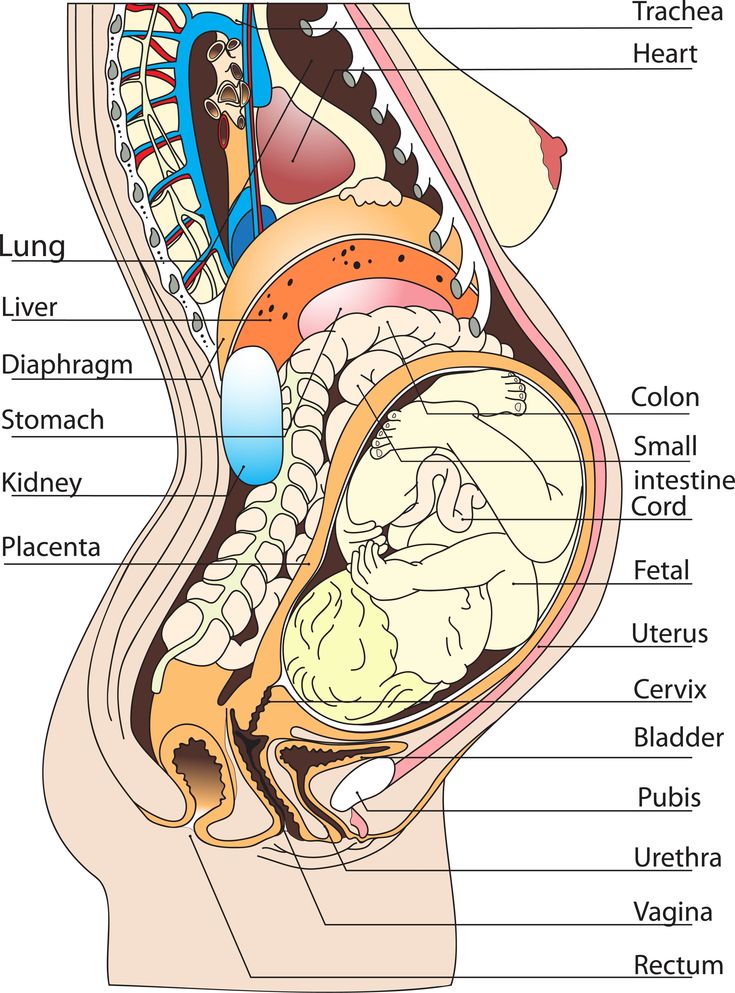
Female pregnant body diagram
Anatomy of pregnancy and birth - uterus
Anatomy of pregnancy and birth - uterus | Pregnancy Birth and Baby beginning of content5-minute read
Listen
What does the uterus look like?
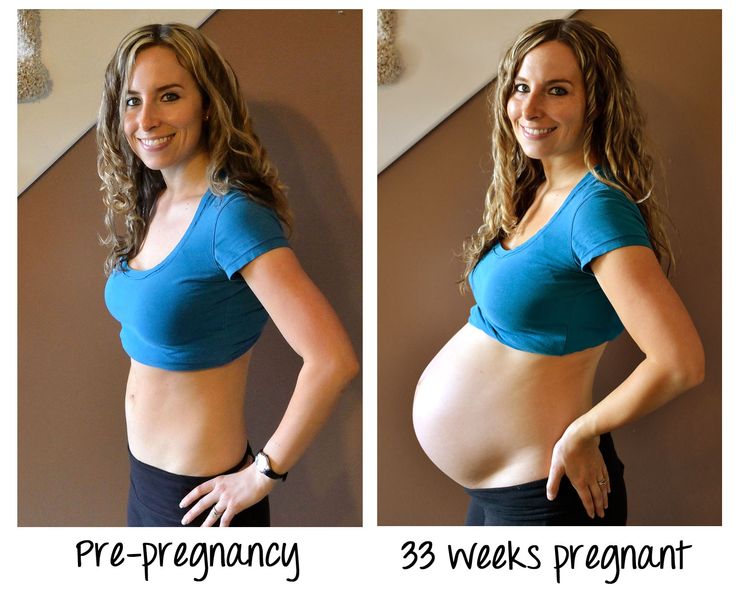
One of the most recognised changes in a pregnant woman’s body is the appearance of the ‘baby bump’, which forms to accommodate the baby growing in the uterus. The primary function of the uterus during pregnancy is to house and nurture your growing baby, so it is important to understand its structure and function, and what changes you can expect the uterus to undergo during pregnancy.
The uterus (also known as the ‘womb’) has a thick muscular wall and is pear shaped. It is made up of the fundus (at the top of the uterus), the main body (called the corpus), and the cervix (the lower part of the uterus ). Ligaments – which are tough, flexible tissue – hold it in position in the middle of the pelvis, behind the bladder, and in front of the rectum.
The uterus wall is made up of 3 layers. The inside is a thin layer called the endometrium, which responds to hormones – the shedding of this layer causes menstrual bleeding. The middle layer is a muscular wall. The outside layer of the uterus is a thin layer of cells.
Illustration showing the female reproductive system.The size of a non-pregnant woman's uterus can vary. In a woman who has never been pregnant, the average length of the uterus is about 7 centimetres. This increases in size to approximately 9 centimetres in a woman who is not pregnant but has been pregnant before. The size and shape of the uterus can change with the number of pregnancies and with age.
How does the uterus change during pregnancy?
During pregnancy, as the baby grows, the size of a woman’s uterus will dramatically increase. One measure to estimate growth is the fundal height, the distance from the pubic bone to the top of the uterus. Your doctor (GP) or obstetrician or midwife will measure your fundal height at each antenatal visit from 24 weeks onwards. If there are concerns about your baby’s growth, your doctor or midwife may recommend using regular ultrasound to monitor the baby.
Your doctor (GP) or obstetrician or midwife will measure your fundal height at each antenatal visit from 24 weeks onwards. If there are concerns about your baby’s growth, your doctor or midwife may recommend using regular ultrasound to monitor the baby.
Fundal height can vary from person to person, and many factors can affect the size of a pregnant woman’s uterus. For instance, the fundal height may be different in women who are carrying more than one baby, who are overweight or obese, or who have certain medical conditions. A full bladder will also affect fundal height measurement, so it’s important to empty your bladder before each measurement. A smaller than expected fundal height could be a sign that the baby is growing slowly or that there is too little amniotic fluid. If so, this will be monitored carefully by your doctor. In contrast, a larger than expected fundal height could mean that the baby is larger than average and this may also need monitoring.
As the uterus grows, it can put pressure on the other organs of the pregnant woman's body. For instance, the uterus can press on the nearby bladder, increasing the need to urinate.
For instance, the uterus can press on the nearby bladder, increasing the need to urinate.
How does the uterus prepare for labour and birth?
Braxton Hicks contractions, also known as 'false labour' or 'practice contractions', prepare your uterus for the birth and may start as early as mid-way through your pregnancy, and continuing right through to the birth. Braxton Hicks contractions tend to be irregular and while they are not generally painful, they can be uncomfortable and get progressively stronger through the pregnancy.
During true labour, the muscles of the uterus contract to help your baby move down into the birth canal. Labour contractions start like a wave and build in intensity, moving from the top of the uterus right down to the cervix. Your uterus will feel tight during the contraction, but between contractions, the pain will ease off and allow you to rest before the next one builds. Unlike Braxton Hicks, labour contractions become stronger, more regular and more frequent in the lead up to the birth.
How does the uterus change after birth?
After the baby is born, the uterus will contract again to allow the placenta, which feeds the baby during pregnancy, to leave the woman’s body. This is sometimes called the ‘after birth’. These contractions are milder than the contractions felt during labour. Once the placenta is delivered, the uterus remains contracted to help prevent heavy bleeding known as ‘postpartum haemorrhage‘.
The uterus will also continue to have contractions after the birth is completed, particularly during breastfeeding. This contracting and tightening of the uterus will feel a little like period cramps and is also known as 'afterbirth pains'.
Read more here about the first few days after giving birth.
Sources:
The Royal Australian and New Zealand College of Obstetricians and Gynaecologists (Labour and birth), StatPearls Publishing (Anatomy, Abdomen and Pelvis), Department of Health (Clinical practice guidelines: Pregnancy care), Better Health Channel Victoria (Pregnancy stages and changes), Mater Mother's Hospital (Labour and birth information), Royal Australian and New Zealand College of Obstetricians and Gynaecologists (The First Few Weeks Following Birth), Queensland Health (Queensland Clinical Guidelines – maternity and neonatal), King Edward Memorial Hospital (Fundal height: Measuring with a tape measure), Royal Hospital for Women (Fetal growth assessment (clinical) in pregnancy), MSD Manual (Female internal genital organs)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: October 2020
Back To Top
Related pages
- Anatomy of pregnancy and birth - perineum and pelvic floor
- Anatomy of pregnancy and birth - pelvis
- Anatomy of pregnancy and birth - cervix
- Anatomy of pregnancy and birth - abdominal muscles
- Anatomy of pregnancy and birth
Need more information?
Prolapsed uterus - Better Health Channel
The pelvic floor and associated supporting ligaments can be weakened or damaged in many ways, causing uterine prolapse.
Read more on Better Health Channel website
Uterus, cervix & ovaries - fact sheet | Jean Hailes
This fact sheet discusses some of the health conditions that may affect a woman's uterus, cervix and ovaries.
Read more on Jean Hailes for Women's Health website
Dilatation and curettage (D&C)
A D&C is an operation to lightly scrape the inside of the uterus (womb).
Read more on WA Health website
Ectopic pregnancy
An ectopic pregnancy occurs when a fertilised egg implants outside the uterus (womb)
Read more on WA Health website
Placental abruption - Better Health Channel
Placental abruption means the placenta has detached from the wall of the uterus, starving the baby of oxygen and nutrients.
Read more on Better Health Channel website
Placenta previa - Better Health Channel
Placenta previa means the placenta has implanted at the bottom of the uterus, over the cervix or close by.
Read more on Better Health Channel website
Pelvic Floor | Family Planning NSW
The pelvic floor is a group of muscles in the pelvic area that support the bladder, bowel and uterus (womb).
Read more on Family Planning NSW website
Mirena IUD | Hormonal IUD Mirena | IUD Mirena insertion | IUD Mirena cost | Mirena IUD Melbourne - Sexual Health Victoria
The hormonal intrauterine device (IUD) is a small contraceptive device that is put into the uterus (womb) to prevent pregnancy.
Read more on Sexual Health Victoria website
Contraception - intrauterine devices (IUD) - Better Health Channel
An intrauterine device (IUD) is a small contraceptive device that is put into the uterus (womb) to prevent pregnancy.
Read more on Better Health Channel website
Endometriosis | Your Fertility
Endometriosis is a condition where the tissue that lines the uterus also grows in other areas of the body
Read more on Your Fertility website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.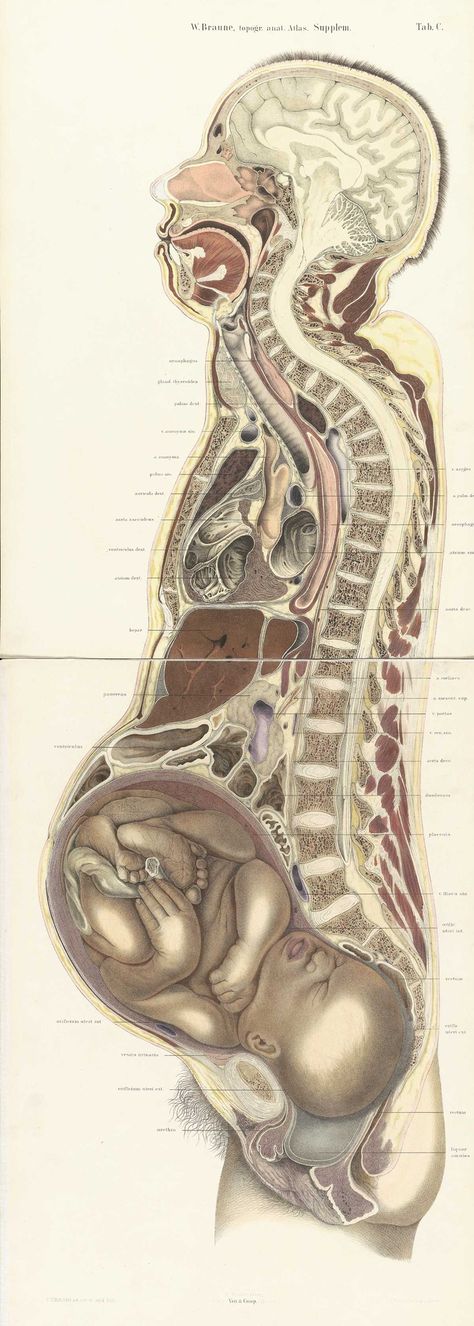
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Your Body throughout Pregnancy
Your Body Before Pregnancy
Next Image
Your Body Before Pregnancy
Before pregnancy, most of the space in your abdomen is taken up by the large and small intestines. There is no real separation between the areas of your pelvis and abdomen.
There is no real separation between the areas of your pelvis and abdomen.
In the picture here, you can see that the vagina is behind the bladder (sac that collects urine) and urethra (tube for moving urine out of bladder and body). In its normal position, your uterus is above and behind the bladder, with the cervix protruding into the vagina. The pelvic colon, rectum and anal canal are behind the vagina and uterus.
Previous | Next
Your Body at 6-7 Weeks of Pregnancy
Next Image
Your Body at 6-7 Weeks of Pregnancy
When you are between 6 and 7 weeks pregnant, you may be experiencing the early signs of pregnancy: your period has stopped and you may have nausea, breast tenderness and swelling, frequent urination and fatigue.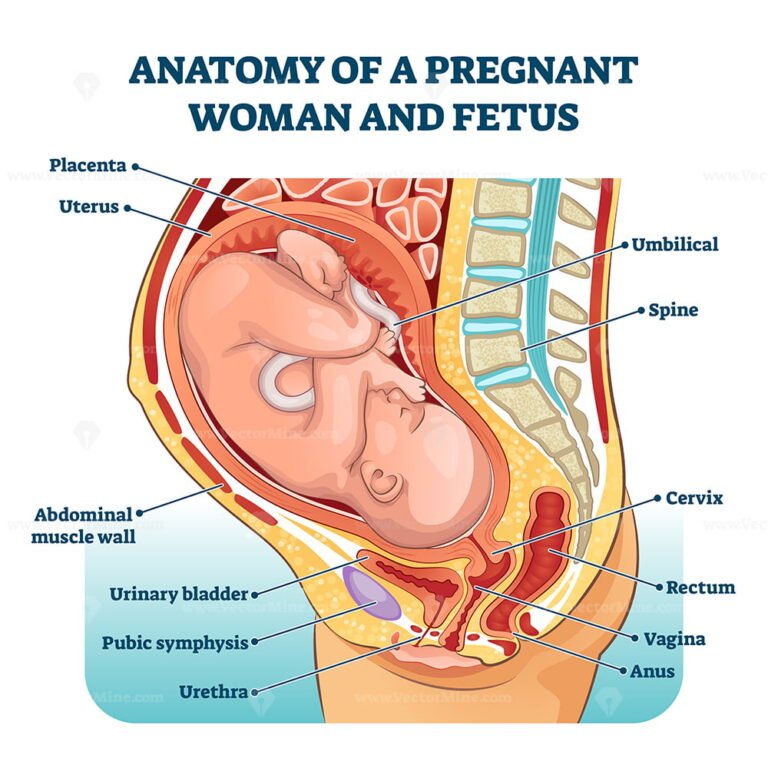
At this point, your uterus has begun to grow and become more egg-shaped. The pressure of the growing uterus on the bladder causes frequent urge to urinate.
In this image, you can see the beginnings of the placenta in the uterus. The embryo is about 1/4 inch to 1/2 inch long and weighs 1/1,000th of an ounce.
The embryo’s head is large in proportion to the rest of the body. The internal organs are forming and the heart has been beating since the end of the 4th week.
The embryo is floating in the amniotic sac. Buds for the arms and legs emerge in the 5th week and, by the 7th week, buds for fingers and toes also appear. The umbilical cord is lengthening and will continue to grow, allowing the fetus freedom to move. The 7th week represents a milestone in development: the embryo is now considered a fetus.
Previous | Next
Your Body at 12 Weeks of Pregnancy
Next Image
Your Body at 12 Weeks of Pregnancy
At the 12th week of pregnancy, the placenta is much larger. It now produces the hormones needed to sustain the pregnancy. Your uterus is the size of a grapefruit and completely fills the pelvis. It rises up into the area of the abdomen, as shown in the image. The fundus, the upper end of the uterus, is just above the top of the symphysis where the pubic bones join together. This upward growth of the uterus takes pressure off the bladder and decreases the need for frequent urination. The mucus plug, a barrier to protect the growing fetus, fills your cervical canal.
It now produces the hormones needed to sustain the pregnancy. Your uterus is the size of a grapefruit and completely fills the pelvis. It rises up into the area of the abdomen, as shown in the image. The fundus, the upper end of the uterus, is just above the top of the symphysis where the pubic bones join together. This upward growth of the uterus takes pressure off the bladder and decreases the need for frequent urination. The mucus plug, a barrier to protect the growing fetus, fills your cervical canal.
The fetus is now about 3 inches long and weighs about 1 ounce. By this week, the fetus has fingernails and toenails and can open and close the fingers. The fetus will start to move, but you will not feel it yet.
Previous | Next
Your Body at 20 Weeks of Pregnancy
Next Image
Your Body at 20 Weeks of Pregnancy
By the 20th week of pregnancy, your uterus can be felt at the level of your belly button (umbilicus). The pelvic colon and small intestines are crowded upward and backward. The ascending and descending colon maintain their usual positions.
The pelvic colon and small intestines are crowded upward and backward. The ascending and descending colon maintain their usual positions.
At this point, your uterus is especially enlarged where the placenta attaches to it (usually on the front or back wall). This gives the uterus an uneven bulge. The wall of the uterus, which lengthens and thickens early in pregnancy, stretches as the fetus grows, and becomes thinner now – just 3 to 5 millimeters thick. Your bladder moves up but not as much as your uterus, which straightens as it moves up.
As your uterus moves up, it rests against the lower portion of the front of your abdominal wall, causing it to bulge forward noticeably by your 20th week. The size of the bulge depends on how strong your abdominal muscles are. If they are firm, the uterus may be pressed against the spinal column, and there will be no noticeable bulge; if they are weak, the pressure of the uterus against the inside wall makes a sizeable bulge.
At this point, you should be able to feel light movements of the fetus. This is called “quickening.” You may recognize this earlier if you have been pregnant before. The fetus sleeps and wakes at regular intervals, is more active, is about 9 inches long and weighs between a half-pound and a pound.
This is called “quickening.” You may recognize this earlier if you have been pregnant before. The fetus sleeps and wakes at regular intervals, is more active, is about 9 inches long and weighs between a half-pound and a pound.
Previous | Next
Next Image
At this point in pregnancy, the top of your uterus is about one-third of the distance between the bellybutton and the xiphoid cartilage at the lower end of your breastbone. Constipation is common because your uterus is pressing on your lower colon and hormones slow down your body’s excretion process. Between the growth of your uterus and general weight gain, you may be feeling fatigued. Some women also experience heartburn as your uterus presses against your stomach.
Your breasts are also changing to get ready for breastfeeding. First colostrum and then milk are produced by the grape-like clusters of tiny sacs (alveoli) deep within the breast tissue. Clusters of alveoli form lobules, which come together to form 15 to 20 lobes. Each lobe connects to a lactiferous duct for conveying milk. As the ducts extend toward the nipple and areola (darker area around the nipple), they widen into the lactiferous sinuses. These sinuses (or milk pools) release the milk through 15 to 20 tiny nipple openings in each breast when the baby nurses.
At week 28, the fetus is about 16 inches long and weighs two to three pounds. The skin is wrinkled but will become less so as more fat builds up under the skin in the next few weeks. Fine, downy hair called lanugo, and a waxy white protective substance covering the skin called vernix, are on the fetus’ body. Its eyes are open, and eyebrows and eyelashes were formed in the fourth month. The fetus sucks its thumb and its taste buds have developed. It kicks, stretches and moves frequently in your uterus—you’ll feel it moving around and others might even be able to see these movements!
It kicks, stretches and moves frequently in your uterus—you’ll feel it moving around and others might even be able to see these movements!
Fetal organs and systems are quite well developed by the 28th week of pregnancy, but the final two months of gestation are important for further maturation of all body systems and organs.
Previous | Next
Your Body at 36 Weeks of Pregnancy
Next Image
Your Body at 36 Weeks of Pregnancy
By the end of the 36th week of pregnancy, your enlarged uterus almost fills the space within your abdomen. The fetus is inside the membrane sac within the uterus and high within the abdomen. The muscles of your abdomen support much of its weight.
During this week, the top of the uterus is at the tip of the xiphoid cartilage at the lower end of the breastbone, which is pushed forward.
The change in the position of the heart and the upward pressure of the diaphragm may make it hard to breathe at this point. The crowding of your stomach and intestines may contribute to discomfort after eating.
Your cervix is long, thick and filled with the mucous plug. By the 36th week, your vagina and urethra are elongated and all the tissues in the perineum (area between vaginal and anal openings) are enlarged. The swollen perineum projects outward in the last weeks of pregnancy and readily expands during labor.
The brain of the fetus is growing rapidly, but bones in the skull are soft so that he or she will fit through your vagina at birth. The lungs are still forming. You will likely feel the fetus kicking and may be aware of rhythmic movements, which could be hiccups or thumb sucking. Another possible sensation, sudden movement, may be a startle response.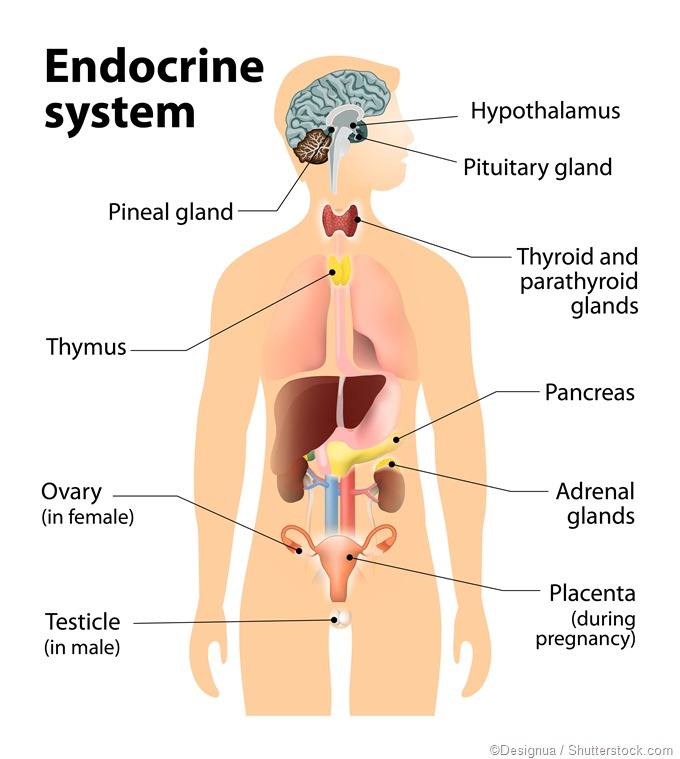
Previous | Next
Your Body at 40 Weeks of Pregnancy (Internal)
Next Image
Your Body at 40 Weeks of Pregnancy (Internal)
At full term, or 40 weeks of pregnancy, the fetus’ head has generally lowered into your pelvis, where it takes up most of the space. This is called “lightening.” In first pregnancies, this may happen a few weeks before labor. In repeat pregnancies, this can happen at the time of labor. The canal of the broad, enlarged cervix is still filled with the plug of mucous. If this is your first pregnancy, the small opening at the bottom of your cervix is usually not dilated, whereas if you have given birth before, it will often be open as wide as two fingers some time before labor begins.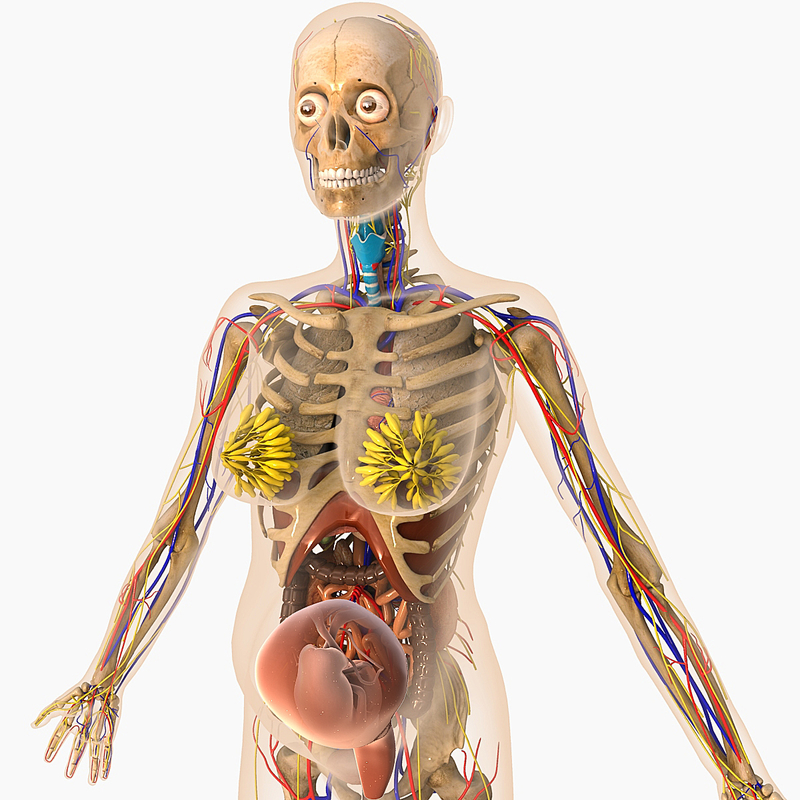
At this point, you may be experiencing frequent urination, increased constipation, edema (water retention) and aching legs or vulva. Varicose veins in the vulva, rectum and legs are also possible. This is because of the position of the uterus, the pressure of the baby's head and a loss of muscle tone as the hormone relaxin loosens your tissues in preparation for birth. Other changes at this time include increased development of blood vessels and increased amount of blood.
Previous | Next
Your Body at 40 Weeks of Pregnancy (External)
Next Image
Your Body at 40 Weeks of Pregnancy (External)
You can see that the round ligament is long and enlarged. It is also farther forward because of the twisting of the uterus. The enlarged uterosacral ligament is shown stretched taut by the enlarged uterus. Backaches in late pregnancy may be due to the stress of the weight of your uterus on the ligaments that connect it to your spine.
It is also farther forward because of the twisting of the uterus. The enlarged uterosacral ligament is shown stretched taut by the enlarged uterus. Backaches in late pregnancy may be due to the stress of the weight of your uterus on the ligaments that connect it to your spine.
Because your uterus dropped a bit, you may be able to breathe and eat more comfortably near the end of your pregnancy.
At this time, the lungs of the fetus are likely fully mature and ready to begin breathing. The fetus gains about a half pound every week at the end of pregnancy, for a birth weight of roughly 7 pounds, and is growing longer for a birth length of about 18 to 21 inches.
Labor starting on its own around week 40 is a sign that your body is ready to give birth and your baby is ready to be born.
Previous | Next
Memo for a pregnant woman
Memo for a pregnant woman about actions in case of influenza, acute respiratory infection, new coronavirus infection COVID-19
Influenza - acute infectious disease. The duration of the incubation period for influenza is from several hours to 7 days, most often 2-3 days.
The duration of the incubation period for influenza is from several hours to 7 days, most often 2-3 days.
The disease begins acutely with a sharp increase in body temperature up to 38°C and above and severe symptoms of intoxication (chills, headache, joint pain, pain in the muscles and when moving the eyeballs). Further (sometimes after a few days), symptoms of respiratory tract damage (dryness of the mucous membranes of the nose and mouth, sore throat, chest pain, dry cough, shortness of breath) join. With the flu, there may be symptoms of an upset gastrointestinal tract: nausea, vomiting, diarrhea.
The new coronavirus infection COVID-19 often has the same symptoms as the flu. Unlike influenza, the incubation period for this infection ranges from 2 to 14 days, with an average of days. In the initial stages of the disease, smell and taste may disappear, catarrhal symptoms are mild, most patients report severe weakness, shortness of breath, dry cough without sputum.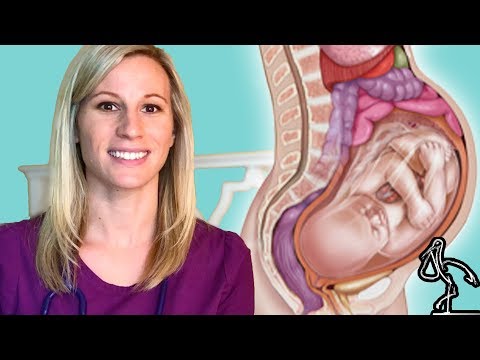 Gastrointestinal disorders are common with COVID-19.
Gastrointestinal disorders are common with COVID-19.
Pregnant women, the elderly and debilitated, and young children are at high risk for severe and complicated forms of influenza. In them, the disease often has a very rapid (within a few hours) development of the disease. With the new coronavirus infection COVID-19, pregnant women are also prone to severe forms, but the course of this infection in children can be very mild and asymptomatic.
It should be remembered that self-treatment or late referral to specialized medical care leads to the development of severe life-threatening complications.
In the absence of timely treatment, a pregnant woman is threatened with the development of complications from the lungs, kidneys, heart and brain, premature birth, thrombosis and thromboembolism, placental abruption, preeclampsia and other obstetric complications. Intrauterine infection of the fetus with the influenza virus in the early stages can lead to developmental abnormalities or miscarriage, in the later stages - to intrauterine death of the fetus, death of a newborn child after birth or the development of serious illnesses in him.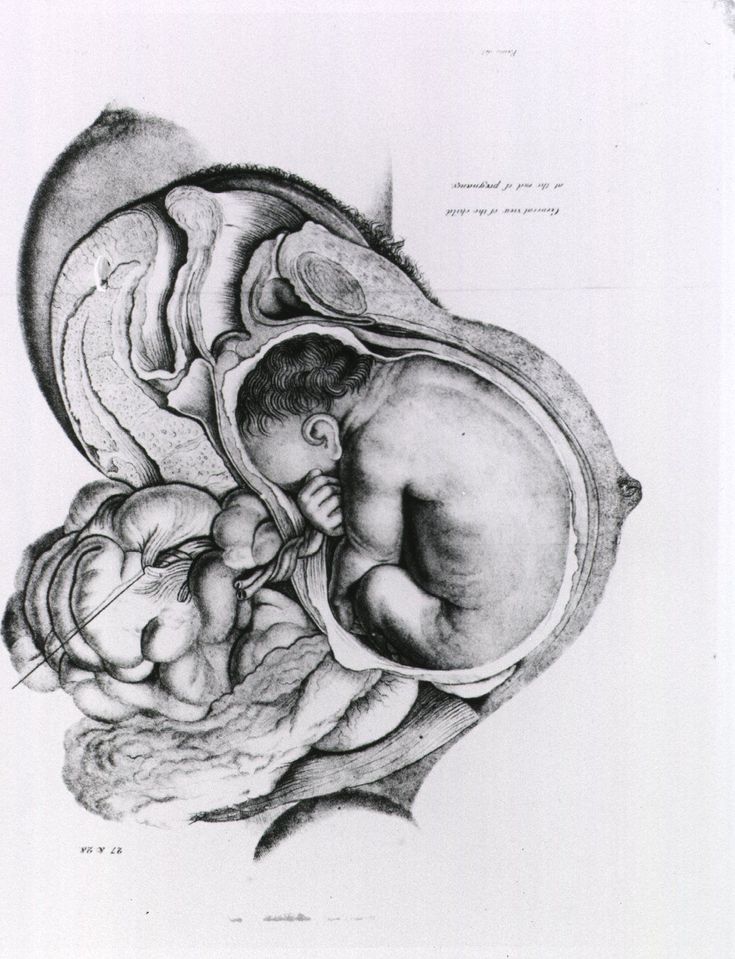 The effect of the novel coronavirus infection on the fetus has not yet been studied.
The effect of the novel coronavirus infection on the fetus has not yet been studied.
The Ministry of Health of the Russian Federation has developed effective regimens for the treatment of influenza and the new coronavirus infection COVID-19 in pregnant women with safe drugs that are selected individually by a doctor, so do not self-medicate!
When to see a doctor immediately:
1. Sudden onset of the disease: fever up to 38°C or more, muscle pain, joint pain, headache, severe weakness.
2. Cough, shortness of breath, sore throat, chest pain, runny nose. Especially dangerous cough with streaks of blood in the sputum!
3. Nausea, vomiting, diarrhea.
4. Pain in the abdomen, increased or decreased blood pressure, bleeding from the genital tract of any intensity, discharge of amniotic fluid, changes in fetal movements (violent or weak).
If you fall ill, you should immediately contact the reception of the territorial polyclinic or call an ambulance at home and be sure to inform your local obstetrician-gynecologist of the antenatal clinic about the disease by phone.
If you are offered hospitalization, do not refuse hospital treatment. Treatment at home does not allow timely detection of complications and monitoring the development and condition of the fetus. In case of an acute infectious disease, you should not visit a polyclinic or a antenatal clinic on your own - medical care will be organized for you by visiting teams of medical workers.
If you have had contact with someone who has the flu or COVID-19, you should consult with the local general practitioner as soon as possible and inform the local obstetrician-gynecologist about this in order to prescribe preventive measures.
Follow the measures to prevent infection with influenza and the new coronavirus infection COVID-19: stay at home in self-isolation, do not visit public places (mass events, entertainment centers, shops, pharmacies, hospitals, etc.) unless absolutely necessary.
If you have sick relatives at home, especially small children and the elderly, do not delay seeking medical help.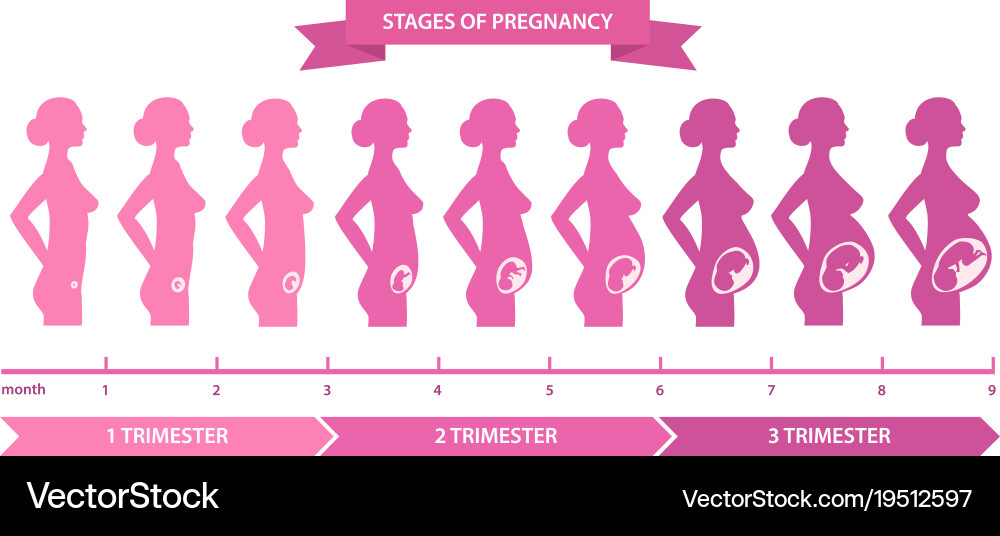 Try to completely isolate yourself from them or have as little contact with the sick person as possible. Wear and change individual disposable medical masks every 2 hours, wash your hands often with soap and treat them with an antiseptic, ventilate the room. Wet cleaning of the premises is required at least 2 times a day.
Try to completely isolate yourself from them or have as little contact with the sick person as possible. Wear and change individual disposable medical masks every 2 hours, wash your hands often with soap and treat them with an antiseptic, ventilate the room. Wet cleaning of the premises is required at least 2 times a day.
Use sea salt nasal rinses and throat gargles, prophylactic ointments or interferon nasal drops 3-4 times a day. Other preparations for the prevention of influenza in contact with the sick person will be recommended by a doctor.
REMEMBER!
Only timely seeking medical help will save the life and health of mother and child
Pregnancy calendar
You are pregnant! Your baby will be born in 40 weeks. What changes will occur in your body, how your baby will grow will tell "Calendar of pregnancy".
1-2 weeks
Pregnancy begins at the moment of fertilization or conception.
Fertilization is a complex biological process of the fusion of female and male germ cells (egg and sperm). The resulting cell (zygote) is a new daughter organism.
A mature egg leaves the ovary approximately on the 12-14th day of the menstrual cycle (ovulation) and enters the fallopian tube, where it remains viable for 24 hours. During an orgasm, a man ejects from 200 to 400 million spermatozoa into the woman's vagina. Some of them penetrate through the cervix into the uterine cavity, and from there into the fallopian tubes. Here, spermatozoa retain the ability to fertilize for 48 hours. Thus, within 6-7 days of a woman's menstrual cycle, conception is possible.
Fertilization of the female egg is performed by a single sperm in the upper part of the fallopian tube. There are two types of sperm: those containing the Y chromosome (“male”) and the X chromosome (“female”). When an egg cell (containing the X chromosome) fuses with a sperm cell, their genetic material is combined and the sex of the child is determined.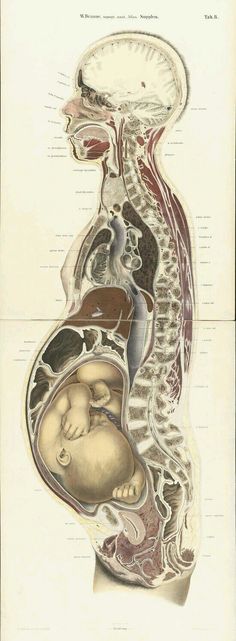 If there are two X chromosomes in the child's genetic makeup, it's a girl; if an X chromosome and a Y chromosome, it's a boy. It is impossible to change the sex of the child, so you should not follow the "folk beliefs" that guarantee the birth of a child of a given gender.
If there are two X chromosomes in the child's genetic makeup, it's a girl; if an X chromosome and a Y chromosome, it's a boy. It is impossible to change the sex of the child, so you should not follow the "folk beliefs" that guarantee the birth of a child of a given gender.
The fertilized egg begins to divide with the formation of a multicellular organism and move through the fallopian tube into the uterine cavity. During this period, the nutrition of the embryo is carried out at the expense of those substances that have been accumulated in the egg. If the peristalsis of the tube is slowed down (due to inflammatory diseases), the embryo penetrates the wall of the fallopian tube with the occurrence of an ectopic pregnancy.
Implantation (introduction) of the embryo into the uterine wall occurs 7-8 days after fertilization.
On the seventh day of pregnancy, the outer layer of the embryo (trophoblast) begins to produce a hormone - chorionic gonadotropin. This hormone gives the mother's body information that pregnancy has occurred, and begins its functional restructuring. Diagnostic test strips detect the chorionic gonadotropin in the urine of a pregnant woman, which makes it possible to diagnose pregnancy at an early stage.
Diagnostic test strips detect the chorionic gonadotropin in the urine of a pregnant woman, which makes it possible to diagnose pregnancy at an early stage.
3-4 weeks
You do not have the expected menstruation, nausea in the morning, and frequent urination during the day. You become emotionally labile, irritable, whiny. Basal body temperature is above 37°C.
In appearance, your unborn baby resembles a small auricle measuring 4 mm, surrounded by a small amount of amniotic fluid. On the 21st day after conception, the brain and spinal cord are formed. By the end of the first month, the circulation of embryonic blood is established, the umbilical cord has formed - the connection of the embryo with the future placenta. The eye sockets, the rudiments of arms and legs appeared, the laying and development of other internal organs of the fetus is underway: the liver, kidneys, urinary tract, and digestive organs.
5-6 weeks
You no longer doubt that you are pregnant.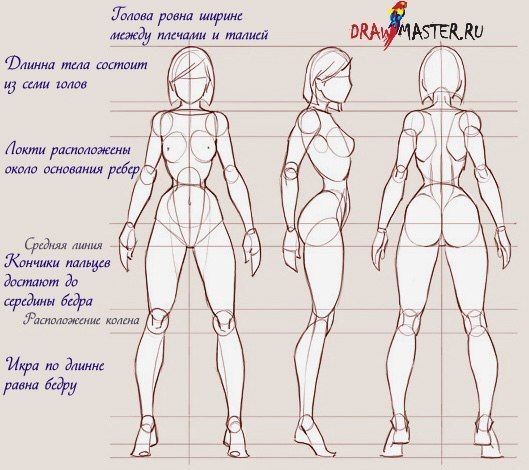 Regardless of how you feel, all pregnant women need to visit a antenatal clinic and undergo an examination that will allow you to identify and correct existing health problems in time.
Regardless of how you feel, all pregnant women need to visit a antenatal clinic and undergo an examination that will allow you to identify and correct existing health problems in time.
Starting from the 5th week, there may be a threat of termination of pregnancy. This will be evidenced by: periodic pain in the lower abdomen and in the lumbar region, a feeling of pressure on the rectum, an increased amount of mucus. If you experience these symptoms, you should consult a doctor.
By week 6, the face is formed in the embryo: eyes, nose, jaws and limbs.
7-8 weeks
From the 7th week of pregnancy, the yellow body of pregnancy undergoes reverse development, the production of hormones begins to be carried out by the forming placenta.
The baby develops large blood vessels, the heart becomes four-chambered. Bile ducts appear in the liver. There is a development of the endocrine glands, the brain. The auricles are already formed, fingers have appeared on the limbs.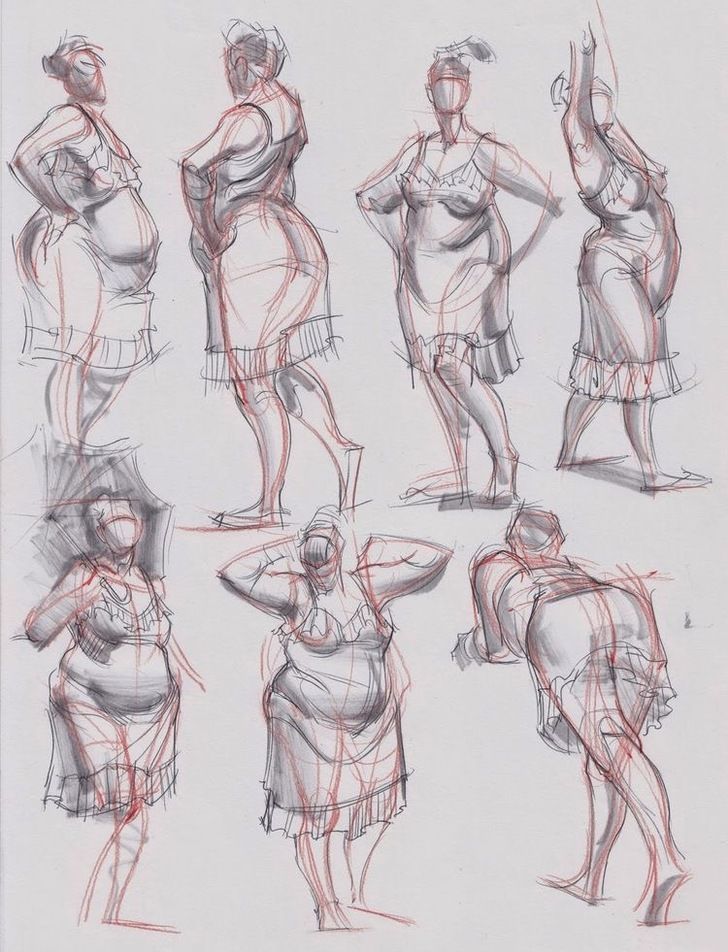 The embryo begins to move. At week 8, under the influence of the Y chromosome, the formation of male gonads (testicles) occurs. They begin to produce testosterone - the male sex hormone, which will lead to the formation of the sexual characteristics of the boy.
The embryo begins to move. At week 8, under the influence of the Y chromosome, the formation of male gonads (testicles) occurs. They begin to produce testosterone - the male sex hormone, which will lead to the formation of the sexual characteristics of the boy.
9-10 weeks
Your metabolism is changing significantly to provide the growing body with all the necessary "building materials" - amino acids, energy. Disadaptation to such a restructuring can result in toxicosis of the 1st half of pregnancy. It is characterized by nausea, vomiting, salivation, weight loss. When the first symptoms appear, consult a doctor.
At the tenth week, the development of the oral cavity, intestines, rectum, and bile ducts ends in the embryo. The formation of the face and hemispheres of the brain was completed. The development of the cerebellum, the main coordinator of movements, begins.
11-12 weeks
The body has adapted to the new conditions. By this time, nausea, vomiting, salivation practically disappear.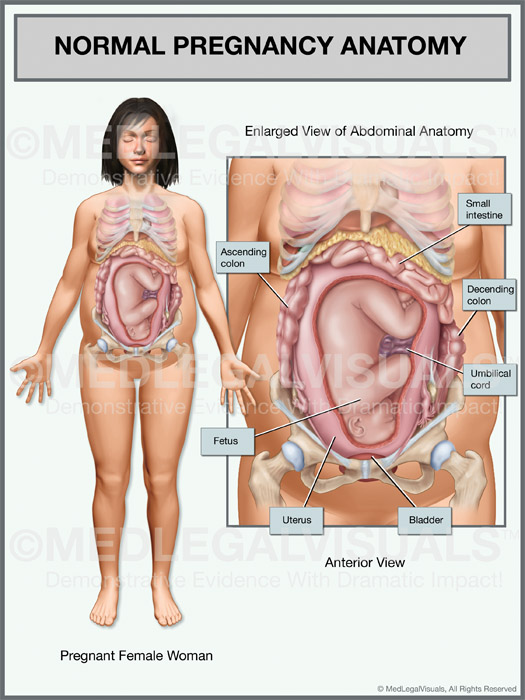 You become balanced, calm.
You become balanced, calm.
Uterine growth becomes visible after 12 weeks
13-14 weeks
By this time, the formation of the main organs of the unborn child is completed. In appearance, the fetus resembles a small person.
15-16 weeks
A change in skin pigmentation is possible - the midline of the abdomen, nipples and the skin around them have darkened. These phenomena should pass soon after childbirth.
The formation of the placenta is coming to an end. The fetus and placenta represent a single functional system. During this period of pregnancy, the fetus floats freely in the amniotic fluid. The composition of the amniotic fluid can determine the condition of the fetus.
17-18 weeks
These days, your unborn child begins to move. His limbs, ligamentous apparatus, cerebellum have already developed enough. By this time, the formation of the immune system is completed.
19-20 weeks
There have been big changes in your body. The pulse quickened, cardiac output increased significantly (40% higher than the initial level) and the volume of circulating blood (almost 500 ml).
The pulse quickened, cardiac output increased significantly (40% higher than the initial level) and the volume of circulating blood (almost 500 ml).
Due to the increased volume of plasma compared to the mass of red blood cells, hemoglobin decreases in blood tests.
Some women during this period experience frequent and painful urination, pain in the lumbar region on the right or left, weakness. A large uterus presses down on the bladder, the mouth of the ureters, disrupting the outflow of urine. Stagnation of urine and incomplete emptying of the renal pelvis create conditions for the development of infection. Bacteriuria develops and pyelonephritis of pregnant women may occur. If there is any suspicion of pyelonephritis, you should immediately consult a doctor, because this disease is not only dangerous for your health, but also for the further growth and development of the fetus.
The weight of the baby is 300-350 grams, he often and quite actively moves, swallows amniotic fluid, begins to open his eyes.
21-22 weeks
In these weeks, the fetus already has a mass of 400-500 grams, and it develops very intensively bones and muscles, which require calcium from your body. Therefore, if you do not want to lose your white-toothed smile, then, on the advice of your obstetrician-gynecologist, start taking calcium supplements regularly. This will help save your teeth and get rid of leg cramps. They appear for the same reason of calcium deficiency.
23-24 weeks
At this time, the weight of the fetus is 500-600 g. It already has all the organs and systems fully formed. Until that time, only his lungs remained immature. And now, by 24 weeks, they begin to ripen. And the cells lining the lung alveoli produce surfactant, a substance that, by lubricating the alveoli, prevents them from sticking together during breathing. However, the amount of surfactant is so small that a child born at this time will not be able to breathe on its own. To survive outside the uterus, he needs sophisticated breathing equipment, incubators, a control system, infusors for nutrition, infusion media, artificial surfactant.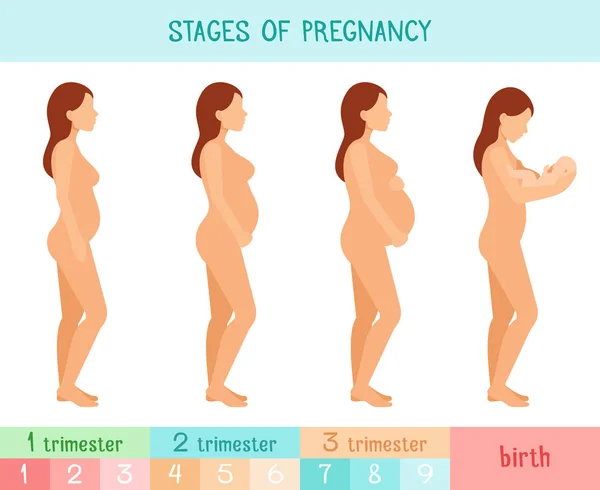
There are perinatal centers where children born during these terms of pregnancy are nursed. It is very difficult. And therefore, the longer the pregnancy is prolonged, the more likely the birth of a healthy and viable child. Therefore, try to do everything so that the child is born on time, full-term and healthy.
By this gestational age, the uterus is at a height of about 24 cm above the pubic bone, and now it not only builds up muscles, but is also stretched by the fetus that completely filled its cavity.
25-26 weeks
The fetus already has a mass of 700-750 g. Due to the improvement of the brain structures in his body, a connection is established with the adrenal cortex and they begin to produce corticoids - hormones necessary for adaptation. The pituitary gland of the fetus reaches such a degree of maturity that the production of adrenocorticotropic hormone begins, which also stimulates hormonal production by the adrenal glands. In short, all forces are thrown to the upcoming "publication".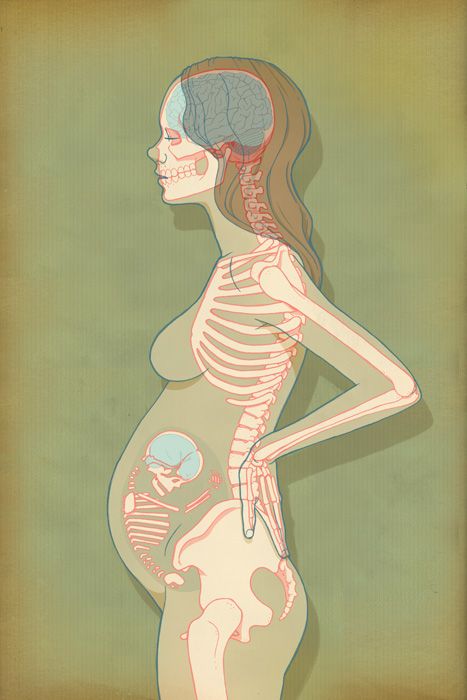 But the most obvious changes in these weeks occur in the lungs - there is an increased maturation of cells that produce surfactant. However, a fetus born during this period can only survive in incubators with artificial lung ventilation, artificial feeding with special infusion media. Therefore, try to keep both him and yourself from rash steps.
But the most obvious changes in these weeks occur in the lungs - there is an increased maturation of cells that produce surfactant. However, a fetus born during this period can only survive in incubators with artificial lung ventilation, artificial feeding with special infusion media. Therefore, try to keep both him and yourself from rash steps.
At this time, it's time to start preparing for the future feeding of the child. Under the influence of placental lactogen, your breasts, that is, the mammary glands, are growing rapidly. From time to time, droplets of colostrum may appear on the nipples. Daily air baths, washing with cool water, rubbing the nipples with a rough towel will help prepare the nipples for feeding. If the nipples are flat, start to stretch them little by little.
27-28 weeks
This period completes the second trimester of pregnancy. By this time, the fetus weighs up to 1000 g and has a height of up to 35 cm. However, he still cannot live on his own, because.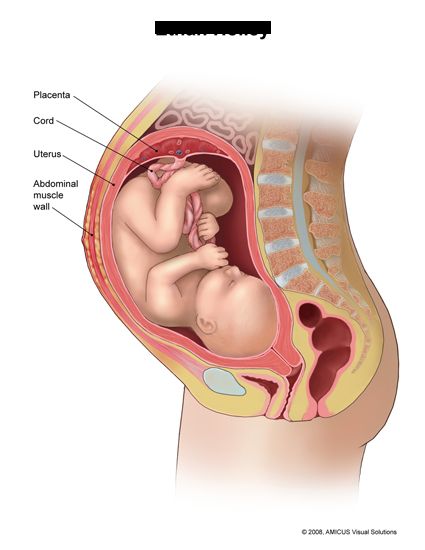 his lungs are not mature enough and special equipment is still needed to nurse him. During these periods of pregnancy, there is an intensive growth of the fetus, the formation of muscles. His movements become more active. Periods of movement alternate with its relatively calm state when the fetus is sleeping. With an ultrasound, you can see that he already knows how to suck his thumb and even smile!
his lungs are not mature enough and special equipment is still needed to nurse him. During these periods of pregnancy, there is an intensive growth of the fetus, the formation of muscles. His movements become more active. Periods of movement alternate with its relatively calm state when the fetus is sleeping. With an ultrasound, you can see that he already knows how to suck his thumb and even smile!
The fundus of the uterus stands on average at a height of 27-28 cm above the womb.
29-30 weeks
The third trimester of pregnancy begins. The uterus stands at a height of 29-30 cm, it becomes more difficult for you to breathe. Now one of the most serious complications can develop - toxicosis of the second half of pregnancy, which is characterized by the appearance of edema, increased blood pressure and the appearance of protein in the urine. For early diagnosis of this complication, it is necessary to carefully observe an obstetrician-gynecologist and follow all his recommendations, incl.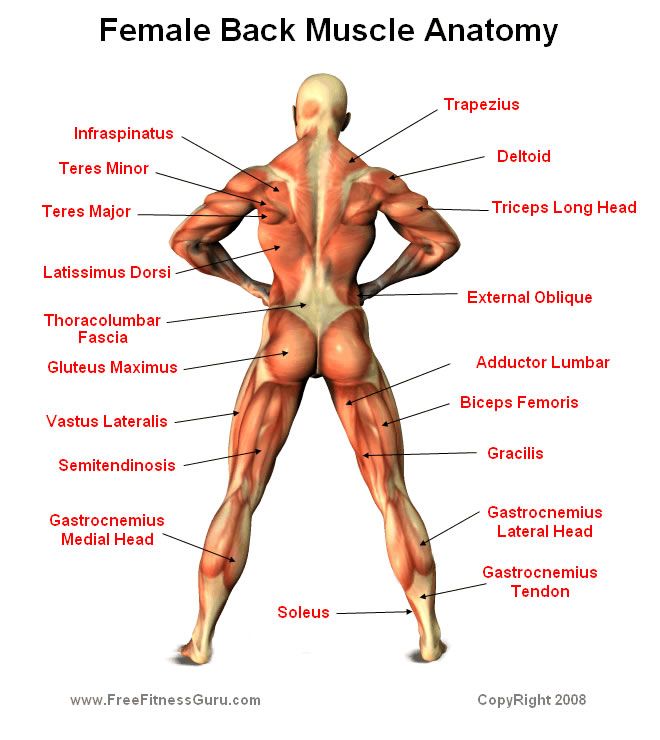 strict weight control. In the III trimester of pregnancy, the daily weight gain should be no more than 50 g, i.e. no more than 300 g per week. You should also monitor the ratio of drunk and secreted fluid.
strict weight control. In the III trimester of pregnancy, the daily weight gain should be no more than 50 g, i.e. no more than 300 g per week. You should also monitor the ratio of drunk and secreted fluid.
31-32 weeks
Have you asked your doctor how the fetus is? Find out now it's very important. Its position can be longitudinal, transverse, oblique. Correct, normal is the longitudinal position of the fetus. Childbirth is safer with cephalic presentation. From this period of pregnancy, it is necessary to wear a prenatal bandage that will support the anterior abdominal wall and help maintain the correct position and presentation of the fetus. If the presentation of the fetus is breech, i.e. above the entrance to the pelvis is the pelvic end of the fetus, then the bandage should not be worn yet. There is gymnastics to correct the presentation of the fetus.
In the morning and evening for 1 hour, do the following: lie down on the bed on your left side and lie quietly for 15 minutes, then turn over to your right side and lie for the next 15 minutes, and then repeat these turns 2 more times.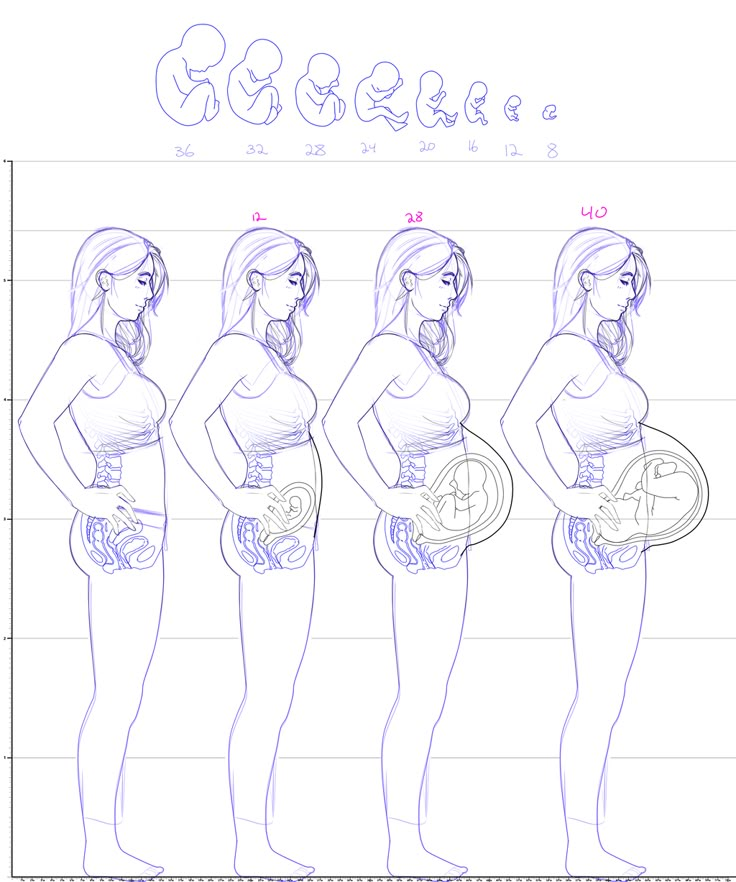
Pregnant women with Rh-negative blood and with O (I) blood type need blood tests for Rh - or group immune antibodies. Immunization of pregnant women with Rh-negative blood is carried out from 28 weeks and within 72 hours after childbirth according to the indications, which will be discussed by the doctor observing you in the antenatal clinic.
33-34 weeks
The fetus already has a mass of 1800-2100 g, a height of 40-41 cm. By the end of this period, its lungs will begin to produce surfactant in full and will be able to breathe without special equipment. The fetus is fully developed, its chances of surviving in case of preterm birth are greatly increased. However, there is still extremely little subcutaneous fat, so his skin is thin and has a red color. Such a newborn retains heat very poorly and at birth needs an incubator or a heating pad. His body is still covered with fluff and cheese-like grease, the auricles are still very small, but they are already beginning to straighten out, the boy's testicles descend into the scrotum.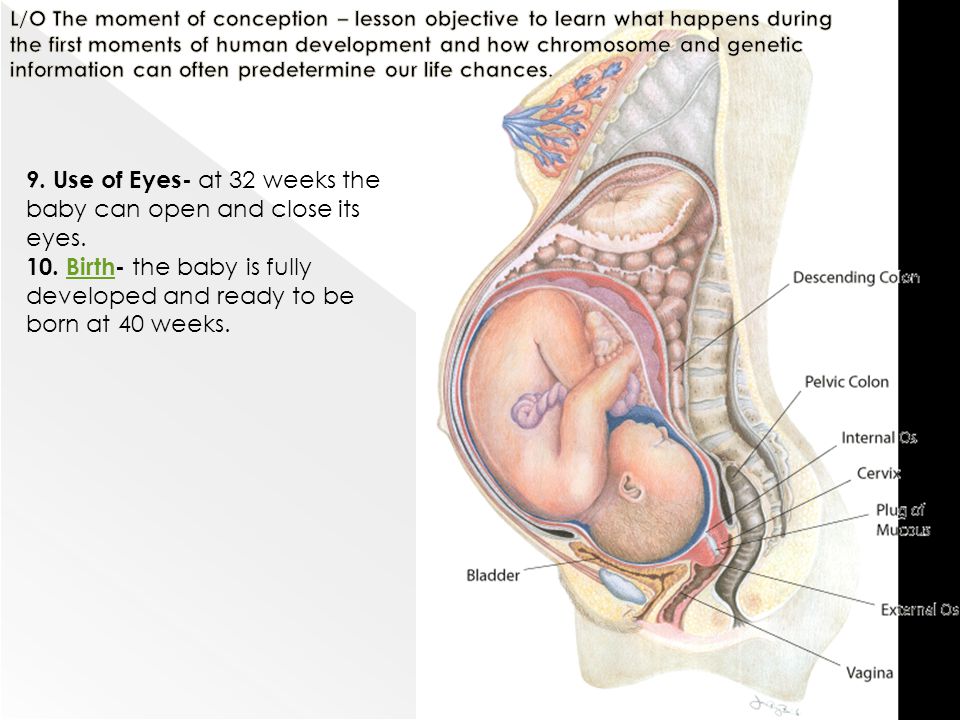
Caring for a premature baby is the hardest work for the whole family, associated with high material costs, physical overload of parents, and this work is not always rewarded, since a child can be born and remain sick. Therefore, up to 37 weeks of pregnancy, a woman should be especially attentive to her condition and, at the slightest suspicion of an increase in the tone of the uterus, starting frequent and regular contractions, immediately consult a doctor.
Doctors know that women, in anticipation of the arrival of a new person in the house, begin to glue walls and paint ceilings during this period. Don't take unnecessary risks. For this, prenatal leave is provided from 30 weeks, so that you can avoid overwork, do not push in transport, and have the opportunity to sleep. So repairs, stuffy shops, queues are no longer for you.
35-36 weeks
The fetus already has a mass of 2100-2700 g and a height of 44-45 cm. It is advisable to see a doctor during this period of pregnancy at least once every 10 days.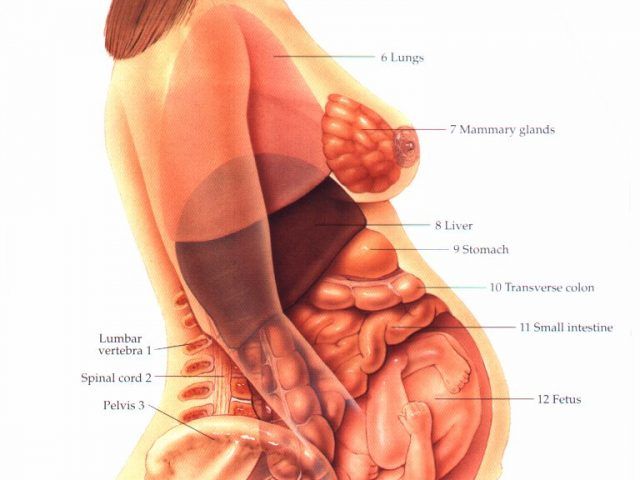
37-38 weeks
From this point on, your pregnancy is considered full-term. And if you have a baby in these weeks, he will live. Its development is complete. Now he has a mass of approximately 2700-3000 g. Height is 49-50 cm. The remaining two weeks he will add a little in weight and height.
It becomes easier for you to breathe, as the fetal head is pressed tightly against the entrance to the pelvis, the uterus pulls the anterior abdominal wall more, and therefore its bottom sank lower. Tension of the uterus; small sharp pulling pains in the lumbar region.
With an exacerbation of extragenital diseases, the appearance of signs of toxicosis in the second half of pregnancy, with an incorrect position of the fetus, with some gynecological diseases, against which pregnancy develops, a scar on the uterus, etc., early prenatal hospitalization is required. Do not forget to take an exchange card, passport, medical insurance policy and birth certificate to the hospital.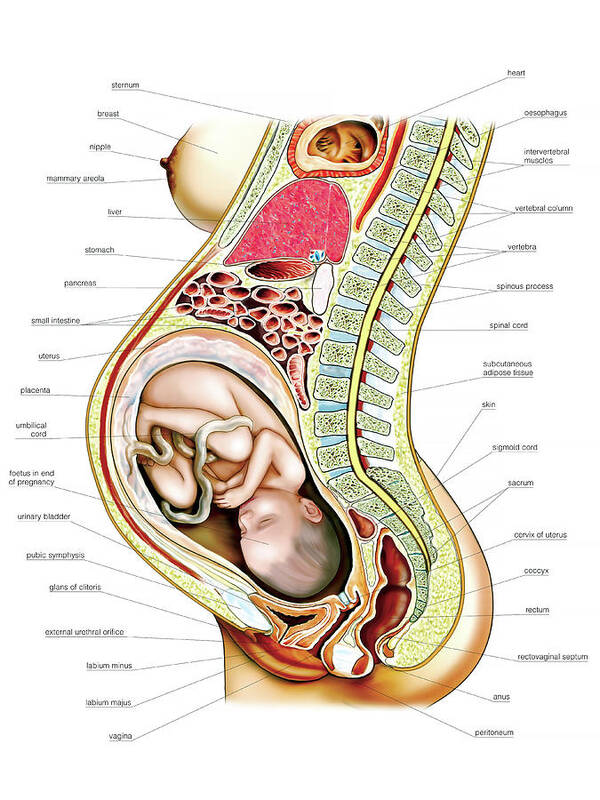
39-40 weeks
You can find out the approximate day of delivery by the date of the last normal menstruation - count back three months and add 7 days. The resulting number will be the estimated date of birth. More precisely, according to many parameters, ultrasound data, additional studies, the date of the first fetal movement, the date of the first visit to the obstetrician-gynecologist, especially if the visit was before 11-12 weeks of pregnancy.
The child already has all the signs of maturity. His weight is more than 3000 g, and his height is more than 50 cm, he has fair skin, a sufficient amount of subcutaneous fat, he retains heat and does not need special heating. He will scream loudly, breathe, suck. There is a very small amount of lubricant on the skin, which will no longer be able to protect it from the effects of amniotic fluid.
For you, regular contractions (1 contraction every 10 minutes) will become an indicator of the beginning of the birth process, or you will feel the outflow of amniotic fluid, you will see scanty bloody discharge - do not panic, call an ambulance, the telephone number for transportation for pregnant women is written on the margins of your exchange card.