Complications of retained placenta
I Wish I’d Known About the Risks of a Retained Placenta After Bir
Health and wellness touch each of us differently. This is one person’s story.
Around this time three years ago, I was preparing for the birth of my first child. I’d spent hours diligently researching birth and the wide range of birth-related questions. So, when I went into labor, I thought I’d done all I could to prepare for any event.
The birth had several obstacles.
I lost a lot of blood, received an episiotomy, and remained mildly conscious as my son was removed with forceps.
What I remember the most — other than my mother’s horrified face because my blood was slow to coagulate — was the pain. When my placenta came out in pieces, it seemed less important at the time. But it significantly shaped my introduction to motherhood.
Little did I know then, it would take over a month and a half to be diagnosed with retained placenta. I’d experience weeks of pain as a consequence of my placenta not being expelled at once.
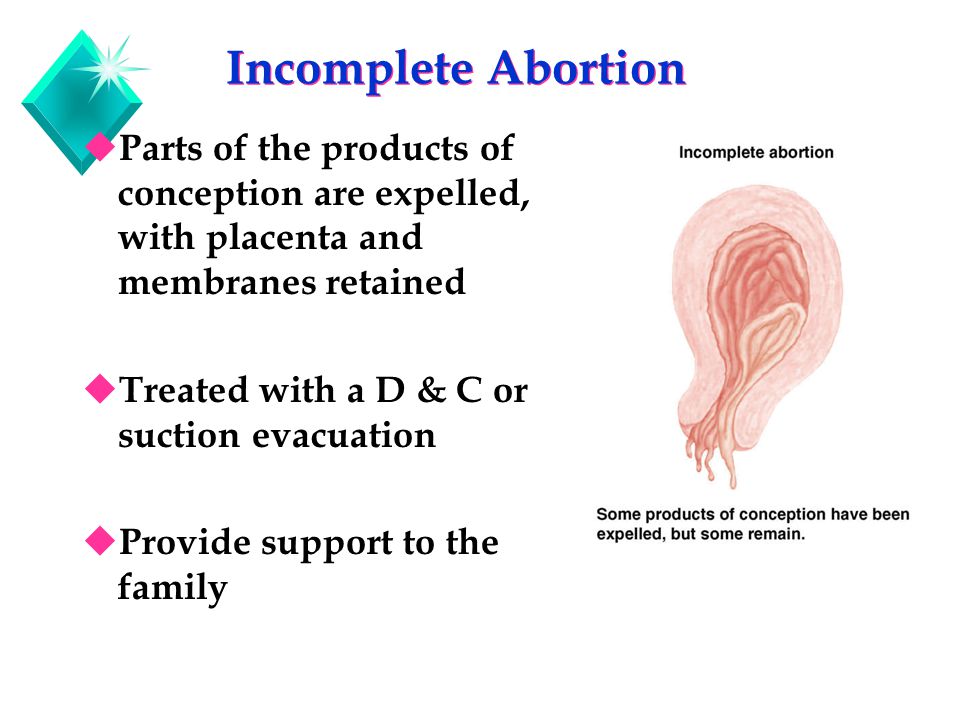
“If the placenta or a part of the placenta does not spontaneously deliver within 30 minutes after the baby has delivered, a retained placenta is diagnosed. Normally the placenta will separate and deliver from the uterus on its own once the baby has been born,” explains Sherry Ross, MD, OB-GYN.
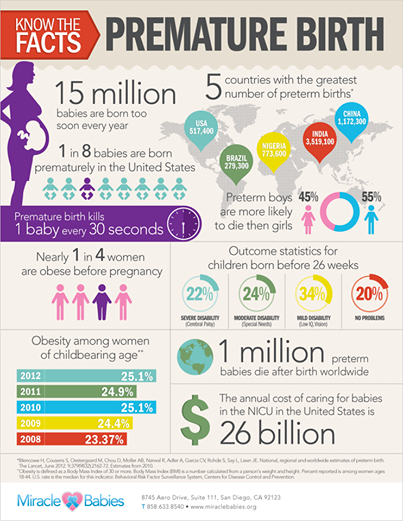
According to Ross, a retained placenta is rare but dangerous, and affects just 2 percent of all deliveries.
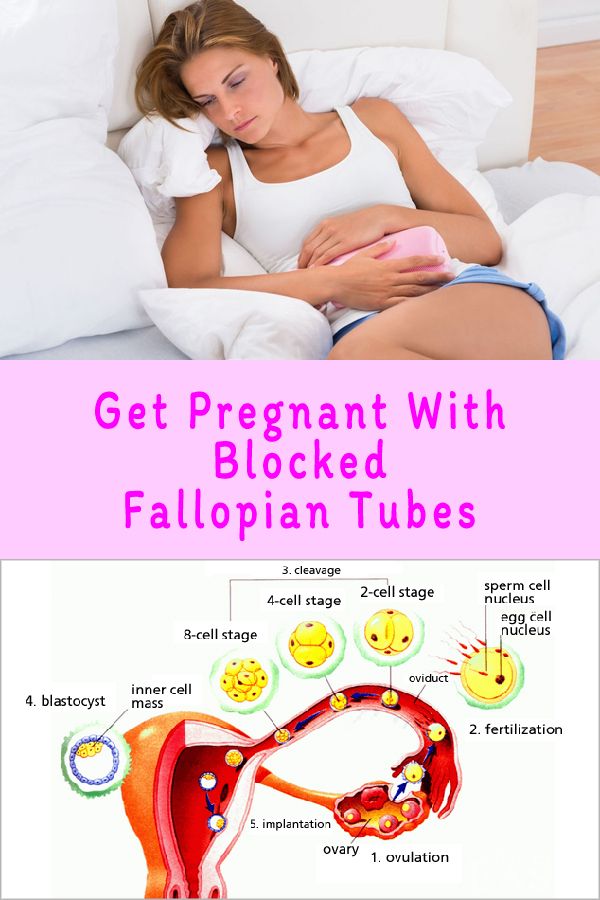
1. Placenta adherents happens when the placenta doesn’t separate spontaneously from the uterus within 30 minutes of the baby being born. This is the most common type of retained placenta.
2. A trapped placenta happens when the placenta separates from the uterus but doesn’t spontaneously leave the uterus.
3. Placenta accreta happens when the placenta grows into the deeper layer of the uterus and is unable to spontaneously detach from the uterus. This is the most dangerous type of retained placenta and can lead to needing a hysterectomy and blood transfusions.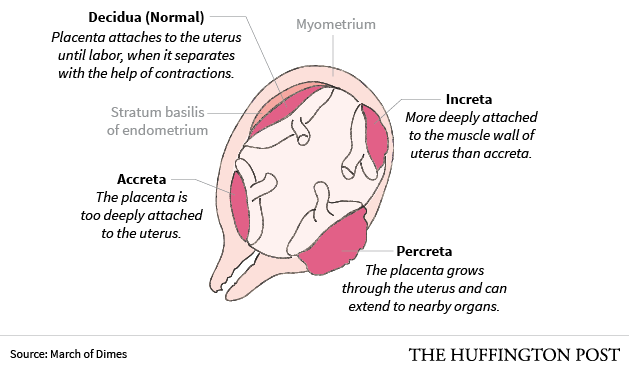
Ross also notes that retained placenta during a C-section is likely placenta accreta, and can be dangerous and the most difficult to treat.
My research had prepared me for the intellectualization of birth-related pain. However, the reality was much worse.
It hurt to sneeze, pee, and I thought I would die during each doctor’s checkup to see if my uterus deflated.
Sadly, research couldn’t prepare me for the physical experience. And my introduction to birth-related pain had only begun.
At first, I was too concerned with my son’s health and the troubles he was having with keeping food down to worry about how I felt.
Any parent who has ever had a child in the NICU for any amount of time will tell you that everything else in the world stops mattering. Your only concern becomes how to help your baby — despite often being powerless.
Thankfully, my son was cleared to come home after 5 days. For the first time in nearly a week, I was present in my body, not just my mind.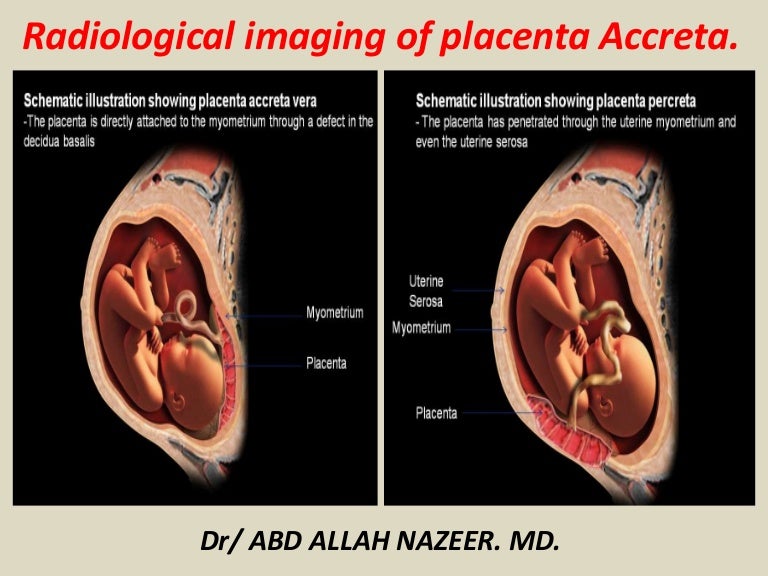 And being present in my body hurt much more than I expected.
And being present in my body hurt much more than I expected.
I was so distracted by the adjustment to motherhood that I was able to ignore my physical discomfort. Until it became too difficult to walk to get diapers.
In addition to extreme tiredness, I would experience intense bouts of abdominal pain at a moment’s notice.
I was three weeks postpartum and even though I had no knowledge of post-birth normalcy, an urge to push followed by lots of blood and large clots during a family outing let me know I needed to go to the emergency room.
But to my dismay, and despite informing them I was still passing large clots while being seen, the doctor declared my experiences a “normal part of the postpartum healing process.”
It didn’t matter what my initial postpartum checkup or the emergency room physician said — I knew something was wrong.
Each day post-birth, I felt progressively weaker instead of stronger
I was struggling so much that my relatives suggested I spend a few weeks in my hometown since my husband had returned to work.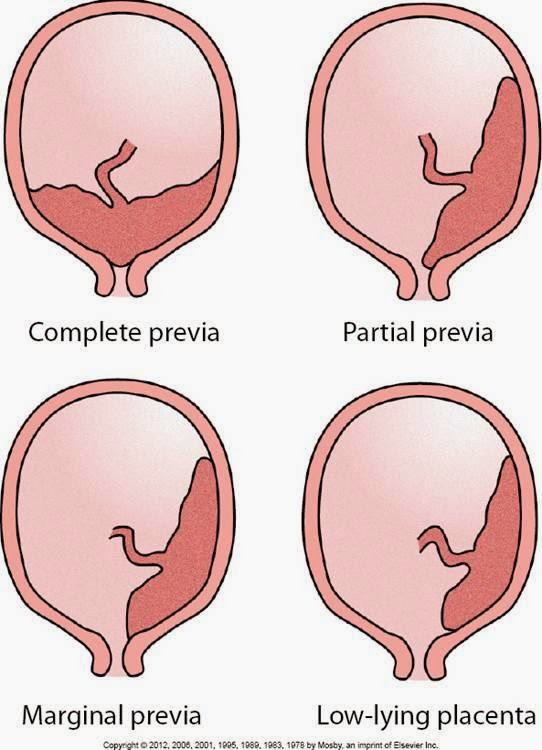 I was hesitant to leave my husband and travel with such a young baby. But I knew I couldn’t take care of a baby alone while my body was in such extreme pain.
I was hesitant to leave my husband and travel with such a young baby. But I knew I couldn’t take care of a baby alone while my body was in such extreme pain.
I didn’t physically feel better there, but I had much more support. One day, I felt gross (pain and motherhood were a setback for self-care) and ambitiously tried to take a bath. The walk down the hall was too much for my body, and I started feeling faint. My son was nearby in his infant car seat but the pain intensified and I couldn’t reach him when he started crying.
I watched in horror as my bathwater became crimson from blood — I was passing clots again. And even though my son was less than 3 feet away, it might as well have been a mile.
Thankfully, my aunt returned shortly after and demanded we go to the hospital. I called the nurse line to inquire about my pain one more time and check that the visit would be covered by our insurance. I was told to go to the local emergency room.
I continued losing blood during the 5-hour wait to be seen in the ER, but the moment I was called back, the doctor knew something was wrong.
When my urine pregnancy test came back positive, I was immediately sent back from an ultrasound where I was diagnosed with retained placenta. I was put under anesthesia for a dilation and curettage (D & C), which is the procedure used to remove tissue left behind in the womb.
The rest was a blur.
Share on Pinterest
Unfortunately, thanks to my first birth experience, I’m at an increased risk for retained placenta if I have more children.
“Women who are high risk for a retained placenta include those who have had previous dilation and curettage (D & C), a premature delivery before 34 weeks, a stillborn, uterine abnormalities, or a long first or second stage of labor. If you have had a previously retained placenta, you are also at risk for having it again with future pregnancies,” Ross explains.
Because of this, it’s important to look out for the symptoms of retained placenta and advocate for yourself if you see them.
Signs of retained placenta “The most common sign of a retained placenta is when the placenta fails to deliver spontaneously after 30 minutes once the baby has been born.
If pieces of the placenta have not delivered days or weeks after delivery, fever, persistent heavy bleeding with blood clots, cramping, pain, and a foul-smelling discharge may occur,” explains Ross.
I explained most, if not all, of those symptoms to a medical professional — so why wasn’t it caught sooner?
It could have been my race, considering the medical system has a long history of false beliefs relating to higher levels of pain tolerance for Black Americans. As a result, our discomfort is often overlooked.
It could have been my gender. Women regularly have their concerns ignored during birth. This mistreatment is one of many reasons things like birth trauma push women to opt out of multiple pregnancies due to the horrors of their first experiences.
And lastly, it could have been an intersection of these factors. The United States has the highest maternal mortality rates of any developed nation. While women of all races are at risk, Black women like myself are at a multiplied risk for complications and even death.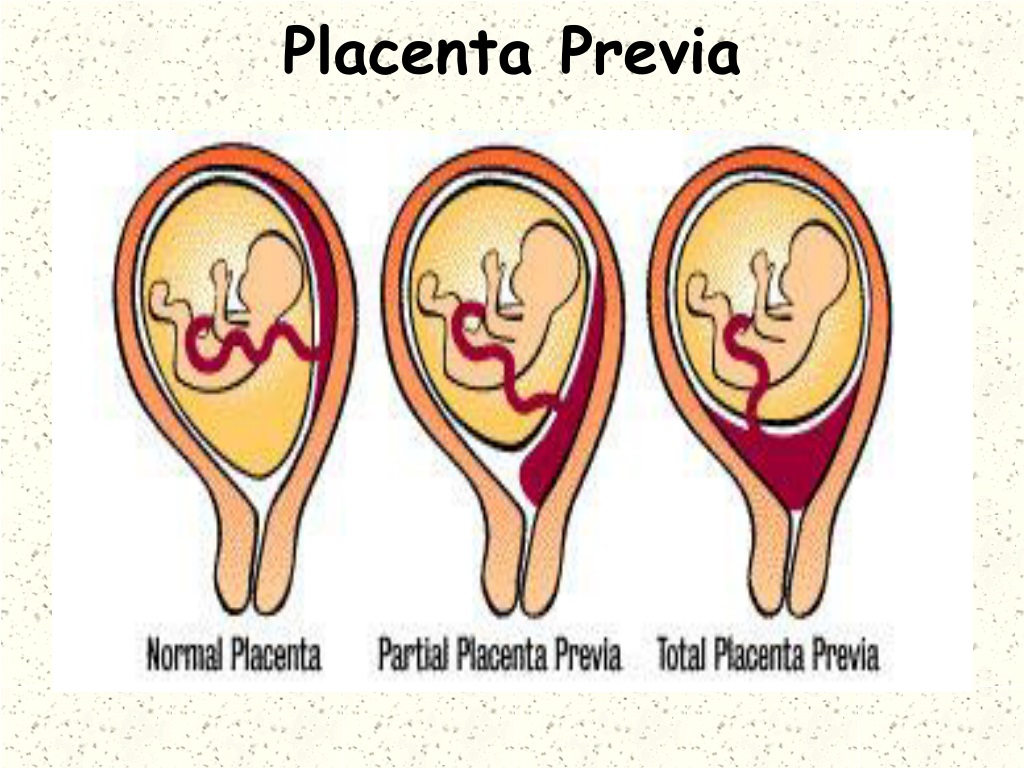
Through the experience, I felt ignored by my healthcare providers, and that hurt almost as much as my physical pain.
You may be at increased risk for a retained placenta if:
- you’re over age 30
- you give birth before the 34th week of pregnancy
- you experience a prolonged first or second stage of labor
- you have a stillbirth
I was lucky I got a diagnosis when I did. I was already over a month into motherhood and things could have easily gone differently.
“Complications of a retained placenta include heavy bleeding, infection, uterine scarring, blood transfusion, and hysterectomy. Any of these complications can lead to death if not diagnosed and treated quickly,” noted Ross.
Retained placenta made the adjustment to new motherhood even more difficult.
I was too fatigued to perform small tasks, like getting diapers from the other side of the room. The condition would also be seen as a potential cause for the breastfeeding challenges I was having — I wasn’t producing very much milk.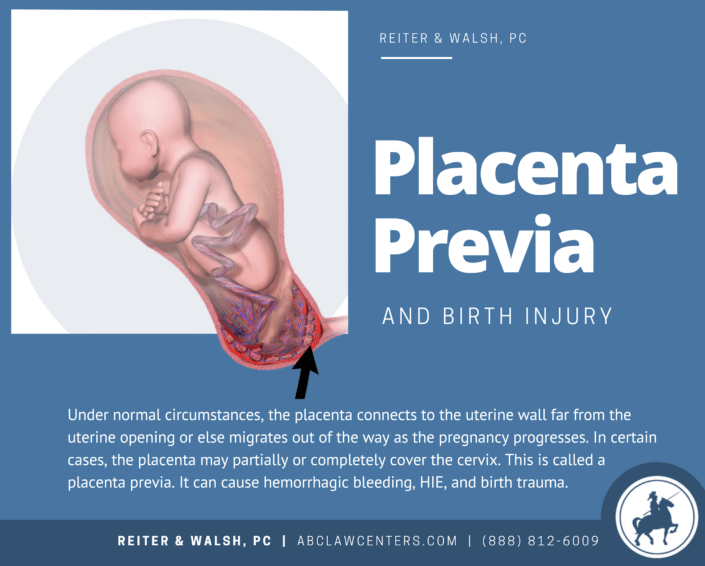
The experience robbed me of my earliest memories of first-time motherhood and left in their place flashbacks of physical pain. But more importantly, my experience greatly impacted my trust in the medical system.
No one should have to jump through that many hoops to get answers about their health.
But, still, being armed with knowledge about the signs of retained placenta might help you get the right treatment more quickly.
Share on Pinterest
Rochaun Meadows-Fernandez is a diversity content specialist whose work can be seen in The Washington Post, InStyle, The Guardian, and other places. Follow her on Facebook and Twitter.
Retained placenta | Pregnancy Birth and Baby
Retained placenta | Pregnancy Birth and Baby beginning of content3-minute read
Listen
A retained placenta is when the placenta is not delivered within 30 minutes of the baby’s birth. It is a serious problem since it can lead to severe infection or life-threatening blood loss.
It is a serious problem since it can lead to severe infection or life-threatening blood loss.
Retained placenta is not a common condition, but because it’s serious, it will need to be managed by a medical team.
What causes retained placenta?
A placenta can be retained if your contractions aren’t strong enough to expel it, or if the cervix closes and traps the placenta inside your uterus.
You are more at risk of a retained placenta if you are over the age of 30, have a premature baby or if your first and second stages of labour were very long. It can also happen if you have a fibroid or another problem with your uterus.
Many women will have an injection of syntocinon (a synthetic version of the hormone oxytocin), which not only helps deliver the placenta but also helps reduce the risk of postpartum bleeding. Having this injection is called ‘active management’. If the mother chooses not to have the injection, it is called ‘expectant management’.
What are the symptoms of retained placenta?
The main symptom of retained placenta is that the placenta doesn’t completely come out of the uterus after the baby is born. Another symptom can be bleeding before the placenta comes out.
If a piece of placenta is left behind, you may develop symptoms days or weeks after the birth. These may include:
- fever
- a bad smelling discharge from the vagina
- heavy bleeding
- large pieces of tissue coming out of the vagina
- pain
What is the treatment for a retained placenta?
Sometimes retained placenta can be treated simply if you empty your bladder, change position and have the doctor or midwife gently pull on the umbilical cord.
If that doesn’t work, you will need a procedure to remove the placenta. You will be taken into surgery after the birth and given an epidural or anaesthetic so you don’t feel anything. Your doctor will use an instrument called a curette to scrape away the lining of the uterus.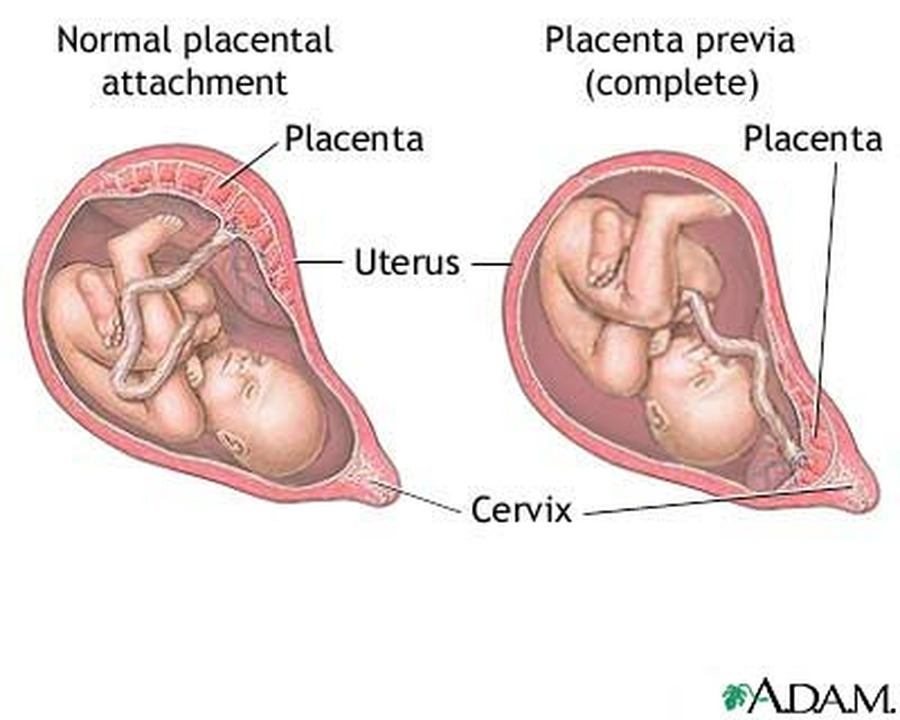
While you’re waiting for surgery, the medical team will keep a close eye on you to check you're not bleeding heavily (postpartum haemorrhage). The procedure itself is quick, but you will need to be monitored for several hours after to make sure you are not bleeding.
If you do start to experience some of the symptoms mentioned above in the days and weeks after you have had your baby, it’s important to see your doctor immediately. It is not always obvious after the placenta has been delivered that some tissue may have been left behind and this can lead to infection and bleeding. If you are bleeding heavily after the birth, you will need surgery to investigate the cause.
Sources:
RANZCOG (Management of Postpartum Haemorrhage (PPH)), King Edward Memorial Hospital (Retained placenta), Women's and Newborn Health Westmead Hospital (The birth of your placenta), International Journal of Women's Health (Retained placenta after vaginal delivery: risk factors and management)Learn more here about the development and quality assurance of healthdirect content.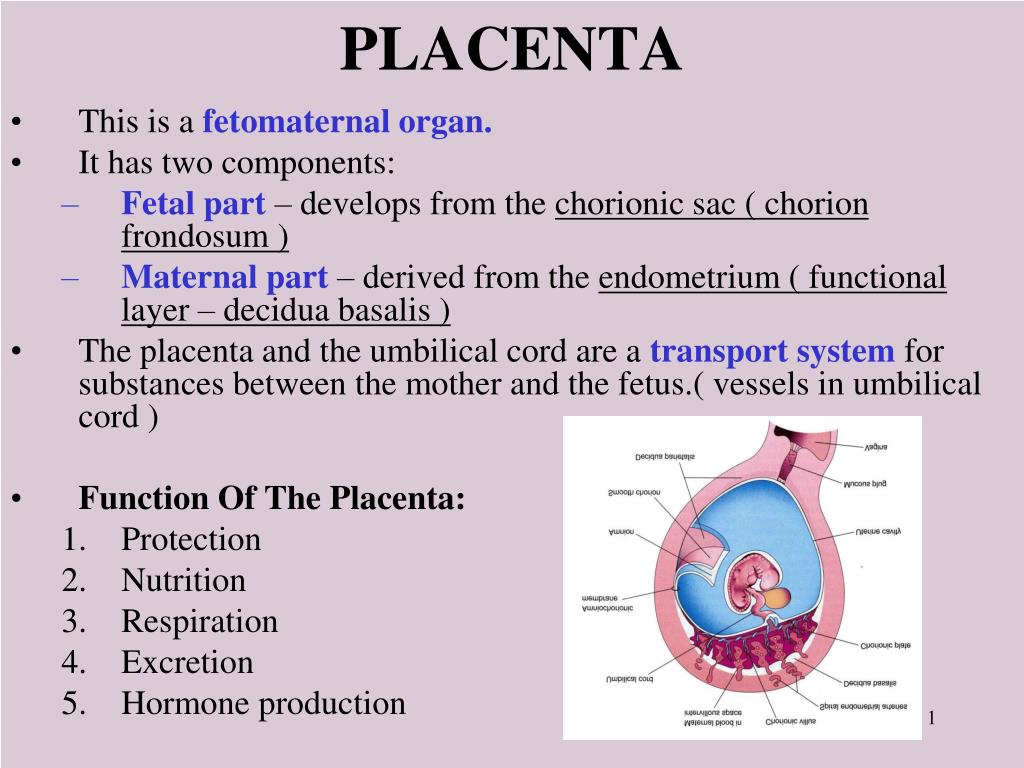
Last reviewed: February 2020
Back To Top
Related pages
- Placenta complications in pregnancy
- About the placenta
Need more information?
Labour complications
Even if you’re healthy and well prepared for childbirth, there’s always a chance of unexpected problems. Learn more about labour complications.
Read more on Pregnancy, Birth & Baby website
Asherman Syndrome
Read more on RANZCOG - Royal Australian and New Zealand College of Obstetricians and Gynaecologists website
Why do some mums stop breastfeeding before 6 months?
Most new parents know 'breast is best', but while more than 9 out of 10 babies are breastfed at birth, few mums are breastfeeding exclusively 5 months later.
Read more on Pregnancy, Birth & Baby website
What is freebirth?
Freebirth is when a woman chooses to birth her baby without medical or midwifery assistance, but this greater independence comes with some risks.
Read more on Pregnancy, Birth & Baby website
About the placenta
The placenta develops inside the uterus (womb) during pregnancy. It gives your baby nutrients and oxygen. Find out more about the placenta here.
Read more on Pregnancy, Birth & Baby website
Postpartum haemorrhage
Postpartum haemorrhage is when you bleed more than normal after giving birth. It can be very serious and requires medical attention right away.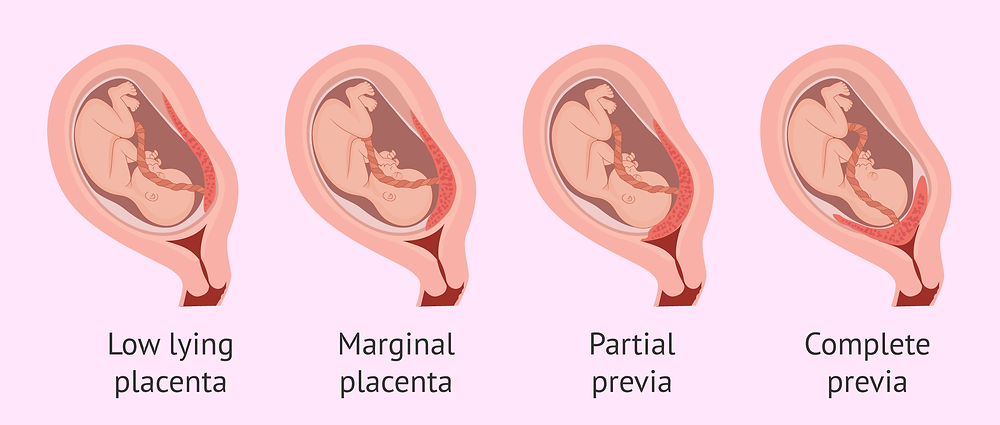
Read more on Pregnancy, Birth & Baby website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.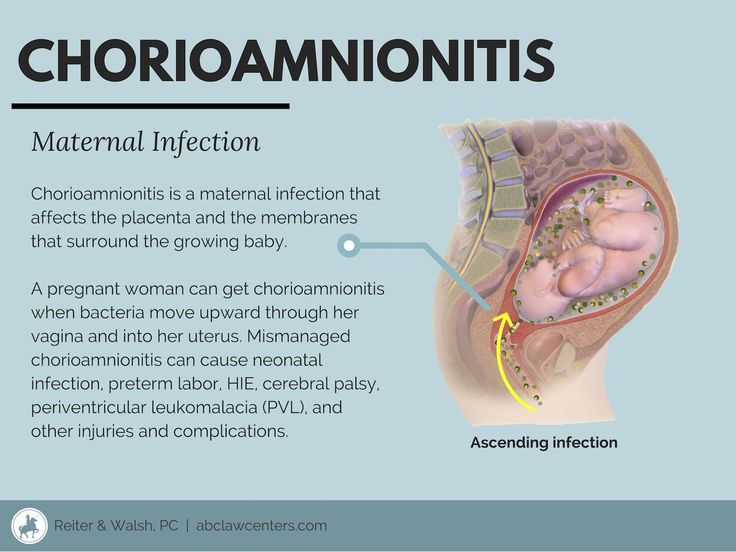
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Delayed placenta separation - causes, symptoms, diagnosis and treatment
Delayed placenta separation is a complication of the third stage of labor, a condition in which the placenta does not fully or partially exfoliate from the uterine walls. Clinically, it can be manifested by pathological bleeding or the absence of bloody discharge normal for this period, soreness, or the absence of attempts.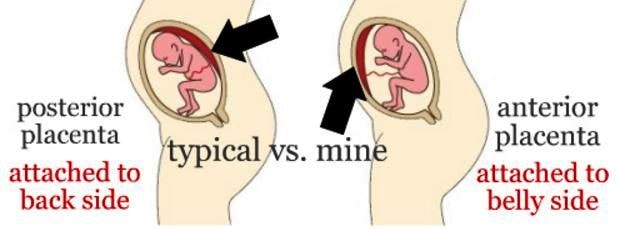 In this case, the standing of the bottom of the uterus corresponds to the period after the expulsion of the fetus, the connection of the umbilical cord with the uterus is indirectly determined. The diagnosis is established on the basis of the results of a physical examination, ultrasound. Most often, manual separation of the placenta or surgical treatment is performed.
In this case, the standing of the bottom of the uterus corresponds to the period after the expulsion of the fetus, the connection of the umbilical cord with the uterus is indirectly determined. The diagnosis is established on the basis of the results of a physical examination, ultrasound. Most often, manual separation of the placenta or surgical treatment is performed.
General
According to the WHO definition, retained placenta is diagnosed if separation does not occur within half an hour after the end of the second stage of labour. The incidence of pathology is 0.8-1.2% of all births. This complication is more often recorded in multiparous, especially those with a history of caesarean section. The disease is a serious problem of modern obstetrics, as it is often accompanied by postpartum hemorrhage. Bleeding is the cause of maternal death in a quarter of cases, 30% of which are the result of delayed separation of the placenta.
Delayed separation of the placenta
Causes
The etiology of delayed separation of the placenta has not been fully understood.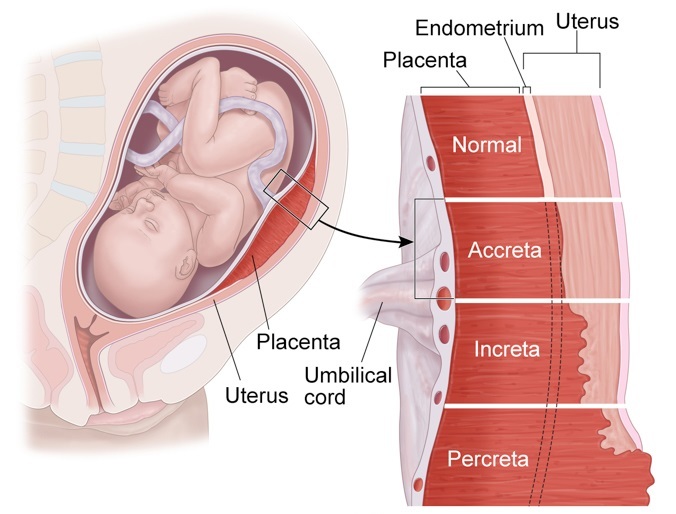 Violations of detachment of the placenta and its parts in the afterbirth period, on the one hand, may be due to defects in uterine contractile activity, on the other hand, due to excessively tight attachment of the child's place. Most women in labor fail to detect any visible disorders. The main causes of pathology include:
Violations of detachment of the placenta and its parts in the afterbirth period, on the one hand, may be due to defects in uterine contractile activity, on the other hand, due to excessively tight attachment of the child's place. Most women in labor fail to detect any visible disorders. The main causes of pathology include:
- Hypotension of the uterus. Weak contractions of the uterine muscles are not enough to start the process of separation of the placenta, even if the placenta does not have specific features that prevent detachment. In the presence of predisposing conditions, a slight decrease in contractile function can become a trigger for the development of pathology.
- Tight attachment of the placenta. Due to the depletion of the basal layer of the decidua and is characterized by a stronger than normal connection with the uterine walls without the germination of the chorionic villi into the myometrium. With the pathology under consideration, the force of uterine contractions is not enough to completely separate the placenta, which leads to bleeding.
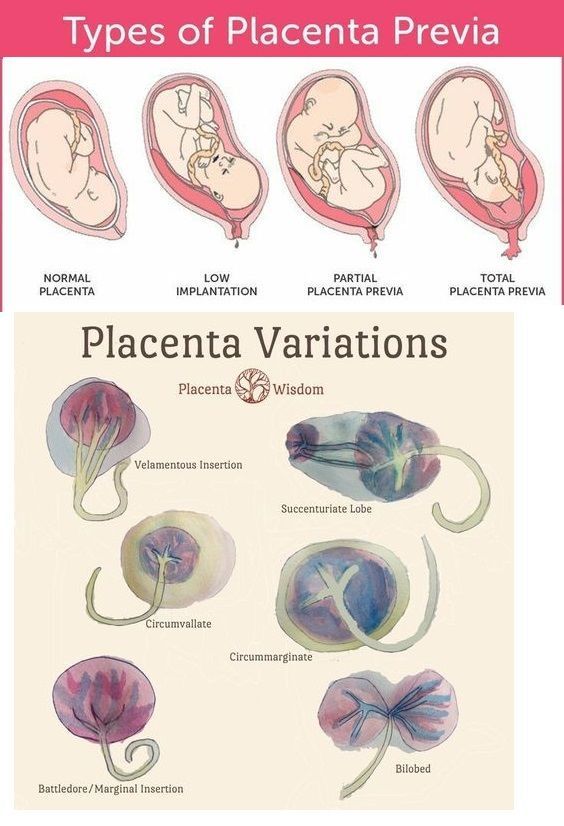
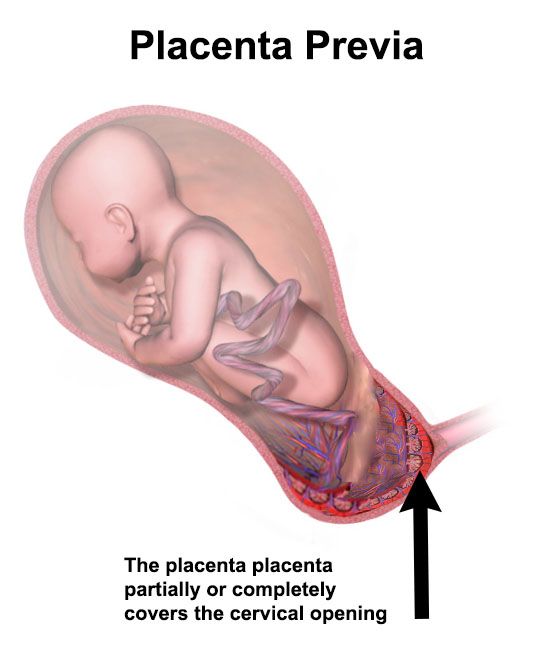
- True placental accreta. Also associated with underdevelopment of the basal layer, however, in this case, there is invasion of the villi into the muscle tissue, and in rare cases, the serosa of the uterus. More common with placenta previa. Spontaneous detachment of the adherent child's place is impossible, manual separation can lead to perforation of the uterine wall.
- Anomalies in the development of the placenta. Delayed detachment is often observed with developmental anomalies (lobed, two- and three-lobed or with additional lobules) of the placenta. The separation of the afterbirth is difficult with the so-called "membraneous" placenta, which is characterized by a slight thickness and a large attachment area, often extending to the entire uterine wall.
The most significant risk factors are the endometritis transferred before the onset of pregnancy, obstetric history (surgery on the uterus, abortions, multiple births), indicating traumatic injuries.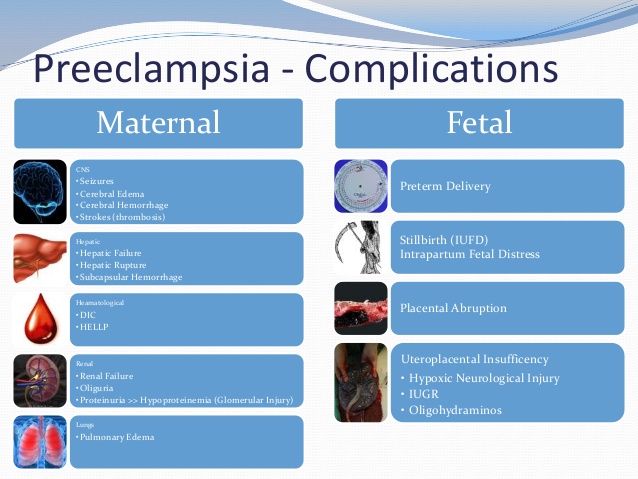 Inflammation and trauma lead to anatomical and histological changes in the uterus, which negatively affects placentogenesis and myometrial tone. Predisposing conditions include hyperandrogenism, malformations of the uterus (bicornuate uterus, intrauterine septum), volumetric formations (myoma, nodular adenomyosis).
Inflammation and trauma lead to anatomical and histological changes in the uterus, which negatively affects placentogenesis and myometrial tone. Predisposing conditions include hyperandrogenism, malformations of the uterus (bicornuate uterus, intrauterine septum), volumetric formations (myoma, nodular adenomyosis).
Pathogenesis
Normally, after the birth of the fetus, afterbirth contractions appear, in which contractions spread to the entire uterus, including the placental site (previously, the muscles of this zone did not function). Labor activity leads to detachment of the child's place in the area of the spongy layer of the mucosa (with the preservation of the basal layer), and then to its exit to the outside. The separation of the placenta is accompanied by damage to blood vessels, physiological bleeding. After his birth, the uterus contracts, which helps to stop the bleeding.
In the presence of unfavorable factors and predisposing conditions, detachment is difficult.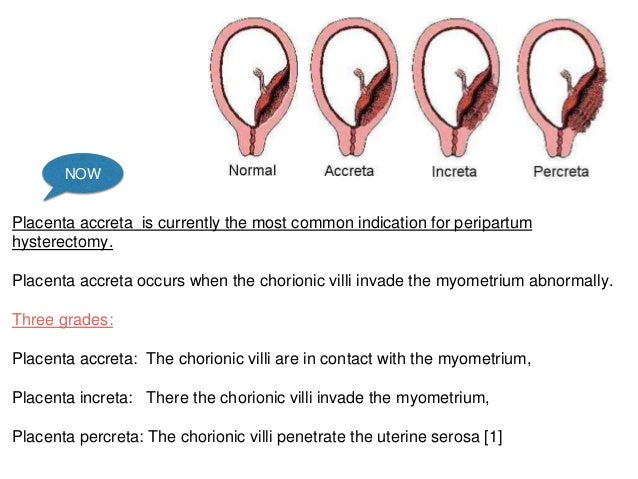 With partial detachment, if the process started, but for some reason stopped, the gaping vessels of the uncontracted uterus become a source of pathological blood loss. Ingrown chorionic villi deep into the myometrium lead to thinning of the uterine wall, so an attempt to manually separate the placenta quickly ends in trauma, accompanied by intense bleeding.
With partial detachment, if the process started, but for some reason stopped, the gaping vessels of the uncontracted uterus become a source of pathological blood loss. Ingrown chorionic villi deep into the myometrium lead to thinning of the uterine wall, so an attempt to manually separate the placenta quickly ends in trauma, accompanied by intense bleeding.
Symptoms
Subjective signs of delayed separation of the placenta include prolonged, painful, ineffective attempts after the birth of a child or their complete absence. An objective sign is intense bleeding observed with partial separation. If detachment of the placenta does not occur at all, even in a partial volume (for example, with a complete increment), bloody discharge from the birth canal may be absent.
Complications
The most common complication of delayed separation of the placenta is bleeding. Significant blood loss leads to such a potentially fatal complication as hemorrhagic shock, accompanied by multiple organ failure. Massive bleeding often develops when professional medical care is not provided in time (the risk increases sharply during childbirth outside a medical institution).
Massive bleeding often develops when professional medical care is not provided in time (the risk increases sharply during childbirth outside a medical institution).
Other frequent complications of this pathology include purulent-inflammatory diseases (postpartum endometritis, pelvioperitonitis, obstetric sepsis), which can be the result of both surgical treatment and retention of placenta fragments in the uterine cavity. In addition, the remaining ingrown placenta can become a source of late postpartum hemorrhage, uterine rupture during a subsequent pregnancy.
Diagnosis
The diagnosis of retained placenta is made by the obstetrician if there is no discharge of the placenta within thirty minutes after the birth of the infant with appropriate results of the physical examination. To establish the causes of the pathological condition (which determines the choice of treatment tactics), an ultrasound examination is additionally used.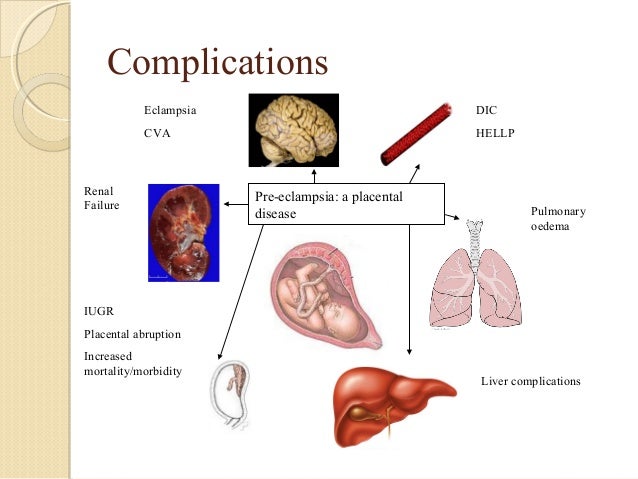
- Clinical examination. Signs of delayed separation of the placenta are determined by the shape and location of the uterus, the mobility of the umbilical cord. If separation has not occurred, the uterus is rounded, the bottom is located at the navel (Schroeder's sign), the outer segment of the umbilical cord does not lengthen (Alfeld's sign). The umbilical cord retracts with pressure over the womb (Kyustner-Chukalov's sign), after inhalation (Dovzhenko's sign), straining (Klein's sign).
- Ultrasonography. Ultrasound of the uterus is prescribed for the diagnosis of placenta accreta. Ultrasound signs of this pathology include deformation of the internal contour of the uterine cavity, its uneven expansion, and the absence of a hypoechoic layer between the myometrium and the placenta. Ultrasound angiography reveals hypervascularization of the anterior wall, chaotic branching of vessels.
If the placenta is retained, the volume of blood lost is estimated (abnormal blood loss is more than 400-500 ml).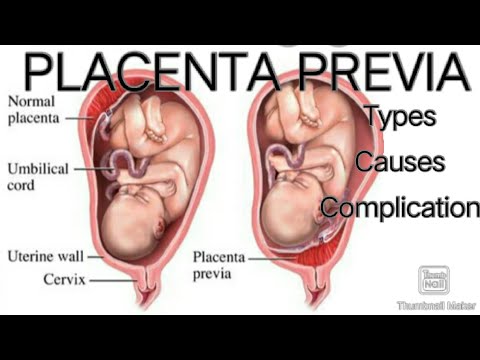 If a surgical operation is necessary, a coagulogram and a clinical blood test are examined. Differential diagnosis is carried out with a delay in the birth of the separated placenta, primarily with its infringement due to uneven or spastic contractions of the myometrium.
If a surgical operation is necessary, a coagulogram and a clinical blood test are examined. Differential diagnosis is carried out with a delay in the birth of the separated placenta, primarily with its infringement due to uneven or spastic contractions of the myometrium.
Treatment of delayed separation of the placenta
Conservative therapy
Therapeutic measures to promote the separation of the placenta are carried out only in the absence of pathological bleeding, and can last for 20-30 minutes. With the ineffectiveness of conservative treatment, surgical methods are used; in case of pathological blood loss, replacement blood transfusion is performed. Therapy is aimed at strengthening uterine contractions and includes:
- Bladder catheterization. Since the muscular layer of the bladder is closely connected with the nerve fibers of the uterine muscles, irritation of the urothelial receptors leads to a reflex contraction of the myometrium.
 Catheterization normalizes the course of the afterbirth period of childbirth, contributes to the timely separation and release of the placenta.
Catheterization normalizes the course of the afterbirth period of childbirth, contributes to the timely separation and release of the placenta. - Medicines. Intravenous or intramuscular administration of uterotonic drugs (oxytocin preparations are preferred) in combination with cord traction is indicated to enhance labor activity. In parallel, intravenous transfusion of crystalloid solutions is performed to correct possible blood loss.
Surgical treatment
Surgical treatment of delayed separation can be performed non-surgical or operatively. Treatment tactics depend on the cause of the pathology. Surgical intervention should be carried out in a timely manner, before the onset of generalized coagulopathy against the background of massive bleeding (otherwise, the operation aggravates the severity of the condition). In order to stop bleeding, embolization of the uterine vessels, the imposition of hemostatic sutures are used.
- Handbook. In case of tight attachment of the child's place or other reasons for the delay in its detachment (with the exception of true increment), manual separation of the placenta is performed with its subsequent removal to the outside. To avoid traumatic shock, intravenous anesthesia is performed before manipulation. Antibiotics (penicillin, cephalosporin) are used to prevent septic complications.
- Surgery. Indicated for failure of conservative bleeding management, true increment. The volume can vary from organ-preserving surgery (excision of the area of a partially ingrown child with affected myometrium and subsequent plasty) to radical (extirpation of the uterus, supravaginal amputation) with complete ingrowth, intractable bleeding.
Forecast and prevention
In case of timely started adequate treatment, the prognosis for life is favorable. The possibility of further implementation of the reproductive function largely depends on the presence of complications, the cause of the delay in the separation of the placenta.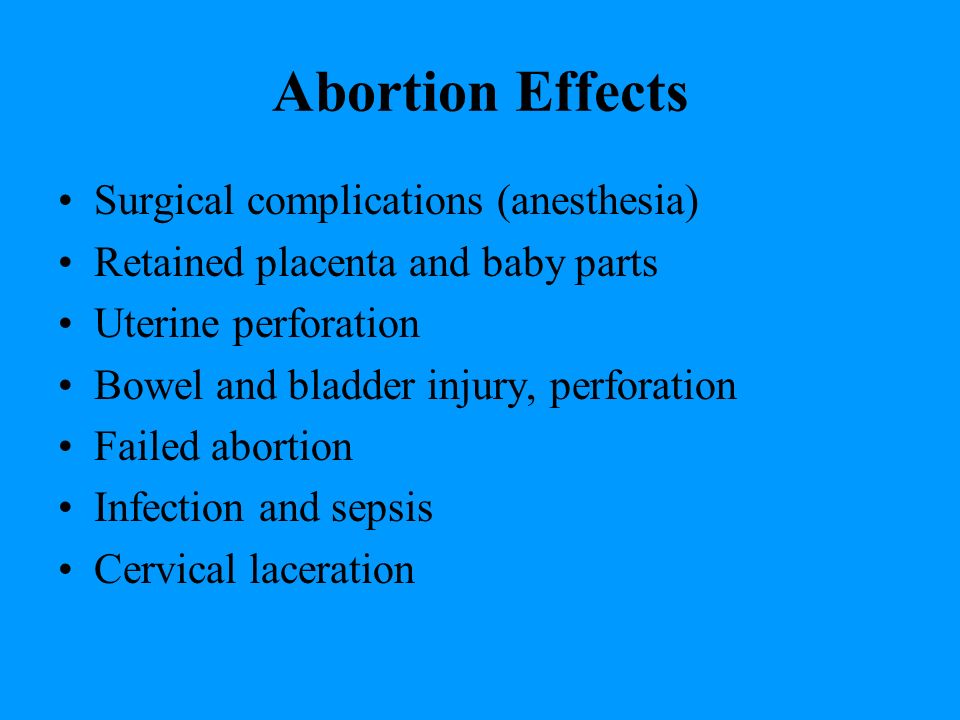 Primary prevention consists in the fight against abortion, the treatment of inflammatory diseases and the correction of endocrine disorders at the stage of preconception preparation. An important aspect of secondary prevention is a planned obstetric ultrasound during the gestation period, which allows early detection of placental accreta and the choice of tactics of labor management.
Primary prevention consists in the fight against abortion, the treatment of inflammatory diseases and the correction of endocrine disorders at the stage of preconception preparation. An important aspect of secondary prevention is a planned obstetric ultrasound during the gestation period, which allows early detection of placental accreta and the choice of tactics of labor management.
Retention or strangulation of the separated placenta
In cases where there is a strangulation of the placenta in the area of the tubal angle, when examining the abdomen, a protrusion is determined, separated by a constriction from the rest of the uterine body. With the infringement of the separated placenta as a result of a spasm of the circular muscles of the internal os, the uterus takes the form of an hourglass. If there was a delay in the separated placenta without infringement, the uterus has a shape and all signs of separation of the placenta.
Retention and incarceration of the separated placenta is differentiated from dense attachment or accreta of the placenta.
Causes of retained placenta
Retained placenta is associated with insufficient contractile activity of the uterus and abdominal muscles. Contributing to this:
- full bladder,
- hyperdistension of the uterus - large fetus, polyhydramnios, multiple pregnancies,
- premature or delayed birth,
- weakness of labor,
- overwork of a woman in labor,
- rapid operative delivery,
- underdeveloped abdominal muscles.
Causes of incarceration
Incarceration of the placenta may occur as a result of uterine spasm with irrational management of the afterbirth period:
- rough massage of the uterus,
- untimely attempts to squeeze out the placenta according to Krede-Lazarevich,
- cord pulling,
- unreasonable use of large doses of oxytocin.
Such unreasonable actions disrupt the physiological rhythm and the force of distribution of subsequent contractions of the uterine muscles, lead to convulsive contraction of individual muscle groups, uneven separation of parts of the placenta and bleeding.
Treatment
In case of placental incarceration , women in labor are injected with antispasmodics and, under intravenous anesthesia, an attempt is made to isolate the placenta according to Krede-Lazarevich. If it turns out to be ineffective, they immediately begin to manually remove the placenta under anesthesia.
In case of retained placenta and compensated blood loss, the woman in labor is catheterized, after which she is offered to push. If attempts are ineffective, they try to isolate the placenta using the Abuladze or Krede-Lazarevich method. With heavy bleeding, as well as in the absence of convincing signs of separation of the placenta, urgent manual removal of the placenta (under anesthesia) is indicated.
Verification of results
The delivered or artificially isolated afterbirth is carefully examined on both sides for integrity. If irregularities, roughness and depressions are found on the smooth shiny surface of the placenta, this is a sign of an afterbirth defect (delay of the placenta lobe or membranes).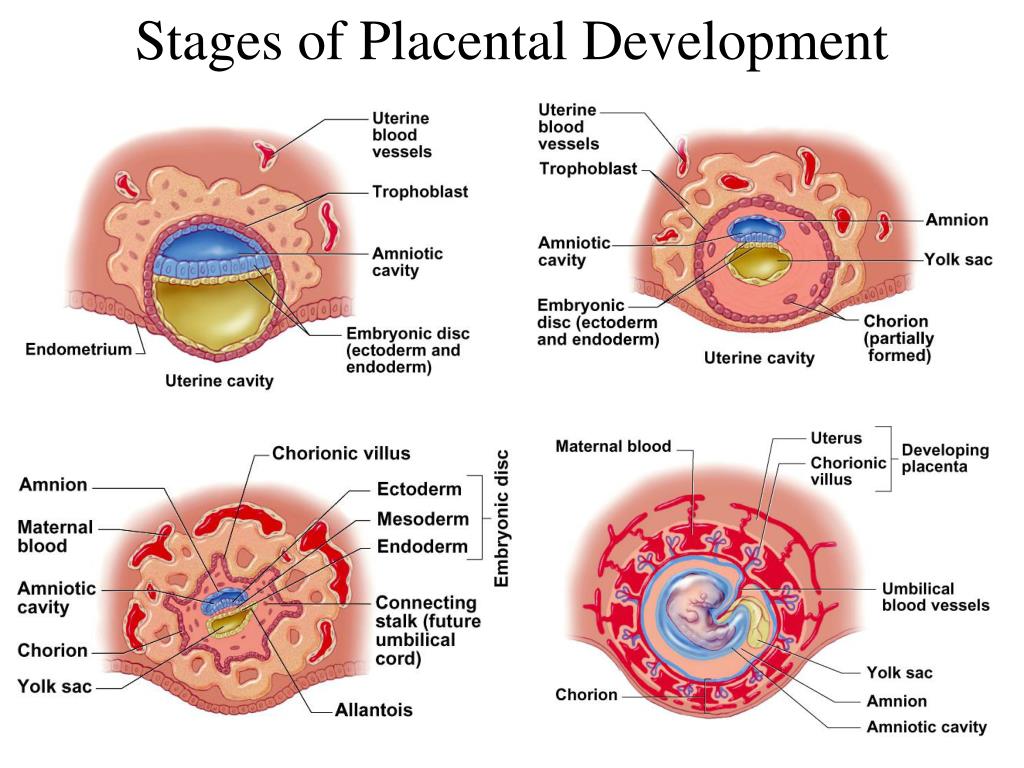
In case of retention of parts of the placenta or most of the membranes, as well as in case of suspicion of their retention, doctors immediately perform an operation - manual examination of the walls of the uterine cavity, separation and isolation of parts of the placenta, blood clots that prevent uterine contraction. The operation ends with intravenous administration of funds that reduce the uterus.
References
- Larroquette M., Peyraud F., Domblides C., Lefort F., Bernhard JC., Ravaud A., Gross-Goupil M. Adjuvant therapy in renal cell carcinoma: Current knowledges and future perspectives. // Cancer Treat Rev - 2021 - Vol97 - NNULL - p.102207; PMID:33906023
- Philips T., Van Royen K., Vanmierlo B., Goubau JF. Spontaneous index finger extensor tendon rupture in a SNAC wrist. // Hand Surg Rehabil - 2021 - Vol - NNULL - p.; PMID:33905941
- Gunjiyal MS., Mohammed S., Bhatia P., Chhabra S., Kumar M., Sharma A. Effect of combined versus sequential injection of 2% lidocaine and 0.
 5% bupivacaine on the onset and duration of supraclavicular brachial plexus block: A double-blinded randomized controlled trial. // J Clin Anesth - 2021 - Vol72 - NNULL - p.110313; PMID:33905902
5% bupivacaine on the onset and duration of supraclavicular brachial plexus block: A double-blinded randomized controlled trial. // J Clin Anesth - 2021 - Vol72 - NNULL - p.110313; PMID:33905902 - Brassard S.L., Balodis IM. A review of effort-based decision-making in eating and weight disorders. // Prog Neuropsychopharmacol Biol Psychiatry - 2021 - Vol - NNULL - p.110333; PMID:33905755
- Njom-Nlend A.E., Efouba N., Brunelle Sandie A., Fokam J. Determinants of Switch to Pediatric Second-Line Antiretroviral Therapy after First-Line Failure in Cameroon. // Trop Med Int Health - 2021 - Vol - NNULL - p.; PMID:33905593
- Biadgo B., Tamir W., Ambachew S. Insulin-like Growth Factor and its Therapeutic Potential for Diabetes Complications - Mechanisms and Metabolic Links: A Review. // Rev Diabetes Stud - 2020 - Vol16 - NNULL - p.24-34; PMID:33905470
- Baymler Lundberg AS., Esbensen BA., Jensen MB., Hauge EM., Thurah A. Facilitators and barriers in diagnosing rheumatoid arthritis as described by general practitioners: a Danish study based on focus group interviews.
 // Scand J Prim Health Care - 2021 - Vol - NNULL - p.1-8; PMID:33905289
// Scand J Prim Health Care - 2021 - Vol - NNULL - p.1-8; PMID:33905289 - Onal C., Kose F., Ozyigit G., Aksoy S., Oymak E., Muallaoglu S., Guler OC., Tilki B., Hurmuz P., Akyol F. Stereotactic body radiotherapy for oligoprogressive lesions in metastatic castration- resistant prostate cancer patients during abiraterone/enzalutamide treatment. // Prostate - 2021 - Vol - NNULL - p.; PMID:33905131
- Çelen Yoldaş T., Özmert EN. Communicative Environmental Factors Including Maternal Depression and Media Usage Patterns on Early Language Development. // Matern Child Health J - 2021 - Vol - NNULL - p.; PMID:33905063
- Schmidt N., Tödt I., Berg D., Schlenstedt C., Folkerts AK., Ophey A., Dimenshteyn K., Elben S., Wojtecki L., Liepelt-Scarfone I., Schulte C., Sulzer P. , Eggers C., Kalbe E., Witt K. Memory enhancement by multidomain group cognitive training in patients with Parkinson's disease and mild cognitive impairment: long-term effects of a multicenter randomized controlled trial.