Can i have a natural birth with gestational diabetes
Gestational Diabetes | Yale Health
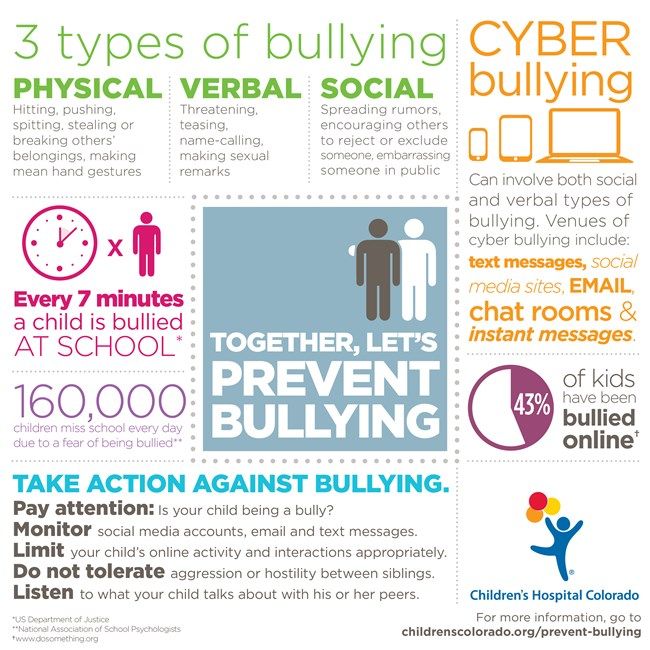
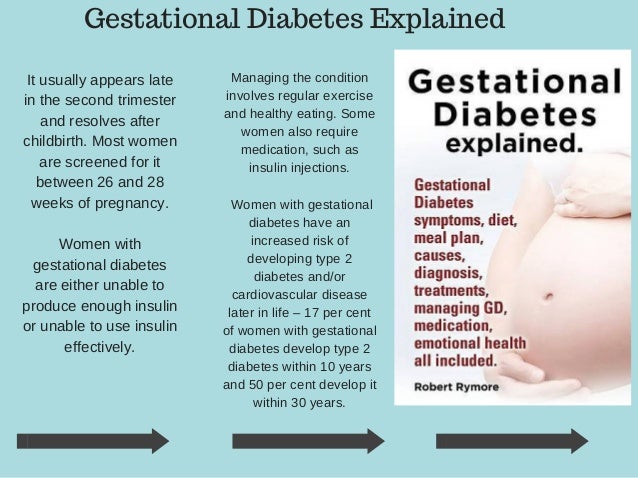
Gestational diabetes (pronounced jess-TAY-shun-ul die-uh-BEET-eez) is one of the most common health problems for pregnant women. It affects about 5 percent of all pregnancies, which means there are about 200,000 cases each year. If not treated, gestational diabetes can cause health problems for mother and fetus.
The good news is that gestational diabetes can be treated, especially if it is found early in the pregnancy. There are some things that women with gestational diabetes can do to keep themselves well and their pregnancies healthy. Controlling gestational diabetes is the key to a healthy pregnancy. and can be achieved by following the Gestational Diabetes Treatment Plan.
Gestational Diabetes is a kind of diabetes that only pregnant women get. In fact, the word gestational means “during pregnancy.” If a woman gets diabetes or high blood sugar when she is pregnant, it is gestational diabetes.
Diabetes
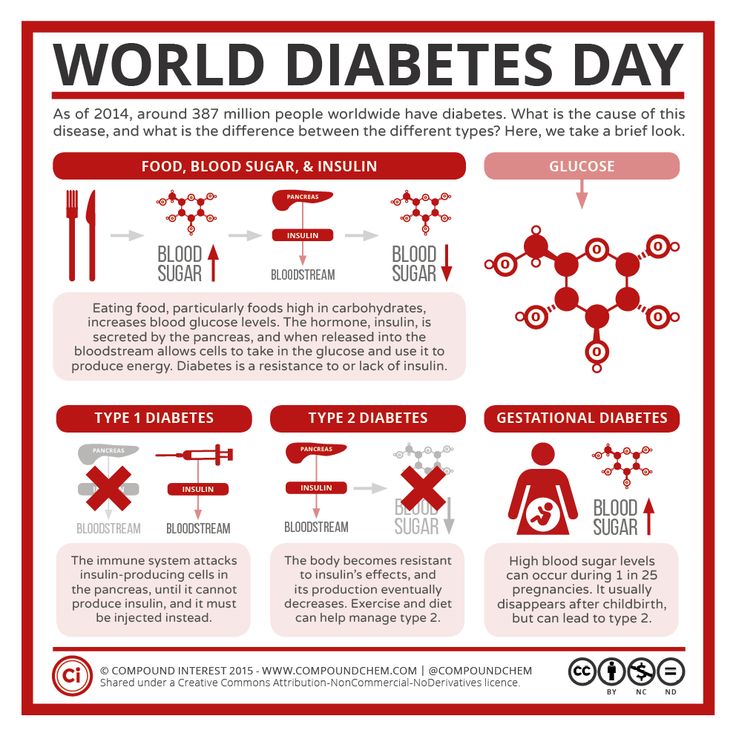
Diabetes means your blood sugar is too high. Diabetes is a disease of metabolism, which is the way your body uses food for energy and growth. Your stomach and intestines break down (or digest) much of the food you eat into a simple sugar called glucose (pronounced GLOO-kos). Glucose is your body’s main source of energy.
After digestion, the glucose passes into your bloodstream, which is why glucose is also called blood sugar. Once in the blood, the glucose is ready for your body cells to use. However, your cells need insulin (pronounced IN-suh-lin), a hormone made by your body, to get the glucose. Insulin “opens” your cells so that glucose can get in. When your metabolism is normal, your body makes enough insulin to move all the glucose smoothly from your bloodstream into your cells.
If you have diabetes, your body does not make enough insulin and your cells can’t use insulin properly. This causes the glucose to builds up in your bloodstream.
This causes the glucose to builds up in your bloodstream.
The Difference Between Diabetes and Gestational Diabetes
Only pregnant women get gestational diabetes. When you are pregnant, your body goes through many changes that can make it difficult for your insulin to work properly. Your body cannot get the sugar out of your blood and into your cells to use for energy as well as it did before.
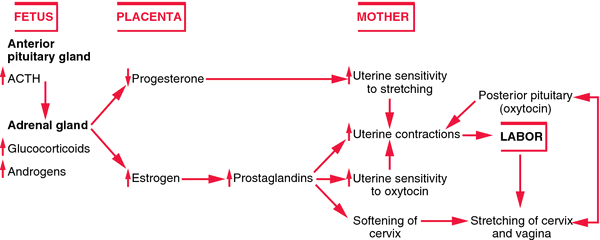
The placenta, a system of vessels that passes nutrients, blood, and water from mother to fetus, makes certain hormones that prevent insulin from working correctly. This is insulin resistance. Your body has to make three times its normal amount of insulin or more to overcome the hormones made by the placenta.
For most women, the body’s extra insulin is enough to keep their blood sugar levels in the healthy range. For about 5 percent of pregnant women, even the extra insulin is not enough to keep their blood sugar level normal. Testing for gestational diabetes is done between the 24th and 28th week of pregnancy.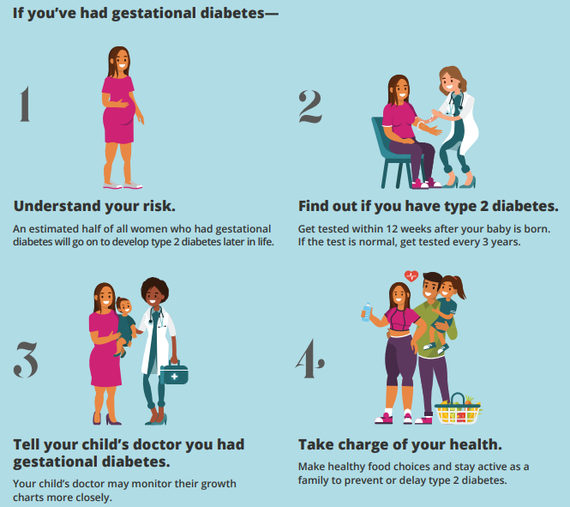
Will gestational diabetes hurt my baby?
If not treated, gestational diabetes can lead to health problems. The best way to promote a healthy pregnancy if you have gestational diabetes is to follow the treatment plan outlined by your health care provider.
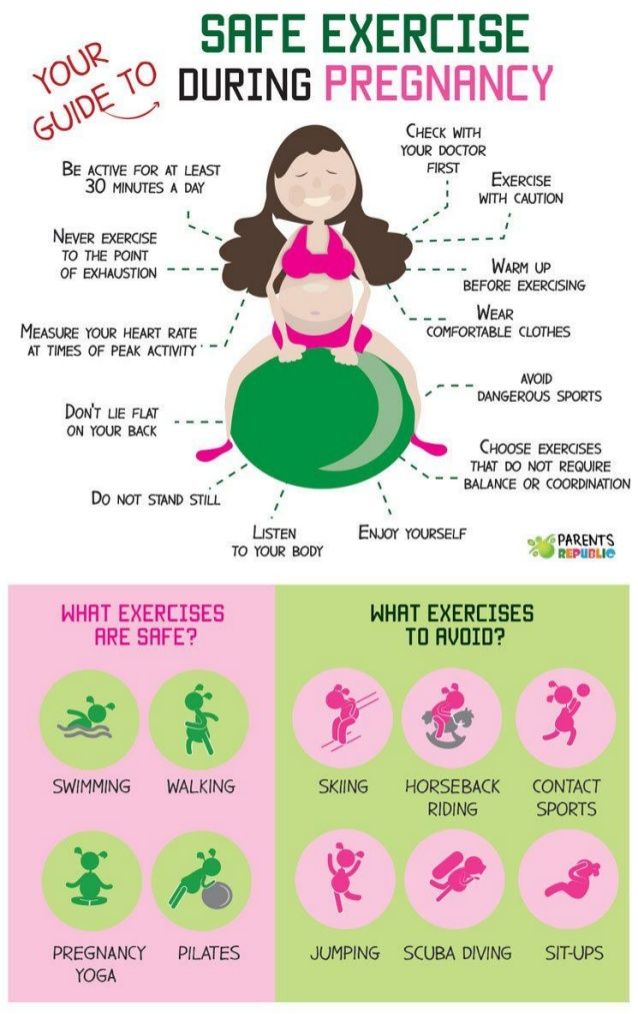
Most women who have gestational diabetes give birth to healthy babies, especially when they keep their blood sugar under control, eat a healthy diet, get regular, moderate physical activity, and gain the right amount of weight. In some cases, though, the condition can affect the pregnancy.
Keeping glucose levels under control may prevent certain problems related to gestational diabetes.
Below are some conditions that can result from your having gestational diabetes. Keep in mind that just because you have gestational diabetes does not mean that these problems will occur.
Macrosomia (pronounced mak-row-SOHM-ee-uh)—Baby’s body is larger than normal. Large-bodied babies can have difficulty by natural delivery through the vagina; the baby may need to be delivered through cesarean section.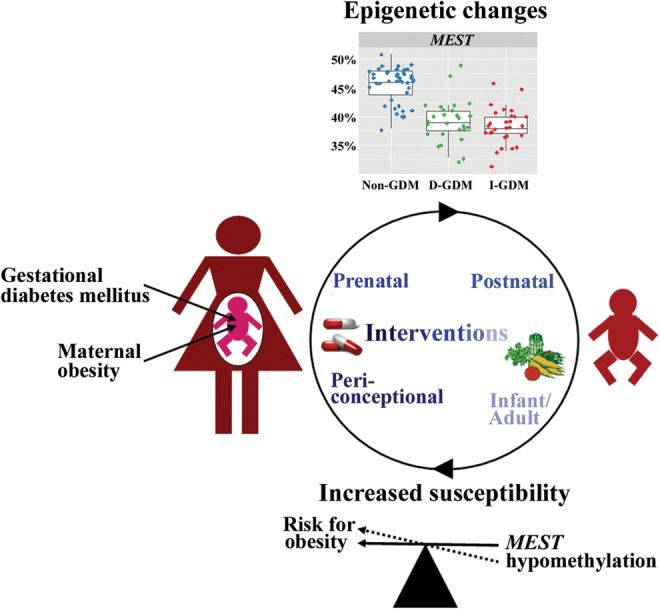 The most common complication for these babies is shoulder dystocia (pronounced dis-TOE-shee-uh).
The most common complication for these babies is shoulder dystocia (pronounced dis-TOE-shee-uh).
Hypoglycemia (pronounced high-po-gl-eye-SEEM-ee-uh)—Baby’s blood sugar is too low. You may need to start breastfeeding right away to get more glucose into the baby’s system. If it is not possible for you to start feedings, the baby may need to get glucose through a thin, plastic tube in his or her arm that puts glucose directly into the blood.
Jaundice (pronounced JAWN-diss)—Baby’s skin turns yellowish; white parts of the eyes may also change color slightly. If treated, jaundice is not a serious problem for the baby.
Respiratory Distress Syndrome (RDS)—Baby has trouble breathing. The baby might need oxygen or other help breathing if he or she has RDS.
Low Calcium and Magnesium Levels in the Baby’s Blood—Baby could develop a condition that causes spasms in the hands and feet, or twitching or cramping muscles.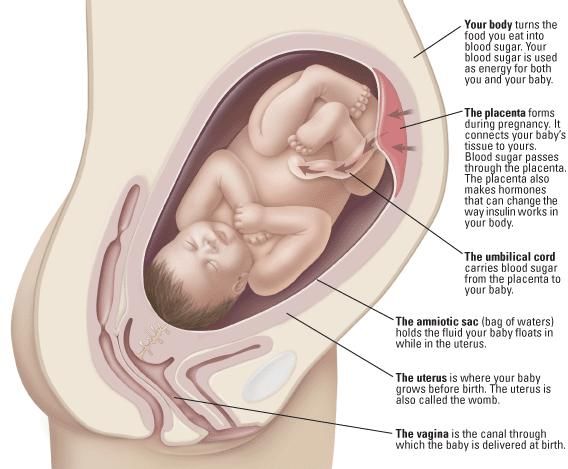 This condition can be treated with calcium and magnesium supplements.
This condition can be treated with calcium and magnesium supplements.
Will gestational diabetes affect my labor and delivery?
Most women with gestational diabetes can make it to their due dates safely and begin labor naturally. In some cases, though, gestational diabetes could change the way you feel or how your baby is delivered. Having gestational diabetes does not mean that you will have any change in delivery.
If you have gestational diabetes, there are things you should know about delivery:
- Blood Sugar and Insulin Balance—keeping your blood sugar level under control during labor and delivery is vital to your own health and to your baby’s health. If you do not take insulin during your pregnancy, you probably will not need it during labor or delivery. If you do take insulin during your pregnancy, you may receive an insulin shot when labor begins, or you may get insulin through a thin, plastic tube in your arm that goes into your bloodstream during labor.
- Early Delivery—Gestational diabetes puts women at higher risk than women without the condition for developing preeclampsia (pronounced pree-ee-KLAMP-see-uh), late in their pregnancies. Preeclampsia is a condition related to a sudden blood pressure increase; it can be a serious. The only way to cure preeclampsia is to deliver the baby; but delivery may not be the best option for your health or for the health of the baby. Your health care provider will keep you under close watch, possibly at the hospital, and will run multiple tests to determine whether early delivery is safe and needed. Your health care provider will give you more information about early delivery, should it be necessary.
- Cesarean Delivery—This is a type of surgery used to deliver the baby, instead of natural delivery through the vagina. Cesarean delivery is also called a cesarean section, or “C” section. Simply having gestational diabetes is not a reason to have a C section, but your health care provider may have other reasons for choosing a cesarean delivery, such as changes in your health or your baby’s health during labor.

Will I have diabetes after I have my baby?
Once you have the baby, your body should be able to use its insulin more effectively. Shortly after the baby is born, the placenta is “delivered.” (This is sometimes called the afterbirth.) Because the placenta causes insulin resistance, when it’s gone, gestational diabetes usually goes away, too.
If you have gestational diabetes, you are at higher-than-normal risk for developing type 2 diabetes later in your life. Type 2 diabetes, like gestational diabetes, occurs when the body doesn’t use its insulin properly.
Eating a healthy diet, keeping your weight within a healthy range and getting regular physical activity after your baby is born can help lower your risk for type 2 diabetes.
Who can I go to for help with gestational diabetes?
Women who have gestational diabetes benefit most from a team approach, which may include management and treatment of the condition. Your team may include obstetricians, advanced practice nurses, registered nurses, a registered dietitian and certified diabetes educator.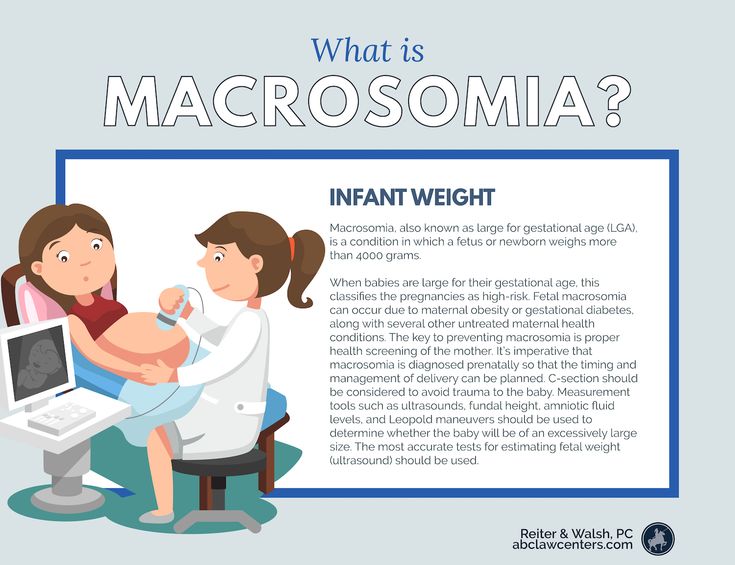
Gestational diabetes and giving birth
Planning the birth
There are some risks associated with giving birth if you have gestational diabetes. Your healthcare professionals should explain your options for giving birth before you make your birth plan.
If your ultrasound scans have shown that your baby is large, you may be advised to have an early induction (starting labour artificially) or planned caesarean section. Even if you’ve had a caesarean section before, you may still be able to give birth vaginally if you want to.
Your team may advise you to give birth in a hospital. This is because it has all the facilities needed to look after you and your baby during and after labour.
If you have any other health problems, such as being overweight or any spinal nerve‑related problems, you may be advised to see an anaesthetist. They can talk to you about the different methods of pain relief suitable for you during the birth.
When to have your baby
If your pregnancy goes on for too long, it may increase the risk of problems for you and your baby.
If you live in England and Wales, you will be advised to have your baby before 41 weeks. If you don’t go into labour naturally by then, you will be offered an induction or advised to have a planned caesarean section. You may be advised to have your baby earlier than this if you have complications, such as high glucose levels, high blood pressure or a big or small baby.
In Scotland, most women with diabetes in pregnancy are advised to have labour induced within 40 weeks.
If your labour starts before 37 weeks
If you go into labour early, you may also be given medication to help your baby’s lungs develop.
If you’re on insulin and have steroids, your insulin dose will be increased and your glucose levels will be closely monitored. This is because steroids can raise your blood glucose.
Monitoring during labour
It’s important that your glucose levels stay in the target range during labour. This will prevent your baby’s glucose getting low in the first few hours after they’re born. This is known as transient neonatal hypoglycaemia.
This is known as transient neonatal hypoglycaemia.
When you are in active labour, your blood glucose should be measured every hour to make sure it stays at a safe level. You may be given insulin and glucose through a drip to help with this.
This is more likely to happen if you are already giving yourself insulin injections. If you managed your glucose levels through diet alone, you may need very little additional monitoring during labour.
If you are exhausted, if your baby is distressed, or if they are not moving out of the birth canal, you may need an assisted birth. This is when the doctor uses special instruments to help deliver the baby during the last stage of labour.
During labour, your baby’s heart rate should also be continuously monitored.
What happens after my baby is born?
Your baby’s health
Your baby will stay with you unless they need extra care.
There is no reason why you can’t breastfeed your baby if you have gestational diabetes.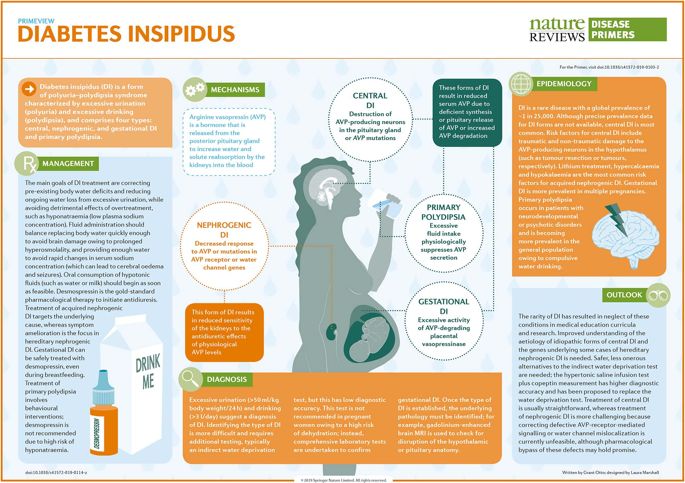 In fact, it can help protect their future health. If you’ve had gestational diabetes your baby may be at greater risk of developing obesity and or diabetes in later life. But breastfeeding can reduce these risks, as well as protect your baby against the risk of infections, asthma and heart disease.
In fact, it can help protect their future health. If you’ve had gestational diabetes your baby may be at greater risk of developing obesity and or diabetes in later life. But breastfeeding can reduce these risks, as well as protect your baby against the risk of infections, asthma and heart disease.
However you choose to feed your baby, you should start feeding them as soon as possible after birth (within half an hour) and then every 2-3 hours. This will help your baby’s glucose stay at a safe level.
A few hours after the birth, your healthcare team will test your baby’s glucose level by pricking their heel to get a drop of blood. Your baby will not enjoy this but it should be very quick, so try not to let it upset you. The test is done to keep your baby safe.
Your baby may need to be looked after in a neonatal unit if they:
- are unwell
- need close monitoring or treatment
- need help with feeding
- were born prematurely.
Find out more about feeding your baby after birth.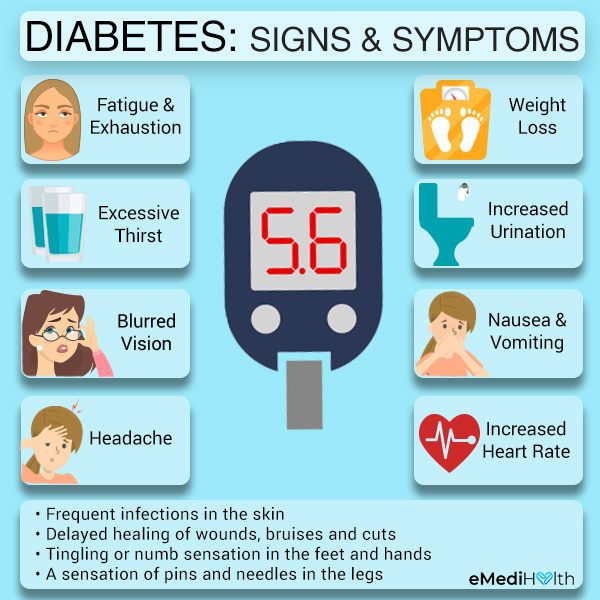
"I was an emotional wreck afterwards for a whole week, crying all the time. I didn't like seeing my baby with tubes in him and he had jaundice as well so we weren't allowed to go home. But now, he's fabulous; constantly crawling around, he's a really busy baby!"
Aisha
Your health
You’ll probably be advised to stop taking any diabetes medication straight away after your baby is born. This is because gestational diabetes usually settles after birth.
Your glucose levels should be tested to make sure they have gone back to normal before you go home. You should also have a diabetes test about 6-8 weeks after your baby is born. This is important, because some women will still have diabetes after pregnancy.
Women who have had gestational diabetes have a higher risk of developing type 2 diabetes. This means you will be advised to have a test once a year, which you can arrange at your GP's surgery.
Find out more about the long-term implications of gestational diabetes.
If you become pregnant again
If you’ve had gestational diabetes before, you are at risk of getting it again in your next pregnancy. If you’re planning to get pregnant again, trying to live a healthy lifestyle now will:
- improve your fertility
- protect your baby’s future health
- reduce your risk of problems in pregnancy.
Find out more about getting pregnant if you’ve had gestational diabetes before.
What does all this mean for you?
If your birth experience is different to what you had hoped for, this can be difficult to come to terms with. It is important to remember that labour and birth often does not go to plan, whether it is complicated by gestational diabetes or not. For many women, knowing more about induction and caesarean births helps them feel mentally prepared for what may happen.
"I'd seen a lot of my friends have children, so I had an idea that labour can change dramatically in minutes. I knew that the ideal wasn't always possible.
I think that helped a bit."
Michelle
If you do feel very emotional about any aspect your birth – even if it’s much later – it can help to talk about it. You can speak to friends or family, your midwife, health visitor or GP.
You can also speak to our midwives on our pregnancy line on 0800 014 7800 (Monday to Friday, 9am to 5pm), or email us at [email protected].
The optimal term for delivery in gestational diabetes mellitus is 39–40 weeks of gestation
Summary. Delayed delivery is often associated with poor neonatal outcome
According to a new study from Wayne State University School of Medicine, Detroit, USA, 39-40 weeks of gestation is the optimal time to induce labor in women c gestational diabetes mellitus (GDM). Delayed delivery is often associated with poor neonatal outcome. The results are published online in the Journal of Perinatology. nine0005
GDM is an impaired glucose tolerance that first developed or was diagnosed during pregnancy. This pathology complicates the course of 5-7% of all pregnancies. Risk factors for developing GDM include the age and overweight of the expectant mother, cases of type 2 diabetes mellitus in close relatives, and the presence of signs of GDM during previous pregnancies. However, GDM can also occur in those women who did not have impaired glucose tolerance before pregnancy. The fact is that pregnancy induces insulin resistance and leads to a decrease in insulin sensitivity as a result of the action of hormones such as human placental lactogen, corticoliberin and somatotropin. Women with marginal insulin secretory ability against the background of ever-increasing levels of these hormones develop hyperglycemic conditions that clinically resemble type 2 diabetes mellitus. It is known that this condition is associated with an increased risk of maternal perinatal death (due to caesarean section or operative vaginal delivery), which leads to fetal macrosomia. In addition, GDM leads to an increased risk of developing preeclampsia in the mother, and in the child - to respiratory distress syndrome, neonatal jaundice and hypocalcemia.
This pathology complicates the course of 5-7% of all pregnancies. Risk factors for developing GDM include the age and overweight of the expectant mother, cases of type 2 diabetes mellitus in close relatives, and the presence of signs of GDM during previous pregnancies. However, GDM can also occur in those women who did not have impaired glucose tolerance before pregnancy. The fact is that pregnancy induces insulin resistance and leads to a decrease in insulin sensitivity as a result of the action of hormones such as human placental lactogen, corticoliberin and somatotropin. Women with marginal insulin secretory ability against the background of ever-increasing levels of these hormones develop hyperglycemic conditions that clinically resemble type 2 diabetes mellitus. It is known that this condition is associated with an increased risk of maternal perinatal death (due to caesarean section or operative vaginal delivery), which leads to fetal macrosomia. In addition, GDM leads to an increased risk of developing preeclampsia in the mother, and in the child - to respiratory distress syndrome, neonatal jaundice and hypocalcemia. nine0005
nine0005
In the course of this work, we analyzed information on 97 thousand pregnancies with GDM and 176 thousand without this pathology. We assessed the risks and neonatal complications when stimulating labor at various gestational ages. The researchers once again confirmed that GDM increases the risk of adverse birth outcomes for both the baby and the mother. They determined that the lowest risk of operative vaginal delivery and caesarean section in women with the studied pathology was noted in cases where childbirth occurred before 39-th week of gestation. The minimum likelihood of developing intranatal complications was observed during childbirth at the 38th week of gestation, the admixture of meconium in the amniotic fluid was most often determined after the 37th week, the risk of chorioamnionitis was lowest during childbirth at the 38th, and fetal distress syndrome - at the 39th week of gestation. It was noted that cases of macrosomia were rarely noted at the 37th week of gestation, and then their frequency increased every week and reached a maximum by the 41st week.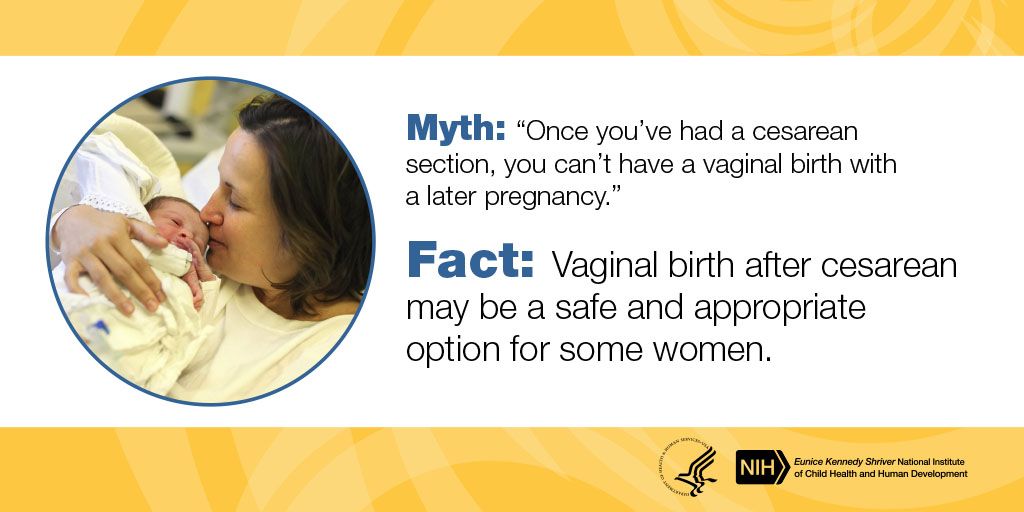
The authors summarized that, according to their results, 39-40th week of gestation is the optimal delivery time for GDM. It is during this period that the risk of developing a distress syndrome in a child and an operative version of vaginal delivery in a mother is minimal. The researchers did not identify indications for both earlier and later births, but insist on the need for additional studies that would examine the risk of neonatal death due to GDM in the expectant mother.
Commenting on this work, Dr. Andrew Garrison from the University of Utah, USA, who recently published a review on the issues of screening, diagnosis and treatment of GDM, noted that all the conclusions made by the authors of the study are fully consistent with results obtained in previous works. Since all the patients with GDM whose condition was studied in the course of this work were artificially stimulated, the scientists were unable to answer the question about the advantage of stimulation over expectant management. However, they obtained additional evidence that induction of labor in GDM should preferably be performed no later than 39-th week of gestation. Dr. E. Harrison emphasized that, according to the recommendations of the American College of Obstetricians and Gynecologists (ACOG), induction of labor before the 39th week of gestation in HD is indicated only if there is any specific symptom (for example, hypertensive disorder , rupture of membranes, deterioration of fetal vital signs) or in case of ineffective glycemic control, which significantly increases the risk of stillbirth. nine0005
However, they obtained additional evidence that induction of labor in GDM should preferably be performed no later than 39-th week of gestation. Dr. E. Harrison emphasized that, according to the recommendations of the American College of Obstetricians and Gynecologists (ACOG), induction of labor before the 39th week of gestation in HD is indicated only if there is any specific symptom (for example, hypertensive disorder , rupture of membranes, deterioration of fetal vital signs) or in case of ineffective glycemic control, which significantly increases the risk of stillbirth. nine0005
Yulia Kotikovich
Gestational diabetes in pregnancy - treatment and diagnosis of diabetes in pregnant women in Moscow, Clinical Hospital on Yauza
Consult a gynecologist
Service in two languages: Russian, English.
Leave your phone number and we will call you back.
Contents
IMPORTANT!
The information in this section should not be used for self-diagnosis or self-treatment. In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor. nine0005
In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor. nine0005
Specialists of the Yauza Clinical Hospital diagnose and treat gestational diabetes and its complications. For a comfortable pregnancy and the safety of the expectant mother and baby, we exercise strict control over the blood sugar level of a pregnant woman, if necessary, prescribe a specially designed diet and medications.
Make an appointment with a gynecologist
- About 7% of pregnant women have manifestations of gestational diabetes. In 50% of cases, the disease is asymptomatic
- Gestational diabetes in pregnancy significantly increases the risk of pregnancy complications for both mother and fetus
- Perinatal mortality increases by 2-3% with a combination of diabetes mellitus and pregnancy
Pregnancy diabetes (gestational diabetes) is an increase in blood glucose that first occurs during pregnancy but is not high enough to warrant a diagnosis of diabetes mellitus.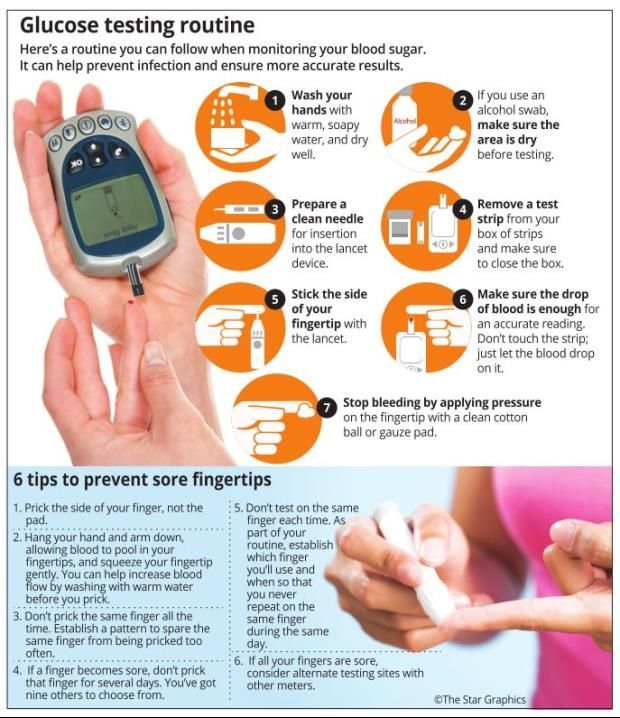 These are hidden disorders of carbohydrate metabolism that threaten to develop into diabetes mellitus. nine0005
These are hidden disorders of carbohydrate metabolism that threaten to develop into diabetes mellitus. nine0005
Pregnant blood glucose norm
During pregnancy, all women experience changes in insulin sensitivity and glucose tolerance. This is fine. The difference between the norm and pathology in the degree of change.
Blood tests for diabetes during pregnancy - norm and pathology
- If a fasting venous blood test shows a glucose level of more than 5.1 mmol/l, this is normal for pregnant women.
nine0044 From 5.1 to 7.0 mmol / l - gestational diabetes. - If 7.0 mmol / l or more - diabetes mellitus.
- Testing of capillary blood (taken from a finger) for the diagnosis of gestational diabetes mellitus is not recommended.
- If during an oral glucose tolerance test (when 75 g of glucose is taken orally during the study) after an hour the glucose level is more than 10.0 mmol/l, and after two hours the blood glucose level is in the range of 7.
 8-8.5 mmol/l - then for pregnant women this is a normal indicator. nine0045
8-8.5 mmol/l - then for pregnant women this is a normal indicator. nine0045
To better understand what gestational diabetes, or diabetes in pregnancy, is, you need to talk a little about hormonal changes in the body in pregnant women.
Causes of gestational diabetes
Hormonal changes that occur during pregnancy are associated with increased production of large amounts of steroid hormones. Some of them, such as cortisol and progesterone, have a significant effect on cell receptors, increasing their resistance to insulin. nine0027 This leads to an increase in blood glucose levels and requires a significant increase in insulin production by the pancreas. In cases where the compensatory capacity of the pancreas is not enough, sugar metabolism gets out of control and a condition called gestational diabetes or gestational diabetes develops.
This condition occurs quite often. Between 3 and 10% of pregnant women develop pathological insulin resistance leading to gestational diabetes. nine0027 Unlike diabetes mellitus diagnosed before pregnancy, pathological insulin resistance that occurs during pregnancy does not cause fetal malformations and in most cases does not require insulin treatment. But, nevertheless, uncompensated gestational diabetes can significantly complicate the course of pregnancy.
nine0027 Unlike diabetes mellitus diagnosed before pregnancy, pathological insulin resistance that occurs during pregnancy does not cause fetal malformations and in most cases does not require insulin treatment. But, nevertheless, uncompensated gestational diabetes can significantly complicate the course of pregnancy.
Specialists of the Yauza Clinical Hospital diagnose, treat and prevent diabetes in pregnant women and its complications, such as impaired fetal growth. The doctors of the Clinical Hospital on the Yauza strictly control the blood sugar level of a pregnant woman, if necessary, prescribe a specially designed diet. This ensures a comfortable pregnancy and the safety of the expectant mother and baby. nine0005
Pregnancy diabetes - consequences for the child
Large disproportionate fruit. The most important and frequent complication of gestational diabetes is fetal growth failure. Developing in conditions of increased blood glucose levels, which penetrate the fetoplacental barrier, the fetus is forced to compensate for the increased sugar level with its own insulin.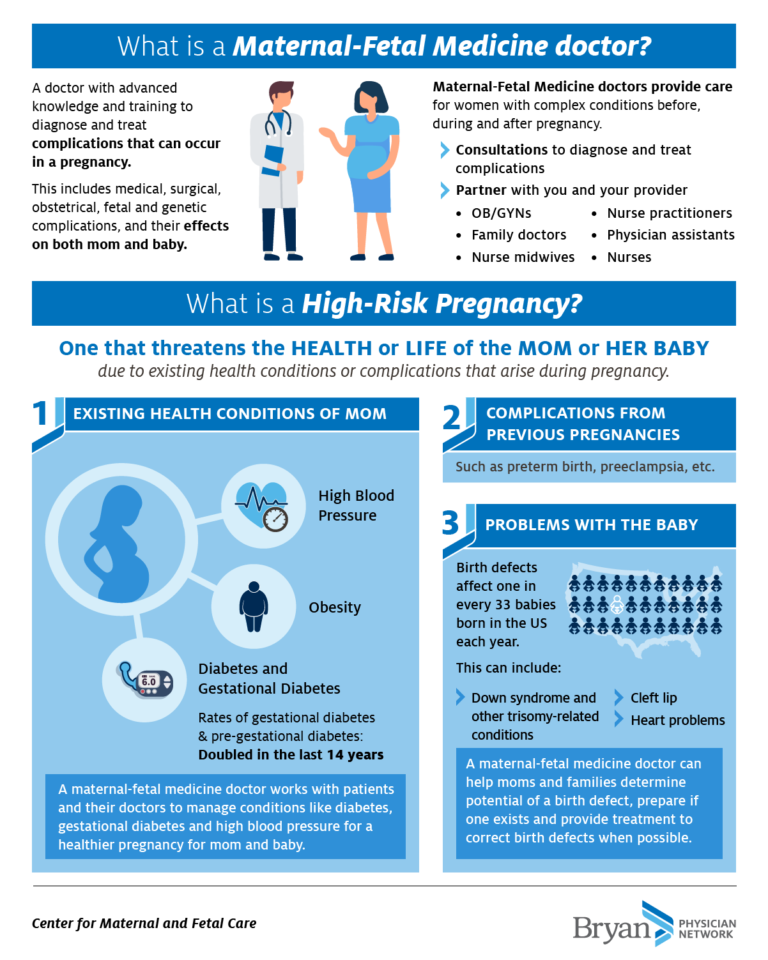 Due to the fact that the structure of insulin and growth hormone are very similar, high levels of insulin stimulate the growth of the fetus. The problem is that a large fetus develops. In such a fetus, body proportions differ from those of normally developing newborns, in which the volume of the head is larger than the volume of the shoulder girdle. In fetuses with uncompensated gestational diabetes, the size of the shoulder girdle predominates, and the size of the abdomen increases. This leads to the fact that during childbirth after the fetus's head passes through the birth canal, the shoulders can get stuck (shoulder dystocia) and the child, along with the mother, can be severely injured or die. nine0005
Due to the fact that the structure of insulin and growth hormone are very similar, high levels of insulin stimulate the growth of the fetus. The problem is that a large fetus develops. In such a fetus, body proportions differ from those of normally developing newborns, in which the volume of the head is larger than the volume of the shoulder girdle. In fetuses with uncompensated gestational diabetes, the size of the shoulder girdle predominates, and the size of the abdomen increases. This leads to the fact that during childbirth after the fetus's head passes through the birth canal, the shoulders can get stuck (shoulder dystocia) and the child, along with the mother, can be severely injured or die. nine0005
Polyhydramnios or oligohydramnios. In addition, with gestational diabetes, the balance of the amount of amniotic fluid may be disturbed and either polyhydramnios or oligohydramnios develops. This is a serious risk factor for intrauterine fetal death or premature birth.
Underdevelopment of the lungs. In pregnant women with diabetes, the lungs of the fetus mature later, as the production of surfactant (a special lubricant for the inner walls of the alveoli, where oxygen is exchanged in the lungs) is disrupted. Therefore, premature birth in gestational diabetes is especially dangerous. nine0005
Hypoglycemia and metabolic disorders in the fetus. Due to the constant increased production of its own insulin during pregnancy, immediately after birth, the child is in a state of hypoglycemia with electrolyte imbalance, which threatens his life.
All this dictates the need for the earliest possible detection of gestational diabetes in pregnant women, the level of sugar in the blood of a pregnant woman and to prevent the development of complications.
. nine0005
Diagnosis of diabetes in pregnant women at the Yauza Clinical Hospital
Signs of diabetes in pregnant women
Gestational diabetes in pregnancy is not usually associated with the classic symptoms of diabetes, such as thirst or excessive urination (polyuria).
Pregnancy tests for diabetes mellitus
First phase. At the first visit of a pregnant woman to a doctor at any time, she is tested for glucose levels in venous blood - fasting glucose, regardless of food intake, glycated hemoglobin. This is the first phase of research to detect diabetes mellitus or gestational diabetes in pregnant women. If diabetes mellitus is detected, the patient is referred for observation and treatment to an endocrinologist. nine0005
Second phase. For a period of 24-28 weeks, all patients who did not show identified disorders of carbohydrate metabolism at the first study are called for a glucose tolerance test (OGTT) to detect "hidden diabetes". This is done because the occurrence of gestational diabetes is associated with the development of insulin resistance under the influence of hormones produced by the placenta. Therefore, in the vast majority of cases, gestational diabetes develops in the second half of pregnancy after 24 weeks, when there is a peak in the production of placental hormones. nine0005
nine0005
Glucose tolerance test
It is carried out to detect pathological insulin resistance, characteristic of latent diabetes in pregnant women. Pregnant women undergo a two-hour test, only in the laboratory.
During the 3 days leading up to the test, the woman should eat her usual diet, including carbohydrates (>150 g of carbohydrates per day), maintain her usual physical activity. The evening before testing, dinner should include 30-50 grams of carbohydrates. nine0027 On the day of the study, before the analysis, you should not smoke and take medications that can affect the level of glucose (vitamins, glucocorticoid hormones, iron preparations, which include carbohydrates, beta-agonists, beta-blockers). You can drink water.
Venous blood is taken on an empty stomach (after 8-14 hours of fasting, usually in the morning, before breakfast).
Then the patient takes a glucose solution (75 g).
And they take blood in an hour and two after the sugar load.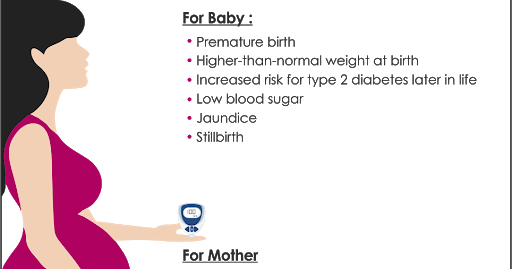 Normally, the level of glucose in the blood after a sugar load should not exceed an hour later - 10 mmol / l, after 2 hours - 8.5 mmol / l. nine0027 If manifest diabetes mellitus is detected, the patient is referred to an endocrinologist, gestational diabetes mellitus is treated by an obstetrician-gynecologist or therapist.
Normally, the level of glucose in the blood after a sugar load should not exceed an hour later - 10 mmol / l, after 2 hours - 8.5 mmol / l. nine0027 If manifest diabetes mellitus is detected, the patient is referred to an endocrinologist, gestational diabetes mellitus is treated by an obstetrician-gynecologist or therapist.
Glucose tolerance test contraindications
- Strict bed rest prescribed for a pregnant woman (until doctor's approval).
- Severe toxicosis of pregnant women (with nausea and vomiting).
- Acute infectious or inflammatory disease. nine0045
- Exacerbation of chronic pancreatitis.
- Dumping syndrome (syndrome of resected stomach).
Prenatal diabetes monitoring
Blood glucose monitoring, self-monitoring diary
When diagnosing gestational diabetes, it is necessary to establish strict control of sugar levels throughout the subsequent pregnancy and during childbirth.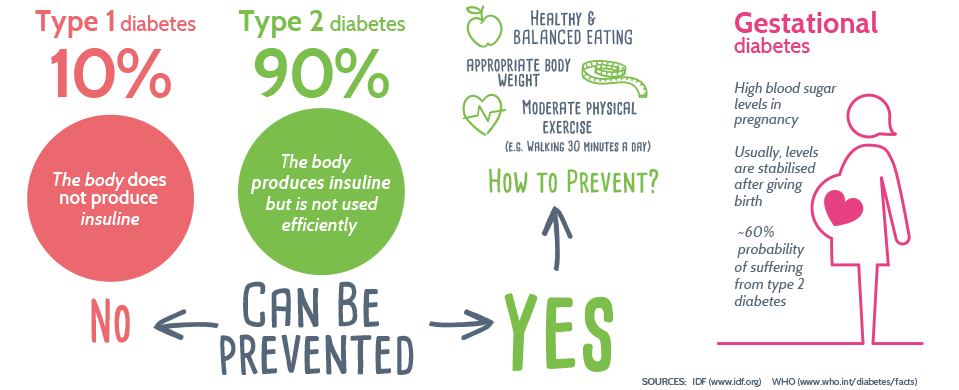 To do this, regularly examine the blood for sugar (glucose). In addition, the patient conducts self-monitoring using a glucometer. nine0005
To do this, regularly examine the blood for sugar (glucose). In addition, the patient conducts self-monitoring using a glucometer. nine0005
It is recommended that a pregnant woman keep a diary of observations in which to record:
- blood glucose (normal <5.1 mmol/l),
- the presence of ketone bodies in the urine, which is determined by test strips sold in a pharmacy (normally, ketone bodies are absent),
- blood pressure readings (normal <130|80 mmHg),
- fetal movements,
- body weight, nine0044 diet.
Expert ultrasound
Conducting an expert ultrasound examination reveals signs of intrauterine suffering of the fetus (diabetic fetopathy), polyhydramnios. Most often, this is a sign of chronically elevated blood glucose levels, penetrating into the blood of the fetus. This requires urgent correction of the diet and normalization of the level of glycemia (blood sugar). If necessary, insulin therapy.
Make an appointment nine0005
Treatment of gestational diabetes
Diet for gestational diabetes
In most cases, it is sufficient to follow a special diet recommended by a nutritionist based on the body mass index of the pregnant woman and her taste preferences. The effectiveness of diet therapy is determined by the maintenance of normal blood glucose levels. Diet in pregnancy diabetes recommends:
The effectiveness of diet therapy is determined by the maintenance of normal blood glucose levels. Diet in pregnancy diabetes recommends:
- Avoid simple carbohydrates - sweets, pastries, white bread, honey, sugar, jam, sweet drinks and fruits, ice cream. nine0045
- Limit complex carbohydrates - cereals (semolina, rice - exclude), potatoes, corn, legumes, durum wheat pasta. Distribute their intake evenly over several meals throughout the day to eliminate starvation (causes the formation of ketone bodies).
- Eat enough protein - meat, fish, seafood, poultry, mushrooms, eggs, hard cheese, dairy and sour-milk products of medium fat content (3-5%).
- It is necessary to enrich the diet with fiber and vitamins - greens, vegetables (except for boiled carrots and beets), sweet and sour berries (excluding grapes). nine0045
- Correctly choose fats, do not exceed their amount recommended by the doctor - vegetable oils (add to ready-made meals), nuts, seeds.
 Animal fats (butter, sausages) - limit.
Animal fats (butter, sausages) - limit. - When cooking, boil, stew, steam and bake dishes. Don't fry. Do not deep fry.
A detailed menu for a pregnant woman with gestational diabetes will be compiled by a doctor, taking into account the individual characteristics of each particular woman. nine0027 It is not worth using table No. 9 in its pure form for pregnant women with diabetes mellitus due to a significant restriction of its calorie content.
In detail, what you can eat with diabetes in pregnant women will be told by the doctor at an in-person consultation.
Pharmacotherapy
In cases where the diet fails to achieve the desired control of the level of glycemia in the blood, there are signs of a negative effect on the fetus - they resort to prescribing drugs - insulin. In case of diabetes in pregnant women, antidiabetic drugs in tablets should not be used. Insulin therapy is prescribed by an endocrinologist. Pregnant women with diabetes who are on insulin therapy are jointly managed by an endocrinologist, an internist and an obstetrician-gynecologist. nine0005
nine0005
Physical activity
Patients are recommended regular physical activity - walking in the fresh air (at least 150 minutes per week), swimming.
Prenatal diabetes - childbirth
With a compensated course of gestational diabetes, normal development of the fetus and the condition of the woman, childbirth is carried out in time in a natural way. The question of early delivery, caesarean section may arise if there are relevant indications from the mother or fetus. nine0005
Specialists of the Yauza Clinical Hospital have included mandatory fetal development screenings and tests to diagnose sugar metabolism disorders in the pregnancy monitoring program. Recommendations are given on a special diet for women with manifestations of gestational diabetes. If necessary, strict glycemic control is carried out throughout pregnancy, ensuring its successful completion and the birth of a healthy child.
Make an appointment nine0005
Cost of services
Prices for services you can see in the price list or check by phone listed on the site.