Breast sores while breastfeeding
Breastfeeding FAQs: Pain and Discomfort (for Parents)
Breastfeeding is natural, but it takes practice to get it right. Here's how to handle pain and discomfort during nursing.
Is It Normal to Have Cramps While Breastfeeding?
Yes. During the first few days to weeks after delivery, you may feel strong, menstrual-like cramps in your uterus when your milk “lets down” (starts to flow). This is your uterus shrinking back to a smaller size.
Is It Normal for My Breasts to Get Engorged?
During the first 2–5 days after birth, it’s normal to have engorged (very full) breasts as your milk supply increases. But if your baby nurses (or you pump) every 2–3 hours, your breasts should not feel engorged.
Engorgement can lead to sore, painful breasts or a breast infection. So it’s best to try to avoid it. The longer you wait to breastfeed or pump, the more uncomfortable and engorged your breasts may get.
If you can't feed your baby right away, use warm compresses and try to pump or manually express your milk. One way to express milk is to put your thumb on top of your areola and a finger below it. Gently but firmly press your thumb and fingers back against your chest wall. Then compress your fingers together to express (push out) your milk.
Is It Normal to Feel Pain During or After Breastfeeding?
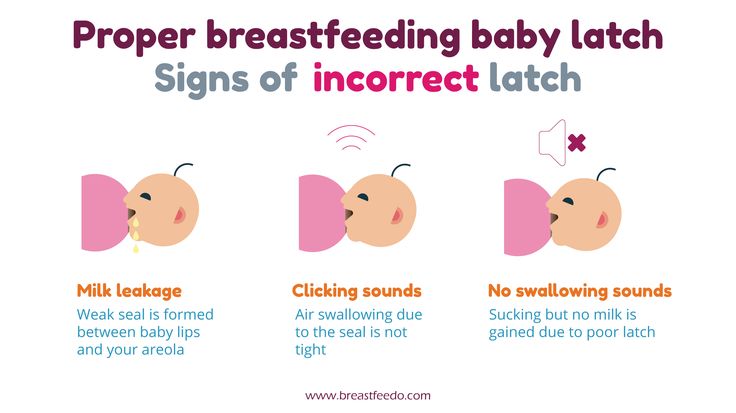
When babies latch on properly, some moms feel a few moments of discomfort at the very beginning of a nursing session. After that, discomfort should ease. You may feel a gentle tug on your breasts while your baby feeds, but it shouldn’t hurt.
If you feel discomfort during nursing, stop nursing and reposition your baby to get a better latch. Your nipple areola (the ring around the nipple) should be mostly in your baby’s mouth. When babies are latched on wrong, it can hurt or feel like a pinch each time your baby sucks. Over time, this can lead to painful, sore, cracked nipples.
If you have pain during breastfeeding, talk to your doctor or lactation consultant to make sure your baby is properly latched or that something else isn't going on.
What Else Can Cause Breast Pain?
The most common causes of breast pain include:
A plugged milk duct. Sometimes milk ducts get plugged. You may feel pain in an area of your breast or a lump may form under the skin where the duct is plugged. To help unclog the duct and ease pain:
- Take warm showers or use warm compresses on the area. Massage the area several times a day. Then, breastfeed your baby right away.
- Position your baby’s chin so that it points toward the clogged area during feeding. This will help that area of the breast empty sooner.
- Gently massage the lump while your baby feeds. It may take 2 to 3 feedings for the lump to go away. You also can use a manual (hand) or electric pump for a few minutes to help draw out the clogged milk while gently massaging the area.
- Apply cold compresses (ice wrapped in a thin towel) between feedings.
- If the lump doesn't go away within a couple of days, or if you have a fever, chills, aches, or red streaking, call your doctor.
Mastitis. This is an inflammation of the breast. If your breasts are sore; have red streaks; or have a hard, red area, you may have mastitis. Some women also get a fever and chills. If you think you have mastitis, call your doctor. In the meantime, continue to breastfeed or pump to drain the milk from your breasts. Switch between warm compresses and gentle massage right before breastfeeding and then apply cold compresses after a session. Mastitis caused by an infection may need treatment with antibiotics.
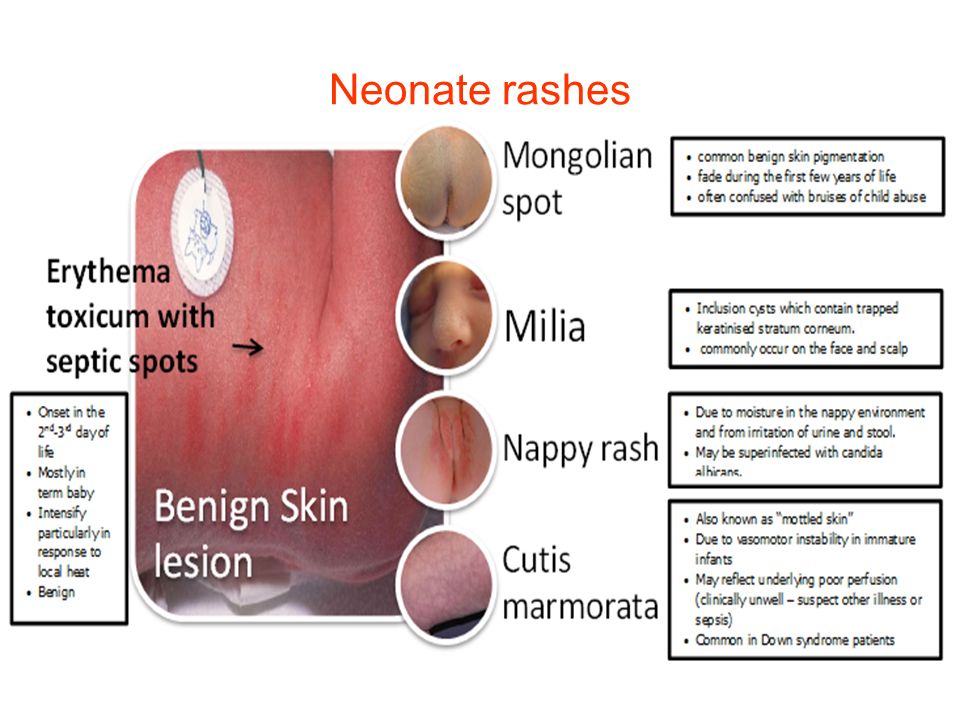
Oral thrush. Sometimes babies develop a yeast infection in the mouth called oral thrush. Babies with this have cracked skin in the corners of the mouth, and whitish or yellowish patches on the lips, tongue, or inside the cheeks. The infection can spread to your breast and cause:
- shooting or burning breast pain either during or after feedings
- pain deep within your breast
- strong pain in the breasts or nipples that doesn't get better after your baby properly latches on or you reposition your baby
- nipples that are cracked, itchy, burning, or are pink, red, shiny, flaky, or have a rash with little blisters
Call your doctor if you or your baby have any of these symptoms.
Inverted or flat nipples. Women who have inverted nipples (nipples that turn in rather than stick out) or flat nipples (that don't become as erect as they should when a baby is nursing) may have a harder time breastfeeding or have nipple pain. If either is the case, talk to your doctor or a lactation consultant about ways to make nursing easier and reduce any pain.
How Can I Ease Breast or Nipple Pain?
During Feedings
- Nurse first on the side that's less sore and vary breastfeeding positions.
- Make sure your baby latches onto your breasts correctly. If breastfeeding is too painful, it may be more comfortable to drain your breasts by pumping the milk.
- If you have sore nipples, ask a lactation consultant or your health care provider if a nipple shield is a good idea. Nipple shields go over the areola and nipple during a feeding to protect sore or cracked nipples. They should only be used when recommended by your care team as they can sometimes affect milk supply.

- Gently break the suction when removing your baby from your breast. Slip your finger in the side of your baby's mouth, between the gums, and then turn your finger a quarter turn to do so.
- At the end of a feeding, massage some breast milk onto your nipples, and then let them air dry.
Between Feedings
- Gently massage the sore area before nursing.
- Use wet or dry heat on your breasts (a warm shower, water bottle, heating pad, or warm washcloth) right before feeding. But if you have a yeast infection in your breast, you'll need to keep your nipples dry because yeast thrives on moisture. Get plenty of rest and fluids.
- Put ice packs or cool compresses on engorged breasts after feedings.
- Make the area where you feed your baby comfortable. Sit in a glider or a cozy chair with armrests. Footstools and pillows can give extra support. Some women like wraparound nursing pillows or "husband" back pillows with arms on each side for nursing in bed.

If breastfeeding is painful or uncomfortable for you, callyour doctor or lactation consultant for help.
Breastfeeding – mastitis and other nipple and breast problems
Nipple or breast pain is not normal
Nipple or breast pain is not a normal part of breastfeeding. Your nipples may be sensitive in the first few days after birth and while breastfeeding, but sore nipples or breasts indicate a problem. If you feel pain, you should seek help immediately.
Blood in breastmilk
If there is a small amount of blood in your breastmilk because of nipple trauma, it will not harm your baby. You can continue to breastfeed unless the pain becomes unbearable.
Breastfeeding parents with some medical conditions (such as hepatitis B or hepatitis C) may be advised to stop breastfeeding temporarily until the nipples have healed and there is no blood in the breastmilk. If this is the case, you can express breastmilk in replacement of a breastfeed to maintain your supply and discard your breastmilk until your nipples have healed.
Tips on caring for your nipples
To prevent nipple problems:
- Ensure correct positioning and attachment of your baby when feeding.
- Avoid soaps and shampoos on the nipples during showering.
- Avoid nipple ointments, powders and tinctures (drug dissolved in alcohol). They may increase nipple problems.
- Leave milk or colostrum to dry on your nipples after breastfeeding. They both contain anti-infective agents.
- Change breast pads frequently. Don’t use pads that hold moisture against the skin.
- If nipple pain or nipple trauma is not improving, seek help from your doctor, lactation consultant or an Australian Breastfeeding Association counsellor.
Some mothers find it more comfortable without a bra. Large-breasted women are usually more comfortable with the support of a properly fitted maternity bra. Breast shells can be used to protect sore nipples. These are silicone with a hard plastic dome to prevent clothing from touching nipples and allowing them to air.
Incorrect attachment is the main cause of nipple problems
Incorrect attachment of the baby onto the breast is the most common cause of nipple pain. Slightly changing the position of the baby on the breast should help. Your midwife, lactation consultant or an Australian Breastfeeding Association counsellor can show you how to attach the baby properly or talk to you about baby-led attachment.
The Australian Breastfeeding Association has a breastfeeding basics video which explains positioning and attachment.
Breastfeeding with inverted nipples
If you have flat or inverted nipples, patience may be needed while you and your baby learn to breastfeed. Strategies that can help include:
- Breastfeed within the first hour of birth – when the baby is alert and ready to suck.
- Use the baby-led attachment technique – immediately after the birth and in the first few days.
- Express either by hand or with a pump to draw out the nipple – use a cup, spoon or finger to feed the milk to the baby if necessary.

- Avoid the use of bottles and dummies as these involve a different sucking action to breastfeeding.
- Occasionally, the use of a nipple shield for breastfeeding with flat or inverted nipples is helpful – the clear silicone types are the most suitable. Ensure the nipple shield used is the correct size for your nipple. Once the baby is sucking well and the nipple is drawn out, the shield may be removed. When using a nipple shield, the baby should still be correctly positioned and attached to the breast.
Breast and nipple thrush
Breast and nipple thrush (a fungal infection) may occur in the first weeks after birth, but can develop at any time. Signs and symptoms include:
- Severe, burning nipple pain for the entire breastfeed – correct attachment does not alter the pain. Burning nipple pain is continuous, not just during feeds. Breast pain may vary with nipple and/or breast. There may be sharp, shooting, burning, stabbing or radiating pain throughout the breast.

- The nipples may be a brighter pink than normal and may be shiny. They may, however, look normal.
- Thrush in the baby’s mouth or on the buttocks.
How to tell if your baby has thrush
Oral thrush appears as white spots in your baby’s mouth that cannot be wiped away. When thrush occurs around the buttocks, it causes a red rash on the skin with spots around it. Your doctor will be able to assess whether your baby has thrush.
Treating thrush – mother
Treatment includes:
- Nipple and breast thrush is treated with antifungal medicine and antifungal nipple gel or creams. Antifungal gels and creams include nystatin, clotrimazole and miconazole. These are applied to the nipple after each feed. Oral antifungal treatment such as fluconazole may also be used.
- Air the nipples or go without a bra.
- Change breast pads frequently to keep your nipples dry.
- Good hygiene – wash your hands after touching your breasts, using the toilet or changing nappies.

- Vaginal antifungal pessaries, if you also have vaginal thrush. It is advisable to consult your doctor.
- Wash bras and nursing pads and towels separately from nappies in hot soapy water and dry all of them in the sun where possible.
Some mothers find it helps to reduce sugar and yeast in their diet. See your doctor or other medical advisor if thrush persists.
If you or your baby have been diagnosed with thrush you will both need to be treated.
Treating thrush – baby
Treatment includes:
- Nystatin liquid or miconazole gel for oral thrush.
- Antifungal ointments for thrush around the buttocks.
- If you use dummies or teats these should be washed thoroughly after use and sterilised either by using a steam steriliser or by placing the dummies and teats in boiling water for 5 minutes. If possible, replace the dummies and teats weekly if you or your baby has thrush.
Bacterial infection of the nipples
Research has found that a bacterial infection of the nipples can be mistakenly diagnosed as nipple thrush or may be present in conjunction with thrush.
Treatment with an antibacterial ointment or a combination antibacterial and antifungal ointment will often heal unresolved ‘thrush’. A combination ointment like kenacomb may be recommended or an antibacterial such as mupirocin. An oral antibiotic can also be used.
Your doctor may send a swab of the nipples to be cultured, to identify the most appropriate antibiotic to use.
Dermatitis (skin irritation) around the nipple
Dermatitis around the nipple and areola can be caused by:
- Ointments and creams you are using on the nipples – stop using them if you develop dermatitis.
- Detergents used to wash your bra, breast pads or undergarments – use pure soap, rinse well and dry in the sun.
- Sensitivity to soaps or shampoo.
- Reaction to the fabric of your bra or bra pads – it may be helpful to go without a bra.
- Sensitivity to the moisture-absorbing gel in some disposable nursing pads.
- Sometimes you may react to complementary foods remaining in your older baby’s mouth after they have eaten.

Nipple eczema can cause considerable pain
Eczema may occur on the nipple and areola. Nipple eczema can cause considerable pain and discomfort for a few women.
Eczema causes inflammation of the skin, with a rash that may be dry or weepy. The rash is usually itchy and may be on both nipples and/or areola or just one. If the rash looks crusty or flaky a bacterial infection may also be present.
You will need to see your doctor and may need a referral to a skin specialist if you develop eczema. Dietary changes and a short, intensive course of cortisone cream may help.
Mastitis and breastfeeding
Mastitis means inflammation of the breast. It can be caused by blocked milk ducts (non-infective mastitis) or a bacterial infection (infective mastitis).
If a blocked milk duct is not cleared, flu-like symptoms such as fever, body aches and pains may develop. Milk duct blockages cause milk to pool in the breast and inflammation (pain and swelling). A cracked nipple can allow bacteria to enter the breast and cause an infection.
A cracked nipple can allow bacteria to enter the breast and cause an infection.
Symptoms of mastitis
Mastitis causes the breast or parts of the breast to become:
- tender or painful
- hot
- reddened
- hard and swollen.
Other symptoms can include:
- The skin may appear tight and shiny, and be streaked with red.
- You feel very ill (‘fluey’) and have a high temperature (over 38 °C).
How mastitis develops
Factors that predispose a woman to blocked milk ducts, which can lead to mastitis, include:
- Poor drainage of the breast – this can be caused by poor attachment of the baby at your breast or limiting your baby’s time at the breast.
- Engorgement of your breast due to a missed feed or delaying a feed.
- A tight or ill-fitting bra or consistently lying in one position during sleep.
- Holding your breast too tightly during feeding.
- Trauma such as a kick from a toddler or pressure from a seatbelt.

Other factors that predispose a woman to mastitis include:
- Poor physical health, being unwell and being anaemic.
- Using a nipple shield.
- Previous or recurrent blocked ducts.
- Nipple trauma caused by incorrect attachment of the baby during feeds.
- Interrupting feeds, cutting feeds short, by limiting feed times.
- The use of nipple creams, which can harbour bacteria.
- Secondary infection like thrush.
Preventing mastitis
To help prevent mastitis:
- Mothers and midwives should thoroughly wash their hands before touching the breasts after a nappy change.
- Make sure the baby is positioned and attached properly on the breast to assist in thorough breastmilk drainage.
- Avoid long periods between feeds. Feed frequently. Avoid skipping feeds, if replacing a breastfeed with a bottle, express to avoid blocked milk ducts or a reduction in your breastmilk supply.
- Wear loose, comfortable clothing.
 Bras, if worn, should be properly fitted.
Bras, if worn, should be properly fitted. - Avoid nipple creams, ointments and prolonged use of nipple pads.
- If the mother has been unwell, see a GP to rule out anaemia.
Treatment for mastitis
It is important to treat blocked milk ducts so they do not progress to mastitis. Options include:
- Making sure the baby is feeding well on the affected breast – offering the affected breast first can help.
- The application of heat for a few minutes before a feed, gentle massage of the affected area during feeding, and cold packs after a feed and between feeds for comfort.
- A change in feeding position.
- Frequent drainage of the breast using breast compression through breastfeeding and expressing.
If the blockage does not clear within 8 to 12 hours or you start to feel unwell, see your doctor.
Treatment for mastitis should begin immediately. Your doctor may not immediately be able to distinguish between simple inflammation and a bacterial infection, but will usually treat you as if it is infected.
Treatment includes:
- Continued breastfeeding and/or expressing to drain the breast. It is important to continue breastfeeding or expressing from both breasts. Start by offering the affected breast first to help clear the blockage. Your breastmilk is safe for your baby even if you have mastitis.
- Gentle massage toward the nipple when breastfeeding or expressing.
- Antibiotics (such as flucloxacillin or cephalexin).
- Anti-inflammatory medication (such as ibuprofen) and/or analgesia (such as paracetamol) to relieve pain, if necessary.
- Rest and adequate fluid intake.
- A warm cloth or heat pack on the affected area may help the milk flow before feeding or expressing. Make sure the cloth or heat pack is not too hot.
- Applying a cold pack wrapped in a cloth after breastfeeding or expressing may help to reduce the inflammation and pain.
- Varying the feeding position to increase breast drainage.
If you wish to stop breastfeeding, it is important to wait until the mastitis has cleared up.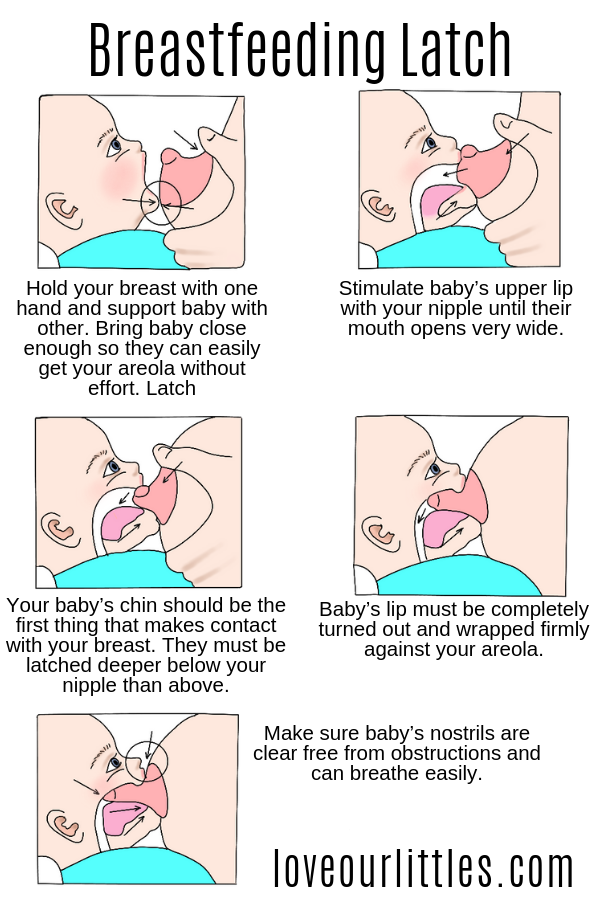 Rapid weaning may lead to a breast abscess.
Rapid weaning may lead to a breast abscess.
Other causes of nipple and breast problems
Nipple trauma can occur when a breast pump has been used incorrectly or from failing to break the suction before removing the baby from the breast (this is done by sliding a clean finger into the corner of your baby’s mouth).
Nipple vasospasm occurs when blood vessels tighten causing pain during, immediately after, or between breastfeeds. It is usually worse when you are cold or have a history of Raynaud’s phenomenon. Nipple vasospasm can cause intense nipple pain. With nipple vasospasm you may see colour changes in your nipple from whitened to purple or red, then back to normal colour. Speak to your doctor, midwife or a lactation consultant if you think you may have nipple vasospasm.
Tongue-tie is a condition in which the thin piece of tissue under a baby’s tongue is abnormally short and may restrict the movement of the tongue. It may interfere with a baby’s ability to latch and suckle at the breast, leading to nipple pain and trauma. If you are concerned that your baby may have tongue-tie which is affecting breastfeeding speak with your doctor, paediatrician, midwife, maternal and child health nurse or lactation consultant.
If you are concerned that your baby may have tongue-tie which is affecting breastfeeding speak with your doctor, paediatrician, midwife, maternal and child health nurse or lactation consultant.
Where to get help
- Your midwife
- Your GP (doctor)
- A lactation consultant – contact Lactation Consultants of Australia and New Zealand (LCANZ) Tel. (02) 9431 8621
- Australian Breastfeeding Association Breastfeeding Hotline Tel. 1800 686 268
- Your maternal and child health nurse
- Maternal and Child Health Line Tel. 13 22 29 (24 hours)
- Breastfeeding clinics – many hospitals have programs which assist women with infant feeding problems
- The Royal Women’s Hospital Breastfeeding Service Tel. (03) 8345 2400
- NURSE-ON-CALL Tel. 1300 606 024 – for expert health information and advice (24 hours, 7 days)
Why does my breast hurt when I feed
Mammology
Breastfeeding gives a young mother pleasure and helps to realize the happiness of motherhood. In cases where the chest hurts after feeding, it is necessary to immediately make an appointment with a mammologist in order not to miss the development of serious diseases in the earliest stages.
In cases where the chest hurts after feeding, it is necessary to immediately make an appointment with a mammologist in order not to miss the development of serious diseases in the earliest stages.
Causes of chest pain during feeding.
response to the release of the hormone oxytocin. Under its influence, there is a strong contraction of the muscle fibers of the lactiferous passages, as a result of which an additional portion of milk is released.
Mothers feel pain at this time, which they characterize as squeezing or stabbing. In nulliparous or emotionally labile women, the reflex to oxytocin can manifest itself even at the mere thought of a child or at the moment when she takes the baby in her arms. Usually, after three months of lactation, this reaction gradually weakens.
Laktostasis. Very often, the chest of a nursing mother hurts when, due to poor patency of the milk ducts, thick milk or a very large amount of it, stagnation occurs in the milk lobules. At the same time, painful seals are felt in the mammary gland. The skin above them may be warmer and bluish due to venous congestion. With lactostasis, it is imperative to express the breast so that the seals disappear. Otherwise, mastitis can quickly develop.
At the same time, painful seals are felt in the mammary gland. The skin above them may be warmer and bluish due to venous congestion. With lactostasis, it is imperative to express the breast so that the seals disappear. Otherwise, mastitis can quickly develop.
Rapid breast filling with milk. During active sucking, in response to irritation of the nipple of the mammary gland, a large amount of the hormones prolactin and oxytocin are released, which stimulate the production of a new portion of milk. In such cases, not only does the chest hurt after feeding, but it also quickly fills with milk, swells and thickens. This phenomenon indicates the normal process of lactation.
Thrush. With candidal stomatitis in an infant, colonies of the fungus can penetrate the skin of the nipple of the mother's breast, and then into the milky passages with the development of thrush. At the same time, the colonies of the fungus are practically invisible, and the main clinical sign is the increased sensitivity of the nipples. Cutting or piercing stabbing pain, itching in the mammary glands are not cured by the usual antiseptics. It is very characteristic that the chest of a nursing mother hurts more precisely after the end of feeding.
Cutting or piercing stabbing pain, itching in the mammary glands are not cured by the usual antiseptics. It is very characteristic that the chest of a nursing mother hurts more precisely after the end of feeding.
Mastitis. As a result of inflammation of the area of lactostasis or when pathogenic microbes penetrate through the fissures of the nipple into the lactiferous lobule, a serous and then purulent process occurs, manifested by severe throbbing pain. The skin over the pathological focus becomes red and hot, often the body temperature rises. The mother needs urgent help from a gynecologist and a surgeon, as in advanced cases, an abscess of the mammary gland quickly develops.
Teat cracks due to improper technique of attaching the baby to the breast during feeding. The pain in the chest is most pronounced during feeding, and after it gradually subsides.
Compression of the chest by an incorrectly fitted bra, during prolonged exposure to an uncomfortable body position (for example, while sleeping on the stomach). In any case, do not delay the visit to the doctor, only he will be able to establish the correct cause of the pain and give the necessary recommendations or prescribe treatment.
In any case, do not delay the visit to the doctor, only he will be able to establish the correct cause of the pain and give the necessary recommendations or prescribe treatment.
More articles on this topic
Laktostasis in a nursing mother
The disease occurs when breast milk cannot pass through the ducts of the mammary gland due to their blockage. It is produced, but cannot go outside. Because of this, pain may occur.
Mammology
Breast cancer
Unfortunately, today many women suffer from breast cancer. This is a malignant formation. In most cases, this disease occurs in women over 40 years of age. However, he occasionally visits teenage girls.
Mammology
Laktostasis
This is a stoppage of milk flow from the milk ducts. As a result of this phenomenon, the formation of milk stagnation occurs. Peripheral tissues become compacted and edematous. Places of compaction turn red and become painful.
Peripheral tissues become compacted and edematous. Places of compaction turn red and become painful.
Mammology
ᐈ Breast pain during GV (breastfeeding) • Induration in a nursing mother
“Advise a mammologist!”
If you are a breastfeeding mother, you probably don't have much time. The child “hangs” on the chest, you get tired like never before in your life, you don’t often manage to sleep normally. What to say about the "campaigns" to the doctors.
It's much easier to go online, type in a symptom in a search engine, ask for advice on the mommies forum.
However, who guarantees that the advice will be correct and the condition will not worsen? The mammologists of our center understand your concerns and are ready to solve all the issues that arise with breastfeeding mothers.
You are breastfeeding. What's going wrong?
Not enough milk
| You think you don't have enough milk. |
| Violation of the rhythm of feeding, improper attachment, overwork. |
| The child is restless, gains or loses weight poorly. |
| Breastfeed more often, consult a mammologist and lactation consultant. |
Too much milk
| | You think there is too much milk. |
| Individual features, excess prolactin. |
| Too much milk is produced. |
| Change the rhythm of feeding, freeze excess milk, consult a mammologist and endocrinologist. |
Teat fissure
| Pain during feeding, skin defect, blood. |
| Heavy workload, slow recovery. |
| Restrict feeding to this breast for the duration of treatment, express adequately when filling, consult a physician for anti-inflammatories, antibiotics and physiotherapy as indicated. |
Milk stasis
| What's bothering you? | Pain and distension in the chest. |
| Possible causes? | Ejection of milk is uneven in different parts of the gland, there is no muscular wall in the milk ducts, and the outward movement of milk is also uneven. The ducts may be compressed or twisted. The ducts may be compressed or twisted. |
| How does it manifest itself? | Painful, tight-elastic lump in the breast, does not disappear after feeding, without fever and redness. |
| What to do? | Change position during feeding, pumping, applying ice, contacting a mammologist, doing ultrasound, microflora culture (bacteria culture), secretion cytology |
| What worries you? | Depends on the stage - first, a painful focus of compaction, a decrease in the amount of milk, an increase in body temperature up to 38 degrees. Further, the focus increases, there is swelling of the skin, axillary lymph nodes, high temperature, impurities in the milk. Further, redness joins, swelling increases, weakness, drowsiness, palpitations, the amount of impurities increases. |
| Possible causes | Unemptied stagnation, curdling of milk and clogging of the duct, penetration of infection through cracks leads to mastitis. |
| How does it manifest itself? | Depends on the stage - painful, stony density, swollen gland, redness of the skin, increased body temperature, symptoms of general intoxication, lactation is sharply reduced. |
| What to do? | Seek immediate medical attention, often requiring hospitalization and surgical treatment. |
There is a lump in the chest, it does not hurt
| What worries | Abruptly appeared soft and painless mass in the mammary gland, the condition is not disturbed. |
| Possible causes | Lactocele is an acute accumulation of milk in an overstretched duct. |
| How it manifests itself | The formation is soft-elastic, painless, appeared acutely, lactation is preserved. |
| What to do | Contact a mammologist, you need ultrasound, aspiration of contents with cytology. |
Breast lump, spotting
| Painless, firm mass without clear contours in the presence of normal lactation. Enlarged axillary lymph nodes on one or both sides. Bloody discharge from the nipples of one or both glands. | |
| Possible causes? | Suspicion of an oncological process due to hormonal changes during lactation. |
| How does it manifest itself? | The formation is dense, painless, axillary lymph nodes are enlarged, lactation is preserved, there is bloody discharge from the nipple. |
| What to do? | Contact a mammologist, you need ultrasound, mammography, biopsy, cytology, histology, comprehensive examination. |
How not to waste a breastfeeding mother's precious time? The CMC offers:
• Consultations of a competent mammologist with more than 15 years of experience with nursing mothers.
• Assistance in organizing breastfeeding - for ordinary issues we involve our consultant, in difficult situations - with the participation of our mammologist.
• Complete examination in 1-2 visits – we perform ultrasound, mammography, cultures, cytology and histology.
• Treatment of breastfeeding according to world standards: we perform therapeutic fine needle biopsy, therapeutic massage and pumping for lactostasis, conservative and surgical treatment.
1. What should a breastfeeding mother eat?
It is best if your diet is complete, balanced in proteins, fats and carbohydrates. It is advisable to drink fluids at least 2 liters per day. Milk will come to you more actively if you drink a cup of warm tea with milk before feeding.
2. What underwear to wear?
Choose by bust size and quality. Best of all - on a wide supporting strap, you can sport a cut. Your bra should not be constricting under your armpits or tight under your bust.