How do you get strep b during pregnancy
Group B Strep and pregnancy
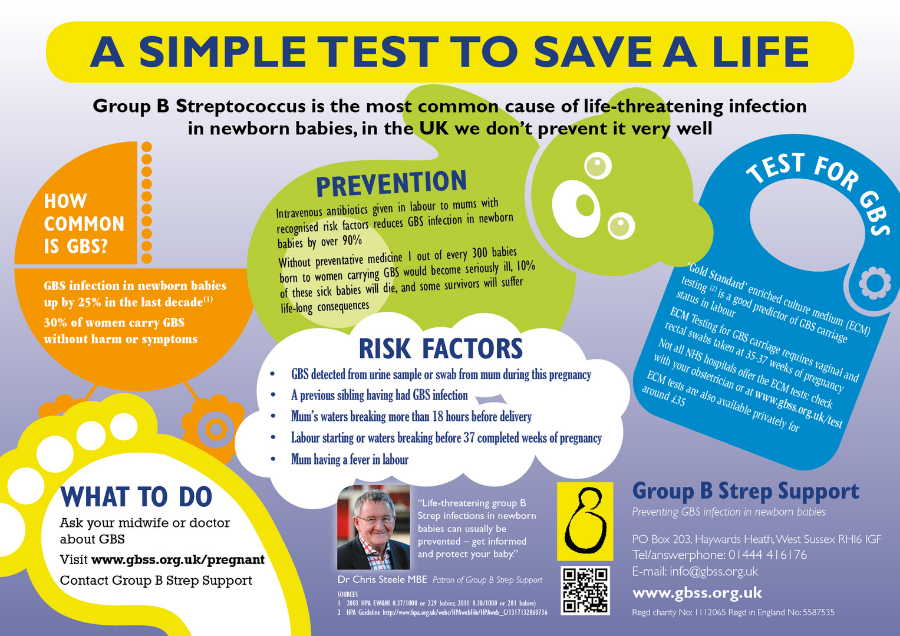
Group B Streptococcus (Group B Strep, Strep B, Beta Strep, or GBS) is a type of bacteria which lives in the intestines, rectum and vagina of around 2-4 in every 10 women in the UK (20-40%). This is often referred to as ‘carrying’ or being ‘colonised with’ GBS.
Group B Strep is not a sexually transmitted disease. Most women carrying GBS will have no symptoms. Carrying GBS is not harmful to you, but it can affect your baby around the time of birth.
GBS can occasionally cause serious infection in young babies and, very rarely, during pregnancy before labour.
Key points
- Group B Strep is one of the many bacteria that normally live in our bodies and which usually cause no harm
- Testing for GBS is not routinely offered to all pregnant women in the UK
- If you carry GBS, most of the time your baby will be born safely and will not develop an infection. However, it can rarely cause serious infection such as sepsis, pneumonia or meningitis
- Most early-onset GBS infections (those developing in the first week of life) are preventable
- If GBS is found in your urine, vagina or rectum (bowel) during your current pregnancy, or if you have previously had a baby affected by GBS infection, you should be offered antibiotics in labour to reduce the small risk of this infection to your baby.
- If GBS was found in a previous pregnancy and your baby was unaffected, you can have a specific swab test (known as the ECM test) to see whether you are carrying GBS when you are 35-37 weeks pregnant. If the test result is positive, you will be offered antibiotics in labour. If the ECM test result is negative at this point, then the risk of your baby developing early-onset GBS infection is low and you may choose not to have antibiotics.
- The risk of your baby becoming unwell with GBS infection is increased if your baby is born preterm, if you have a temperature while you are in labour, or if your waters break before you go into labour
- If your newborn baby develops signs of GBS infection, they should be treated with antibiotics straight away
The information below is for you, a friend or a relative who is expecting a baby, planning to become pregnant or has recently had a baby.
FIND OUT HOW TO ORDER AN ECM TEST FOR GBS
WHERE TO Order your GBS test
How do people become carriers of group B Strep?
Like many bacteria, GBS may be passed from one person to another through skin-to-skin contact, for example, hand contact, kissing, close physical contact, etc. As GBS is often found in the vagina and rectum of colonised women, it can be passed through sexual contact.
As GBS is often found in the vagina and rectum of colonised women, it can be passed through sexual contact.
There are no known harmful effects of carriage itself and the GBS bacteria do not cause genital symptoms or discomfort. GBS carriage is not a sexually transmitted disease, nor is GBS carriage a sign of ill health or poor hygiene.
No-one should ever feel guilty or dirty for carrying GBS – it’s normal. Around 20-40% of women carry GBS.
GBS may be passed from one person to another by skin-to-skin contact. Everyone (regardless of whether they know they carry GBS) should wash their hands properly and dry them properly before handling a newborn baby.
How is group B Strep found?Most women carrying GBS have no symptoms, so GBS is often found by chance through a vaginal or rectal swab test or a urine test.
The NHS does not routinely test all pregnant women for group B Strep.
Tests designed specifically to find GBS carriage, known as the Enriched Culture Medium (ECM) test, are increasingly becoming available within the NHS and are widely available privately.
Since September 2017, the Royal College of Obstetricians & Gynaecologists (RCOG) has recommended in their guideline on group B Strep that selected pregnant women should be offered the ECM test. Many maternity units still use a standard test that misses up to half of the women carrying group B Strep, so ask your health professionals what is available locally.
There are private home ECM testing kits for GBS carriage you can order.
What could group B Strep mean for my baby?Many babies come into contact with group B Strep during labour, or around or after birth and the vast majority will not become ill.
However, there is a small chance that your newborn baby will develop group B Strep infection and become seriously ill, or even die, and this chance is increased if you are carrying GBS.
The infections that group B Strep most commonly causes in newborn babies are sepsis (infection of the blood), pneumonia (infection in the lungs), and meningitis (infection of the fluid and lining around the brain).
Around 1 in every 1750 babies in the UK and Ireland is diagnosed with early-onset group B Strep infection (developing in babies aged 0-6 days).
Around 1 in every 2700 babies in the UK and Ireland is diagnosed with late-onset group B Strep infection (developing in babies aged 7-90 days).
Although group B Strep infection can make your baby very unwell, with prompt treatment most babies will recover fully.
Of the babies who develop GBS infection, 1 in 19 (5.2%) will die from early-onset GBS infection and 1 in 13 (7.7%) from late-onset GBS infection. Of those who survive their GBS infection, 1 in 14 (7.4%) will have a long-term disability following early-onset GBS infection and 1 in 8 (12.4%) following late-onset GBS infection.
On average in the UK and Republic of Ireland, every month
- 66 babies are diagnosed with group B Strep infection
- 40 early-onset + 26 late-onset GBS infection
- 56 babies make a full recovery
- 35 early-onset + 21 late-onset GBS infection
- 6 babies survive with long-term physical or mental disabilities
- 3 early-onset + 3 late-onset GBS infection
- 4 babies die from their group B Strep infection
- 2 early-onset + 2 late-onset GBS infection
Any baby can develop a group B Strep infection, but early-onset group B Strep infection (developing in the first 6 days of life, and usually on the first day of life) is more likely if:
- your baby is born preterm (before 37 weeks of pregnancy) – the earlier your baby is born, the greater the risk
- you have previously had a baby who developed a group B Strep infection
- you have had a high temperature (or other signs of infection) during labour
- you have had any group B Strep positive urine or swab test in this pregnancy
- your waters have broken more than 24 hours before your baby is born
Late-onset group B Strep infection (developing in babies aged 7-90 days) is less common than early-onset GBS infection and is more likely if:
- your baby is born preterm (before 37 weeks of pregnancy)
- you have had group B Strep positive test in this pregnancy
Most early-onset group B Strep infection can be prevented by giving intravenous antibiotics in labour to women whose babies are at raised risk of developing the infection.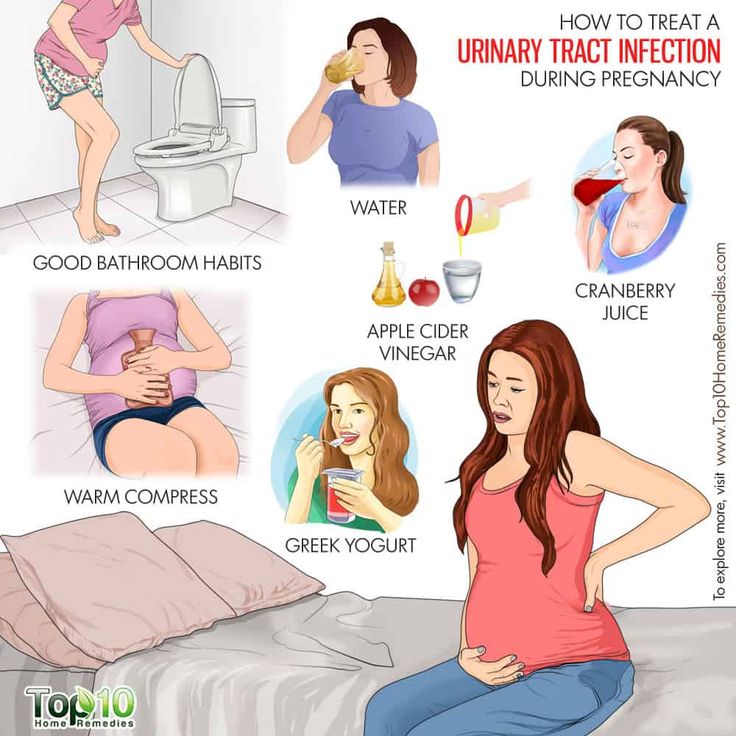 At present, there are no known methods to prevent late-onset GBS infection.
At present, there are no known methods to prevent late-onset GBS infection.
- A urine infection caused by group B Strep should be treated with antibiotic tablets straight away and you should also be offered intravenous (IV) antibiotics during labour.
- You should be offered IV antibiotics during labour if you have had a GBS-positive swab or urine test from an NHS or other accredited laboratories (see www.gbss.org.uk/test).
- If you have previously had a baby who was diagnosed with GBS infection, you should be offered IV antibiotics when you are in labour.
- If GBS was found in a previous pregnancy and your baby was unaffected, you can have a specific swab test (known as the ECM test) to see whether you are carrying GBS when you are 35-37 weeks pregnant. If the test result is positive, you will be offered antibiotics in labour. If the ECM test result is negative at this point, then the risk of your baby developing early-onset GBS infection is low and you may choose not to have antibiotics.
- If your waters break after 37 weeks of your pregnancy and you are known to carry GBS, you will be offered induction of labour straight away. This is to reduce the time that your baby is exposed to GBS before birth. You should also be offered IV antibiotics.
- Even if you are not known to carry GBS, if you develop any signs of infection in labour, you will be offered IV antibiotics that will treat a wide range of infections including GBS.
- If your labour starts before 37 weeks of your pregnancy, your healthcare professional will recommend that you have IV antibiotics even if you are not known to carry GBS.
At present, there are no known methods to prevent late-onset GBS infection, so knowledge of the typical signs of infection is vital.
If you are worried about your baby, you should urgently contact your healthcare professional and mention any history of GBS when you do.
Download a copy of this leaflet
If you have any questions about Group B Strep, please call our helpline
Mon-Fri 9am-5pm
0330 120 0796
Or email us at info@gbss. org.uk
org.uk
Related pages
Where to order a group B Strep test
What does my test result mean?
After your baby is born
Group B Strep In Pregnancy: Test, Risks & Treatment
Overview
What is group B strep?
Group B strep infection (also GBS or group B Streptococcus) is caused by bacteria typically found in a person's vagina or rectal area. About 25% of pregnant people have GBS, but don't know it because it doesn't cause symptoms. A pregnant person with GBS can pass the bacteria to their baby during vaginal delivery. Infants, older adults or people with a weakened or underdeveloped immune system are more likely to develop complications from group B strep.
Most newborns who get GBS don't become sick. However, the bacteria can cause severe and even life-threatening infections in a small percentage of newborns. Healthcare providers screen for group B strep as part of your routine prenatal care. If you test positive, your provider will treat you with antibiotics.
If you test positive, your provider will treat you with antibiotics.
How do you get group B strep?
GBS bacteria naturally occur in areas of your body like your intestines and genital and urinary tracts. Adults can't get it from person-to-person contact or from sharing food or drinks with an infected person. Experts aren't entirely sure why the bacteria spreads, but they know that it’s potentially harmful in babies and people with weakened immune systems.
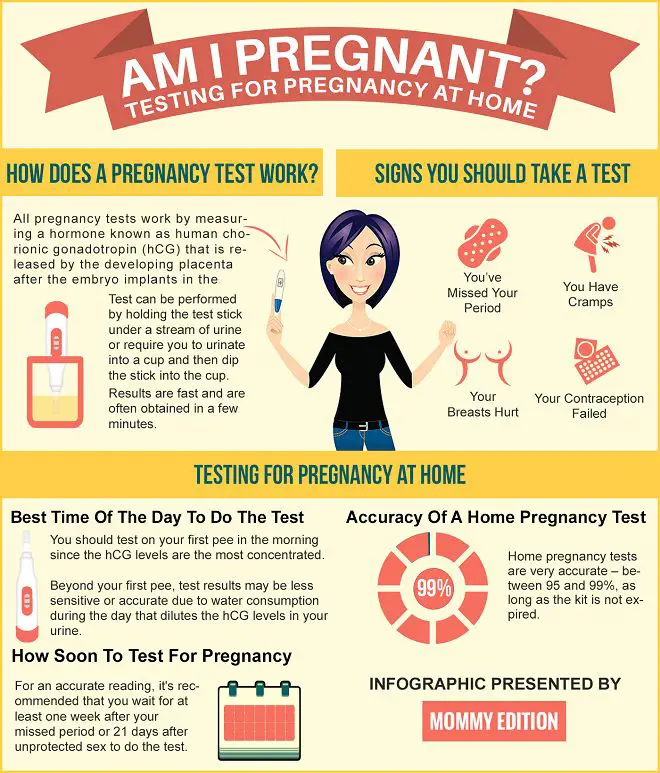
When do you get tested for group B strep?
The Centers for Disease Control and Prevention (CDC) recommends routine screening for group B strep in all pregnancies. You're screened for GBS between 36 and 37 weeks of pregnancy. Group B strep testing involves your provider taking a swab of your vagina and rectum and then sending it to a lab for analysis.
Can Group B strep affect a developing fetus?
GBS doesn't affect the fetus baby while it's still inside your uterus. However, your baby can get GBS from you during labor and delivery. Taking antibiotics for GBS reduces your chances of passing it to your baby.
Taking antibiotics for GBS reduces your chances of passing it to your baby.
How does a baby get GBS?
There are two main types of Group B strep in babies:
- Early-onset infection: Most (75%) babies with GBS become infected in the first week of life. GBS infection is usually apparent within a few hours after birth. Premature babies face greater risk if they become infected, but most babies who get GBS are full-term.
- Late-onset infection: GBS infection can also occur in infants one week to three months after birth. Late-onset infection is less common and is less likely to result in a baby's death than early-onset infection.
How common is GBS?
Group B strep screening during pregnancy has decreased the number of cases. According to the CDC, about 930 babies get early-onset GBS, and 1,050 get late-onset GBS. About 4% of babies who develop GBS will die from it.
Symptoms and Causes
What are the symptoms of group B strep?
Most adults don't experience symptoms of group B strep. It can cause symptoms in older people or people with certain medical conditions, but this is rare. These symptoms include:
It can cause symptoms in older people or people with certain medical conditions, but this is rare. These symptoms include:
- Fever, chills and fatigue.
- Difficulty breathing.
- Chest pains.
- Muscle stiffness.
Newborns with GBS have symptoms like:
- Fever.
- Difficulty feeding.
- Irritability.
- Breathing difficulties.
- Lack of energy.
These symptoms can become serious quickly because newborns lack immunity. Group B strep infection can lead to severe problems like sepsis, pneumonia and meningitis in infants.
Can I pass group B strep to my partner?
Other people that live with you, including other children, aren't at risk of getting sick.
Diagnosis and Tests
Will I be tested for group B strep?
Yes, your healthcare provider will test you for GBS late in your pregnancy, around weeks 36 to 37.
Your obstetrician uses a cotton swab to obtain samples of cells from your vagina and rectum.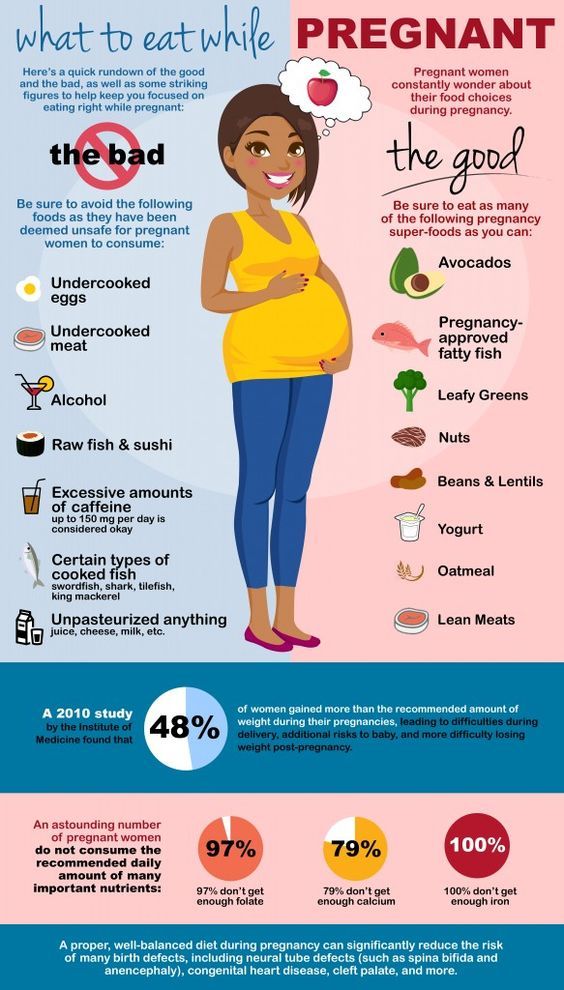 This test doesn't hurt and takes less than a minute. Then, the sample is sent to a lab where it's analyzed for group B strep. Most people receive their results within 48 hours. A positive culture result means you're a GBS carrier, but it doesn't mean that you or your baby will become sick.
This test doesn't hurt and takes less than a minute. Then, the sample is sent to a lab where it's analyzed for group B strep. Most people receive their results within 48 hours. A positive culture result means you're a GBS carrier, but it doesn't mean that you or your baby will become sick.
If you’re using a midwife, you might be given instructions on how to test yourself at home and submit the swab to a lab.
Is Group B strep an STI?
No, group B strep isn't an STI (sexually transmitted infection). The type of bacteria that causes GBS naturally lives in your vagina or rectum. It doesn't cause symptoms for most people.
Management and Treatment
What happens if you test positive for group B strep during pregnancy?
Healthcare providers prevent GBS infection in your baby by treating you with intravenous (IV) antibiotics during labor and delivery. The most common antibiotic to treat group B strep is penicillin or ampicillin. Giving you an antibiotic at this time helps prevent the spread of GBS from you to your newborn. It's not effective to treat GBS earlier than at delivery. The antibiotics work best when given at least four hours before delivery. About 90% of infections are prevented with this type of treatment.
It's not effective to treat GBS earlier than at delivery. The antibiotics work best when given at least four hours before delivery. About 90% of infections are prevented with this type of treatment.
One exception to the timing of treatment is when GBS is detected in urine. When this is the case, oral antibiotic treatment begins when GBS is identified (regardless of the stage of pregnancy). Antibiotics should still be given through an IV during labor.
Any pregnant person who has previously given birth to a baby who developed a GBS infection or who has had a urinary tract infection in this pregnancy caused by GBS will also be treated during labor.
How is group B strep treated in newborns?
Some babies still get GBS infections despite testing and antibiotic treatment during labor. Healthcare providers might take a sample of the baby's blood or spinal fluid to see if the baby has GBS infection. If your baby has GBS, they're treated with antibiotics through an IV.
Prevention
How can I reduce my risk of group B strep?
Anyone can get GBS. Some people are at higher risk due to certain medical conditions or age. The following factors increase your risk for having a baby born with group B strep:
Some people are at higher risk due to certain medical conditions or age. The following factors increase your risk for having a baby born with group B strep:
- You tested positive for GBS.
- You develop a fever during labor.
- More than 18 hours pass between your water breaking and your baby being born.
- You have medical conditions like diabetes, heart disease or cancer.
Getting screened for GBS and taking antibiotics (if you're positive) is the best way to protect your baby from infection.
Outlook / Prognosis
What are long term problems of Group B strep in newborns?
Infants with GBS can develop meningitis, pneumonia or sepsis. These illnesses can be life-threatening. Most infants don't develop any long-term issues; however, about 25% of babies with meningitis caused by GBS develop cerebral palsy, hearing problems, learning disabilities or seizures.
Can I get tested for group B strep again?
No, once you test positive for GBS, you're considered positive for the rest of your pregnancy.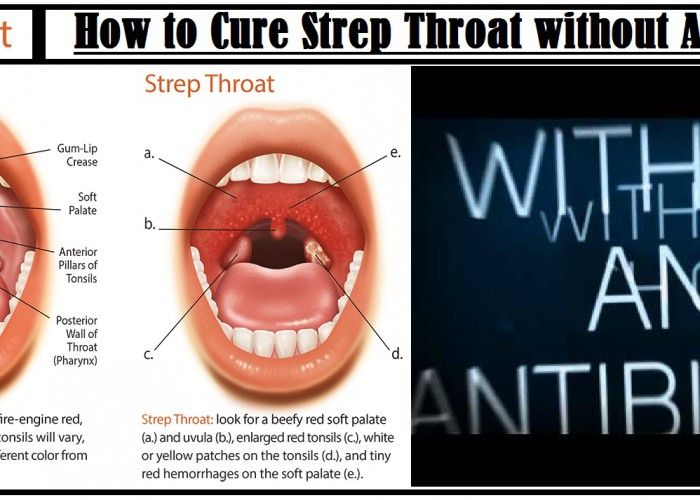 You will not get re-tested.
You will not get re-tested.
Do I need treated for group B strep if I am having a c-section?
No, you don't need antibiotics if you're having a c-section delivery. However, you'll still be tested for GBS because labor could start before your scheduled c-section. If your water breaks and you're GBS positive, your baby is at risk of contracting the disease.
Living With
When should I see my healthcare provider if I’m positive for group B strep?
In some cases, GBS causes infections during pregnancy. Symptoms of infection include fever, pain and increased heart rate. Let your provider know if you have any of those symptoms as it could lead to preterm labor.
GBS can also cause urinary tract infection (UTI), which requires oral antibiotics.
Talk to your provider about what you can expect during labor and delivery if you have group B strep.
A note from Cleveland Clinic
Try not to panic if your healthcare provider tells you you're positive for group B strep during pregnancy.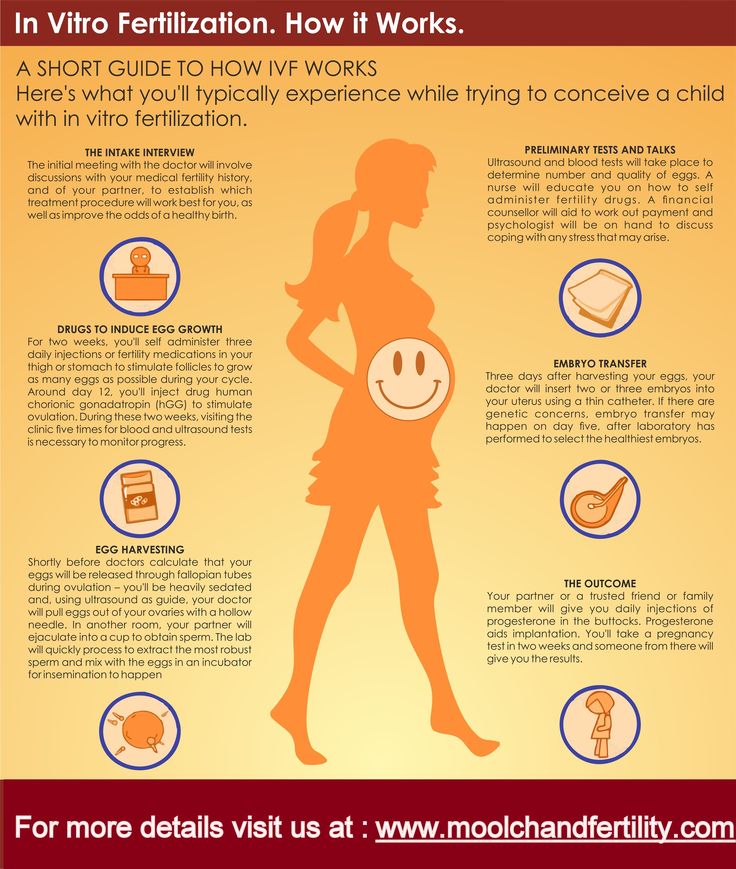 It's caused by bacteria that occur naturally in your body, not by anything you did wrong. The chances of you passing group B strep to your baby are quite low, especially if you take antibiotics during labor. Talk to your provider about group B strep and share any concerns you have. In most cases, testing positive for GBS causes no problems, and your baby is healthy.
It's caused by bacteria that occur naturally in your body, not by anything you did wrong. The chances of you passing group B strep to your baby are quite low, especially if you take antibiotics during labor. Talk to your provider about group B strep and share any concerns you have. In most cases, testing positive for GBS causes no problems, and your baby is healthy.
Infections during pregnancy. Detection of group B streptococcus
05/16/2017
Infections during pregnancy that can be transmitted from mother to fetus deserve great attention, as they carry a potential risk of infection of the fetus or newborn and may lead to undesirable consequences. In addition, the diagnosis of infections during pregnancy has certain characteristics due to the asymptomatic course of most maternal infections or non-specific signs and symptoms.
Group B Streptococcus (GBS, Streptococcus agalactiae ) - Causes severe neonatal illness and poses a risk to certain patients in other age groups.
It has been estimated that GBS in 30% of pregnant women can be found in the vagina and often in the urethra of their sexual partners. Despite the fact that GBS can occur as part of the normal intestinal microflora of a woman, their colonization of the urogenital tract of a pregnant woman poses a significant risk to the fetus due to the possibility of ascending infection. There is a significant relationship between the carriage of GBS in the vagina, not only with early infection of newborns (sepsis, pneumonia and meningitis), but also with premature birth, premature discharge of amniotic fluid, urinary infection in pregnant women, development of chorioamnionitis during childbirth, endometritis.
In the USA, Canada and European countries, regulated National programs for the prevention and treatment of GBS infections have been adopted, which are mandatory for all medical institutions.
From 01.05.17, DILA ML introduces a new study “Identification of group B streptococcus (streptococcus agalactiae) with sensitivity to antibiotics”.
| Prompt identification of pregnant women who are positive for group B streptococcus and who have risk factors for an increased chance of infection in the newborn allows to conduct intravenous antibiotic prophylaxis with the onset of labor and prevent early infection of the newborn with group B streptococcus:
|
Rules for preparation : 24 hours before the use of intravaginal and rectal medications should be excluded, before taking the biomaterial, do not wash the external genital organs.
The biomaterial is taken from two points: the lower third of the vagina and the next - the rectum, the overall result is evaluated.
Detection of group B streptococcus is carried out by a cultural method with the determination of sensitivity to antibiotics.
Research period: 6 days (Kyiv), 7.5 days (Regions).
Adequate assessment of the risk of infection of the newborn with group B streptococcus will significantly reduce the possibility of complications and ensure a favorable pregnancy outcome.
Literature:
1. Australasian society for infectious diseases, 2014
2. Antibiotic Prevention for Maternal Group B Streptococcal Colonization on Neonatal GBS-Related Adverse Outcomes: A Meta-Analysis, Shunming Li, Jingya Huang, 2017.
3. Early onset Group B Streptococcal disease Queensland clinical guidelines, 2016
4. Effect of group B streptococci colonizing the urogenital tract of pregnant women on the course and outcome of pregnancy / Oganyan K. A., Zatsiorskaya S.L., Arzhanova O.N., Savicheva A.M. – St. Petersburg, 2014
A., Zatsiorskaya S.L., Arzhanova O.N., Savicheva A.M. – St. Petersburg, 2014
5. Digest of professional medical information. Congenital and perinatal infections: prevention, diagnosis and treatment. / Catherine S. Peckham. - No. 1 (4). – 2008.
0 0
Rate satisfaction
DILA for you
Clinical consulting service for clinical support of doctors and patients before visiting a doctor
0-800-600-911
Strept. Agalactiae (group B streptococci) (determination in the material by PCR)
Article: 00162
Cost of analysis
in the online store: 7% discount!
Plain
577 rublesLab:
Regular
620 rubles
the price does not include the cost of taking biological material
Add to Basket
Analysis results ready
Regular*: 1-2 working days
Analysis submission date:
Completion date:
*not counting the day of delivery, see rules.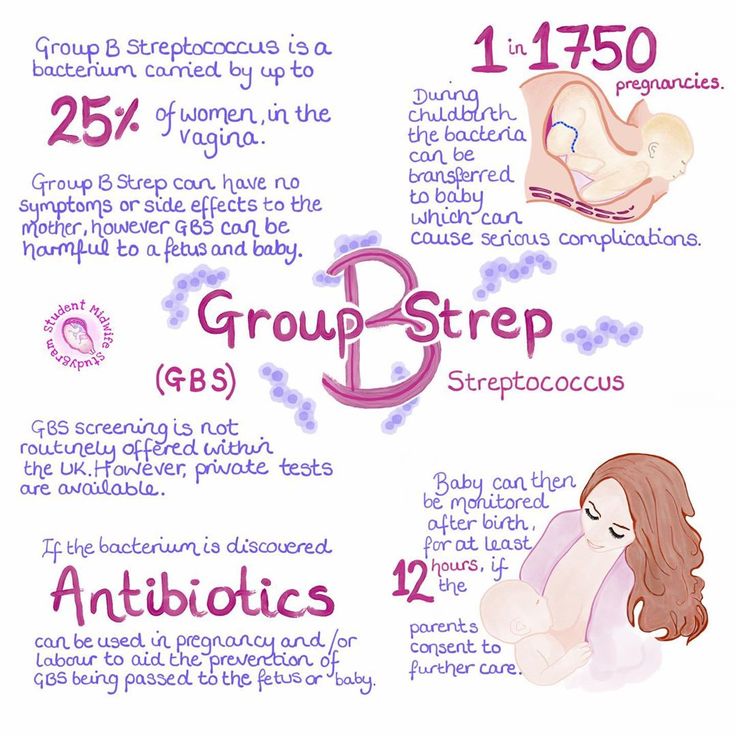
Where and when you can rent
- Buninskaya alley
- Voykovskaya
- Dubrovka
- Maryino
- Novokuznetskaya
- Podolsk
- Weekdays: from 7.45 to 21.00
- Weekends: from 8.45 to 17.00
Changes in work schedule
Preparation for analysis
General recommendations for testing
For women: Give after menstruation. Sexual life, douching, vaginal showers, the use of tampons, suppositories and other local preparations are prohibited for 24 hours. It is advisable not to take a bath. Only the external toilet of the genitals is allowed. It is advisable to take smears for infections and crops no earlier than 3 weeks after taking antibiotics (for any reason). This does not apply to the diagnosis of viral infections. For men: Do not urinate for 1.5-2 hours. It is advisable to take smears for infections and crops no earlier than 3 weeks after taking antibiotics (for any reason). This does not apply to the diagnosis of viral infections.
This does not apply to the diagnosis of viral infections.
Biomaterial sampling
- Swab sampling
Methods and tests
PCR (polymerase chain reaction). Qualitative
Files
Download a sample of the result of the analysis
What is it for
Group B streptococci (Streptococcus agalactiae) are bacteria found in the lower intestines of 10-35% of healthy men and in the vagina and/or lower intestines of 10-35% of healthy women. These bacteria are a normal part of the human microflora. Although group B streptococcus is generally safe for adults, it can cause serious complications during pregnancy and severe illness in newborns. Also, group B streptococcus can affect people with a weakened immune system, chronic diseases, and the elderly.
How can a newborn become infected with streptococcus
Most infections occur during childbirth. Possible infection with premature rupture of the membranes. It is possible that infection can also occur through intact fetal membranes.
Possible infection with premature rupture of the membranes. It is possible that infection can also occur through intact fetal membranes.
Risk factors for streptococcal infection
- presence of streptococcus on examination in vaginal discharge or urine;
- rupture of membranes;
- fever during labor;
- maternal age less than 20 years;
- streptococcal infection of the newborn in past births.
Streptococcal infection can threaten a newborn
First of all, infection with streptococcus is dangerous not for the mother, but for the baby.
- Inflammation of the lungs (pneumonia)
- Inflammation of the meninges - meningitis
- Streptococci may cause septic complications
- If infected before delivery, may cause premature birth, miscarriage, stillbirth.
What disorders can be caused by group B streptococcus in a pregnant woman and after childbirth
Usually streptococcus does not affect healthy adults, however, in rare cases, it can cause infectious complications in a pregnant woman:
- Urinary tract infection
- Infection of the placenta and amniotic fluid (chorioamnionitis)
- Bacteremia (circulation of bacteria in the blood)
- Terrible complication - sepsis
- Rarely, after childbirth, streptococcus can cause inflammation and infection of the lining of the uterine cavity - endometritis
- Streptococcus can cause wound infection in women after caesarean section
Should pregnant women be tested?
The first examination is desirable to be done in the first trimester of pregnancy, especially if there have been miscarriages or premature births in the past. It is advisable to re-examine at 35-37 weeks of pregnancy.
It is advisable to re-examine at 35-37 weeks of pregnancy.
Testing is also recommended for elective caesarean section, even though the baby is not in contact with the birth canal.
How to test for streptococcus
Preliminary preparation for the delivery of the analysis is not required. An analysis for group B streptococcus is taken from the vagina with a special swab, which is placed in the environment and then analyzed in the laboratory by PCR.
What to do with the results of the analysis
If the test is negative, no action is required.
If you test positive for group B streptococcus, it does not mean that you or your child will definitely get sick. But the risk of infection in this case is higher. To prevent diseases of the child during childbirth or in case of premature outflow of water, antibiotics are prescribed prophylactically.