How long does acid reflux last during pregnancy
Indigestion and heartburn in pregnancy
Indigestion, also called heartburn or acid reflux, is common in pregnancy. It can be caused by hormonal changes and the growing baby pressing against your stomach.
You can help ease indigestion and heartburn by making changes to your diet and lifestyle, and there are medicines that are safe to take in pregnancy.
Symptoms of indigestion and heartburn
Symptoms of indigestion and heartburn include:
- a burning sensation or pain in the chest
- feeling full, heavy or bloated
- burping or belching
- feeling or being sick
- bringing up food
Symptoms usually come on soon after eating or drinking, but there can sometimes be a delay between eating and developing indigestion.
You can get symptoms at any point during your pregnancy, but they are more common from 27 weeks onwards.
Things you can do to help with indigestion and heartburn
Changes to your diet and lifestyle may be enough to control your symptoms, particularly if they are mild.
Eat healthily
You're more likely to get indigestion if you're very full.
If you're pregnant, it may be tempting to eat more than you would normally, but this may not be good for you or your baby.
Find out more about a healthy diet in pregnancy and foods to avoid.
Change your eating and drinking habits
You may be able to control your indigestion with changes to your eating habits.
It can help to eat small meals often, rather than larger meals 3 times a day, and to not eat within 3 hours of going to bed at night.
Cutting down on drinks containing caffeine, and foods that are rich, spicy or fatty, can also ease symptoms.
Keep upright
Sit up straight when you eat. This will take the pressure off your stomach. Propping your head and shoulders up when you go to bed can stop stomach acid coming up while you sleep.
Stop smoking
Smoking when pregnant can cause indigestion, and can seriously affect the health of you and your unborn baby.
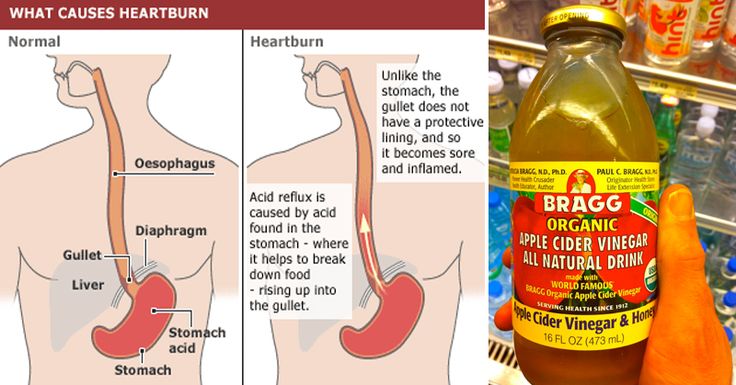
When you smoke, the chemicals you inhale can contribute to your indigestion. These chemicals can cause the ring of muscle at the lower end of your gullet to relax, which allows stomach acid to come back up more easily. This is known as acid reflux.
Smoking also increases the risk of:
- your baby being born prematurely (before week 37 of your pregnancy)
- your baby being born with a low birthweight
- sudden infant death syndrome (SIDS), or "cot death"
There's lots of help available to stop smoking. Talk to your midwife or call the NHS Smokefree helpline on 0300 123 1044. Find out more about stopping smoking in pregnancy.
Talk to your midwife or call the NHS Smokefree helpline on 0300 123 1044. Find out more about stopping smoking in pregnancy.
Avoid alcohol
Drinking alcohol can cause indigestion. During pregnancy, it can also lead to long-term harm to the baby. It's safest to not drink alcohol at all in pregnancy.
Find out more about alcohol and pregnancy
When to get medical help
See your midwife or GP if you need help managing your symptoms or if changes to your diet and lifestyle do not work. They may recommend medicine to ease your symptoms.
You should also see your midwife or GP if you have any of the following:
- difficulty eating or keeping food down
- weight loss
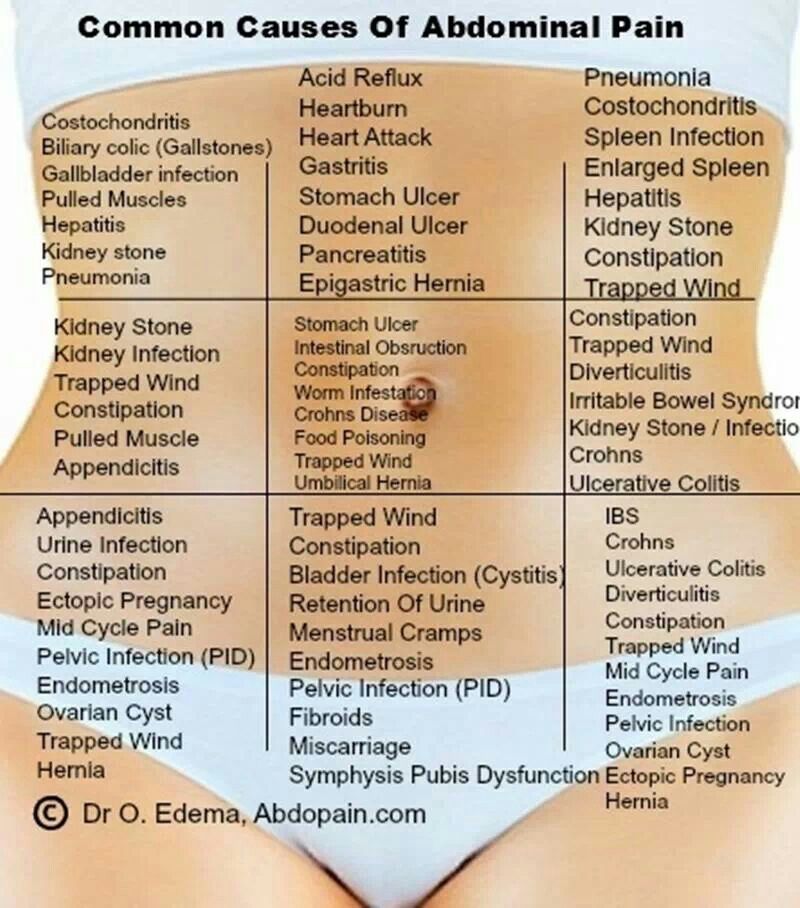
- stomach pains
Your midwife or GP may ask about your symptoms and examine you by pressing gently on different areas of your chest and stomach to see whether it's painful.
If you're taking prescription medicines
Speak to your GP if you're taking medicine for another condition, such as antidepressants, and you think it may be making your indigestion worse. They may be able to prescribe an alternative medicine.
Never stop taking a prescribed medicine unless you're advised to do so by your GP or another qualified healthcare professional who's responsible for your care.
Medicines for indigestion and heartburn
Medicines for indigestion and heartburn during pregnancy include:
- antacids – to neutralise the acid in your stomach (some are available over the counter from a pharmacist)
- alginates – to relieve indigestion caused by acid reflux by stopping the acid in your stomach coming back up your gullet
You may only need to take antacids and alginates when you start getting symptoms.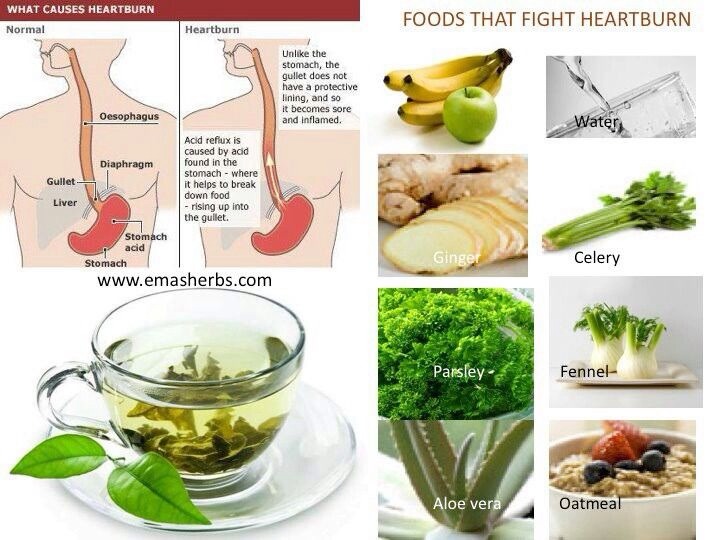 However, your GP may recommend taking them before symptoms come on – for example, before a meal or before bed.
However, your GP may recommend taking them before symptoms come on – for example, before a meal or before bed.
If you're taking iron supplements as well as antacids, do not take them at the same time. Antacids can stop iron from being absorbed by your body.
If antacids and alginates do not improve your symptoms, your GP may prescribe a medicine to reduce the amount of acid in your stomach. 2 that are widely used in pregnancy and not known to be harmful to an unborn baby are:
- ranitidine – a tablet you take twice a day
- omeprazole – a tablet you take once a day
Causes of indigestion in pregnancy
Symptoms of indigestion come when the acid in your stomach irritates your stomach lining or your gullet. This causes pain and a burning feeling.
When you're pregnant, you're more likely to have indigestion because of:
- hormonal changes
- the growing baby pressing on your stomach
- the muscles between your stomach and gullet relaxing, allowing stomach acid to come back up
You may be more likely to get indigestion in pregnancy if:
- you had indigestion before you were pregnant
- you've been pregnant before
- you're in the later stages of pregnancy
Video: Eating well on a budget
In this video, a dietitian gives advice on how to eat healthily on a budget.
Media last reviewed: 13 January 2021
Media review due: 13 January 2024
Acid reflux in pregnancy: Symptoms and treatments
Acid reflux occurs when stomach acid leaks out of the stomach and up into the esophagus. The primary symptom is heartburn, which is an uncomfortable, burning sensation in the chest. Pregnant women are particularly prone to acid reflux and heartburn.
According to the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), severe acid reflux affects about 20% of people in the United States each year.
In this article, we outline the symptoms of acid reflux and explain what causes it during pregnancy. We also list some medical treatments and home remedies for treating heartburn during pregnancy.
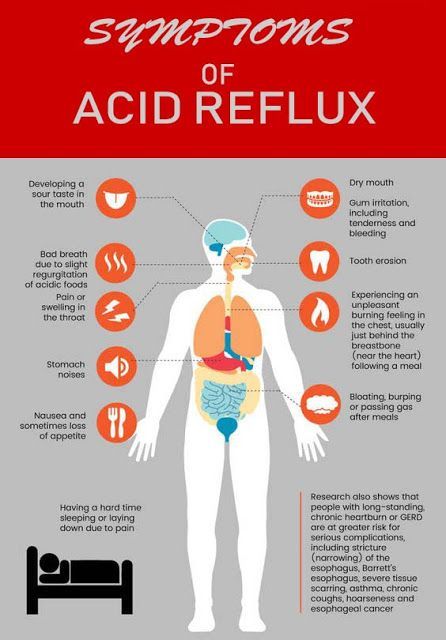
Share on PinterestHormonal changes may cause acid reflux during pregnancy.The primary symptom of acid reflux is heartburn, which is a burning sensation in the middle of the chest. It may accompany a feeling of heaviness or fullness in the chest or stomach.
A person may be more likely to experience heartburn:
- after eating a meal or drinking
- when lying down
- when bending over
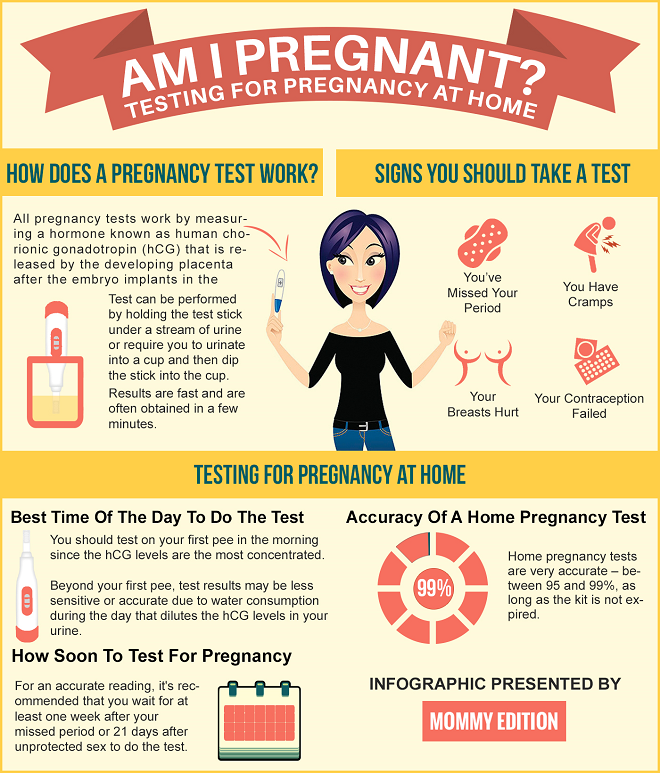
Heartburn can affect anyone at any time, but it is particularly common during pregnancy.
Other potential symptoms of acid reflux include:
- a bitter taste in the mouth
- sore throat
- cough
- bloating
- belching
- nausea
- vomiting
According to an older study from 2010, severe acid reflux or gastroesophageal reflux disease (GERD) affects about 80% of pregnancies. Heartburn can develop at any stage of the pregnancy, but it is most common during the second and third trimesters.
Researchers do not fully understand why acid reflux begins or worsens later in pregnancy. However, below are some factors that they believe to play a role.
Hormonal changes
During pregnancy, a woman produces increased amounts of the hormone progesterone. This hormone is responsible for relaxing smooth muscle tissue throughout the body. It plays an important role in relaxing the uterus so that it can stretch and grow as the fetus develops.
It plays an important role in relaxing the uterus so that it can stretch and grow as the fetus develops.
However, progesterone can also relax the sphincter muscle that connects the esophagus to the stomach. The sphincter allows food to enter the stomach while preventing food and stomach acid from leaking up into the esophagus. Progesterone loosens the sphincter, allowing acid to travel back up the esophagus.
Increased pressure on the stomach
In the later stages of pregnancy, the growing uterus and fetus put increasing pressure on the stomach. This pressure can cause acid to leak out of the stomach and up the esophagus. This leakage is more likely to occur after a meal when the stomach is full.
Women should talk to their doctor before taking a particular heartburn medication during pregnancy. A doctor can offer advice on which medications are safe for the woman and the developing fetus.
According to UT Southwestern Medical Center, there are three main types of heartburn medication that are safe for a woman to take during pregnancy. These medications are:
These medications are:
Oral antacids
Oral antacids (OAs) neutralize stomach acid, making it less acidic. Examples of OAs include aluminum and magnesium hydroxide (e.g., Maalox and Mylanta) and calcium carbonate (e.g., TUMS).
Oral antacids are available over the counter and via prescription.
h3-receptor antagonists
h3-receptor antagonists are medications that stop the cells in the stomach from producing too much acid. They work by reducing levels of the chemical h3 histamine, which stimulates cells in the stomach to produce stomach acid.
Examples of h3-receptor antagonists include cimetidine (Tagamet HB) and famotidine (Pepcid).
The above brands are available over the counter.
Proton pump inhibitors
Proton pump inhibitors (PPIs) are medications that stop the stomach from producing too much acid. They work by blocking an enzyme necessary for producing stomach acid.
Examples of PPIs include lansoprazole (Prevacid) and omeprazole (Prilosec).
People should be aware that PPIs can take several days to work effectively. As such, people may wish to consider trying an antacid or h3-receptor antagonist first.
PPIs are available over the counter and via prescription.
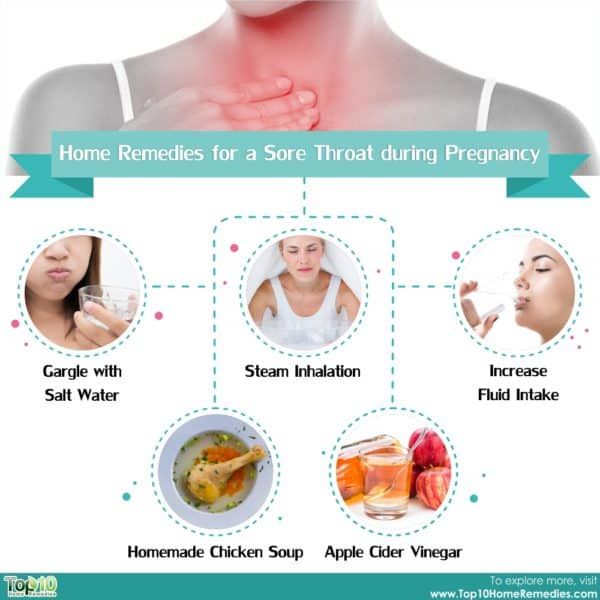
In addition to medication, a person can help treat their acid reflux using home remedies. The NIDDK provide the following tips for reducing stomach acid naturally:
- raising the head of the bed off the floor by 6–8 inches to sleep at a slight angle
- sitting in an upright position for 3 hours following a meal
- wearing loose fitting clothing around the abdomen
- avoiding eating food within 2–3 hours of going to bed
- eating smaller meals
- avoiding spicy or greasy foods that can trigger heartburn
Pregnant women should talk to their healthcare provider before consuming any natural remedies for heartburn. A healthcare provider can help determine whether the remedy may be effective and whether it will be safe for the woman and fetus.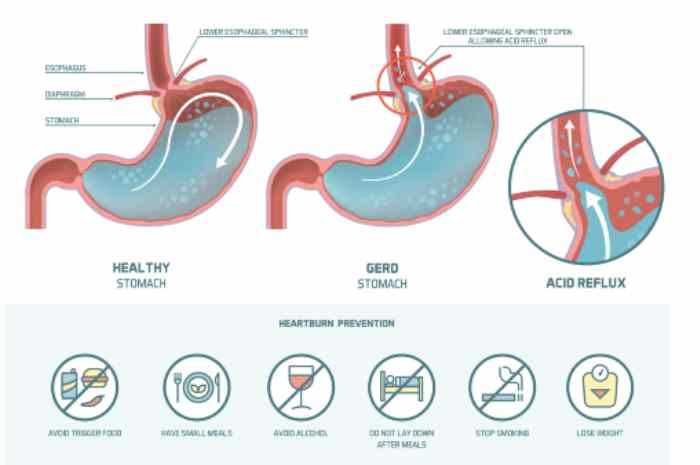
It may not always be possible to prevent acid reflux and heartburn during pregnancy. However, practicing the techniques above can help women manage symptoms when they occur.
Pregnant women should see their doctor if they experience severe or persistent heartburn that does not respond to over-the-counter or at-home treatments. Heartburn-type pains below the ribs can sometimes be a sign of preeclampsia. Without regular monitoring and any necessary treatment, this serious condition can threaten the life of the woman and fetus.
Other signs and symptoms of preeclampsia include:
- high blood pressure
- swelling of the face, hands, and feet
- severe headache
- problems with vision
It is important to attend all scheduled routine antenatal appointments. Doing this will help ensure that healthcare providers pick up on any health issues that arise during the pregnancy.
Acid reflux during pregnancy is a common occurrence. In most cases, acid reflux and its associated symptoms should go away once a woman gives birth.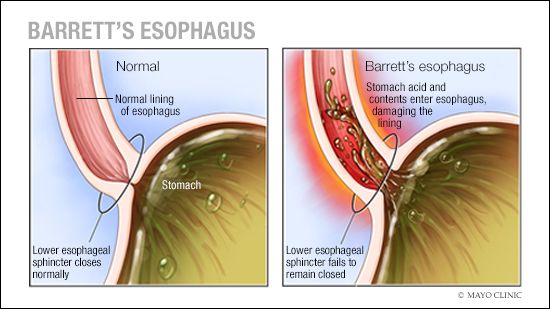
Several medications are suitable for treating acid reflux and heartburn during pregnancy. Women can also try home remedies, such as wearing loose fitting clothes, eating smaller meals, and avoiding foods that can trigger heartburn.
Women should see a doctor if they experience heartburn that is severe or persistent during pregnancy. Heartburn-type symptoms can sometimes mimic those of other conditions, such as preeclampsia. Attending all routine antenatal appointments reduces the risk of complications developing during the pregnancy.
90,000 GERD during pregnancy. What is GERD during pregnancy? IMPORTANT
The information in this section should not be used for self-diagnosis or self-treatment. In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
GERD during pregnancy is an acid-dependent disease of the esophagus caused by damage to the mucosa during the reflux of stomach contents, which has arisen or worsened under the influence of gestational factors.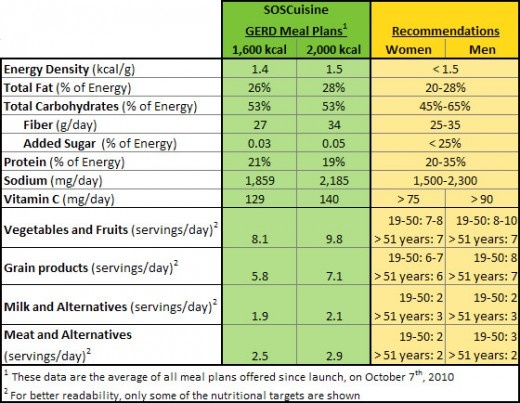 Manifested by heartburn, sour eructation, odynophagia, less often - nausea, vomiting, dysphagia, epigastric pain, cough, dysphonia, hypersalivation in sleep, taste perversions, depressed mood. It is diagnosed using alkaline and omeprazole tests, esophagoscopy, pH-metry, manometry. For treatment, alginates, antacids, selective histamine blockers, drugs that inhibit the proton pump, prokinetics are used.
Manifested by heartburn, sour eructation, odynophagia, less often - nausea, vomiting, dysphagia, epigastric pain, cough, dysphonia, hypersalivation in sleep, taste perversions, depressed mood. It is diagnosed using alkaline and omeprazole tests, esophagoscopy, pH-metry, manometry. For treatment, alginates, antacids, selective histamine blockers, drugs that inhibit the proton pump, prokinetics are used.
ICD-10
K21 Gastroesophageal reflux
- Causes
- Pathogenesis
- Classification
- Symptoms of GERD during pregnancy
- Complications
- Diagnostics
- Treatment of GERD during pregnancy
- Prognosis and prevention
- Prices for treatment
General
GERD (gastroesophageal reflux disease, gastroesophageal reflux) is one of the most common diseases of the gastrointestinal tract, contributing to such a common symptom as pregnancy heartburn. According to the observations of specialists in the field of obstetrics and gynecology, from 30 to 95% of patients during the period of bearing a child experience heartburn, which some experts even consider a natural manifestation of pregnancy. In 21-80% of patients suffering from GERD, the disease debuted precisely in connection with gestation.
According to the observations of specialists in the field of obstetrics and gynecology, from 30 to 95% of patients during the period of bearing a child experience heartburn, which some experts even consider a natural manifestation of pregnancy. In 21-80% of patients suffering from GERD, the disease debuted precisely in connection with gestation.
Women who have given birth multiple times are more susceptible to the disease. The relevance of timely detection of gastroesophageal reflux is due to a significant deterioration in the quality of life of a pregnant woman and the need to prescribe pharmacotherapy to almost half of the patients.
GERD during pregnancy
Causes
Gastroesophageal reflux of acidic gastric contents develops with a weakening of the cardiac sphincter, impaired motility of the esophagus and stomach, increased gastric secretion, and a decrease in the protective properties of the esophageal mucosa. The occurrence of GERD is promoted by congenital and acquired hernia of the esophageal opening of the diaphragm with displacement into the posterior mediastinum of the abdominal esophagus, part or all of the stomach, smoking, dietary errors, and obesity.
The occurrence of GERD is promoted by congenital and acquired hernia of the esophageal opening of the diaphragm with displacement into the posterior mediastinum of the abdominal esophagus, part or all of the stomach, smoking, dietary errors, and obesity.
A certain role is played by the intake of nitrates, antidepressants, progestins, anticholinergics, calcium channel blockers and other drugs that cause transient relaxation of the esophageal sphincter. Specialists in the field of modern gastroenterology consider pregnancy as a separate prerequisite for the development of gastroesophageal reflux disease. The high incidence of GERD during gestation is associated with the action of factors such as:
- Increased progesterone levels. Under the action of progestins, the lower esophageal sphincter relaxes, the tone of which is restored only in the postpartum period. By reducing the tone of smooth muscle fibers and reducing the sensitivity of intestinal receptors to histamine and serotonin, physiological hyperprogesteronemia slows down gastrointestinal motility and impairs gastric emptying.
 As a result, reflux occurs more frequently.
As a result, reflux occurs more frequently. - Increased intra-abdominal pressure. During pregnancy, the relative position of the internal organs of the abdominal cavity is disturbed, which is associated with the development of the fetus and the growth of the uterus. When the stomach is displaced towards the diaphragm, evacuation stagnation of its contents is formed faster and the risk of diaphragmatic hernia formation increases. The factor of increasing intra-abdominal pressure is most significant in carrying multiple pregnancies and large fetuses.
Pathogenesis
The mechanism of development of GERD during pregnancy is based on the reflux of aggressive stomach contents into the lower esophagus. Gastroesophageal reflux usually occurs when the pressure of the cardiac sphincter is less than 2 mm Hg. Art. or an increase in intragastric pressure of more than 5 mm Hg. Art. Both of these factors are found in pregnant women. Refluxate containing hydrochloric acid, pepsin, and in some cases bile acids, has an irritating effect on the epithelium of the esophagus, causes a local inflammatory reaction, and in some patients provokes the onset of erosive processes.
Classification
When systematizing the forms of GERD in pregnant women, the same criteria are taken into account as outside the gestational period - the nature of the course of the disease and the condition of the esophageal mucosa. This approach makes it possible to develop optimal medical tactics aimed at eliminating clinical symptoms and the morphological basis of their occurrence without the risk of negative effects on the fetus. Depending on the time of existence of the disorder, acute gastroesophageal reflux disease is distinguished, lasting up to 3 months, and a chronic process that exists for 3 months or more. Taking into account the characteristics of damage to the esophageal mucosa, such forms of GERD are distinguished as:
- Gastroesophageal reflux without esophagitis. With a non-erosive variant of the disorder, detected in 55-70% of patients, there are no endoscopic signs of damage to the epithelium. Although the likelihood of complications in this case is lower, the patient's quality of life deteriorates in the same way as in the presence of erosions.
- Reflux esophagitis. In 30-45% of pregnant women with GERD during endoscopy, visible signs of esophagitis caused by the aggressive action of the contents of the stomach are determined. In the erosive form of gastroesophageal reflux, acute and long-term consequences of the disease are more often observed.
When predicting the outcome of GERD in a pregnant woman, the severity of the endoscopically positive variant of the disease according to the Los Angeles classification is also taken into account. The most favorable during pregnancy is reflux esophagitis A and B degrees, in which the defects extend to 1-2 folds of the mucosa, and their sizes, respectively, are up to or more than 5 mm. With C degree of GERD, less than 75% of the esophageal circumference is affected, and with D - 75% or more, which significantly increases the likelihood of a complicated course.
Symptoms of GERD during pregnancy
75% of patients with gastroesophageal reflux complain of heartburn, which gradually increases as labor approaches. Discomfort and burning behind the sternum often occur after eating spicy, fatty, fried foods, overeating, exercise, lying down and bending over. Heartburn attacks can recur several times a day and last from minutes to several hours. Pregnant women suffering from GERD may experience sour or bitter belching, sensation of a lump in the throat, retrosternal pain when swallowing with irradiation to the precordial region, neck, lower jaw, interscapular space.
Discomfort and burning behind the sternum often occur after eating spicy, fatty, fried foods, overeating, exercise, lying down and bending over. Heartburn attacks can recur several times a day and last from minutes to several hours. Pregnant women suffering from GERD may experience sour or bitter belching, sensation of a lump in the throat, retrosternal pain when swallowing with irradiation to the precordial region, neck, lower jaw, interscapular space.
Sometimes in the II-III trimesters, nausea and vomiting are noted, it is extremely rare that swallowing solid and then liquid food is difficult. Extra-esophageal manifestations of reflux disease during pregnancy are a feeling of fullness in the epigastrium, rapid satiety, repeated attacks of coughing and suffocation, a hoarse voice, sore throat, increased salivation during sleep, burning cheeks and tongue, taste perversion, bad breath. Often, pregnant women experience a sad, depressed mood. Rarely, GERD is asymptomatic.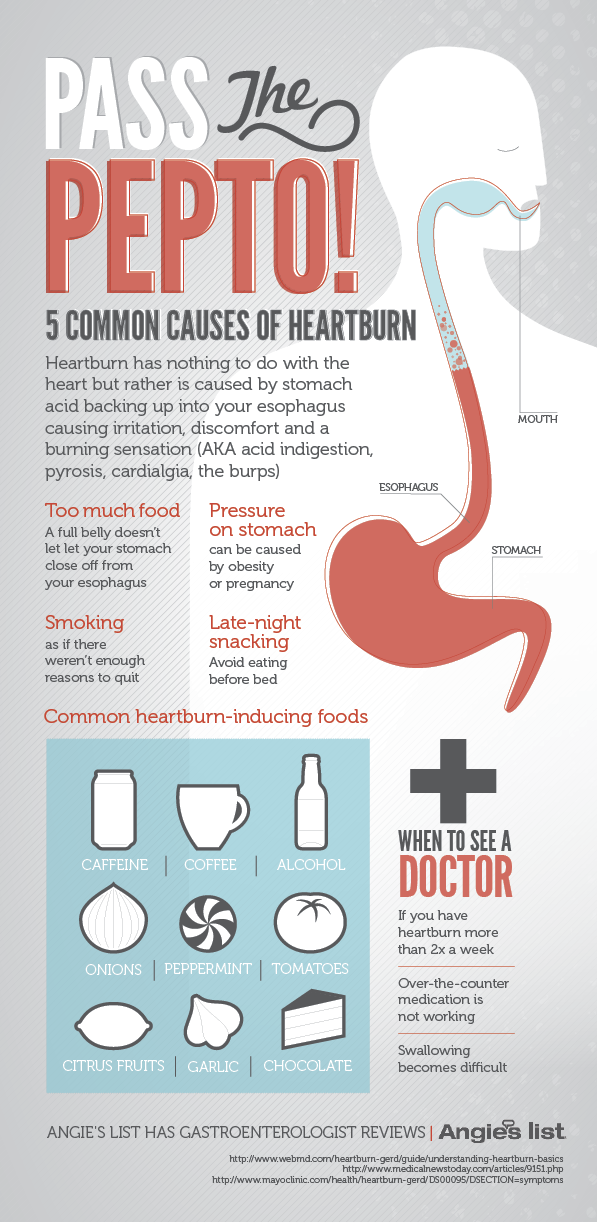
Complications
Usually, gastroesophageal reflux does not contribute to the occurrence of any obstetric complications, however, with extensive erosive damage to the esophagus, a more pronounced anemia of pregnant women may develop. In two thirds of patients, GERD worsens during pregnancy: in 10-11% of cases, a relapse occurs in the 1st trimester, aggravated by early toxicosis, in 33-34% - in the 2nd trimester, and in more than half of pregnant women - in the 3rd.
Rare specific complications that occur against the background of physiological immunodeficiency during pregnancy are acute esophagitis caused by candidal and herpes infections. There is a risk of ulceration of the mucosa with the development of esophageal bleeding. Long-term consequences of reflux disease are narrowing (strictures) of the esophagus, dysplasia and metaplasia of the epithelium (Barrett's esophagus) and esophageal adenocarcinoma.
Diagnostics
In pregnancy, the diagnosis of GERD is usually made on the basis of typical clinical symptoms with daily occurrence of heartburn.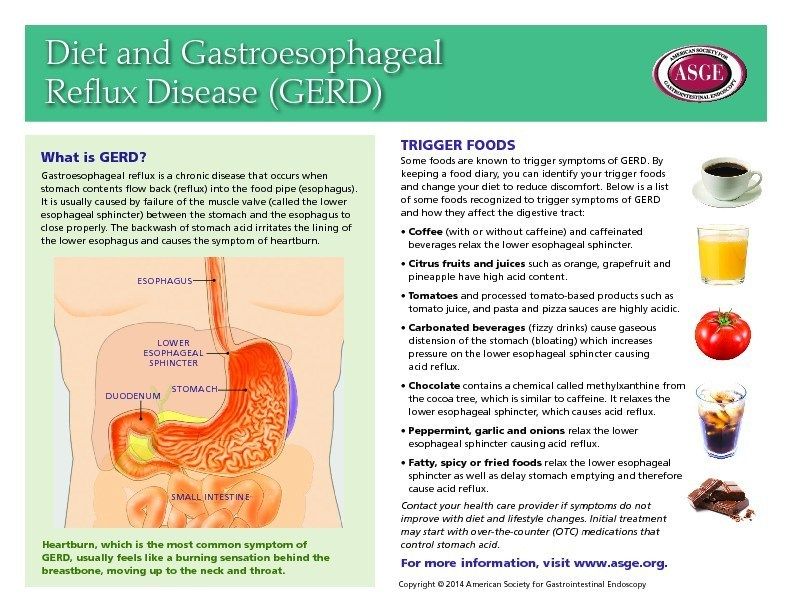 An obstetrician-gynecologist and a gastroenterologist are involved in the diagnosis. Instrumental methods traditionally used in the diagnosis of the disease are used to a limited extent in pregnant women due to the possible provocation of preterm labor and the aggravation of other complications (nephropathy, early toxicosis, preeclampsia, eclampsia). Recommended for diagnostic purposes:
An obstetrician-gynecologist and a gastroenterologist are involved in the diagnosis. Instrumental methods traditionally used in the diagnosis of the disease are used to a limited extent in pregnant women due to the possible provocation of preterm labor and the aggravation of other complications (nephropathy, early toxicosis, preeclampsia, eclampsia). Recommended for diagnostic purposes:
- Alkaline test. Reception of absorbable antacids quickly stops an attack of heartburn. The positive effect of alkaline preparations is associated with the neutralization of hydrochloric acid coming from the stomach into the esophagus. In the presence of extraesophageal manifestations, the study is supplemented with an omeprazole test aimed at eliminating symptoms by inhibiting gastric secretion.
- Endoscopy of the esophagus. Esophagoscopy is performed if extensive erosion, ulceration, esophageal bleeding, strictures are suspected, and neoplasia can be ruled out. In endoscopic examination, GERD is manifested by swelling and slight vulnerability of the esophageal mucosa, it is possible to identify areas of damaged epithelium.
 In some cases, it is possible to visualize the reflux of gastric juice.
In some cases, it is possible to visualize the reflux of gastric juice. - Intraesophageal pH-metry. The method is effective in non-erosive forms of gastroesophageal reflux. Electrometric determination of the acidity of the contents of the esophagus is carried out using a flexible intraesophageal probe attached to an acidogastrometer. pH-metry allows you to identify episodes of reflux of gastric juice and determine the conditions for their occurrence.
- Manometry. Registration of pressure in different parts of the gastrointestinal tract using special catheters with strain gauges verifies the weakening of the cardiac sphincter and dysmotility. A manometric study also provides an objective assessment of elasticity, tone, contractile activity of the esophageal wall, and pressure profiling in the esophagus.
If necessary, the examination is supplemented with gastrocardiomonitoring, gastrointestinal impedancemetry, bilemetry. X-ray studies of the esophagus during pregnancy are not performed. GERD is differentiated from functional dyspepsia, gastric and duodenal ulcers, acute infectious esophagitis, benign tumors and esophageal cancer. If extraesophageal symptoms are detected, differential diagnosis with angina pectoris, bronchial asthma may be required.
GERD is differentiated from functional dyspepsia, gastric and duodenal ulcers, acute infectious esophagitis, benign tumors and esophageal cancer. If extraesophageal symptoms are detected, differential diagnosis with angina pectoris, bronchial asthma may be required.
Treatment of GERD during pregnancy
Therapeutic tactics are aimed at the rapid elimination of clinical symptoms, restoration of the esophageal mucosa, prevention of complications and relapses. In 25% of cases, the condition can be improved by non-drug methods. Pregnant women with mild GERD are recommended to stop smoking, correct diet and diet with frequent small meals, reduce the amount of high-protein and low-lipid foods, and exclude citrus juices, chocolate, caffeine-containing drinks, spices, mint, and alcohol.
Care must be taken when using drugs that transiently reduce the tone of the cardia. Efficient sleep with a raised headboard, chewing chewing gum with calcium carbonate. Identification of severe clinical symptoms requires the appointment of special drug therapy. During pregnancy, some of the drugs used in standard treatment regimens for gastroesophageal reflux are used with caution due to possible effects on the fetus or the occurrence of obstetric complications. Patients with severe GERD are shown:
Identification of severe clinical symptoms requires the appointment of special drug therapy. During pregnancy, some of the drugs used in standard treatment regimens for gastroesophageal reflux are used with caution due to possible effects on the fetus or the occurrence of obstetric complications. Patients with severe GERD are shown:
- Nonabsorbable antacids and alginates. Considered 1st line drugs for the treatment of gastroesophageal reflux disease in pregnant women. By neutralizing hydrochloric acid, reducing the digestive capacity of pepsin, adsorbing lysolecithin, bile acids, improving the evacuation of stomach contents, stimulating the secretion of prostaglandins, antacids reduce the damaging effect of refluxate. Alginates have a protective effect on the esophageal mucosa.
- Histamine h3 receptor blockers. They are used when antacid therapy for GERD is ineffective. The antisecretory activity of selective histamine blockers is due to the action on the receptors of the parietal cells of the stomach.
 Due to inhibition of secretion, the acidity and volume of gastric contents decrease, which helps to reduce its aggressiveness and pressure on the cardiac sphincter. The effect of h3-histamine blockers on the fetus is not well understood, which limits their use.
Due to inhibition of secretion, the acidity and volume of gastric contents decrease, which helps to reduce its aggressiveness and pressure on the cardiac sphincter. The effect of h3-histamine blockers on the fetus is not well understood, which limits their use. - Proton pump inhibitors. High efficiency and rapid achievement of therapeutic results in the appointment of PPIs are based on blocking the secretion of hydrochloric acid at the level of the secretory tubules of parietal cells. The limited use of pump inhibitors is due to a decrease in the bactericidal properties of gastric juice, which, against the background of natural suppression of immunity, contributes to the development of food infections and impaired calcium absorption, which is necessary for the normal course of gestation.
As additional means, prokinetics that improve gastrointestinal motility and herbal enveloping preparations can be used. During gestation, surgical treatment of severe and complicated forms of GERD is not performed. Pregnancy is recommended to be completed by natural childbirth at a physiological time. Caesarean section is performed when obstetric indications are identified.
Pregnancy is recommended to be completed by natural childbirth at a physiological time. Caesarean section is performed when obstetric indications are identified.
Prognosis and prevention
With the appointment of adequate treatment, the damaged mucosa of the esophagus usually fully recovers after 4-12 weeks, with non-erosive variants of the disease, improvement occurs within 4-10 days. Prevention of gastroesophageal reflux involves the normalization of diet and lifestyle: giving up bad habits, adequate rest and sleep, controlling weight gain with a tendency to obesity, eliminating foods that irritate the esophageal mucosa or stimulate gastric hypersecretion, taking drugs that can disrupt gastrointestinal motility, only as directed and under medical supervision. To prevent recurrence of GERD in a pregnant woman, a 1-3-day intake of alginates and antacids "on demand" is recommended when symptoms appear.
You can share your medical history, what helped you in the treatment of GERD in pregnancy.
Sources
- Gastroesophageal reflux disease during pregnancy/ Elohina TB, Tyutyunnik VL// Experimental and clinical gastroenterology. - 2009 - No. 3.
- Pregnancy heartburn: an everyday trifle that must be endured, or gastroesophageal reflux disease that should be stopped? / Argunova IA// Gastroenterology. - 2015 - No. 3.
- Features of the course of gastroesophageal reflux disease in pregnant women/ Grishechkina IA, Kusakina AA, Miermanova MK// Young scientist. - 2015. - No. 13.
- Gastroesophageal reflux disease / Babak O.Ya., Fadeenko G.D. – 2000.
- This article was prepared based on the materials of the site: https://www.krasotaimedicina.ru/
IMPORTANT
Information from this section cannot be used for self-diagnosis and self-treatment. In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.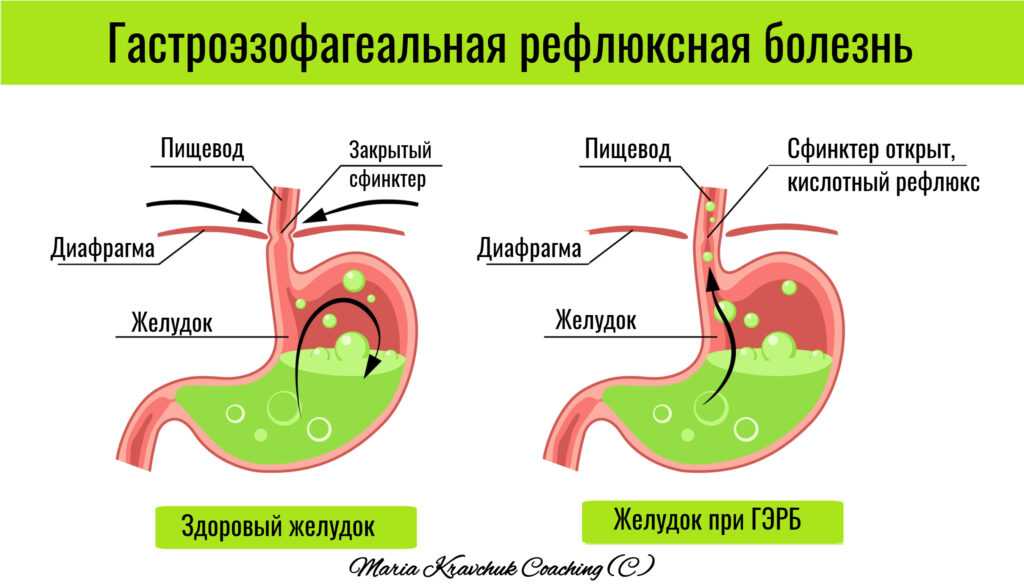
Toxemia, Intestinal Problems & Heartburn
Find out how pregnancy affects the digestive tract, which trimesters are more likely to cause indigestion and nausea, and what to do to manage them.
During pregnancy, the burden on the mother's body increases. The body needs more nutrients, the body produces additional hormones. And the growing fetus puts pressure on neighboring organs, including the stomach and intestines. We tell you what symptoms are observed in each trimester, how to cope with toxicosis and get rid of heartburn.
Contents:
- 2. Toxicosis and pregnancy
- 3. Causes, risks and treatment of diarrhea during pregnancy
- 4. Heartburn and stomach pain during pregnancy
- 5. Bloating, constipation and microbiota during pregnancy
- 6. Note
Changes in the functioning of the gastrointestinal tract by trimesters of pregnancy
The average duration of pregnancy is 40 weeks, which are usually divided into trimesters in accordance with the stages of intrauterine development of the child.
Each trimester is accompanied by a number of changes in the body, including in the gastrointestinal tract:
| The first trimester 26 weeks | Third trimester of pregnancy 27–40 weeks |
| Morning sickness Morning sickness 9 |
The Atlas Genetic Test will help you find out how your genes affect the level of female sex hormones necessary for fertility and pregnancy.
Causes of gastrointestinal problems during pregnancy
Every pregnancy is accompanied by inevitable changes in the functioning of the digestive system. They are most often caused by hormonal changes and increased stress on the organs, but they can also be associated with lifestyle and health conditions, for example:
- Sedentary lifestyle and unbalanced diet;
- Certain drugs, including calcium or aluminum antacids;
- Viral and bacterial infections;
- Intolerance to certain nutrients and allergic reactions;
- Stress;
- Diseases of the thyroid gland.
If you have chronic diseases of the gastrointestinal tract and you are planning a pregnancy, try to consult your doctor in advance. Symptoms of conditions such as irritable bowel syndrome (IBS) or acid reflux are more likely to get worse during pregnancy. Your doctor will help prepare your body and create a prevention plan to help relieve symptoms during this time.
Irritable bowel syndrome, or IBS, is a functional bowel disease that causes frequent abdominal pain, impaired peristalsis, bloating, constipation, or diarrhea.
Morning sickness, vomiting and general malaise during pregnancy
Morning sickness and morning sickness during early pregnancy are common, because the body undergoes important changes necessary for the development of the child.
up to 90%
women experience nausea during pregnancy
Doctors find it difficult to say with certainty why pregnant women feel sick in the morning. The main theory is hormonal changes. But there are some patterns associated with an increased risk of morning sickness:
The main theory is hormonal changes. But there are some patterns associated with an increased risk of morning sickness:
- Multiple pregnancy;
- Toxicosis during a previous pregnancy;
- History of morning sickness during pregnancy in close relatives;
- Tendency to motion sickness in transport;
- Use of oral contraceptives containing estrogen before pregnancy;
- Frequent migraines;
- BMI 30 and above;
- Increased levels of stress hormones
Risks of severe morning sickness and how to reduce nausea
Nausea and vomiting are usually not associated with a risk for mother and child and will pass by 16-20 weeks of pregnancy, but it is not necessary to wait so long - there are ways that can help reduce nausea and enjoy the process of waiting for a new person:
- Get plenty of rest - fatigue increases toxicosis;
- Avoid smells and foods that cause nausea;
- Eat something right after waking up.
 A toast or a slice of bread will help reduce nausea;
A toast or a slice of bread will help reduce nausea; - Avoid hunger - empty stomach increases nausea. Eat small meals often, prefer low-fat, high-carbohydrate foods;
- Try ginger - studies show it helps with nausea;
- Sip as often as possible and prefer still water.
Rarely, pregnant women may develop hyperemesis gestationis or excessive vomiting. This is a serious condition that can lead to dehydration, kidney damage, seizures, abnormal heart rhythms, and even death.
Signs of dehydration include dry mouth, dizziness, dark urine, infrequent urination and/or dizziness.
Symptoms of excessive pregnancy vomiting:
- frequent nausea for a long time and regular vomiting after meals;
- dry skin and lips;
- sudden weight loss;
- low blood pressure (below 90/60).
If symptoms of excessive pregnancy vomiting occur, do not wait until the condition resolves on its own.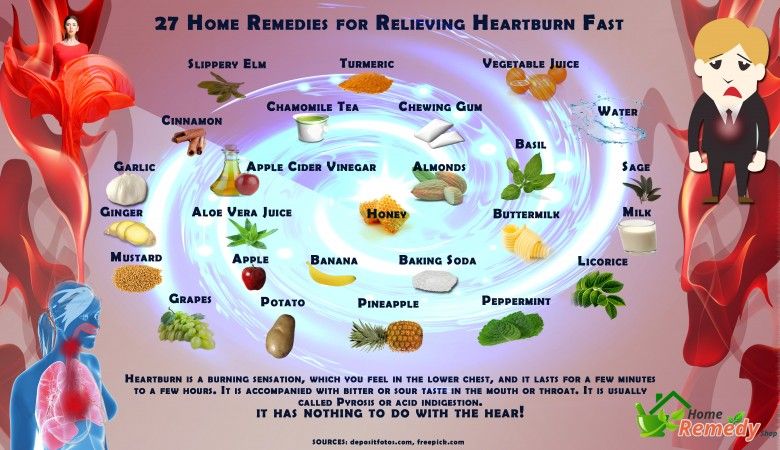 It is necessary to seek medical help as soon as possible - the doctor will prescribe treatment, help adjust the diet and lifestyle of the expectant mother.
It is necessary to seek medical help as soon as possible - the doctor will prescribe treatment, help adjust the diet and lifestyle of the expectant mother.
0.5–2%
pregnant women experience excessive vomiting
Diarrhea during pregnancy
The word "diarrhea" comes from the Greek language and literally means "to flow through". This is a condition during which bowel movements or bowel movements occur three times a day or more often. This phenomenon is especially typical for the third trimester of pregnancy, but it can also occur earlier.
Symptoms of diarrhea:
- Three or more bowel movements per day
- Urgent urge to have a bowel movement
- Abdominal pain and cramps
- Bloating
Causes of diarrhea during pregnancy poisoning, dysbacteriosis, bacterial and viral infections:
| Gastroenteritis | Lactose and gluten use for those intolerant to these nutrients |
| Bacterial infections: listeriosis or salmonella | Chronic gastrointestinal diseases: Crohn's disease, IBS, ulcerative colitis |
| Some antibiotics and antacids to reduce acidity | Laxatives |
| Sugar substitutes such as sorbitol | Overconsumption of certain foods |
Tip: If you have recently returned from a holiday in an exotic country with nausea and diarrhea and find out you are pregnant, see your doctor as soon as possible.
Gastroenteritis
One common cause of diarrhea during pregnancy is gastroenteritis, or stomach flu. It is caused by bacterial or viral infections: norovirus, rotavirus, E. coli, salmonella, which enter the body through contact with contaminated surfaces, dishes, food and water.
Gastroenteritis usually lasts about three days. However, severe illness is a health hazard, especially during pregnancy, as it can cause dehydration, electrolyte imbalance, and lead to preterm labor.
The main symptoms of gastroenteritis include diarrhea without blood, nausea and vomiting, stomach cramps and pain, slight fever, headache and muscle pain.
Take extra precautions to reduce your risk of getting sick: frequent handwashing and surface disinfection. If the expectant mother has small children, they are not recommended to use the same cutlery.
Risks of diarrhea during pregnancy
Usually diarrhea during pregnancy is not a cause for concern.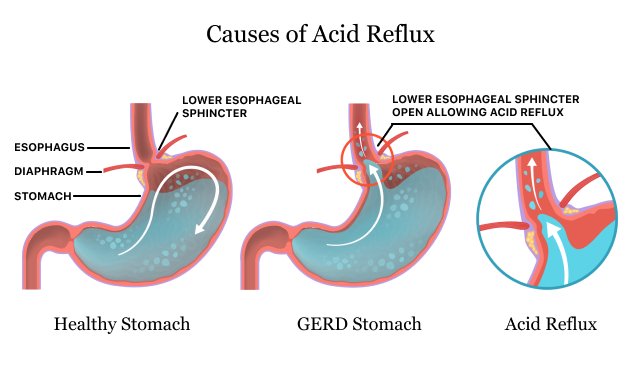 However, you should consult a doctor if the following symptoms occur during this period:
However, you should consult a doctor if the following symptoms occur during this period:
- Diarrhea for more than two days;
- Stools with blood or mucus;
- Sudden weight loss;
- Abdominal pain;
- Dehydration.
How to treat diarrhea during pregnancy
If you have diarrhea during pregnancy, drink plenty of fluids, avoid foods high in fat and sugar, avoid dairy products, and caffeinated drinks.
Dehydration is a serious risk, especially during pregnancy, so electrolyte balance should be restored first with fluids and simple foods:
| Moderate fruit juices | Drinks without alcohol and caffeine |
| Bananas | Potato |
| Rice | Toast |
| Rusks | Light soups and broths |
| Pasta | Applesauce |
Find out about your body's ability to break down lactose and gluten with the Atlas Microbiota Test.
Stomach pain and heartburn during pregnancy
Many women experience stomach pain during pregnancy, especially the upper part of the stomach, as well as heartburn - a burning sensation in the chest and esophagus.
This is more common in the third trimester, after about 27 weeks. This is an unpleasant but natural phenomenon during pregnancy: the baby grows inside the uterus and presses on other organs, including the stomach. And hormones cause the muscles to relax, which causes acid from the stomach to enter the esophagus and irritate it. In addition, pain can be caused by problems with certain organs such as the gallbladder, or inflammation of the pancreas.
Symptoms of heartburn during pregnancy:
- Burning in chest and esophagus;
- Feeling of overeating, heaviness or bloating;
- Belching, including with acid and/or food particles;
- Nausea.
Avoid cramps and heartburn during pregnancy is unlikely. However, some tips can help reduce their frequency:
However, some tips can help reduce their frequency:
Nutrition : try to avoid overeating - eat easily digestible food in small portions; do not eat three hours before bedtime; watch your posture while eating - so the pressure on your stomach will be less.
Smoking and alcohol: In addition to known harms to mothers and babies, tobacco smoke also relaxes the muscles in the lower esophagus, allowing acid to enter the esophagus. And alcohol provokes heartburn and acid reflux.
Although stomach pain and heartburn often accompany pregnancy, abdominal pain, especially in the third trimester, should be taken seriously. It can be a sign of preterm labor or placental abruption, and puts mother and baby at risk.
If you experience severe abdominal pain during pregnancy that is accompanied by the following symptoms, seek medical attention as soon as possible:
| Abdominal pain and fever | Bleeding |
| Regular seizures | Unusual vaginal discharge / spotting |
| Vomiting | Low back pain |
| Pain or burning when urinating | Severe pain that lasts 30-60 minutes |
Bloating, constipation and microbiota during pregnancy
Excessive gas and constipation during pregnancy can be caused by hormonal changes, such as increased production of progesterone. This hormone, essential for nourishing the uterus and fetus, relaxes the muscles of the body, including the muscles in the intestines, which slows down digestion and increases flatulence. A similar reaction of the body can be observed before each menstruation, when the production of progesterone increases.
This hormone, essential for nourishing the uterus and fetus, relaxes the muscles of the body, including the muscles in the intestines, which slows down digestion and increases flatulence. A similar reaction of the body can be observed before each menstruation, when the production of progesterone increases.
Flatulence - bloating of the abdomen due to the accumulation of gases.
Here are a few simple rules that will help improve intestinal motility and avoid constipation and bloating:
- If you don't usually eat a lot of fiber and indigestible foods like legumes, try to gradually introduce them into your diet;
- Avoid carbonated drinks and fatty foods;
- Move more;
- Drink plenty of fluids.
If bloating and constipation are accompanied by severe pain that lasts more than 30 minutes, or if you have been constipated for two or more weeks, see your doctor.
Gut microbiota and bacteria during pregnancy
A woman's body goes through many changes during pregnancy, and this can affect the microbiota, the bacterial ecosystem that lives in the gut. Trillions of microorganisms do important work for the whole body: they synthesize vitamins and essential acids, keep your intestines working and protect it from disease and inflammation.
Trillions of microorganisms do important work for the whole body: they synthesize vitamins and essential acids, keep your intestines working and protect it from disease and inflammation.
The additional influx of female hormones that accompanies pregnancy alters gut function and affects the microbiota. This is good, because the bacterial community is constantly adjusting to external and internal conditions in order to keep up with the needs of the body.
To keep your gut bacteria running smoothly, they need your help. Provide them with healthy foods and plant fibers. Fruits, vegetables, whole grains, nuts, and seeds contain prebiotics, special substances that beneficial bacteria feed on. When properly balanced, the bacteria even increase your body's defenses against harmful microorganisms that can cause gastroenteritis during pregnancy.
The Atlas Microbiota Test will help you understand how to prepare your intestines for future pregnancy and reduce the risk of digestive problems.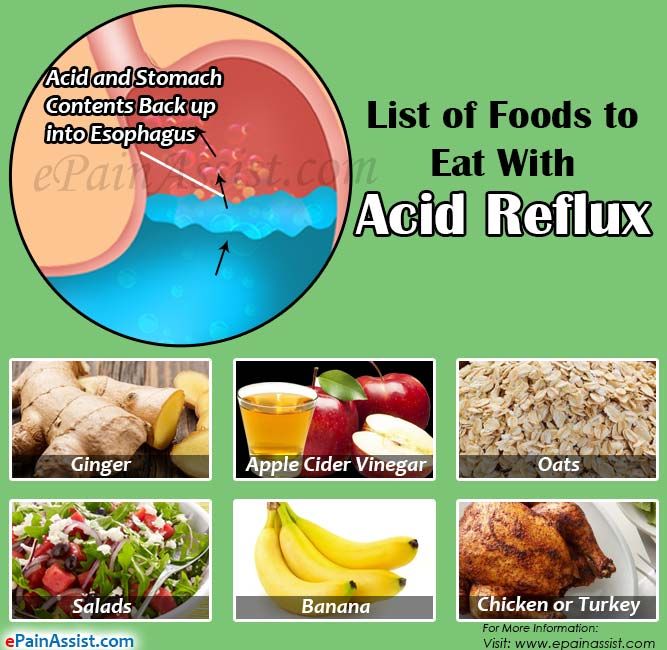
☝️ Take note
Now you have all the necessary knowledge and tools to help you cope with digestive problems during pregnancy. They are quite varied and quite natural, but in some cases it is necessary to immediately seek medical help:
- Vomiting blood;
- Blood in stool;
- Diarrhea for more than two days;
- Constipation for more than two weeks;
- Sudden weight loss;
- Severe pain interfering with daily activities;
- Difficulty breathing;
- Pain when swallowing or difficulty swallowing;
- Excessive fatigue.
More articles on the causes of digestive problems on the blog:
- 7 foods that cause gas and bloating
- Lindsey J Wegrzyniak, Treatment of Hyperemesis Gravidarum, 2012
- Edwards A. et al., The Maternal Gut Microbiome During Pregnancy, 2018
- National Health and Safety (NHS), Vomiting and morning sickness in pregnancy
- Kudzai Kanhutu, Travel and pregnancy: an infectious diseases perspective, 2011
- CDC, Pregnant travelers
- U.