Pregnancy headache location
Headaches during pregnancy | Pregnancy Birth and Baby
Headaches during pregnancy | Pregnancy Birth and Baby beginning of content9-minute read
Listen
If you have a severe headache during pregnancy that is not usual for you, seek medical help immediately.
Key facts
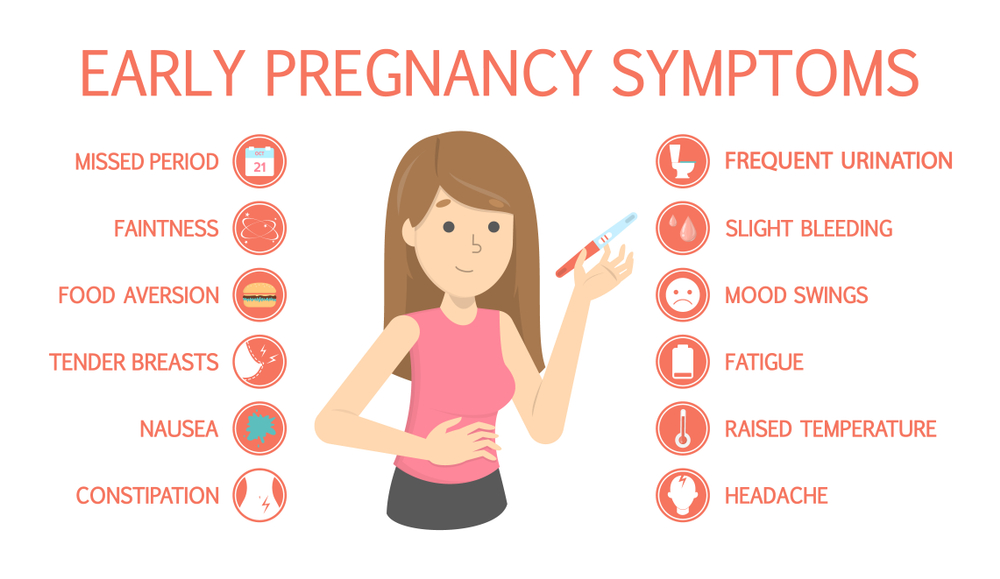
- It’s common to get mild headaches in the first few months of pregnancy because of hormonal changes.
- If you usually suffer from migraines, they may get better, worse, change or stay the same when you’re pregnant.
- Headaches during pregnancy may be triggered by poor sleep, stress, dehydration, low blood sugar or eye strain.
- If your headache doesn’t settle with simple measures (for example, rest and rehydration), you can take paracetamol.
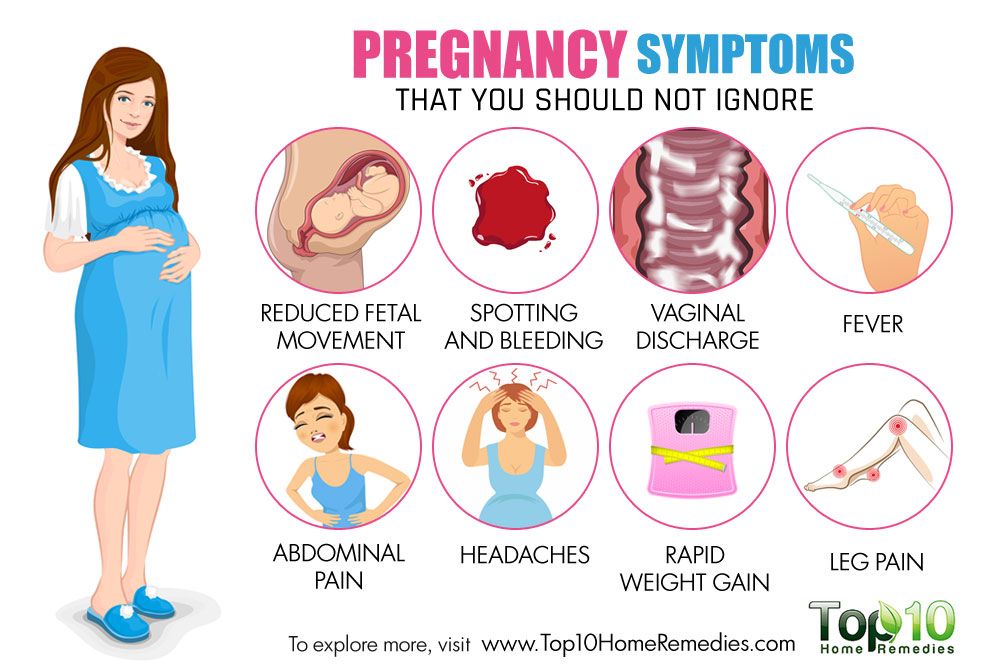
- A headache after 20 weeks can be a sign of pre-eclampsia, which is a serious pregnancy condition that needs medical attention – see your doctor or midwife.
Does pregnancy cause headaches?
Many people get mild headaches when they are pregnant. Headaches can often be triggered by a change in hormones. They are more common in the first few months of pregnancy.
If you usually suffer from migraines, you might notice a change when you’re pregnant. There’s a good chance that your migraines will improve after the first trimester. This may be because your oestrogen level starts to stabilise. However, some people don’t notice a change, or may get worse migraines during pregnancy. You also might notice different changes from one pregnancy to the next.
Headaches can develop for many different reasons — it’s not always because of pregnancy hormones.
Why else might I get headaches during pregnancy?
Besides hormonal changes, there are many triggers that cause headaches in general, but might occur more often when you’re pregnant, such as:
- not getting enough sleep
- withdrawal from caffeine — such as in coffee, tea or cola drinks
- low blood sugar from not eating regularly
- dehydration
- feeling stressed, anxious or depressed
- eye strain — especially as your eye muscles relax during pregnancy
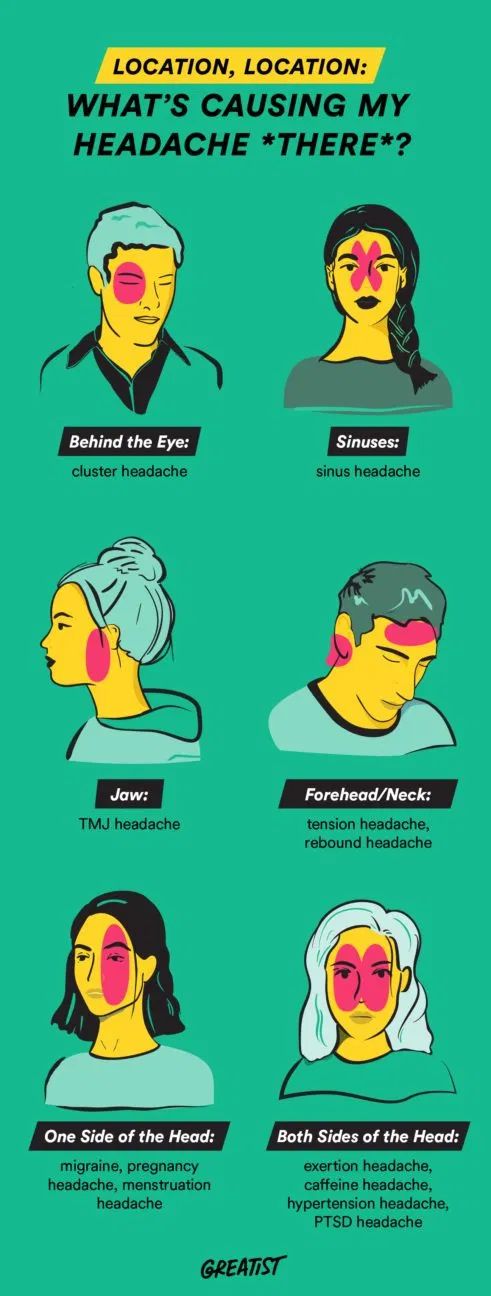
Many of these triggers can cause tension headaches, which are very common. The pain is usually mild and on both sides of your head.
The pain is usually mild and on both sides of your head.
Some of these triggers can cause migraines, which are more severe and mostly occur on one side of your head. If you have migraines, you might also feel sick or vomit and be sensitive to light or sound.
Pre-eclampsia
If you start getting frequent headaches after 20 weeks of pregnancy, this could be a sign of a more serious pregnancy condition called pre-eclampsia. Pre-eclampsia is when you have high blood pressure that affects your kidneys and sometimes other parts of your body. If you have a pre-eclampsia headache, you may find that simple pain-relieving medicines like paracetamol don’t help.
It’s very important to tell your doctor or midwife if you are getting headaches in the second half of pregnancy, or if your headaches are very severe.
If you have a severe headache during pregnancy, call your doctor or midwife. It could be something more serious.
Health conditions
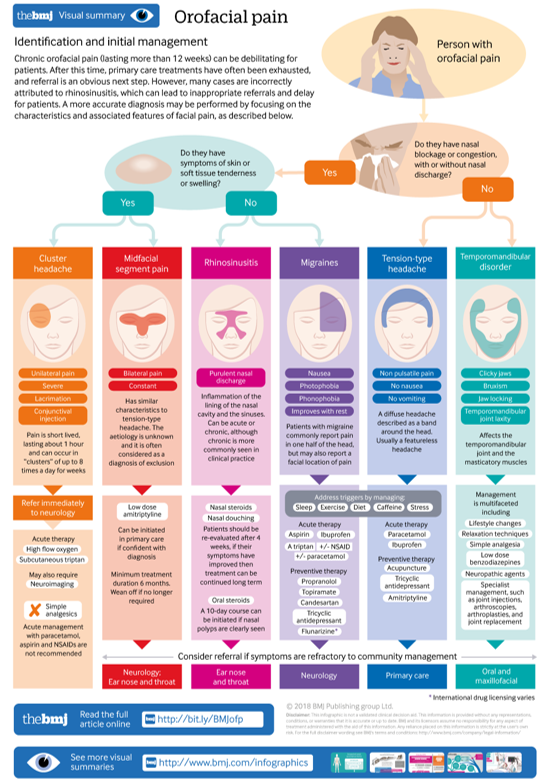
Just like when you’re not pregnant, a headache can sometimes be a sign of other health conditions, including:
- infections, such as an ear infection or flu
- sinusitis
- problems with your teeth
- an aneurysm or stroke
What can I do to treat a headache when I’m pregnant?
If you have a headache, you could try:
- having a nap, or resting with your eyes closed
- drinking water
- having something to eat
- putting a cold or heat pack on your forehead or the back of your neck
- asking someone to give you a gentle neck massage
If you need to take medicine for pain relief, paracetamol is safe during pregnancy.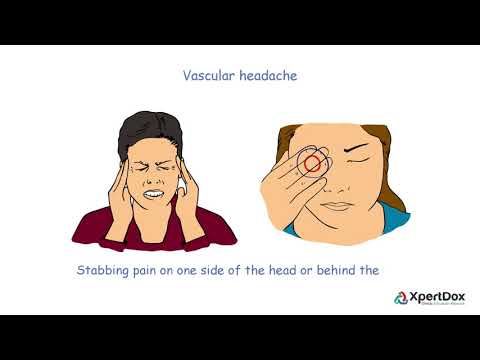 Pain-relieving medicines can actually cause headaches if you take them too often, so don’t take paracetamol more than 3 times a week.
Pain-relieving medicines can actually cause headaches if you take them too often, so don’t take paracetamol more than 3 times a week.
When you’re pregnant, avoid anti-inflammatories such as ibuprofen or aspirin and medicines that contain caffeine.
What can I do to prevent headaches during pregnancy?
If you find you are getting mild headaches often, it’s a good idea to:
- getting more sleep
- drink at least 8 cups of water a day
- go to pregnancy yoga classes or do some other type of exercise
- learn relaxation or stress management techniques
- don't go more than 4 hours without eating
- avoid processed foods
- see an optometrist for an eye check
What can I do if I suffer from migraines during pregnancy?
If you suffer from migraines, try to avoid things that may trigger migraines for you. People have different triggers for migraines, so it’s important to learn what your personal triggers are. Keep a headache diary, and see if your triggers include:
Keep a headache diary, and see if your triggers include:
- specific foods such as chocolate, or food additives such as caffeine or MSG
- bright or flickering lights, strong smells and loud sounds
- not enough sleep, or too much sleep
- skipping meals
- computer or movie screens
- strenuous exercise
- emotional triggers such as arguments or stress
Check with your doctor, pharmacist or midwife before you take a medicine for your migraine, to make sure it’s safe during pregnancy.
Paracetamol is the safest option for pain relief. If paracetamol doesn’t help and you need something stronger, ask your doctor about if you can take codeine. Try not to take codeine often, as you could become dependent on it and your baby could have withdrawal symptoms after they are born.
Most triptans (migraine medicines) are not considered safe in pregnancy. If you don’t get relief from paracetamol and codeine, you may be able to take sumatriptan occasionally. This medicine is available from a pharmacist and requires a prescription. Speak with your doctor or pharmacist before using it to help you understand the risks and the benefits of this medicine during pregnancy.
This medicine is available from a pharmacist and requires a prescription. Speak with your doctor or pharmacist before using it to help you understand the risks and the benefits of this medicine during pregnancy.
You can take metoclopramide if you suffer from nausea or vomiting with migraines.
Acupuncture can help treat migraines. Talk to your doctor or midwife first to check it’s safe for you. Make sure to tell your acupuncturist that you’re pregnant, so they can avoid certain points that shouldn’t be used in pregnancy.
When should I see a doctor?
See your doctor or midwife if you have symptoms of pre-eclampsia, including:
- a headache that doesn’t get better with paracetamol
- severe pain below your ribs
- heartburn that doesn’t disappear after taking antacids
- sudden swelling in your face, hands or feet
- blurred vision
Headaches can sometimes be a sign of other serious health conditions. Contact your doctor straightaway if you have:
- a sudden severe headache
- a change in your usual headaches
- your first-ever migraine
- a headache together with fever, neck stiffness, sensitivity of your eyes to light, drowsiness or weakness of your arm or leg
- a recent head injury
CHECK YOUR SYMPTOMS — If you are feeling unwell and not sure what to do next, check your symptoms using the healthdirect Symptom Checker tool.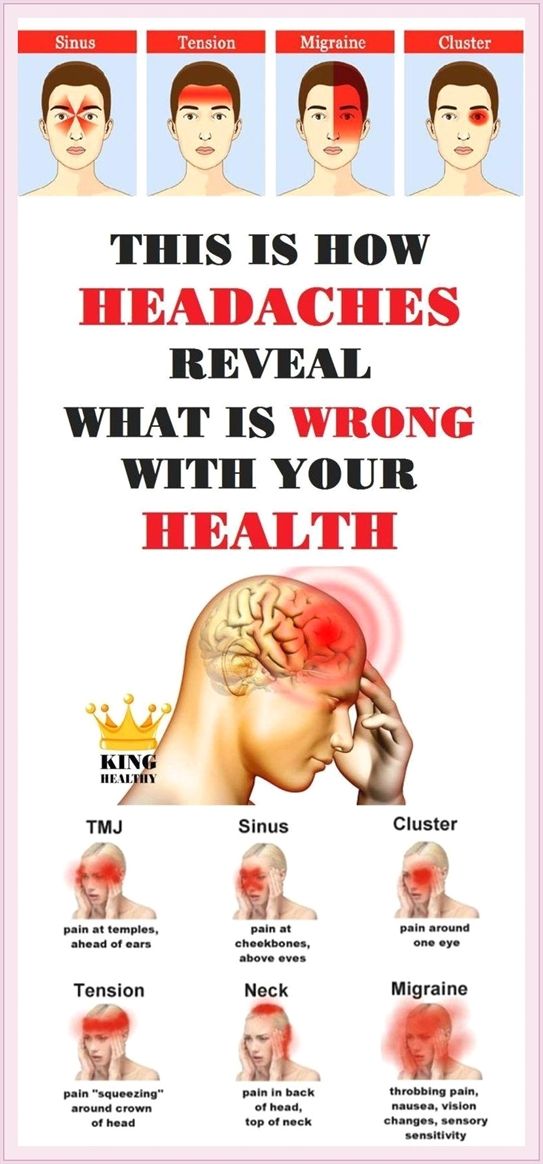
- Speak with your doctor or midwife, particularly if you have any concerns about pre-eclampsia.
- For more information about headaches, visit Migraine and Headache Australia.
- For more information about medicines you can take during pregnancy, talk to your doctor or pharmacist.
Speak to a maternal child health nurse
Call Pregnancy, Birth and Baby to speak to a maternal child health nurse on 1800 882 436 or video call. Available 7am to midnight (AET), 7 days a week.
Sources:
Tommy’s (Headaches in pregnancy – should I be worried?), NSW Government (Having a baby), Migraine & Headache Australia (Adults and headache), Migraine & Headache Australia (Migraine), Migraine & Headache Australia (Headache triggers), Migraine & Headache Australia (Headache treatment – no absolute cure), Migraine & Headache Australia (What is headache?), Migraine & Headache Australia (Tension headache), RANZCOG (Pre-eclampsia and high blood pressure in pregnancy), Royal Women's Hospital (Medicines in pregnancy), NSW Health (Migraine in pregnancy and breastfeeding), RANZCOG (Q&A: severe headache in the third trimester), Migraine & Headache Australia (Self-Care & Trigger Management)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: September 2022
Back To Top
Related pages
- Common discomforts during pregnancy
Need more information?
Common discomforts during pregnancy
Your body has a great deal to do during pregnancy. Sometimes the changes taking place will cause irritation or discomfort, and on occasions they may seem quite alarming.
Read more on Pregnancy, Birth & Baby website
Treatment of Headache - Migraine & Headache Australia
There is no absolute cure for headache, but many effective treatments exist which can prevent and treat different headache types.
Read more on Migraine and Headache Australia website
Taking medicines in pregnancy - NPS MedicineWise
If you are thinking of taking a medicine while you’re pregnant, take your doctor's advice and consider the risks and benefits.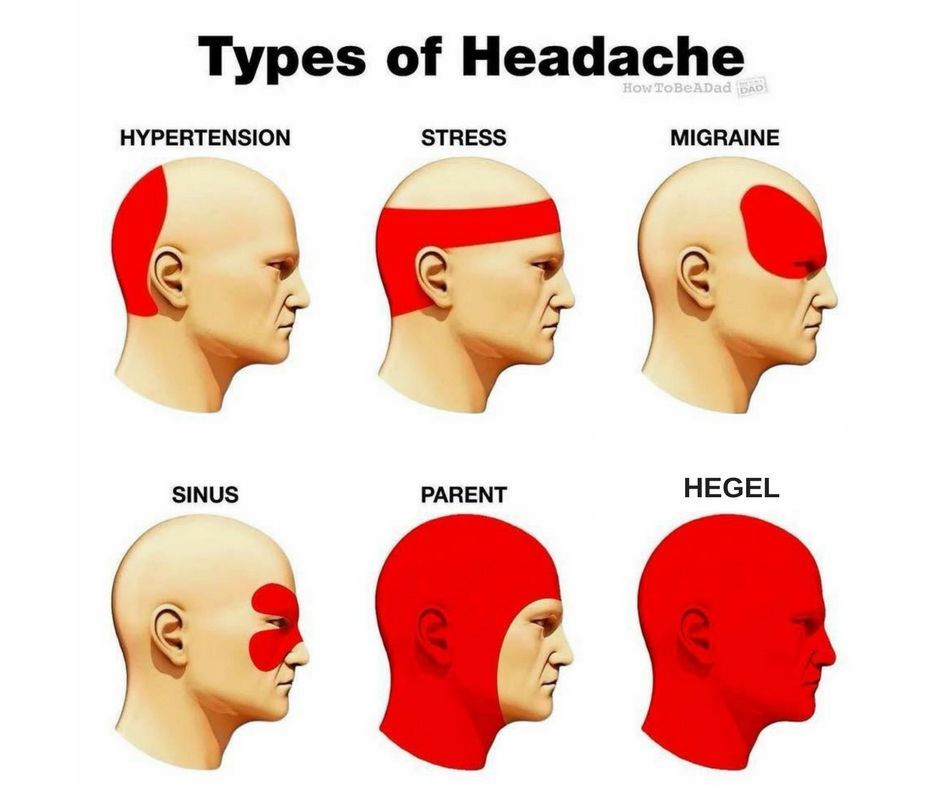
Read more on NPS MedicineWise website
Adults and Headache - Headache Australia
Studies confirm that tension-type headache and migraine are more common in women while cluster headache, a rare form of headache, is more common in men.
Read more on Migraine and Headache Australia website
Tension-type Headache - Migraine & Headache Australia
Tension-type headache is one of the most common everyday headaches. It causes a dull, non-throbbing pain and can be caused by stress.
Read more on Migraine and Headache Australia website
Migraine Management Tips - Headache Australia
It’s important to be organized and informed about your migraine attacks and how they impact your life. Here are some migraine management tips to assist.
Here are some migraine management tips to assist.
Read more on Migraine and Headache Australia website
Six ways to manage migraine without drugs | The George Institute for Global Health
We’ve all heard of the crushing headache pain that comes with migraine but did you know that one in every seven people experience them, three in every four people with migraine are females, and migraine is the number one cause of disability in young people? With so many people affected worldwide, you’d think modern medicine would have developed a solution by now but unfortunately there’s still no definite cure for migraine.
Read more on The George Institute for Global Health website
Mumps and pregnancy
Find out about mumps and its symptoms, how it spreads, how to manage it at home, and how to avoid mumps if you’re planning a pregnancy.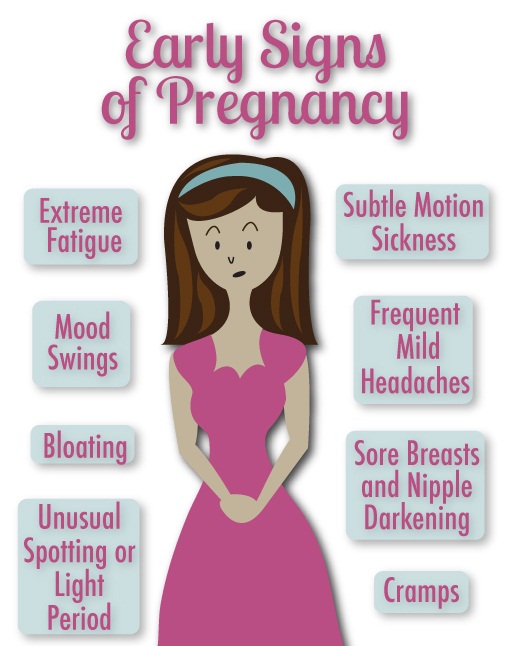
Read more on Pregnancy, Birth & Baby website
Stress and pregnancy
Stress is a normal response to major life changes but there are things you can do to reduce pregnancy-related stress. Learn more here about how it affects you.
Read more on Pregnancy, Birth & Baby website
Toxaemia of pregnancy (pre-eclampsia) - MyDr.com.au
Pre-eclampsia, also known as pre-eclamptic toxaemia, or just toxaemia, occurs in pregnancy, causing problems for the baby and mother.
Read more on myDr website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.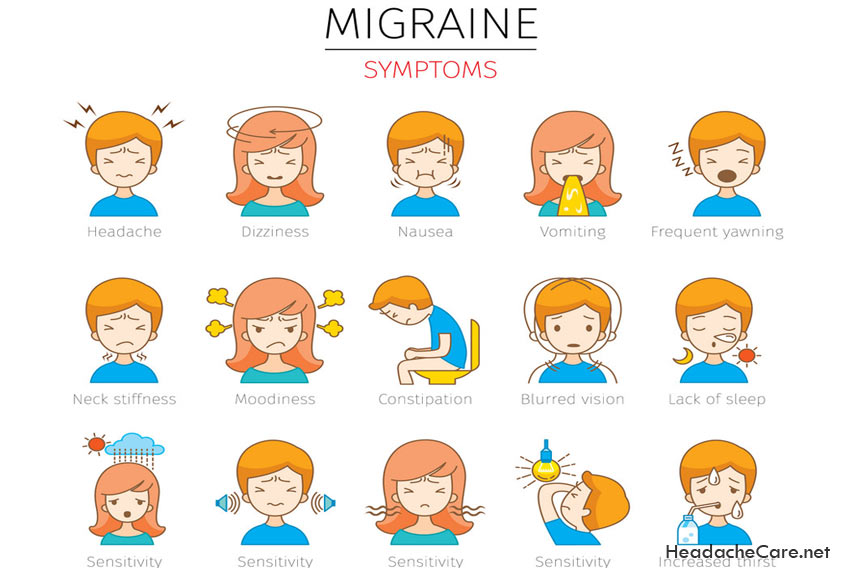
Need further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari.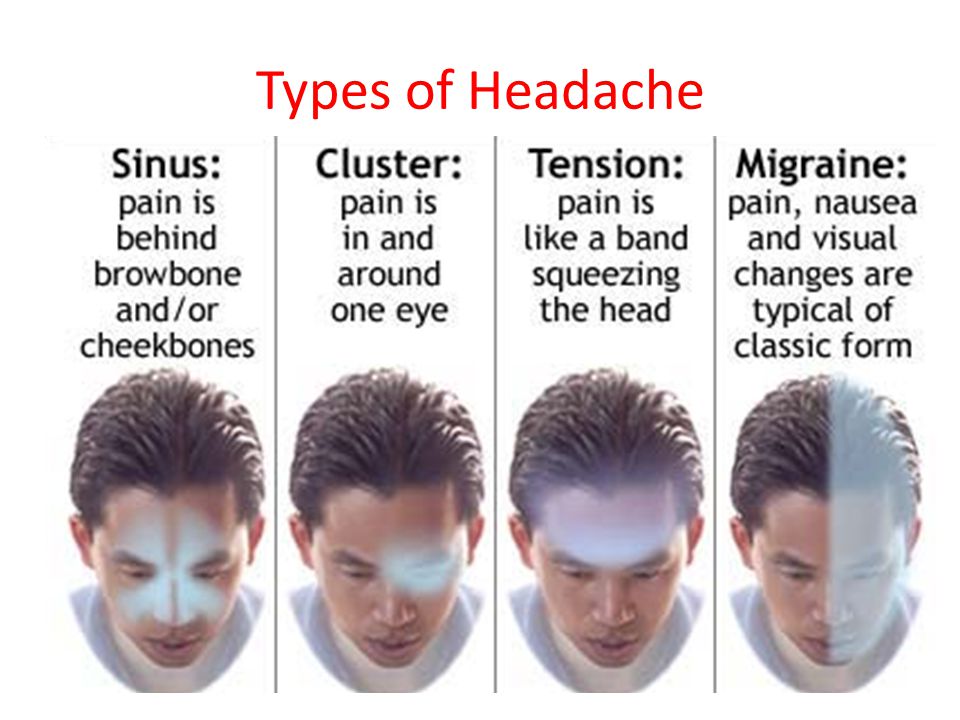 For more information, please visit the links below:
For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Pregnancy and Headaches: When Should I Worry?
Pregnancy is a beautiful thing to be celebrated, but few people fill you in on the not-so-great symptoms that may occur during the journey. Namely, heartburn, gas, constipation and, for some pregnant mamas, headaches.
While headaches can be just another normal symptom of pregnancy, should they ever be a cause for concern?
“Headaches are common in women both in and outside of pregnancy,” said Kelley Saunders, MD, an OBGYN with Banner – University Medicine Women’s Institute. “But whether they are normal or not should always be discussed with your doctor."
Here is some insight into what causes headaches during pregnancy, some remedies to treat them and why your doctor should be kept in the loop.
Is it a headache or something else?
It isn’t always easy to tell what kind of headache you’re having, but the most common types of headaches during pregnancy are tension-type headaches, migraines and cluster headaches.
Tension headaches are the most common kind of headache in pregnant women. It can feel like someone is trying to squish your head like a watermelon. If you carry your stress in your shoulders and neck, you may be more susceptible to this kind of headache.
Migraines are a particular type of headache that occur on one side of the head. For some women, migraines can get worse the first few months and then improve in later stages of pregnancy. For others, they may experience no change, decrease or difference in their migraines.
Cluster headaches are less common but can occur during pregnancy. You’ll suddenly have severe pain around your eyes or temples usually about the same time every day.
The good news is that there are plenty of pregnancy-safe things you can do to prevent and relieve the most common pregnancy headaches.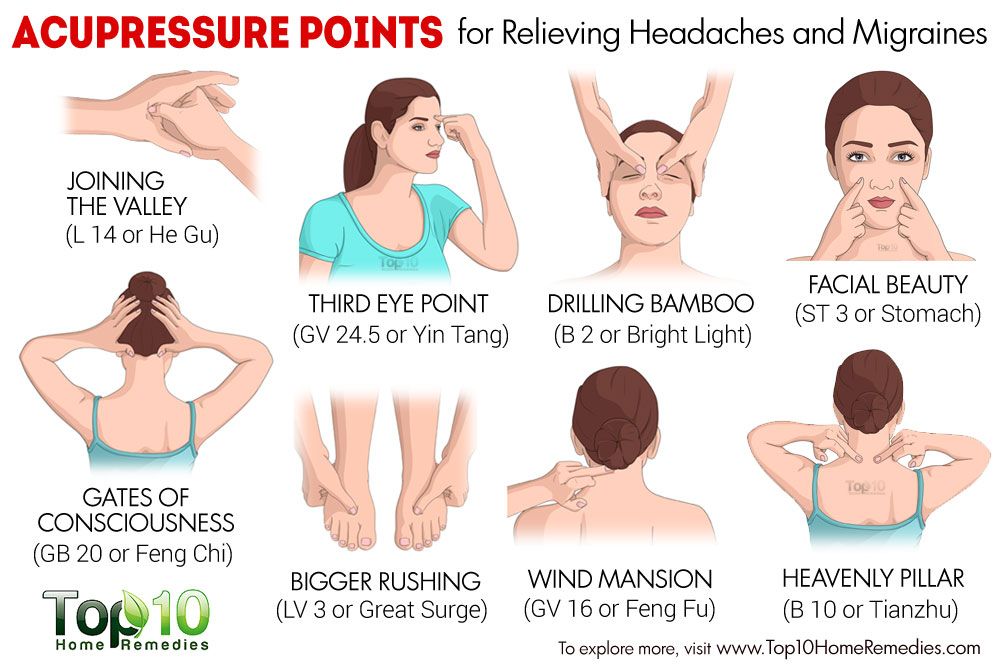
Tips for relieving mild headaches
- Get plenty of rest. Sleep is especially hard later in your pregnancy but is so important to physical and mental health. Find yourself a comfy prenatal pillow and snuggle away.
- Drink plenty of water. Pregnant moms require more water than the average person. While you may want to avoid extra trips to the bathroom, adequate fluid intake is important for you and baby.
- Eat regular, well-balanced meals. To prevent low blood sugar, eat small meals throughout the day. Avoid sugar, like soda and candy.
- Get a prenatal massage. A full-body massage can release tension in the muscles of your neck, shoulders and back.
- Use warm compresses on head, neck and shoulders.
- Avoid triggers. Keep a journal to help identify specific triggers so you can learn what to avoid. Some common headache triggers include strong odors and nitrites or nitrates.

- Try exercise and relaxation techniques. There’s evidence that regular exercise can reduce stress and boost overall mood. Check with your doctor first before starting any new fitness routines.
- Take acetaminophen to relieve symptoms (as approved by doctor).
- Take caffeine in doses less than 200mg in a day (as approved by doctor).
If you have a history of migraines, however, your doctor may treat them differently during pregnancy. Discuss with your doctor what medications are safe to take during pregnancy.
Is my headache a cause for concern?
Sometimes. Headaches tend to be more common in the first and third trimesters, but they can occur in the second trimester as well. While there are common causes for headaches during pregnancy, it’s important to note that headaches during the second and third trimester can also be due to high blood pressure, called preeclampsia.
“Preeclampsia is a pregnancy-related condition that requires prompt evaluation and management with an obstetrician or maternal fetal medicine specialist,” Dr.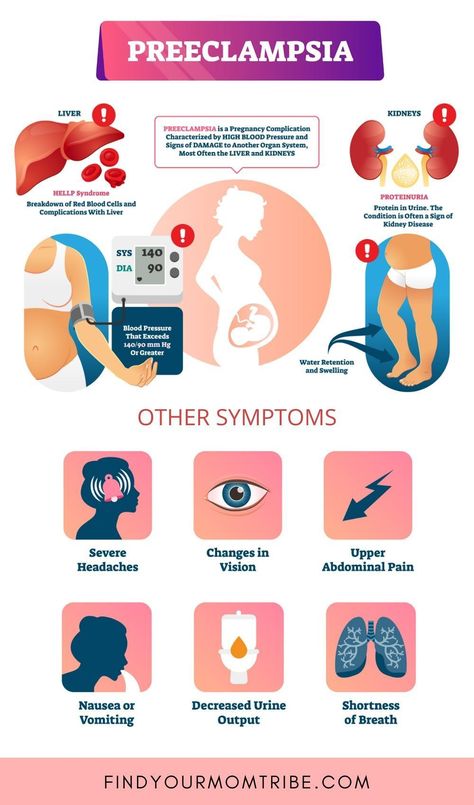 Saunders said. “Elevated blood pressure prior to pregnancy puts a woman at increased risk for preeclampsia.”
Saunders said. “Elevated blood pressure prior to pregnancy puts a woman at increased risk for preeclampsia.”
When should I call my doctor?
Whether you experience headaches or not, it’s always important to discuss your pre-pregnancy history, obstetrical history and concerns with your doctor for an individualized assessment and management plan. However, if none of the above treatments resolve your mild headache or your headaches become more frequent and severe, talk to your doctor to determine the cause.
“This includes new headaches that present after 20 weeks, a sudden onset of severe headaches, headaches associated with a fever, mental health changes, elevated blood pressure and vision changes,” Dr. Saunders said. “It’s important to keep an open line of communication with your physician and let them know about any changes in your health so they can rule out anything serious."
Got questions? We can help!
If a headache is keeping you up at night and your doctor isn’t available, call the Banner Nurse Now line, a free health care service that offers advice 24-hours a day, seven days a week. Call 844-259-9494.
Call 844-259-9494.
Check out other pregnancy articles on our Banner Health blog
Pregnancy is an exciting, but also a bit scary time (especially if this is your first baby). Here are some other reads to help guide you through the trimesters and welcoming baby:
- 5 Tips for Having a Happy, Healthy Pregnancy
- Expect the Unexpected: How Your Body Changes During Pregnancy
- What To Expect In The Second Trimester
- Understanding Pulmonary Embolism Risk During Pregnancy
Women's Health Pregnancy
Join the Conversation
a particular example of the course of the disease uMEDp
Migraine is one of the most common forms of headache. There is evidence for the role of magnesium deficiency in the pathogenesis of migraine. The disease most often occurs in women of reproductive age. The frequency of migraine attacks during pregnancy tends to decrease.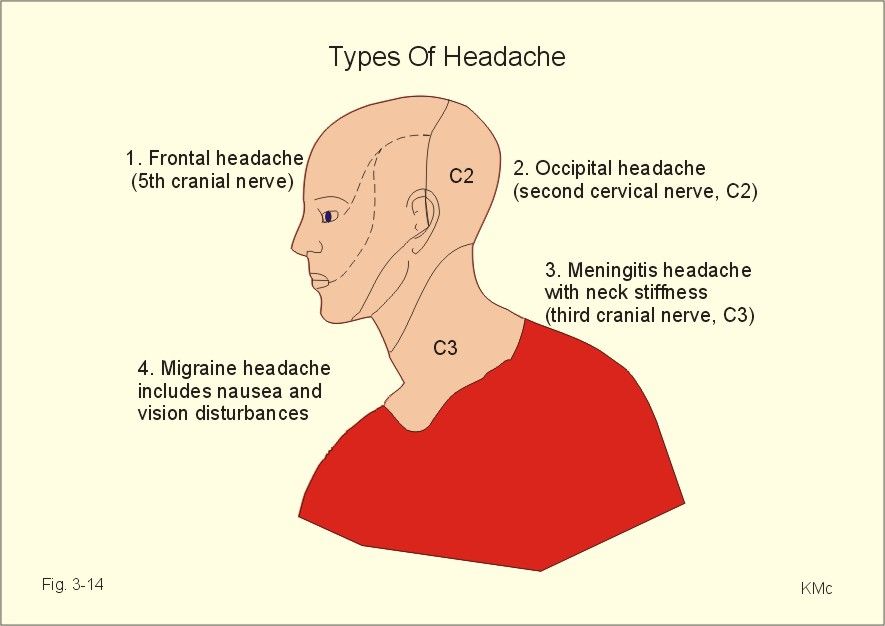 However, in cases where migraine attacks persist during pregnancy, difficulties arise in the selection of a drug. Magnesium preparations (Magnerot) are effective and safe drugs and can be recommended for prophylactic treatment of migraine in pregnant women.
However, in cases where migraine attacks persist during pregnancy, difficulties arise in the selection of a drug. Magnesium preparations (Magnerot) are effective and safe drugs and can be recommended for prophylactic treatment of migraine in pregnant women.
Migraine is the second most common form of primary headache after tension headache. Epidemiological studies have confirmed the high prevalence of migraine and its socio-economic significance, negative impact on the quality of life and performance [1].
Periodically recurring migraine headache attacks are pulsating, often unilateral in nature, accompanied by nausea, vomiting, photo and sound phobia. After an attack, drowsiness and lethargy are observed. Migraine is a chronic, heterogeneous disease. There are more than 15 subtypes of migraine, but in practice migraine with aura and without aura is usually distinguished [1]. The frequency, duration, and intensity of seizures vary greatly among patients. Each patient has their own specific precipitating factors.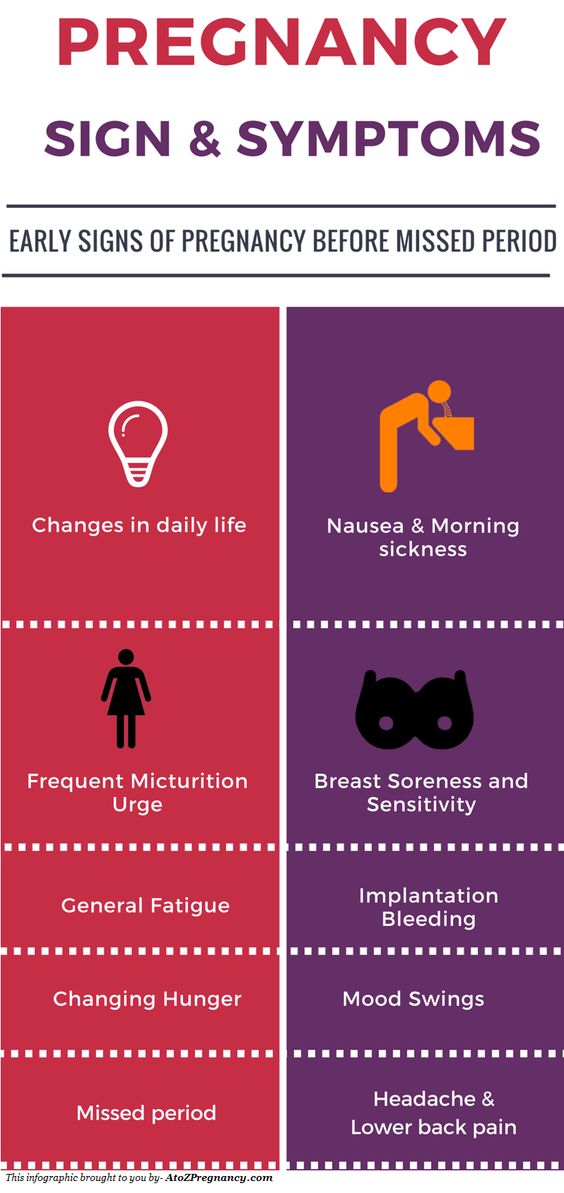 Young women suffer from migraine three times more often than men. A change in the hormonal status associated with menarche, pregnancy, lactation or menopause is accompanied by a change in the clinical course of the disease in them. Women note a clear relationship between headache attacks and the onset of menstruation [2]. During pregnancy, approximately 70% of women with migraine, mostly without aura, improve, the frequency of headache attacks decreases as the gestational age increases. However, in migraine with aura, the frequency and intensity of attacks persist throughout pregnancy [3]. In this case, it is necessary to exclude the secondary nature of migraine, in particular, an increase or decrease in blood pressure (BP), the development of venous vascular dyscirculation, intracranial hypertension, preeclampsia / eclampsia. It is also necessary to conduct a differential diagnosis of primary headaches according to international diagnostic criteria, to determine the subtype of migraine [1].
Young women suffer from migraine three times more often than men. A change in the hormonal status associated with menarche, pregnancy, lactation or menopause is accompanied by a change in the clinical course of the disease in them. Women note a clear relationship between headache attacks and the onset of menstruation [2]. During pregnancy, approximately 70% of women with migraine, mostly without aura, improve, the frequency of headache attacks decreases as the gestational age increases. However, in migraine with aura, the frequency and intensity of attacks persist throughout pregnancy [3]. In this case, it is necessary to exclude the secondary nature of migraine, in particular, an increase or decrease in blood pressure (BP), the development of venous vascular dyscirculation, intracranial hypertension, preeclampsia / eclampsia. It is also necessary to conduct a differential diagnosis of primary headaches according to international diagnostic criteria, to determine the subtype of migraine [1].
Tactics of migraine therapy in pregnant women in most cases does not differ from the traditional one and includes two directions - relief of a headache attack and prophylactic therapy for frequent (more than 2-3 per month) attacks. For mild or moderately intense migraine attacks, the drugs of choice are simple analgesics (paracetamol, ibuprofen), as well as their combination with caffeine. Given that during migraine attacks, many patients have pronounced atony of the stomach or intestines, which makes it difficult for the absorption of oral drugs, antiemetics (metoclopramide or domperidone) are added to therapy. For more severe migraine attacks, specific triptan preparations are used that effectively eliminate headaches. The most studied is sumatriptan, which can be used in pregnant women.
As a preventive therapy for migraine in pregnant women, the use of low doses of beta-blockers, tricyclic antidepressants, non-steroidal anti-inflammatory drugs, and magnesium preparations is recommended [4]. Most drugs for the treatment of migraine are allowed to be used during pregnancy, however, before prescribing a particular drug, it is necessary to take into account factors such as the form of migraine, its intensity, gestational age, fetal condition, concomitant extragenital diseases, the benefit-risk ratio of the intended therapy.
Most drugs for the treatment of migraine are allowed to be used during pregnancy, however, before prescribing a particular drug, it is necessary to take into account factors such as the form of migraine, its intensity, gestational age, fetal condition, concomitant extragenital diseases, the benefit-risk ratio of the intended therapy.
On the example of a clinical case, let us consider the features of the course of migraine in a pregnant woman and the tactics of its management in case of a change in the nature of cephalalgia.
Patient management
Patient V., 36 years old. She was under the supervision of an obstetrician-gynecologist in the antenatal clinic from 10 weeks of pregnancy. Married. Works as a nurse.
Second birth, third pregnancy. The first birth at the age of 24, during pregnancy was observed due to the threat of termination, blood pressure during pregnancy did not increase. Term delivery, newborn boy, weight 3050 g,
height 51 cm.
From the age of 18, the patient has been suffering from attacks of unilateral throbbing headache lasting up to 24 hours with nausea and photophobia. The frequency of migraine attacks before pregnancy is 1-2 times a month. The patient was seen by a neurologist for headache. Diagnosis of migraine without aura. The secondary nature of the headache was excluded. The headache was stopped by simple analgesics or passed after rest, sleep.
History of aggravated heredity - arterial hypertension (AH) in the father, migraine in the mother.
Smoker, has not smoked for the last 10 years.
A year before the expected pregnancy, she underwent a clinical, laboratory and instrumental examination at the place of residence, including an electrocardiographic study, 24-hour blood pressure monitoring (ABPM), electroencephalography, and ultrasound duplex scanning of the vessels of the main parts of the head. AH, vascular disease of the head were not detected, there was no pathology of the kidneys.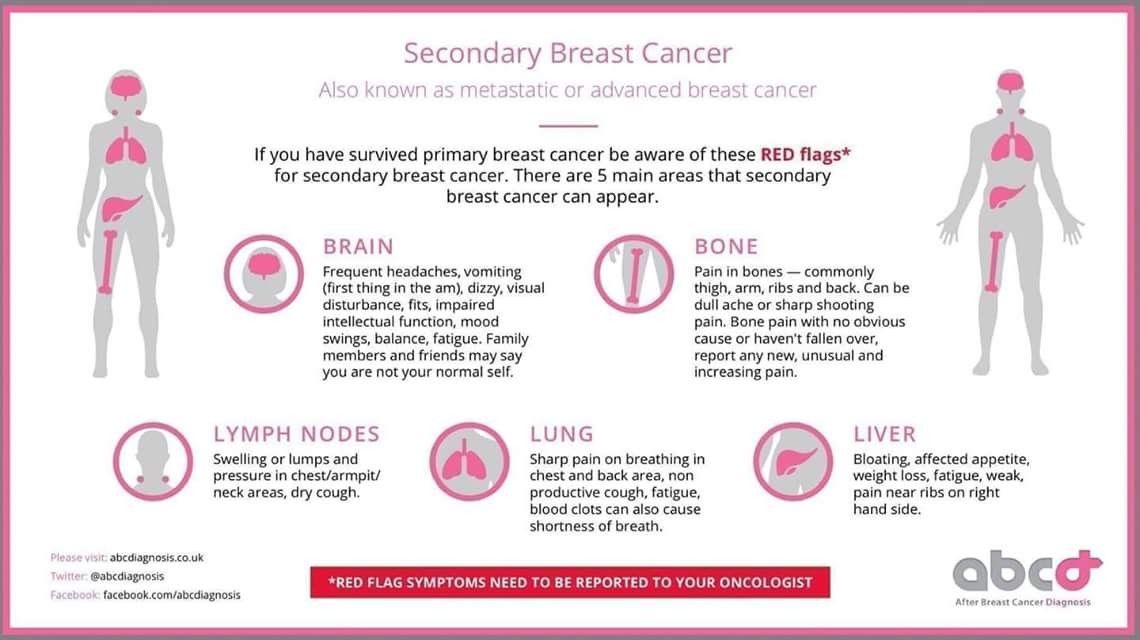
First examination: 12 weeks pregnant
Objectively: the condition is satisfactory. Height 158 cm, weight 70.3 kg (weight before pregnancy 67 kg, body mass index 26.8 kg / m², overweight). BP 110/60 mm Hg. Art. Heart rate (HR) 88 beats / min. No changes were found according to clinical blood and urine tests. Biochemical blood test: total cholesterol 3.8 mmol/l, glucose
3.86 mmol/l, uric acid 172 µmol/l. Coagulogram without deviations from the reference values.
Urinalysis: specific gravity 1012, protein negative, leukocytes 8–10 per field of view.
Electrocardiogram (ECG) - sinus rhythm, heart rate 80 bpm, vertical position of the electrical axis of the heart.
ABPM: daily average BP 110/65 mm Hg. Art., standard deviation from the mean value of blood pressure (standard deviation - STD)
14/9 mm Hg. Art.; day - BP 116/66 mm Hg. Art., STD 10/9 mm Hg. Art.; night - 94/53 mm Hg. Art., STD 10/8 mm Hg. Art.; SI (daily BP index) 18/9%, VI (time index) 0/0%.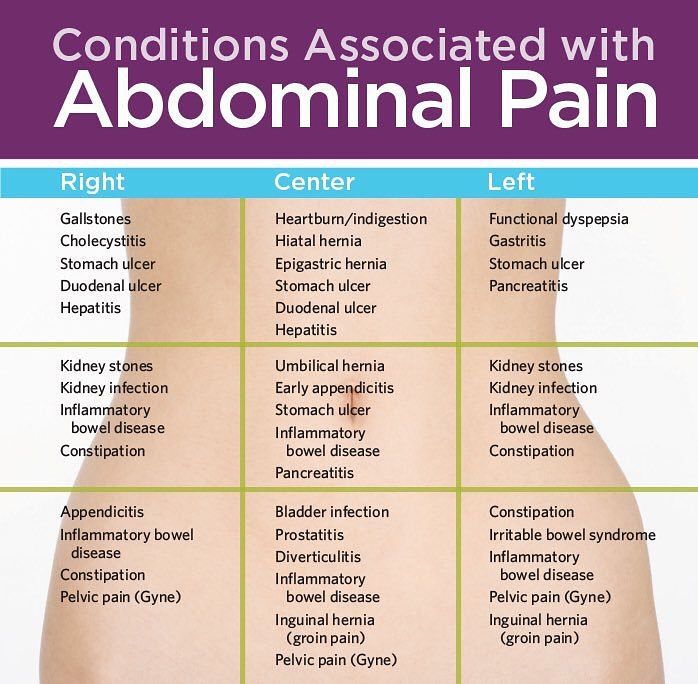 Conclusion: normal average daily blood pressure indicators are recorded, the circadian rhythm of blood pressure for diastolic blood pressure is disturbed - non-dipper, blood pressure variability is within the normal range.
Conclusion: normal average daily blood pressure indicators are recorded, the circadian rhythm of blood pressure for diastolic blood pressure is disturbed - non-dipper, blood pressure variability is within the normal range.
Echocardiography (EchoCG): morphofunctional parameters within the normal range: interventricular septal thickness (IVSD) - 0.83 cm, thickness of the posterior wall of the left ventricle (PVSLV) - 0.83 cm, end diastolic size (EDD) of the left ventricle - 4, 4 cm, end systolic size (SSR) of the left ventricle - 2.23 cm, ejection fraction (EF) - 65%, myocardial mass index (IMM) of the left ventricle - 74.7 g / m³, total peripheral vascular resistance (OPVR) -
1212 dyne x s x cm-5.
Due to a history of headaches, the patient was referred for a consultation with a neurologist. No focal symptoms were found in the neurological status. Diagnosis: migraine without aura. Due to rare migraine attacks, prophylactic therapy is not indicated. Relief of seizures with paracetamol in combination with caffeine.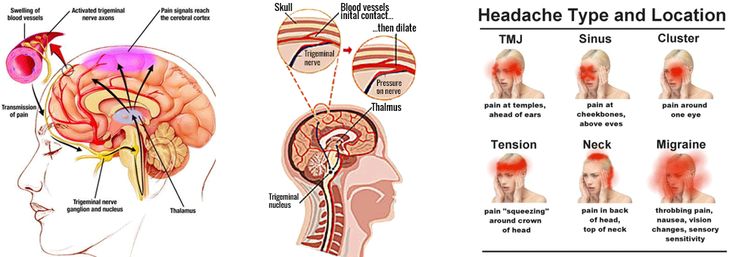
The patient is assigned to the high-risk group: age, complicated obstetric anamnesis, heredity burdened by hypertension, overweight, circadian rhythm disturbances in diastolic blood pressure.
Re-examination: pregnancy 20 weeks
No active complaints at the time of examination. He notes an increase in the frequency of headaches up to 2-3 times a week. The characteristic of cephalgia is the same.
Objectively: satisfactory condition, weight 73.1 kg, blood pressure 118/68 mm Hg. Art., heart rate 76 beats / min.
No abnormalities were found in general blood and urine tests. Biochemical blood test: total cholesterol 5.7 mmol/l, glucose 4.0 mmol/l, uric acid 256 µmol/l. The coagulogram corresponds to the reference values.
ECG - sinus rhythm, heart rate 80 bpm, vertical position of the electrical axis of the heart.
Echocardiography: TMZhP 0.8 cm, TLSLV 0.8 cm, EDR 4.8 cm, EFR 2.2 cm, EF 67%, IMM 79.1 g/m³, TPVR 1714 dyn × s × cm-5.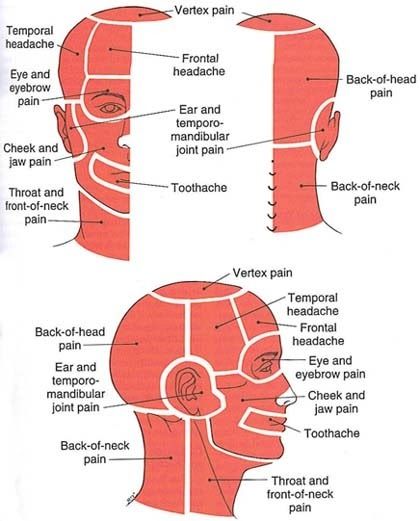
ABPM: daily average BP 111.7/66.5 mm Hg. Art., STD 15 / 9.6 mm Hg. Art.; day - BP 114.3 / 68.3 mm Hg. Art., STD 10.9 / 9.6 mm Hg. Art.; night - 103/62.1 mm Hg. Art., STD 11.3 / 9.1 mm Hg. Art.; SI 9.7/9.1%, CI 5/2%.
Conclusion: normal 24-hour BP levels are recorded, disturbed circadian BP rhythm with a decrease in day/night pressure drop of less than 10% - non-dipper, systolic 24-hour BP variability is increased. In comparison with the data of the previous study, there is an increase in the level of nocturnal blood pressure by 9/9 mmHg Art.
In neurological status without negative dynamics.
Despite the patient's satisfactory condition, the normal level of blood pressure, the absence of any laboratory markers of a complicated course of pregnancy, the trend towards an increase in TPVR and a change in the daily profile of blood pressure according to the non-dipper type, an increase in the frequency of cephalalgia, is of concern.
It is recommended to continue monitoring, re-examination every 14 days with an assessment of weight gain, measurement of blood pressure, urinalysis.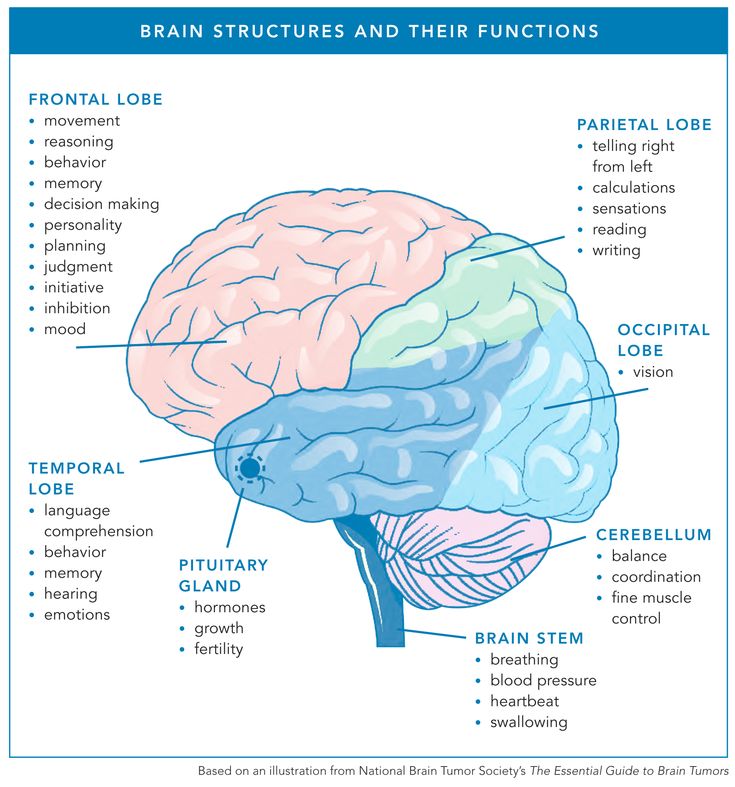 Magnesium preparations are recommended for a long time. Over the next 6 weeks, the patient took Magnerot 500 mg 3 times a day, noted an improvement in well-being. During the first 2 weeks of therapy, one mild attack of headache was noted, in the future, attacks of headache did not bother.
Magnesium preparations are recommended for a long time. Over the next 6 weeks, the patient took Magnerot 500 mg 3 times a day, noted an improvement in well-being. During the first 2 weeks of therapy, one mild attack of headache was noted, in the future, attacks of headache did not bother.
Pregnancy 32 weeks: hospitalization
At 32 weeks, during the next visit, the patient complained of a bilateral headache of a pressure-pulsating nature of the frontotemporal localization. The pain is most pronounced in the morning, decreases somewhat with the vertical position of the body, sleep is disturbed. Objectively: the condition is satisfactory, weight is 79.1 kg, blood pressure is 150/90 mm Hg. Art., heart rate 72 beats / min.
In the general analysis of urine: specific gravity 1014, traces of protein, leukocytes up to 10–12 per field of view. Complete blood count (30 weeks): hemoglobin 109g/l, hematocrit 34.1%, the number of erythrocytes, platelets are normal, there are no deviations in the leukocyte blood count, ESR 32 mm/h.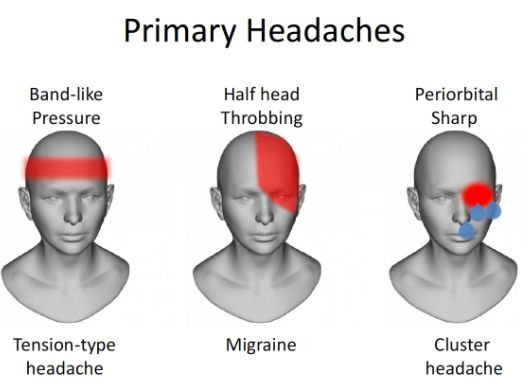 Biochemical blood test: total cholesterol 7.2 mmol/l, glucose 3.8 mmol/l , uric acid 286 µmol/l.
Biochemical blood test: total cholesterol 7.2 mmol/l, glucose 3.8 mmol/l , uric acid 286 µmol/l.
ECG - sinus rhythm, heart rate 76 beats/min, ventricular extrasystole was registered.
Ultrasound of the fetus: dimensions correspond to a period of 30 weeks, no signs of disturbance of the uteroplacental and fetoplacental blood flow were detected, the threat of termination of pregnancy.
Examination by a neurologist revealed no focal symptoms. Headache is most likely due to the manifestation of hypertensive syndrome.
Diagnosis: 32 weeks pregnant. Gestational arterial hypertension. Preeclampsia (PE)? The threat of abortion. Anemia.
Immediate hospitalization to the maternity hospital is recommended to clarify the diagnosis and conduct intensive drug treatment. Later, the patient developed PE: an increase in blood pressure up to 150/9 was recorded.0 mmHg Art., was determined protein in the urine more than 0.3 g / day. Therapy was carried out with antihypertensive drugs - Dopegyt 1500 mg / day, as well as magnesium therapy.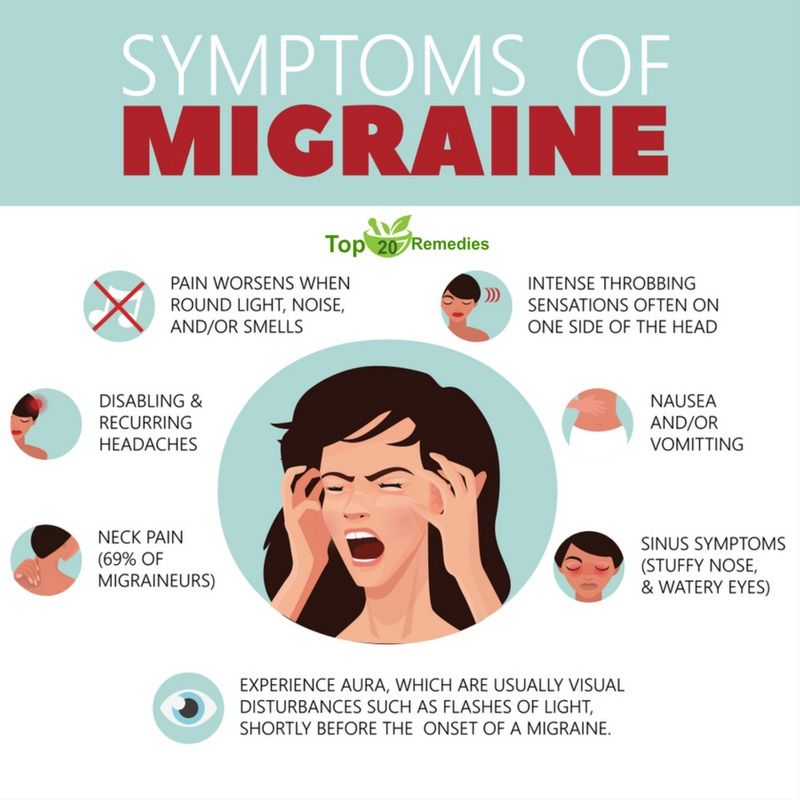 At 34 weeks, the patient had a premature birth, the newborn was a boy, weight 2600 g, height 49 cm with an Apgar score of 7.8 points at the 1st and 5th minutes, respectively.
At 34 weeks, the patient had a premature birth, the newborn was a boy, weight 2600 g, height 49 cm with an Apgar score of 7.8 points at the 1st and 5th minutes, respectively.
Summary: the development of PE in a pregnant woman with a burdened somatic and neurological history, an increased risk of vascular complications was preceded by structural and functional changes in the cardiovascular system from the beginning of pregnancy; the use of magnesium preparations (Magnerot) improved the patient's condition at the 20-26th week of pregnancy due to a decrease in headache attacks; monitoring of blood pressure levels, its circadian rhythm and laboratory data contributed to the timely detection of gestational complications, timely hospitalization and adequate complex antihypertensive and magnesium therapy.
Cephalgic syndrome in women during pregnancy is noted quite often, accompanies hypertensive disorders, vegetative-vascular dystonia syndrome, depression and is considered the leading manifestation of migraine. Frequent and intense headaches reduce performance, significantly worsen the quality of life. Difficulties in differential diagnosis dictate the need to find effective and safe methods of preventive therapy for headache in pregnant women. In our patient, a migraine headache that preceded pregnancy recurred during pregnancy, which was the basis for prophylactic treatment. Certain difficulties were caused by the choice of the drug. We preferred magnesium preparations.
Frequent and intense headaches reduce performance, significantly worsen the quality of life. Difficulties in differential diagnosis dictate the need to find effective and safe methods of preventive therapy for headache in pregnant women. In our patient, a migraine headache that preceded pregnancy recurred during pregnancy, which was the basis for prophylactic treatment. Certain difficulties were caused by the choice of the drug. We preferred magnesium preparations.
Migraine is a magnesium deficiency disease
Clinical and experimental data allow us to consider migraine as a magnesium deficiency disease [5]. Patients suffering from migraine, compared with healthy people, often have lower concentrations of magnesium in serum and blood cells, saliva and cerebrospinal fluid [6]. Magnesium is the second intracellular cation after potassium; it is involved as a cofactor in more than 300 metabolic reactions in the body, including protein synthesis, intracellular energy metabolism, DNA and RNA reproduction, and stabilization of mitochondrial membranes. Magnesium plays an important role in nerve impulse transmission, cardiac excitability, neuromuscular conduction, muscle contraction, vasomotor tone, and the regulation of glucose and insulin metabolism. Low levels of magnesium in the body are associated with the development of hypertension, type 2 diabetes, Alzheimer's disease, and migraines. It is suggested that one of the mechanisms for the development of migraine headache may be a violation of the intracellular interaction of magnesium and calcium. Altered activity of ion channels plays the role of a trigger in the development of spreading cortical depression [7].
Magnesium plays an important role in nerve impulse transmission, cardiac excitability, neuromuscular conduction, muscle contraction, vasomotor tone, and the regulation of glucose and insulin metabolism. Low levels of magnesium in the body are associated with the development of hypertension, type 2 diabetes, Alzheimer's disease, and migraines. It is suggested that one of the mechanisms for the development of migraine headache may be a violation of the intracellular interaction of magnesium and calcium. Altered activity of ion channels plays the role of a trigger in the development of spreading cortical depression [7].
Magnesium deficiency contributes to platelet hyperaggregation, negatively affects the function of serotonin receptors, the synthesis and release of various neurotransmitters, which causes the development of vascular spasm [8]. Magnesium is involved in modulating the level of nitric oxide in the cell [9], a decrease in which is noted in migraine, especially in women with migraine pain, potentially mediated by sex hormones [10].
Magnesium deficiency in migraine sufferers may be due to genetic causes of malabsorption or increased excretion [11].
The Mitochondrial Theory of Migraine: Drugs
Recent studies have shown that several migraine subtypes are associated with mitochondrial damage to neurons and astrocytes due to intracellular calcium accumulation, free radicals, and a deficiency in oxidative phosphorylation. Markers of these disorders are low superoxide dismutase activity, activation of cytochrome oxidase and nitric oxide, high levels of lactate and pyruvate, and a low ratio of phosphocreatine-inorganic phosphates and N-acetylaspartate-choline in patients with migraine. Mitochondrial dysfunctions are genetically determined; mitochondrial DNA polymorphisms have been described in migraine with vomiting in pediatric practice [12]. The therapeutic evidence of the mitochondrial theory of migraine can be recognized as the effectiveness of a number of drugs with a positive effect on mitochondrial metabolism. These drugs include primarily magnesium preparations, as well as riboflavin, coenzyme Q10, carnitine, topiramate, lipoic acid, niacin.
These drugs include primarily magnesium preparations, as well as riboflavin, coenzyme Q10, carnitine, topiramate, lipoic acid, niacin.
Empiric magnesium therapy seems reasonable in all patients with migraine, as half of them are magnesium deficient, and routine determination of blood magnesium levels does not reflect its real status. At the same time, magnesium preparations are available, safe and inexpensive [11]. The effectiveness of magnesium therapy in patients with migraine has been proven in a number of clinical studies [13].
For patients with episodic migraine (headache ≤ 14 days per month), recommendations for preventive therapy have been developed based on an analysis of the results of randomized trials and Cochrane reviews. Magnesium preparations along with some other drugs (topiramate, propranolol, nadolol, metoprolol, amitriptyline, gabapentin, candesartan, butterbur, riboflavin, coenzyme Q10) were found to be effective and recommended for migraine prevention [14].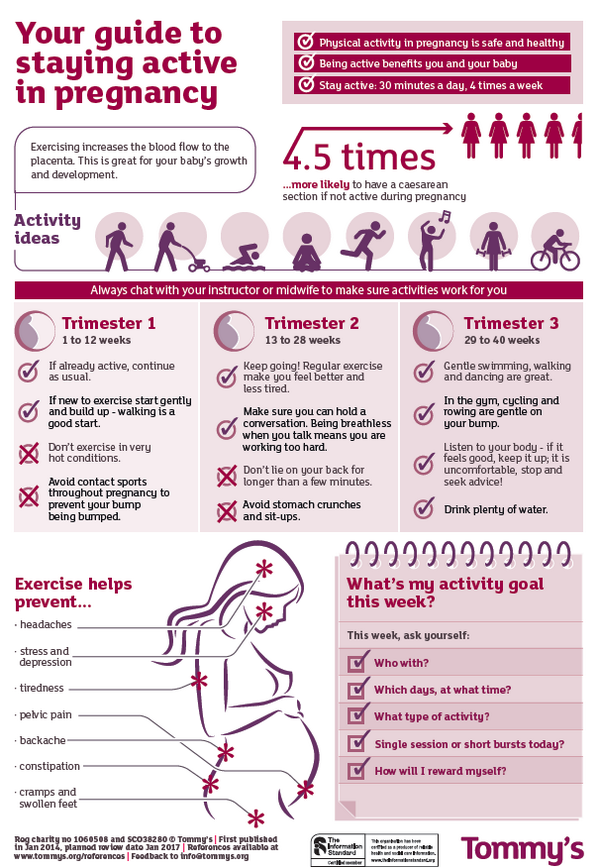
Magnerot during pregnancy
During pregnancy, the administration of magnesium preparations allows achieving a satisfactory effect without fear of embryotoxic and teratogenic effects, unlike many drugs traditionally used to treat headache [15].
For our patient, we recommended taking Magnerot in medium therapeutic doses for a long time (at least 8 weeks). Correction of magnesium deficiency during pregnancy is necessary, since magnesium deficiency is associated with a wide range of complications of pregnancy and childbirth. As is known, a decrease in the content of magnesium leads to an increase in the tone of the myometrium and underlies preterm labor [16, 17]. A low level of intracellular magnesium contributes to the development of AH in pregnant women [18, 19]. Magnesium deficiency during pregnancy can lead to intrauterine growth retardation (IUGR) [20] and poor offspring survival [21]. At the same time, experimental data on the study of IUGR treatment methods in pregnant rats demonstrate the possibility of therapy with a magnesium-enriched diet, which reduced induced fetal growth retardation by 64%, and also reduced the level of pro-inflammatory cytokines in the amniotic fluid and placenta [22].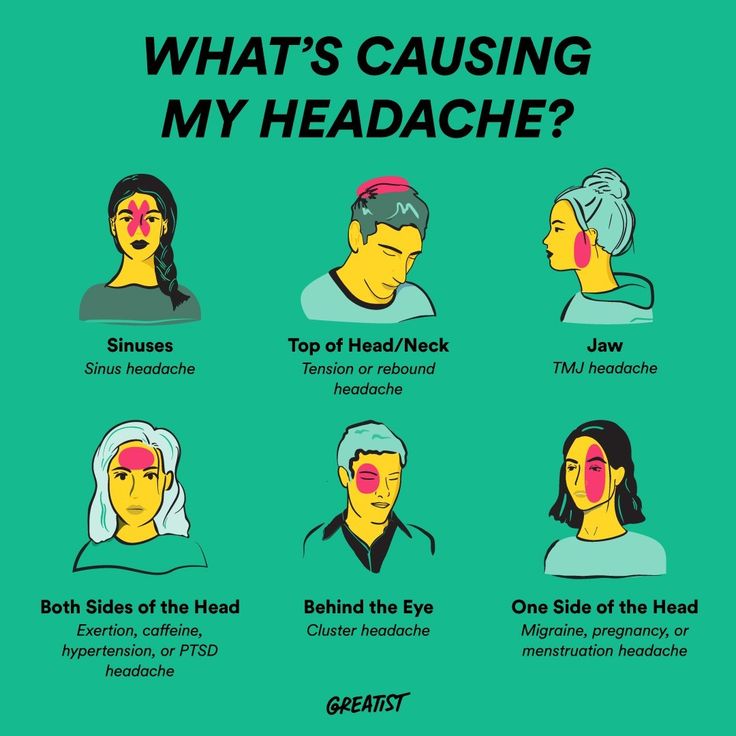
In addition, it has been proven that magnesium inhibits platelet aggregation, reduces the likelihood of coronary artery thrombosis, prevents myocardial ischemia and, as a result, reduces the risk of arrhythmias [23].
It seems that the above arguments justify the use of magnesium preparations (Magnerot) in pregnant women with migraine. Using the example of the described clinical case, we tried to consider the tactics of managing a patient at different stages of pregnancy, the differential diagnosis in cephalalgia, and the significance of indicators of vascular tone and circadian blood pressure in assessing the patient's condition.
What kind of pain occurs during pregnancy, when is it normal and what to do for pain during pregnancy - advice from an obstetrician-gynecologist | ufa1.ru
1
How to determine which pains in pregnant women are correct?
Previously, any kind of pain that pregnant women complained about was perceived as a pathology.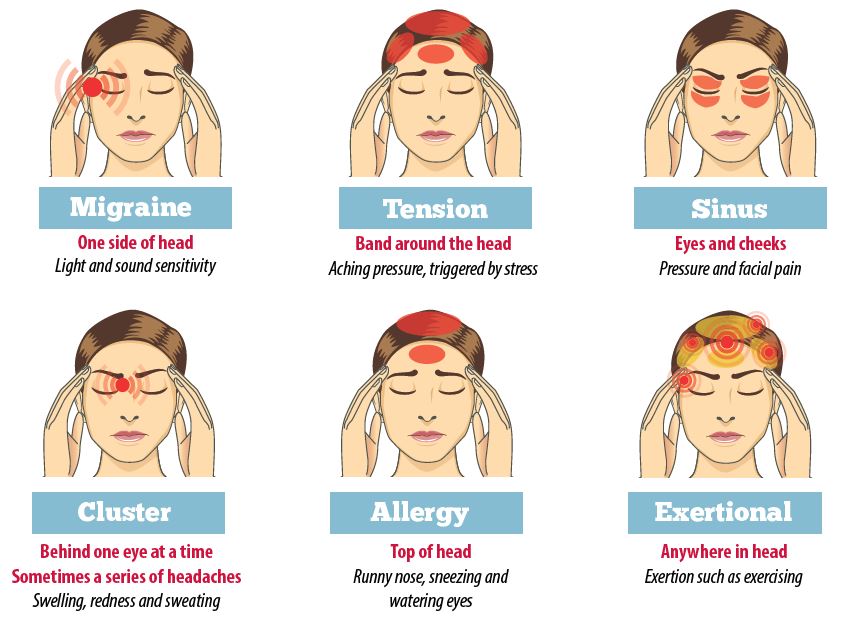 Now, with the advent of new studies, ideas about the features of the course of pregnancy are changing, and today in our work we use the clinical recommendations “Normal pregnancy”, approved by the Ministry of Health of Russia, formed on the basis of world medical experience. They indicate that not every pain in the expectant mother requires hospitalization. We usually divide pain into several subspecies depending on their localization, but most often a pregnant woman experiences abdominal pain. Let's dwell on them in more detail.
Now, with the advent of new studies, ideas about the features of the course of pregnancy are changing, and today in our work we use the clinical recommendations “Normal pregnancy”, approved by the Ministry of Health of Russia, formed on the basis of world medical experience. They indicate that not every pain in the expectant mother requires hospitalization. We usually divide pain into several subspecies depending on their localization, but most often a pregnant woman experiences abdominal pain. Let's dwell on them in more detail.
Share
2
Which symptoms require urgent hospitalization?
- Pain becomes nagging (like before menstruation), occurs every 15 minutes or more, lasts 15–20 seconds and subsides. This may be a sign of a threatened abortion and the onset of preterm labor. It is especially dangerous if such pains are accompanied by bleeding from the genital tract of any intensity.
- Acute pains that do not go away even after the woman has taken a free lying position, and which cause a deterioration in her general condition: dizziness, severe weakness, cold sweat, fainting.
 It can also indicate serious pregnancy complications.
It can also indicate serious pregnancy complications.
- A rapid pulse and low blood pressure combined with pain in the uterus may indicate the development of obstetric complications, such as placental abruption or ectopic pregnancy (if the pregnancy is short term and it is not clear where the ovum is located).
- Women who have a scar on the uterus after a caesarean section or removal of myomatous nodes, it is very important to monitor their condition, because any constant discomfort in the lower abdomen - bursting and aggravated by the movement of the fetus - requires examination and ultrasound for the viability of the scar, in order to prevent complications, such as, for example, uterine rupture.
- A pregnant woman must pay attention to the pain that occurs in the epigastrium (upper abdomen). This is not always a symptom of a disease of the stomach, liver or pancreas, as patients themselves and even doctors often believe.
 In late pregnancy, such pain may indicate the development of a severe complication - preeclampsia.
In late pregnancy, such pain may indicate the development of a severe complication - preeclampsia.
- Periodic headaches. There is a tendency that expectant mothers very often endure headaches, do not complain about them, but this can also be a harbinger of severe obstetric complications. It is very important that women go to the doctors with such symptoms, especially if they are combined with edema, with high blood pressure, with an increased level of protein in the urine. A headache is unbearable.
- Of particular note is the increase in blood pressure in pregnant women (over 140/90 mmHg Art.). Even if a woman has hypertension, to which she was accustomed before pregnancy, does not feel worse when the pressure rises, the fetus and placental vessels are designed for a pressure of no more than 140/90 mm Hg. Art. Anything above this level causes vasospasm, fetal malnutrition, the risk of placental abruption and other hemorrhages, including cerebral hemorrhages in the patient herself.

Important! In any case, when the woman lay down, rested, but the pain in the abdomen did not go away or it is very strong, constant and excessive and causes disturbances in the condition, a quick response is required, calling an ambulance or seeking medical help. If timely help is not provided to the mother and child, the outcome can be very unfavorable. A pregnant woman should not refuse hospitalization recommended by doctors! All this is done only in the interests of mother and child.
Share
3
What kind of pain can you endure?
- Rare pain in the lower abdomen, pulling or indefinite, not more than 2-3 times a day. It should be recalled that the uterus, which is smaller than a fist in a non-pregnant woman, increases significantly in size in an expectant mother, and as it grows, pushes neighboring organs apart to take its position. This mechanical squeezing of other organs by the growing uterus can give unpleasant painful sensations.
 Also, the consequences of this can be frequent urination and discomfort when urinating in early pregnancy (up to 14 weeks, when the uterus is in the small pelvis) and later, when the fetal head descends and presses against the mother's pelvis.
Also, the consequences of this can be frequent urination and discomfort when urinating in early pregnancy (up to 14 weeks, when the uterus is in the small pelvis) and later, when the fetal head descends and presses against the mother's pelvis.
- A woman may occasionally experience spasms and pain in the intestinal area, especially with constipation, which is typical for pregnancy. But all these infrequent functional pains are acceptable and do not require medical intervention.
- Pain in the lumbosacral spine is not considered dangerous if they do not have a periodic cramping character (pulled - got sick - let go) every 15 minutes or more. According to statistics, back pain during pregnancy occurs in 35-60% of women. Among women with back pain, 47% to 60% of women experience back pain for the first time between 5 and 7 months of pregnancy. The most common cause of back pain during pregnancy is an increase in the load on the spine due to an increase in the abdomen and a shift in the center of gravity, as well as relaxation of the ligaments under the influence of relaxin.
 As a rule, such pains pass in the supine position, rest or wearing a bandage.
As a rule, such pains pass in the supine position, rest or wearing a bandage.
Share
4
How can you relieve non-urgent pain yourself?
- The most important tip: give the pregnant woman the opportunity to lie down and rest, especially if the pain is associated with fatigue or overexertion.
- If your back hurts, a light massage in the lumbar region will help, it can be done by a pregnant woman's spouse or someone close. Warming procedures and ointments should not be used. The mode of physical activity is important, including a change of loads and rest, swimming, physical exercises.
- A light sedative antispasmodic herbal tea can help with various types of tolerable pain, it is allowed for pregnant women. These are chamomile, valerian, motherwort, mint, lemon balm and others. Herbal tea for pregnant women also helps to cope with functional disorders of the gastrointestinal tract and early toxicosis (nausea and vomiting).

- We do not prohibit pregnant women from bathing or swimming, if it is pleasant and enjoyable for a woman, then this is permissible. But we do not recommend taking a hot bath: you can overdo it with the temperature of the water, which can increase blood circulation and cause complications during pregnancy. It is allowed to take a light warm shower.
Share
5
What to do if the pain does not go away?
If a pregnant woman has a deterioration in her general condition, we recommend that you seek medical help and be examined. For this, no one will scold! If the general condition is severe, contractions have begun, amniotic fluid has broken, bleeding has appeared, a severe headache is bothering you, call an ambulance. In other cases, you can contact your own or the doctor on duty at the antenatal clinic where you are being observed. It happens that women go to the emergency room of the maternity hospital on their own - we do not refuse anyone to be examined and examined. For example, in our Republican Clinical Perinatal Center, we perform ultrasound, cardiotocography (we examine the fetal heartbeat), fully examine the patient, assess the situation, and after a complete examination, if the pathology is detected, we accompany to the hospital or, if there are no complications, for each pregnant woman who comes to us with pain, sent home for outpatient follow-up. And then the women, with the confidence that everything is fine with them, leave. Other institutions of obstetrics work in the same way. And, of course, it’s right to make sure that everything is fine with the baby if there were worries and pains. Many expectant mothers fear that “I will still be admitted to the hospital, regardless of whether I have health problems or not.” This position is fundamentally wrong! Today we are moving away from unnecessary hospitalization and offer inpatient treatment to a pregnant woman only if there are serious grounds for this after a full examination.
For example, in our Republican Clinical Perinatal Center, we perform ultrasound, cardiotocography (we examine the fetal heartbeat), fully examine the patient, assess the situation, and after a complete examination, if the pathology is detected, we accompany to the hospital or, if there are no complications, for each pregnant woman who comes to us with pain, sent home for outpatient follow-up. And then the women, with the confidence that everything is fine with them, leave. Other institutions of obstetrics work in the same way. And, of course, it’s right to make sure that everything is fine with the baby if there were worries and pains. Many expectant mothers fear that “I will still be admitted to the hospital, regardless of whether I have health problems or not.” This position is fundamentally wrong! Today we are moving away from unnecessary hospitalization and offer inpatient treatment to a pregnant woman only if there are serious grounds for this after a full examination.
Share
6
I don't want to go to the hospital, but the doctor insists.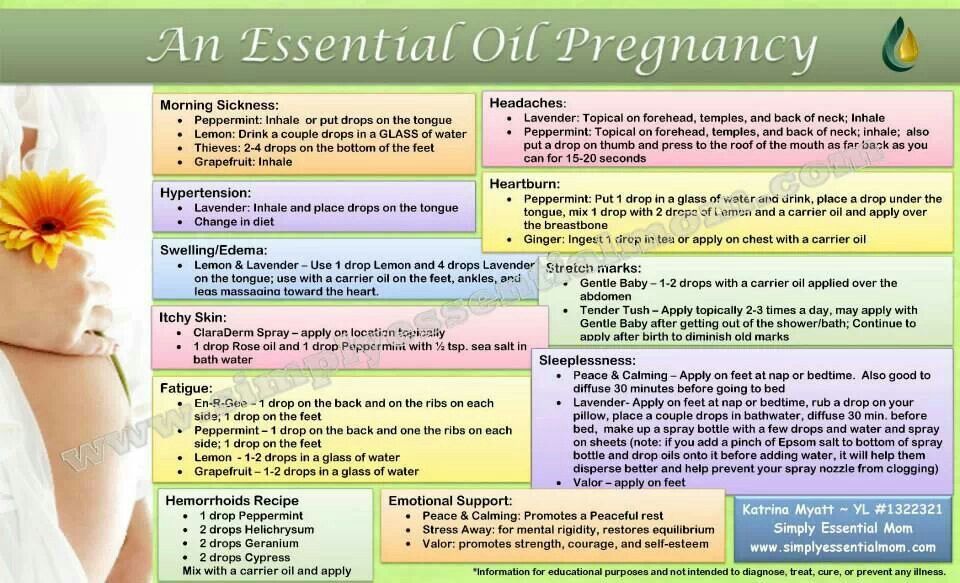 How to proceed?
How to proceed?
But at the same time, the obstetric service has another serious problem: pregnant women often hide their complications, pain, and thus cross the threshold of a serious complication. And then they categorically refuse to provide medical care, and their spouses and relatives support them in this. If the doctor insists on hospitalization, relatives should release the expectant mother from all problems and affairs, let her go to the hospital calmly, and husbands should not convince their spouse that she does not need medical help! We are constantly faced with such a problem, and we have to persuade not only worried expectant mothers, but also all their relatives. In emergency situations, when minutes count, such lengthy persuasion is simply unacceptable!
If a pregnant woman does not feel well, no matter what it is, or you see that she is close to passing out, she has a severe headache, muscle twitching, sharp abdominal pain, any discharge, not you need to do Internet diagnostics or help a pregnant woman with improvised means! This is an occasion to send a pregnant woman to the hospital as quickly as possible by calling an ambulance.
Share
7
What should I do if I start bleeding?
One of the most dangerous complications that a pregnant woman can experience is bleeding. In this case, the woman must be placed on a horizontal surface and an ambulance should be called immediately. In no case do we wait until it passes by itself!
- Until the ambulance arrives, a woman must remain in a horizontal position - not on her back, but on her side, because blood circulation in the uterus is disturbed on her back. Under no circumstances should she walk.
- It is undesirable to take the patient to the hospital on your own, because blood loss can be large and fast, and, accordingly, moving in your own car, without medical equipment and without special systems that are in the ambulance, can lead to worsening condition of the pregnant woman. It is better to wait for the arrival of specialists, because bleeding is a very serious pathology during pregnancy.
Share
8
Can a pregnant woman take painkillers while she is waiting for the doctor?
While waiting for the doctors to arrive, do not experiment with pregnant women! Even a glass of water, tea, pain pills can interfere with further medical care. For example, a pregnant woman became ill due to placental abruption (but she does not know about this yet). Upon arrival at the maternity hospital, if an emergency caesarean section is necessary, taking food, water, and medicines will make it difficult to choose and perform anesthesia for the operation. Therefore, when it comes to an incomprehensible condition that suddenly developed in an expectant mother, it is better not to take any unnecessary actions and be aware that some of these conditions may require an emergency delivery. The doctor should understand the situation, not others.
Share
9
What should I do if I have seizures?
Emergency care may be required for convulsions in pregnant women . We are talking about a convulsive attack, which is manifested by a violation of consciousness, twitching of facial and skeletal muscles, involuntary convulsive movements and arching of the trunk and limbs, respiratory disorders. Such an attack may be a manifestation of epilepsy, intracerebral hemorrhage, or a severe complication of pregnancy for a period of more than 20 weeks - eclampsia. You should immediately call an ambulance, even if the attack did not last long and completely passed. Unfortunately, it may happen again in the near future. You can not forcefully hold a woman and try to stop the convulsions with mechanical efforts, this can lead to injury. It is necessary, in the supine position on the left side, to carefully protect the head and limbs from blows, to ensure the patency of the respiratory tract - to make sure that there is not a large amount of mucus or vomit in the oral cavity: when breathing is restored after a convulsive seizure, a woman can inhale this content. If necessary, clean the oral cavity with a tissue, handkerchief.
We are talking about a convulsive attack, which is manifested by a violation of consciousness, twitching of facial and skeletal muscles, involuntary convulsive movements and arching of the trunk and limbs, respiratory disorders. Such an attack may be a manifestation of epilepsy, intracerebral hemorrhage, or a severe complication of pregnancy for a period of more than 20 weeks - eclampsia. You should immediately call an ambulance, even if the attack did not last long and completely passed. Unfortunately, it may happen again in the near future. You can not forcefully hold a woman and try to stop the convulsions with mechanical efforts, this can lead to injury. It is necessary, in the supine position on the left side, to carefully protect the head and limbs from blows, to ensure the patency of the respiratory tract - to make sure that there is not a large amount of mucus or vomit in the oral cavity: when breathing is restored after a convulsive seizure, a woman can inhale this content. If necessary, clean the oral cavity with a tissue, handkerchief.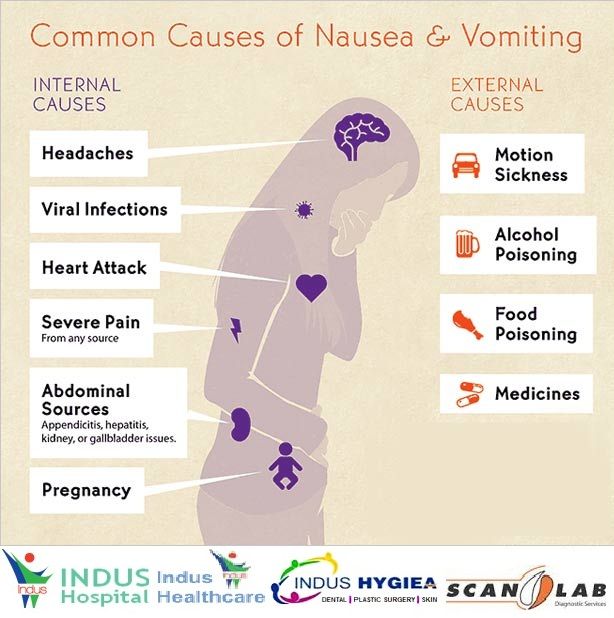 All other assistance will be provided by ambulance specialists.
All other assistance will be provided by ambulance specialists.
Share
10
What should I do if my water breaks?
Amniotic fluid discharge requires immediate response . The woman should take a horizontal position and call an ambulance. It is desirable that the expectant mother does not get to the maternity hospital on her own - by taxi or by her husband's car - but accompanied by ambulance workers, because here there are certain risks for the health of mother and baby. On average, the first birth in women occurs within 8-12 hours, the second - 6-8 hours. This time is enough to get to the hospital. Today we are faced with such problems as waiting at home for the onset of labor when the amniotic fluid breaks. This is a very dangerous phenomenon, since with an increase in the duration of the anhydrous period, the risk of infection in the fetus increases, and if the woman's birth canal is not ready, then delaying with the use of special methods of preparing for natural childbirth can lead to a forced caesarean section.
Share
11
What should I do if I have contractions?
If a woman feels that regular contractions have begun during a premature pregnancy, she must go to the hospital, there is no need to wait for it to “go away by itself”. In case of premature birth, it is especially necessary to rush to the maternity ward, because in some cases doctors can stop the process: special drugs are used that restrain labor, and sometimes doctors manage to prolong the pregnancy. Or doctors do everything necessary to properly and quickly prepare a premature baby for birth.
Share
12
What should a pregnant woman take with her to the hospital?
Every pregnant woman at home should have a "duty" bag ready to take with her to the maternity hospital or gynecological department in case complications arise, you call an ambulance and hospitalization is required. This bag should contain copies of documents - a passport, a compulsory medical insurance policy, SNILS, personal hygiene items, clothes and removable shoes that are necessary for a stay in the hospital, and those drugs that a pregnant woman regularly takes as prescribed by a doctor.