Pregnancy safe anti itch cream
Is It Safe to Use Hydrocortisone Cream While Pregnant?
Pregnancy brings with itself numerous changes in a woman’s body which may lead to unwanted consequences. During pregnancy, your skin will stretch extensively to make way for an enlarging uterus and to accommodate the baby. However, this may result in an itching sensation and you may be tempted to itch your body parts, particularly your tummy. Hydrocortisone cream is an anti-itch cream that can provide you with some relief, however, topical application of hydrocortisone cream during pregnancy may not be the safest option.
What Is Hydrocortisone?
Hydrocortisone, cortisone, or hydrocortisone cream is a form of medication which has steroids in it, which helps treat certain skin conditions. This cream falls under the ‘C’ category of pregnancy-related medicines, which makes it harmful for the foetus, even in its lowest strength. This is the very reason why a doctor’s recommendation is highly required before using it.
For Which Skin Conditions Is Hydrocortisone Cream Used?
Hydrocortisone cream can provide relief from some skin problems like skin allergies, itching, redness, and rashes. And since this cream treats various skin conditions, it is a primary choice of medication, even among pregnant women. As the instances of suffering from eczema or dermatitis, along with swelling of the skin, redness, and rashes are high in pregnancy, and if a woman sweats during pregnancy, these skin problems might exacerbate. A woman might be tempted to use this cream if she experiences any skin problems; however, this cream should be used only after consulting with a doctor.
Is it Important to Consult a Doctor Before Using Cortisone Cream During Pregnancy?
Sometimes, a doctor might suggest hydrocortisone cream to a pregnant woman, depending on the condition of her pregnancy and the body part where the cream needs to be used. However, the application of any kind of topical corticosteroid should not be taken lightly. Although the hydrocortisone cream is available over-the-counter, it does not mean that you can use it on your tummy and breasts without consulting your doctor. If you have any skin problem during pregnancy, let your doctor examine your skin condition and recommend you a remedy accordingly. Chances are your doctor will suggest you a better alternative to hydrocortisone cream.
Although the hydrocortisone cream is available over-the-counter, it does not mean that you can use it on your tummy and breasts without consulting your doctor. If you have any skin problem during pregnancy, let your doctor examine your skin condition and recommend you a remedy accordingly. Chances are your doctor will suggest you a better alternative to hydrocortisone cream.
Can Using Cortisone Cream Be Harmful to the Foetus?
There is a high chance that hydrocortisone cream can prove to be harmful to the health of your baby. Drugs can easily find their way to the placenta once they enter the body. Usage of this cream in a higher strength for an extended duration can affect the development of the foetus.
Can You Use the Low-strength Hydrocortisone Cream?
Low-strength hydrocortisone cream is available without any prescription and can provide relief from itching and rashes. High-strength creams, on the other hand, can treat inflammation and skin problems and is usually prescribed by the doctor in case the condition is severe. However, neither is safe during pregnancy, so it best that you avoid using hydrocortisone cream.
However, neither is safe during pregnancy, so it best that you avoid using hydrocortisone cream.
Remedies for Itching
While there is no way to avoid the occurrence of itching during pregnancy, there are definitely some ways in which you can lower the intensity. Avoid using hot water while bathing. Similarly, replace your usual soap with a moisturizing one that is made from natural substances. For intense bouts of itching, an oatmeal bath is highly recommended. Also, wear clothes in which your skin can breathe and soak in sweat easily.
If you are not sure about using hydrocortisone cream during pregnancy, it is recommended that you consult a doctor whom you trust implicitly. In either case, try out natural alternatives to combat itching and choose the cream only when they fail to have a considerable effect.
References and Resources: Livestrong.com
Also Read: Is It Safe to Use Hair Removal Cream in Pregnancy?
The Safety Of Anti-Itch Creams During Pregnancy
Pregnancy
What medications can be used to reduce itching in pregnancy
Megha Trivedi, MD
AUTHOR
Raja Sivamani, MD MS AP
EDITOR
Some of us have dealt with itchiness our entire lives and have become masters at deciding which medications we can use to control those itching urges. However, whether or not you’ve had experience with itchiness, pregnancy can be a challenging time and many women have questions about medication safety when trying to control their symptoms. This article aims to give you the information you need about systemic (medications that get into the bloodstream) therapies for itch and their safety for a developing baby. Antihistamines are the major category of drugs which will be discussed.
However, whether or not you’ve had experience with itchiness, pregnancy can be a challenging time and many women have questions about medication safety when trying to control their symptoms. This article aims to give you the information you need about systemic (medications that get into the bloodstream) therapies for itch and their safety for a developing baby. Antihistamines are the major category of drugs which will be discussed.
Antihistamines can be divided into two major categories: first-generation and second-generation. The major difference is that the first-generation drugs have been around longer and have greater penetration into the circulation of the central nervous system. This means that they have greater sedative effects compared to second-generation agents (why many people feel sleepy after taking a medication with diphenhydramine). For the same reason, the first generation drugs are also used to control nausea and vomiting during pregnancy.[1] Some common first-generation agents include Diphenhydramine (ingredient in Benadryl), hydroxyzine (ingredient in Vistaril and Atarax), and chlorpheniramine (ingredient in Aller-Chlor, and Teldrin). Common second-generation agents include Loratadine (ingredient in Claritin), cetirizine (ingredient in Zyrtec), and fexofenadine (ingredient in Allegra).[2]
Common second-generation agents include Loratadine (ingredient in Claritin), cetirizine (ingredient in Zyrtec), and fexofenadine (ingredient in Allegra).[2]
Pregnancy Category B Antihistamines
Pregnancy category B indicates that there are very few human studies, if any, but animal studies do not show an increased risk of adverse effects on the fetus with use of the medication.
The first generation antihistamines - diphenhydramine and chlorpheniramine - and the second-generation antihistamines - loratadine and cetirizine - are considered pregnancy category B medications. The “Allergic Rhinitis and its Impact on Asthma” guidelines recommend using second-generation antihistamines over first-generations because of fewer sedative and other side effects in the general population.[3] However, it can be argued that first-generation agents are preferred during pregnancy since there is a greater amount of safety data published for these medications in pregnant women. [2]
[2]
Several large meta-analyses (combines the results of many reports/studies on one topic and presents the major conclusion) on safety data of antihistamine use in pregnancy have concluded there is no definitive risk of an increased rate of birth defects or other adverse fetal outcomes compared to the general population. Overall, these reports have indicated the relative safety of these medications in pregnancy. One recent large report that included 32 individual studies stated no significant correlation between antihistamine use and fetal malformations, prematurity, spontaneous abortions, low birth weight, or stillbirths. This report went on to further state that 3 cases in which expectant mothers were accidentally exposed to overdoses of medication did not result in any adverse fetal outcomes.[4]
Current recommendations are that first-generation antihistamines are preferred over second-generation agents in pregnant women. However, care should be used with all antihistamines in the third trimester close to the time of birth. IV antihistamines and high doses should be avoided especially during this time, as they are known to stimulate uterine contractions which can result in lack of oxygen to the baby (especially diphenhydramine). Of the second-generation medications, loratadine should be used before trying cetirizine.[2]
IV antihistamines and high doses should be avoided especially during this time, as they are known to stimulate uterine contractions which can result in lack of oxygen to the baby (especially diphenhydramine). Of the second-generation medications, loratadine should be used before trying cetirizine.[2]
In terms of lactation safety, diphenhydramine and cetirizine are considered L2 (safer), but the baby should be monitored for effects of sedation. Chlorpheniramine is L3 (moderately safe), and again the baby should be monitored for excessive sedation. Loratadine is considered L1 (safest), but the baby should be monitored for effects of sedation, fast heart rate, and dry mouth.[2]
Pregnancy Category C Antihistamines
Pregnancy category C includes medications for which there is no human data, and animal studies do not exist or show adverse effects to the fetus.
This category includes the first-generation antihistamine, hydroxyzine, and the second-generation antihistamine, fexofenadine.
Care should be used when using these agents during pregnancy, as there have been reports of adverse fetal outcomes in human reports and/or animal studies with both medications. High doses of hydroxyzine use in pregnant mothers have been associated with withdrawal symptoms in newborns, including tonic-clonic seizures in one report. Currently, hydroxyzine is not prescribed to pregnant women by allergists.[5] There is limited data on the use of fexofenadine in pregnant women, but a few reports have correlated its use with low birth weight in animal studies. Since there is very little known about this drug, it is not recommended as a first-line agent in pregnant women with an itch.[5]
Hydroxyzine is L1 in lactation safety (safest), but the baby should be monitored for sedation, dry mouth, and high heart rate. Fexofenadine is L2 (safer), and the baby should be monitored for sedation.[2]
A Word About Oral Doxepin
This drug is known as tricyclic antidepressant, and its original use was to treat depression and sleep disorders. However, it has also been found to be useful in the treatment of itch. No animal studies have demonstrated fetal malformations or adverse fetal side effects with the use of this drug. This being said, there are very few, if any, human studies evaluating this drug during pregnancy. There has been one report of polydactyly, heart defects, and oral cleft abnormalities correlated with maternal exposures to the medication in the first trimester. It is recommended to use antihistamines before attempting to use this medication to control the itch. This drug should especially be avoided in the third trimester due to the risk of reduced muscle tone, vomiting, and weak suck in the newborn.[2]
However, it has also been found to be useful in the treatment of itch. No animal studies have demonstrated fetal malformations or adverse fetal side effects with the use of this drug. This being said, there are very few, if any, human studies evaluating this drug during pregnancy. There has been one report of polydactyly, heart defects, and oral cleft abnormalities correlated with maternal exposures to the medication in the first trimester. It is recommended to use antihistamines before attempting to use this medication to control the itch. This drug should especially be avoided in the third trimester due to the risk of reduced muscle tone, vomiting, and weak suck in the newborn.[2]
In terms of lactation safety, it is considered L5 (contraindicated), as this drug is thought to be secreted in breast milk and can cause an infant to experience breathing difficulties, loss of muscle tone, decreased suckling and vomiting.[6]
* This Website is for general skin beauty, wellness, and health information only. This Website is not to be used as a substitute for medical advice, diagnosis or treatment of any health condition or problem. The information provided on this Website should never be used to disregard, delay, or refuse treatment or advice from a physician or a qualified health provider.
This Website is not to be used as a substitute for medical advice, diagnosis or treatment of any health condition or problem. The information provided on this Website should never be used to disregard, delay, or refuse treatment or advice from a physician or a qualified health provider.
References
- Gilboa SM, Ailes EC, Rai RP, et al.: (2014). Antihistamines and birth defects: A systematic review of the literature. Expert Opinion on Drug Safety, 13(12):1667–98. PMID: 25307228
- Murase JE, Heller MM, Butler DC. (2014). Safety of dermatologic medications in pregnancy and lactation: Part I. Pregnancy. Journal of the American Academy of Dermatology, 70(3):401-e1. PMID: 24528911
- Ridolo E, Caminati M, Martignago I, et al.: (2016). Allergic rhinitis: pharmacotherapy in pregnancy and old age. Expert Review in Clinical Pharmacology, 9(8):1081–9. PMID: 27177184
- Etwel F, Faught LH, Rieder MJ, et al.: (2016). The Risk of Adverse Pregnancy Outcome After First Trimester Exposure to h2 Antihistamines: A Systematic Review and Meta-Analysis.
 Drug Safety, 22:1-2. PMID: 27878468
Drug Safety, 22:1-2. PMID: 27878468 - Gonzalez-Estrada A, Geraci SA. (2016). Allergy Medications During Pregnancy. American Journal of the Medical Sciences, 352(3):326-3. PMID: 27650241
- Frey OR, Scheidt P, von Brenndorff AI. (1999). Adverse effects in a newborn infant breast-fed by a mother treated with doxepin. Annals of Pharmacotherapy, 33(6):690-3. PMID: 10410181
Share
Itchy skin during pregnancy: causes and remedies
Itching of the skin during pregnancy can be psychogenic. In this case, itching is a consequence of stress, an early symptom of multiple sclerosis.
In the early stages, itching occurs due to loss of skin elasticity caused by hormonal changes and excessive dryness of the skin. In the second and third trimester, the reasons may be the rapid weight gain of the expectant mother, the developing stretching of the skin of the abdomen as it increases. nine0003
Some expectant mothers experience intimate itching. It is provoked by genital infections, urological and proctological diseases.
It is provoked by genital infections, urological and proctological diseases.
The causes of itching of the skin also include dermatoses of pregnant women (atopic dermatitis, cholestasis of pregnancy). They are provoked by a hereditary predisposition, a decrease in immunity, physiological changes (stretching of the skin with damage to the connective tissue).
Atopic dermatitis is the most common cause of itching during pregnancy. A specific condition is caused by hormonal immune restructuring of the whole organism. In 80% of cases, the disease manifests itself exclusively during pregnancy, and all signs disappear after childbirth without specific treatment. nine0003
Atopic dermatitis is more common in nulliparous women in the early stages and in the second trimester. Itching is caused by papular and exametic rashes localized on the face, neck, limbs, elbows, palms.
Atopic dermatitis is the most benign form of dermatosis of pregnancy and usually does not adversely affect the fetus. However, children born to mothers who suffered from this disease at the stage of gestation are also prone to allergic skin diseases. nine0003
However, children born to mothers who suffered from this disease at the stage of gestation are also prone to allergic skin diseases. nine0003
Itching of the skin, as a symptom of cholestasis, is provoked by intrahepatic stagnation of bile as a reaction to increased estrogen production. The disease occurs at the end of the second - beginning of the third trimester, closer to the date of birth. A pregnant woman experiences severe itching in the abdomen, back, palms, legs.
Cholestasis is dangerous for the health of the mother and unborn child in severe cases of the disease. There is a risk of fetal hypoxia, delayed development and even premature birth. nine0003
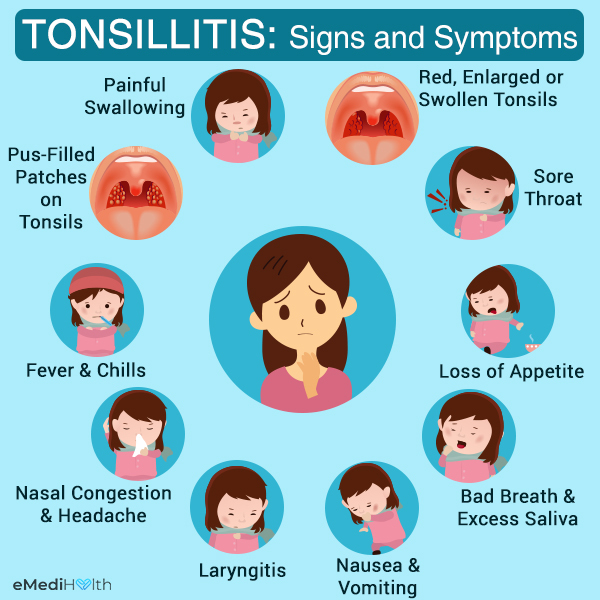
Symptoms
The main sign of pathological changes is the appearance of irritating-itchy sensations in different parts of the body. Locally, a woman may also feel a tingling and burning sensation.
Other symptoms include:
- blistering or eruption of blistering character;
- peeling, irritation and redness of the skin;
- formation of scaly spots;
- sores and sores caused by scratching; nine0028
- deterioration of general condition caused by sleep disorders and emotional depression.

In most cases, itching of the skin during pregnancy does not pose a real danger to the intrauterine development of the fetus, but significantly worsens the quality of life of the expectant mother, acts depressingly on the state of her nervous system and general well-being.
Diagnostics
In order to successfully deal with itching, it is necessary to establish the cause that causes it. The choice of diagnostic methods is determined based on the degree of intensity and localization of itching, the presence of concomitant symptoms and chronic diseases, the duration of pregnancy, and the individual characteristics of the health of the expectant mother. nine0003
Treatment is prescribed only after the exact cause of the itching is established.
At the initial examination, the doctor listens to the patient's complaints, examines the condition of the skin, paying attention to the appearance of rashes or spots. This allows you to draw a preliminary conclusion and determine what laboratory tests and instrumental studies will be needed.
The main diagnostic measures for itchy skin in pregnant women include: nine0003
- general urine and blood tests;
- biochemical blood test;
- studies of hormone levels - if endocrine pathologies are suspected;
- analysis of vaginal smear for microflora;
- skin scraping examination;
- allergy testing;
- Ultrasound of the digestive tract, liver and kidneys;
- histological examination;
- analysis of feces for the detection of helminth eggs. nine0028
The choice of research methods is determined individually. In some cases, a pregnant woman is shown a consultation with an endocrinologist, urologist, gastroenterologist, venereologist.
Identification of atopic dermatitis is usually not difficult. In addition to the general examination, such types of diagnostics as dermatoscopy and examination under the Voodoo lamp are carried out.
If itching in a pregnant woman is allergic in nature, a mandatory diagnostic measure is the determination of the allergen (pathogen). nine0003
nine0003
Treatment of itching
Although itching during pregnancy is not dangerous in many cases, it should not be tolerated either. You need to tell the gynecologist about unpleasant sensations, who will determine the diagnostic methods and, if necessary, give a referral to other specialists. Treatment of itching during pregnancy is carried out by the attending gynecologist together with a dermatologist.
You can not self-medicate and use medicines without the approval of a doctor. Many of them have contraindications and can cause severe side effects. A pregnant woman should remember the prohibition of scratching itchy places. This leads to a violation of the integrity of the skin, the appearance of wounds and abrasions, which will become sites of infection. nine0003
The treatment regimen depends on the disease that causes itching. When choosing drug therapy, the risks of negative effects on the fetus are taken into account. This is especially true in the case of the appointment of antibiotics, hormonal and antifungal drugs. Self-medication is unacceptable!
Self-medication is unacceptable!
In the treatment of itching during pregnancy, the following types of drugs can be prescribed:
- antihistamines - to eliminate itching caused by dermatitis, urticaria; nine0028
- glucocorticoids - used to treat dermatitis;
- emollients - have a moisturizing and regenerating effect in case of excessive dryness and dehydration of the skin;
- adsorbents and hepatoprotectors - to normalize the liver;
- choleretic preparations - for the correction of the state of the digestive tract;
- sedatives - to normalize the state of the nervous system, if a pregnant woman has signs of increased anxiety and sleep disturbances. nine0028
With moderate itching, a pregnant woman is shown taking baths with a decoction of a string or oatmeal. An oatmeal bath is effective for itching caused by stretch marks, eczema, or psoriasis. To prepare it, crushed oatmeal is mixed with baking soda and a little milk is added, the mixture is poured into a warm bath.
Lotions on herbal decoctions can be applied to itchy areas of the skin. Chamomile, succession or St. John's wort is poured with boiling water and insisted. After a few hours, the decoction for lotions is ready for use. nine0003
To eliminate itching of the genital organs, medicinal suppositories with local action are prescribed. Of great benefit are sitz baths of decoctions of sage or chamomile.
Itching in the abdomen, caused by skin tension, can cause stretch marks. To prevent aesthetic imperfections, it is necessary to moisturize the skin with special means.
To reduce itching, a pregnant woman should only wear clothes made from natural fabrics, preferably cotton. Natural fabrics allow the skin to breathe freely. It is useful for future mothers to take a cool shower without the use of soaps or bathing gels. The skin needs to be effectively protected from external aggressive factors: sun, frost and wind. nine0003
When itching of the skin appears, it is better to refuse the use of perfumes, take the choice of cosmetics very responsibly.
Prophylaxis
Itching during pregnancy can be prevented if you follow the doctor's recommendations and preventive measures. Tips for expectant mothers:
- carefully observe body hygiene, take a regular shower or bath without the use of fragrances;
- refuse underwear and clothes made of synthetic fabrics; nine0028
- after taking a shower or bath, moisturize the skin of the body with special products, with a neutral pH level, creams, lotions, emulsions are suitable for this;
- use phosphate-free laundry detergents;
- wear loose clothing that does not restrict movement;
- avoid stuffy rooms or open places under the scorching summer sun;
- exclude intense physical activity that provokes increased sweating; nine0028
- provide the expectant mother with a plentiful drinking regimen that prevents dehydration of the body;
- avoid stressful situations, get positive impressions.
Proper nutrition plays an important role in the prevention of itching of the skin. This is especially important if itching is provoked by various foods. The woman is recommended a hypoallergenic diet, with the exception of fast food, smoked, salty and pickled foods, as well as foods with preservatives, emulsifiers and artificial flavors. The diet of the future mother should be rich in vitamins, minerals, fatty acids, antioxidants. To do this, the menu includes sour-milk products, meat and fish of low-fat varieties, vegetable dishes, fruits. nine0003
This is especially important if itching is provoked by various foods. The woman is recommended a hypoallergenic diet, with the exception of fast food, smoked, salty and pickled foods, as well as foods with preservatives, emulsifiers and artificial flavors. The diet of the future mother should be rich in vitamins, minerals, fatty acids, antioxidants. To do this, the menu includes sour-milk products, meat and fish of low-fat varieties, vegetable dishes, fruits. nine0003
Itching during pregnancy when following medical recommendations has a favorable prognosis and is not an obstacle to natural childbirth.
If a woman had signs of atopic dermatitis during her first pregnancy, the likelihood of a recurrence of the disease during subsequent pregnancies is high. At the stage of planning a child, it is necessary to visit a dermatologist.
Itching
A series of products "Emolium" effectively eliminates the symptoms of skin diseases, including itching, peeling, irritability.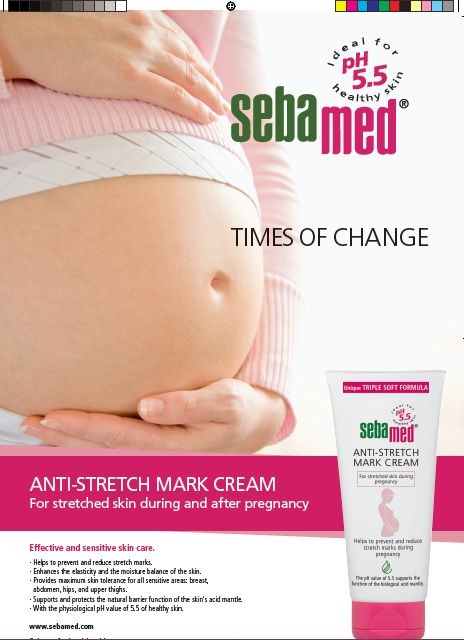 They are prescribed to moisturize the skin, eliminate dryness and tightness in atopic dermatitis, psoriasis, eczema, and allergies. Means of the Emolium series are used in the complex treatment of these and other diseases that provoke itching. nine0003
They are prescribed to moisturize the skin, eliminate dryness and tightness in atopic dermatitis, psoriasis, eczema, and allergies. Means of the Emolium series are used in the complex treatment of these and other diseases that provoke itching. nine0003
The main advantages of the series:
- have a mild anti-inflammatory effect;
- ensure the normal functioning of the skin;
- restore the structure of the skin;
- retain moisture in cells and intercellular space;
- restore the water-lipid layer;
- relieve irritation and itching.
The delicate and delicate consistency of the products makes it easy to apply and distribute them over the entire surface of the affected areas. nine0003
With severe itching of pregnant women, a triactive series is recommended, taking care of atopic and damaged skin. Triactive cream enriched with rapeseed oil and sodium hyaluronate has anti-inflammatory, antibacterial and antipruritic effects. The tool also provides an analgesic effect and additional protection against infection. The cream is applied twice a day after bathing.
The tool also provides an analgesic effect and additional protection against infection. The cream is applied twice a day after bathing.
For bathing use triactive emulsion "Emolium". It effectively and at the same time gently cleanses the skin, saturating them with fatty acids and vitamins. The emulsion is used during the period of exacerbation of psoriasis, atopic dermatitis and other diseases that cause itching and irritation. nine0003
Ecofucin for the treatment of thrush during pregnancy.
Thrush is a disease of the vaginal and vulvar mucosa caused by yeast-like fungi of the genus Candida, which affects 35% of women during pregnancy 1 .
At risk for the occurrence of a recurrent form of thrush are those pregnant women who have already had episodes of thrush in their anamnesis the level of estrogens rises, in connection with which glycogen accumulates in the vaginal mucosa - a nutrient medium for yeast-like fungi of the genus Candida. nine0003
Lactobacillus is the predominant microorganism in the vaginal microflora of a healthy woman. A normal concentration of lactobacilli provides the necessary acidity in the vagina, which inhibits the growth of fungi. Lactobacilli also participate in the formation of local immunity
A normal concentration of lactobacilli provides the necessary acidity in the vagina, which inhibits the growth of fungi. Lactobacilli also participate in the formation of local immunity
In addition, during thrush, the vaginal microflora is disturbed - the number of lactobacilli decreases sharply. These changes lead to the growth and reproduction of pathogenic fungi of the genus Candida, which leads to an increase in the number of manifestations of acute and recurrent forms of thrush. nine0003
Symptoms of thrush in a pregnant woman:
- itching and burning in the vulva and/or vagina, swelling and irritation in the vulva
- vaginal discharge of a "curdled character", sometimes with an unpleasant odor
- pain during and after intercourse
- urination disorder and pain
The appearance of at least one of the symptoms is a reason for an unscheduled visit to the doctor. nine0003
Why is it important to diagnose and treat thrush in a pregnant woman in time?
Some women are asymptomatic carriers of yeast-like fungi of the genus Candida and do not experience any discomfort or manifestation of the disease throughout the entire period of pregnancy 2
A pregnant woman with thrush (including an asymptomatic carrier) is a source of infection for her unborn child. Infection from mother to child occurs in 75-80% of cases 3 . Infection of a newborn occurs when passing through the birth canal (the skin of the child comes into contact with the infected mucous membranes of the mother's birth canal). In newborns, candidiasis is manifested by lesions of the mucous membranes and skin 2 , which can lead to negative consequences. For premature babies, infection with Candida is especially dangerous 2 .
Infection from mother to child occurs in 75-80% of cases 3 . Infection of a newborn occurs when passing through the birth canal (the skin of the child comes into contact with the infected mucous membranes of the mother's birth canal). In newborns, candidiasis is manifested by lesions of the mucous membranes and skin 2 , which can lead to negative consequences. For premature babies, infection with Candida is especially dangerous 2 .
Timely and effective treatment of thrush in a pregnant woman is an important task
Treatment of thrush
Safety and efficacy are the main criteria for choosing a drug in the treatment of thrush in pregnant women
The earlier a pregnant woman is diagnosed and treated for thrush, the less the risk of negative consequences and complications for the course of pregnancy and for the health of the mother and her unborn child. In the treatment of thrush, experts recommend an integrated approach to therapy.
It is important to follow the recommendations of a specialist, following the prescribed dosages and regimen. nine0003
Comprehensive treatment should be aimed at solving two problems: eliminating the cause of thrush (fungi of the genus Candida) and restoring the vaginal microflora. It is important to know that not all drugs are approved for use during pregnancy. For example, most oral (systemic) drugs and some topical drugs for treating thrush are contraindicated during pregnancy.
Ecofucin
® in the treatment of thrush in pregnancyEcofucin
® is allowed at all stages of pregnancy and lactation 4
Natamycin
- practically is not absorbed into the blood and has no systemic effect
- has fungicidal action - causes fungal cell death
- resistance to it does not develop
- does not inhibit the growth of natural microflora
+
Prebiotic 5
- is actively fermented by the normal microflora of the vagina, stimulates the growth of lactobacilli 6
- causes restoration of the vaginal microflora, stimulates local immunity 6
The active substance 7 of the drug Ecofucin ® eliminates the cause of thrush, and the prebiotic 5 in the preparation Ecofucin ® helps to restore the vaginal microflora and strengthen local immunity 6 .
Efficacy and safety of the drug Ecofucin proven by clinical studies
Ecofucin promotes faster recovery of patients with thrush. nine0003
More details
For pregnant women
Moscow 40 patients
For non-pregnant women
St. Petersburg 36 patients
Clinical cure occurred significantly earlier in the group of patients who used Ecofucin.
Kuzmin V.N., Bogdanova M.N. Ecofucin® is the first drug for the eradication of Candida fungi with the effect of stimulating the growth of lactobacilli in pregnant women. breast cancer. 2020; one; 28-33
Ecofucin increases the number of own lactobacilli in the vagina and reduces the risk of recurrence of thrush. nine0003
More details
For pregnant women
Moscow 40 patients
For non-pregnant women
St. Petersburg 36 patients
Clinical cure occurred significantly earlier in the group of patients who used Ecofucin.
Kuzmin V.N., Bogdanova M.N. Ecofucin® is the first drug for the eradication of Candida fungi with the effect of stimulating the growth of lactobacilli in pregnant women. breast cancer. 2020; one; 28-33
Dosage and Administration
The regimen for the use of Ecofucin ® in a pregnant woman is prescribed by the attending physician individually.
Additional conditions for effective treatment of thrush are: giving up bad habits, a diet with carbohydrate restriction, wearing underwear made from natural fabrics, etc.
It is important to consult a gynecologist in a timely manner and exclude self-medication.
1. Tikhomirov A.L., Sarsania S.I. Features of candidal vulvovaginitis in pregnant women at the present stage. // Farmateka No. 9, 2009, p. 64-70.
2. Prilepskaya V.N., Mirzabalaeva A.K., Kira E.F., Gomberg M.A., Apolikhina I.A., Bairamova G.R. Federal clinical guidelines "Urogenital candidiasis".