How can you tell if your child is tongue tied
4 Ways To Tell If Your Child Has A Tongue-Tie And What To Do About It - Alabama Tongue-Tie Center | Dr. Richard Baxter
It seems that everywhere you read online, a tongue-tie seems to be one of the first issues suggested when babies can’t eat or kids can’t speak well. Let’s go through some easy ways that parents can tell if their baby or child might be affected by this condition.
1. The Obvious
If your child has a heart-shaped tongue, a short tongue, can’t lift or stick out their tongue, there might be a problem. Sticking the tongue out is not a great test. Instead, ask your child to lift their tongue (or do it for them). If you can see an obvious string attaching near the top of the tongue, then there is very likely a restriction present that could be affecting your child. Go on to point #3.
2. The Not-So-Obvious
Many times a parent will think their child has some or all of the symptoms of a tongue-tie, but when they lift the tongue the string (frenum) isn’t attached to the tip or even near it. It’s 50% of the way back, or maybe even 25% visible or there might be no appearance of a frenum at all. A posterior tongue tie is a term that describes a less obvious variant of tongue restriction that is more common than the classic to-the-tip variety but is less easy to identify. Healthcare providers have not been taught about its existence in medical or dental school, or in continuing education courses.
The posterior tie is most easily identified by coming from behind the patient and lifting the tongue with both index fingers on either side of the tongue. The fascia or connective tissue bunches up and forms the appearance of a string or frenum, and often there is a good bit of tension as well. But the presence of this appearance alone does not mean the baby or child has a tie. They must be having symptoms in addition to the tight string of tissue in order to qualify as a tongue-tie.
You gotta lift it up to see it!
Notice the restrictive lip-tie and not obvious (at first) tongue-tie, until tension is applied.
3. The Symptoms
Regardless of the appearance under the tongue, it’s the symptoms that count. No symptoms, no treatment. If it ain’t broke, don’t fix it! Common infant and child symptoms are listed below. Contrary to popular opinion, none of these symptoms are required or the absence of a symptom doesn’t rule out a tongue-tie. Sometimes a tongue-tied infant has poor weight gain, other times they can be chunky and the mother is compensating for the inefficient feeding, or has a large milk supply. Sometimes nursing hurts worse than labor, other times there is moderate pain, and sometimes there is zero pain from a tongue-tied baby. (And very often, the painful latch happens in babies with a not-so-obvious posterior tongue-tie.)
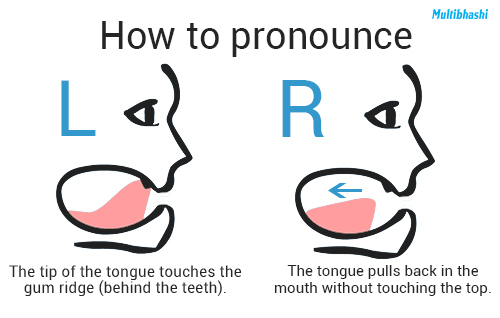
Some kids with a tongue-tie have perfect speech, others have a significant speech delay or speech issues with mumbling, clarity, sounds (R, L, S, etc.) and confidence. Same with feeding (slow and picky eating, especially with meat), and with sleep (restless sleep, snoring, teeth grinding, etc. ). So it’s the overall picture of the child’s limitations that are important. Look at all of the issues together, or check off a form like ours, the Infant Assessment Sheet or the Child Assessment Sheet. If you have more than a few checkmarks on there, there is likely a problem.
). So it’s the overall picture of the child’s limitations that are important. Look at all of the issues together, or check off a form like ours, the Infant Assessment Sheet or the Child Assessment Sheet. If you have more than a few checkmarks on there, there is likely a problem.
Infant’s Issues
- Poor latch
- Poor weight gain
- Reflux or spitting up often
- Clicking or smacking noises
- Gassy or fussy often
- Milk leaking out of the mouth
- Frustration with eating
- Prolonged nursing or feeding sessions
- Constantly hungry
Mother’s Issues
- Painful nursing
- Creased, flattened, blanched nipples
- Blistered or cut nipples
- Poor breast Drainage
- Plugged ducts or mastitis
- Nipple shield required for nursing
Child’s Issues
- Frustration with communication
- Trouble with speech sounds, hard to understand, mumbling
- Speech delay
- Slow eater
- Picky eater, especially with textures (meat, mashed potatoes)
- Choking or gagging on liquids or foods
- Spitting out food or packing food in cheeks
- Restless sleep (kicking or moving while asleep)
- Grinds teeth at night
- Sleeps with mouth open
- Snores (quiet or loud)
- Frequent headaches or neck pain
4.
 Trust Your Mother’s Instinct
Trust Your Mother’s Instinct
Sometimes you have to go with your gut. If you think something is “off” with your child, 99% of the time, something IS wrong. Even in the face of professionals telling you “it’s fine we see this sometimes,” or “all babies are fussy, gassy, colicky, etc.,” or “his siblings talk for him,” trust your instincts. It’s common for babies to be gassy and fussy, and not eat well, because frankly, tongue-ties ARE common (25% at our best current estimates). Because these symptoms are so common, they are confused for being normal.
Dental cavities are common, but not normal. If a baby is spitting up all the time, “toots” like a grown man, and milk leaks out everywhere when eating, those are common symptoms, but not normal symptoms. There is very likely a physical reason to explain those. And very often, it’s a lip or tongue-tie.
So What Should You Do About It?
It’s helpful to see a lactation consultant or feeding therapist if you are concerned with your infant or child’s feeding, but make sure they have contemporary knowledge of tongue or lip ties.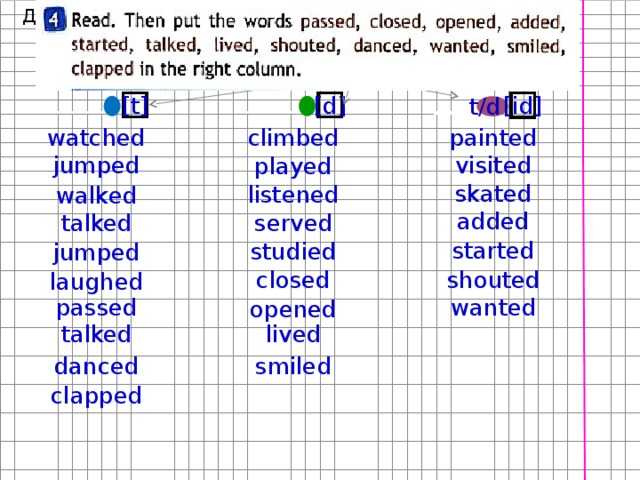 Ask if they have taken a course recently because it’s not taught in schools yet (even though it’s been around since Biblical times).
Ask if they have taken a course recently because it’s not taught in schools yet (even though it’s been around since Biblical times).
It’s also helpful to rule out other issues, so see the speech therapist, or a myofunctional therapist, and initiate therapy. But if the tongue-tie is obvious, no amount of therapy will correct a structural problem. If it is less obvious, then maybe therapy can help the issue, but if you hit a wall, or your child has symptoms in multiple domains (speech and feeding and sleep) then have the tongue-tie treated as part of a comprehensive therapy plan, working alongside your therapist’s recommendations.
That’s why it’s so critical to find a therapist who has gone out of their way to gain knowledge (or here, or here, or here, lots of options for education!) in this emerging field of tongue and lip-ties, or tethered oral tissues (TOTs). At the same time, we have seen children who have been in therapy for years, or even over a decade, that had a significant to-the-tip or close to the tip tongue-tie! The dentist, pediatrician, therapist, no one even mentioned it to the parent.
Make sure you have your child evaluated by a knowledgable provider, who has taken additional CE courses, attended recent conferences on tongue-ties, treats them routinely (several a week at least), and assesses for all the symptoms and possible presentations (anterior and posterior tongue-tie). It’s a spectrum of restriction, and some are obvious, other tongue restrictions are barely visible. Ensure they recommend stretches and exercises in addition to treatment, and ask what method they use to release.
Educate yourself on the effects a tongue restriction can have on an infant, child, or adult, and spread the word. We have some additional information on our webpage, The Facts.
We’re trying to spread the word with our recent book, Tongue-Tied: How a Tiny String Under the Tongue Impacts Nursing, Speech, Feeding, and More (download PDF sample here) as well as our latest article published in Clinical Pediatrics on the functional improvements after a proper tongue-tie release.
In our study (download the PDF here!), 89% of the children had improved speech after the procedure, 83% had better feeding, and 83% had better sleep. So it’s not every child has improvements in every area, but many do. When combined with therapy, those numbers are even better.
If you are a parent and concerned your child might have a tongue-tie, we’d be happy to chat with you or schedule a consultation. Just call us at 205-419-4333 or send us a message.
If you are a provider and have any questions about this post, or want to learn more, check out our recent course, Tongue-Tied Academy designed to help providers learn the procedure and Tongue-Tied Academy LITE for therapists who want to learn more. There is even a free preview of the course available. You can use the coupon code BLOG to save $250 off the full version or save $50 off the LITE version.
How to Tell if Your Baby is Tongue-Tied – Children’s Health
Share:
When you have a newborn in the house, your whole world suddenly revolves around the baby. Naturally, you search for the latest information to make sure your little one is eating right, sleeping right, and is happy and healthy. Keeping them fed is a priority, and sometimes it can be surprisingly challenging.
Naturally, you search for the latest information to make sure your little one is eating right, sleeping right, and is happy and healthy. Keeping them fed is a priority, and sometimes it can be surprisingly challenging.
One issue that new parents might hear about is tongue-tie, especially if their baby is having trouble breastfeeding.
So what is tongue-tie, and do you need to worry? Read on to learn about how to tell if your baby is tongue-tied.
What does it mean when a baby is tongue-tied?
Everyone is born with a bit of tissue under the tongue, called a frenum or frenulum. It connects the bottom of the tongue to the floor of the mouth. Tongue-tie is when the tissue under the tongue is too short or too thick and restricts the tongue's range of motion. The medical term for tongue-tie is ankyloglossia.
"In some cases, the central part of the tongue cannot elevate, which is why people say it is 'tied' to the floor of the mouth," explains Felicity Lenes-Voit, M. D., Pediatric Otolaryngologist with Children's Health℠ and Assistant Professor of UT Southwestern. "When looking for tongue-tie, we also examine several other factors related to the tongue's movement, which include how well it moves side to side, how well the tongue 'cups' while sucking and if there is a wavelike motion from the front to the back of the tongue."
D., Pediatric Otolaryngologist with Children's Health℠ and Assistant Professor of UT Southwestern. "When looking for tongue-tie, we also examine several other factors related to the tongue's movement, which include how well it moves side to side, how well the tongue 'cups' while sucking and if there is a wavelike motion from the front to the back of the tongue."
How common is tongue-tie?
Tongue-tie may affect 4-11% of newborns and infants, though an exact number is not known.
"It could be that even up to 25% of babies have some degree of tissue under their tongues, but we see a wide variety and severity, and not every baby needs corrective surgery or treatment," says Dr. Lenes-Voit.
What does tongue-tie look like?
To check for tongue-tie, you can look at the shape of your baby's tongue. If your baby is tongue-tied, the tip of the tongue may look like a little heart. That's because the tissue that attaches the baby's tongue to the bottom of the mouth is too short or too thick. It tethers or pulls down the tongue in one area, causing the tip of the tongue to form a heart shape.
It tethers or pulls down the tongue in one area, causing the tip of the tongue to form a heart shape.
You might see this heart shape when the baby is crying or lifting the tongue. If you don't see it, you might notice other signs or symptoms of tongue-tie.
What are tongue-tie symptoms in babies?
Typically, parents first notice signs of tongue-tie in babies during breastfeeding. Babies with tongue-tie might:
- Cause pain with breastfeeding
- Compress the breast rather than suck
- Have noisy feeding sessions as they swallow lots of air (this can also be related to positioning issues or reflux)
- Have trouble latching when breastfeeding
- Not make enough wet or dirty diapers
- Require long feeding times
Other signs that a baby might have tongue-tie include if the baby cannot:
- Lift the tongue to the roof of the mouth
- Keep a pacifier in the mouth (though many babies without tongue-tie also refuse pacifiers)
- Move the tongue from side to side
- Move the tongue past the gumline where teeth will grow
As children get older, parents often worry about a tongue-tie causing speech problems, but there is no scientific evidence to support this.
Not all symptoms mean your baby is tongue-tied
If your baby has trouble taking a pacifier or nursing, this doesn't necessarily mean your baby has tongue-tie.
"Breastfeeding can take a lot of work. Teaching a baby to develop a good latch takes time and patience," says Kandi Trevino, SLP, a Speech-Language Pathologist at Children's Health who cares for babies with tongue-tie.
To improve breastfeeding, the mother and baby may need to try another position. If feeding issues continue, your baby may need a thorough evaluation to check other physical factors that can affect feeding.
"Sometimes the baby's inability to generate good suction while feeding is an issue with the overall oral motor function or the coordination of the suck, swallow, breathe reflex," says Dr. Lenes-Voit. "Maybe the baby has issues with muscle tone or strength. If a baby is having to take frequent breaks to breathe while eating, or ever stops breathing or turns blue, they need to be evaluated. "
"
What should you do if you think your baby has tongue-tie?
If you're concerned about tongue-tie symptoms in your baby such as feeding issues, start by talking with your pediatrician or a lactation consultant.
"Go to someone who is very knowledgeable and will consider the big picture, and not recommend a tongue-tie procedure unnecessarily," advises Trevino.
Your pediatrician may refer you to a pediatric ear, nose and throat (ENT) specialist for further evaluation.
"It's important that we perform a comprehensive evaluation and make sure nothing more serious than tongue-tie is going on," says Dr. Lenes-Voit. "Certainly, if a mother experiences pain every time a baby feeds, and no matter what she tries, the baby cannot latch properly, that's concerning. If tongue-tie is the reason for the pain and feeding problems, we can intervene. The ability to nurse is incredibly precious for many parents, and we support that.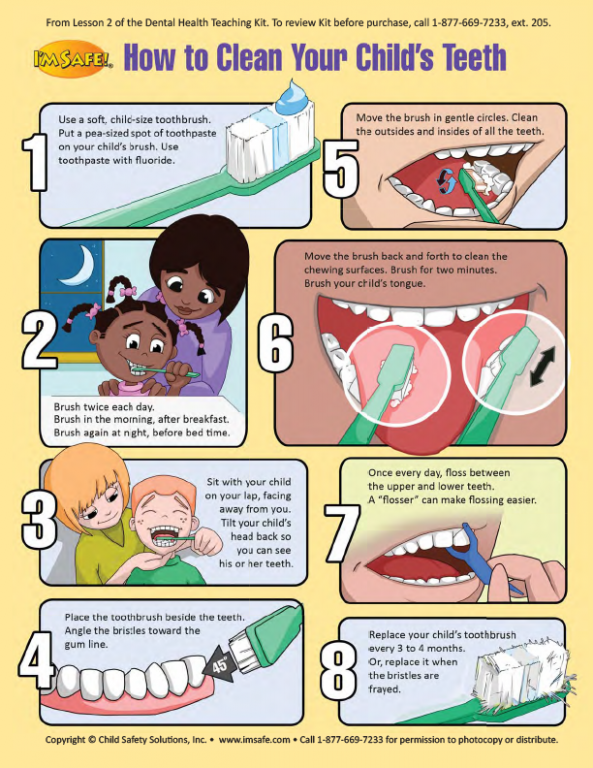 "
"
How is tongue-tie treated?
If treatment is needed, your pediatrician or ENT specialist can perform a frenotomy, removing part of the tissue that restricts the baby's tongue movement. If your baby is less than 3 months old, the procedure can be performed in the physician's office. If the baby is older than 3 months, the doctor will treat the baby in a hospital setting. Typically, babies do very well after treatment.
See more advice for feeding a baby with a tongue-tie, including after a frenotomy.
Learn more
The Pediatric Ear, Nose and Throat program at Children's Health provides convenient, accessible ENT care to families. If you're concerned about tongue-tie in babies, contact us for a comprehensive evaluation or second opinion in our Multidisciplinary Tongue-Tie Clinic.
Children’s Health Family Newsletter
Get health tips and parenting advice from Children’s Health experts sent straight to your inbox twice a month. Sign up now.
Sign up now.
If your child has an erased form of dysarthria.
Many children with disabilities come to the speech therapist at the CPC. Most of them are diagnosed with dysarthria, but they look quite normal, like all ordinary children. And the terrible word "dysarthria" does not seem to suit them at all. After all, dysarthria means a violation of the supply of a nerve signal from the brain to the muscles of the articulatory apparatus, as a result of which the face is inactive, amimic, the lips are clamped or the corners are lowered down. For some, the mouth does not close and the tongue falls out of the mouth. Recently, there have been a lot of dysarthric children with mobile facial muscles, emotional, smiling well, many do not even have salivation, but when you ask to stick out your tongue, you see a depressing picture. The tongue is thick, tense, when stretched it shrinks into a ball. It immediately becomes clear that this is dysarthria, but since there are no obvious external signs and signs of a violation of the prosodic side of speech, we diagnose an erased form of dysarthria. It is often confused with complex dyslalia, since the pronunciation of many sounds is disturbed here and there, but with dyslalia, the child’s tongue is quite normal, and with dysarthria, it is hyper or hypotonic. How to treat the erased form of dysarthria - we will tell in detail. nine0003
It is often confused with complex dyslalia, since the pronunciation of many sounds is disturbed here and there, but with dyslalia, the child’s tongue is quite normal, and with dysarthria, it is hyper or hypotonic. How to treat the erased form of dysarthria - we will tell in detail. nine0003
Signs of obliterated dysarthria.
Typically, dysarthric children are distinguished by clumsiness, impaired coordinated movements, and underdevelopment of finger motor skills. They hardly master the skills of fastening buttons, lacing, do not know how to hold scissors, do not like to draw and sculpt. But in practice in recent years there have been many children 5-7 years old with good coordination and developed fine motor skills of their hands, they love to draw, paint, sculpt, hold a pencil well, successfully cope with shading. Signs of the disease are visible only on the face, and even then not in everyone. One of the noticeable signs of erased dysarthria: a static sedentary face, tense lips or, conversely, sagging lips and cheeks, the mouth does not close.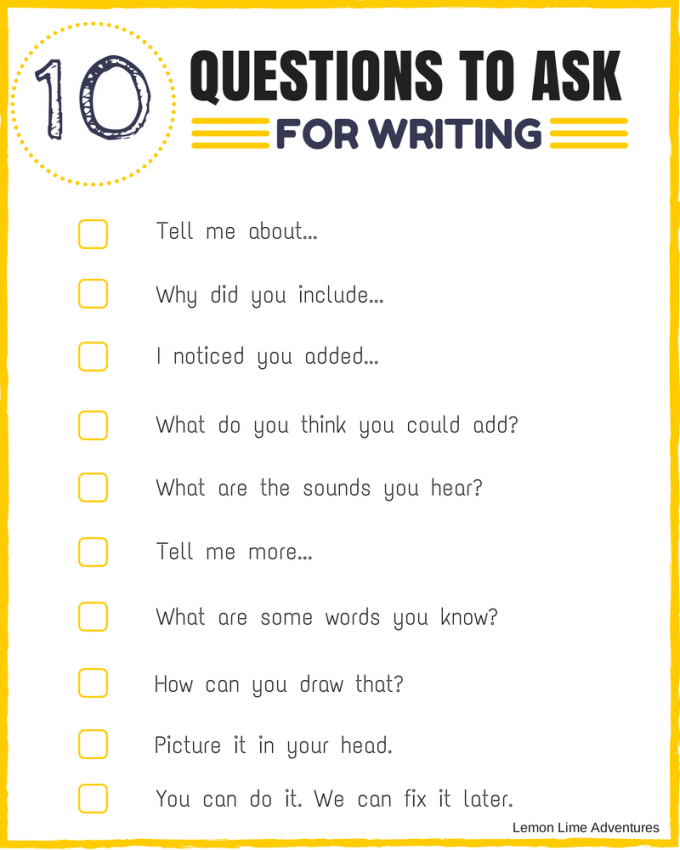 nine0003
nine0003
Of particular interest in the erased form of dysarthria is the tongue. In most cases, the tongue is thick, massive, and when pulled out, the back of the tongue tenses and gathers into a ball. Due to this, the pronunciation of many sounds is difficult for the child. When pronouncing hard sounds, soft sounds are heard, since the back of the tongue automatically rises to the sky, as a result, instead of [n] we hear [n '], instead of [b] - [b '], instead of [s] - [s '], instead of [s] - [s '], etc. The tense back of the tongue closes the hole for the free passage of the air stream, so whistling and hissing sounds have an overtone [c]. When syllables and words are repeated, many sounds acquire overtones [l']. For example, tya-tya-tya sounds like tlyat-tlyat-tlya. The tip of the tongue with erased dysarthria is usually not expressed, that is, it is impossible to determine where the tip is. Often, due to the paresis of the muscles of the tongue, the child cannot lift it up, lick the upper lip, or reach the upper teeth with the tip. In this regard, the baby does not have hissing sounds and [p].
In this regard, the baby does not have hissing sounds and [p].
Many children there is a deviation - deviation of the tongue in the direction of the paralyzed muscle. When you ask the child to pull out the tongue and hold it on the lower lip for a count of five, the tongue shakes, trembles and strives to move to the side. This is a clear sign of dysarthria. Due to hyperkinesis, the pronunciation of a group of whistling, hissing and sonorous sounds is disturbed, and prosody also suffers. Speech is inexpressive, slurred, inarticulate, monotonous, often quiet, with a slight crackle in the sound, nothing can be made out. They say about such children: "he has porridge in his mouth." nine0003
A distinctive feature of dysarthria is their unstable psyche. Such children often rush from one extreme to another. Either they are overly touchy, vulnerable, whiny, painfully react to every little thing, then they become aggressive, rude, refuse to study, talk, and even throw themselves at others with their fists. Dysarthric children have very reduced motivation and motivation to learn.
Dysarthric children have very reduced motivation and motivation to learn.
Help for a child with an erased form of dysarthria.
The diagnosis of dysarthria is made only by a neurologist or therapist. If such a diagnosis is recorded in the child’s card, the approach to treating dysarthria should be comprehensive. The pedagogical intervention of one speech therapist is not enough. Here, medical support and a course of massage of the collar zone are required to relieve muscle tension in the neck, chin and organs of the articulatory apparatus. In the classroom with a speech therapist, in addition to training in sound pronunciation, manual massage of the face and probe tongue is necessary. nine0003
Manual speech therapy massage.
In case of hypertonicity, it is necessary to do a relaxing facial massage, in case of hypotonicity, firming. To normalize the muscle tone of the cheeks do the following exercises:
- Standing in front of the child, place two fingers, index and middle, under the lobes, pressing slightly, begin spiral movements along the cheeks past the corners of the mouth to the center of the chin (5-6 times ).
 To strengthen the muscles of the cheeks - movements are made in the opposite direction from the center of the chin to the earlobes. nine0056
To strengthen the muscles of the cheeks - movements are made in the opposite direction from the center of the chin to the earlobes. nine0056 - With the index and middle fingers, to achieve the effect of relaxation, we make spiral movements with a slight pressure from the earlobes to the wings of the nose. The reverse movement is the compression effect.
- We place the fingers of the brush at the temples and move with smooth sliding movements to the center of the forehead, where we make a light pressure, like a point. It is important that the fingers are elastic, rounded and springy. The effect of relaxation is achieved, the opposite effect does not occur in practice. This exercise is best done while standing behind the child. nine0056
- To achieve the effect of relaxation: the fingers of the hands are placed on the pads near the hair zone, (standing in front of the child), we begin sliding movements along the forehead down to the eyebrows with strong pressure. At the eyebrows, the fingers diverge, trying to cover the entire face.
 A sharp throw of the hands across the face to the neck is carried out, while the pads touch the face. Neck trapping is possible.
A sharp throw of the hands across the face to the neck is carried out, while the pads touch the face. Neck trapping is possible. - We place our thumbs at the bridge of the nose (to stand in front of the child), push through and start moving around the eyes, first moving to the lower part of the eyebrows and the edges of the eyes and returning to the bridge of the nose, the landmark is the bone on the bridge of the nose. On the soft part, the fingers should not slip off, pressing should be intense. nine0056
To relax the lips, use the following exercises:
- With index fingers, stretch the corners of the lips towards the ears, count to five - let go (better done behind the back of the child).
- Standing behind the child's back, place the index and middle fingers on the upper lip, stretch the lip as much as possible and then squeeze it as much as possible so that the lip folds seem to swell.
- Place the thumbs in the center on the lower lip, the rest of the brush is located under the chin.
 Exercise is best performed in front of the object. We begin grinding pulling movements along the lip with a slight movement to the right, then to the left. nine0056
Exercise is best performed in front of the object. We begin grinding pulling movements along the lip with a slight movement to the right, then to the left. nine0056 - We perform behind the back of the child. Index fingers set one on the left side of the upper lip, the other on the right side of the lower lip, move the fingers in opposite directions, moving the lips together with the fingers. A similar movement is performed in the opposite direction - "Arlekino".
Parents can do these simple exercises at home, but it is best to do them every day to enhance the effect. In speech therapy classes, a speech therapist also does a manual facial massage by connecting a probe tongue. nine0003
Correctional and pedagogical work.
At speech therapy classes, as well as at home every day, it is very important for a child with erased dysarthria to perform articulation exercises.
- To relax the tongue, the best exercise is “Knead the dough” : stick out the tongue, pronouncing “pya-pya-pya”, slap on the tongue with your lips, moving it back and forth, back and forth.
- To fix the upper rise of the tongue, it is useful to lick saucers after eating, spoons, and also perform exercise "Delicious jam" : lick the upper and lower lip alternately.
- "Let's brush our teeth" - run the tip of the tongue over the upper teeth, on one side, then on the other.
- "Painter " - we draw the tip of the tongue across the sky, as if we are painting the ceiling.
- When the muscles of the lateral edges of the tongue are paretic, exercise "Sled" is very useful : we pronounce the sound [And], at the same time we press the teeth on the lateral edges of the tongue, a hollow appears in the middle of the tongue like in a sleigh. nine0012
Parents should prepare in advance for the fact that the production of sounds in dysarthria is difficult and slow due to the peculiarities of the muscle tone of the tongue. Even more slowly is the automation of sounds from 3 to 7 months, this is a distinctive feature of corrective work in the case of erased dysarthria.  Surprisingly, often the automation of even the simplest sounds, such as [l '], takes a very long time. Parents sometimes think that speech therapy classes do not bring the desired results, but this is not so. nine0012 Classes always have at least a small, but result, since the muscles of the tongue relax gradually and with constant mechanical and physical impact. Practice shows that when using an integrated approach in the treatment of an erased form of dysarthria, the improvement in sound pronunciation occurs much faster. And with regular exposure to the tongue with probe massage, muscle tone returns to normal after three months of use. You just need to be patient and actively cooperate with a neurologist, masseur and speech therapist. nine0003
Surprisingly, often the automation of even the simplest sounds, such as [l '], takes a very long time. Parents sometimes think that speech therapy classes do not bring the desired results, but this is not so. nine0012 Classes always have at least a small, but result, since the muscles of the tongue relax gradually and with constant mechanical and physical impact. Practice shows that when using an integrated approach in the treatment of an erased form of dysarthria, the improvement in sound pronunciation occurs much faster. And with regular exposure to the tongue with probe massage, muscle tone returns to normal after three months of use. You just need to be patient and actively cooperate with a neurologist, masseur and speech therapist. nine0003 When it's time to take your child to the orthodontist Make an appointment
Correction of bite Dentistry for teenagers
10/19/2021
There are so many things to keep an eye on as your child grows! And teeth are no exception. In the absence of any complaints, a visit to the orthodontist is recommended at the age of 3-3.5 years. Then, when the child is 5.5-6 years old. Well, closer to the full formation of bite - at the age of 10-11 years. And what should you pay attention to? What complaints can be addressed to the orthodontist? nine0003
In the absence of any complaints, a visit to the orthodontist is recommended at the age of 3-3.5 years. Then, when the child is 5.5-6 years old. Well, closer to the full formation of bite - at the age of 10-11 years. And what should you pay attention to? What complaints can be addressed to the orthodontist? nine0003
Irregular teeth
You visually notice that permanent teeth are growing unevenly (this can be age 5 years or older). Milk teeth that grow unevenly, with turns, are not an indication for orthodontic treatment and do not require correction. If during the eruption of the first permanent teeth (usually the lower incisors) you see that the teeth erupt unevenly, or begin to erupt from the side of the tongue, this is a reason to contact the orthodontist. Most often, the first permanent teeth erupt at the age of 5.5-6.5 years. It is important not to miss the moment: during this period, the child's jaws are actively growing - this is the most effective time when we can help create space for erupting teeth. nine0003
nine0003
Bad habits
In dentistry, “bad” habits include sucking a nipple, finger, lips, biting lips or tongue, habitually holding various objects in the mouth. If you have discovered bad habits in your child, a visit to the orthodontist is recommended, regardless of the age of the child and the stage of formation of his bite. Why are bad habits dangerous? They form the wrong bite. The mechanism of malocclusion is associated with the prolonged presence of some object that should not be between the teeth - be it a finger or tongue. So, for example, sucking a finger, nipples (if the habit persists in children for more than 2 years) - leads to the formation of a narrow upper jaw, protrusion of the front teeth forward, the formation of an open bite (when the teeth of the upper and lower jaws do not close vertically with each other). It can also lead to the formation of an underbite (when the upper and lower jaw do not correspond to each other when viewed from the side). nine0003
In the future, the protrusion of the anterior upper teeth due to bad habits leads to an increased risk of injury to the teeth, up to their loss. If you have discovered any bad habit in your child, it is important to contact an orthodontist as early as possible for recommendations and exercises to eliminate the bad habit and correct the bite, if violations have already occurred.
If you have discovered any bad habit in your child, it is important to contact an orthodontist as early as possible for recommendations and exercises to eliminate the bad habit and correct the bite, if violations have already occurred.
Mouth breathing
If you find that your child mainly breathes through the mouth, snores at night, I advise you to immediately contact an ENT doctor first. Orthodontic measures for oral breathing in children can be started from 3-4 years. Mouth breathing in children leads to a violation of the position of the tongue: the tongue descends down the oral cavity and ceases to occupy the desired position. So it does not have a stimulating effect on the upper jaw - and it does not develop in the proper volume. As a result, there is not enough space for permanent teeth, and they begin to grow unevenly. In addition, a narrow upper jaw can cause a habitual lateral displacement of the lower jaw. Crossbite and facial asymmetry will form. With oral breathing, it is important to work in conjunction with an ENT doctor and often with a speech therapist. In some cases (for example, if the cause of mouth breathing is allergic rhinitis), we also connect an allergist. The task of the ENT doctor is to normalize the airway so that the child can physically breathe through the nose. Further, the orthodontist and speech therapist are included in the work. The speech therapist works with the muscles of the lips and tongue to train them and teach them to work normally. The orthodontist eliminates the consequences of oral breathing and can also prescribe myogymnastics - training for the muscles of the lips, cheeks, tongue. nine0003
In some cases (for example, if the cause of mouth breathing is allergic rhinitis), we also connect an allergist. The task of the ENT doctor is to normalize the airway so that the child can physically breathe through the nose. Further, the orthodontist and speech therapist are included in the work. The speech therapist works with the muscles of the lips and tongue to train them and teach them to work normally. The orthodontist eliminates the consequences of oral breathing and can also prescribe myogymnastics - training for the muscles of the lips, cheeks, tongue. nine0003
Impaired pronunciation of certain sounds
If a child stubbornly does not pronounce some sounds, despite all the efforts made with a speech therapist, it makes sense to visit an orthodontist. It is advisable to do this after 5 years. The reason for the violations may be in the anatomical features or in the wrong bite. A short frenulum of the tongue, for example, can lead to impaired pronunciation of sounds. Open bite, "reverse" bite - also lead to speech distortion. The orthodontist will assess the degree of malocclusion or peculiarities of the anatomy of the frenulum of the tongue, give recommendations or prescribe treatment. nine0003
Open bite, "reverse" bite - also lead to speech distortion. The orthodontist will assess the degree of malocclusion or peculiarities of the anatomy of the frenulum of the tongue, give recommendations or prescribe treatment. nine0003
Asymmetry in the face, smile, bite
If you notice any signs of asymmetry in a child, this is a reason to immediately consult a doctor. At any age of the child - as soon as noticed. Of course, all people are naturally asymmetrical. But the natural asymmetry is not visible to the eye, does not draw attention to itself. What you need to pay attention to in terms of asymmetry: • shift of the chin to the side • the smile is not symmetrical • the central lines of the upper and lower jaws do not coincide (between themselves and with the central line of the face). The orthodontist will be able to examine and prescribe the necessary treatment or examination to identify the causes of asymmetry. nine0003
Early loss of deciduous teeth
Premature removal of deciduous teeth is a reason to visit an orthodontist at any age. Every tooth is needed and important for a child. If any of the temporary teeth is removed prematurely, it must be replaced. So that neighboring teeth do not move and do not take someone else's place, so that one-sided chewing does not form, so that the muscular balance between the lips and tongue is not disturbed and bad habits are not formed. To replace lost teeth in children, various designs of so-called prophylactic prostheses are used, which are selected individually, depending on the clinical situation. The task of these devices is to prevent other teeth from moving and to allow the child to chew (if the loss of teeth is significant). nine0003
Every tooth is needed and important for a child. If any of the temporary teeth is removed prematurely, it must be replaced. So that neighboring teeth do not move and do not take someone else's place, so that one-sided chewing does not form, so that the muscular balance between the lips and tongue is not disturbed and bad habits are not formed. To replace lost teeth in children, various designs of so-called prophylactic prostheses are used, which are selected individually, depending on the clinical situation. The task of these devices is to prevent other teeth from moving and to allow the child to chew (if the loss of teeth is significant). nine0003
Reverse incisor overlap
Reverse incisor overlap is when the lower teeth protrude). The reverse overlap blocks the normal growth of the maxilla in length. The most optimal time for correcting such an overbite is from 5-6 years. At this age, the incisors of the upper and lower jaws erupt and this is the most favorable time to start orthodontic correction.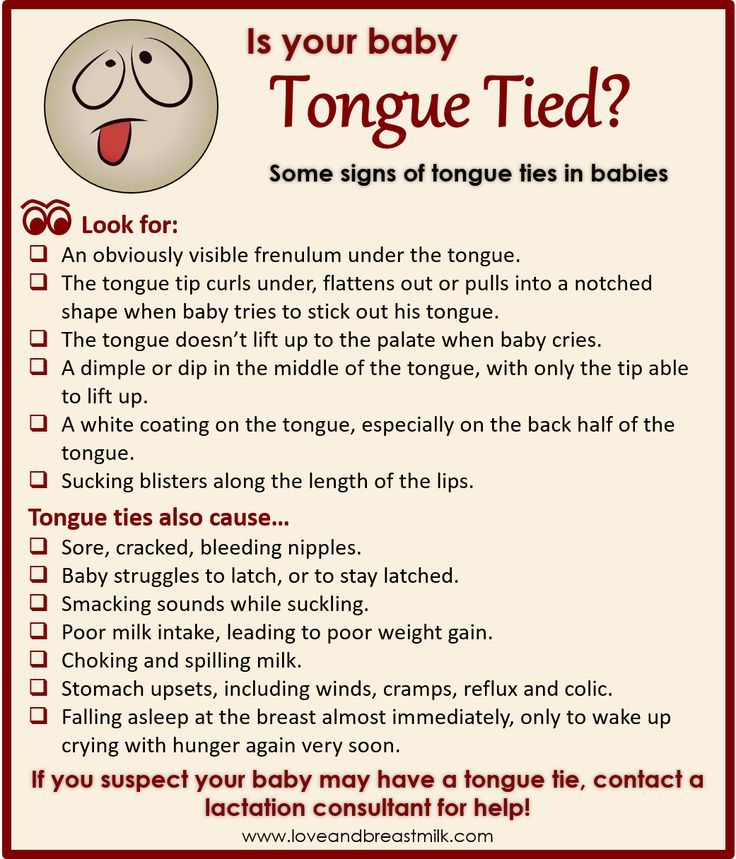 If you notice reverse overlap in a child at a later age, it is also important to see an orthodontist in order to get rid of the blockage of the upper jaw as soon as possible and allow it to grow further actively. nine0003
If you notice reverse overlap in a child at a later age, it is also important to see an orthodontist in order to get rid of the blockage of the upper jaw as soon as possible and allow it to grow further actively. nine0003
Large gap between maxillary and mandibular teeth
Large gap between maxillary and mandibular teeth increases the risk of injury to the anterior teeth. If the distance between the teeth of the upper and lower jaws is significant (6 mm or more), this increases the risk of injury to the front teeth. In this case, the orthodontist performs treatment aimed at reducing the risk of damage to the front teeth in children by reducing this gap.
No gaps between teeth at the age of 5-5.5 years.
At the age of 5-5.5 years, the jaws should already be very actively preparing for the change of milk teeth to permanent ones. The jaws should grow - after all, the permanent teeth are wider than the milk teeth, they will need more space. Gaps should appear between temporary teeth - both on the upper and lower jaws.