Uterus position by week
Your Body throughout Pregnancy
Your Body Before Pregnancy
Next Image
Your Body Before Pregnancy
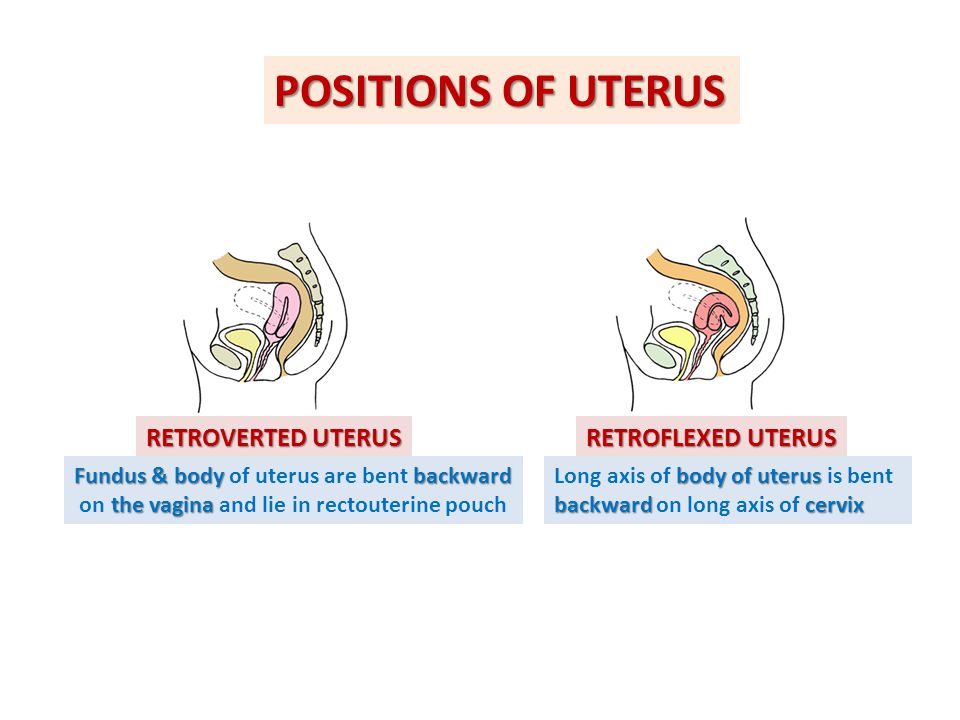
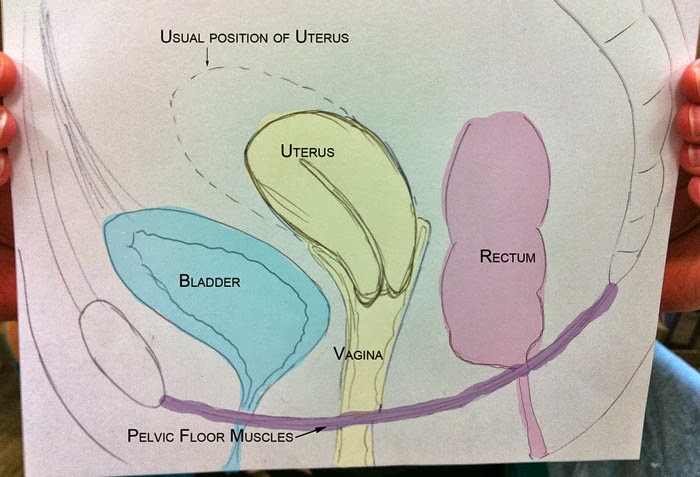
Before pregnancy, most of the space in your abdomen is taken up by the large and small intestines. There is no real separation between the areas of your pelvis and abdomen.
In the picture here, you can see that the vagina is behind the bladder (sac that collects urine) and urethra (tube for moving urine out of bladder and body). In its normal position, your uterus is above and behind the bladder, with the cervix protruding into the vagina. The pelvic colon, rectum and anal canal are behind the vagina and uterus.
Previous | Next
Your Body at 6-7 Weeks of Pregnancy
Next Image
Your Body at 6-7 Weeks of Pregnancy
When you are between 6 and 7 weeks pregnant, you may be experiencing the early signs of pregnancy: your period has stopped and you may have nausea, breast tenderness and swelling, frequent urination and fatigue.
At this point, your uterus has begun to grow and become more egg-shaped. The pressure of the growing uterus on the bladder causes frequent urge to urinate.
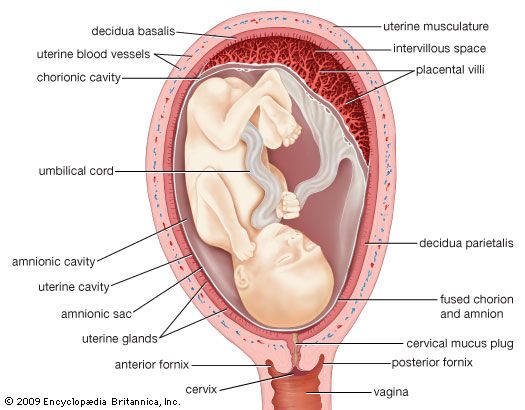
In this image, you can see the beginnings of the placenta in the uterus. The embryo is about 1/4 inch to 1/2 inch long and weighs 1/1,000th of an ounce.
The embryo’s head is large in proportion to the rest of the body. The internal organs are forming and the heart has been beating since the end of the 4th week.
The embryo is floating in the amniotic sac. Buds for the arms and legs emerge in the 5th week and, by the 7th week, buds for fingers and toes also appear. The umbilical cord is lengthening and will continue to grow, allowing the fetus freedom to move. The 7th week represents a milestone in development: the embryo is now considered a fetus.
Previous | Next
Your Body at 12 Weeks of Pregnancy
Next Image
Your Body at 12 Weeks of Pregnancy
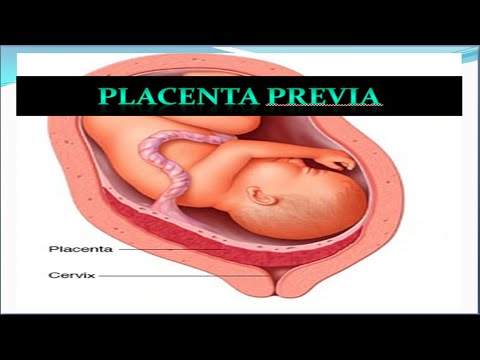
At the 12th week of pregnancy, the placenta is much larger.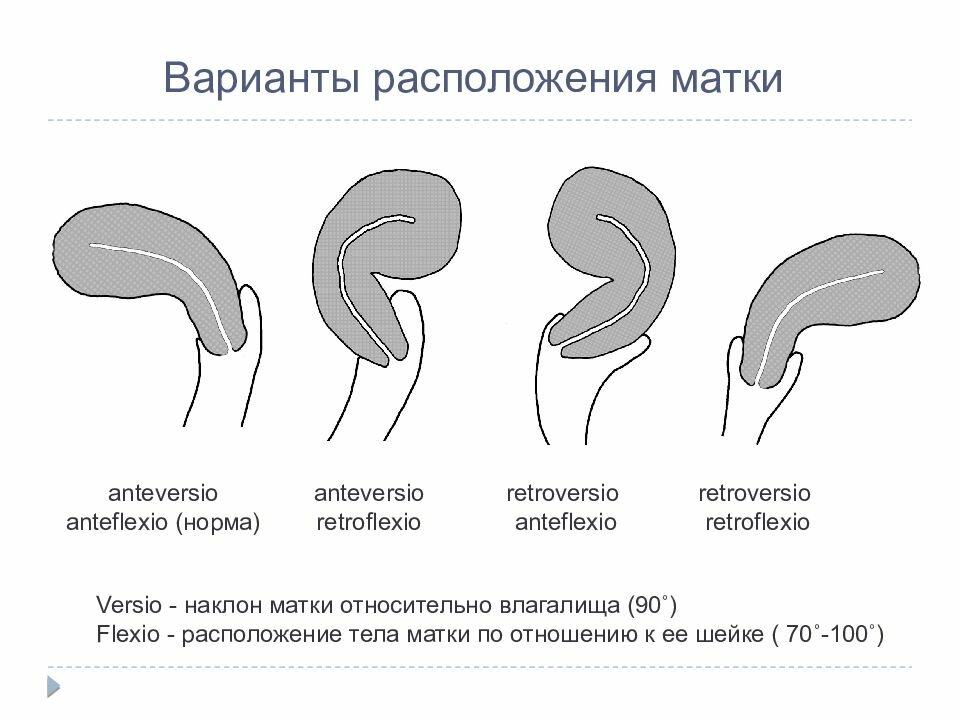 It now produces the hormones needed to sustain the pregnancy. Your uterus is the size of a grapefruit and completely fills the pelvis. It rises up into the area of the abdomen, as shown in the image. The fundus, the upper end of the uterus, is just above the top of the symphysis where the pubic bones join together. This upward growth of the uterus takes pressure off the bladder and decreases the need for frequent urination. The mucus plug, a barrier to protect the growing fetus, fills your cervical canal.
It now produces the hormones needed to sustain the pregnancy. Your uterus is the size of a grapefruit and completely fills the pelvis. It rises up into the area of the abdomen, as shown in the image. The fundus, the upper end of the uterus, is just above the top of the symphysis where the pubic bones join together. This upward growth of the uterus takes pressure off the bladder and decreases the need for frequent urination. The mucus plug, a barrier to protect the growing fetus, fills your cervical canal.
The fetus is now about 3 inches long and weighs about 1 ounce. By this week, the fetus has fingernails and toenails and can open and close the fingers. The fetus will start to move, but you will not feel it yet.
Previous | Next
Your Body at 20 Weeks of Pregnancy
Next Image
Your Body at 20 Weeks of Pregnancy
By the 20th week of pregnancy, your uterus can be felt at the level of your belly button (umbilicus).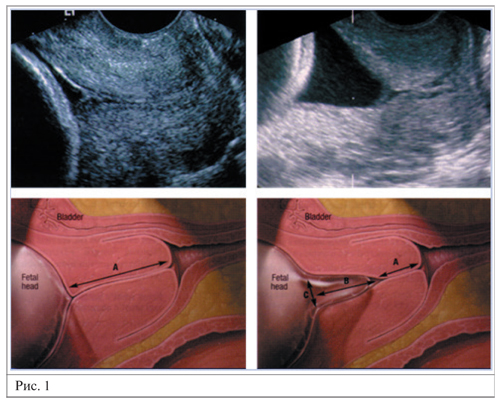 The pelvic colon and small intestines are crowded upward and backward. The ascending and descending colon maintain their usual positions.
The pelvic colon and small intestines are crowded upward and backward. The ascending and descending colon maintain their usual positions.
At this point, your uterus is especially enlarged where the placenta attaches to it (usually on the front or back wall). This gives the uterus an uneven bulge. The wall of the uterus, which lengthens and thickens early in pregnancy, stretches as the fetus grows, and becomes thinner now – just 3 to 5 millimeters thick. Your bladder moves up but not as much as your uterus, which straightens as it moves up.
As your uterus moves up, it rests against the lower portion of the front of your abdominal wall, causing it to bulge forward noticeably by your 20th week. The size of the bulge depends on how strong your abdominal muscles are. If they are firm, the uterus may be pressed against the spinal column, and there will be no noticeable bulge; if they are weak, the pressure of the uterus against the inside wall makes a sizeable bulge.
At this point, you should be able to feel light movements of the fetus. This is called “quickening.” You may recognize this earlier if you have been pregnant before. The fetus sleeps and wakes at regular intervals, is more active, is about 9 inches long and weighs between a half-pound and a pound.
This is called “quickening.” You may recognize this earlier if you have been pregnant before. The fetus sleeps and wakes at regular intervals, is more active, is about 9 inches long and weighs between a half-pound and a pound.
Previous | Next
Next Image
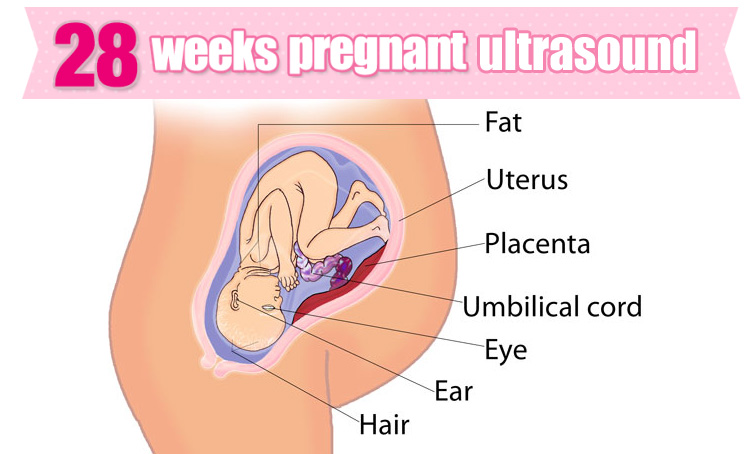
At this point in pregnancy, the top of your uterus is about one-third of the distance between the bellybutton and the xiphoid cartilage at the lower end of your breastbone. Constipation is common because your uterus is pressing on your lower colon and hormones slow down your body’s excretion process. Between the growth of your uterus and general weight gain, you may be feeling fatigued. Some women also experience heartburn as your uterus presses against your stomach.
Your breasts are also changing to get ready for breastfeeding. First colostrum and then milk are produced by the grape-like clusters of tiny sacs (alveoli) deep within the breast tissue. Clusters of alveoli form lobules, which come together to form 15 to 20 lobes. Each lobe connects to a lactiferous duct for conveying milk. As the ducts extend toward the nipple and areola (darker area around the nipple), they widen into the lactiferous sinuses. These sinuses (or milk pools) release the milk through 15 to 20 tiny nipple openings in each breast when the baby nurses.
At week 28, the fetus is about 16 inches long and weighs two to three pounds. The skin is wrinkled but will become less so as more fat builds up under the skin in the next few weeks. Fine, downy hair called lanugo, and a waxy white protective substance covering the skin called vernix, are on the fetus’ body. Its eyes are open, and eyebrows and eyelashes were formed in the fourth month. The fetus sucks its thumb and its taste buds have developed.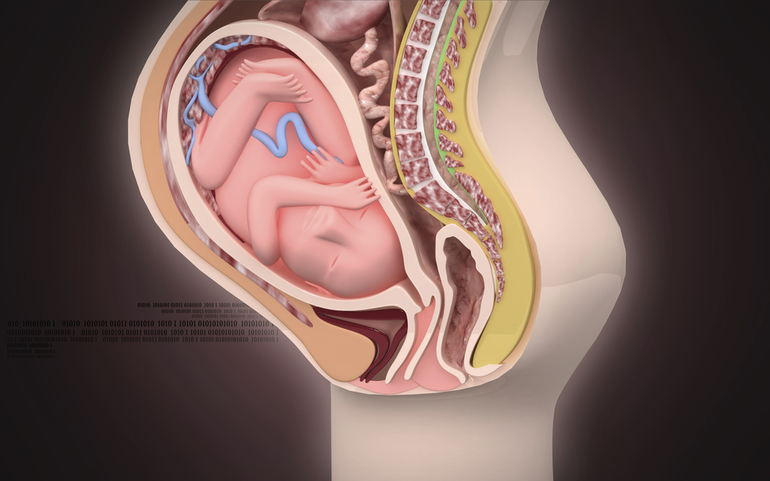 It kicks, stretches and moves frequently in your uterus—you’ll feel it moving around and others might even be able to see these movements!
It kicks, stretches and moves frequently in your uterus—you’ll feel it moving around and others might even be able to see these movements!
Fetal organs and systems are quite well developed by the 28th week of pregnancy, but the final two months of gestation are important for further maturation of all body systems and organs.
Previous | Next
Your Body at 36 Weeks of Pregnancy
Next Image
Your Body at 36 Weeks of Pregnancy
By the end of the 36th week of pregnancy, your enlarged uterus almost fills the space within your abdomen. The fetus is inside the membrane sac within the uterus and high within the abdomen. The muscles of your abdomen support much of its weight.
During this week, the top of the uterus is at the tip of the xiphoid cartilage at the lower end of the breastbone, which is pushed forward.
The change in the position of the heart and the upward pressure of the diaphragm may make it hard to breathe at this point. The crowding of your stomach and intestines may contribute to discomfort after eating.
Your cervix is long, thick and filled with the mucous plug. By the 36th week, your vagina and urethra are elongated and all the tissues in the perineum (area between vaginal and anal openings) are enlarged. The swollen perineum projects outward in the last weeks of pregnancy and readily expands during labor.
The brain of the fetus is growing rapidly, but bones in the skull are soft so that he or she will fit through your vagina at birth. The lungs are still forming. You will likely feel the fetus kicking and may be aware of rhythmic movements, which could be hiccups or thumb sucking. Another possible sensation, sudden movement, may be a startle response.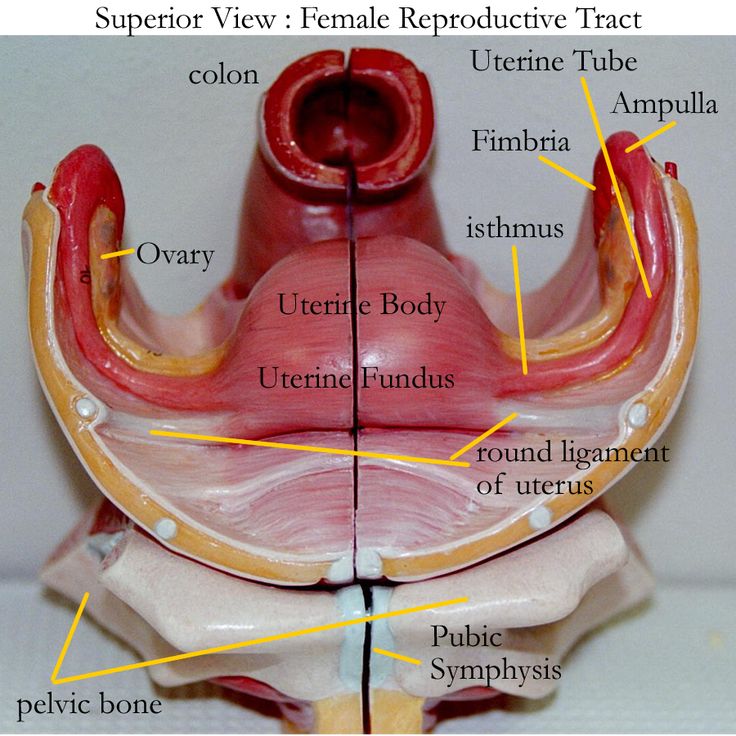
Previous | Next
Your Body at 40 Weeks of Pregnancy (Internal)
Next Image
Your Body at 40 Weeks of Pregnancy (Internal)
At full term, or 40 weeks of pregnancy, the fetus’ head has generally lowered into your pelvis, where it takes up most of the space. This is called “lightening.” In first pregnancies, this may happen a few weeks before labor. In repeat pregnancies, this can happen at the time of labor. The canal of the broad, enlarged cervix is still filled with the plug of mucous. If this is your first pregnancy, the small opening at the bottom of your cervix is usually not dilated, whereas if you have given birth before, it will often be open as wide as two fingers some time before labor begins.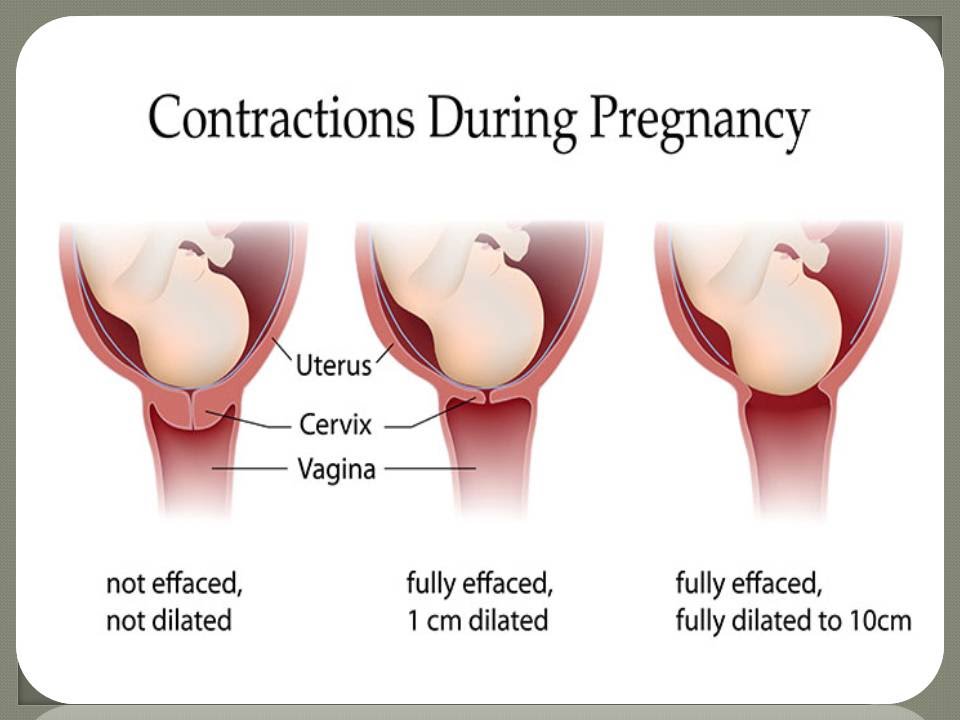
At this point, you may be experiencing frequent urination, increased constipation, edema (water retention) and aching legs or vulva. Varicose veins in the vulva, rectum and legs are also possible. This is because of the position of the uterus, the pressure of the baby's head and a loss of muscle tone as the hormone relaxin loosens your tissues in preparation for birth. Other changes at this time include increased development of blood vessels and increased amount of blood.
Previous | Next
Your Body at 40 Weeks of Pregnancy (External)
Next Image
Your Body at 40 Weeks of Pregnancy (External)
You can see that the round ligament is long and enlarged.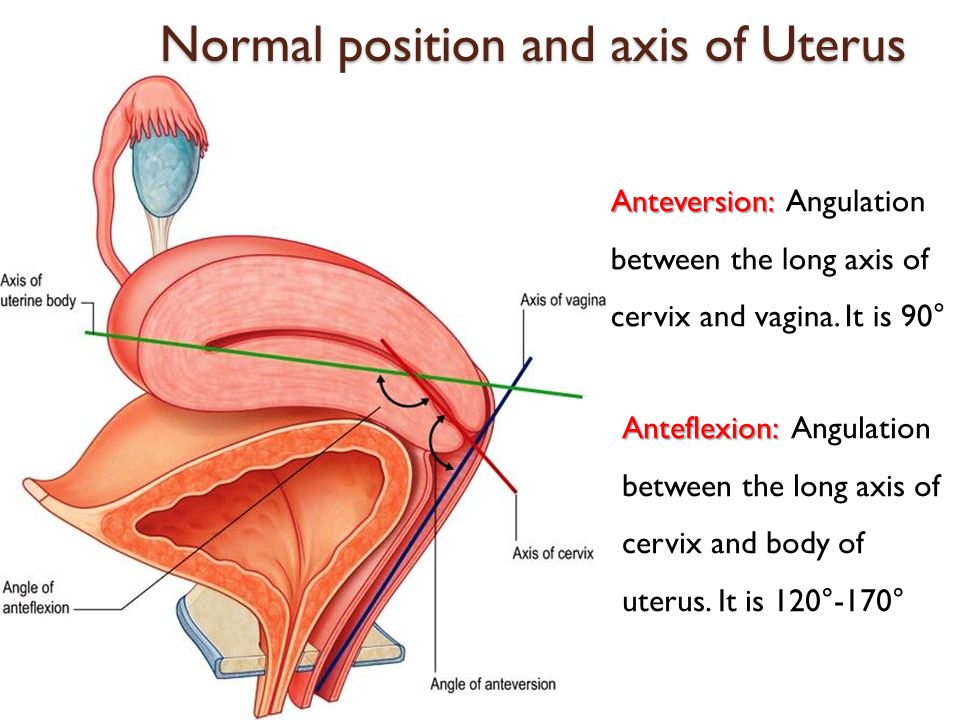 It is also farther forward because of the twisting of the uterus. The enlarged uterosacral ligament is shown stretched taut by the enlarged uterus. Backaches in late pregnancy may be due to the stress of the weight of your uterus on the ligaments that connect it to your spine.
It is also farther forward because of the twisting of the uterus. The enlarged uterosacral ligament is shown stretched taut by the enlarged uterus. Backaches in late pregnancy may be due to the stress of the weight of your uterus on the ligaments that connect it to your spine.
Because your uterus dropped a bit, you may be able to breathe and eat more comfortably near the end of your pregnancy.
At this time, the lungs of the fetus are likely fully mature and ready to begin breathing. The fetus gains about a half pound every week at the end of pregnancy, for a birth weight of roughly 7 pounds, and is growing longer for a birth length of about 18 to 21 inches.
Labor starting on its own around week 40 is a sign that your body is ready to give birth and your baby is ready to be born.
Previous | Next
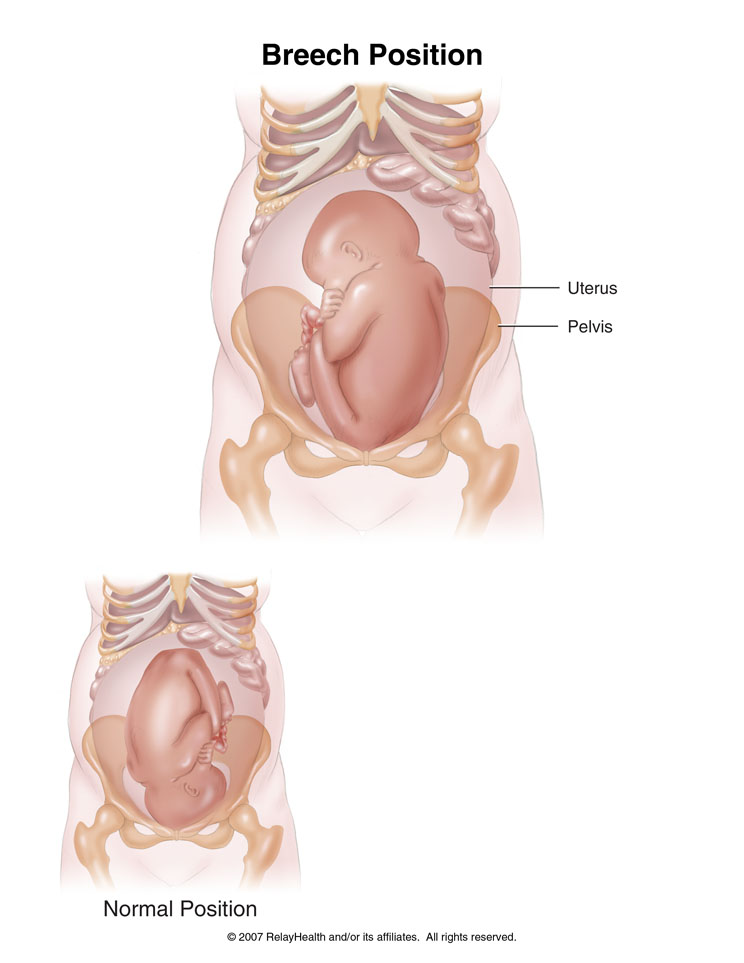
Baby Positions in Womb: What They Mean
As your baby grows during pregnancy, they may move around quite a bit in the womb.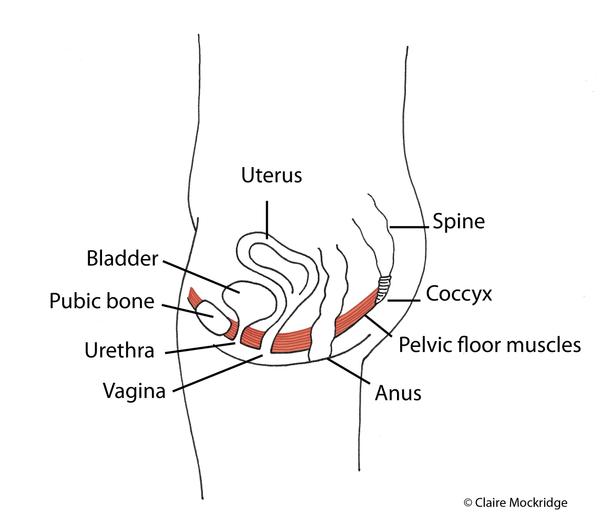 You might feel kicking or wiggling, or your baby may twist and turn.
You might feel kicking or wiggling, or your baby may twist and turn.
During the last month of pregnancy, your baby is bigger and doesn’t have much wiggle room. The position of your baby becomes more important as your due date nears. This is because your baby needs to get into the best position to prepare for delivery.
Your doctor will continually assess the position of your baby in the womb, especially during the last month.
Read on to find out what it means when your doctor uses words like anterior, posterior, transverse, or breech to describe the position of your baby. You’ll also learn what to do if your baby isn’t in the best position before your due date.
The baby is head down, with their face facing your back. The baby’s chin is tucked into their chest and their head is ready to enter the pelvis.
The baby is able to flex their head and neck, and tuck their chin into their chest. This is usually referred to as occipito-anterior, or the cephalic presentation.
The narrowest part of the head can press on the cervix and help it to open during delivery. Most babies generally settle in the head-down position around the 33- to 36-week range. This is the ideal and safest position for delivery.
Share on Pinterest
The baby is facing head down, but their face is positioned toward your stomach instead of your back. This is typically called the occipito-posterior (OP) position.
In the first stage of labor, about one-tenth to one-third of babies are in this position. Most of these babies will spontaneously rotate themselves to face in the right direction before birth.
But a number of cases, the baby doesn’t rotate. A baby in this position increases your chances of having a prolonged delivery with severe back pain. An epidural might be needed to ease some of the pain during delivery.
Share on Pinterest
A breech baby is positioned with their buttocks or feet first. There are three variations of a breech presentation:
- Complete breech.
 The buttocks are pointing toward the birth canal (downward), with the legs folded at the knees. The feet are near the buttocks.
The buttocks are pointing toward the birth canal (downward), with the legs folded at the knees. The feet are near the buttocks. - Frank breech. The buttocks are toward the birth canal, but the baby’s legs are straight up in front of their body, and the feet are near the head.
- Footling breech. One or both of the baby’s feet are pointing downward toward the birth canal.
A breech position is not ideal for delivery. Though the majority of breech babies are born healthy, they may have a higher risk of birth defects or trauma during delivery.
In a breech birth, the baby’s head is the last part of its body to emerge from the vagina, which makes it more difficult to get through the birth canal.
This position can also be problematic because it increases the risk of forming a loop in the umbilical cord that could cause injury to the baby if they’re delivered vaginally.
Your doctor will discuss options for trying to turn the baby into a head-down position before you enter into your final weeks.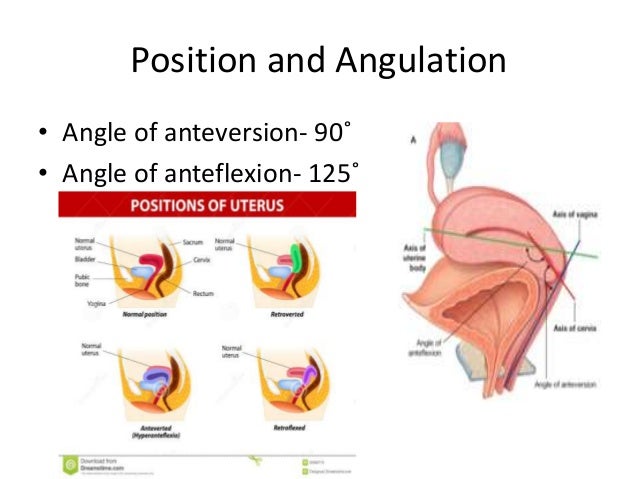 They might suggest a technique called an external cephalic version (ECV).
They might suggest a technique called an external cephalic version (ECV).
This procedure involves applying pressure to your abdomen. It may be uncomfortable for you, but it isn’t dangerous. The baby’s heartbeat will be monitored very closely and the procedure will be stopped immediately if a problem develops.
The ECV technique is successful about half of the time.
If ECV doesn’t work, you may need a cesarean delivery to safely give birth to a breech baby. This is especially true in the case of a footling breech.
In such cases, the umbilical cord may be squeezed as the baby moves toward the birth canal. This could cut off the baby’s supply of oxygen and blood.
Share on Pinterest
The baby is lying horizontally in the uterus. This position is known as transverse lie.
It’s extremely rare at delivery, since most babies will turn themselves to be head down prior to their due date. If not, babies in this position will require a cesarean delivery.
This is because there is a small risk of the umbilical cord prolapsing (coming out of the womb before the baby) when your water breaks.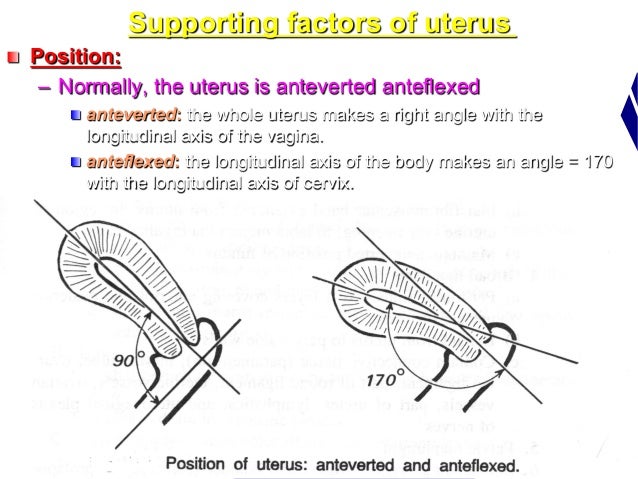 An umbilical cord prolapse is a medical emergency, and the baby must be delivered very quickly via cesarean if it happens.
An umbilical cord prolapse is a medical emergency, and the baby must be delivered very quickly via cesarean if it happens.
Want to track your baby’s position prior to delivery? You can use a process known as “belly mapping” starting around month 8.
All you’ll need are a nontoxic washable marker or paint, and a doll for visualizing how your baby is positioned in the womb.
It’s best to do belly mapping right after a visit with your doctor, so you’ll know for sure if your baby’s head is facing up or down. Just follow these easy steps:
- Lie down on your bed and put slight pressure around your pelvic area to feel around for the baby’s head. It’ll feel like a mini bowling ball. Mark it on your belly.
- Use a fetoscope or during an ultrasound, locate your baby’s heartbeat and mark it on your belly.
- Use the doll to start playing around with positions, based on the position of your baby’s head and heart.
- Find your baby’s bum. It will be hard and round.
 Draw it on your belly.
Draw it on your belly. - Think of your baby’s movement. Where are they kicking? Use their kicks and wiggles as clues to their position. This will give you a good idea where their legs or knees are located. Mark it down on your belly.
- Use the markings to draw your baby on your stomach. Some mothers get creative and paint their baby’s position on their stomach like a piece of art.
Share on Pinterest
Occasionally, a baby may not end up in the correct position for delivery. It’s important to know if your baby isn’t in the occipito-anterior position right before birth. The exact position of a baby could lead to complications during delivery.
There are some methods you can use to coax your baby into the right position.
You can try the following:
- When you sit down, tilt your pelvis forward instead of backward.
- Spend time sitting on a birth ball or exercise ball.
- Make sure your hips are always higher than your knees when you sit.
- If your job requires lots of sitting, take regular breaks to move around.
- In your car, sit on a cushion to lift up and tilt your bottom forward.
- Get on your hands and knees (like you’re scrubbing the floor) for a few minutes at a time. Try this a few times a day to help move your baby into the anterior position.
These tips don’t always work. If your baby stays in a posterior position when labor starts, it may be because of the shape of your pelvis rather than your posture. In some cases, a cesarean delivery will be necessary.
Toward the end of your pregnancy, it may feel like your baby has dropped lower into your abdomen. This is referred to as lightening.
The baby is settling deeper into your pelvis. This means less pressure on your diaphragm, which makes it easier to breathe and also brings fewer baby kicks to the ribs. Your baby dropping is one of the first signs that your body’s getting ready for labor.
Babies toss and turn frequently during pregnancy. You probably won’t feel their movement until the middle of the second trimester. They’ll eventually settle into a position for delivery — ideally head down, facing your back — by week 36.
You probably won’t feel their movement until the middle of the second trimester. They’ll eventually settle into a position for delivery — ideally head down, facing your back — by week 36.
Before that time, you shouldn’t worry too much about your baby’s position. It’s common for posterior babies to adjust their position themselves during delivery and before the pushing stage. Try to stay relaxed and positive during this time.
A baby who isn’t in the ideal position before your delivery date should always be delivered in a hospital setting for the best care.
Emergencies during this type of labor need to be handled by skilled medical staff. Be sure to talk to your doctor if you have any concerns about the position of your baby as your due date nears.
“In most cases of poor positioning in the womb, the baby will turn spontaneously before the start of labor. There are many things that a woman can do to help it along, though. Try positioning, acupuncture, and chiropractic care. Speak with your doctor about using some of these techniques during your pregnancy.” — Nicole Galan, RN
Speak with your doctor about using some of these techniques during your pregnancy.” — Nicole Galan, RN
Share on Pinterest
How the belly grows - articles from the specialists of the clinic "Mother and Child"
Bagriy Alexander Tarasovich
Anesthesiologist-resuscitator
Clinical hospital "AVICENNA" GC "Mother and Child"
Let's say right away that how the belly looks and grows during pregnancy depends on many reasons: the physique of a woman, the structure of the pelvis, the state of the muscles, height uterus and baby, the amount of amniotic fluid. Therefore, for some, the belly grows faster, for some it is slower, for some mothers it is large, for others it can be almost invisible. But still, there are some general patterns of growth and size of the abdomen during pregnancy.
Growth rate
1st trimester
As a rule, in the early stages of pregnancy, the belly does not increase in size or increases very slightly. This is due to the fact that the uterus is still very small and takes up little space in the pelvis. So, for example, by the end of 4th week the uterus reaches only the size of a chicken egg, by the 8th week increases to the size of a goose, but most importantly, at this time it still does not reach the pubic articulation (located in the lower abdomen ). That is why in the early stages no increase in the abdomen is visible. And only after 12th week (end of the first trimester of pregnancy) the fundus of the uterus begins to rise above the womb.
This is due to the fact that the uterus is still very small and takes up little space in the pelvis. So, for example, by the end of 4th week the uterus reaches only the size of a chicken egg, by the 8th week increases to the size of a goose, but most importantly, at this time it still does not reach the pubic articulation (located in the lower abdomen ). That is why in the early stages no increase in the abdomen is visible. And only after 12th week (end of the first trimester of pregnancy) the fundus of the uterus begins to rise above the womb.
II trimester
At this time, the child is rapidly gaining height and weight, and the uterus is also growing rapidly. That is why, at a period of 12-16 weeks, an attentive mother will see that the stomach has already become noticeable. True, others will pay attention to the woman’s new position at about 20-q weeks, especially if she wears tight-fitting things.
III trimester
By the beginning of the third trimester, no one doubts pregnancy. The abdomen is clearly visible even if the woman is wearing loose clothing.
The abdomen is clearly visible even if the woman is wearing loose clothing.
Sharp, round, various
Approximately from the second trimester of pregnancy, during each examination, the obstetrician-gynecologist determines the height of the uterine fundus and measures the circumference of the abdomen at the level of the navel. Why does the doctor so carefully monitor the increase in mother's tummy? The fact is that this is the easiest way to control the growth and development of the unborn baby.
One of the formulas for estimating fetal weight by fundal height (FHH): the shape of the abdomen often tried to determine the sex of the child. It was believed that a round belly portends a girl, and an elongated, oblong, “sharp” one portends a boy. However, these predictions did not always come true, since the shape and size of the abdomen do not depend at all on the sex of the child.
- In large, tall women, the belly may be small and not very noticeable until advanced pregnancy, and in thin, petite women (especially with a narrow pelvis or large baby), the belly seems very large.
- Significant influence on the shape of the abdomen has a state of muscle tone of the anterior abdominal wall and uterus. During the first pregnancy and good muscle tone, the abdomen may look more "tight" than in subsequent pregnancies. In addition, with repeated pregnancies as a result of reduced muscle tone of the anterior abdominal wall, the child does not take the final position until the last month of pregnancy. Because of this, the shape of the abdomen can also be "stretched".
- If a woman is expecting twins, her belly will be larger than with a single pregnancy.
- And often the belly can be large simply because a woman ceases to limit herself in nutrition, eats "for two."
- If the baby grows quickly or is large, then the mother's belly can grow faster and be larger.
- Babies are located in the uterus in different ways. With some types of presentation, the stomach will be less noticeable, with others it will begin to grow earlier and will appear larger.

Feeling the belly
The belly of the expectant mother changes not only externally. From the 20th week of pregnancy, the mother begins to feel movements of the baby . At first, they look like light flutters, over time, the movements become more intense, because by the end of pregnancy, the mass and size of the child increase, and now it is not as spacious in the uterus as before. The number of movements gradually decreases, but their strength grows.
The movements of the crumbs, especially intense ones, can cause unpleasant sensations in a woman, especially in the right or left hypochondrium .
This is explained by the fact that during cephalic presentation (the baby is located in the uterus head down), the blows of the baby's legs are projected into the region of the mother's internal organs: the liver, stomach, intestines and spleen. Such sensations and even pains are natural and do not require treatment.
And sometimes pains appear in the lateral sections of the abdomen.
They occur due to the fact that during pregnancy the ligaments that support the uterus and ovaries are stretched.
In addition, changes occur in the fallopian tubes (they thicken, blood circulation increases in them), in the ovaries (they increase slightly in size, cyclic processes stop in them, and the position of the ovaries changes due to an increase in the size of the uterus). Slight pain in the lower abdomen may occur several times during the day, but, as a rule, they quickly disappear if the woman takes a position that is comfortable for her. Sometimes periodic discomfort in the lower lateral parts of the abdomen appear with constipation, which is also common in pregnant women: during pregnancy, hormones are produced that relax the uterus, they have a similar effect on the intestines: its peristalsis is disturbed, resulting in constipation.
The belly can be large or small, bulging forward or as if swollen, low or high - everything will depend on the individual characteristics of the pregnancy.
How the belly grows and looks during pregnancy depends on many factors: the physique of the woman, the structure of the pelvis, the condition of the muscles, the growth of the uterus and the baby, the amount of amniotic fluid.
Most often, the belly begins to grow after the 12th week of pregnancy, and others will be able to notice the woman's interesting position only from the 20th week. However, everything is strictly individual, there is absolutely no exact definition of the timing of the appearance of the abdomen, it is simply impossible to predict.
Don't be upset if the shape or size of your belly does not match the average, because everyone is different. Focus on your constitution, the work of your body and the development of the baby.
REFERENCE
At 4 weeks, the uterus reaches the size of a hen's egg.
Goose egg at 8 weeks.
At 12 weeks, the uterus reaches the upper edge of the pubic bone.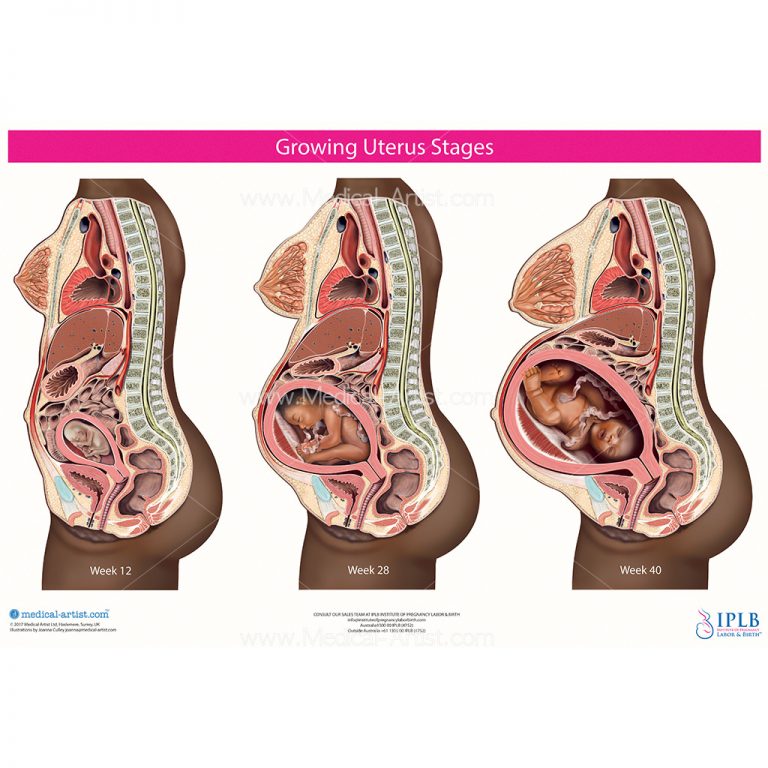 The belly is not visible yet.
The belly is not visible yet.
At 16 weeks, the abdomen is rounded, the uterus is in the middle of the distance between the pubis and the navel.
At 20 weeks, the abdomen is visible to others, the fundus of the uterus is 4 cm below the navel.
At 24 weeks, the fundus of the uterus is at the level of the navel.
At 28 weeks, the uterus is already above the navel.
At 32 weeks, the navel begins to smooth out. Abdominal circumference - 80-85 cm.
At 40 weeks, the navel protrudes noticeably. Abdominal circumference 96-98 cm
Make an appointment
to the doctor - Bagriy Alexander Tarasovich
Clinical Hospital "AVICENNA" Group of Companies "Mother and Child"
Anesthesiology and resuscitation
By clicking on the send button, I consent to the processing of personal data
Attention! Prices for services in different clinics may vary. To clarify the current cost, select a clinic
Clinical Hospital "AVICENNA" GC "Mother and Child"Novosibirsk Center for Reproductive Medicine
All directionsGynecological proceduresSpecialist consultations (adults)Specialist consultations (children)Laboratory of molecular geneticsGeneral clinical studiesProcedure roomTherapeutic studiesUltrasound examinations for adults
01.
Gynecological procedures
02.
Specialist consultations (adults)
03.
Specialist consultations (children)
04.
Laboratory of molecular genetics
05.
General studies
06.
Procedure cabinet
07.
Therapeutic studies
08.
08.
The administration of the clinic takes all measures to timely update the price list posted on the website, however, in order to avoid possible misunderstandings, we advise you to clarify the cost of services and the timing of the tests by calling
Changes in the cervix during pregnancy
Pregnancy is always pleasant, but sometimes not planned. And not all women have time to prepare for it, to be fully examined before its onset. And the detection of diseases of the cervix already during pregnancy can be an unpleasant discovery.
The cervix is the lower segment of the uterus in the form of a cylinder or cone.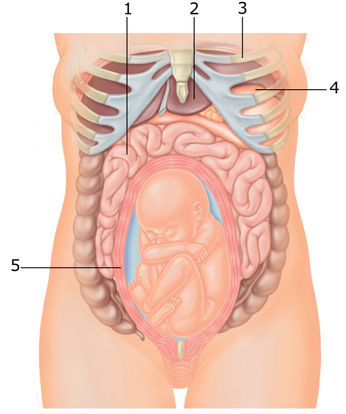 In the center is the cervical canal, one end of which opens into the uterine cavity, and the other into the vagina. On average, the length of the cervix is 3–4 cm, the diameter is about 2.5 cm, and the cervical canal is closed. The cervix has two parts: lower and upper. The lower part is called the vaginal, because it protrudes into the vaginal cavity, and the upper part is supravaginal, because it is located above the vagina. The cervix is connected to the vagina through the vaginal fornices. There is an anterior arch - short, posterior - deeper and two lateral ones. Inside the cervix passes the cervical canal, which opens into the uterine cavity with an internal pharynx, and is clogged with mucus from the side of the vagina. Mucus is normally impervious to infections and microbes, or to spermatozoa. But in the middle of the menstrual cycle, the mucus thins and becomes permeable to sperm.
In the center is the cervical canal, one end of which opens into the uterine cavity, and the other into the vagina. On average, the length of the cervix is 3–4 cm, the diameter is about 2.5 cm, and the cervical canal is closed. The cervix has two parts: lower and upper. The lower part is called the vaginal, because it protrudes into the vaginal cavity, and the upper part is supravaginal, because it is located above the vagina. The cervix is connected to the vagina through the vaginal fornices. There is an anterior arch - short, posterior - deeper and two lateral ones. Inside the cervix passes the cervical canal, which opens into the uterine cavity with an internal pharynx, and is clogged with mucus from the side of the vagina. Mucus is normally impervious to infections and microbes, or to spermatozoa. But in the middle of the menstrual cycle, the mucus thins and becomes permeable to sperm.
Outside, the surface of the cervix has a pinkish tint, it is smooth and shiny, durable, and from the inside it is bright pink, velvety and loose.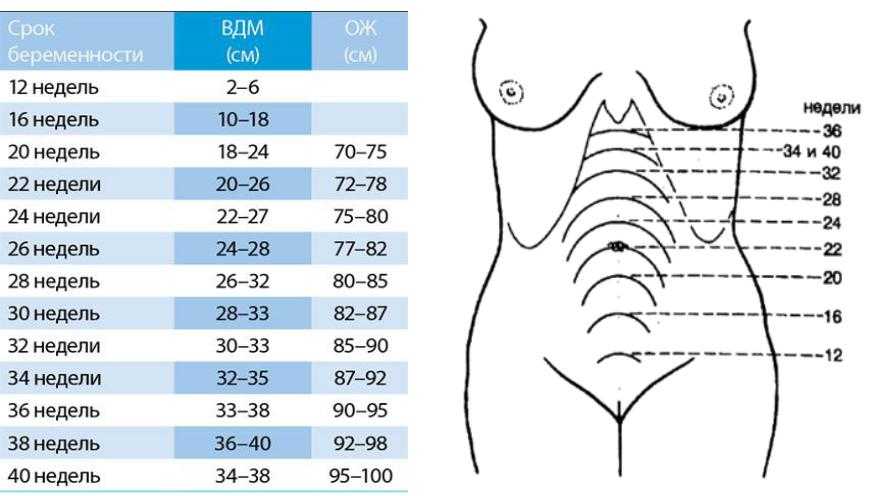
The cervix during pregnancy is an important organ, both in anatomical and functional terms. It must be remembered that it promotes the process of fertilization, prevents infection from entering the uterine cavity and appendages, helps to "endure" the baby and participates in childbirth. That is why regular monitoring of the condition of the cervix during pregnancy is simply necessary.
During pregnancy, a number of physiological changes occur in this organ. For example, a short time after fertilization, its color changes: it becomes cyanotic. The reason for this is the extensive vascular network and its blood supply. Due to the action of estriol and progesterone, the tissue of the cervix becomes soft. During pregnancy, the cervical glands expand and become more branched.
Screening examination of the cervix during pregnancy includes: cytological examination, smears for flora and detection of infections. Cytological examination is often the first key step in the examination of the cervix, since it allows to detect very early pathological changes that occur at the cellular level, including in the absence of visible changes in the cervical epithelium. The examination is carried out to identify the pathology of the cervix and the selection of pregnant women who need a more in-depth examination and appropriate treatment in the postpartum period. When conducting a screening examination, in addition to a doctor's examination, a colposcopy may be recommended. As you know, the cervix is covered with two types of epithelium: squamous stratified from the side of the vagina and single-layer cylindrical from the side of the cervical canal. Epithelial cells are constantly desquamated and end up in the lumen of the cervical canal and in the vagina. Their structural characteristics make it possible, when examined under a microscope, to distinguish healthy cells from atypical ones, including cancerous ones.
The examination is carried out to identify the pathology of the cervix and the selection of pregnant women who need a more in-depth examination and appropriate treatment in the postpartum period. When conducting a screening examination, in addition to a doctor's examination, a colposcopy may be recommended. As you know, the cervix is covered with two types of epithelium: squamous stratified from the side of the vagina and single-layer cylindrical from the side of the cervical canal. Epithelial cells are constantly desquamated and end up in the lumen of the cervical canal and in the vagina. Their structural characteristics make it possible, when examined under a microscope, to distinguish healthy cells from atypical ones, including cancerous ones.
During pregnancy, in addition to physiological changes in the cervix, some borderline and pathological processes may occur.
Under the influence of hormonal changes that occur in a woman's body during the menstrual cycle, cyclic changes also occur in the cells of the epithelium of the cervical canal.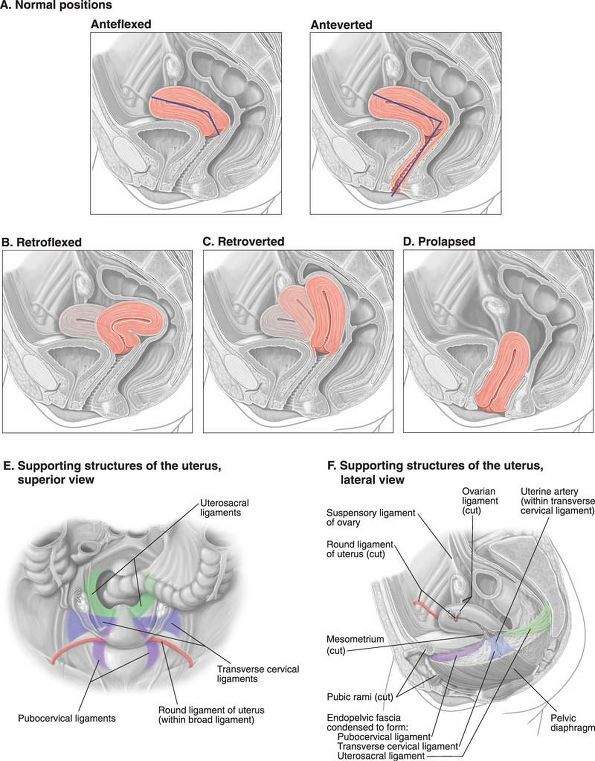 During the period of ovulation, the secretion of mucus by the glands of the cervical canal increases, and its qualitative characteristics change. With injuries or inflammatory lesions, sometimes the glands of the cervix can become clogged, a secret accumulates in them and cysts form - Naboth follicles or Naboth gland cysts that have been asymptomatic for many years. Small cysts do not require any treatment. And pregnancy, as a rule, is not affected. Only large cysts that strongly deform the cervix and continue to grow may require opening and evacuation of the contents. However, this is very rare and usually requires monitoring during pregnancy.
During the period of ovulation, the secretion of mucus by the glands of the cervical canal increases, and its qualitative characteristics change. With injuries or inflammatory lesions, sometimes the glands of the cervix can become clogged, a secret accumulates in them and cysts form - Naboth follicles or Naboth gland cysts that have been asymptomatic for many years. Small cysts do not require any treatment. And pregnancy, as a rule, is not affected. Only large cysts that strongly deform the cervix and continue to grow may require opening and evacuation of the contents. However, this is very rare and usually requires monitoring during pregnancy.
Quite often, in pregnant women, during a mirror examination of the vaginal part, polyps cervix. The occurrence of polyps is most often associated with a chronic inflammatory process. As a result, a focal proliferation of the mucosa is formed, sometimes with the involvement of muscle tissue and the formation of a pedicle. They are mostly asymptomatic. Sometimes they are a source of blood discharge from the genital tract, more often of contact origin (after sexual intercourse or defecation). The size of the polyp is different - from millet grain rarely to the size of a walnut, their shape also varies. Polyps are single and multiple, their stalk is located either at the edge of the external pharynx, or goes deep into the cervical canal. Sometimes during pregnancy there is an increase in the size of the polyp, in some cases quite fast. Rarely, polyps first appear during pregnancy. The presence of a polyp is always a potential threat of miscarriage, primarily because it creates favorable conditions for ascending infection. Therefore, as a rule, more frequent monitoring of the cervix follows. The tendency to trauma, bleeding, the presence of signs of tissue necrosis and decay, as well as questionable secretions require special attention and control. Treatment of cervical polyps is only surgical and during pregnancy, in most cases, treatment is postponed until the postpartum period, since even large polyps do not interfere with childbirth.
They are mostly asymptomatic. Sometimes they are a source of blood discharge from the genital tract, more often of contact origin (after sexual intercourse or defecation). The size of the polyp is different - from millet grain rarely to the size of a walnut, their shape also varies. Polyps are single and multiple, their stalk is located either at the edge of the external pharynx, or goes deep into the cervical canal. Sometimes during pregnancy there is an increase in the size of the polyp, in some cases quite fast. Rarely, polyps first appear during pregnancy. The presence of a polyp is always a potential threat of miscarriage, primarily because it creates favorable conditions for ascending infection. Therefore, as a rule, more frequent monitoring of the cervix follows. The tendency to trauma, bleeding, the presence of signs of tissue necrosis and decay, as well as questionable secretions require special attention and control. Treatment of cervical polyps is only surgical and during pregnancy, in most cases, treatment is postponed until the postpartum period, since even large polyps do not interfere with childbirth.
The most common pathology of the cervix in women is erosion . Erosion is a defect in the mucous membrane. True erosion is not very common. The most common pseudo-erosion (ectopia) is a pathological lesion of the cervical mucosa, in which the usual flat stratified epithelium of the outer part of the cervix is replaced by cylindrical cells from the cervical canal. Often this happens as a result of mechanical action: with frequent and rough sexual intercourse, desquamation of the stratified squamous epithelium occurs. Erosion is a multifactorial disease. The reasons may be:
- genital infections, vaginal dysbacteriosis and inflammatory diseases of the female genital area;
- is an early onset of sexual activity and a frequent change of sexual partners. The mucous membrane of the female genital organs finally matures by the age of 20-23. If an infection interferes with this delicate process, erosion is practically unavoidable;
- is a cervical injury.
 The main cause of such injuries is, of course, childbirth and abortion;
The main cause of such injuries is, of course, childbirth and abortion; - hormonal disorders;
- , cervical pathology may also occur with a decrease in the protective functions of immunity.
The presence of erosion does not affect pregnancy in any way, as well as pregnancy on erosion. Treatment during pregnancy consists in the use of general and local anti-inflammatory drugs for inflammatory diseases of the vagina and cervix. And in most cases, just dynamic observation is enough. Surgical treatment is not carried out throughout the entire pregnancy, since the excess of risks and benefits is significant, and after treatment during childbirth, there may be problems with opening the cervix.
Almost all women with various diseases of the cervix safely bear and happily give birth to beautiful babies!
Attention! Prices for services in different clinics may vary. To clarify the current cost, select a clinic
Clinical Hospital of IDKClinic "Mother and Child" Entuziastov Samara
All directionsSpecialist consultations (adults)Specialist consultations (children's)Laboratory of molecular geneticsGeneral clinical examinationsProcedural roomOther gynecological operationsTelemedicine for adultsTherapeutic examinationsUltrasound examinations for adults
01.