women are still in the cervical ripening/very early labor stage. These irregular contractions may even slow down or stop to give the mom’s a break.
 When the frequency starts to increase and contractions are five minutes apart or less for an hour or more, there tends to be cervical dilation and changes that mark the start of early labor progression.
When the frequency starts to increase and contractions are five minutes apart or less for an hour or more, there tends to be cervical dilation and changes that mark the start of early labor progression.
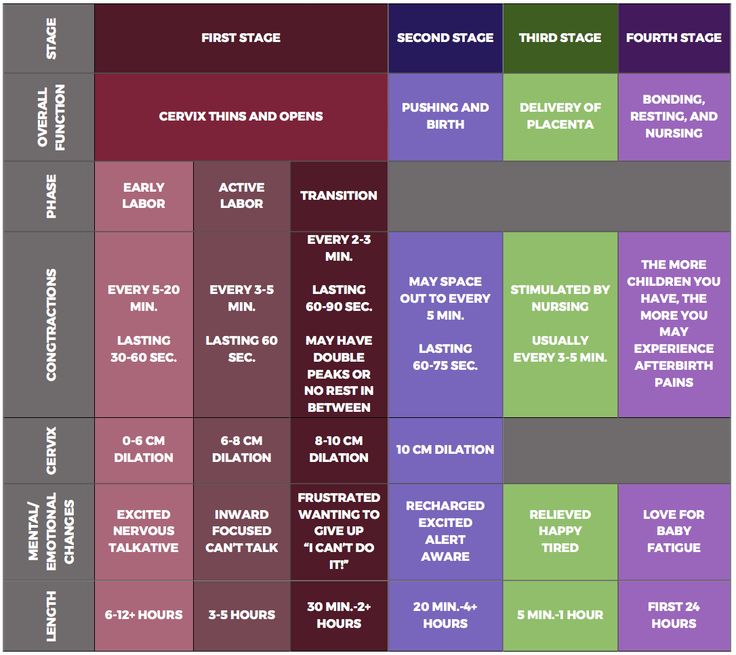
What are the stages of labor and the pain associated with each stage?
The first stage of labor is cervical dilation, or the opening of the cervix, from 0 to 10 centimeters. Early labor is when the cervix starts to dilate from closed to five centimeters with regular contractions. Early labor contractions tend to be a bit shorter in duration (60 seconds or less) and more menstrual like-cramping in the lower abdomen and back. Early labor can take several hours or even a day or more.
When the contractions intensify, include the upper abdomen and are around two to three minutes apart, active labor is most likely starting, which is the stage from 6 to 10 centimeters. Active labor contractions are a lot stronger, longer (one to two minutes in duration) and almost always necessitate more focus, breathing and position changes/labor support. Women usually also have more regular cervical dilation at intervals of one or more centimeters per hour on average. Of course, every labor can be different for each woman so this can be a variable continuum.
Women usually also have more regular cervical dilation at intervals of one or more centimeters per hour on average. Of course, every labor can be different for each woman so this can be a variable continuum.
Once women get to 10 centimeters, the second stage of labor starts and pushing begins until the baby is delivered. This can take minutes to hours depending on the baby’s position, maternal effort and anesthesia interventions.
The third stage of labor is when the baby is out and the placenta is delivered.
What type of non-medicated interventions does UC San Diego Health provide for labor pain?
Still of Katherine Heigl and Seth Rogen from Universal Picture's Knocked Up.
Multiple position changes: Walking, lunges, squats, birthing balls, birthing stools and using Rebozos (a fabric shawl originally from Mexico that when placed appropriately can help to lift lower abdomen weight off the pubic bone, squeeze hips with back labor or help during the pushing stage by pulling on the fabric in different positions both sitting, squatting or standing). All of these positions help to move the baby in position to descend down the birth canal while helping the women cope with the contractions. Women can often times focus on the movement instead of the contraction.
All of these positions help to move the baby in position to descend down the birth canal while helping the women cope with the contractions. Women can often times focus on the movement instead of the contraction.
Doulas: Women can hire private doulas or ask for one of our volunteer Hearts & Hands Program. Doulas are beneficial in so many ways, but specifically they give continuous non-medical labor support, including help with breathing techniques, counter pressure, position changes and massage and can be an advocate for your preference of labor process and birth.
Hydrotherapy (Labor tubs): Buoyancy can help with freedom of movement during contractions. Warm water helps to relax between contractions, eases body aches, including back aces, improves circulation and is a safe and effective form of pain relief.
Showers: Warm water helps with relaxation and decreases maternal tension during the peak of the contractions. Partners are invited to join to help with support.
Partners are invited to join to help with support.
Waterproof Wireless Monitors: These allow laboring women to be in the shower for pain relief while still allowing the benefits of hydrotherapy and close monitoring of the baby. The wireless monitors also allow women to change positions easily and walk freely about in their rooms or down the hallways if they so desire.
What type of medicated interventions does UC San Diego Health provide for labor pain?
Nitrous Oxide: Nitrous is a gas women breathe in through a mask during contractions. Women are still aware of the contractions, but the nitrous helps to decrease anxiety during them. Some women may experience nausea or dizziness initially but that usually resolves in a few minutes. This intervention allows freedom of movement, such as standing or sitting on a birthing ball, to help the baby descend down the birthing canal. Women can use nitrous as the only form of pain relief or it can also be used as a bridge to other forms of pain relief as labor progresses. It is safe and effective for both mom and baby. It is not as strong as the gas you receive at your dental office visit and you will not be laughing through labor. It can be used at any time during labor, pushing stage, or even during the repair of lacerations if a mother is unmedicated.
It is safe and effective for both mom and baby. It is not as strong as the gas you receive at your dental office visit and you will not be laughing through labor. It can be used at any time during labor, pushing stage, or even during the repair of lacerations if a mother is unmedicated.
Intravenous Pain Relief: Narcotics or opioids help to relax the mind and body during the peak of the contractions. These help to decrease the sensations of pain, and depending on the stage of labor, may even allow the woman to rest and sleep a bit. It does cross over to the baby through the placenta but in time, just like the mother, it wears off and has little side effects. Some women feel initial dizziness and nausea as well but that often resolves with time. We often combine the narcotic with an anti-emetic (anti-nausea) medication to help but also to prolong the duration of the pain relief. There are different types of narcotics used for different stages of labor to decrease side effects in the newborn in case of a quick delivery.
Regional Anesthesia (Epidurals): This is a pain relief method that decreases pain sensations from the abdomen and below by placing a small tube into in an area surrounding the spinal cord in the lower back and is connected to a pump. The medicine is continuously infusing during the course of labor while women remain awake and alert. Most women do not feel the majority of the pain sensations of contractions, but some will feel the pressure of the baby descending in the pelvis, which helps women to push when ready. Women are not allowed to walk with epidurals but are able to change positions in bed.
Learn more about labor pain management options at UC San Diego Health.
About UC San Diego Health Midwives
To learn more about the featured medical specialties, please visit:
- Pregnancy and Birth Care
Stages of labor | March of Dimes
Every woman’s labor is different. And it may be different each time you have a baby.

Learning about stages of labor before your due date can help you know what to expect so you can feel ready for your baby’s birth.
Use a birth plan so your health care provider and hospital staff know what your plans are for labor and after birth.
Having a professional support person, like a doula, during labor can help you have a better experience with labor and birth.
Try to stay comfortable and relaxed through labor. Move around and try different positions to find what works best for you.
What are stages of labor?
Labor (also called childbirth) is the process of your baby leaving the uterus (womb). Labor is divided into three stages:
- Labor
- Pushing and birth
- Delivery of the placenta
Every woman’s labor is different. And your labor may be different each time you have a baby. But there are patterns to labor that are true for most women. Learning about the stages of labor and what happens during each one can help you know what to expect once labor begins.
What is a birth plan?
A birth plan is a set of instructions you make about your baby’s birth. It includes things like:
- Where you want to have your baby
- Who you want to be with you during labor and birth
- If you want medicine to help with labor pain
- If there are cultural traditions you’d like to follow during labor and birth
- If you plan to breastfeed
Before your due date, use the March of Dimes birth plan to help you think about how you want your labor to be. Share the completed plan with your partner, your health care provider and the staff at the hospital where you plan to give birth.
What is a doula?
You may want to have a professional support person help you through labor and childbirth. A doula is a professional labor assistant. This is someone who is trained to give physical and emotional care and support to women and their families before, during and after childbirth. For example, a doula can:
For example, a doula can:
- Help you stay comfortable
- Explain what’s happening during labor and birth and any procedures you may have
- Encourage you and give you confidence
- Support your family and friends who are with you during labor
- Let hospital staff know what you need
- Help you get started breastfeeding
Having a support person like a doula can be good for you, your baby and your family. It can help you feel good about your birth experience. Having a doula can help:
- Shorten your labor
- Reduce your need for pain medicine during labor
- Reduce your risk of needing a cesarean birth or the need for your provider to use forceps or suction with a vaginal birth
- Your baby get a good Apgar score at birth. Your baby gets an Apgar test right after birth to check his overall health. The test checks his heart rate, breathing, muscle tone, reflexes and skin color.
To find a certified doula, ask your provider or go to DONA International.
You also may want to have your partner, a friend or a family member be a support person to help you through labor. They can go to childbirth education classes with you to learn ways to help, like timing your contractions, helping you relax and helping you move around to find a comfortable position. Ask your provider about childbirth education classes in your area.
If you decide to have a doula or another support person help you with labor and birth, put their names and contact information in your birth plan. Share your plan with your provider and with hospital staff.
What happens in the first stage of labor?
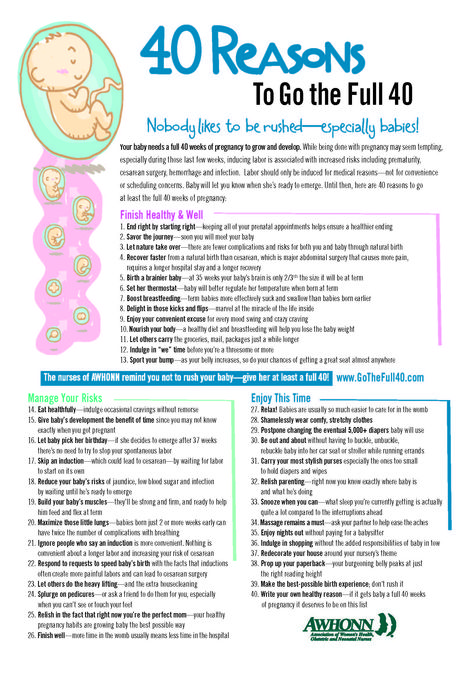
The first stage of labor is the longest stage. For first-time moms, it can last from 12 to 19 hours. It may be shorter (about 14 hours) for moms who’ve already had children. It’s when contractions become strong and regular enough to cause your cervix to dilate (open) and thin out (efface). This lets your baby move lower into your pelvis and into your birth canal (vagina). This stage of labor ends when you are 10 centimeters dilated. The first stage is divided into three parts: early labor, active labor and transition to stage 2 of labor.
This stage of labor ends when you are 10 centimeters dilated. The first stage is divided into three parts: early labor, active labor and transition to stage 2 of labor.
Early labor
For most first-time moms, early labor lasts about 6 to 12 hours. You can spend this time at home or wherever you’re most comfortable. During early labor:
- You may feel mild contractions that come every 5 to 15 minutes and last 60 to 90 seconds.
- You may have a bloody show. This is a pink, red or bloody vaginal discharge. If you have heavy bleeding or bleeding like your period, call your provider right away.
What you can do in early labor:
This is a great time for you to rely on your doula or labor support person. Try the methods you learned about in childbirth education classes about how to relax and cope with pain. During early labor:
- Rest and relax as much as you can.
- Take a shower or bath.
- Go for a walk.

- Change positions often.
- Make sure you’re ready to go to the hospital.
- Take slow, relaxing breaths during contractions.
Active labor
This is when you head to the hospital! Active labor usually lasts about 4 to 8 hours. It starts when your contractions are regular and your cervix has dilated to 6 centimeters. In active labor:
- Your contractions get stronger, longer and more painful. Each lasts about 45 seconds and they can be as close as 3 minutes apart.
- You may feel pressure in your lower back, and your legs may cramp.
- You may feel the urge to push.
- Your cervix will dilate up to 10 centimeters.
- If your water hasn’t broken, it may break now.
- You may feel sick to your stomach.
What you can do in active labor:
- Make sure the hospital staff has a copy of your birth plan.
- Try to stay relaxed and not think too hard about the next contraction.
- Move around or change positions. Walk the hallways in the hospital.
- Drink water or other liquids. But don’t eat solid foods.
- If you’re going to take medicine to help relieve labor pain, you can start taking it now. Your choice about pain relief is part of your birth plan.
- Go to the bathroom often to empty your bladder. An empty bladder gives more room for your baby’s head to move down.
- If you feel like you want to push, tell your provider. You don’t want to start pushing until your provider checks your cervix to see how dilated it is.
Transition to the second stage of labor
This can be the toughest and most painful part of labor. It can last 15 minutes to an hour. During the transition:
- Contractions come closer together and can last 60 to 90 seconds. You may feel like you want to bear down.
- You may feel a lot of pressure in your lower back and rectum. If you feel like you want to push, tell your provider.

What happens in the second stage of labor?
In the second stage of labor, your cervix is fully dilated and ready for childbirth. This stage is the most work for you because your provider wants you to start pushing your baby out. This stage can be as short as 20 minutes or as long as a few hours. It may be longer for first-time moms or if you’ve had an epidural. An epidural is pain medicine you get through a tube in your lower back that helps numb your lower body during labor. It's the most common kind of pain relief used during labor. The second stage ends when your baby is born.
During the second stage of labor:
- Your contractions may slow down to come every 2 to 5 minutes apart. They last about 60 to 90 seconds.
- You may get an episiotomy. This is a small cut made at the opening of the vagina to help let the baby out. Most women don't need an episiotomy.
- Your baby’s head begins to show. This is called crowning.
- Your provider guides your baby out of the birth canal. She may use special tools, like forceps or suction, to help your baby out.
- Your baby is born, and the umbilical cord is cut. Instructions about who’s cutting the umbilical cord are in your birth plan.
What you can do:
- Find a position that is comfortable for you. You can squat, sit, kneel or lie back.
- Push during contractions and rest between them. Push when you feel the urge or when your provider tells you.
- If you’re uncomfortable or pushing has stopped, try a new position.
What happens in the third stage of labor?
In the third stage of labor, the placenta is delivered. The placenta grows in your uterus and supplies your baby with food and oxygen through the umbilical cord. This stage is the shortest and usually doesn’t take more than 20 minutes.
During the third stage of labor:
- You have contractions that are closer together and not as painful as earlier.
 These contractions help the placenta separate from the uterus and move into the birth canal. They begin 5 to 30 minutes after birth.
These contractions help the placenta separate from the uterus and move into the birth canal. They begin 5 to 30 minutes after birth. - You continue to have contractions even after the placenta is delivered. You may get medicine to help with contractions and to prevent heavy bleeding.
- Your provider squeezes and presses on your belly to make sure the uterus feels right.
- If you had an episiotomy, your provider repairs it now.
- If you’re storing your umbilical cord blood, your provider collects it now. Umbilical cord blood is blood left in the umbilical cord and placenta after your baby is born and the cord is cut. Some moms and families want to store or donate umbilical cord blood so it can be used later to treat certain diseases, like cancer. Your instructions about umbilical cord blood can be part of your birth plan.
- You may have chills or feel shaky. Tell your provider if these are making you uncomfortable.
What happens after your baby is born?
Congratulations! It’s time to hold your baby! Right after birth your provider places your baby skin-to-skin on your chest and covers him with a blanket. Holding your baby skin-to-skin helps your baby stay warm as he gets used to being outside the womb. It’s also a great way to get started breastfeeding. You can start breastfeeding even within an hour of your baby’s birth. Even if you don’t plan to breastfeed, hold your baby skin-to-skin so you get to know each other right away. Your baby will welcome your gentle touch, and this closeness can help you and your baby bond.
Holding your baby skin-to-skin helps your baby stay warm as he gets used to being outside the womb. It’s also a great way to get started breastfeeding. You can start breastfeeding even within an hour of your baby’s birth. Even if you don’t plan to breastfeed, hold your baby skin-to-skin so you get to know each other right away. Your baby will welcome your gentle touch, and this closeness can help you and your baby bond.
After birth, your body starts to change to help you heal. Your provider takes your temperature and checks your heart and blood pressure to make sure you’re doing well. If you had anesthesia during labor, your provider makes sure you’re recovering without any complications.
Last reviewed: March, 2019
How to distinguish real contractions from training ones?
Shemyakina Natalya Nikolaevna, head of the obstetric department of the Leleka maternity hospital will help you figure it out.
Training contractions, or as they are also called, fake, or Braxton-Hicks contractions, are irregular contractions that do not have increasing intensity. The uterus may tone up, but normally, it should pass quickly.
The uterus may tone up, but normally, it should pass quickly.
For example, the tone appeared once in half an hour and the uterus relaxed rather quickly. Then the tone reappeared only after two hours and again passed. These are training contractions, they do not increase in intensity and do not become more frequent. nine0005
Training bouts are physiologically provided by our body. So the uterus is preparing to do the hard work in the process of childbirth. Normally, training contractions appear in terms of pregnancy close to childbirth - from the 37th week of pregnancy.
The appearance of training contractions in the early stages of pregnancy is not the norm
The uterus can tone up with an active lifestyle, physical activity, with a change in body position, but this tone should quickly pass. Normally, the uterus should not often come into tone. And even more so, contractions, as such, should not be until the 37th week of pregnancy. nine0015 Braxton Hicks contractions in the early stages are a threat of preterm labor. If a woman has contractions periodically during the day: after an hour, after 2, then again after an hour, (even if they are not regular), for periods up to 37 weeks, such a tone should alert the expectant mother.
If a woman has contractions periodically during the day: after an hour, after 2, then again after an hour, (even if they are not regular), for periods up to 37 weeks, such a tone should alert the expectant mother.
Because this is not the norm, but the threat of premature birth. This is an occasion to contact a specialist and change your rhythm of life, put on a bandage. The causes of premature birth are most often internal, caused by hormonal disorders and a violation of the physical health of a woman. But significant physical activity and stress can also cause premature birth. nine0005
Labor pains
Unlike training contractions, labor pains are regular. The uterus comes to tone first once every 15 minutes, and after a while - once every 7-10 minutes. Contractions gradually become more frequent, longer and stronger. And already occur every 5 minutes, then 3 and finally every 2 minutes.
True labor pains are contractions every 2 minutes, 40 seconds. If within an hour or two the contractions intensify - pains that begin in the lower abdomen or in the lower back and spread to the stomach - most likely, these are real labor pains. nine0005
nine0005
Training contractions are NOT so much painful as unusual for a woman. When the expectant mother sees how the stomach comes into tone, its shape changes and it becomes dense, like an inflated ball. This might scare you a little. But a woman must understand that in real, labor pains, there must be a clear periodicity, intensification and acceleration over a certain period of time. Real fights never stop, but practice fights do. The uterus then comes to tone, then relaxes. nine0015 Often women confuse contractions with tone, which is caused by other physiological processes in the body. For example, increased intestinal peristalsis, intestinal infections, colic, etc.
What else should alert a woman?! If within an hour or two the uterus periodically comes into tone and mucous, bloody (streaked with blood or brown) discharge appears, then most likely there are structural changes in the cervix - it opens. Also an important sign to seek help is the discharge of the mucous plug long before childbirth. Her departure in terms of childbirth, a week or two before childbirth is normal. nine0005
Her departure in terms of childbirth, a week or two before childbirth is normal. nine0005
Tracking labor pains
There are several methods for determining the types of contractions. A woman can do this herself, writing down the frequency and duration of contractions on paper or tracking them using special programs for a computer and phone. Or you can contact a doctor at antenatal clinic or at the maternity hospital, where a specialist will conduct fetal monitoring (fetal CTG). With the help of 2 sensors, the fetal heartbeat, uterine contractions are monitored and it is determined whether these are training contractions or labor. nine0005
When should I go to the maternity hospital?
If within an hour or two there is an increase and intensification of pain, its intensity increases, the frequency of contractions is clear and regular, you can go to the maternity hospital. A woman can make a mistake, but it’s better to come and make sure for sure whether these are labor or training contractions.
If the amniotic fluid breaks, you can slowly pack up and go to the maternity hospital. Since, normally, after this labor activity should begin.
The main thing is that a woman should not panic. nine0025 The latent phase of labor can last 8-10 hours until the cervix is fully dilated. Labor activity does not proceed in 30 seconds. In the process of labor, the cervix of the uterus in women giving birth for the first time opens about 1 cm in an hour. She needs to open up to 10 cm, that is, a woman has about 10:00 by the time the baby is born.
Happy pregnancy and childbirth!
Harbingers - childbirth is coming soon!
Wrestler Maria Vladimirovna nine0005
Obstetrician-gynecologist
MD GROUP Clinical Hospital, Mother and Child Clinic Savelovskaya
False contractions
They may appear after the 38th week of pregnancy. False contractions are similar to Braxton-Hicks contractions, which a woman could already feel starting from the second trimester of pregnancy (the uterus seems to stiffen for a few seconds - a couple of minutes, then the tension in it subsides). False contractions train the uterus before childbirth, they are irregular and painless, the intervals between them are not reduced. Real labor pains, on the contrary, are regular, their strength gradually increases, they become longer and more painful, and the intervals between them are reduced. That's when you can already say that the birth began for real. In the meantime, false contractions are going on, it is not necessary to go to the maternity hospital - you can easily survive them at home. nine0005
False contractions train the uterus before childbirth, they are irregular and painless, the intervals between them are not reduced. Real labor pains, on the contrary, are regular, their strength gradually increases, they become longer and more painful, and the intervals between them are reduced. That's when you can already say that the birth began for real. In the meantime, false contractions are going on, it is not necessary to go to the maternity hospital - you can easily survive them at home. nine0005
Abdominal prolapse
Approximately two to three weeks before birth, the baby, in preparation for birth, presses the presenting part (usually the head) against the lower part of the uterus and pulls it down. As a result, the uterus moves lower into the pelvic region, its upper part ceases to put pressure on the internal organs of the chest and abdominal cavity. In the people it is called - the stomach dropped. As soon as the stomach drops, the expectant mother notices that it has become easier for her to breathe, but, on the contrary, it becomes more difficult to sit and walk. Heartburn and belching also disappear (after all, the uterus no longer presses on the diaphragm and stomach). But, having dropped down, the uterus begins to put pressure on the bladder - naturally, urination becomes more frequent. nine0005
Heartburn and belching also disappear (after all, the uterus no longer presses on the diaphragm and stomach). But, having dropped down, the uterus begins to put pressure on the bladder - naturally, urination becomes more frequent. nine0005
For some, uterine prolapse causes a feeling of heaviness in the lower abdomen and even slight pain in the area of the inguinal ligaments. These sensations arise due to the fact that the child's head, moving down, irritates the nerve endings of the pelvic organs.
During the second and subsequent births, the belly drops later - just before the birth. It happens that this harbinger of childbirth is not at all.
Removal of the mucous plug
This is one of the main and obvious harbingers of childbirth. During pregnancy, the glands in the cervix produce a secret (it looks like a thick jelly and forms the so-called cork), which prevents various microorganisms from entering the uterine cavity. Before childbirth, under the influence of estrogens, the cervix softens, the cervical canal opens slightly and the cork can come out - the woman will see that there are mucus clots on the linen that look like jelly. Cork can be of different colors - white, transparent, yellowish-brown or pink-red. Often it is stained with blood - this is completely normal and may indicate that childbirth will occur within the next day. The mucus plug can come out all at once (at once) or come out piecemeal throughout the day. nine0005
Cork can be of different colors - white, transparent, yellowish-brown or pink-red. Often it is stained with blood - this is completely normal and may indicate that childbirth will occur within the next day. The mucus plug can come out all at once (at once) or come out piecemeal throughout the day. nine0005
Weight loss
Approximately two weeks before delivery, weight loss may occur, usually by 0.5–2 kg. This happens because excess fluid is removed from the body and swelling decreases. If earlier during pregnancy, under the influence of the hormone progesterone, fluid in the body of a pregnant woman accumulated, now, before childbirth, the effect of progesterone decreases, but other female sex hormones - estrogens - begin to work hard, they remove excess fluid from the body of the expectant mother. nine0005
In addition, the expectant mother often notices that at the end of pregnancy it became easier for her to put on rings, gloves, shoes - this means that swelling on the hands and feet has decreased.
Change of stool
Right before childbirth, hormones often act on the intestines - they relax its muscles, as a result, stool disorder begins. Sometimes such frequent (up to 2-3 times a day) and even loose stools are mistaken for an intestinal infection. But if there is no nausea, vomiting, discoloration and smell of feces, or any other symptoms of intoxication, you should not worry: this is one of the harbingers of the upcoming birth. nine0005
And on the eve of childbirth, you often don't feel like eating at all. All this is also the preparation of the body for natural childbirth.
Mood changes
Many women experience mood changes a few days before giving birth. The expectant mother gets tired quickly, she wants to have more rest, sleep, even some kind of apathy appears. This state is quite understandable - you need to gather strength to prepare for childbirth. Often, just before giving birth, a woman wants to retire, looking for a secluded place where you can hide and focus on yourself and your experiences.