How long do triplets stay in nicu
NICU Experience with Triplets | Milk 101 Article
by Melissa Hauser
I knew very early in my pregnancy that I was having triplets, and we would be spending time in a Neonatal Intensive Care Unit (NICU). My birthing plan was to make it to at least 31 weeks in order to have them at the level II NICU close to my house, and that my OBGYNs would deliver the triplets. After six weeks of bed rest, I delivered at 31 weeks and was the first and only triplets my OBGYNs have ever delivered. That always puts a smile on my face. They were as excited as I was.
I toured the NICU a few months before having the babies, so I had a rough idea how things would work. That doesn’t fully prepare you for a 6 week stay and all the things that go on around you. Right after delivery the babies were in open units, and by the time I was wheeled down to see them, they were hooked up to IVs, monitors, feeding tubes and oxygen. It is hard for a momma to get a good look at her babies like that. There was no holding them, I could only touch them and look at them. They were so tiny! Noah (aka Bubba) was 3lb 11oz, Harrison 2lb 15oz, and Chloe 3 lb. 1 oz.
For the first few days the triplets were being given nutrition through their IVs. None of the nurses that were taking care of me even mentioned breastfeeding or pumping, for that matter. I didn’t really have warm fuzzies about breastfeeding three babies, so it didn’t bother me at the time. In my mind I pictured myself being hooked up to a baby all the time. By day three, the babies were ready to receive nutrition through the feeding tube, and the NICU nurses started talking to me about pumping, aggressively, to the point that I felt pressured and guilted into pumping and even felt the nurses were being mean to me because I didn’t want to pump.
Before going home on day 4, I decided to pump, and let me just say, it was not a good experience for me. It was very difficult to get the colostrum/milk flowing. I can remember the lactation consultant squeezing, and it really hurt. On the bright side, the NICU nurses were much nicer too me after that. Hindsight has me thinking about the advice I would give the hospital about how to work with NICU mommies, better ways to talk to moms about breastfeeding, and the benefits for the babies, especially premature babies.
On the bright side, the NICU nurses were much nicer too me after that. Hindsight has me thinking about the advice I would give the hospital about how to work with NICU mommies, better ways to talk to moms about breastfeeding, and the benefits for the babies, especially premature babies.
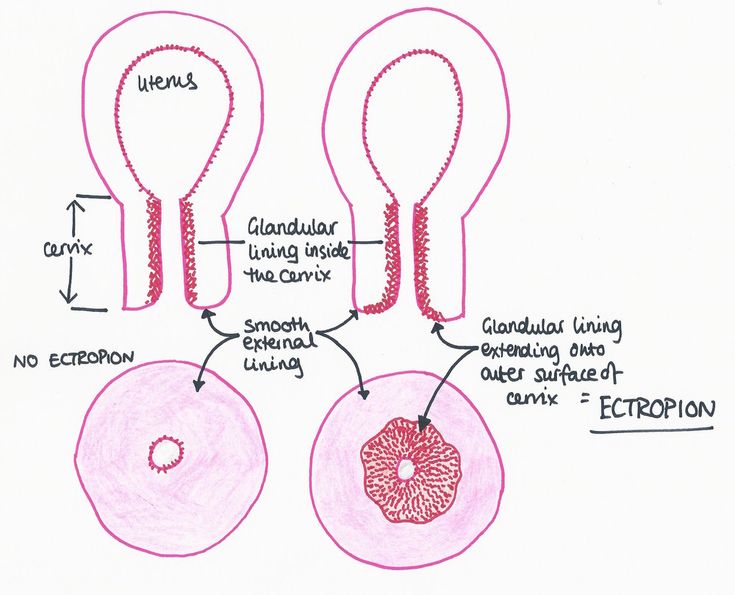
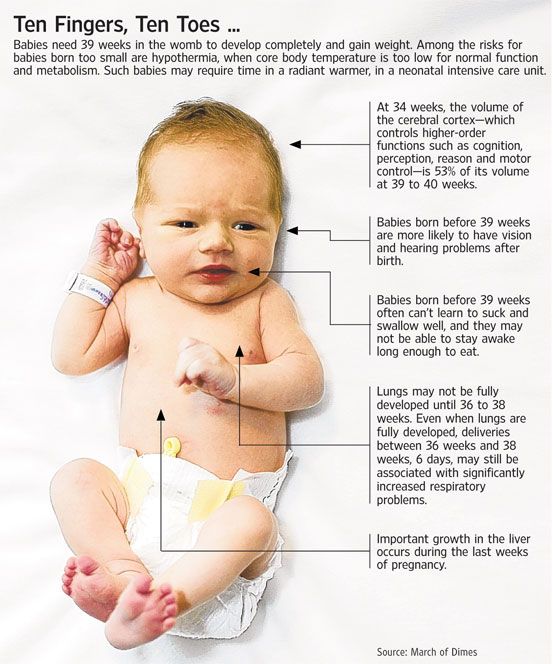
I began my daily routine for the kids: get up, pump, go to the hospital, hold each baby for a little bit, pump, eat lunch, hold babies, pump, hold babies, pump … Because the babies were so early they didn’t have a suck reflex and all the milk was given to them through the feeding tube. We would hold one of them and also have to hold the tube up in the air to let gravity take the milk to the stomach. All of this was attached to a large mechanical thing that monitored them. This went on through their 34/35 weeks, until the neonatologist felt the babies could start learning to suck.
Premature babies in the NICU are treated very different when it comes to feeding. Every cc the babies ingest is measured and charted. I was never given an option to physically try and breastfeed. I always had to pump, and then it was put into a bottle. I was never able to establish a good milk supply. I took supplements, ate well, got sleep, but I was never able to get more than 2-4 oz at a time. Four ounces was a great pump for me. Maybe if I had been allowed to pump near the babies, I would have produced more. You just don’t know. I never had the experience of feeling my milk coming in. I just pumped on a schedule. I made it four weeks pumping and then decided to stop. It is hard when you know you are not supplying your babies with enough milk on your own. It left me feeling a little defeated.
I was never given an option to physically try and breastfeed. I always had to pump, and then it was put into a bottle. I was never able to establish a good milk supply. I took supplements, ate well, got sleep, but I was never able to get more than 2-4 oz at a time. Four ounces was a great pump for me. Maybe if I had been allowed to pump near the babies, I would have produced more. You just don’t know. I never had the experience of feeling my milk coming in. I just pumped on a schedule. I made it four weeks pumping and then decided to stop. It is hard when you know you are not supplying your babies with enough milk on your own. It left me feeling a little defeated.
Nursing was the hardest thing for the babies to learn and for me to have go through with them. Each baby had to learn the process of sucking, swallowing and breathing. They were hooked up to monitors that measured their oxygen intake and an alarm would go off when they went below 84. This happened a lot the first week they were learning. It took months for me to get that alarm out of my head. Feeding time was a scary time for a while always looking at the monitors to make sure everything was OK. It was wonderful to come in in the morning and hear that they did great during feedings throughout the night.
It took months for me to get that alarm out of my head. Feeding time was a scary time for a while always looking at the monitors to make sure everything was OK. It was wonderful to come in in the morning and hear that they did great during feedings throughout the night.
To come home, each baby had to reach the goal of drinking 2oz of milk and having no breathing episodes. They had other goals, but this was the really important one. One by one they were starting to meet this goal. Noah was the first one to come home after about 5 weeks in the NICU. At 5 lbs. 6oz, he was still my big boy. Harrison was able to come home just two days later weighing 5lbs. The little princess had the most trouble, she was only drink 1 oz of milk at a time. The NICU nurses finally said she just needed to go home because they felt she would do better. They were right.
It has been almost eight years since my munchkins where in the NICU. I thank God every day that they are healthy and happy kids that drive their momma crazy. I hope the hospital that I delivered in has advanced in the way they promote breastfeeding and or pumping and the way they treat moms who feel that it is not something they feel comfortable doing.
I hope the hospital that I delivered in has advanced in the way they promote breastfeeding and or pumping and the way they treat moms who feel that it is not something they feel comfortable doing.
DISCLAIMER:
Ameda strives to present you with accurate and useful breastfeeding information. This article may contain information and ideas that are not necessarily the views of Ameda. It does not constitute medical advice. If you have any questions please contact your healthcare professional.
What to expect if your multipes have to spend time in the NICU
Go to any twin mom club, Facebook group, or baby board, and the most commonly asked question by expectant twin moms is:
“How far along were you when you delivered and how long was your NICU stay?”
Your chances of preterm labor and delivery increase with each additional baby you are growing, as well as your type of twin pregnancy (mono/mono, mono/di, di/di).
Preterm labor is defined as delivery before 37 weeks and most doctors will not let a multiple birth go past 38 weeks. Nearly 60 percent of all twins, and more than 90 percent of triplets, are born prematurely (before 37 weeks). WHOA.
On average, twin pregnancies last 35 weeks, triplet pregnancies last 33 weeks and quad pregnancies last 29 weeks. Remember these are averages, so there are definitely MOMs out there that went all 40 weeks (or beyond 😮), and others that delivered earlier.
Most of this is out of your control, so there is no use in stressing over it. Just be sure to take care of yourself: lots of rest, fluids, and frequent healthy snacks.
The bottom line is: the earlier you deliver, (usually) the longer the NICU stay. Just as every pregnancy and delivery is different, every NICU stay is also a little different. There are babies born at 38 weeks that need NICU time, while others born at 35 weeks don’t stay in the NICU at all. So keep in mind these are just averages. A good rule of thumb is to expect to be in the NICU until your original due date.
A good rule of thumb is to expect to be in the NICU until your original due date.
And if you don’t have to, then you’ll be pleasantly surprised 🙂
Preterm Birth Milestones
I know some of this stuff is scary to read about, but this is life with multiples. Most people enjoy having this info, but if you’d rather not know (we understand!), skip over this section…
- 23 weeks is considered to be the age of viability; over half of the babies born at this time will survive past the NICU. These micro preemies will need help breathing and support to finish developing their body’s systems. They will most likely need to stay in the NICU for several months.
- At 27 weeks babies are no longer micro preemies! They are now “very premature” and have a much higher rate of survival – 95%. Their eyelids are no longer fused and their lungs are more developed (although they still might need help breathing). They have developed the startle reflex and have coordinated sleep/awake cycles.

- At 32 weeks babies are now “moderately preterm”. This week babies can mostly control their own body temperatures. They might still need help eating or breathing on their own, which are milestones required for NICU discharge. On average, babies born at 32 weeks will stay in the NICU for about a month. Making it to 32 weeks was my first “goal”, since babies born on or past this point have less chance of life-threatening complications. 32 week-ers have a 98% survival rate.
- 34 weeks was my next “goal”. Most doctors will not stop preterm labor at 34 weeks or later. These babies are in their final stages of lung development, and are fine-tuning the suck-swallow-breathe reflex needed for successful eating. This means that babies born at 34 weeks may not need much, or any, assistance breathing or eating.
- At 36 weeks, “late preterm” babies might only need a little help growing and feeding. These babies may only be in the NICU for a few weeks, until they can maintain their body temperatures, master feeding and breathing simultaneously, and breathe on their own.

The NICU [pronounced NICK-you]:
Neonatal Intensive Care Unit
Now that you know the milestones, let’s talk about what to expect in the NICU.
Usually, no matter how you deliver (vaginally or via c-section), if the babies are preterm, your OB will likely first show them to you (Yay! Hi babies!), and then they will be whisked away to get checked out by the neonatal staff. The staff are usually in the delivery or an adjacent room, and if the babies don’t require oxygen or any kind of immediate help, once they are assessed, the neonatal staff will bring them back to you.
If they do need immediate intervention, your partner can go with the babies while your OB finishes up with you. Plan for who will go where ahead of time so you’re not stressing about it in the moment. Keep in mind that both babies may not have the same prognosis; many times, one baby will need to go to the NICU while the other can stay with mom.
For an uplifting and beautiful book that helps families navigate and document their NICU journeys, check out Our NICU Journey: Tiny Keepsake for Tiny Miracles. This book also serves as a lovely reminder to families with babies in the NICU that they are most definitely not alone.
This book also serves as a lovely reminder to families with babies in the NICU that they are most definitely not alone.
NICU tips:
- Depending on your condition, you may not be able to go see your babies right away in the NICU. Send your partner to keep you updated and informed.
- The nurses are your best friends. Ask them all the questions you have and tell them your concerns. They will help you in every way possible and be your daily support system.
- Be clear on your wishes. All of our doctors and nurses knew I was pumping; the girls were to have my breast milk first, and then formula if needed. We wanted to be there for every feeding so, if possible, they would wait for us to arrive.
- Don’t forget to take care of yourself. The best gift we got in the hospital was a snack care package: almonds, cookies, granola bars and fruit. It got us (mostly me) through the few days we we had to camp out at the hospital. I needed to eat all the time to help build my breast milk supply.
 I also brought my HUGE water bottle from pregnancy with to make sure I stayed hydrated. The nurses were very insistent about making sure we slept. They encouraged us to get some rest even if it meant missing a feeding. They helped us realize that we needed to put our own “oxygen masks” on first before we could care for our babies.
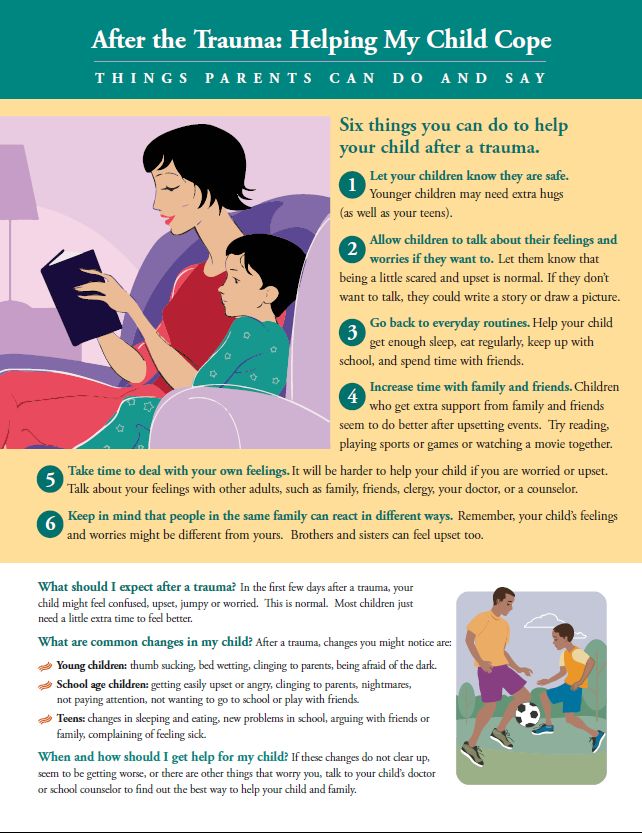
I also brought my HUGE water bottle from pregnancy with to make sure I stayed hydrated. The nurses were very insistent about making sure we slept. They encouraged us to get some rest even if it meant missing a feeding. They helped us realize that we needed to put our own “oxygen masks” on first before we could care for our babies. - The entire experience will probably be emotionally difficult. You might feel helpless and worried, but you will get through it.
- NICU nurses sing, rock the babies, and comfort them when you are not there. It is important to remember your babies are being cared for while you are unable to be there.
- Call the NICU as much as you want. You won’t be bothering them and they are happy to talk with you about how your baby is doing. You can even call when you are up pumping at 3 am.
- Be prepared for separation: you from the babies, and the babies from each other.
- Take care of yourself. Did I say this already? The NICU is hard.
 You have no control, you feel like you can’t help, and that you are useless as a parent. It was the most stressful, overwhelming, difficult time in my life. Not to mention your body is already whacked from all your hormones after giving birth. So give yourself a break; have a good cry and just remember that you can do this. If you are feeling too overwhelmed, talk to your doctor or the nurses. They are there to help you.
You have no control, you feel like you can’t help, and that you are useless as a parent. It was the most stressful, overwhelming, difficult time in my life. Not to mention your body is already whacked from all your hormones after giving birth. So give yourself a break; have a good cry and just remember that you can do this. If you are feeling too overwhelmed, talk to your doctor or the nurses. They are there to help you. - Don’t worry about anyone else. I was in no shape to be updating everyone on FB or via text. I called my mom when I could. She shared the information with my close family and friends. Don’t let anyone make you feel guilty. If your MIL or Grandma is upset because they want an update, then they need to reach out and be ready to wait for a response. If you say “no visitors”, they need to suck it up and respect that. The nurses are a great help here: if you don’t want to be the “bad guy”, they will tell your sister she can’t come in, or that the baby is sleeping, so no visitors.
 NICU’s usually won’t allow anyone in without a parent present, and have a strict limit of how many visitors can be there at one time. Special Nurseries may not allow visitors at all. Children are usually not allowed in the NICU, especially for the higher levels of care. Prepare for this if you have older children.
NICU’s usually won’t allow anyone in without a parent present, and have a strict limit of how many visitors can be there at one time. Special Nurseries may not allow visitors at all. Children are usually not allowed in the NICU, especially for the higher levels of care. Prepare for this if you have older children. - Finally, remember that this too shall pass. Though hard to believe when you’re going through it, your NICU stay is a small blip in your vast lifetime with your babies. There will come a day when you will all be home and back together again. Keep that perspective in mind.
Don’t stress, parents, you’ve got this!!
— the Lucie’s List team
Read a singleton mom’s NICU experience here.
Did you miss?
- Recognizing Preeclampsia
- Gestational Diabetes
About the Author
Marissa Bader is our Twins Editor and mental health writer, as well as the author of the children's book, The Only Me. She holds a BA in journalism and a MA in marriage and family therapy. Mama to twins girls and their singleton big sis, when she’s not kissing owies, playing dress-up, or mediating sister squabbles, Marissa enjoys dancing (you should see her get down when nobody’s watching!), and writing about topics pertaining to mental health, wellness, fitness and parenthood. Marissa lives in the frozen tundra, aka, Minneapolis, MN.
She holds a BA in journalism and a MA in marriage and family therapy. Mama to twins girls and their singleton big sis, when she’s not kissing owies, playing dress-up, or mediating sister squabbles, Marissa enjoys dancing (you should see her get down when nobody’s watching!), and writing about topics pertaining to mental health, wellness, fitness and parenthood. Marissa lives in the frozen tundra, aka, Minneapolis, MN.
Children in the palm of your hand
Alexey. Born in April 2015 on the 32nd week of pregnancy. Birth weight - 2000 grams, height - 44 centimeters.
Mom remembers Aleksey, Nina Gubareva:
- My husband and I have been together since 2006. The pregnancy was long-awaited. From the very beginning of pregnancy, everything was not very good. WITH On the 7th week, my uterus began to tone, I lay 3 times on conservation. At 26 weeks I was placed in the 4th maternity hospital, the disclosure began ... Thank God, the process was successfully stopped. Then, I remember, the doctor told me: if you give birth now, the child will die or remain profoundly disabled. Then I clearly decided - it is necessary to convey at least up to 30 weeks. If talk about hurrying, then for them every week in the womb is a chance for life.
Then, I remember, the doctor told me: if you give birth now, the child will die or remain profoundly disabled. Then I clearly decided - it is necessary to convey at least up to 30 weeks. If talk about hurrying, then for them every week in the womb is a chance for life.
In general, I took care of myself as best I could. But at 32 weeks I got sick. Very strong cough aggravated my hypertonicity, contractions began. Further as in a fog: an ambulance, the Russian Orthodox Church, dropper with ginepral - the doctor was still trying to stop the contractions. Outcome - emergency cesarean.
I remember everything, I specifically refused general anesthesia, I wanted to hear my son's cry and see him. He was so small - 2 kg and 44 cm, but he breathed on his own. However, after 5 hours he was connected to the ventilator, he could not breathe.
The next morning I got up after the operation and walked sideways along the wall to look for my son. To me they said he was in the OP. Arriving there, I did not find it, I immediately realized that the trouble was. He lay in intensive care in an incubator. So small, in tubes, in droppers. God, I cried so much. I was choking with anger at myself that it was my fault that he was hurting.
Arriving there, I did not find it, I immediately realized that the trouble was. He lay in intensive care in an incubator. So small, in tubes, in droppers. God, I cried so much. I was choking with anger at myself that it was my fault that he was hurting.
It's terrible to see your child in such a state between life, death and the unknown.
It was hard to be discharged from the hospital without a child - you see the happiness of other mothers, but yourself, quietly taking her husband's hand, you get into a taxi and go home without your son. Traveled every day to the intensive care unit, then to the emergency room. Doctors said that the child's condition was moderate. Was it is not clear what awaits us: blindness, deafness, problems in neurology? Nobody could give response and exact guarantee. They said that the brain is immature, hypoxia, cerebral ischemia and still a bunch of diagnoses on the whole sheet.
In general, our son is a hero, breathless. days We spent ten in intensive care. Then we were sent to the OPN to gain weight and learn to eat. I had to feed the baby for 1.5 hours with 30 ml of the mixture, it was very difficult. After all, the usual the child eats such a portion in 5 minutes.
Then we were sent to the OPN to gain weight and learn to eat. I had to feed the baby for 1.5 hours with 30 ml of the mixture, it was very difficult. After all, the usual the child eats such a portion in 5 minutes.
We were discharged with a weight of 2300 grams home. A little baby who can’t even keep warm and eat properly, a lot of diagnoses and fear. During the year we went through a lot, a huge number of doctors, 5 courses massage, exercise therapy, permanent ultrasound, rehabilitation and daily activities, as if in an Olympic school.
Of course, we were lagging behind in development. It was often unpleasant to hear: "Ah Are you still not sitting at 7 months? ”, When the son only rolled over from his back to belly at 7.5 months. But all our “skills” brought such happiness! I'm proud of my son. I am grateful to him, he taught me to live and love for real. He taught me to be mom.
Now he is one and a half years old, he is very smart. He loves music, constructor and cars and is always smiling, a very kind kid.
Yekaterinburg | Happiness cubed: triplets
were born in YekaterinburgPhoto: xn--80acgfbsl1azdqr.xn--p1ai
Newborns were born in the obstetric hospital No. 1 of the ECPC.
Two boys and a girl were born in obstetric hospital No. 1 of the Yekaterinburg Clinical Perinatal Center (EKPC).
The center's specialists operated on a mother at the 34th week of pregnancy due to high blood pressure - preeclampsia. According to doctors, this is one of the most serious complications that occur in women during pregnancy.
Thanks to the well-coordinated work of the ERPC staff and the timely decision on delivery, the mother of many children and newborns feel well.
Babies born with low and very low birth weight are now under the supervision of doctors. Two of them were transferred to the neonatal intensive care unit, where they are with their mother. The third child still needs respiratory support, so for now he remains in the intensive care unit for newborns. But from day to day he will also be transferred to the ward to his mother, brother and sister.
But from day to day he will also be transferred to the ward to his mother, brother and sister.
This is the first pregnancy for Tatiana, she came on her own. The fact that there will be a triple replenishment in the family, the expectant mother found out already at the 11th week. During pregnancy, she managed to come up with names for all the children and named them immediately after birth.
Text and photo prepared by Yana Lomaeva
Triplets were born in Yekaterinburg
Two boys and a girl were born in obstetric hospital No. 1 of the Yekaterinburg Clinical Perinatal Center (EKPC).
10:20 12/14/2019 UralWeb.Ru - Yekaterinburg
Triplets were born in Yekaterinburg
Two boys and a girl were born in obstetric hospital No. 1 of the Yekaterinburg Clinical Perinatal Center (EKPC).
09:50 12/14/2019 UralWeb.Ru - Yekaterinburg
Happiness cubed: a resident of Yekaterinburg gave birth to triplets
Two boys and a girl were born in a perinatal center. A resident of the Ural capital named Tatyana recently became a mother for the first time.
A resident of the Ural capital named Tatyana recently became a mother for the first time.
16:51 12/13/2019 Ural worker - Yekaterinburg
A resident of Yekaterinburg gave birth to triplets
Triplets were born in the Ural capital. Two boys and a girl were born in obstetric hospital No. 1 of the Yekaterinburg Clinical Perinatal Center (EKPC).
16:41 12/13/2019 Nakanune.Ru - Yekaterinburg
Happiness cubed: triplets were born in Yekaterinburg
Newborns were born in obstetric hospital No. 1 of the ECPC. Two boys and a girl were born in obstetric hospital No. 1 of the Yekaterinburg Clinical Perinatal Center (EKPC).
16:17 12/13/2019 Administration of Yekaterinburg - Yekaterinburg
A rare case: triplets were born in the maternity hospital of Yekaterinburg
The mother-to-be found out that the family will have three children at the 11th week of pregnancy The condition of the mother and her babies now does not cause concern Photo:
15:21 12/13/2019 e1. Ru - Yekaterinburg
Ru - Yekaterinburg
e1.Ru An electronic birth certificate will allow paying for medical services to pregnant women, mothers and newborns, regardless of the place of their provision on an extraterritorial basis.
City Hospital No. 4 Turin urban district API JustMedia Ministry of Health Ural worker Tonight, a 12-year-old boy tragically died in the Chelyabinsk region.
EaNews.Ru Operational services have begun preparations for the season of forest fires. On March 9, a review of equipment took place in Pervouralsk.
city news photo: pexels EKATERINBURG. In the Sverdlovsk region on March 11, sleet, deposits in the form of sleet and wind with gusts of up to 20 m/s are expected.
API Since December 2022, an unfavorable epidemiological situation for measles has developed in the Russian Federation: multiple introductions of the infection are recorded with spread in medical organizations.