How does a child get hpv
Pediatric Human Papillomavirus (HPV)
Our commitment to keeping you safe
We have never taken for granted the sacred trust you place in us to care for your child, and today we are more grateful than ever for that privilege. To learn about all the ways we are working to keep you, your family and our team members safe, visit our COVID-19 updates page.
Learn More about our commitment to keeping you safe
Learn More about our commitment to keeping you safe
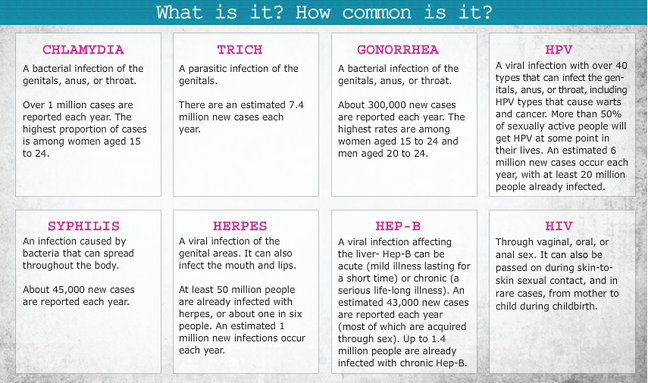
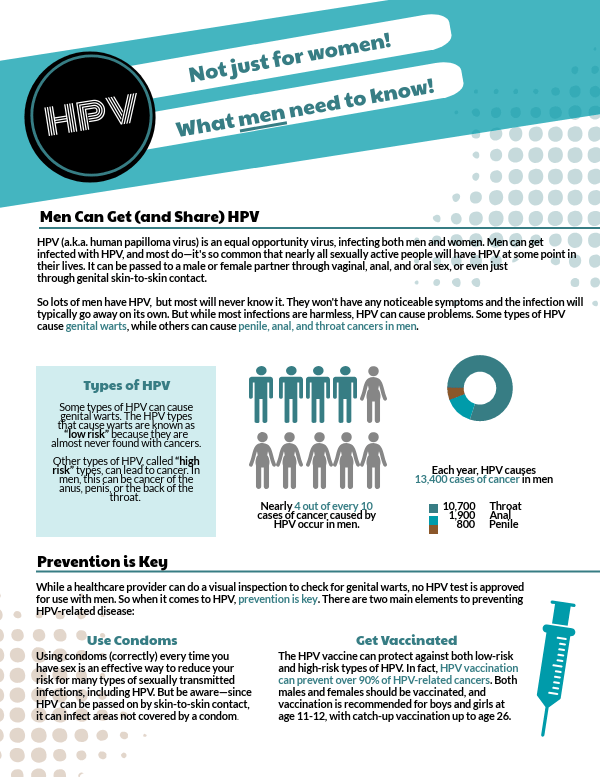
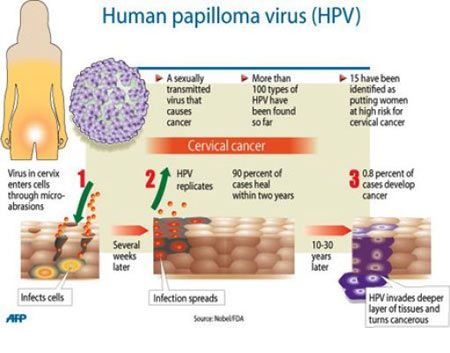
Pediatric human papillomavirus (HPV) is the most common sexually transmitted infection, according to the Centers for Disease Control (CDC) It can cause genital warts and certain types of cancer.
What is Pediatric Human Papillomavirus (HPV)?
Human papillomavirus is a widespread, sexually transmitted infection (STI). It has become well-known due to its link to cervical cancer. While not every child with HPV will develop cervical cancer, HPV increases the risk. The main feature of HPV is genital warts, but not all children will develop them. Even though HPV is called an STI, it can be transmitted through non-sexual routes like hand to hand contact, or from mother to child during a vaginal delivery, for example.
What are the signs and symptoms of Pediatric Human Papillomavirus (HPV)?
Warts are the most frequently occurring symptom of HPV; however, most HPV infections will not cause symptoms.
How is Pediatric Human Papillomavirus (HPV) diagnosed?
In children and adolescents, if there is a concern for a wart, an examination in the office will the first step in the evaluation of this condition.
What are the causes of Pediatric Human Papillomavirus (HPV)?
The HPV infection is primarily spread through skin-to-skin contact. There are several risk factors that increase the chance of a child getting a HPV infection:
- Having a cut – The disease can enter the blood stream through an opening in the skin (like a cut).

- Having a mother with HPV – It is possible for a mother to infect her child during vaginal childbirth.
- Being sexually active – Those that are sexually active have a greater risk of contracting HPV. Further, the more sexual partners you have, the more likely you are to get HPV. Being with a partner that has had multiple partners also increases your risk.
- Weakened immune system – Immune systems can be weakened by HIV/AIDS, immune-suppressing medications (organ transplants) or other reasons.
How is Pediatric Human Papillomavirus (HPV) treated?
This condition can be treated with observation, with various creams or ointments to be placed on the wart, or with surgery. Your provider will help determine what is best for your child.
Pediatric Human Papillomavirus (HPV) Doctors and Providers
-
M. Brett Cooper, MD Adolescent Medicine Specialist
-
Nirupama De Silva, MD Pediatric Gynecologist
-
Jenny Francis, MD Adolescent Medicine Specialist
-
Jason Jarin, MD Pediatric Gynecologist
HPV infection - Symptoms and causes
Overview
HPV infection is a viral infection that commonly causes skin or mucous membrane growths (warts).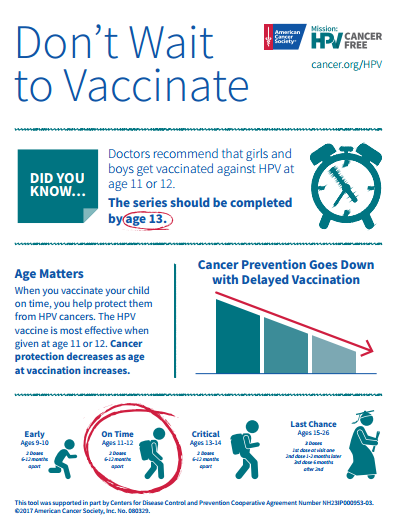 There are more than 100 varieties of human papillomavirus (HPV). Some types of HPV infection cause warts, and some can cause different types of cancer.
There are more than 100 varieties of human papillomavirus (HPV). Some types of HPV infection cause warts, and some can cause different types of cancer.
Most HPV infections don't lead to cancer. But some types of genital HPV can cause cancer of the lower part of the uterus that connects to the vagina (cervix). Other types of cancers, including cancers of the anus, penis, vagina, vulva and back of the throat (oropharyngeal), have been linked to HPV infection.
These infections are often transmitted sexually or through other skin-to-skin contact. Vaccines can help protect against the strains of HPV most likely to cause genital warts or cervical cancer.
Products & Services
- Book: Mayo Clinic Family Health Book, 5th Edition
- Book: Your Sexual Health
Symptoms
Common warts
Common warts
Common warts can grow on your hands or fingers. They're small, grainy bumps that are rough to the touch.
They're small, grainy bumps that are rough to the touch.
Plantar warts
Plantar warts
Plantar warts are caused by the same type of virus that causes warts on your hands and fingers. But, because of their location, they can be painful.
Flat warts
Flat warts
Flat warts are smaller and smoother than other warts. They generally occur on the face or legs and are more common in children and teens than in adults.
Female genital warts
Female genital warts
Genital warts are a common sexually transmitted infection. They can appear on the genitals, in the pubic area or in the anal canal. In women, genital warts can also grow inside the vagina.
Male genital warts
Male genital warts
Genital warts are a common sexually transmitted infection. They can appear on the genitals, in the pubic area or in the anal canal.
In most cases, your body's immune system defeats an HPV infection before it creates warts. When warts do appear, they vary in appearance depending on which kind of HPV is involved:
-
Genital warts. These appear as flat lesions, small cauliflower-like bumps or tiny stemlike protrusions. In women, genital warts appear mostly on the vulva but can also occur near the anus, on the cervix or in the vagina.
In men, genital warts appear on the penis and scrotum or around the anus. Genital warts rarely cause discomfort or pain, though they may itch or feel tender.
- Common warts. Common warts appear as rough, raised bumps and usually occur on the hands and fingers. In most cases, common warts are simply unsightly, but they can also be painful or susceptible to injury or bleeding.
- Plantar warts. Plantar warts are hard, grainy growths that usually appear on the heels or balls of your feet.
 These warts might cause discomfort.
These warts might cause discomfort. - Flat warts. Flat warts are flat-topped, slightly raised lesions. They can appear anywhere, but children usually get them on the face and men tend to get them in the beard area. Women tend to get them on the legs.
Cervical cancer
Nearly all cervical cancers are caused by HPV infections, but cervical cancer may take 20 years or longer to develop after an HPV infection. The HPV infection and early cervical cancer typically don't cause noticeable symptoms. Getting vaccinated against HPV infection is your best protection from cervical cancer.
Because early cervical cancer doesn't cause symptoms, it's vital that women have regular screening tests to detect any precancerous changes in the cervix that might lead to cancer. Current guidelines recommend that women ages 21 to 29 have a Pap test every three years.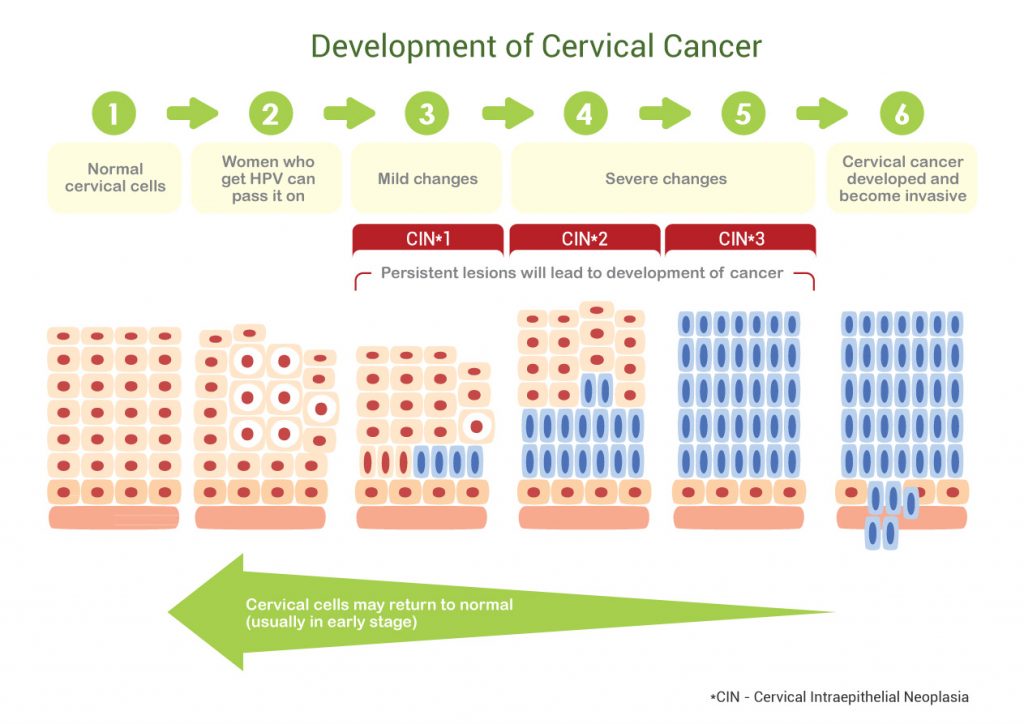
Women ages 30 to 65 are advised to continue having a Pap test every three years, or every five years if they also get the HPV DNA test at the same time. Women over 65 can stop testing if they've had three normal Pap tests in a row, or two HPV DNA and Pap tests with no abnormal results.
When to see a doctor
If you or your child has warts of any kind that cause embarrassment, discomfort or pain, seek advice from your doctor.
Request an Appointment at Mayo Clinic
From Mayo Clinic to your inbox
Sign up for free, and stay up to date on research advancements, health tips and current health topics, like COVID-19, plus expertise on managing health.
To provide you with the most relevant and helpful information, and understand which
information is beneficial, we may combine your email and website usage information with
other information we have about you.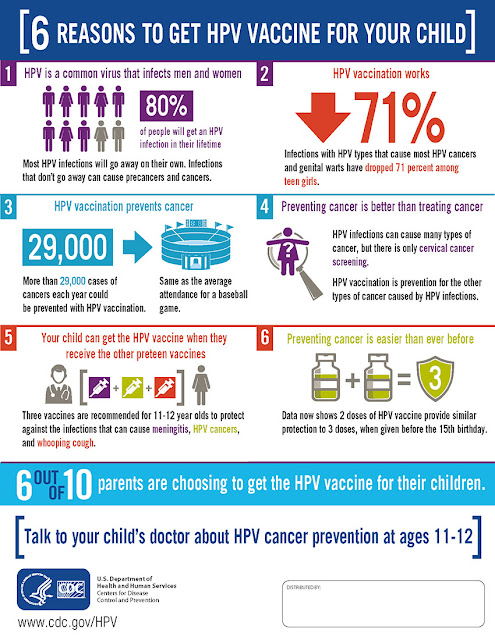 If you are a Mayo Clinic patient, this could
include protected health information. If we combine this information with your protected
health information, we will treat all of that information as protected health
information and will only use or disclose that information as set forth in our notice of
privacy practices. You may opt-out of email communications at any time by clicking on
the unsubscribe link in the e-mail.
If you are a Mayo Clinic patient, this could
include protected health information. If we combine this information with your protected
health information, we will treat all of that information as protected health
information and will only use or disclose that information as set forth in our notice of
privacy practices. You may opt-out of email communications at any time by clicking on
the unsubscribe link in the e-mail.
Causes
HPV infection occurs when the virus enters your body, usually through a cut, abrasion or small tear in your skin. The virus is transferred primarily by skin-to-skin contact.
Genital HPV infections are contracted through sexual intercourse, anal sex and other skin-to-skin contact in the genital region.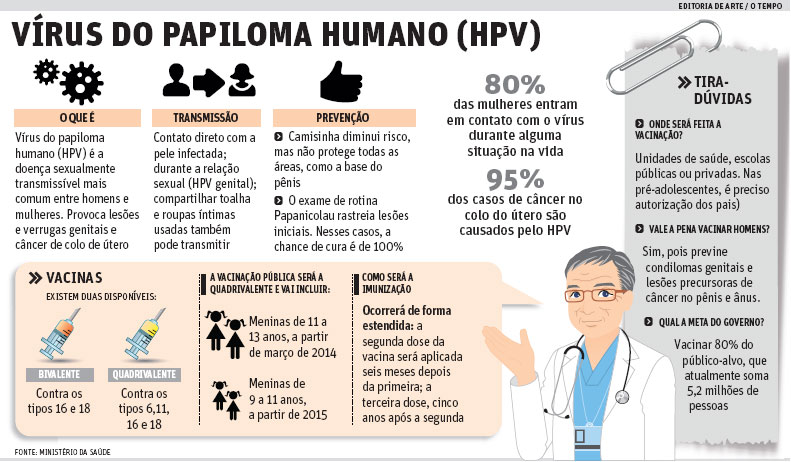 Some HPV infections that result in oral or upper respiratory lesions are contracted through oral sex.
Some HPV infections that result in oral or upper respiratory lesions are contracted through oral sex.
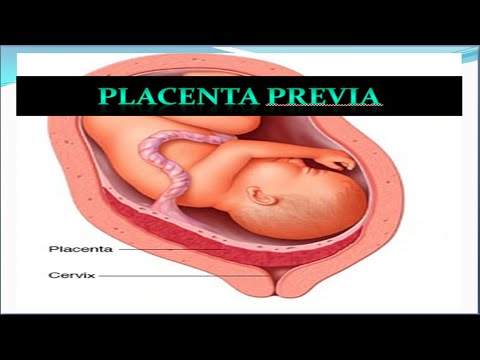
If you're pregnant and have an HPV infection with genital warts, it's possible your baby may get the infection. Rarely, the infection may cause a noncancerous growth in the baby's voice box (larynx).
Warts are contagious. They can spread through direct contact with a wart. Warts can also spread when someone touches something that already touched a wart.
Risk factors
HPV infections are common. Risk factors for HPV infection include:
- Number of sexual partners. The more sexual partners you have, the more likely you are to contract a genital HPV infection. Having sex with a partner who has had multiple sex partners also increases your risk.

- Age. Common warts occur mostly in children. Genital warts occur most often in adolescents and young adults.
- Weakened immune systems. People who have weakened immune systems are at greater risk of HPV infections. Immune systems can be weakened by HIV/AIDS or by immune system-suppressing drugs used after organ transplants.
- Damaged skin. Areas of skin that have been punctured or opened are more prone to develop common warts.
- Personal contact. Touching someone's warts or not wearing protection before contacting surfaces that have been exposed to HPV — such as public showers or swimming pools — might increase your risk of HPV infection.
Complications
- Oral and upper respiratory lesions. Some HPV infections cause lesions on your tongue, tonsils, soft palate, or within your larynx and nose.

- Cancer. Certain strains of HPV can cause cervical cancer. These strains might also contribute to cancers of the genitals, anus, mouth and upper respiratory tract.
Prevention
Common warts
It's difficult to prevent HPV infections that cause common warts. If you have a common wart, you can prevent the spread of the infection and formation of new warts by not picking at a wart and not biting your nails.
Plantar warts
To reduce the risk of contracting HPV infections that cause plantar warts, wear shoes or sandals in public pools and locker rooms.
Genital warts
You can reduce your risk of developing genital warts and other HPV-related genital lesions by:
- Being in a mutually monogamous sexual relationship
- Reducing your number of sex partners
- Using a latex condom, which can reduce your risk of HPV transmission
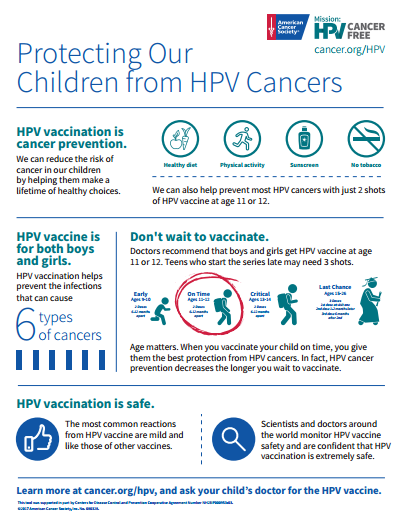
HPV vaccines
Gardasil 9 is an HPV vaccine approved by the U.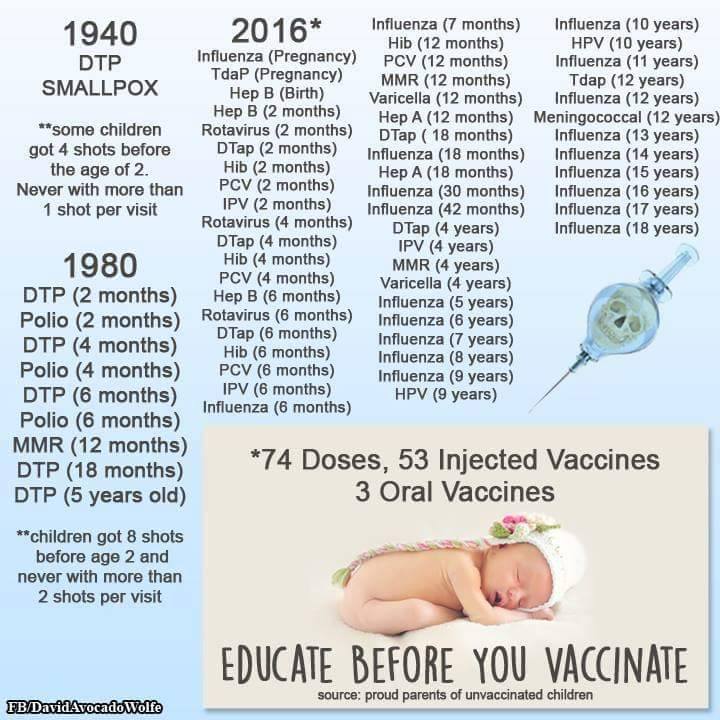 S. Food and Drug Administration and can be used for males and females to protect against cervical cancer and genital warts.
S. Food and Drug Administration and can be used for males and females to protect against cervical cancer and genital warts.
The Centers for Disease Control and Prevention (CDC) recommends routine HPV vaccination for girls and boys ages 11 and 12, although it can be given as early as age 9. It's ideal for girls and boys to receive the vaccine before they have sexual contact and are exposed to HPV. Research has shown that receiving the vaccine at a young age isn't linked to an earlier start of sexual activity.
Once someone is infected with HPV, the vaccine might not be as effective or might not work at all. Also, response to the vaccine is better at younger ages than older ones. But, if given before someone is infected, the vaccine can prevent most cases of cervical cancer.
The CDC recommends that all 11- and 12-year-olds receive two doses of HPV vaccine at least six months apart.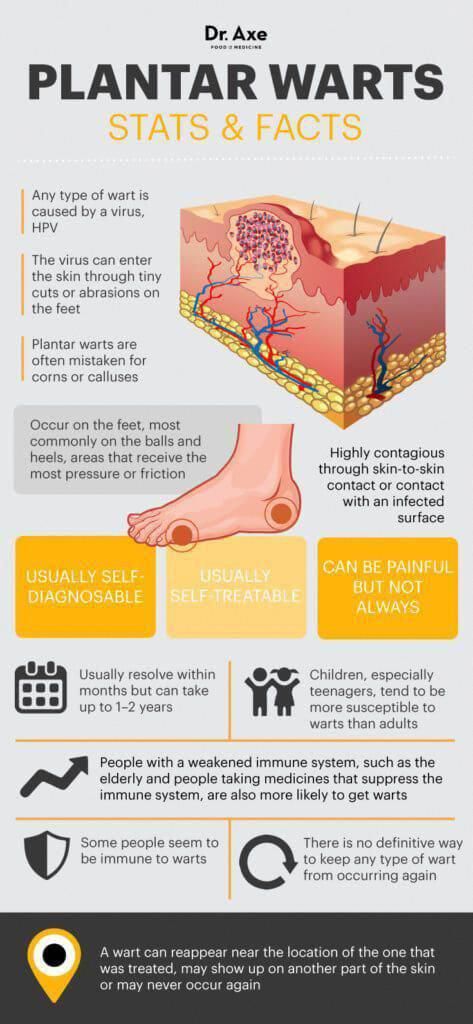 Younger adolescents ages 9 and 10 and teens ages 13 and 14 can also receive vaccination on the updated two-dose schedule. Research has shown that the two-dose schedule is effective for children under 15.
Younger adolescents ages 9 and 10 and teens ages 13 and 14 can also receive vaccination on the updated two-dose schedule. Research has shown that the two-dose schedule is effective for children under 15.
Teens and young adults who begin the vaccine series later, at ages 15 through 26, should continue to receive three doses of the vaccine.
The CDC recommends catch-up HPV vaccinations for all people through age 26 who aren't adequately vaccinated.
The U.S. Food and Drug Administration recently approved the use of Gardasil 9 for males and females ages 9 to 45. If you're age 27 to 45, discuss with your doctor whether he or she recommends that you get the HPV vaccine.
More Information
- HPV vaccine
By Mayo Clinic Staff
Related
Associated Procedures
News from Mayo Clinic
Products & Services
Papillomas in children causes and treatment in 2019
Remember in childhood there was such a "scarecrow" - do not touch the frog, otherwise warts will jump from it? So: science has stepped forward a long time ago, today it is known for sure that frogs are not the cause of “warts” in children.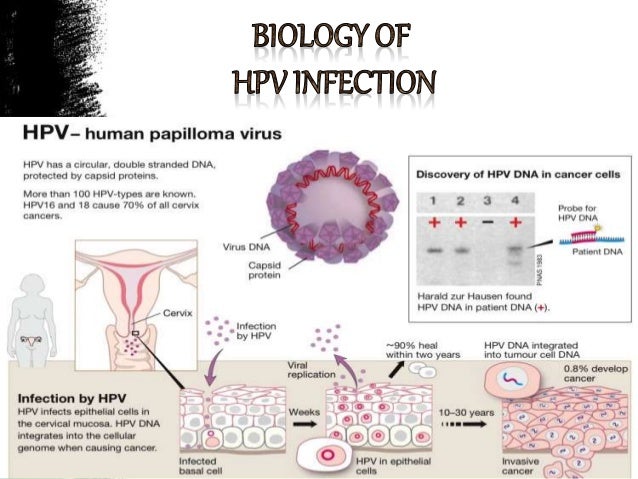
What is papillomavirus, how can a child get it?
Papillomas, warts and condylomas are neoplasms of the skin and mucous membranes that occur when infected with the human papillomavirus (HPV). The virus can infect the outer layer of the skin and the smooth, moist mucous membranes of the mouth, rectum, anus, and genitals in men and women. There are over 100 different types of virus. Many of these types of virus cause warts and papillomas that appear on the hands and feet. HPV types 6 and 11 cause genital warts, while HPV types 16 and 18 can lead to cervical cancer and, less commonly, cancer of the vagina, penis, scrotum, or rectum.
In neonates and young children, papillomatosis (or HPV) presents as skin warts, genital warts, and juvenile recurrent respiratory papillomatosis. Adolescent girls may have squamous intraepithelial lesions of the cervix.
In children aged 5 to 15 years, HPV types 1, 2 and 3 predominate in skin warts, while in adolescents, HPV type 4 predominates.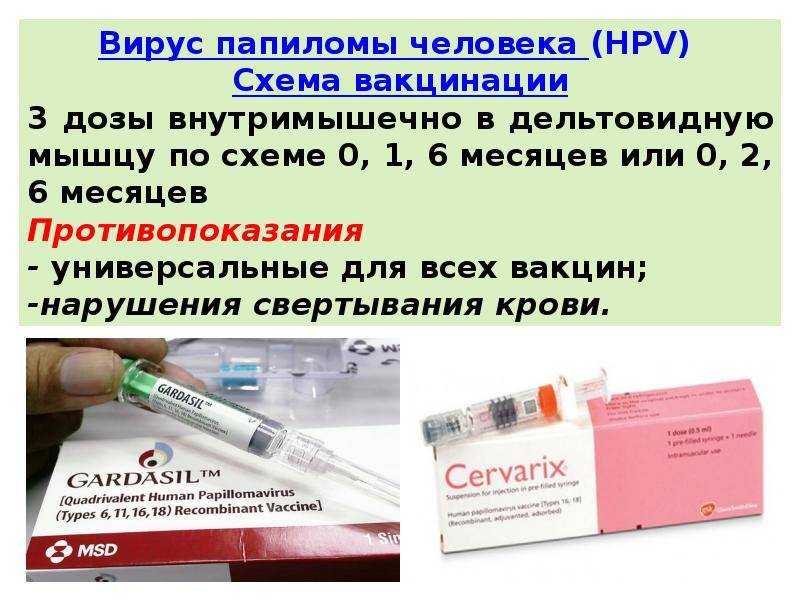 Recurrent respiratory papillomatosis is caused by HPV types 13, 39, 40 and 56.
Recurrent respiratory papillomatosis is caused by HPV types 13, 39, 40 and 56.
How is the virus transmitted to children?
HPV is spread by skin-to-skin contact or through blood:
- A pregnant mother can pass the infection to her baby through the bloodstream before delivery or through the vaginal canal during childbirth. This is called perinatal transmission.
- Children with warts on their hands can transmit the virus through skin contact. The spread of the virus to the genital area occurs when you touch them with your hands. This route of infection is called autoinoculation.
- A caregiver with warts can transmit the virus through skin-to-skin contact with a child's hands or genitals. This is called heteroinoculation.
- HPV can be transmitted from human skin to the genital area of a child through sexual contact - in case of violence.
- Rarely, HPV can be transmitted through contact with inanimate objects or surfaces.
 If an adult with warts uses a towel and then a child uses the same towel, the virus can be passed on to the child. This is called fomite transmission.
If an adult with warts uses a towel and then a child uses the same towel, the virus can be passed on to the child. This is called fomite transmission.
HPV is transmitted through skin contact, even if there are no warts or papillomas on the skin. Once infected, the virus remains in the body. The person may be a carrier
Papilloma virus vaccine
2-3 vaccinations are required to create immunity. The effectiveness of the vaccine varies from 97.9% to 100%.
More details can be found on the page: Vaccinations against papillomavirus
Prevention of HPV infection
Like many other viruses, HPV reactivates and causes illness in immunocompromised individuals. That is why it is children who are susceptible to the development of papillomatosis. In some people, HPV can go away without treatment if the body mounts an immune response to the virus.
It is especially important to vaccinate girls because For them, HPV infection is fraught with the development of oncology.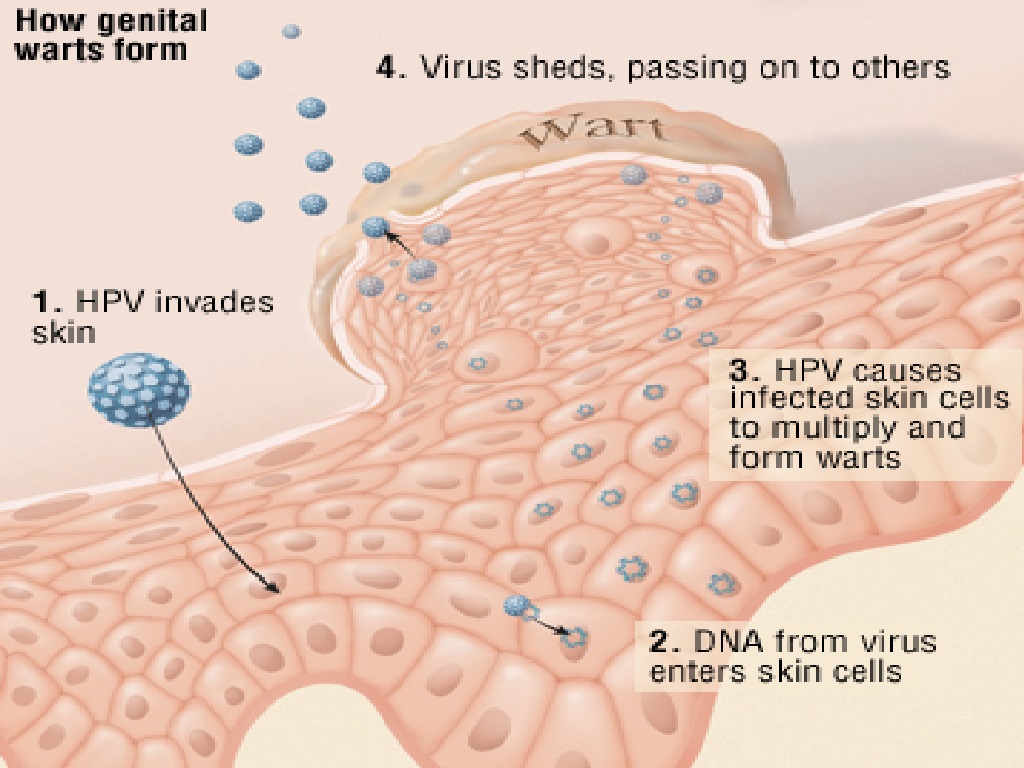 The best and most modern way to protect against papillomavirus is vaccination. Girls should get the vaccine (Gardasil, Cervarix) before they become sexually active
The best and most modern way to protect against papillomavirus is vaccination. Girls should get the vaccine (Gardasil, Cervarix) before they become sexually active
The most common vaccine is called Gardasil, which is currently used to immunize school-age girls nine years of age and older. The vaccine provides immunity to two strains of HPV that cause cervical cancer and two strains associated with genital warts. Vaccination is carried out by three injections of the vaccine within six months. It is recommended to get vaccinated before sexual activity. The vaccine is effective against HPV types 6, 11, 16 and 18. Vaccination is also possible after the onset of sexual activity before the age of 26 years. Boys are vaccinated against colorectal cancer caused by HPV.
Rarely, the virus causes recurrent respiratory papillomatosis, in which there is growth of viral warts in the larynx, causing a benign tumor of the larynx in children. These neoplasms are treatable, but, unfortunately, completely incurable. In large numbers, neoplasms caused by HPV can cause airway obstruction.
In large numbers, neoplasms caused by HPV can cause airway obstruction.
HPV diagnostics
The pediatrician will definitely pay special attention to the diagnosis of HPV and genital warts in a child. If you see that your child has a wart, visit a doctor immediately and start treatment. There is no need to hope that "it will go away by itself" and "it's okay." Just the opposite: it’s scary, it threatens with oncology or big problems in the future. It is especially necessary to monitor the presence of papillomas and warts if you have a daughter.
Any child with genital warts needs a complete medical examination, which includes the following:
- Examination of the child's anus and genital area.
- Questioning parents about the presence of HPV infection, genital or common warts.
- Questioning the mother for an abnormal Pap smear that may indicate HPV infection.
- Interviewing parents for any indication of possible child sexual contact and possible child abuse.
Girls of puberty may have a colposcopy and Pap smear to look for signs of problems that could lead to cervical cancer. Early detection of a problem allows treatment.
An immunological HPV type test is available to identify high-risk strains that can cause cancer.
Treatment
Without treatment, genital warts and papillomas may disappear on their own or may persist for years. The treatment carried out unfortunately does not guarantee that the warts do not recur.
Genital warts are usually treated with gels or creams applied to the warts:
- Imiquimod (Aldara), wart cream applied by the patient.
- Podofilox, gel or cream applied to warts by the patient
- Trichloroacetic acid (TCA) or dichloroacetic acid (BCA), which a doctor applies to warts.
Less common is cryotherapy with liquid nitrogen or surgery.
Recurrent respiratory papillomatosis is treated surgically conventional or laser surgery may be used to remove benign lesions. The procedure is not painful and takes about 30 minutes, but due to the recurrent nature of the tumor, it may be required to be performed regularly up to several times a year. Drugs used include cidofovir, interferon alfa, and other experimental chemotherapy regimens.
The procedure is not painful and takes about 30 minutes, but due to the recurrent nature of the tumor, it may be required to be performed regularly up to several times a year. Drugs used include cidofovir, interferon alfa, and other experimental chemotherapy regimens.
Remember:
Unfortunately, today the most effective is vaccination. HPV treatment is symptomatic only. Do not "save" on the health of your child. Vaccination against the human papillomavirus is not included in the national vaccination schedule; unfortunately, such vaccinations are not given free of charge in polyclinics. We recommend that you take no risks and ensure that your child is vaccinated against HPV in a timely manner.
You can make an appointment by phone: +7(812)331-88-94
HPV (human papillomavirus) - symptoms, treatment
HUMAN PAPILLOMA VIRUS
skin of the perineum and around the anus, as well as in the respiratory tract.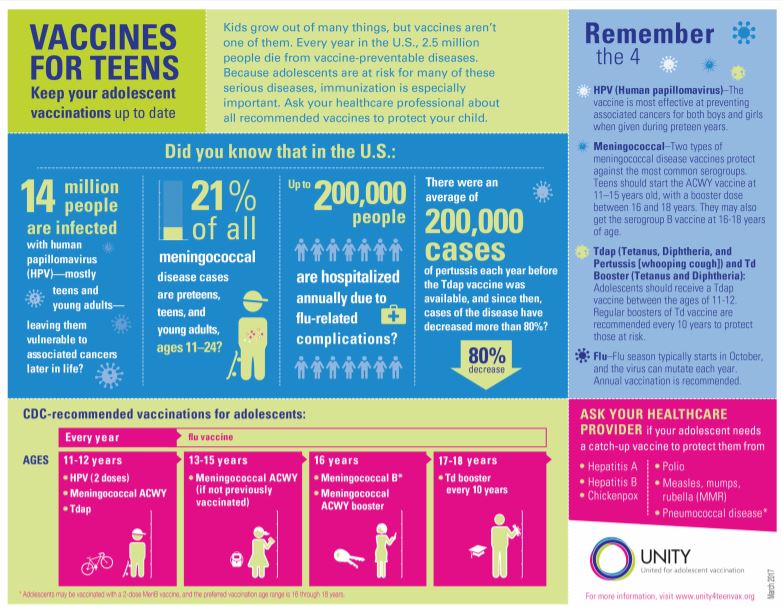
Papillomas are caused by human papillomaviruses ( HPV ) . To date, more than 120 types of HPV are known.
Papillomavirus infection is one of the most common viral diseases.
Certain types of HPV do not harm the human body, however, some can cause a variety of malignant tumors that arise from epithelial cells, primarily in the genital area: women.
Precancerous and pathological changes of the cervix (the so-called changes in the cells of the cervix, which carry the risk of development and transformation into a malignant tumor).
Malignant tumor of the female external genitalia (cancer of the vulva and vagina).
Condylomas (warts) in the genital area in the female and male population.
Currently, there is an increase in cancer incidence. Despite the availability of diagnostic studies, cervical cancer ranks second in the world among malignant tumors of the reproductive organs in women and is second only to breast cancer.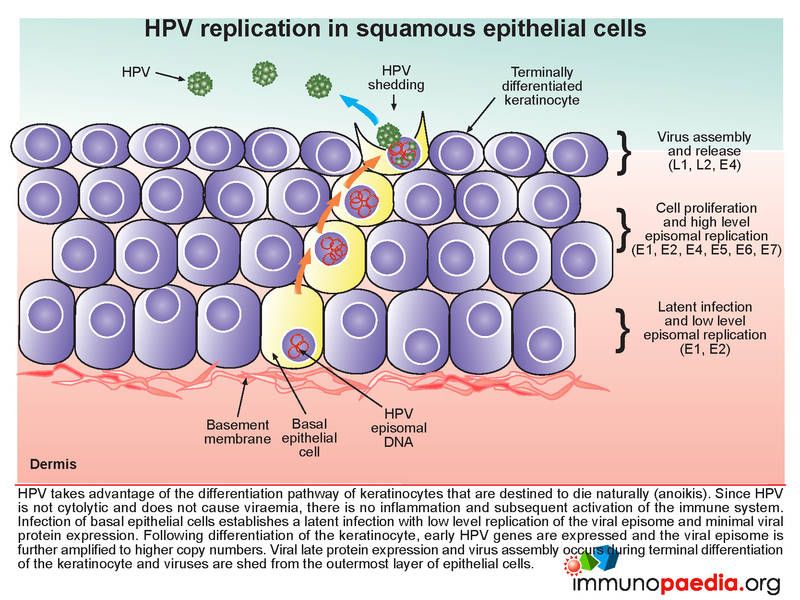
How is HPV transmitted and spread?
- If the rules of personal hygiene are not observed. When several people use the same things. For example, a towel and clothes (underwear).
- When visiting public places. These can be baths, saunas, swimming pools, sports clubs.
- Contact with a carrier of the virus. Certain strains of the virus can be transmitted even by shaking hands. What about close relationships? If there is an HPV carrier in the family, then the likelihood that the rest of the family is infected is very high.
- Vertical transmission path. The frequency of HPV transmission from mother to fetus varies greatly - from 4 to 87%. The most likely ascending HPV is an infection of the amniotic fluid and placenta.
- Self-infection.
 Transfer of the virus from one area of the body to another during hair removal or shaving.
Transfer of the virus from one area of the body to another during hair removal or shaving.
People between the ages of 16 and 20 are most at risk of HPV infection. In the chronic course of the disease, it contributes to the development of a precancerous condition, and later (in 20-30 years) it turns into cancer.
Risk Factors of HPV infection:
· Early on the beginning of sexual life,
· The presence of a large number and frequent change of sexual partners,
· High distribution of the transmitted permissions.
young,
smoking, alcohol,
pregnancy,
endometriosis,
endogenous factors (avitaminosis, changes in immune status). Symptoms of the disease.
One of the most striking manifestations of HPV is genital warts.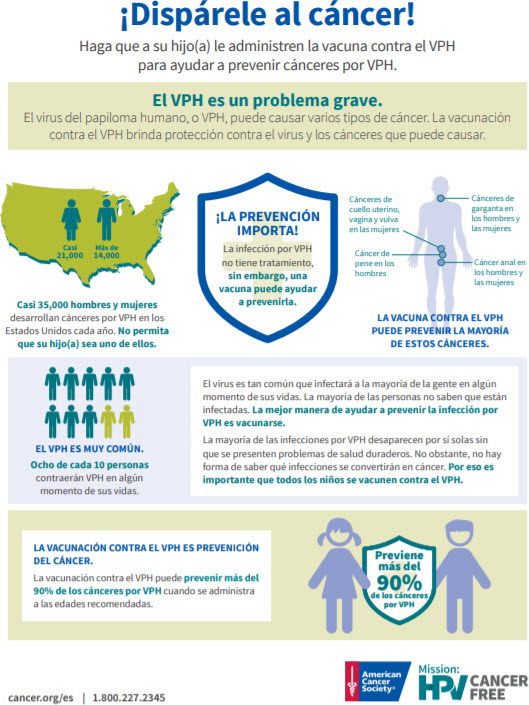 These mastoid formations are pink in color, more often they are lighter than the mucosa, but sometimes they have a brighter color.
These mastoid formations are pink in color, more often they are lighter than the mucosa, but sometimes they have a brighter color.
Human papillomavirus symptoms in men may differ from those seen in women. This is due to the difference in the structure of their reproductive organs.
HPV in women affects the cervical mucosa, sometimes polyps can also form in the uterine cavity.
In men, it more often affects the skin of the perianal region and the rectal mucosa. It is in these areas that the development of genital warts is observed, and they often lead to squamous cell carcinoma of the rectum.
There are 2 main directions:
Elimination of the virus from the human body. For this, various antiviral, immunomodulatory agents are used.
Correction of cosmetic defects. For this, various methods of removing papillomas are used: liquid nitrogen, coagulator, laser, etc.