Red spots on infants face
Common childhood rashes | Pregnancy Birth and Baby
If your child has a seizure, call triple zero (000) immediately and ask for an ambulance.
If you think your child might have meningococcal rash, go to the nearest emergency department immediately.
Key facts
- There are many different types of childhood rashes. Many are not serious.
- If your child has a rash and fever, they should see their doctor.
- If your child has a meningococcal rash, go immediately to the emergency department.
Meningococcal rash
If you think your child might have meningococcal rash, go to the nearest emergency department immediately.
You can read more about serious childhood rashes here.
Rashes with no fever or itching
Milia (blocked oil glands)
Up to 1 in every 2 newborn babies develop small white spots called milia on their face, especially on the nose. These are just blocked pores, and they’re not itchy or contagious. They usually clear up without treatment within a few weeks.
Erythema toxicum
Many newborns develop a blotchy red skin reaction called erythema toxicum, which can appear between 2 days and 2 weeks after birth. Flat, red patches or small bumps often first appear on the face and spread to the body and limbs. The rash is harmless, not contagious, and will clear after a few days or a week.
Baby acne
Some babies get pimples on their cheeks and nose in the first three months of life. These pimples normally disappear without any treatment, usually within a few months.
Nappy rash
Nappy rash is inflammation of the skin in the nappy area. It can look red, sore and inflamed. Nappy rash is usually caused by urine (wee) or faeces (poo) irritating the skin.
To avoid nappy rash, keep the nappy area clean and dry with frequent nappy changes and nappy-free time. You can help protect the skin by putting on a barrier cream such as zinc or soft white paraffin at each nappy change.
Persistent nappy rash can be treated with a medicated cream. Don’t use talcum powder or antiseptics to treat nappy rash. If your baby develops a fungal infection, you’ll need to use an antifungal ointment. Ask your doctor or pharmacist for advice.
Erythema multiforme (minor)
Erythema multiforme is a rash triggered by an infection (most commonly herpes simplex virus), medicine or an illness. Your baby might feel unwell or have a mild fever before the rash appears. Red spots develop on the hands, feet, arms and legs and spread symmetrically across both sides of the body. The spots often become raised or blistered and then develop into classic target-like lesions.
Erythema multiforme is not contagious, and usually resolves without treatment in 3 to 6 weeks.
Keratosis pilaris (‘chicken skin’)
Keratosis pilaris is a harmless condition where the skin becomes rough and bumpy, as if permanently covered in goose pimples. These bumps most commonly occur on the upper arms and thighs. You can try several things to help the rash to clear up, including moisturising regularly.
You can try several things to help the rash to clear up, including moisturising regularly.
Rashes that might be itchy
Eczema (Atopic dermatitis)
Eczema is a very common skin condition affecting 1 in 3 Australians. It causes the skin to become itchy, red, dry and cracked, often in the creases at the knees and elbows.
Eczema commonly starts before a baby is 12 months old. Eczema follows a relapsing-remitting course. This means that there are flare-ups of the rash, followed by periods where there is no rash or a minimal rash.
Eczema management includes preventative treatment such as avoiding skin irritants, moisturising regularly and using bath oil. Treatment of flare-ups includes using steroid and anti-inflammatory creams.
Ringworm (tinea)
Ringworm is a common, contagious skin infection that causes a ring-like red rash with a clear centre. It commonly occurs on the scalp, feet and groin, but it can appear almost anywhere on the body.
Ringworm is caused by a fungus, not a worm, and is usually treated with over-the-counter antifungal creams. You should keep your child home from childcare or school until a day after you have started treatment to prevent spreading the infection.
You should keep your child home from childcare or school until a day after you have started treatment to prevent spreading the infection.
Prickly heat (heat rash)
Heat rash might appear if your baby gets hot in a humid environment. The rash shows as tiny red bumps or blisters on the skin, which can be very itchy. Cooling your baby down and avoiding humidity is the best way to prevent heat rash, which usually clears within 2 to 3 days without treatment.
Impetigo (school sores)
Impetigo is a highly contagious bacterial infection of the skin. It causes red sores and blisters that form a yellow crust. It is very common in children aged 2 to 6, and it is not usually serious in this age group, but it can be dangerous for newborn babies.
If your child has impetigo, you should see your doctor, who might prescribe an antibiotic cream, ointment or tablet. This should clear the infection within 7 to 10 days. Keep your child home from childcare or school and away from young babies until the sores have dried up, usually a few days after treatment starts.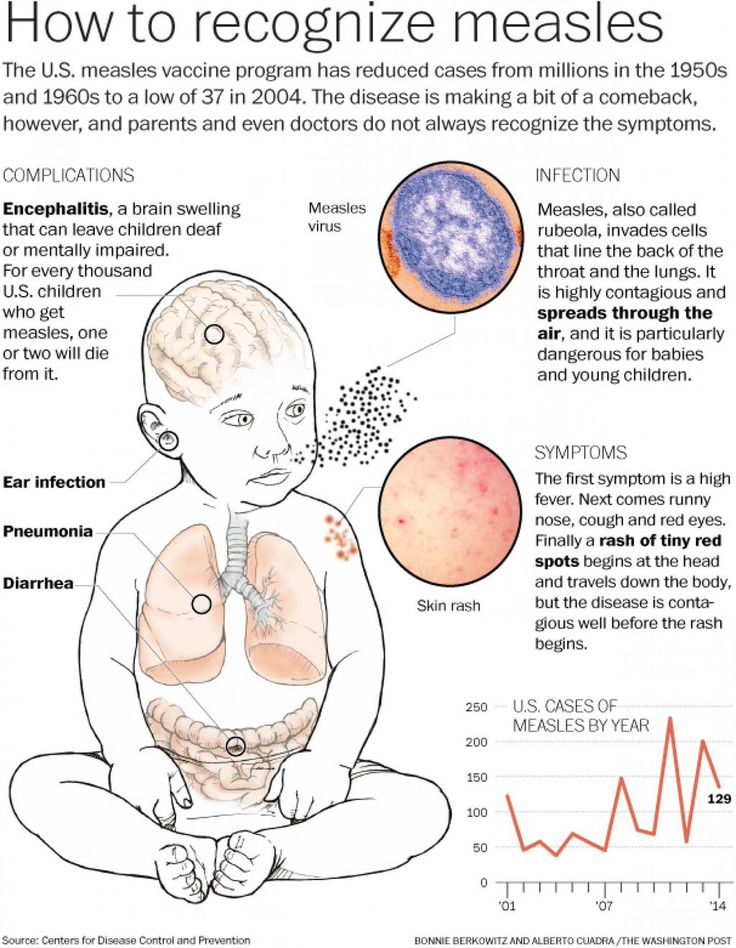
Hives (urticaria)
Hives is a raised, red, itchy rash. It is common on the chest, stomach and back, as well as the throat and limbs, but it can appear on any part of the body. Hives usually disappears within a few days without any treatment. Antihistamines can be given to relieve itching. If the rash doesn't go away, you should see your doctor.
Hives isn’t usually serious, but it can be a sign of a more serious allergic reaction (anaphylaxis). If your child develops hives after eating, or together with other symptoms such as vomiting, dizziness or trouble breathing, you should seek urgent medical attention.
If your child has symptoms of a serious allergic reaction (anaphylaxis), call triple zero (000) immediately and ask for an ambulance.
Pityriasis rosea
Pityriasis rosea is a mild skin rash that sometimes appears after a sore throat, cold or fever. It begins with a single pink or tan-coloured patch on the chest or back. Red, oval-shaped patches, which may be itchy, then appear on the chest or back and limbs over the next weeks.
The exact cause of pityriasis rosea is unclear, and it is not thought to be contagious. The rash usually clears up within a couple of months without treatment.
If you are pregnant, pityriasis rosea can in rare cases lead to complications. See your doctor if you are pregnant and have contact with a child who has pityriasis rosea.
Molluscum contagiosum
Molluscum contagiosum is a viral skin infection that is spread by skin-to-skin contact or by sharing swimming pool water, bath water or towels.
Molluscum contagiosum spots look like pimples and grow into round pearly white lumps, usually 2 to 5 millimetres in size. They can be itchy. They usually heal without treatment within 6 months, but sometimes longer.
Rashes with fever
Slapped cheek disease (fifth disease)
Slapped cheek disease is a viral infection that mainly affects pre-school and school-age children. It typically causes a bright red rash on both cheeks that spreads as a ‘lacy’ rash on the body and limbs. Occasionally, it causes a fever.
Occasionally, it causes a fever.
Slapped cheek disease is usually mild and clears up in a few days without treatment. The child is contagious before the rash appears, but not once it has appeared.
If you are pregnant and catch the virus, it may cause a type of anaemia in your unborn baby. It can also cause miscarriage. If you suspect you or your child has slapped cheek disease, you should avoid contact with people who might be pregnant.
Hand, foot and mouth disease
Hand, foot and mouth disease is a mild but highly contagious viral illness. It causes a rash on the palms of the hands and soles of the feet and blisters in the mouth. It is not the same as the foot-and-mouth disease that affects farm animals.
The disease is common in childcare and kindergartens. Your child might feel unwell and have a fever and blisters on the hands and feet and in the mouth and in the nappy area. The illness usually lasts about 7 to 10 days. Children with hand, foot and mouth disease should stay away from childcare or school until all the blisters have dried up.
Hand, foot and mouth disease usually resolves on its own without complications. In rare cases, it can be more serious, especially if you have a weakened immune system or are pregnant. Complications can include infections of the brain and heart muscle and miscarriage.
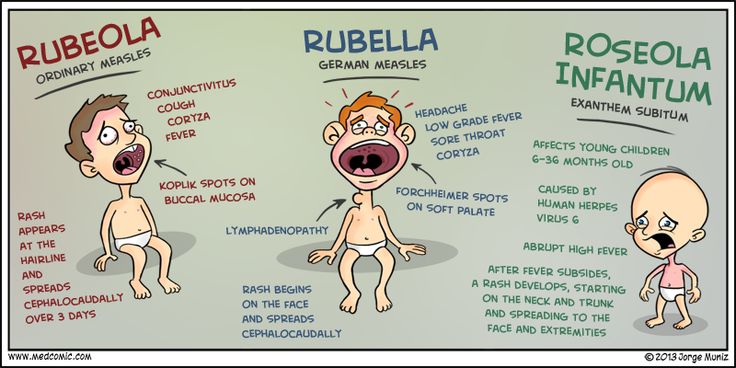
Roseola infantum
Roseola infantum is a contagious viral infection that can cause cold-like symptoms and a high fever. The high fever may last for a few days. Roseola infantum can also cause some children to have a febrile convulsion (seizure).
Children with roseola infantum develop a rash after the fever has resolved. The rash looks like raised pink spots that start on the chest, stomach and back and spread to the limbs. The child is contagious before the rash appears, but not after. The rash usually lasts 3 to 5 days.
Febrile convulsions can look scary but are generally not harmful.
If your child has a seizure, call triple zero (000) immediately and ask for an ambulance.
When to seek help
Many babies develop a skin rash in their first days or weeks of life as their sensitive skin adapts to a new environment. Most rashes are harmless and go away on their own, but if your baby seems unwell, or if you’re worried, you should see your doctor. They can advise about the cause and whether treatment is necessary.
Most rashes are harmless and go away on their own, but if your baby seems unwell, or if you’re worried, you should see your doctor. They can advise about the cause and whether treatment is necessary.
Whatever their age, you should take your child to the doctor if they have a rash and persistent high temperature, cold or cough symptoms or swollen neck glands.
Treatment of common childhood rashes
If you think your child might be contagious, they should stay at home. Keep them away from school, childcare and other children. You should also keep them away from people who are pregnant, or who might be pregnant, since some childhood infections can cause serious problems in unborn babies.
You can use paracetamol or ibuprofen (in babies aged over 3 months) to reduce fever — read the packet instructions carefully to ensure your child receives the right amount for their age and weight.
Your pharmacist can advise you on treating the symptoms of common rashes. For example, you can use over-the-counter creams to prevent itchiness.
If you are concerned about your child’s rash, call Pregnancy, Birth and Baby on 1800 882 436 to talk to a maternal child health nurse, or call Healthdirect on 1800 022 022 to talk to a registered nurse. Alternatively, contact your doctor.
Speak to a maternal child health nurse
Call Pregnancy, Birth and Baby to speak to a maternal child health nurse on 1800 882 436 or video call. Available 7am to midnight (AET), 7 days a week.
Learn more here about the development and quality assurance of healthdirect content.
Is It Baby Acne, a Rash, or Something Else?
Even adults can find it difficult to identify their skin issues. Everyone’s skin is different, and the way rashes and acne flare up can vary. Babies can’t tell you what they’re feeling, so you’ll have to go on looks alone.
Read on to learn about some of the most common skin issues that babies face and how you can treat them at home.
Baby acne usually develops about 2 to 4 weeks after birth. Tiny red or white bumps appear on the baby’s cheeks, nose, and forehead. The cause is unknown. It typically clears up on its own in about 3 to 4 months without leaving marks.
Tiny red or white bumps appear on the baby’s cheeks, nose, and forehead. The cause is unknown. It typically clears up on its own in about 3 to 4 months without leaving marks.
To treat baby acne, don’t use any of the over-the-counter acne products you’d use on yourself. These can damage your baby’s delicate skin.
Regular home care should be enough to treat baby acne:
- Wash your baby’s face daily with warm water. You may also try a gentle, unscented soap.
- Do not scrub hard or pinch irritated areas.
- Avoid lotions and oily face products.
If you’re concerned that your baby’s acne isn’t going away, their doctor can recommend or prescribe safe treatments.
Eczema is a skin condition that causes a dry, red, itchy, and sometimes painful rash. It’s more common in children and often develops in the first 6 months of life. The condition can continue as the child gets older, or they may grow out of it.
In babies up to 6 months old, eczema often appears on the cheeks or forehead. As the baby gets older, the rash may move to the elbows, knees, and skin creases.
As the baby gets older, the rash may move to the elbows, knees, and skin creases.
Eczema flares up when the skin is dry or when the skin comes into contact with an allergen or irritant, such as:
- pet dander
- dust mites
- detergent
- household cleaner
Drooling can also irritate eczema around the chin or mouth.
There’s no cure for eczema, but there are ways to manage your baby’s symptoms:
- Give your baby short, lukewarm baths (between 5 and 10 minutes) and use an unscented or gentle soap on the affected areas.
- Use a thick, unscented cream or ointment as a moisturizer twice a day.
- Use fragrance-free laundry detergent designed for sensitive skin.
Your baby’s pediatrician may be able to prescribe a steroid ointment to help reduce inflammation. Use this as directed by their doctor.
Milia are tiny white bumps on a newborn’s nose, chin, or cheeks that look similar to acne. They can also appear on the baby’s arms and legs. The bumps are caused by dead skin flakes becoming trapped near the skin’s surface. Like baby acne, milia go away without treatment.
The bumps are caused by dead skin flakes becoming trapped near the skin’s surface. Like baby acne, milia go away without treatment.
However, you can use the same at-home care:
- Wash your baby’s face daily with plain water or if needed, an unscented or gentle soap.
- Do not scrub hard or pinch the irritated areas.
- Avoid lotions or oily face products.
Cradle cap looks like scaly, yellowish, crusty patches on the baby’s head. Depending on your baby’s skin tone, the patches may appear yellowish, brown, purple, or grey.
Cradle cap usually develops when a baby is 2 or 3 months old. There may also be redness surrounding the patches. This rash may also appear on the baby’s:
- face
- eyebrows
- neck
- ears
- armpits
Cradle cap is not harmful to your baby. It’s not itchy like eczema. It’ll go away on its own in a few weeks or months without treatment.
Some things you can do at home to manage cradle cap are:
- Wash your baby’s hair and scalp with a gentle shampoo.

- Brush scales out with a soft-bristled hairbrush.
- Avoid washing hair too often, as it’ll dry out the scalp.
- Use baby oil to soften the scales so they’re easier to brush out.
Heat rash is caused when sweat gets trapped under the skin because of blocked pores. It’s usually caused by exposure to hot or humid weather. When a baby gets heat rash, they develop tiny, red, fluid-filled blisters. These can appear on the:
- neck
- shoulders
- chest
- armpits
- elbow creases
- groin
The rash generally goes away within a few days without treatment. However, see your baby’s doctor if they develop a fever or if the rash:
- does not go away
- looks worse
- gets infected
To avoid overheating, dress your baby in loose-fitting cotton clothing during hot summer months. Take off extra layers if they get too hot in cooler weather.
Hand, foot, and mouth disease (HFMD) is a highly contagious viral infection.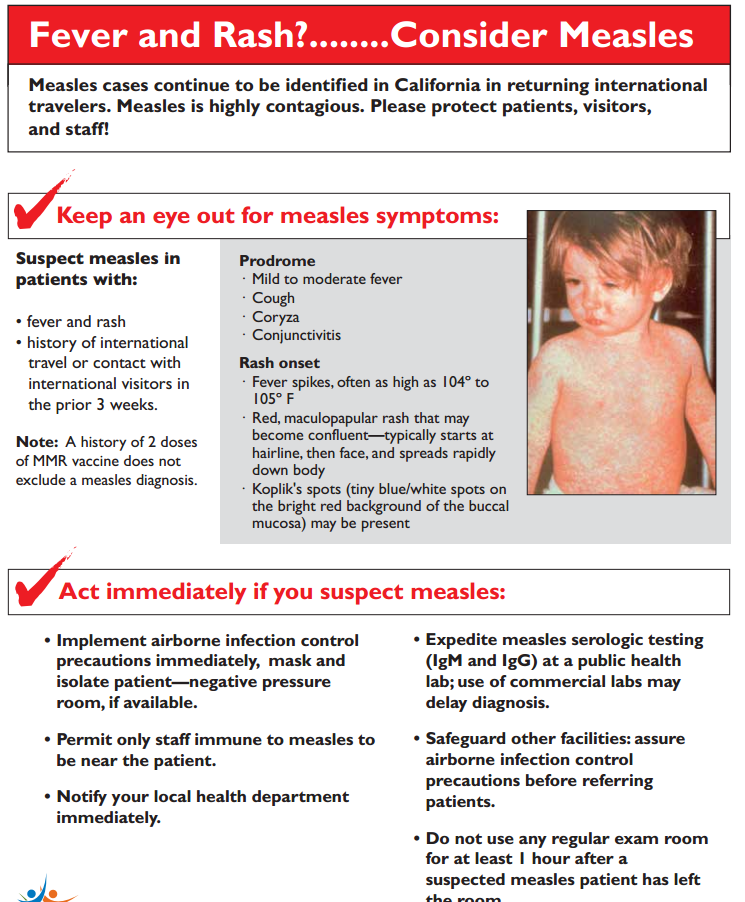 HFMD commonly causes blisters or sores to appear in or around the mouth or on the hands or feet. The rash may be seen in one or more of these locations.
HFMD commonly causes blisters or sores to appear in or around the mouth or on the hands or feet. The rash may be seen in one or more of these locations.
The rash looks like red blisters or bumps. As the disease progresses, the sores may crust over. The spots may be harder to identify on darker skin tones.
While it can occur in anyone, it’s more commonly seen in children under 5 years old.
Additional symptoms may include:
- fever
- decreased appetite
- general malaise
- drooling
- irritability
- sore throat
- headache
Because HFMD is a viral infection, there is no treatment. People typically recover within 7 to 10 days.
Talk with your baby’s pediatrician to determine if you can offer baby acetaminophen (Tylenol) to help make your child more comfortable while they recover. Your pediatrician may also recommend ibuprofen (Motrin) in babies 6 months and older.
A pediatrician may also be able to recommend over-the-counter or prescription topical ointments to help relieve pain from the sores.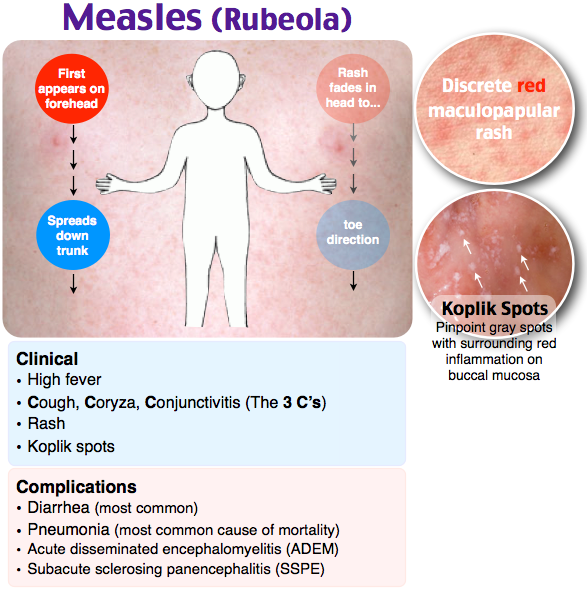
Limit acidic or spicy foods, such as citrus, as these can irritate the sores. Instead, offer cold foods, like popsicles, to help soothe sores in the mouth. It’s also important to keep your child isolated and out of care settings until the sores have healed. HFMD is extremely contagious.
These skin conditions are generally harmless and usually go away on their own with little or no treatment. You can help your baby avoid irritating the area by keeping their nails short and putting soft cotton gloves or socks on them at night.
If you’re concerned or feel that your child may require medical intervention, talk with their pediatrician.
Stork sting. What are newborn mothers afraid of? Society news
Any seemingly insignificant change in the baby's condition can frighten the newly-made mom and dad. Although sometimes nothing really bad happens. In the first month of life, neonatologists observe babies. It is on them that a flurry of parental fears falls.
“There is such a thing as a transient state of newborns.
This is an intermediate period between the time when the child was in the mother's womb and the time when he begins to settle down outside, says Lina Komisar . - When a woman who has given birth asks: “How is the baby?”, We answer: “He is in the period of adaptation.” A transient state is not a diagnosis, not a disease! This condition is also called borderline, since with defects in care or a breakdown in adaptation, it can turn into a pathological one. Therefore, neonatologists daily, and sometimes twice a day, examine children in the neonatal department.”
Body weight
“Sometimes mothers tell doctors: “My baby has lost weight. Probably because he didn't eat." But this happens not only for this reason. In the first three days, the child receives only a small amount of colostrum and, due to a lack of total fluid volume, loses weight.
In addition, at this time, the umbilical residue dries up and the original feces are excreted, due to which the baby also loses grams.
Lina Komisar / Photo: Natalia Malyihina
Read also 17 Aug 2022 11:08
Small does not mean sick. Does the weight of a newborn affect its further development 28 May 2022 09:eleven
Doctors in Belgorod gave birth to two residents of the Kharkiv region 29 Mar 2022 10:52
2 boys and 1 girl were born on New Year's Eve in Belgorod 01 Jan 2022 10:49
Since the beginning of the year, the 2021st baby was born in the Belgorod region 05 Mar 2021 17:04
The maximum loss occurs before the third or fourth day.
If a child was born weighing 3 kg, then he can lose up to 300 g. Such a loss is not a contraindication for discharge from the hospital. Everything will be restored.
From the fourth day, a gradual increase begins. The mother receives more milk, the child becomes more active, sleeps less and adds 10–50 g daily.”
"It was scary. I prayed." Moms - about the first days of life of children born prematurely
Jaundice
“I can say right away that if a child develops jaundice, this is not a consequence of hepatitis B vaccination, as some parents believe.
There is a special kind of jaundice that occurs only in newborns.
Pathological jaundice occurs with Rh conflicts, liver dysfunction, infections and other abnormalities. It is very rare.
Physiological jaundice begins due to the difference between the hemoglobin of the fetus and the child who has already been born.
In a newborn, fetal hemoglobin breaks down, transforming, among other things, into bilirubin. But due to the fact that the baby's liver is immature (this organ is formed before the age of five), it does not have time to utilize this bilirubin. Here the child turns yellow. If certain indicators are not exceeded, this condition does not require special treatment. Bilirubin will be excreted naturally.
One child may turn yellow on the second day, the other on the fifth. Jaundice disappears from the beginning of the second to the end of the third week, sometimes it can last up to a month.
Hyperthermia
“It happens that the baby turns red, screams, and the mother cannot calm him down. This is due to the immature nervous system and thermoregulation center. Roughly speaking, babies accept the temperature of the environment: they dressed warmly - overheated, opened - cooled down.
If the child's temperature is above 37.5°, you need to untie him and bathe him, remove the diaper and just keep him in a thin diaper.
And everything will pass. Antipyretics are prescribed only in very rare cases.
Photo: pixabay.com
Sexual crisis
“On the third or fourth day, the external genitalia of girls increase, the scrotum of boys swells. In children, the mammary glands may increase, there will be discharge from them. Girls can also have false periods, which is especially frightening for mothers. This is not scary, because every child receives a lot of hormones during pregnancy and childbirth. Everything will go by itself."
Physiological dysbacteriosis
“Mother calls me to the ward with the words: “My child has diarrhea, what should I do? This is probably because of the antibiotics that they inject me!” No, it's not because of the antibiotics. This is a transition chair.
The baby is born with sterile intestines. During the first day of life, after being applied to the mother's breast, it is populated by the maternal microflora.
The sterile intestine reacts to lacto- and bifidobacteria. It's not a disease."
Skin problems
“Most of the time mothers ask why the baby is so red. So, red is the physiological color of the skin in the first three days. The protective lubricant was removed from the baby, and his skin is thin, and the capillaries are close. In fact, it is very good that the baby is red, and not some other color.
It happens that a child has white pimples on his nose, chin and cheeks. Some mothers are very worried when they are discharged: “God, I have a photo session, what should I do?! Why is he so ugly!” Don't worry, you have a beautiful baby! He just has thin skin and no subcutaneous fat layer. In the area of the face, he has clogged immature sebaceous glands. Nothing needs to be done about it.
Some babies have red spots on the forehead, eyelids and back of the head. People say that redness in front is the kiss of an angel, and behind it is the bite of a stork, that is, the bird took the baby by the neck and carried it to the parents.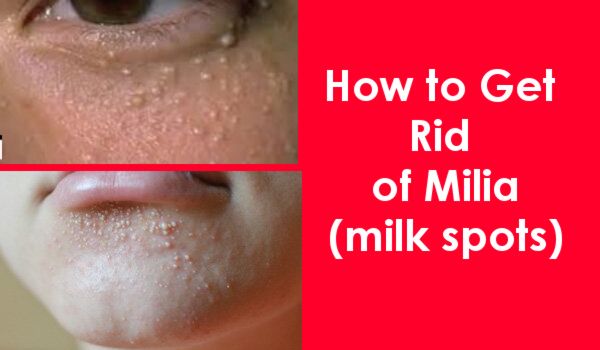 They also say that these are birthmarks, but this is not so. These are pathologically dilated capillaries. Up to a year they will pass, but they will appear in the heat, with screaming and crying. All of these are not diagnoses either.”
They also say that these are birthmarks, but this is not so. These are pathologically dilated capillaries. Up to a year they will pass, but they will appear in the heat, with screaming and crying. All of these are not diagnoses either.”
Photo: pixabay.com
Toxic erythema
“If the baby is covered with pimples, most likely it is toxic erythema - a transitional skin condition. It can be caused by toxicosis in the mother, disorders of the endocrine system, the mother taking certain drugs, heredity.
The rash resolves on its own. It has a migratory character: it disappeared on the arm, appeared on the leg. You just need to keep the baby dry and not overheat it.”
Urinary crisis
“It happens that on the first day the baby does not pee. This is fine. He can urinate at the end of the first day or on the second day. In the first three days, he will go to the toilet a little, but then the diapers will be wet four to six times a day.
And if you see something red in a diaper, don't be afraid that it's blood. This is a consequence of uric acid diathesis. The kidneys began to work actively, so salts of uric acid are released. Boys before urination may cry for the first three days, as the grains have a painful effect on the urethra.
Photo: Pixabay.com
News BRF
Red Pimples on the face of a newborn: Symptoms, causes and treatment
Allergic rash in the newborn
In the baby is an unfavorable Immunity response of the child organism 9000 potentially dangerous substance. Most often, an allergic rash occurs against the background of the use by a nursing mother of products that can act as an irritant. This group includes:
- cow's milk;
- soy [1] and egg white;
- fish;
- strawberries;
- nuts.
The first sign of developing allergic rash is peeling. Pathological foci with dry skin on the face of a newborn are formed symmetrically, localized on the cheeks and on the forehead.
Pathological foci with dry skin on the face of a newborn are formed symmetrically, localized on the cheeks and on the forehead.
It is necessary to consult a doctor if the appearance of rashes affects the general condition of the baby. Irritability, restless sleep, disorders of the gastrointestinal tract, fever and vomiting are dangerous symptoms that should be stopped immediately under the supervision of a pediatrician.
Neonatal acne
Neonatal acne may appear in the first weeks of a child's life in the forehead, nose and cheeks. In appearance, they resemble acne with purulent heads, characteristic of a teenage rash. It is assumed that the cause of the appearance of acne is increased production of sebum , which clogs the ducts of the sebaceous glands and provokes an inflammatory reaction.
The pathogenesis of the appearance of small pimples in newborns is also associated with the processes of the formation of the hormonal system.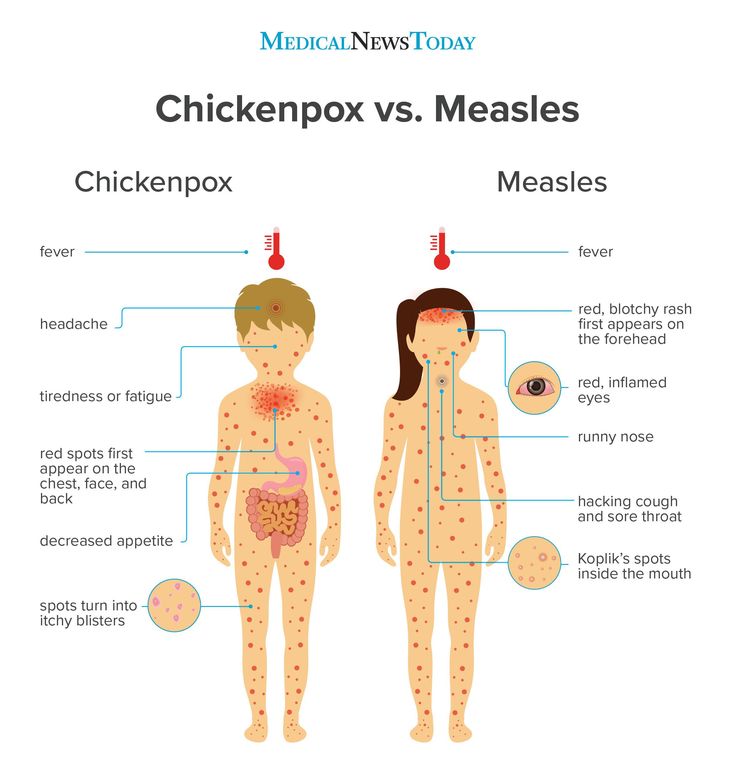 The body gets rid of the transplacental influence of maternal androgens [2], adrenal hormones begin to be produced more intensively, which affect the condition of the skin.
The body gets rid of the transplacental influence of maternal androgens [2], adrenal hormones begin to be produced more intensively, which affect the condition of the skin.
Neonatal acne does not require treatment [9] - standard daily care using delicate soap or baby cosmetics is sufficient. In most cases, pimples that appear on the face go away on their own by 4 months of age.
Sweating
Sweating is a skin lesion that is associated with hyperfunction of the sweat glands and irritation of the excretory ducts . The disease can develop due to improper skin care newborn, with a long stay in hot rooms and the wrong choice of clothing (the child is heavily wrapped up).
Miliaria resembles an allergic rash, but differs from it in localization. Signs of allergy most often appear on the skin of the child's face, and with miliaria, rashes form throughout the body - most often in natural folds, on the neck, lower abdomen and upper chest.
What prickly heat looks like:
- small blisters with clear contents, prone to burning and itching;
- in difficult cases, reddish nodules with an inflamed rim;
- with extensive skin lesions - weeping areas.
Prickly heat by itself is not dangerous to the health of the child. But damage to the skin is fraught with the addition of a bacterial or fungal infection. In this case, purulent processes develop, the skin becomes edematous, a putrid odor appears. Red pimples with prickly heat cause discomfort in the child - he becomes capricious and irritable, refuses to eat and sleeps poorly.
Seborrheic dermatitis
In addition to red pimples, yellowish scales may appear on the skin of a newborn. These are signs of seborrheic dermatitis, a disease associated with increased secretion of sebum. Scales are formed in the first month of life in areas of the body with a large accumulation of sebaceous glands - on the scalp, upper third of the back, on the face, chest and in the area of the auricles. Seborrheic dermatitis is sometimes called "milky crusts", which may be associated with the use of unsuitable cosmetic products for baby skin care.
Seborrheic dermatitis is sometimes called "milky crusts", which may be associated with the use of unsuitable cosmetic products for baby skin care.
In fact, the disease is caused by high blood levels of maternal hormones or changes in the biochemical composition of lipids on the surface of the skin [4].
Most childhood seborrheic dermatitis resolves on its own. Parents need only take care of proper care , but diligently remove the crusts is not recommended - you risk damaging delicate skin and causing infection. It is better to use specially designed products - such as Shampoo-foam from "milk crusts" for newborns. He facilitates the removal of scales in 90% of cases and soothes the scalp in 95% of babies [5.2]. The product contains 99% ingredients of natural origin. The shampoo is fragrance-free and has a tear-free formula.
In the presence of thick, dense scales, which are located not only on the scalp, but also in other areas, a good helper will be Cream for "milk crusts" which helps to completely remove "milk crusts" in an average of 7 days [5. 3].
3].
Atopic dermatitis
Atopic dermatitis is an allergic disease that is accompanied by chronic inflammation of the skin. Causes of an uncontrolled allergic reaction in infants are:
- food allergens - animal protein, soy products, certain types of vegetables;
- airborne allergens - household dust, pollen, pet hair, tobacco smoke, etc.;
- pathogenic microflora - fungi, viruses, bacteria.
Newborns are most often diagnosed with erythematous-squamous form of atopic dermatitis with signs of an acute inflammatory reaction:
- hyperemia of the skin;
- peeling;
- flat small papules.
Red spots are localized on the arms and legs in the area of the folds , on the sides of the neck, on the back of the hands and on the cheeks.
Children with atopic dermatitis are advised to regularly cleanse and moisturize their skin [6]. Anti-inflammatory drugs are prescribed only for extensive skin lesions that impair the quality of life of the baby - in this case, you should contact your pediatrician.
Anti-inflammatory drugs are prescribed only for extensive skin lesions that impair the quality of life of the baby - in this case, you should contact your pediatrician.
For daily care it is recommended to use STELATOPIA Emollient Cream . Studies [5.1] have shown that emollient:
- In 90% of cases reduces increased dryness of the skin [5.1] and reduces the likelihood of clinical signs of AD by 51% [10]
- Soothes itching in 91% of cases [5.1]
- Reduces inflammation after 32 hours [11]
Diaper dermatitis
This disease is better known as diaper rash and is accompanied by inflammation of the skin in the diaper area in infants. Rash appears as a result of prolonged body contact with wet diapers - the skin becomes excessively moist and defenseless against damaging factors (chemical, physical, infectious). The situation is aggravated by the simultaneous effect on the skin of children's feces that remain in a diaper or diaper.
The situation is aggravated by the simultaneous effect on the skin of children's feces that remain in a diaper or diaper.
Diaper dermatitis is not localized on the face - pimples in newborns appear on the lower abdomen, on the convex surfaces of the thighs and buttocks.
For non-drug treatment of pathology, air baths [7], bathing in a decoction of string and celandine [8], and thorough hygiene procedures are indicated. For the prevention of diaper dermatitis and redness, it is recommended to use Diaper Cream 1 2 3.
Useful properties of the product:
- reduces redness and irritation by 80% from the first application [5];
- does not interfere with skin breathing;
- reduces the risk of exacerbations by 74% [5];
- protects, repairs and soothes inflamed skin.
A number of dermatological diseases of newborns develop as a result of improper care, so parents should pay special attention to children's hygiene, and if the baby's condition worsens, immediately consult a doctor.
____________________________________________________________________________________________
References:
1. Bhatia J, Greer F, for the Committee on Nutrition of the American Academy of Pediatrics. The use of mixtures based on soy protein in infant feeding.// Pediatrics, 2008; 121:1062–1068.
2. Herani M.I., Ando I. Acne in infancy and acne genetics // Dermatology 2003. Volume 206. Number 1. pp. 24-28. DOI: 10.1159/000067819
3. Zanko NI Efficiency of new technologies for skin care in young children: Ph.D. dis. ... cand. honey. Sciences, M., 2000
4. Naldi L., Rebora A. Clinical practice. Seborrheic dermatitis.
N Engle Gee Med. 360(4):387-96 (2009 January).
5. Results of the study 1035 F4.
5.1 Test results 1016F10.01.02
5.2 Test results 1008F4.01.16
5.3 Results of the study 1042F3.01.24
6. Thompson M., Hanifin J. Effective treatment of atopic dermatitis in children alleviates problems associated with food allergies
// GM Akad Dermatol.