Asthma symptoms pregnancy
Symptoms, Diagnosis, Risks, and More
According to March of Dimes, asthma affects 4 percent to 8 percent of pregnancies. When unmanaged, this inflammatory disease of the airways makes breathing difficult and can reduce the amount of oxygen in the blood for the birthing parent and their developing baby.
If you’re pregnant and impacted by asthma (or just care about someone who is), you may have a lot of questions. While it’s important to talk with your healthcare professional about your specific concerns, we’ve gathered some basic information to help you feel prepared for those conversations.
Having an asthma attack reduces the amount of oxygen in your blood, which can mean that your growing baby won’t get the oxygen they need.
The most common pregnancy complications from asthma are:
- a slightly increased chance of preterm labor and delivery
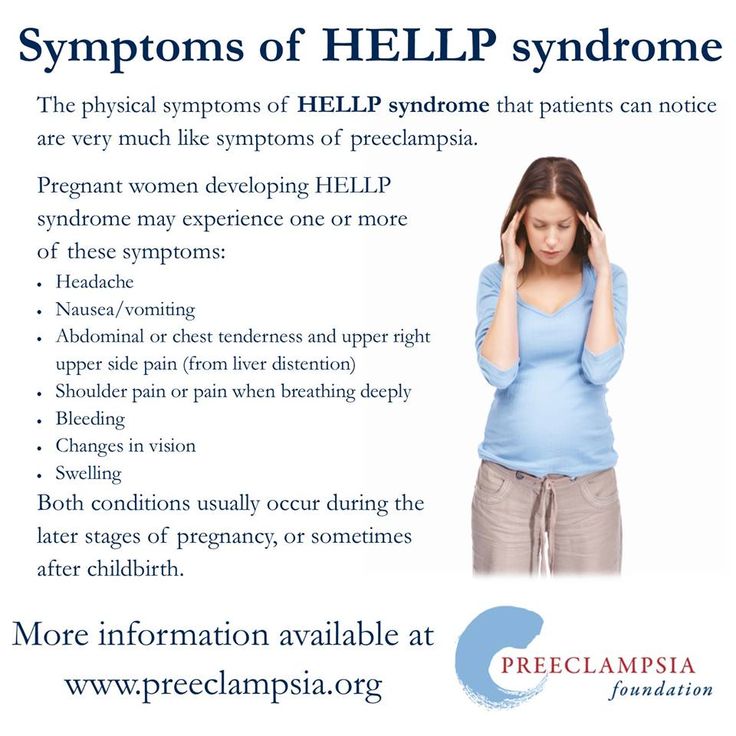
- high blood pressure and the related condition preeclampsia
- low birth weight
Managing asthma can ensure that your baby always has sufficient oxygen, decreasing the chance of complications, especially severe ones like stillbirth.
Being pregnant can make your asthma better or worse. The American College of Allergy, Asthma & Immunology says that in about one-third of pregnancies affected by asthma, the asthma improves. In another third, asthma worsens, and in the final third, there is no noticeable change in their asthma during pregnancy.
While it’s difficult to predict how your asthma will change during pregnancy, you may experience the same type of changes in future pregnancies.
If your asthma does get worse, don’t fear. The majority of people with changes during pregnancy see their asthma return to prepregnancy levels by about 3 months postpartum.
Your healthcare professional will check in about your asthma during prenatal visits and monitor your lungs.
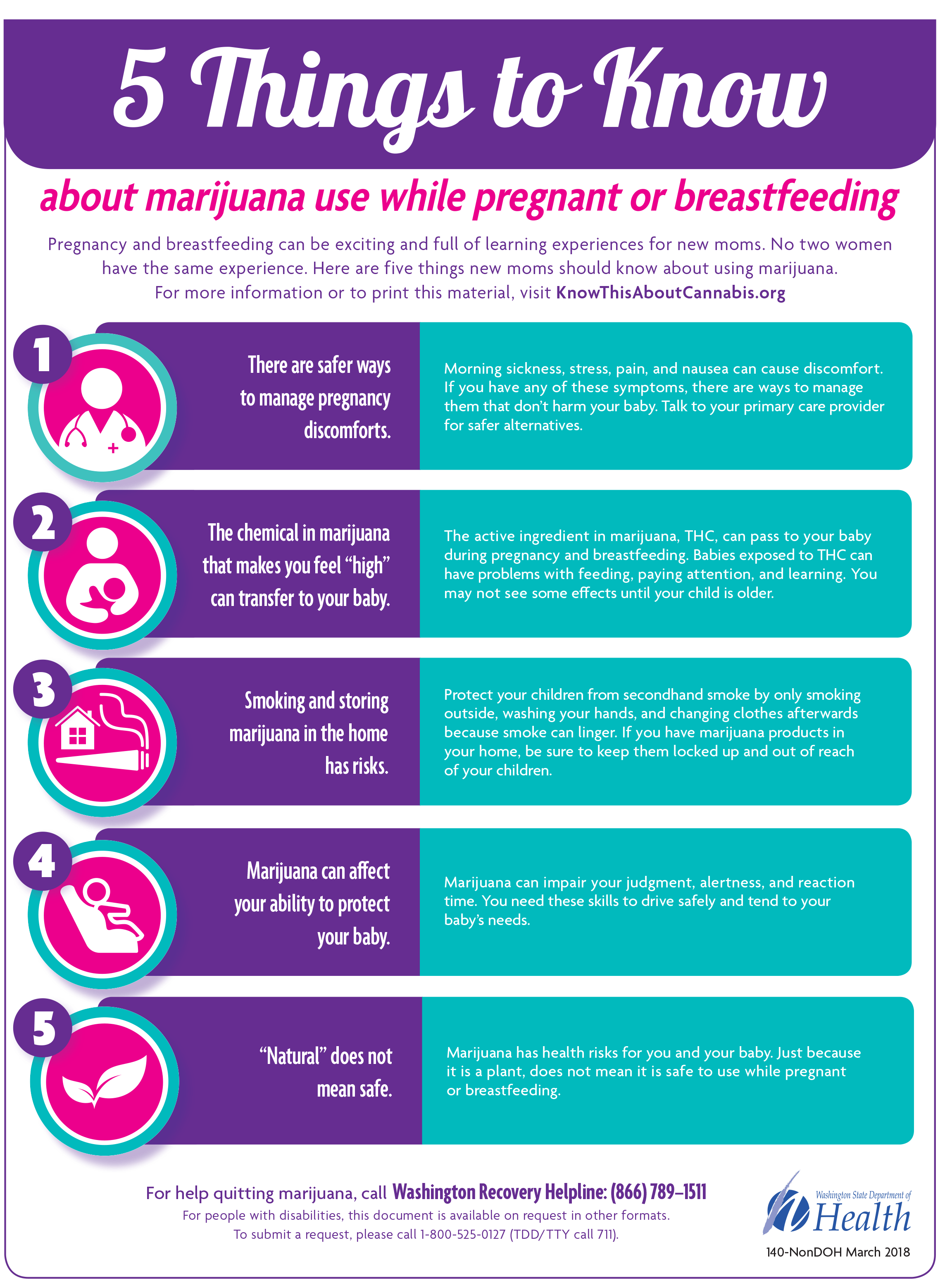
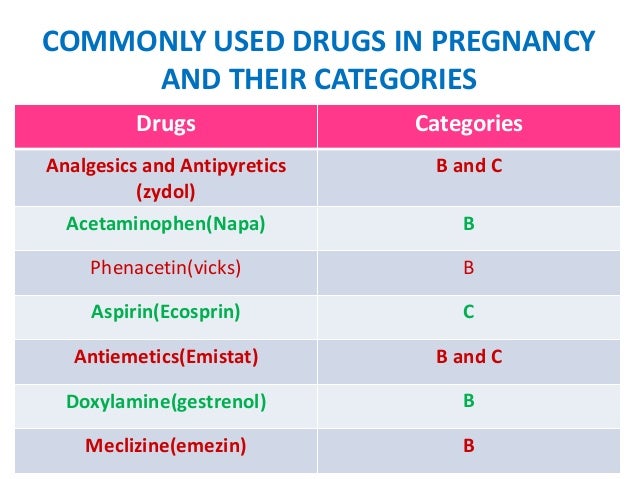
If you’ve been taking medications before pregnancy to help manage your asthma, talk with your doctor about them. They may need to adjust your asthma medications and dosage levels.
Getting the flu can increase the chance of asthma problems during pregnancy. Since flu shots are recommended during pregnancy, you may not experience this. Check with your healthcare professional. Also, talk with your doctor if you take allergy shots to help manage your asthma.
Since flu shots are recommended during pregnancy, you may not experience this. Check with your healthcare professional. Also, talk with your doctor if you take allergy shots to help manage your asthma.
Heartburn, or acid reflux, can make asthma symptoms worse, so you may wish to take steps to minimize the chances of it. Some things you can do include:
- sleeping in a more elevated position
- eating smaller meals
- not lying down immediately after eating
You can also speak with your doctor about various medications that can help with heartburn if it is a frequent problem.
If you have a difficult time managing your asthma or experience an asthma attack during pregnancy, your healthcare professional will probably want to do additional ultrasounds to check the baby’s growth. They may also ask you to track how much fetal movement you feel.
March of Dimes says that only about 10 percent of pregnancies affected by asthma involve asthma symptoms during labor and delivery.
If you take asthma medication during pregnancy, continue to take it during labor and delivery unless otherwise instructed.
Earlier in your pregnancy, you may want to discuss a care plan for any asthma symptoms you may have during labor and delivery.
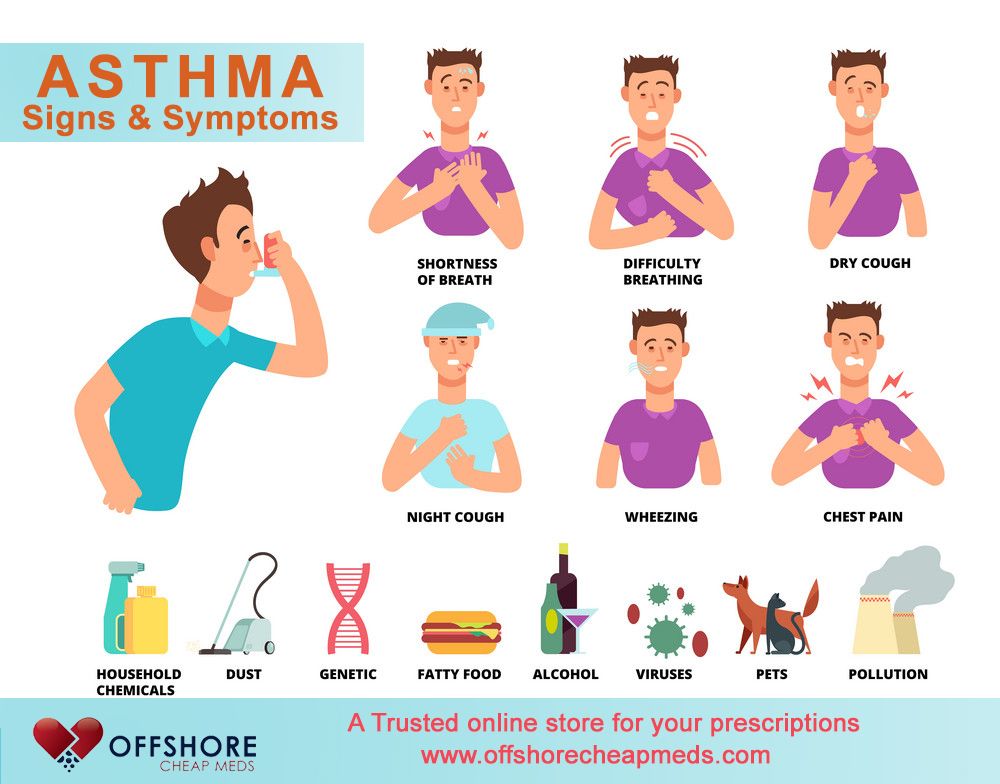
Symptoms of asthma may include:
- tightness in the chest
- constant coughing
- shortness of breath
- wheezing
Restricted airways mean that you’ll have trouble getting deep breaths when asthma hits. You may feel tired and faint as less oxygen circulates through your body. You may also feel your anxiety levels rising.
Questions for your doctor or healthcare professional
- Are there any additional tests/procedures you would recommend based on my asthma?
- Are the medications I’m currently taking safe? Would you recommend different medications or dosages?
- Are there things you would suggest doing to reduce the chance of my asthma during pregnancy?
- What will happen if I have an asthma attack during labor and delivery?
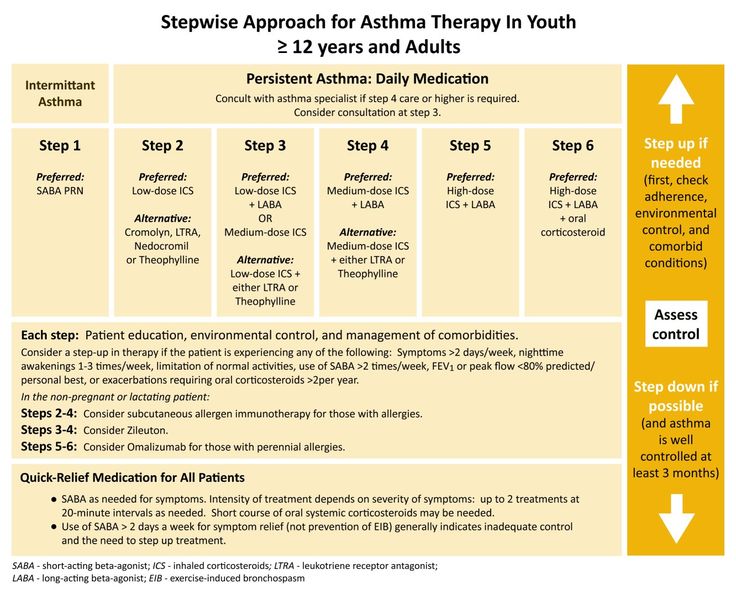
If your asthma is already managed with medications, chances are, treatment for it will continue to look similar during pregnancy.
Your doctor may advise an inhaled medication where smaller amounts enter the bloodstream. They might also try to minimize the amount of medication you’re taking — especially during the first trimester when many of the baby’s organs are developing.
Asthma can be triggered by many things including:
- allergens (pollen, nuts, etc.)
- irritants (dust, mold, etc.)
- infections
- exercise
- strong emotions
If you smoke, it’s recommended that you quit, especially while pregnant.
Even if you’re taking medication to manage asthma, it’s a good idea to avoid any of your asthma triggers.
If you manage your asthma during your pregnancy, chances are good that you’ll experience a fairly healthy pregnancy and delivery.
The risks are higher if your asthma is unmanaged. If this is the case, you can expect more monitoring from your doctor during your pregnancy, labor, and delivery.
If you have asthma, it’s important to make sure that you manage the condition as best you can.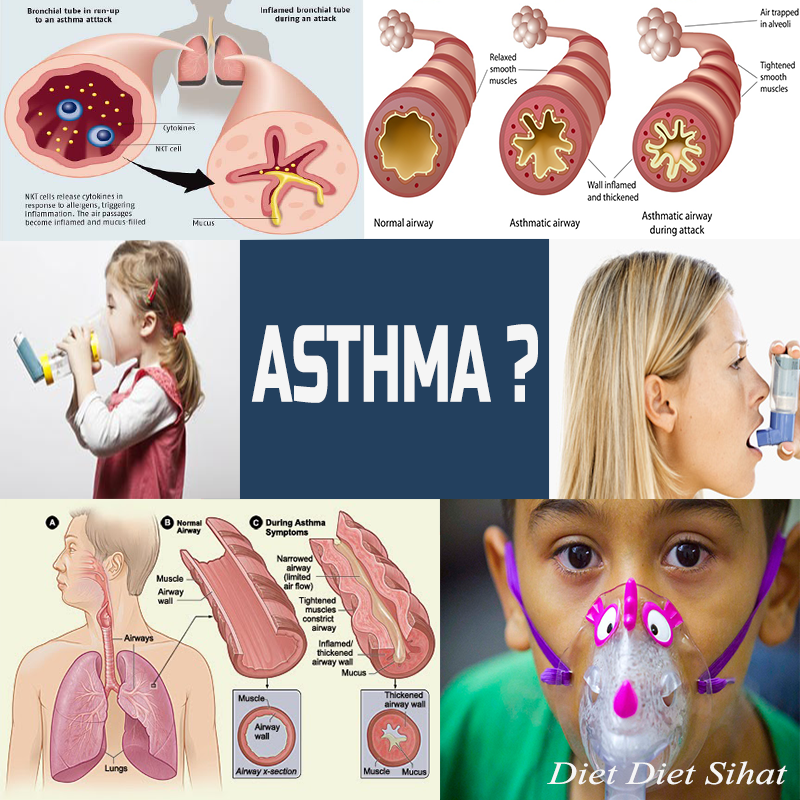 Because asthma can get better, worse, or stay the same during pregnancy, your healthcare professional will monitor your asthma during your prenatal appointments.
Because asthma can get better, worse, or stay the same during pregnancy, your healthcare professional will monitor your asthma during your prenatal appointments.
It’s important that your blood has sufficient oxygen for you and your growing baby, so if you take medications to manage your asthma, continue taking them as your doctor prescribes.
Pregnancy and Asthma | ACAAI Public Website
Overview
When you’re pregnant, it is particularly important to manage your asthma properly.
According to the Centers for Disease Control and Prevention, asthma affects 4–12 percent of women in their childbearing years. Most methods for controlling asthma are not harmful to your developing baby, and your baby will develop better if you are breathing easily.
Tell all your doctors that you have asthma. And if you’re pregnant or planning a pregnancy, talk with your allergist. Allergists are specially trained to help you take control of your asthma, so you can live the life you want – including becoming pregnant. A close partnership with your allergist is the secret to well-managed asthma.
Find expert care.
Don’t let allergies or asthma hold you back from the things you love.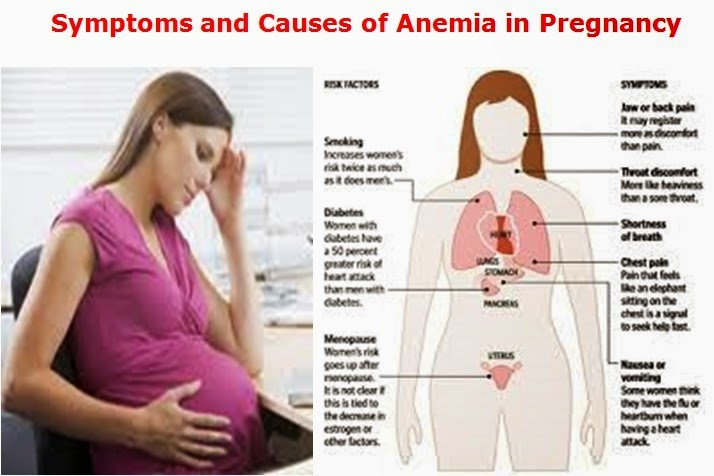
Effects of Pregnancy on Asthma
There is no significant risk to you or your unborn child if your asthma is well controlled, but uncontrolled asthma can cause serious complications. For you, the mother, these complications include high blood pressure, toxemia, premature delivery and, rarely, death. For your baby, complications include increased risk of stillbirth.
While pregnant, about a third of women with asthma experience improved symptoms, about a third have worse symptoms and about a third experience no change.
Studies on the overall effect of pregnancy on asthma have found the following:
- While pregnant, women with severe asthma are more likely to see their asthma worsen, whereas women with mild asthma are more likely to see improvement or no change.
- The change a woman experiences during her first pregnancy is usually similar in future pregnancies.
- Asthma is most likely to worsen during weeks 24 to 36. About 10 percent of women with asthma have symptoms during labor and delivery.
- If asthma symptoms change during pregnancy, they usually return to pre-pregnancy status within three months of delivery.
Pregnancy may affect women with asthma in several ways. Hormonal changes that occur during pregnancy can affect both your nose and sinuses, as well as your lungs. The increase in estrogen contributes to congestion, which causes a stuffy nose, especially during the third trimester. A rise in progesterone may cause a feeling of shortness of breath. Your allergist can help determine if asthma is the cause of your shortness of breath during pregnancy.
Treatment and Management
Don’t be afraid to take your asthma medication during pregnancy. Your allergist will help you choose medications that can be taken safely while pregnant.
Asthma symptoms can vary in intensity from day to day, month to month or season to season, regardless of pregnancy. You and your allergist should create a treatment plan based on the severity of your asthma and your experience with asthma medicines while pregnant.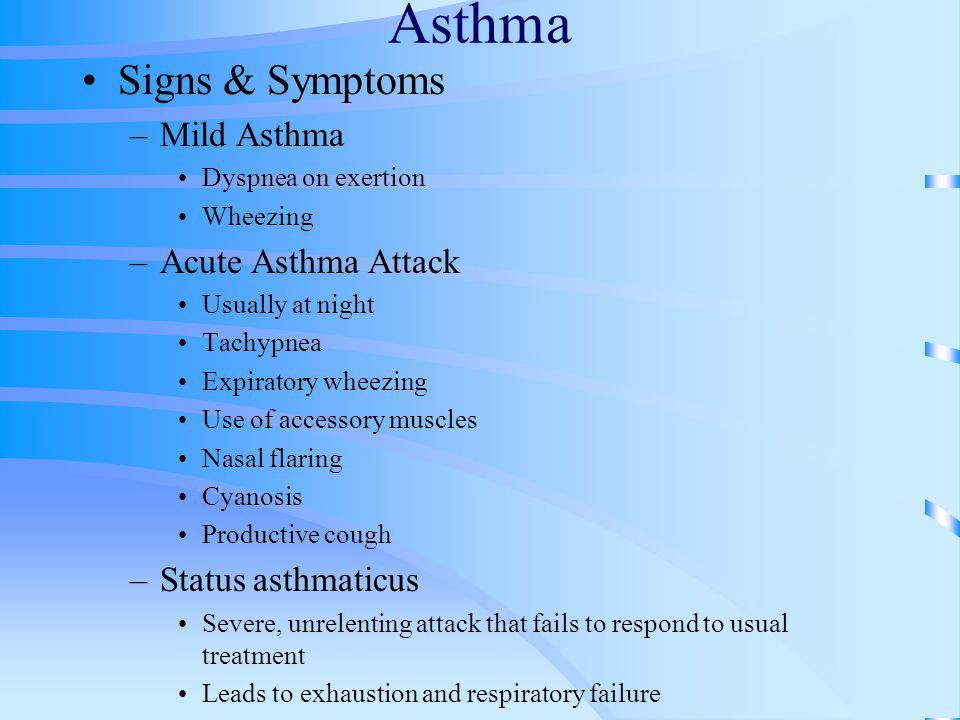 Remember that medicines should not replace avoidance of your triggers. Avoiding irritants and triggers may reduce the amount of medicine you need.
Remember that medicines should not replace avoidance of your triggers. Avoiding irritants and triggers may reduce the amount of medicine you need.
Your allergist will take the following into consideration when discussing the use of asthma medicines during pregnancy:
- Inhaled medicines are generally preferred because they have a more targeted effect, with only small amounts entering the bloodstream.
- When appropriate, time-tested medicines are preferred, because there is more experience with their use during pregnancy.
- It is best to limit medicines as much as possible in the first trimester, when the baby is first developing. But birth defects from medications are rare; no more than one percent of all birth defects are caused by medicines.
- In general, the same medicines used during pregnancy are appropriate during labor and delivery and when nursing.
Fortunately, most asthma patients do well during labor and delivery, although the baby should be monitored closely.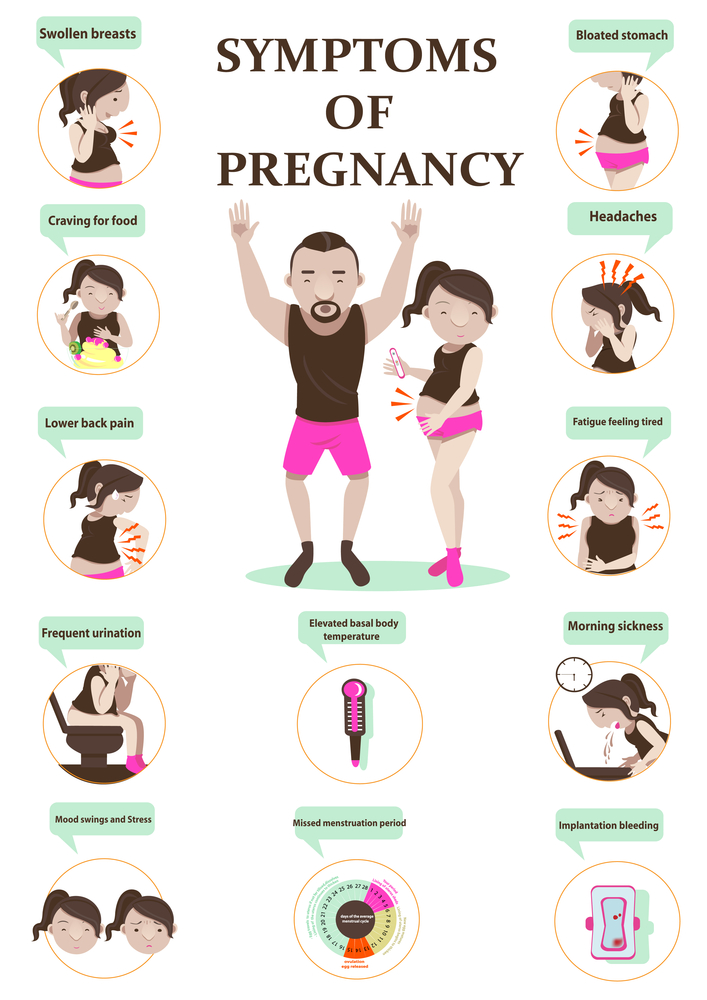 In low-risk women whose asthma is well controlled, the routine monitoring that is conducted with all babies should be sufficient. More intensive monitoring with careful observation is recommended for women who enter labor and delivery with severe asthma or other risk factors.
In low-risk women whose asthma is well controlled, the routine monitoring that is conducted with all babies should be sufficient. More intensive monitoring with careful observation is recommended for women who enter labor and delivery with severe asthma or other risk factors.
The most important goal is to maintain control of your asthma throughout your pregnancy. The best way to meet this goal is to follow your treatment plan and to take your medications as directed.
Can you develop asthma during pregnancy?
There is no research that indicates you can develop asthma from being pregnant. However, pregnancy can cause asthma symptoms to worsen. It’s possible that a woman who does not realize she has mild asthma will recognize asthma symptoms for the first time while pregnant. However, most women with asthma are aware of their asthma prior to becoming pregnant.
Will asthma have any effect on my pregnancy and my baby?
If uncontrolled, severe asthma may be harmful to your developing baby.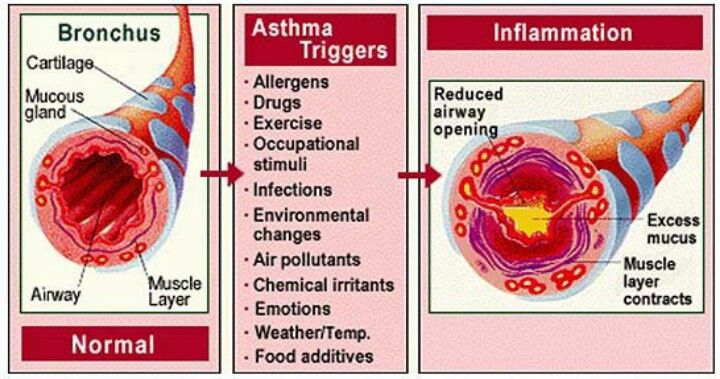 However, if well controlled, it should not have any effect on you or your baby.
However, if well controlled, it should not have any effect on you or your baby.
Will my asthma worsen during pregnancy? Is there any greater risk during labor and delivery?
Your asthma may worsen, stay unchanged or possibly improve during pregnancy. Although it cannot be accurately predicted in a first pregnancy, asthma usually follows a similar pattern in the pregnancies that come after. For reasons not totally understood, asthma usually improves during labor and delivery, but even if a severe attack occurs, appropriate treatment can be given, and complications are rare.
Can I use asthma medicines safely while pregnant?
Most medicines used to treat asthma appear to be safe during pregnancy, especially those that have been around for many years and have been studied. Though no medicine has been proven entirely safe for use during pregnancy, your allergist will carefully balance medication risks and the need for symptom control.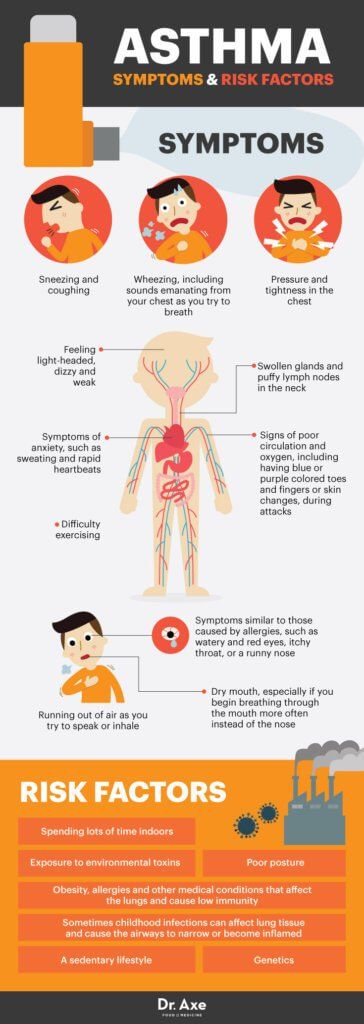 Your treatment plan will be individualized, so that potential benefits outweigh the potential risks of your medications or of uncontrolled asthma.
Your treatment plan will be individualized, so that potential benefits outweigh the potential risks of your medications or of uncontrolled asthma.
Since we cannot prove the safety of drugs taken while pregnant, should I stop taking my asthma medication as soon as I discover that I have become pregnant?
No. A moderate to severe asthma attack could be a risk to both you and the baby. The risks of stopping your medication are far greater than any potential risk to your baby from medication. Therefore, do not stop your regular asthma medication without first discussing it with your primary care physician or your allergist.
Are there any medications that should be avoided while pregnant?
Unless a life-threatening illness requires their use, the following medications should be avoided during pregnancy, either entirely or during certain stages:
- Sulfonamides (the sulfa drugs) are safe early in pregnancy, but their use in the last trimester might cause jaundice in your infant.
- Tetracyclines at any stage of pregnancy may cause skeletal and dental deformities.
Are other medications taken for my hay fever or other allergies also safe?
Many of them are safe. Consult your allergist before continuing antihistamines or nasal sprays, even if they are available over the counter.Accordion Content
How does severe, uncontrolled asthma adversely affect my baby?
The developing baby depends on you to supply oxygen for growth and survival. Uncontrolled asthma causes a decrease in your oxygen, which in turn reduces the oxygen flow to your baby. This may result in impaired growth or other complications.
Bronchial asthma during pregnancy. What is bronchial asthma during pregnancy?
IMPORTANT
The information in this section should not be used for self-diagnosis or self-treatment. In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
For diagnosis and proper treatment, you should contact your doctor.
Bronchial asthma during pregnancy is an atopic bronchospastic respiratory disease that occurred during gestation or existed earlier and can affect its course. Manifested by attacks of characteristic suffocation, unproductive cough, shortness of breath, noisy wheezing. It is diagnosed using physical examination methods, laboratory determination of markers of allergic reactions, spirography, peak flowmetry. For basic treatment, combinations of inhaled glucocorticoids, antileukotrienes, beta-agonists are used, and short-acting bronchodilators are used to stop attacks. nine0006
ICD-10
O99.5 J45
- Causes
- Pathogenesis
- Classification
- Asthma symptoms in pregnancy
- Complications
- Diagnostics
- Treatment of asthma in pregnancy
- Prognosis and prevention
- Prices for treatment
General
Bronchial asthma (BA) is the most common pathology of the respiratory system during pregnancy, occurs in 2-9% of patients.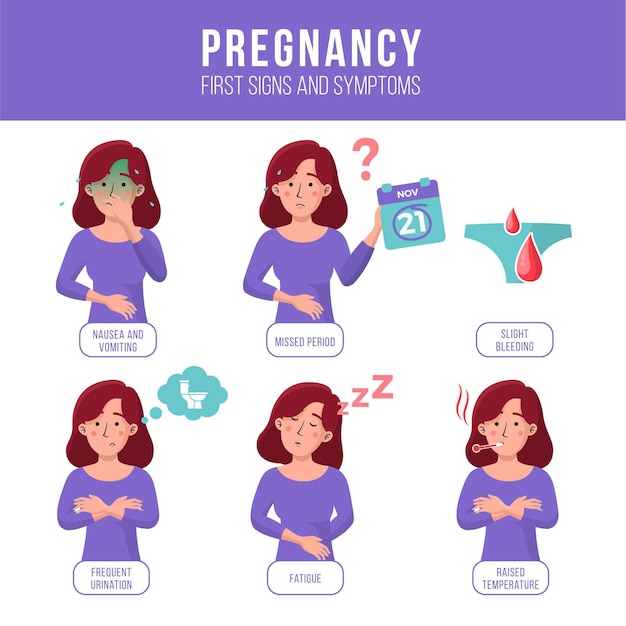 According to observations of obstetricians-gynecologists and pulmonologists, the progression of the disease is observed in 33-69% of pregnant women. At the same time, in some women, the condition remains stable and even improves. Mild forms of asthma are diagnosed in 62% of women, moderate - in 30%, severe - in 8%. Although an exacerbation of the disease is possible at any stage of pregnancy, it occurs more often in the second trimester, and during the last 4 weeks spontaneous improvement usually occurs due to an increase in free cortisol. The relevance of timely diagnosis of asthma is associated with the almost complete absence of complications with proper medical control. nine0006
According to observations of obstetricians-gynecologists and pulmonologists, the progression of the disease is observed in 33-69% of pregnant women. At the same time, in some women, the condition remains stable and even improves. Mild forms of asthma are diagnosed in 62% of women, moderate - in 30%, severe - in 8%. Although an exacerbation of the disease is possible at any stage of pregnancy, it occurs more often in the second trimester, and during the last 4 weeks spontaneous improvement usually occurs due to an increase in free cortisol. The relevance of timely diagnosis of asthma is associated with the almost complete absence of complications with proper medical control. nine0006
Bronchial asthma during pregnancy
Causes
The occurrence of the disease in a pregnant woman is provoked by the same factors as in non-pregnant patients. Atopy plays a significant role in the development of bronchial asthma - a hereditary predisposition to allergic diseases due to hypersensitization of the body with increased synthesis of immunoglobulin (IgE).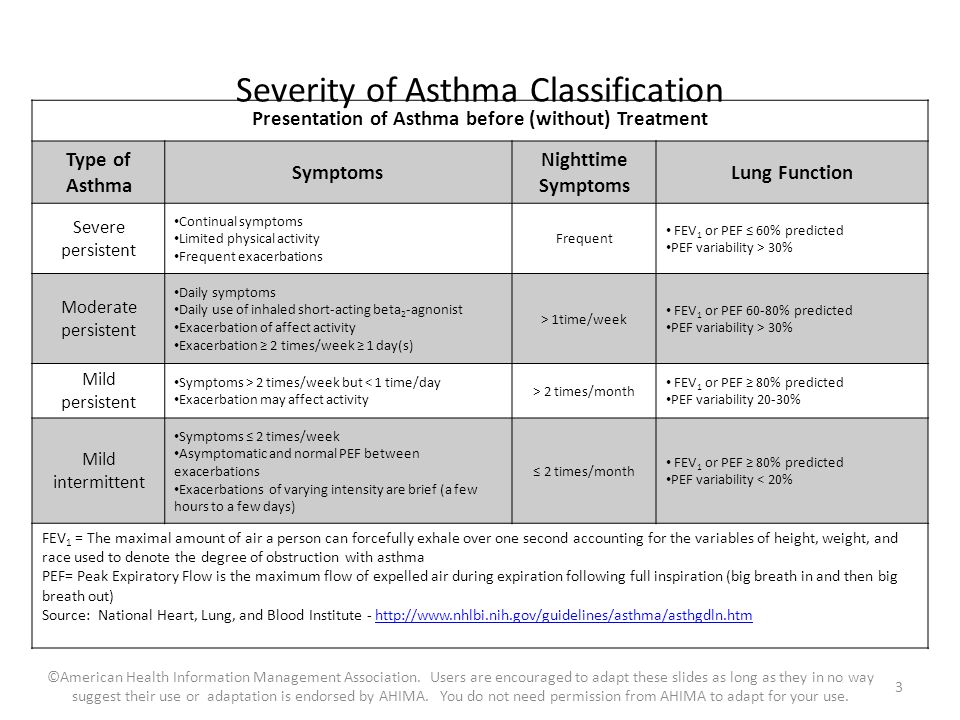 The starting point of bronchospastic conditions in these cases is the action of external triggers - household allergens (dust, paint fumes, building materials), plant pollen, animal hair, food products, pharmaceuticals, tobacco smoke, occupational hazards, etc. The onset of symptoms in predisposed pregnant women may be provoked by respiratory viral infections, chlamydia, mycobacterium tuberculosis, intestinal and other parasites. nine0006
The starting point of bronchospastic conditions in these cases is the action of external triggers - household allergens (dust, paint fumes, building materials), plant pollen, animal hair, food products, pharmaceuticals, tobacco smoke, occupational hazards, etc. The onset of symptoms in predisposed pregnant women may be provoked by respiratory viral infections, chlamydia, mycobacterium tuberculosis, intestinal and other parasites. nine0006
The topic of the influence of changes during gestation on the occurrence and course of AD is still considered insufficiently studied. According to various authors in the field of obstetrics, in some cases the onset of the disease is associated with pregnancy, and its symptoms may persist or completely disappear after childbirth. A number of neuroendocrine, immune and mechanical factors have been identified that contribute to the development of bronchospasm during gestation. They also cause exacerbation of the disease and aggravation of its symptoms in pregnant women with bronchial asthma: nine0006
- Increased secretion of endogenous bronchoconstrictors.
 The maternal part of the placenta and uterine tissues synthesize prostaglandin F2α, which stimulates smooth muscle contraction. Its concentration rises towards the end of gestation, ensuring the timely onset of labor. The substance also provokes respiratory obstruction due to spasm of the smooth muscle fibers of the bronchi.
The maternal part of the placenta and uterine tissues synthesize prostaglandin F2α, which stimulates smooth muscle contraction. Its concentration rises towards the end of gestation, ensuring the timely onset of labor. The substance also provokes respiratory obstruction due to spasm of the smooth muscle fibers of the bronchi. - Increased concentration of immunoglobulin E. A high level of IgE is an important link in the pathogenesis of an atopic reaction to the action of sensitizing factors. Immune restructuring in response to constant exposure to fetal antigens leads to an increase in the content of this immunoglobulin in the blood of a pregnant woman and increases the likelihood of developing bronchospasm and asthma. nine0015
- Increase in the number of α-adrenergic receptors. Hormonal shifts that occur towards the end of pregnancy are aimed at ensuring adequate labor activity. Stimulation of α-adrenergic receptors is accompanied by an increase in the contractile activity of the myometrium.
 The number of such receptors also increases in the bronchi, which facilitates and accelerates the onset of bronchospasm.
The number of such receptors also increases in the bronchi, which facilitates and accelerates the onset of bronchospasm. - Decreased sensitivity to cortisol. Glucocorticoids have a complex anti-asthmatic effect that affects different parts of the pathogenesis of the disease. During pregnancy, due to competition with other hormones, pulmonary receptors become less sensitive to cortisol. As a result, the likelihood of bronchospasm increases. nine0015
- Changes in breathing mechanics. The stimulating effect of progesterone contributes to the occurrence of hyperventilation and an increase in the partial pressure of carbon dioxide in the first trimester. The pressure of the growing uterus in the II-III trimesters and increased resistance of the vessels of the pulmonary circulation potentiate the appearance of shortness of breath. In such conditions, bronchospasm develops more easily.
An additional factor that increases the likelihood of developing asthma during gestation is progesterone-induced swelling of the mucous membranes, including those lining the airways.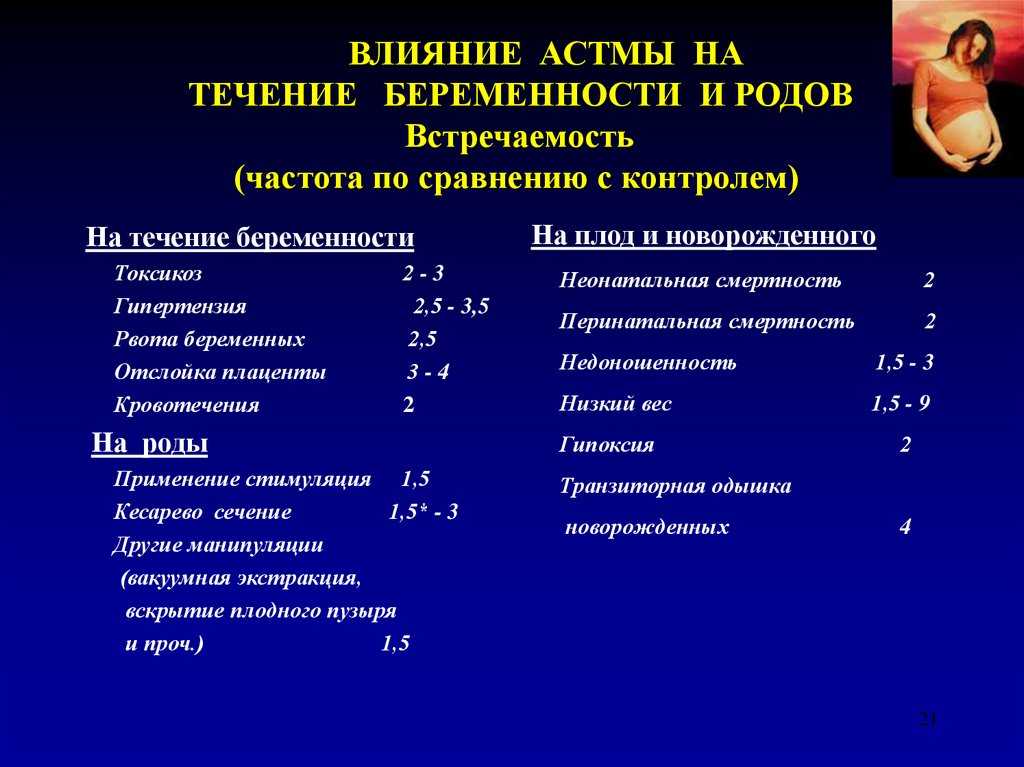 In addition, due to the relaxation of the smooth muscles of the esophageal-gastric sphincter in pregnant women, gastroesophageal reflux is more often formed, which serves as a trigger for the development of bronchospasm. An exacerbation of the disease in a patient with manifestations of bronchial asthma can also occur if maintenance treatment with glucocorticoid drugs is refused due to fear of harming the child. nine0006
In addition, due to the relaxation of the smooth muscles of the esophageal-gastric sphincter in pregnant women, gastroesophageal reflux is more often formed, which serves as a trigger for the development of bronchospasm. An exacerbation of the disease in a patient with manifestations of bronchial asthma can also occur if maintenance treatment with glucocorticoid drugs is refused due to fear of harming the child. nine0006
Pathogenesis
A key link in the development of asthma during pregnancy is an increase in the reactivity of the bronchial tree caused by specific changes in the autonomic nervous system, inhibition of cyclic nucleotides (cAMP), degranulation of mast cells, the influence of histamine, leukotrienes, cytokines, chemokines, and other inflammatory mediators. The action of trigger allergens triggers reversible bronchial obstruction with an increase in airway resistance, overstretching of the alveolar tissue, and a mismatch between lung ventilation and perfusion.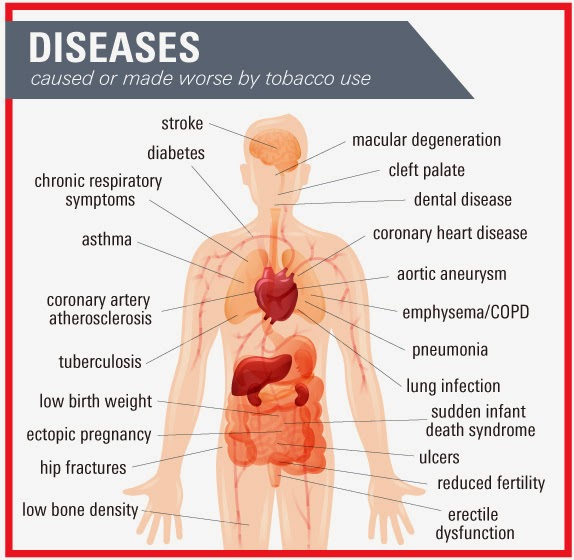 The final stage of respiratory failure is hypoxemia, hypoxia, metabolic disorders. nine0006
The final stage of respiratory failure is hypoxemia, hypoxia, metabolic disorders. nine0006
Classification
In the management of pregnant women suffering from bronchial asthma, clinical systematization of the forms of the disease is used, taking into account the severity. The classification criteria for this approach are the frequency of asthma attacks, their duration, changes in external respiration. There are the following options for bronchial asthma during pregnancy:
- Episodic (intermittent). Attacks of suffocation are observed no more than once a week, at night they disturb the patient no more than 2 times a month. The periods of exacerbations last from several hours to several days. Outside of exacerbations, the functions of external respiration are not impaired. nine0015
- Light persistent. Characteristic symptoms occur during the week several times, but not more than once a day. With exacerbations, sleep and habitual activity may be disturbed.
 Peak expiratory velocity and its second volume during forced breathing during the day change by 20-30%.
Peak expiratory velocity and its second volume during forced breathing during the day change by 20-30%. - Persistent moderate. There are daily episodes. Choking at night develops more than once a week. Changed physical activity and sleep. A 20-40% decrease in the peak expiratory flow rate and its second volume is characteristic when forcing with a daily variability of indicators of more than 30%. nine0015
- Severe persistent. The pregnant woman is disturbed by daily attacks with frequent exacerbations and the appearance at night. There are restrictions on physical activity. The basic indicators of the assessment of the functions of external respiration are reduced by more than 40%, and their daily fluctuations exceed 30%.
Asthma symptoms during pregnancy
The clinical picture of the disease is represented by attacks of suffocation with a short breath and a long labored exhalation. In some pregnant women, classic symptoms are preceded by an aura - nasal congestion, sneezing, coughing, and the appearance of a severely itchy urticarial rash on the skin. To facilitate breathing, a woman takes a characteristic orthopnea posture: she sits or stands, leaning forward and raising her shoulders. During an attack, intermittent speech is noted, an unproductive cough occurs with the discharge of a small amount of vitreous sputum, wheezing wheezing is heard remotely, the heartbeat quickens, cyanosis of the skin and visible mucous membranes is observed. nine0006
To facilitate breathing, a woman takes a characteristic orthopnea posture: she sits or stands, leaning forward and raising her shoulders. During an attack, intermittent speech is noted, an unproductive cough occurs with the discharge of a small amount of vitreous sputum, wheezing wheezing is heard remotely, the heartbeat quickens, cyanosis of the skin and visible mucous membranes is observed. nine0006
In breathing, auxiliary muscles are usually involved - the shoulder girdle, the abdominal press. The intercostal spaces expand and retract, and the chest takes on a cylindrical shape. On inspiration, the wings of the nose swell. Asphyxiation is provoked by the action of a certain aeroallergen, a nonspecific irritant (tobacco smoke, gases, harsh perfumes), and physical activity. Periodically, symptoms develop at night, disturbing sleep. With a prolonged course, pain may appear in the lower parts of the chest, associated with overstrain of the diaphragm. The attack ends spontaneously or after the use of bronchodilators. In the interictal period, clinical manifestations are usually absent. nine0006
In the interictal period, clinical manifestations are usually absent. nine0006
Complications
In the absence of proper drug control, a pregnant woman with signs of bronchial asthma develops respiratory failure, arterial hypoxemia, and peripheral microcirculation is disturbed. As a result, 37% of patients have early toxicosis, 43% have preeclampsia, 26% have a threat of abortion, and 14.2% have preterm birth. The occurrence of hypoxia at the time when the laying of the main organs and systems of the child occurs, leads to the formation of congenital developmental anomalies. According to research results, heart defects, developmental disorders of the gastrointestinal tract, spine, and nervous system are observed in almost 13% of children born by women with exacerbations and asthma attacks in the 1st trimester. nine0006
Immune complexes circulating in the blood damage the endothelium of the uteroplacental vessels, which leads to placental insufficiency in 29% of pregnancies with BA.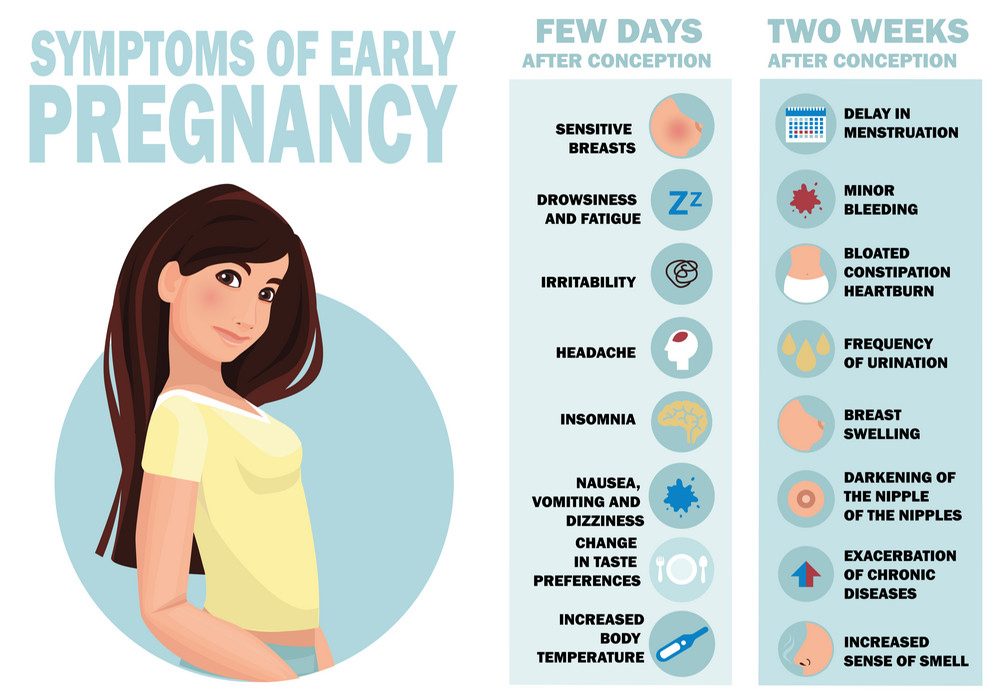 Fetal growth retardation is found in 27% of patients, malnutrition - in 28%, hypoxia and asphyxia of newborns - in 33%. Every third child born to a woman with a clinic of bronchial asthma is underweight. This figure is even higher in the steroid-dependent form of the disease. Constant interaction with the mother's antigens sensitizes the child to allergens. In the future, 45-58% of children have an increased risk of developing allergic diseases, they are more likely to suffer from acute respiratory viral infections, bronchitis, and pneumonia. nine0006
Fetal growth retardation is found in 27% of patients, malnutrition - in 28%, hypoxia and asphyxia of newborns - in 33%. Every third child born to a woman with a clinic of bronchial asthma is underweight. This figure is even higher in the steroid-dependent form of the disease. Constant interaction with the mother's antigens sensitizes the child to allergens. In the future, 45-58% of children have an increased risk of developing allergic diseases, they are more likely to suffer from acute respiratory viral infections, bronchitis, and pneumonia. nine0006
Diagnostics
The appearance of recurring attacks of suffocation and a sudden unproductive cough in a pregnant woman is a sufficient basis for a comprehensive examination to confirm or refute the diagnosis of bronchial asthma. In the gestational period, there are certain restrictions on the conduct of diagnostic tests. Due to the possible generalization of an allergic reaction, provocative and scarifying tests with probable allergens, provocative inhalations of histamine, methacholine, acetylcholine and other mediators are not prescribed to pregnant women.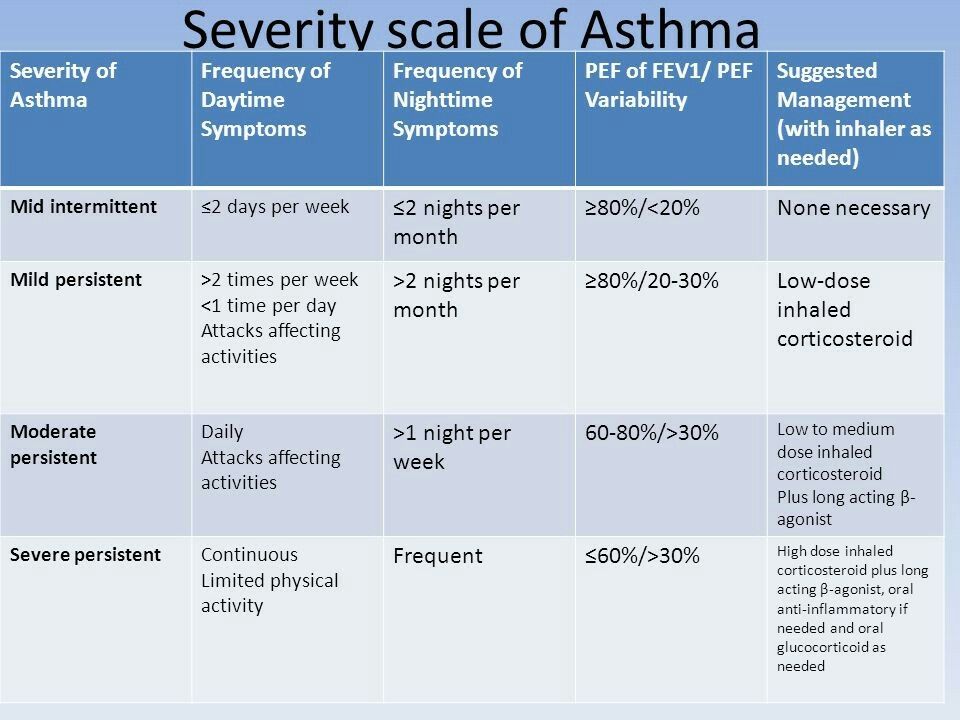 The most informative for the diagnosis of bronchial asthma during pregnancy are: nine0006
The most informative for the diagnosis of bronchial asthma during pregnancy are: nine0006
- Percussion and auscultation of the lungs. During an attack, a box sound is noted above the lung fields. The lower borders of the lungs are shifted down, their excursion is practically not determined. Weakened breathing with scattered dry rales is heard. After coughing, mainly in the posterior lower parts of the lungs, wheezing intensifies, which in some patients can persist between attacks.
- Allergy markers. Bronchial asthma is characterized by an increase in the levels of histamine, immunoglobulin E, eosinophilic cationic protein (ECP). The content of histamine and IgE is usually increased both during an exacerbation and between asthmatic attacks. An increase in the concentration of ECP indicates a specific immune response of eosinophils to the allergen + immunoglobulin E complex. nine0015
- Spirometry and peak flowmetry. A spirographic study allows, on the basis of data on the forced expiratory second volume (EF1), to confirm functional disorders of external respiration of an obstructive or mixed type.
 In the course of peak flowmetry, latent bronchospasm is detected, the degree of its severity and the daily variability of peak expiratory flow rate (PSV) are determined.
In the course of peak flowmetry, latent bronchospasm is detected, the degree of its severity and the daily variability of peak expiratory flow rate (PSV) are determined.
Additional diagnostic criteria are an increase in the content of eosinophils in the general blood test, the detection of eosinophilic cells, Charcot-Leyden crystals and Kurshman spirals in the analysis of sputum, the presence of sinus tachycardia and signs of overload of the right atrium and ventricle on the ECG. Differential diagnosis is carried out with chronic obstructive pulmonary diseases, cystic fibrosis, tracheobronchial dyskinesia, constrictive bronchiolitis, fibrosing and allergic alveolitis, tumors of the bronchi and lungs, occupational diseases of the respiratory organs, pathology of the cardiovascular system with heart failure. According to the indications, the patient is consulted by a pulmonologist, an allergist. nine0006
Treatment of asthma during pregnancy
When managing patients with asthma, it is important to ensure high-quality monitoring of the state of the pregnant woman, the fetus, and to maintain respiratory function at a normal level.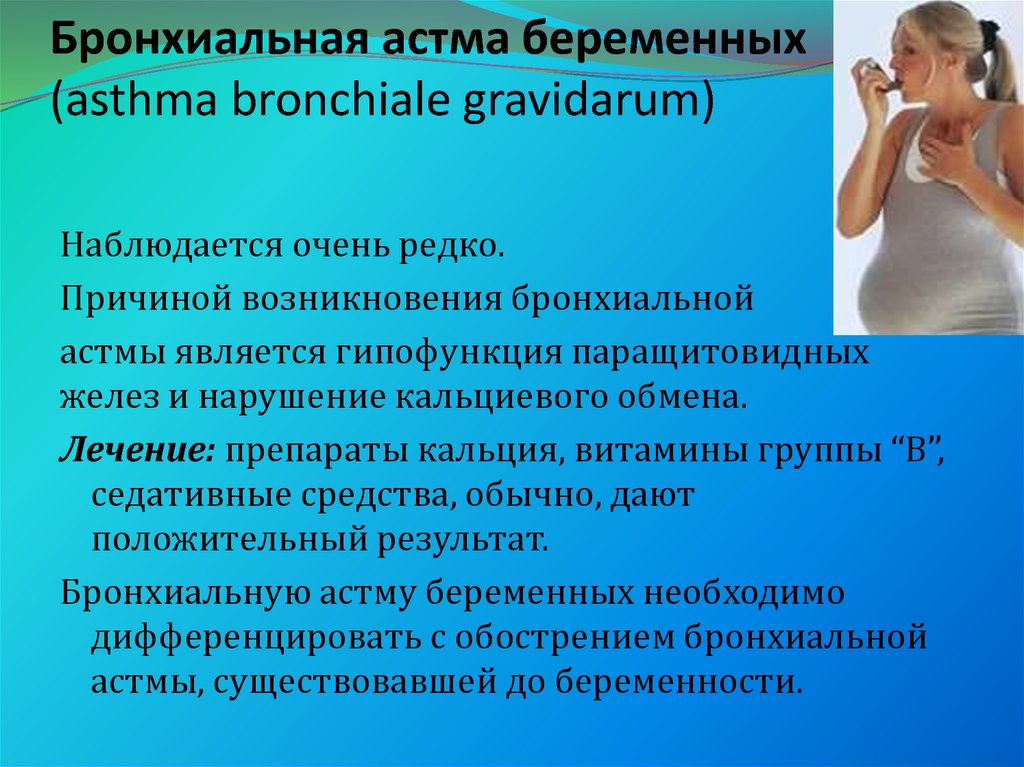 With a stable course of the disease, a pulmonologist examines a woman three times during pregnancy - at 18-20, 28-30 weeks of gestation and before childbirth. The function of external respiration is monitored using peak flowmetry. Taking into account the high risk of placental insufficiency, fetometry and dopplerography of placental blood flow are regularly performed. When choosing a pharmacotherapy regimen, the severity of bronchial asthma is taken into account: nine0006
With a stable course of the disease, a pulmonologist examines a woman three times during pregnancy - at 18-20, 28-30 weeks of gestation and before childbirth. The function of external respiration is monitored using peak flowmetry. Taking into account the high risk of placental insufficiency, fetometry and dopplerography of placental blood flow are regularly performed. When choosing a pharmacotherapy regimen, the severity of bronchial asthma is taken into account: nine0006
- In case of intermittent form of asthma, the basic drug is not prescribed. Before probable contact with an allergen, when the first signs of bronchospasm appear and at the time of an attack, inhaled short-acting bronchodilators from the group of β2-agonists are used.
- In persistent forms of asthma: basic therapy with category B inhaled glucocorticoids is recommended, which, depending on the severity of asthma, are combined with antileukotrienes, short-acting or long-acting β-agonists. The attack is stopped with the help of inhaled bronchodilators.
 nine0015
nine0015
The use of systemic glucocorticosteroids, which increase the risk of developing hyperglycemia, gestational diabetes, eclampsia, preeclampsia, and low birth weight, is justified only if basic pharmacotherapy is not effective enough. Triamcinolone, dexamethasone, depot forms are not shown. Prednisolone analogs are preferred. During exacerbation, it is important to prevent or reduce possible fetal hypoxia. For this, inhalations with quaternary atropine derivatives are additionally used, oxygen is used to maintain saturation, in extreme cases, artificial ventilation is provided. nine0006
Although vaginal delivery is recommended for the calm course of bronchial asthma, in 28% of cases, in the presence of obstetric indications, a caesarean section is performed. After the onset of labor, the patient continues to take basic drugs in the same dosages as during gestation. If necessary, oxytocin is prescribed to stimulate uterine contractions. The use of prostaglandins in such cases can provoke bronchospasm. During breastfeeding, it is necessary to take basic anti-asthma drugs in doses that correspond to the clinical form of the disease. nine0006
The use of prostaglandins in such cases can provoke bronchospasm. During breastfeeding, it is necessary to take basic anti-asthma drugs in doses that correspond to the clinical form of the disease. nine0006
Prognosis and prevention
Adequate therapy of bronchial asthma during pregnancy can completely eliminate the danger to the fetus and minimize the threat to the mother. Perinatal prognosis with controlled treatment does not differ from prognosis for children born by healthy women. For prophylactic purposes, patients at risk who are prone to allergic reactions or suffering from atopic diseases are recommended to quit smoking, limit contact with household, industrial, food, plant, and animal exoallergens. To reduce the frequency of exacerbations, pregnant women with asthma are shown exercise therapy, therapeutic massage, special sets of breathing exercises, and speleotherapy. nine0006
You can share your medical history, what helped you in the treatment of bronchial asthma during pregnancy.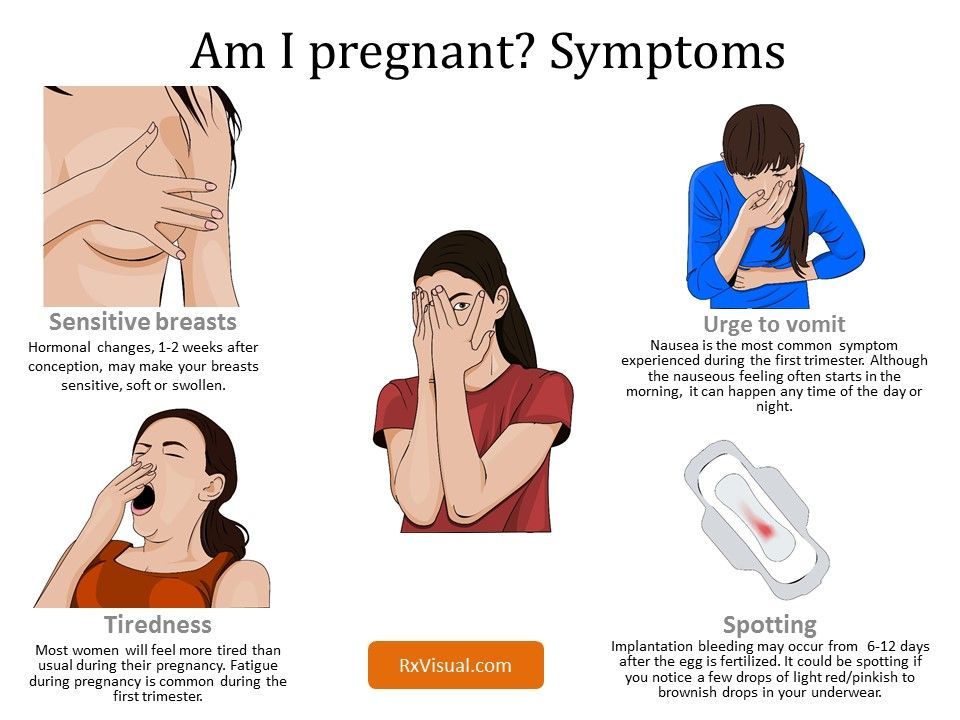
Sources
- Bronchial asthma in pregnant women / Ignatova G.L., Antonov V.N. // Medical review. - 2015 - No. 4.
- Bronchial asthma and pregnancy / Belan EB, Klyausov AS// Medicinal Bulletin. - 2014 - Vol. 8, No1 (53).
- Bronchial asthma and pregnancy / Lavrova OV, Dymarskaya Yu.R.// Practical pulmonology. – 2015.
- Features of pregnancy outcomes in patients suffering from bronchial asthma of varying severity / Lavrova OV, Shapovalova EA, Dymarskaya Yu.R.// Journal of Obstetrics and Women's Diseases. – 2017.
- This article was prepared based on the materials of the site: https://www.krasotaimedicina.ru/
IMPORTANT
Information from this section cannot be used for self-diagnosis and self-treatment. In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor. nine0006
nine0006
Bronchial asthma and pregnancy
220045, Minsk, st. Semashko, 10
This email address is being protected from spambots. You must have JavaScript enabled to view.
version of the site for visually impaired
Healthcare Institution
Minsk Clinical Consultative and Diagnostic Center
Coll-Center (Registration)
| +375 17 311 10 19 (10 lines) | |
| +375 17 355 94 50 (7 lines) | |
| +375 29 238 00 90 (mobile MTS 4 lines) | |
| +375 44 550 00 90 (mobile A1 4 lines) |
Apply online
Minsk Clinical Consultative and Diagnostic Center Book online Bronchial asthma is one of the most common lung diseases in pregnant women. This disease is characterized by inflammation and temporary obstruction of the airways and occurs against the background of increased excitability of the airways in response to various influences. Symptoms Regardless of the form of bronchial asthma, three stages of its development are distinguished: pre-asthma, asthma attacks and status asthmaticus. All forms and stages of the disease occur during pregnancy. In the initial stage of asthma, asthma attacks develop periodically. They begin more often at night, last from several minutes to several hours. Suffocation is preceded by a sensation of scratching in the throat, sneezing, runny nose, tightness in the chest. The attack begins with persistent paroxysmal cough, no sputum. There is a sharp difficulty in exhaling, tightness in the chest, nasal congestion. Breathing becomes noisy, whistling, hoarse, audible at a distance. The face becomes bluish. The skin is covered with perspiration. By the end of the attack, sputum begins to separate, which becomes more and more liquid and plentiful. Features of the course of bronchial asthma during pregnancy and childbirth When pregnancy develops in women with bronchial asthma, pathological changes occur in the immune system, which have a negative impact on both the course of the disease and the course of pregnancy. Bronchial asthma usually begins before pregnancy, but may first appear during it. In some patients, asthma attacks develop at the beginning of pregnancy, in others - in the second half. Asthma that occurs at the beginning of pregnancy, like early toxicosis, may disappear by the end of its first half. In these cases, the prognosis for the mother and fetus is usually quite favorable. According to some data, during pregnancy, 20% of patients remain in the same condition as before pregnancy, 10% improve, and in most women (70%) the disease is more severe, with moderate and severe exacerbations predominating with repeated daily attacks. suffocation, periodic asthmatic conditions, unstable effect of treatment. Treatment of bronchial asthma during pregnancy When treating asthma in pregnant women, it should be borne in mind that all drugs used for this purpose pass through the placenta and can harm the fetus, and since the fetus is often in a state of hypoxia (oxygen starvation ), the minimum amount of drugs should be administered. If the course of asthma during pregnancy does not worsen, there is no need for drug therapy. Prevention of complications of pregnancy It is necessary for the woman to eliminate risk factors for exacerbation of the disease. In this case, the removal of the allergen is very important. This is achieved by wet cleaning of the premises, excluding food products that cause allergies (oranges, grapefruits, eggs, nuts, etc.), and non-specific food irritants (pepper, mustard, spicy and salty dishes). In some cases, the patient needs to change jobs if it is associated with chemicals that play the role of allergens (chemicals, antibiotics, etc.). Pregnant women with bronchial asthma should be registered with a antenatal clinic physician. Each "cold" disease is an indication for treatment with antibiotics, physiotherapy, expectorants, for the prophylactic administration of drugs that dilate the bronchi, or for increasing their dose. +375 17 355 94 50 (Horizontal) +375 29 238 00 90 (mobile MTS) +375 44 550 00 90 (mobile A1) You are here:
 nine0006
nine0006 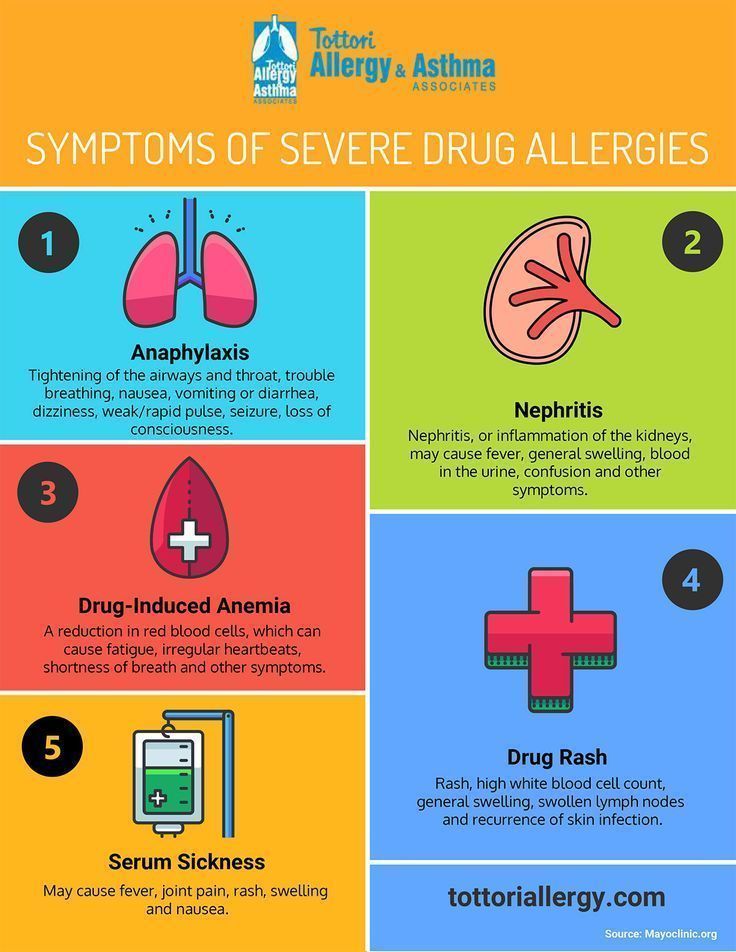 nine0006
nine0006 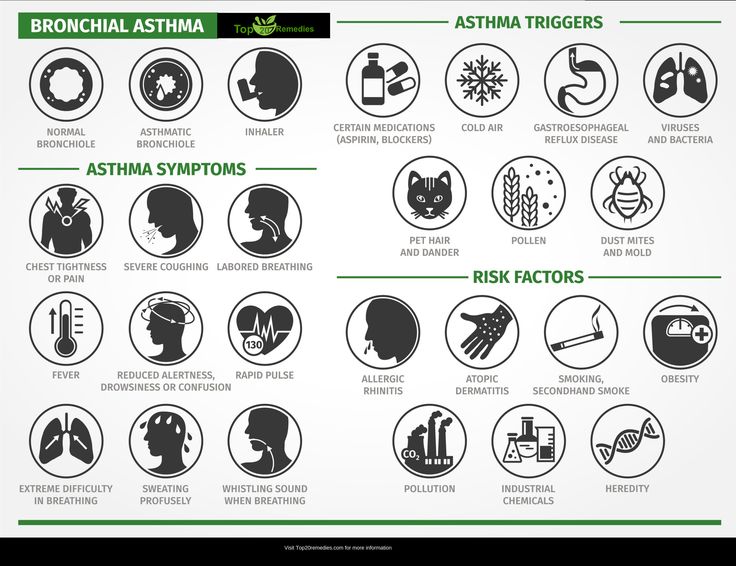 The course of asthma usually worsens already in the first trimester of pregnancy. In the second half of the disease is easier. Attacks of bronchial asthma during childbirth are rare, especially with the prophylactic use of glucocorticoid drugs (prednisolone, hydrocortisone) or bronchodilators (eufillin) during this period. After childbirth, the course of bronchial asthma improves in 25% of women (these are patients with a mild form of the disease). In 50% of women, the condition does not change, in 25% it worsens. Patients with bronchial asthma are more likely than healthy women to develop early toxicosis, the threat of miscarriage, labor disorders, rapid and rapid labor, resulting in high birth traumatism, premature and underweight babies can be born. Cases of fetal death before and during childbirth are noted only in severe cases of the disease and inadequate treatment of asthmatic conditions. The illness of the mother can affect the health of the child. In 5% of children, asthma develops in the first year of life, in 58% - in subsequent years.
The course of asthma usually worsens already in the first trimester of pregnancy. In the second half of the disease is easier. Attacks of bronchial asthma during childbirth are rare, especially with the prophylactic use of glucocorticoid drugs (prednisolone, hydrocortisone) or bronchodilators (eufillin) during this period. After childbirth, the course of bronchial asthma improves in 25% of women (these are patients with a mild form of the disease). In 50% of women, the condition does not change, in 25% it worsens. Patients with bronchial asthma are more likely than healthy women to develop early toxicosis, the threat of miscarriage, labor disorders, rapid and rapid labor, resulting in high birth traumatism, premature and underweight babies can be born. Cases of fetal death before and during childbirth are noted only in severe cases of the disease and inadequate treatment of asthmatic conditions. The illness of the mother can affect the health of the child. In 5% of children, asthma develops in the first year of life, in 58% - in subsequent years. Newborns of the first year of life often develop diseases of the upper respiratory tract. The postpartum period in 15% of puerperas with bronchial asthma is accompanied by an exacerbation of the underlying disease. Patients with bronchial asthma during full-term pregnancy usually give birth through the natural birth canal, since asthma attacks during childbirth are not difficult to prevent. Frequent asthma attacks and asthmatic conditions observed during pregnancy, the ineffectiveness of the treatment are indications for early delivery at 37-38 weeks of pregnancy. nine0006
Newborns of the first year of life often develop diseases of the upper respiratory tract. The postpartum period in 15% of puerperas with bronchial asthma is accompanied by an exacerbation of the underlying disease. Patients with bronchial asthma during full-term pregnancy usually give birth through the natural birth canal, since asthma attacks during childbirth are not difficult to prevent. Frequent asthma attacks and asthmatic conditions observed during pregnancy, the ineffectiveness of the treatment are indications for early delivery at 37-38 weeks of pregnancy. nine0006 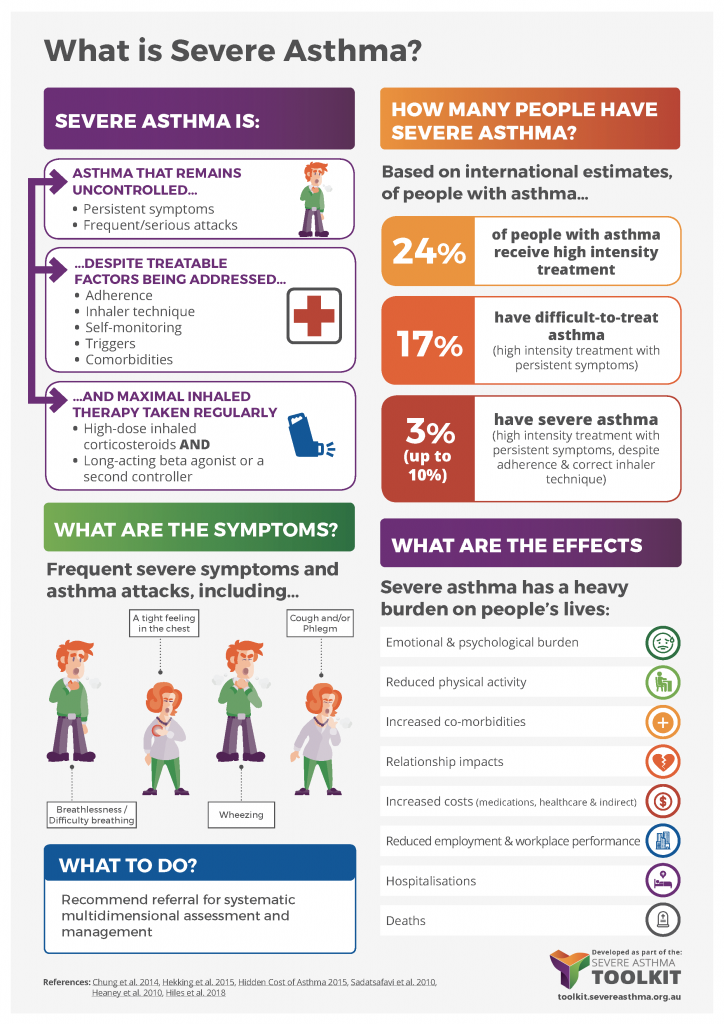 However, it should be borne in mind that severe and poorly treated asthma poses a much greater risk to the fetus than the drug therapy used to treat it. But in all cases, a pregnant woman suffering from bronchial asthma should use medications only as directed by a doctor. . nine0006
However, it should be borne in mind that severe and poorly treated asthma poses a much greater risk to the fetus than the drug therapy used to treat it. But in all cases, a pregnant woman suffering from bronchial asthma should use medications only as directed by a doctor. . nine0006