Cramping means in pregnancy
When Should Cramps During Pregnancy Be Worrisome?
New moms to be may feel a jolt of fear when they experience cramps during pregnancy. You might have it in your head that you’re in the middle of a miscarriage. In reality, most cramping during pregnancy is actually normal and is something that occurs during all three trimesters. It’s important to know why they happen.
Normal Cramps in Early Pregnancy
During your first trimester, you experience cramps as your body prepares for the pregnancy. You may initially experience cramping in your lower abdomen or lower back even before you know you’re pregnant. This is due to implantation, which is the process of the fertilized egg implanting in the uterus. You may feel a small twinge or sharper cramps that may double you over at times. After you know you’re pregnant, cramping is due to your uterus growing and expanding to accommodate your growing baby. It’s perfectly normal and happens to all women. Cramps often feel similar to your normal menstrual cramps. Once you pass your first trimester, you might experience occasional cramping. It’s important to remember that the uterus is a muscle, which means it can contract and cause pain or discomfort. The same can happen when you have gas, constipation, bloating, or even a full bladder.
Normal Cramps in Later Pregnancy
You may experience less cramping in your second trimester compared with your first and third trimesters. Generally, moms who are pregnant with multiple children experience more cramping during the second trimester compared to those who are having a single baby. This typically occurs as the body is making more room to accommodate the babies. In women carrying single babies, this occurs in the third trimester.
Abnormal Cramps During Pregnancy
Any cramping that seems out of the ordinary, such as cramps that feel severe and that don’t go away, should be reported to your doctor. It’s possible that you’re perfectly fine, but it’s important to be absolutely sure just to be safe. Sometimes, severe cramping can signify an ectopic pregnancy, which occurs when the fertilized egg implants in one of the fallopian tubes instead of the uterus. Ectopic pregnancy is a very serious, dangerous condition that requires immediate surgery as the pregnancy cannot be sustained. It can also threaten the mom’s health if the fallopian tube ruptures. Cramping on one side should also be reported to your doctor as it might mean an ectopic pregnancy. Cramping accompanied by vaginal bleeding should also be immediately reported to the doctor. It might mean you’re experiencing a miscarriage. The doctor can diagnose it or rule it out by ordering an ultrasound or hCG blood test. If you’re concerned about cramps during pregnancy, contact WFMC Health to schedule an in-office or telehealth appointment.
Sometimes, severe cramping can signify an ectopic pregnancy, which occurs when the fertilized egg implants in one of the fallopian tubes instead of the uterus. Ectopic pregnancy is a very serious, dangerous condition that requires immediate surgery as the pregnancy cannot be sustained. It can also threaten the mom’s health if the fallopian tube ruptures. Cramping on one side should also be reported to your doctor as it might mean an ectopic pregnancy. Cramping accompanied by vaginal bleeding should also be immediately reported to the doctor. It might mean you’re experiencing a miscarriage. The doctor can diagnose it or rule it out by ordering an ultrasound or hCG blood test. If you’re concerned about cramps during pregnancy, contact WFMC Health to schedule an in-office or telehealth appointment.
Do you have more questions about pregnancy cramps in Salem Oregon? Talk to our staff at WFMC Health or become a new patient today!
Filed Under: Maternity Health Care
WFMC
Pregnancy Cramps: What They Mean and When to Worry
When you’re pregnant, your body undergoes many changes as it makes room for your little one (or two or more!).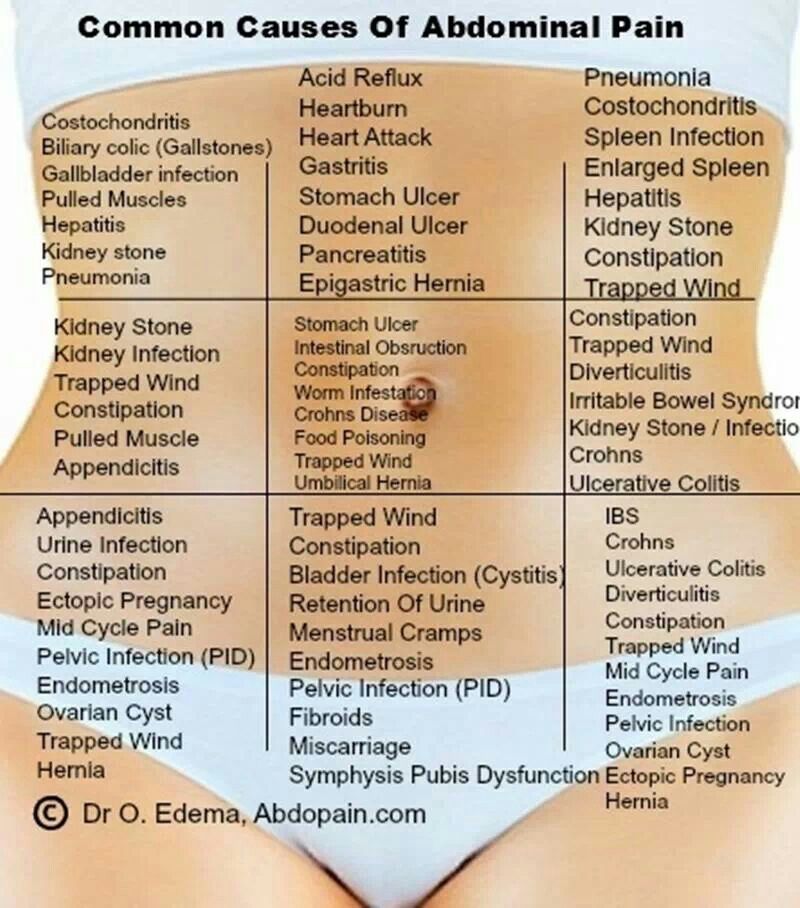 While some of these changes may be no big whoop, others, particularly things like cramping, can have you quickly searching Google for their causes.
While some of these changes may be no big whoop, others, particularly things like cramping, can have you quickly searching Google for their causes.
While some mild pregnancy cramps are a normal symptom of your ever-expanding body, other cramps could indicate a serious problem. Pregnancy cramps can give many women anxiety, so it’s important to know the common reasons for their occurrence and what you should do about them.
We asked Srijaya Soujanya Nalla, MD, an OBGYN at Banner Health Clinic in Loveland, CO, to help explain the normal causes for cramping, abnormal causes and treatment recommendations for both.
[However, if you’re experiencing severe cramping with or without bleeding, stop reading this article and call your doctor immediately.]
What’s considered normal cramping during pregnancy?
“Early on in your pregnancy, it’s natural to feel some mild cramping in your lower abdomen at infrequent times as your body prepares for your growing baby,” Dr. Nalla said.
Nalla said.
As your belly grows, so does your uterus. This may cause you to feel some slight pulling, tugging or stretching similar to menstrual cramps.
“Later in your pregnancy, you may experience some mild lower abdominal discomfort due to the tightening of your uterus. These are normal as long as they occur in irregular intervals and subside on their own,” Dr. Nalla said. “A common cause later in pregnancy is due to round ligament pain, a muscle that supports the uterus. As it stretches, it can cause some mild aches and pains.”
Other causes for mild cramping include:
- Implantation bleeding
- Gas, bloating and constipation
- Sex
- Exercise
- Braxton Hicks contractions
What should I do for mild cramping while pregnant?
Time your cramps to see how regular they are and how often you feel them. “As long as they don’t fall into the abnormal category, there are some things that you can do to make them better,” Dr. Nalla said. Some of these activities include:
Nalla said. Some of these activities include:
- Rest: Try to sit, lie down or change positions.
- Soak in the tub: Take a warm soak in the tub or a warm shower.
- Take some acetaminophen: Products like Tylenol are commonly used by pregnant women for pain and fever but talk to your health care provider first.
- Practice deep breathing: Use relaxation techniques such as meditation, yoga or controlled breathing.
- Stay hydrated: Pregnant women need 50 percent more water. Keep a bottle of water on hand wherever you go.
When should I be concerned about cramping during pregnancy?
While cramping can be common, there are some serious causes of abdominal pain you shouldn’t ignore.
“Any cramping that is severe in intensity, occurs at regular intervals and progressively gets worse with time is abnormal,” Dr. Nalla said. “In addition, any amount of cramping associated with vaginal bleeding, increased/watery vaginal discharge, or pelvic pressure is not normal either. ”
”
Some causes for abnormal cramping may be due to:
- Ectopic pregnancy
- Miscarriage
- Preeclampsia
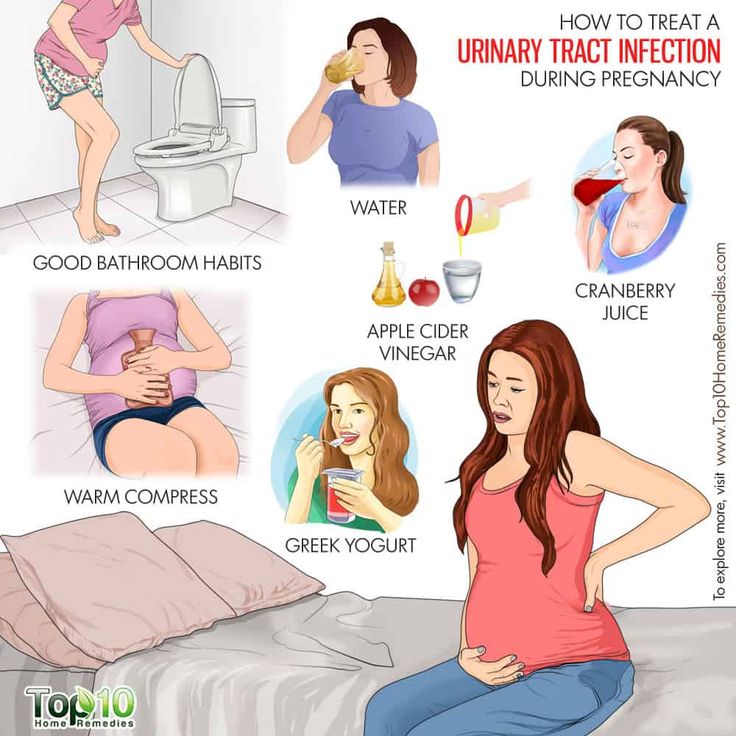
- Bladder infection or urinary tract infection
What should I do if I’m concerned about the cramping?
It’s normal to experience some mild cramping during pregnancy, but always speak with your health care provider if you are ever concerned or are experiencing the above warning symptoms.
“In some cases, an ultrasound can be done to help determine the cause for severe cramping,” Dr. Nalla said. “Sometimes severe cramping can be the first sign of an ectopic pregnancy or a miscarriage. Other times, it could be non-pregnancy related issues like a bladder infection or constipation which are quite common in pregnancy.”
When it comes to your health and the health of your baby, it’s better to err on the side of caution and talk to your health care provider.
You can find a Banner Health specialist near you by visiting bannerhealth. com or for general pregnancy-related questions, you can call the Banner Health Nurse Now at 844-259-9494 for free, 24/7 medical advice.
com or for general pregnancy-related questions, you can call the Banner Health Nurse Now at 844-259-9494 for free, 24/7 medical advice.
Related pregnancy articles:
- Is a Headache During Pregnancy Something to Worry About?
- If You’re Expecting and Your Hands and Feet Itch, It Could Be Cholestasis
- Expect the Unexpected: How Your Body Changes During Pregnancy
- Prenatal Screenings and Tests: What to Expect Every Trimester
- Driving While Pregnant: Common Questions Answered
Women's Health Pregnancy
Join the Conversation
Anticonvulsants in pregnancy: new encouraging evidence
PUBLICATIONS
Materials and methods
The current study included 289 women with epilepsy and 89 women without epilepsy; all women participated in the study during pregnancy.
74% of women with epilepsy received monotherapy: 43% - lamotrigine and 37% - levetiracetam.
4% were not taking any medication and 22% were taking more than one medication. nine0009 Of those taking more than one drug, nearly half were taking a combination of lamotrigine and levetiracetam.
Drug levels in the blood of women with epilepsy were measured in the third trimester.
For the current analysis, children born to mothers with epilepsy were screened at age 3 with a series of cognitive and developmental tests that measured vocabulary, listening comprehension, number recall, and pattern recognition; results were adjusted for the mother's IQ, educational level, age, postpartum period, Beck Anxiety Inventory (Beck Anxiety Inventory) scores, and the child's ethnicity, gender, and breastfeeding status. nine0003
Results
-
Neither monotherapy nor polytherapy has been evaluated separately.
-
When the verbal index scores for major antiepileptic drug groups were analyzed separately, the level of exposure to levetiracetam was the only significant P 0.
 028.
028. -
The primary outcome showed that verbal index scores at age 3 did not differ between children from women with epilepsy and children from women without epilepsy (LS mean 102.7 vs 102.1). nine0003
-
Exposure to anticonvulsants, as evidenced by peak blood levels in the third trimester, was not associated with verbal index scores (n = 265; adjusted parameter estimate, -1.9; 95% CI, -6.8 to 3.1 ).
-
Scores for general conceptual ability also did not differ between the two groups: 105.1 for children of women with epilepsy and 103.5 for children of healthy women. nine0003
-
The maximum observed ratio of blood levels of anticonvulsants in the third trimester was not significantly associated with adjusted measures of general conceptual ability for children from women with epilepsy.
Conclusion
Currently, lamotrigine and levetiracetam are the two safest drugs to use during pregnancy. nine0009 The Maternal Outcomes and Effects of Antiepileptic Drugs on Neurodevelopment Study (MONEAD) found no difference in neurobehavioral development in children at 3 years of age born to women with epilepsy compared with children of healthy women without epilepsy.
nine0009 The Maternal Outcomes and Effects of Antiepileptic Drugs on Neurodevelopment Study (MONEAD) found no difference in neurobehavioral development in children at 3 years of age born to women with epilepsy compared with children of healthy women without epilepsy.
This is the first study to evaluate drug exposure and blood levels, which is important because drug clearance increases during pregnancy but varies from drug to drug and from person to person using the same drug. nine0009 The risk of side effects of anticonvulsants must always be balanced against the risk of seizures.
The researchers plan to screen children at an older age, when the estimates will be more sensitive to the final results.
More research is needed on the underlying pathogenic mechanisms, including genetic predisposition, as teratogens act on susceptible genotypes.
The advice regarding regular folic acid supplementation by pregnant women remains relevant, as it has been shown to be associated with improved cognitive and behavioral outcomes in children. nine0003
nine0003
Source:
medscape.com/viewarticle/947241#vp_1
Pregnancy with epilepsy - GBUZ MO MONIIAG
Having healthy children is a natural desire of every woman. Many myths and prejudices prevent women with epilepsy from deciding to have a child, while many misconceptions have no basis. With the right approach to pregnancy planning and drug therapy, it is likely that a woman suffering from epilepsy will be able to give birth to a healthy child. nine0003
Epilepsy complicates approximately 0.3-0.5% of pregnancies. From 14 to 32% of these patients report an increase in the frequency of seizures during pregnancy. Pregnant women with ongoing or newly diagnosed seizures are at high risk and require close monitoring by a neurologist and an obstetrician-gynecologist.
There is also a risk of having a child with malformations due to the fact that most antiepileptic drugs (AEDs) have a negative effect on the fetus. This exposure is called a "teratogenic effect" and can cause birth defects in a child or developmental and learning disabilities as the child grows. nine0003
nine0003
If a woman is not planning a pregnancy while being treated for epilepsy, it is recommended to use reliable contraception to avoid an unplanned pregnancy.
What are the actions of a woman with epilepsy who is planning a pregnancy?
IT IS NECESSARY TO OBTAIN A CONSULTATION WITH AN EPILEPTOLOGIST BEFORE CONCEPTION
TO DECIDE THE FOLLOWING ISSUES
1. The need for anticonvulsant therapy.
2. Determination of the minimum amount (ideally monotherapy) and the minimum effective dose of AEDs that do not cause seizures. nine0003
3. Taking slow-release AEDs or dividing the daily dose to lower peak blood levels, which may reduce the risk of malformations in the child.
4. Start taking folic acid at a dosage of at least 1 mg per day.
TERATOGENIC EFFECT OF ANTIEPILEPTIC DRUGS
1. All AEDs are teratogenic, there is no consensus on which AED is the safest.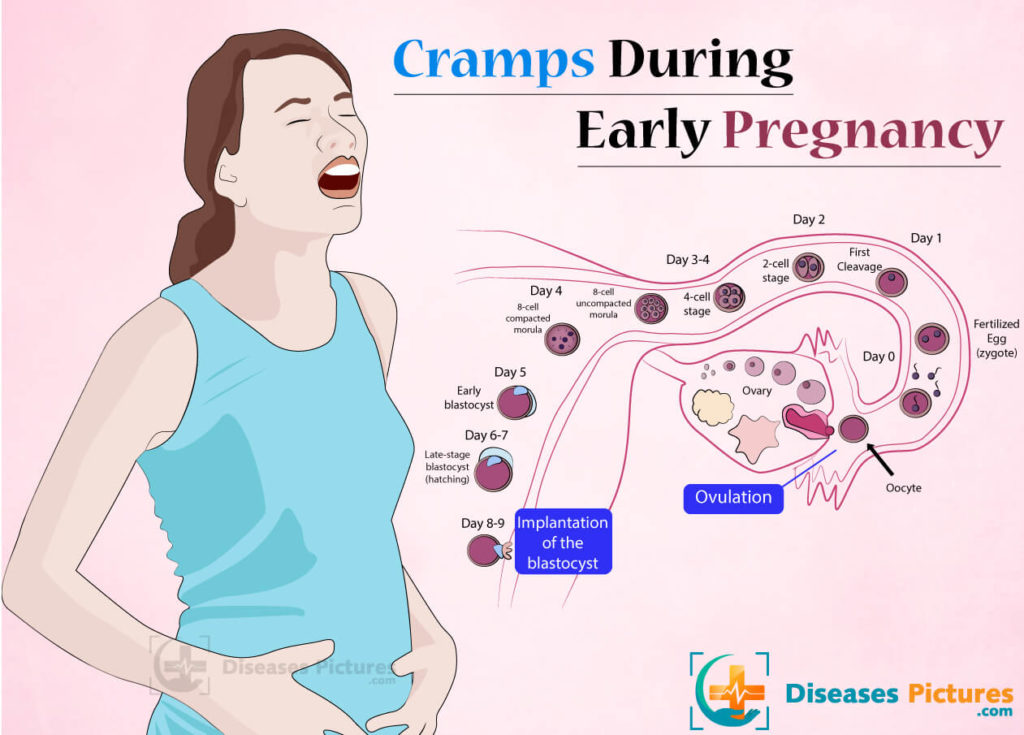
2. The risk of fetal abnormalities increases with the number and dosage of AEDs taken.
3. Anomalies in the development of the fetus, due to the use of AEDs, can occur only in the first weeks of pregnancy, when all systems and organs of the fetus are formed.
4. Changing AED therapy after the first trimester does not affect the risk of congenital malformations.
5. 95% of children born to mothers receiving AED treatment have no abnormalities!
I HAVE BEEN PREGNANT, WHAT'S NEXT?
1. Epilepsy is not a contraindication for pregnancy.
2. Do not cancel PEP! Do not change the dosage of PEP yourself! Do not replace AEDs that have resulted in remission of epilepsy - taking AEDs during pregnancy is vital, as many factors increase the risk of recurrence of even well-controlled seizures before pregnancy. The most common provocateurs of seizures during pregnancy are skipping AEDs, emotional stress and sleep disturbances!!! nine0003
3. It is necessary to register for pregnancy for timely prenatal screening, get advice from an epileptologist.
4. Treatment of obstetric complications is carried out according to clinical guidelines.
5. Epilepsy is not a contraindication for natural childbirth, and labor management and pain management are up to standard. In most cases, prolonged epidural analgesia can be used.
6. Epilepsy is not an indication for caesarean section, even if there are several seizures during pregnancy!!! Indications for cesarean section are an increase in epileptic seizures, convulsive seizures more than once a week in the 3rd trimester of pregnancy, serial or status epilepsy, and a seizure during childbirth. nine0003
POSTPARTUM AND BREASTFEEDING
1. Continue taking AED!!! There is a risk of epilepsy decompensation in the postpartum period!!!
2. In case of drowsiness, double vision and involuntary movement in the eyes, ataxia, an urgent study of the concentration of AED in the blood is necessary.