How long can postpartum psychosis last
Postpartum psychosis - NHS
Postpartum psychosis is a serious mental health illness that can affect someone soon after having a baby. It affects around 1 in 500 mothers after giving birth.
Many people who have given birth will experience mild mood changes after having a baby, known as the "baby blues". This is normal and usually only lasts for a few days.
But postpartum psychosis is very different from the "baby blues". It's a serious mental illness and should be treated as a medical emergency.
It's sometimes called puerperal psychosis or postnatal psychosis.
Symptoms of postpartum psychosis
Symptoms usually start suddenly within the first 2 weeks after giving birth - often within hours or days of giving birth. More rarely, they can develop several weeks after the baby is born.
Symptoms can include:
- hallucinations - hearing, seeing, smelling or feeling things that are not there
- delusions – thoughts or beliefs that are unlikely to be true
- a manic mood – talking and thinking too much or too quickly, feeling "high" or "on top of the world"
- a low mood – showing signs of depression, being withdrawn or tearful, lacking energy, having a loss of appetite, anxiety, agitation or trouble sleeping
- sometimes a mixture of both a manic mood and a low mood - or rapidly changing moods
- loss of inhibitions
- feeling suspicious or fearful
- restlessness
- feeling very confused
- behaving in a way that's out of character
When to get medical help
Postpartum psychosis is a serious mental illness that should be treated as a medical emergency. It can get worse rapidly and the illness can risk the safety of the mother and baby.
It can get worse rapidly and the illness can risk the safety of the mother and baby.
See a GP immediately if you think you, or someone you know, may have developed symptoms of postpartum psychosis. You should request an urgent assessment on the same day.
You can call 111 if you cannot speak to a GP or do not know what to do next. Your midwife or health visitor may also be able to help you access care.
Call your crisis team if you already have a care plan because you've been assessed as being at high risk of developing postpartum psychosis.
Go to A&E or call 999 if you think you, or someone you know, may be in danger of imminent harm.
Be aware that if you have postpartum psychosis, you may not realise you're ill. Your partner, family or friends may spot the signs and have to take action.
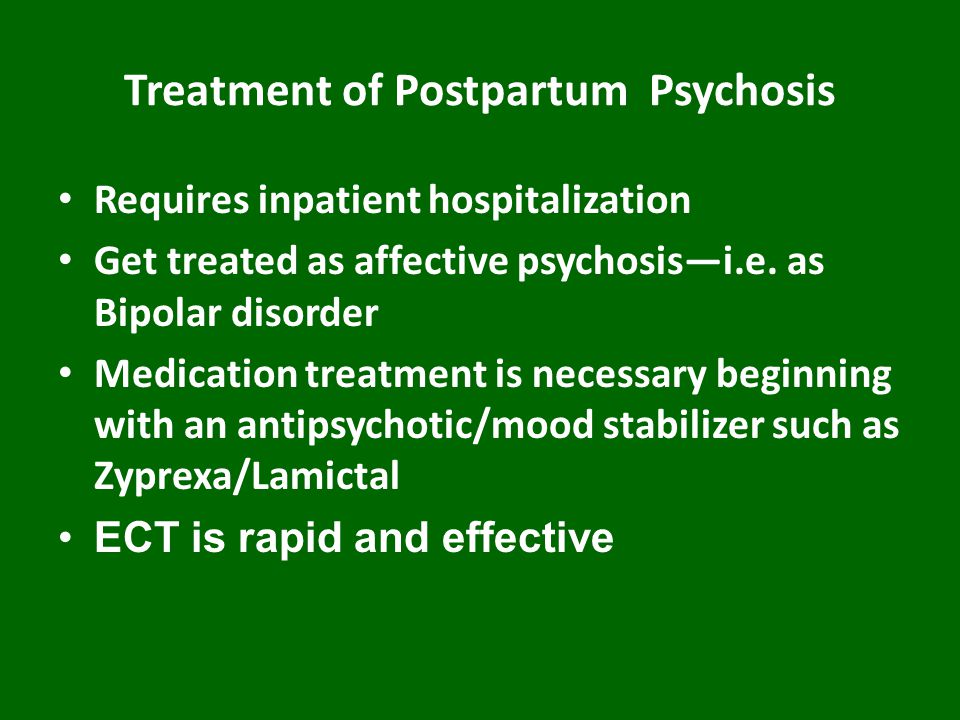
Treating postpartum psychosis
Treatment usually happens in hospital. Ideally, this would be with your baby in a specialist psychiatric unit called a mother and baby unit (MBU). But you may be admitted to a general psychiatric ward until an MBU is available.
Ideally, this would be with your baby in a specialist psychiatric unit called a mother and baby unit (MBU). But you may be admitted to a general psychiatric ward until an MBU is available.
Medicine
You may be prescribed 1 or more of the following:
- antipsychotics – to help with manic and psychotic symptoms, such as delusions or hallucinations
- mood stabilisers (for example, lithium) – to stabilise your mood and prevent symptoms recurring
- antidepressants – to help ease symptoms if you have significant symptoms of depression and may be used alongside a mood stabiliser
Electroconvulsive therapy (ECT)
Electroconvulsive therapy (ECT) is sometimes recommended if all other treatment options have failed, or when the situation is thought to be life threatening.
Most people with postpartum psychosis make a full recovery as long as they receive the right treatment.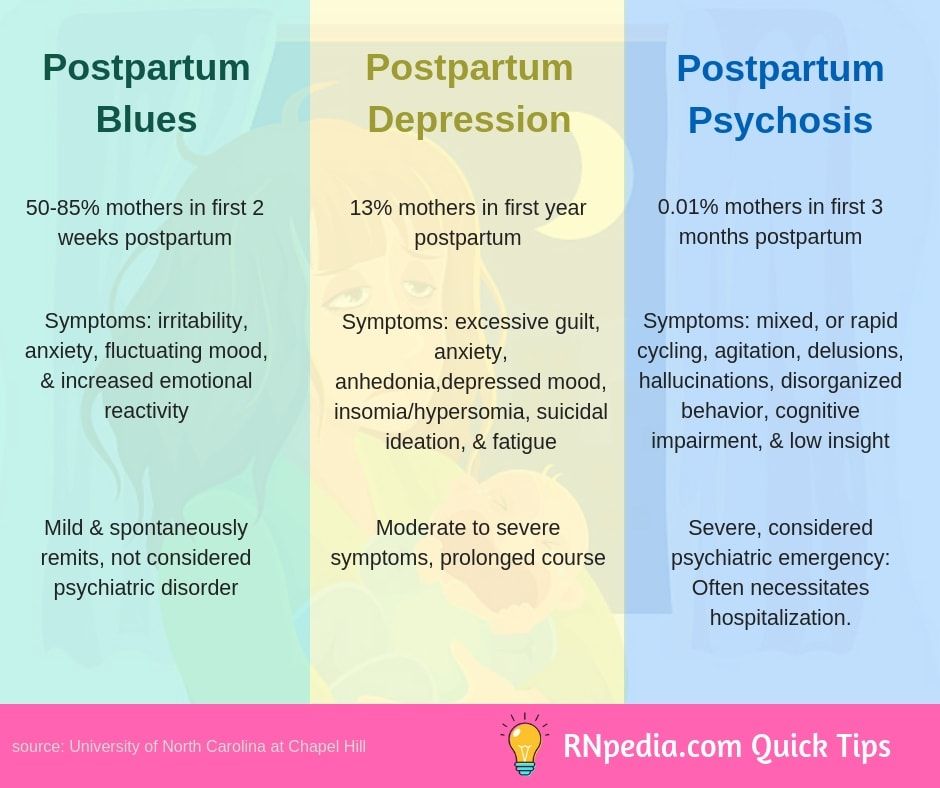
Psychological therapy
As you move forward with your recovery, you may benefit from seeing a therapist for cognitive behavioural therapy (CBT). CBT is a talking therapy that can help you manage your problems by changing the way you think and behave.
Other forms of support
It can be hard to come to terms with the experience of postpartum psychosis as you recover.
Talking to peers and others with lived experience of the illness may be helpful. Some inpatient units and communities have peer support workers who have experienced the illness, and you can also access support through charities.
Causes
We're not sure what causes postpartum psychosis, but you're more at risk if you:
- already have a diagnosis of bipolar disorder or schizophrenia
- have a family history of mental health illness, particularly postpartum psychosis (even if you have no history of mental illness)
- developed postpartum psychosis after a previous pregnancy
Reducing the risk of postpartum psychosis
If you're at high risk of developing postpartum psychosis, you should have specialist care during pregnancy and be seen by a perinatal psychiatrist.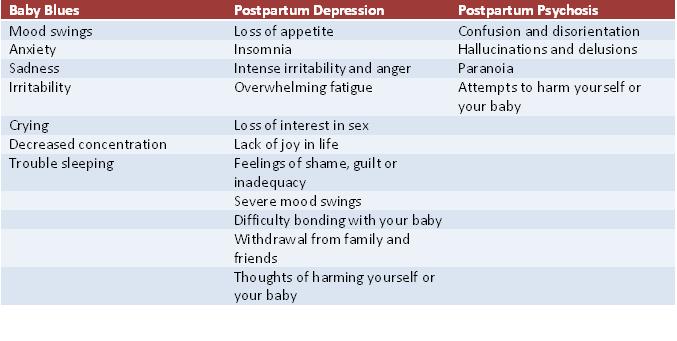
You should have a pre-birth planning meeting at around 32 weeks of pregnancy with everyone involved in your care. This includes your partner, family or friends, mental health professionals, your midwife, obstetrician, health visitor and GP.
This is to make sure that everyone is aware of your risk of postpartum psychosis. You should all agree on a plan for your care during pregnancy and after you've given birth.
You'll get a written copy of your care plan explaining how you and your family can get help quickly if you become ill, as well as strategies you can use to reduce your risk of becoming ill.
In the first few weeks after your baby is born, you should have regular home visits from a midwife, health visitor and mental health nurse.
Recovering from postpartum psychosis
The most severe symptoms tend to last 2 to 12 weeks, and it can take 6 to 12 months or more to recover completely from the condition. But with treatment and the right support, most people with postpartum psychosis do make a full recovery.
But with treatment and the right support, most people with postpartum psychosis do make a full recovery.
An episode of postpartum psychosis is sometimes followed by a period of depression, anxiety and low confidence. It might take a while for you to come to terms with what happened.
Some mothers have difficulty bonding with their baby after an episode of postpartum psychosis, or feel some sadness at missing out on time with their baby. With support from your partner, family, friends and your mental health team, or talking to others with lived experience, you can overcome these feelings.
Many people who've had postpartum psychosis go on to have more children. Although there is about a 1 in 2 chance you will have another episode after a future pregnancy, you should be able to get help quickly with the right care and the risks can be reduced with appropriate interventions.
Support for postpartum psychosis
Postpartum psychosis can have a big impact on your life, but support is available.
It might help to speak to others who've had the same condition, or connect with a charity.
You may find the following links useful:
Action on Postpartum Psychosis (APP)
Action on Postpartum Psychosis (APP) have produced a series of guides with the help of women who have experienced postpartum psychosis.
These guides cover topics such as:
- recovering from postpartum psychosis
- supporting partners
- planning pregnancy
- parenting after postpartum psychosis
- pregnancy for women with bipolar disorder
There is also an APP forum, where you can connect with others affected by postpartum psychosis.
Other useful links
- Mind: what is postpartum psychosis?
- Royal College of Psychiatrists: postpartum psychosis
Supporting people with their recovery
People with postpartum psychosis will need support to help them with their recovery.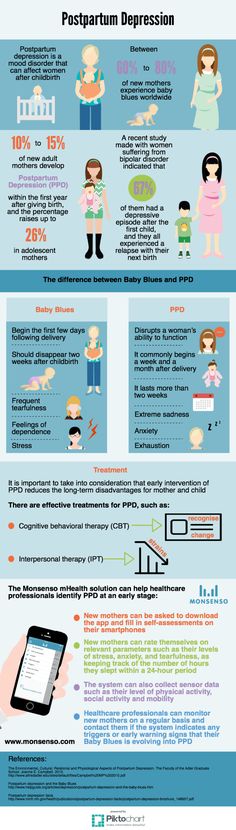
You can help your partner, relative or friend by:
- being calm and supportive
- taking time to listen
- helping with housework and cooking
- helping with childcare and night-time feeds
- letting them get as much sleep as possible
- helping with shopping and household chores
- keeping the home as calm and quiet as possible
- not having too many visitors
Support for partners, relatives and friends
Postpartum psychosis can be distressing for partners, relatives and friends, too.
If your partner, relative or friend is going through an episode of postpartum psychosis or recovering, do not be afraid to get help yourself.
Talk to a mental health professional or approach the charities listed.
Postpartum psychosis | Royal College of Psychiatrists
Urgent help
If you start to have symptoms of postpartum psychosis, you need to be seen urgently.14 If you have been told, during pregnancy, that you have a high risk of postpartum psychosis, look at your care plan. This should have emergency contact numbers for your mental health team or local crisis service.
If you don’t have this type of plan, or have not had a mental illness before, see your GP urgently (the same day) or go to your local A&E department. If you are told you do not have postpartum psychosis but your symptoms then get worse, go back to be re-assessed.
Most women with postpartum psychosis need to be treated in hospital. Ideally you should be offered a bed in a Mother & Baby Unit (MBU).14 This is a specialist psychiatric unit where mothers with mental illness are admitted with their babies. You will be supported in caring for your baby whilst you have the care and treatment you need.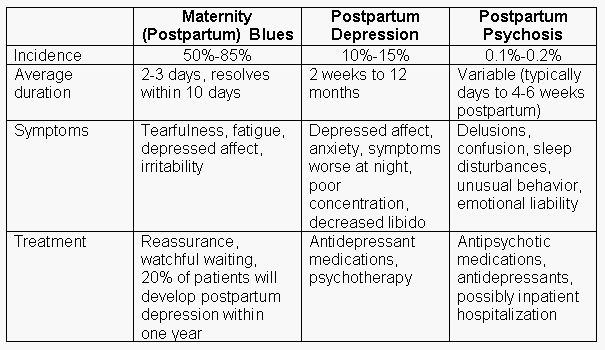 See our page on Mother & Baby Units for more information.
See our page on Mother & Baby Units for more information.
If there is no MBU, bed available, you may have to come into a general psychiatric ward. If that happens, your partner or family will need to care for your baby. If you have nobody else who can look after your baby, social workers can find a temporary carer. This will only be until an MBU bed is available, or until you are well enough to care for your baby yourself. You may prefer to be admitted to a local general ward if the nearest specialist MBU is far from your home.
Medication and breastfeeding
If you have a postpartum psychosis, you will probably need treatment with an antipsychotic ;medication, a mood stabiliser or both13-14,18
You can breastfeed whilst taking some medications.13,14 Discuss the risks and benefits of doing this with your psychiatrist.
You may find that you can’t breastfeed. You may be too unwell, or may have to be in hospital without your baby. You may need a medication which is not safe in breastfeeding. You might feel guilty about being unable to breastfeed - but it’s not your fault, just as the psychosis is not your fault. It’s just important that you have the treatment you need so that you can get better and get on with looking after and enjoying your baby.
You may need a medication which is not safe in breastfeeding. You might feel guilty about being unable to breastfeed - but it’s not your fault, just as the psychosis is not your fault. It’s just important that you have the treatment you need so that you can get better and get on with looking after and enjoying your baby.
You might feel guilty about being unable to breastfeed - but it’s not your fault, just as the psychosis is not your fault. It’s just important that you have the treatment you need so that you can get better and get on with looking after and enjoying your baby.
Help in caring for my baby
During the worst part of your postpartum psychosis you will need practical help to care for your baby – and also help to bond with your baby. Mother and Baby Unit (MBU) staff are trained to support you with every aspect of caring for your baby. If you do not go to an MBU, health visitors and mental health professionals can help and support you at home. There may be a local perinatal or parent-infant mental health service. In some areas, Children’s Centre staff and/or voluntary organisations can also help.
In some areas, Children’s Centre staff and/or voluntary organisations can also help.
It is normal to lack confidence with your mothering after postpartum psychosis. Remember - most new mothers, who have not had an illness, also feel like this. But, it can be hard to go to mother and baby groups while getting over a postpartum psychosis. Health visitors and community psychiatric nurses can give you one-to-one advice until you feel up to attending groups with other mothers.
Some mothers have difficulty bonding with their babies after an episode of postpartum psychosis. This can be very distressing, but usually doesn’t last long. Most women who have had postpartum psychosis go on to bond well with their babies and have good relationships with them.
Ask your health visitor, or other professional involved in your care, what help is available in your area. Health professionals can support you in learning how to interact with and respond to your baby. You may find baby massage and other groups for new parents helpful.
Care and support for you during recovery
Allow your partner, family or friends to help and support you while you get better (see section on partners below).
You will usually need to have care from a community perinatal mental health service until you fully recover. This team can advise you about treatment and support for you and your family. You may also have a general adult mental health team.
Your health visitor and GP will also continue to support you whilst you recover.
Do ask for advice about contraception. It is a good idea to avoid getting pregnant again too soon after an episode of postpartum psychosis.
Postpartum depression
Page 2 of 7
At least one in 10 mothers suffers from postpartum depression. It is one of the most frequent postpartum complications and occurs in 10-13% of women in labor. As a rule, in such cases it is not always possible to make a correct diagnosis, because mothers are reluctant to seek medical help. Psychotic states in the postpartum period occur in no more than 0.1-0.3% of cases. That is, out of every thousand women who give birth, from 1 to 3 suffer from an even more severe form of depression - postpartum psychosis, in which a woman develops delusions or hallucinations, often accompanied by an obsession with harming herself or the child. The psychotic state significantly impairs the woman's ability to function naturally in family and social life, and also poses a significant risk of committing a suicide attempt. In most cases, the postpartum psychotic state requires urgent hospitalization of the patient. Early postpartum depression develops in the first days or weeks after childbirth, and usually lasts from a week to a month. Late postpartum depression usually develops several months after pregnancy. Its duration can be different, but more often it lasts more than a month.
Psychotic states in the postpartum period occur in no more than 0.1-0.3% of cases. That is, out of every thousand women who give birth, from 1 to 3 suffer from an even more severe form of depression - postpartum psychosis, in which a woman develops delusions or hallucinations, often accompanied by an obsession with harming herself or the child. The psychotic state significantly impairs the woman's ability to function naturally in family and social life, and also poses a significant risk of committing a suicide attempt. In most cases, the postpartum psychotic state requires urgent hospitalization of the patient. Early postpartum depression develops in the first days or weeks after childbirth, and usually lasts from a week to a month. Late postpartum depression usually develops several months after pregnancy. Its duration can be different, but more often it lasts more than a month.
Most often, depression appears 30-35 days after birth and in some cases can last up to 1.5-2 years.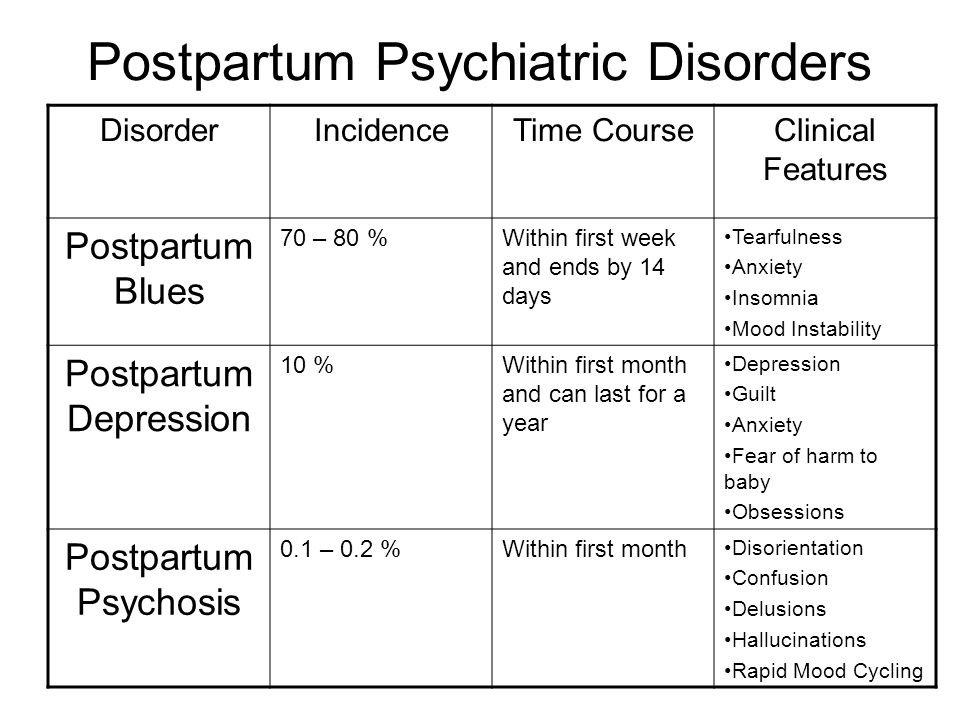 However, in most cases, a depressive episode ends spontaneously safely 3-6 months after birth. Symptoms of postpartum depression meet the diagnostic criteria for depressive disorder. The patient has a deterioration in mood, a decrease in energy, activity, the ability to rejoice, have fun, a decrease in interests and difficulty in long-term concentration of attention. Severe fatigue is common, even after minimal effort. As a rule, sleep is disturbed and appetite worsens. Self-esteem and self-confidence are almost always reduced, even in mild forms of the disease. Often there are thoughts of one's own guilt and worthlessness. Low mood, which varies little from day to day, does not depend on circumstances and may be accompanied by symptoms such as loss of interest in the environment and the loss of sensations that give pleasure. Typical is awakening in the morning several hours earlier than usual, increased depression in the morning, severe psychomotor retardation, anxiety, loss of appetite, weight loss and decreased libido.
However, in most cases, a depressive episode ends spontaneously safely 3-6 months after birth. Symptoms of postpartum depression meet the diagnostic criteria for depressive disorder. The patient has a deterioration in mood, a decrease in energy, activity, the ability to rejoice, have fun, a decrease in interests and difficulty in long-term concentration of attention. Severe fatigue is common, even after minimal effort. As a rule, sleep is disturbed and appetite worsens. Self-esteem and self-confidence are almost always reduced, even in mild forms of the disease. Often there are thoughts of one's own guilt and worthlessness. Low mood, which varies little from day to day, does not depend on circumstances and may be accompanied by symptoms such as loss of interest in the environment and the loss of sensations that give pleasure. Typical is awakening in the morning several hours earlier than usual, increased depression in the morning, severe psychomotor retardation, anxiety, loss of appetite, weight loss and decreased libido.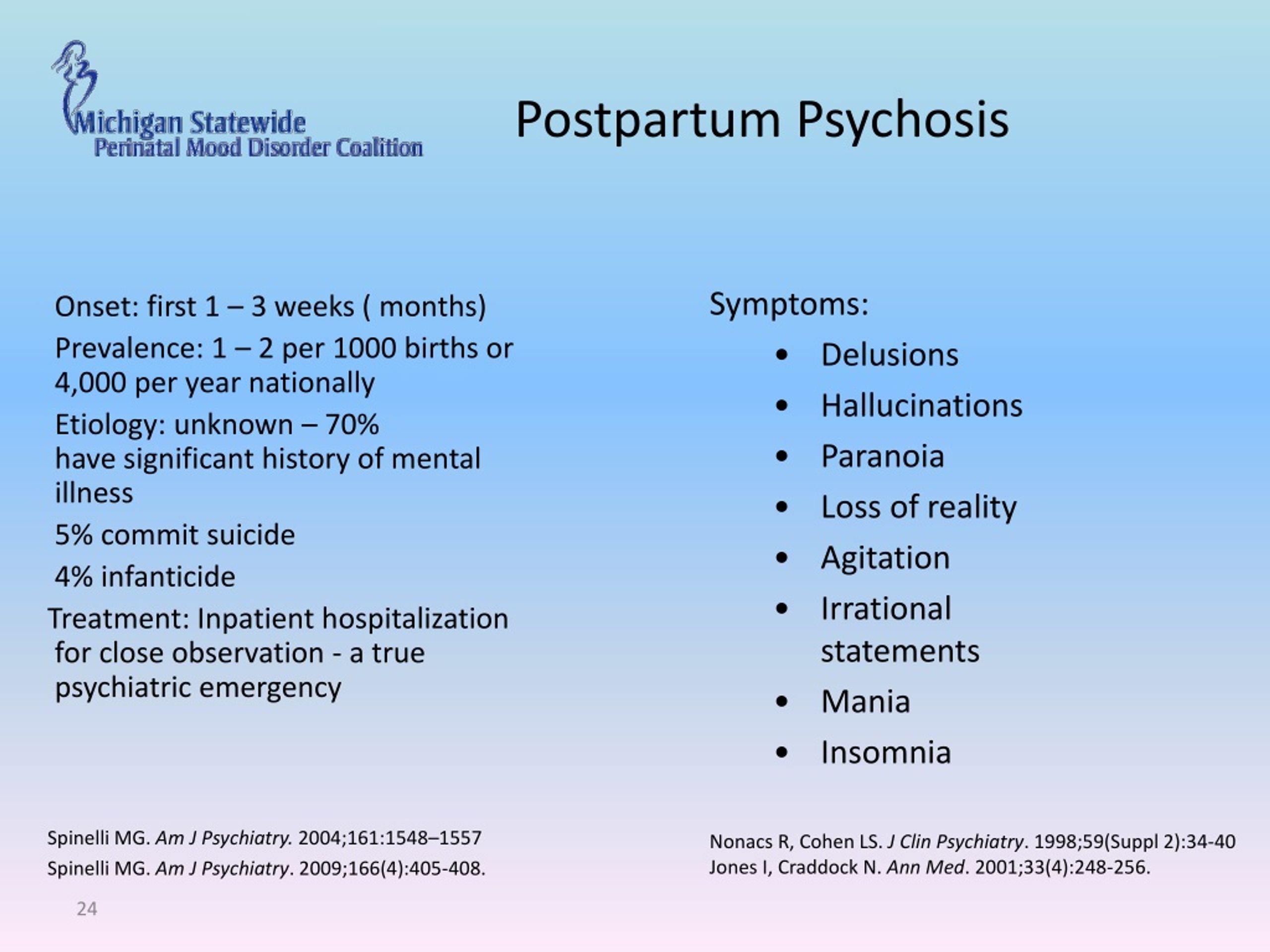
In most cases, postpartum depression remains unrecognized in the initial period. The most typical example is the prevailing idea of the "natural whims" or character flaws of a woman in labor who turns to her relatives for help instead of actively caring for the child. Loss of initiative and energy or fear of being judged and discussed by others often prevents a woman from seeking medical help. However, even when contacting a doctor, the disease often remains unrecognized, since some doctors tend to consider this condition as a temporary and natural reaction to the stress that childbirth is, especially for primiparas. At the same time, depression can increase over several months, and the treatment of this condition is delayed until there is an indication for emergency hospitalization.
<< First < Previous 1 2 3 4 5 6 7 Next > Last >>
What is postpartum psychosis and how does it manifest? This is a rather rare condition, it occurs in one or two women out of a thousand.
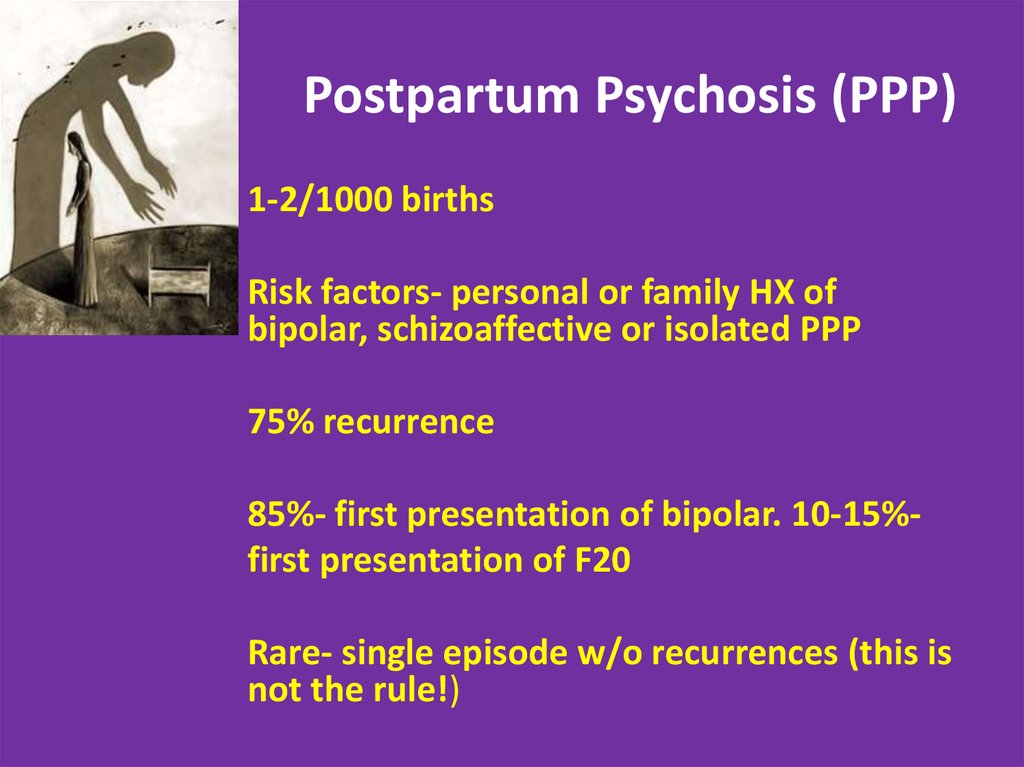 Risk groups include: women with bipolar disorder, schizoaffective disorder, or schizophrenia (risk of developing postpartum psychosis 1:4), women whose mothers or sisters had postpartum psychosis (1:3), women who have already had an episode of postpartum psychosis ( 1:2). These are statistics, and this does not mean that if you are at risk, then you will definitely have psychosis after childbirth. But women who are at risk are advised to be more attentive to themselves and their experiences and get expert advice.
Risk groups include: women with bipolar disorder, schizoaffective disorder, or schizophrenia (risk of developing postpartum psychosis 1:4), women whose mothers or sisters had postpartum psychosis (1:3), women who have already had an episode of postpartum psychosis ( 1:2). These are statistics, and this does not mean that if you are at risk, then you will definitely have psychosis after childbirth. But women who are at risk are advised to be more attentive to themselves and their experiences and get expert advice. | The causes of postpartum psychosis are not yet well understood. Judging by the research, most likely the main cause is a combination of several factors: genetic predisposition, hormonal changes associated with pregnancy, childbirth and adaptation to a new life, lack of sleep, stress, traumatic experience. |
Symptoms
The main symptoms of postpartum psychosis are psychotic: strange beliefs that cannot be true (delusions), sounds, sights, smells and sensations that other people do not feel (hallucinations), loss of connection with reality, a confused state of consciousness.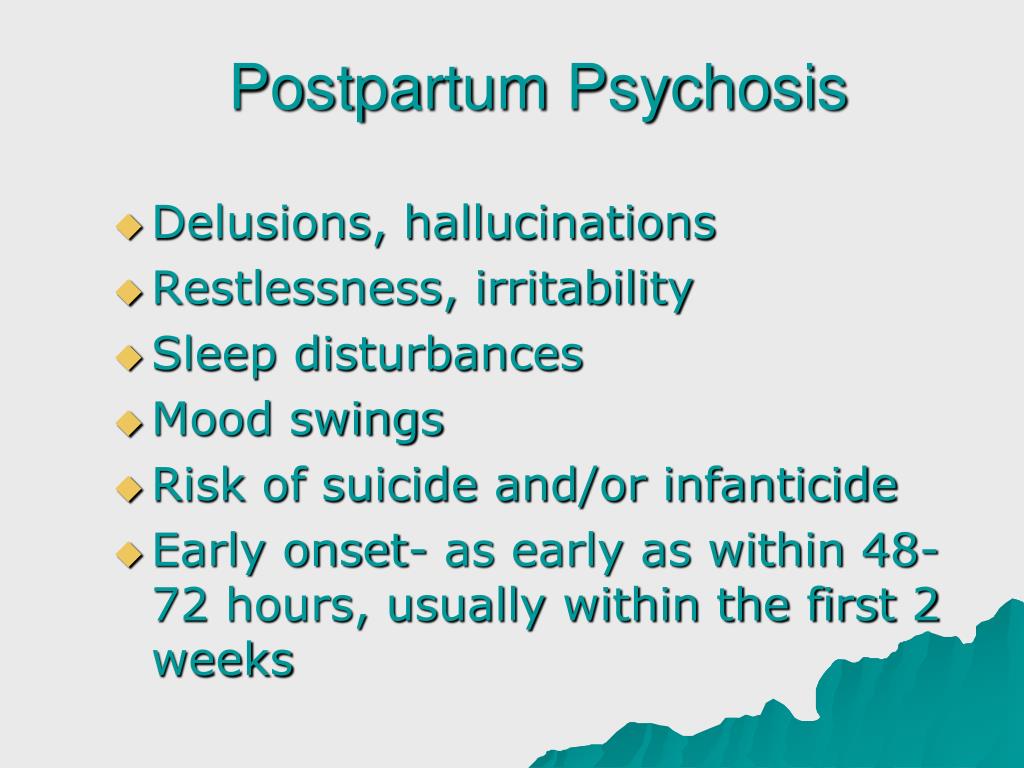
At the same time, a woman in postpartum psychosis may be agitated, very irritable, or depressed and anxious, sometimes her mood may be very changeable. In addition, a woman or her relatives may notice:
- Sleep problems, insomnia, or vice versa - drowsiness
- A woman may become more talkative, sociable in comparison with her usual state, spend more time talking on the phone
- Constantly in her head many different thoughts, you can feel the jump of ideas
- Feeling like a "supermom", high energy or restlessness and agitation
- Uncharacteristic behavior for a woman, feeling that she is not in control of herself to her
- Feeling that the child is somehow connected with supernatural forces
Therapy
Postpartum psychosis develops rapidly, and the loss of connection with reality, which occurs due to its symptoms, is dangerous for mother and child. That is why hospitalization is indicated in this state, where, under the supervision of doctors, the condition is stabilized.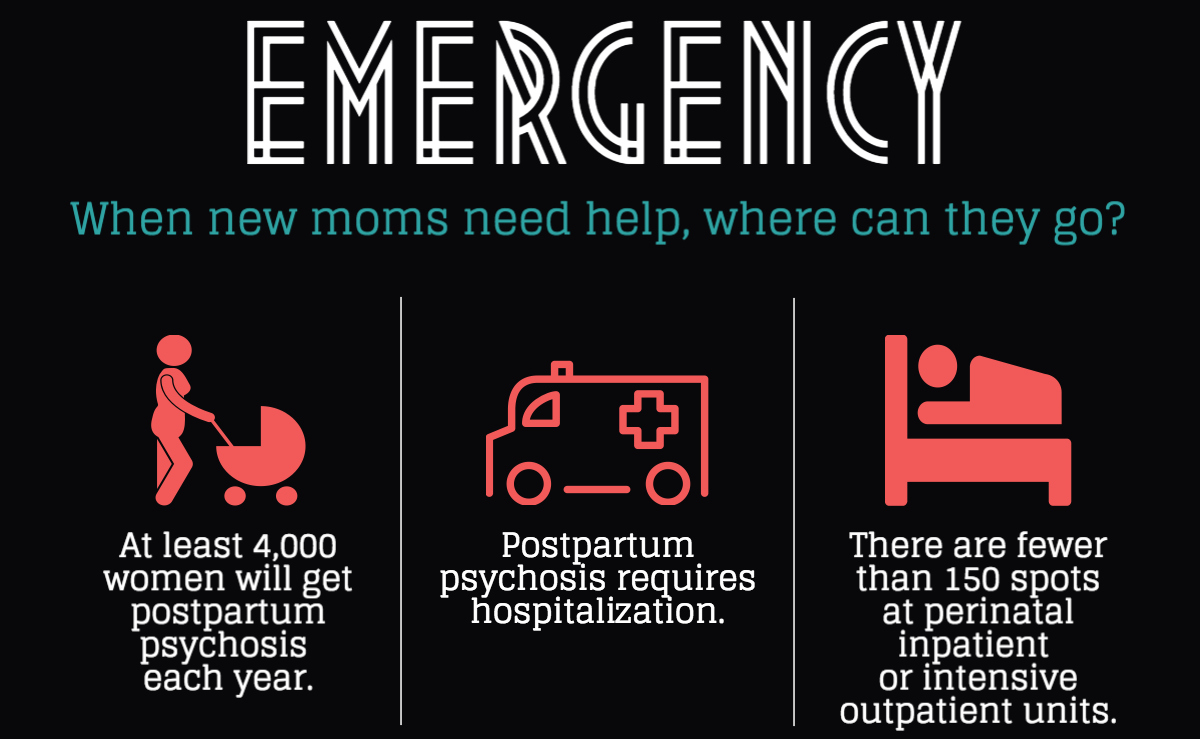 Postpartum psychosis is treated with antipsychotic medications. In severe cases, and if other treatments have not worked, your doctor may suggest electroconvulsive therapy (ECT).
Postpartum psychosis is treated with antipsychotic medications. In severe cases, and if other treatments have not worked, your doctor may suggest electroconvulsive therapy (ECT).
Prevention
For women at high risk of postpartum psychosis, your doctor may suggest the following options: start antipsychotics in the last trimester of pregnancy, immediately after delivery, or when the first signs of psychosis appear. If there is a high risk, it makes sense to find a doctor in advance with whom you can be in touch throughout the postpartum period, a clinic in case there is a need for hospitalization, think in advance who can help at first and who will care for the child in an emergency .
Recovery
The good news is that postpartum psychosis is well treated, and within a year the woman returns to a completely normal life. What happened is often hard for a woman, she can face shock, anger, anxiety, guilt, self-doubt, feeling like an incompetent mother.