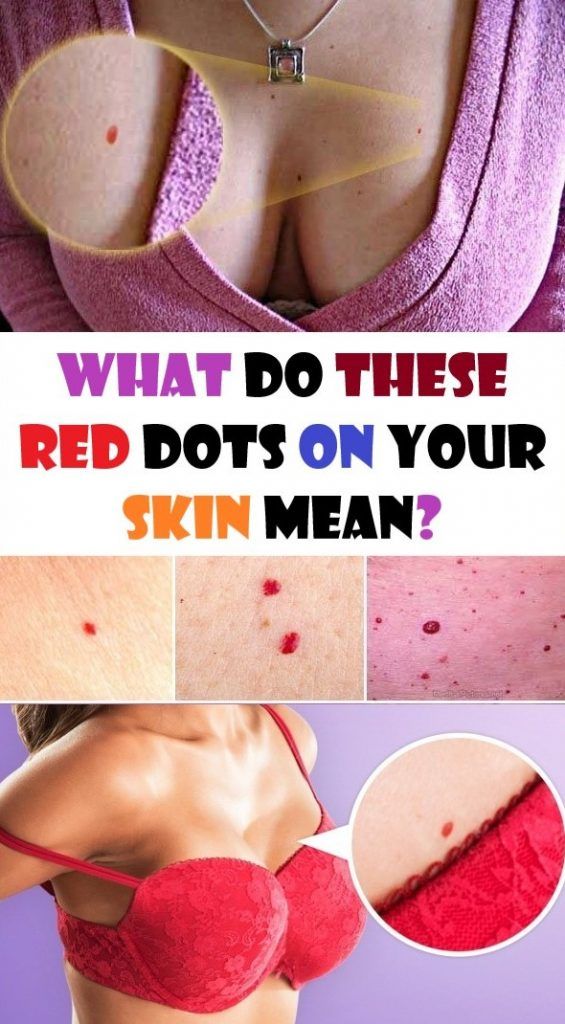
Red dot skin rash
Pictures, causes, treatment, and when to seek help
A person may notice red dots on their skin for a number of reasons, ranging from allergic reactions to heat exposure.
Many causes of red dots on the skin are harmless and resolve on their own. Others may require at-home or over-the-counter (OTC) treatment.
In this article, we discuss some of the possible causes of red dots on the skin, their treatment options, and when to contact a doctor.
Skin rashes come in a variety of sizes, colors, and textures.
Not all rashes require emergency medical treatment. However, people should seek immediate medical attention if they have a rash and notice any of the following symptoms:
- a rash that covers the entire body
- fever
- blisters or open wounds
- difficulty breathing, speaking, or swallowing
- swelling of the face, eyes, or lips
- stiff neck
- light sensitivity
- seizures
- drowsiness or unresponsiveness
People should also seek immediate attention for any new rashes that are painful and that affect the eyes, inside of the mouth, or genitalia.
When in doubt, a person should seek the opinion of a primary care provider or board-certified dermatologist.
Heat rash, or miliaria, occurs when the sweat glands become blocked, trapping sweat in the deep layers of the skin.
While anyone can have heat rash, this condition is most common among infants and young children with immature sweat glands.
Symptoms of heat rash include:
- clusters of small red bumps called papules
- firm, flesh-colored bumps
- itchy or prickly sensation
- mild or absent sweating in the affected area
- inflammation and soreness
- dizziness
- nausea
Treatment
Heat rash usually goes away within 24 hours.
Treatment typically involves using lotions to soothe the itching, irritation, and swelling.
People can also keep the skin cool and avoid tight-fitting clothing.
Learn more about the treatment options for heat rash here.
Keratosis pilaris (KP) is a common skin condition that causes tiny red, white, or flesh-colored bumps on the skin.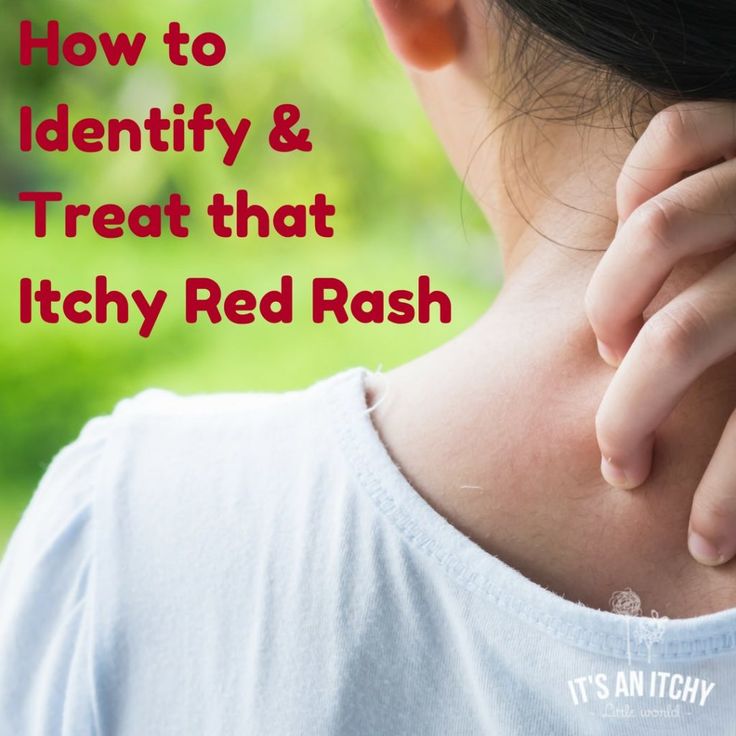
It most often affects the outer parts of the upper arms. It can also affect the forearms and upper back, but this is less common.
Symptoms of KP include:
- skin that feels rough or dry
- patches of small, painless bumps on the skin
- itching
Treatment
People can treat the symptoms of KP with:
- moisturizers containing urea or lactic acid
- alpha hydroxy acid
- glycolic acid
- lactic acid
- retinoids
- salicylic acid
- laser or light therapy
Learn more about home management for KP here.
Contact dermatitis occurs when a person comes into contact with a substance that irritates their skin or triggers an allergic reaction.
Contact dermatitis symptoms vary depending on the trigger and the severity of the reaction.
Symptoms of contact dermatitis include:
- a rash that appears in geometric patterns or shapes
- dry skin that flakes and cracks
- a bright, flushed skin rash
- clusters of small red dots on the skin
- hives, or extremely itchy welts on the skin
- intense itching, tightness, or burning sensation
- fluid-filled blisters that ooze and crust over
- dark, thickened skin
- sensitivity to sunlight
Learn more about contact dermatitis here.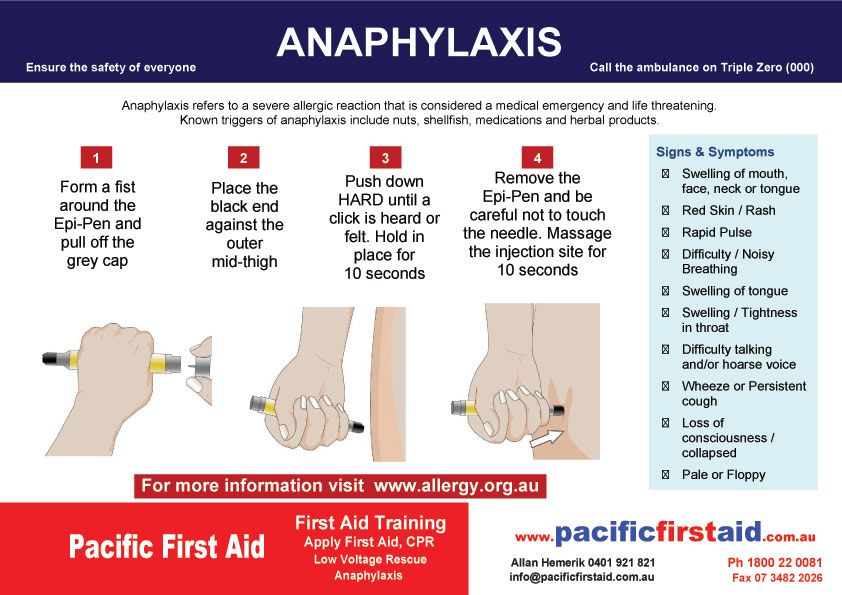
Treatment
Treatment for contact dermatitis depends on the cause and severity of a person’s symptoms.
Mild to moderate symptoms improve when a person avoids contact with the irritant or allergen. If possible, people should:
- avoid skin care products that contain harsh or irritating chemicals
- avoid nickel- or gold-plated jewelry
- avoid foods or medicines that cause allergic reactions
- wear protective clothing in work environments or areas with poisonous plants
If the dermatitis is limited to a small area, a person can apply 1% hydrocortisone cream.
A doctor can prescribe stronger topical or oral antihistamines for people who do not respond to OTC medication.
Atopic dermatitis, also known as eczema, is a chronic inflammatory skin condition.
There are many different types of eczema, including:
- Follicular eczema: This type of eczema affects the hair follicles.
- Papular eczema: This presents as small red bumps on the skin that healthcare professionals refer to as papules.

Alongside red bumps on the skin, eczema can cause:
- extremely itchy skin
- warmth and swelling of the skin
- dry, flaky skin
- clusters of small, fluid-filled blisters
- blisters that leak fluid and crust over
Treatment
People can manage atopic dermatitis symptoms and even prevent flare-ups with the following treatments:
- taking prescription medications, such as steroids and antihistamines
- undergoing phototherapy or light therapy
- applying a moisturizer to treat dry, cracking skin
- using unscented, nonirritating laundry detergent
- avoiding triggers, such as dry air, stress, and allergens
For severe atopic dermatitis that does not respond to the above treatment options, a person should see a board-certified dermatologist.
Taking bleach baths, which require using half a cup of bleach per 40-gallon tub, 1–2 times per week may also help.
Learn more about the treatment options for eczema here.
Rosacea is a skin condition that causes skin irritation, redness, and small pimples.
Although anyone can develop rosacea at any point in their lives, this condition most often occurs among adults aged 30–60 years, people with fair skin, and those going through menopause.
Symptoms of rosacea include:
- irritated or red skin on the forehead, nose, cheeks, and chin
- blood vessels that are visible under the skin
- clusters of small bumps or pimples
- thick skin on the face
- red, itchy, or watery eyes
- inflammation of the eyelids
- blurred vision
Treatment
People can treat rosacea with various strategies and medication. Some strategies that can help relieve rosacea include:
- avoiding triggers, such as ultraviolet light, alcohol, and harsh chemicals
- washing the face with pH-balanced cleansers
- frequently using moisturizers
- wearing a broad-spectrum sunscreen with SPF 30 or higher
People should also avoid caffeinated products and spicy foods, as these can also trigger rosacea.
Medical treatments for rosacea include:
- brimonidine tartrate
- azelaic acid
- metronidazole
- electrosurgery
- light therapy
- topical ivermectin
- oral tetracyclines
Learn more about the treatment options for rosacea here.
Certain infections can also lead to red dots on the skin.
If a person suspects an infection of the skin, they should consult a doctor.
Examples of these include:
Chickenpox or shingles
The varicella-zoster virus causes these infections, which produce red, itchy, fluid-filled blisters that can appear anywhere on the body.
Chickenpox usually occurs in infants and young children. However, adolescents and adults can also develop chickenpox.
Shingles occurs in adults who have already had chickenpox. According to the National Institute on Aging, shingles usually affects one area on one side of the body.
Rubella
This contagious viral infection causes a distinctive rash of small red or pink dots.
The rash usually starts on the face before spreading to the trunk, arms, and legs. Rubella infections also cause a fever, a headache, and swollen lymph nodes.
The Centers for Disease Control and Prevention (CDC) note that rubella is a relatively rare infection in the United States due to the widespread use of the MMR vaccine. The vaccine is available for infants and children aged between 9 months and 6 years.
Meningitis
Meningitis is a medical emergency. It is the inflammation of the membranes that cover the spinal cord and brain. It typically occurs due to a bacterial or viral infection.
Symptoms of meningitis include:
- fever
- stiff neck
- headache
- nausea
- light sensitivity
- confusion
- vomiting
A rash does not always appear. However, if it does, a person might notice small pink, red, brown, or purple pinpricks on the skin. Also, it will not fade when a person rolls a glass over it.
MRSA (staph) infection
The CDC define Methicillin-resistant Staphylococcus aureus (MRSA) as “a type of bacteria that is resistant to several antibiotics. ”
”
MRSA often infects the skin, leading to painful areas of inflamed skin. People may also experience pus drainage from the affected skin and fever.
Other bacterial infections of the skin may also cause painful and inflamed areas of the skin. If a person suspects that they are experiencing a skin infection, they should consult a doctor.
Scarlet fever
Streptococcus bacteria cause this infection.
These bacteria naturally inhabit the nose and throat. They cause a red rash on the neck, under the armpit, and on the groin. The rash consists of small red dots that are rough to the touch.
If a person suspects an infection of the skin, they should always consult a doctor.
People should also speak with a doctor if their rash does not improve despite using OTC or at-home treatments.
People should also seek medical attention if they have a skin rash accompanied by the following symptoms:
- fever
- severe head or neck pain
- joint pain or stiffness
- difficulty breathing
- frequent vomiting or diarrhea
- confusion
- dizziness
If a person suspects a skin infection, they should contact a healthcare professional before trying any home remedies.
To relieve and manage skin rashes, people can try the following home treatments:
- using mild, unscented soaps, body washes, and cleansers
- avoiding bathing or showering in hot water
- keeping the affected skin dry and clean
- wearing loose-fitting, breathable clothing
- avoiding rubbing or scratching the skin rash
- applying a cold compress to relieve swelling and pain
- applying aloe vera to the affected skin to reduce swelling and soothe pain
- using moisturizers to hydrate dry, flaky skin
There are several possible causes for red dots on the skin, including heat rash, KP, contact dermatitis, and atopic dermatitis.
Red dots on the skin may also occur due to more serious conditions, such as a viral or bacterial infection.
If people suspect that they have a skin infection, they should contact a doctor rather than use home remedies.
People can treat some skin rashes and their accompanying symptoms with home remedies and OTC treatments. These include avoiding the source of irritation and using OTC anti-itch ointments.
These include avoiding the source of irritation and using OTC anti-itch ointments.
People can contact a doctor or dermatologist if their symptoms persist despite using at-home or OTC treatments. A doctor or dermatologist can diagnose the underlying cause and make appropriate treatment recommendations.
Read this article in Spanish.
Bumps on the skin: Pictures, causes, and treatments
We include products we think are useful for our readers. If you buy through links on this page, we may earn a small commission Here’s our process.
Medical News Today only shows you brands and products that we stand behind.
Our team thoroughly researches and evaluates the recommendations we make on our site. To establish that the product manufacturers addressed safety and efficacy standards, we:
- Evaluate ingredients and composition: Do they have the potential to cause harm?
- Fact-check all health claims: Do they align with the current body of scientific evidence?
- Assess the brand: Does it operate with integrity and adhere to industry best practices?
We do the research so you can find trusted products for your health and wellness.
Many types of bumps can appear on the skin. Papules, skin tags, and other bumps are often not serious, but some skin changes can be a sign of cancer.
As a result, anyone who notices any changes to their skin should speak with a doctor to rule out severe conditions.
In this article, we look at the symptoms, diagnosis, and treatment of some of the most common causes of bumps on the skin.
Common types of bumps on the skin include papules, skin tags, angiomas, and hemangiomas.
Papules
Doctors define a papule as any raised lesion or new growth on the skin that is less than 1 centimeter in diameter. For example, a small pimple or wart would be a papule.
A pustule is a type of papule that contains fluid or pus and typically has discolored or inflamed skin around it.
Both inflamed acne papules and pustules can appear when the pores of the skin become clogged with old skin cells, oil from the skin, and bacteria.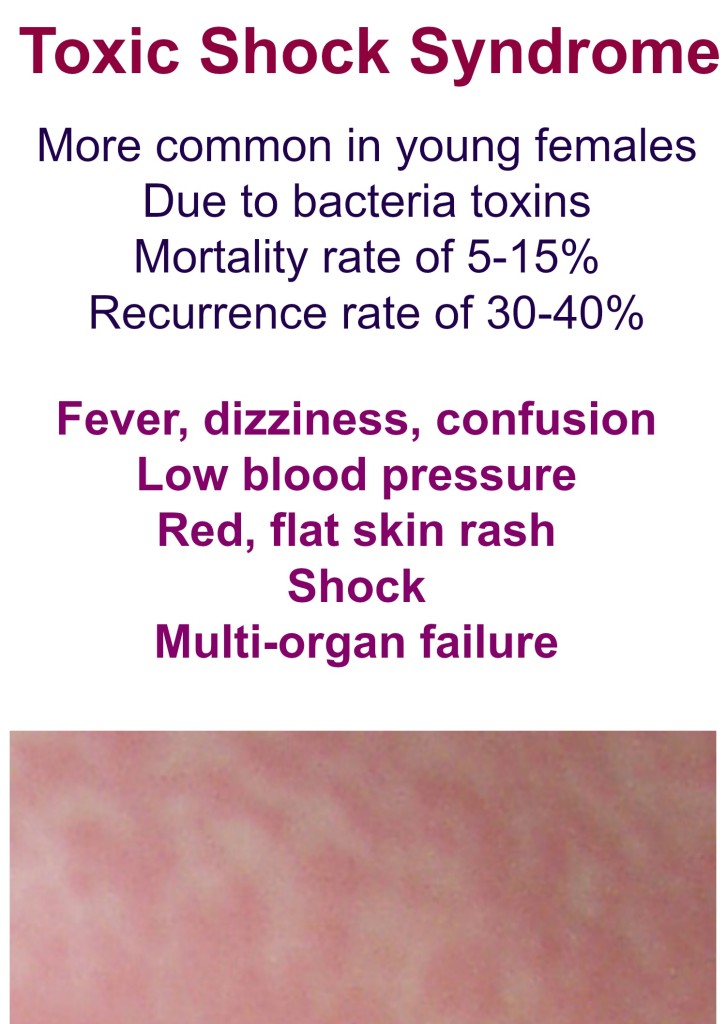
Over-the-counter medications can occasionally treat acne. If these do not work, a dermatologist — a doctor who specializes in the skin — can prescribe medications.
Although it is not always possible to prevent acne, practicing good skin care can help. People should wash their face twice a day and use lotion or makeup that is noncomedogenic.
Although it can be tempting to squeeze pimples, doing so can make the inflammation worse and possibly cause the skin to scar instead.
Skin tags
Skin tags are another common type of growth on the skin. The medical name for a skin tag is acrochordon. Skin tags tend to be flesh-colored growths that hang from the surface of the skin by a “stalk.”
Skin tags are more common in older people, and they usually appear in areas where skin rubs on skin, such as in the armpits, the groin, and around the neck.
These growths do not usually cause pain, and they are almost always benign, so doctors consider them a cosmetic concern rather than a medical issue. However, in rare cases, some forms of skin cancer can resemble a skin tag.
However, in rare cases, some forms of skin cancer can resemble a skin tag.
Skin tags do not go away on their own. Anyone looking to remove them will need to see a doctor.
The removal process is quick and easy. Doctors can cut skin tags away with scissors or a sharp blade, and they may use an electric cauterizing tool to prevent bleeding.
Doctors can usually diagnose skin tags easily by looking at them. However, if it is not obvious that a growth is a skin tag, a doctor may perform a biopsy. This involves removing a sample of the growth and sending it to a laboratory for testing.
Angiomas and hemangiomas
Hemangiomas are a type of noncancerous growth that can appear on the skin. They are typically red or dark purple, depending on skin tone, and people sometimes call them birthmarks or “strawberry marks.” A baby may be born with this growth, or it may appear in the first few weeks after birth.
If someone has multiple hemangiomas on their skin, they are at increased risk of an internal hemangioma.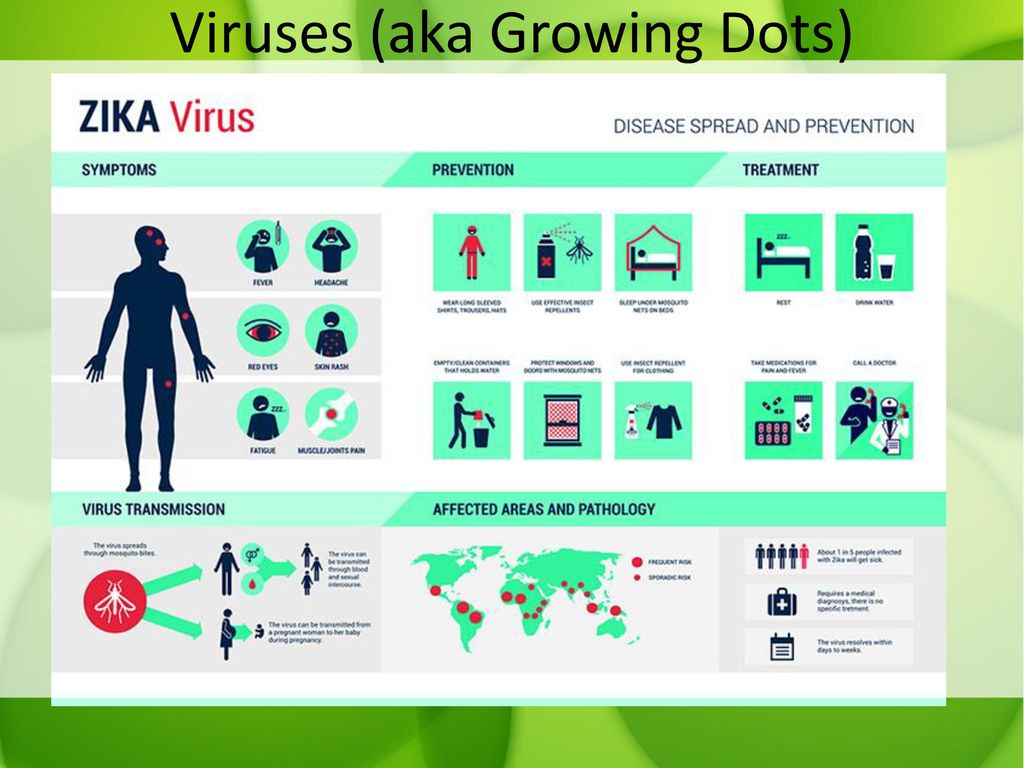 Internal hemangiomas grow in the internal organs — most often, the liver. They may also grow on muscles and bones.
Internal hemangiomas grow in the internal organs — most often, the liver. They may also grow on muscles and bones.
Angiomas are small, discolored papules that develop on the skin. They can appear at any age but are more common among older people. They may be less noticeable in people with skin of color.
It is possible to develop multiple angiomas, which does not increase a person’s risk of internal angiomas or hemangiomas.
These skin bumps do not require treatment unless they bleed or are painful, but some people may wish to remove them for cosmetic reasons.
A doctor may use electrocauterization, laser therapy, or liquid nitrogen to remove angiomas. More extensive surgery may be necessary to remove a hemangioma if it is damaging nearby tissue or organs.
Doctors can typically diagnose both conditions during an appointment, but they may monitor the growths for signs of other skin conditions, including skin cancer. If the skin bumps are not causing issues, doctors may choose to observe them rather than treat them.
Although there are many benign causes of skin bumps, this symptom might indicate cancer in some cases.
Actinic keratosis
Skin cancers and precancerous lesions usually result from excessive exposure to the sun or other sources of UV light. Precancerous growths include actinic keratoses.
Actinic keratosis is most likely to appear on areas of the body that get exposure to UV light. These areas include the:
- face
- scalp
- ears
- lips
- shoulders
- neck
- chest
- arms
- legs
- back
- back of the hands
Actinic keratoses appear as rough, scaly patches that people often describe as “dry patches.” Occasionally, they are raised in texture. They can come and go and typically show up more when in the sun. They can sometimes be tender to the touch.
About 10% of actinic keratoses can turn into squamous cell carcinoma, although this percentage is higher among people with a weakened immune system.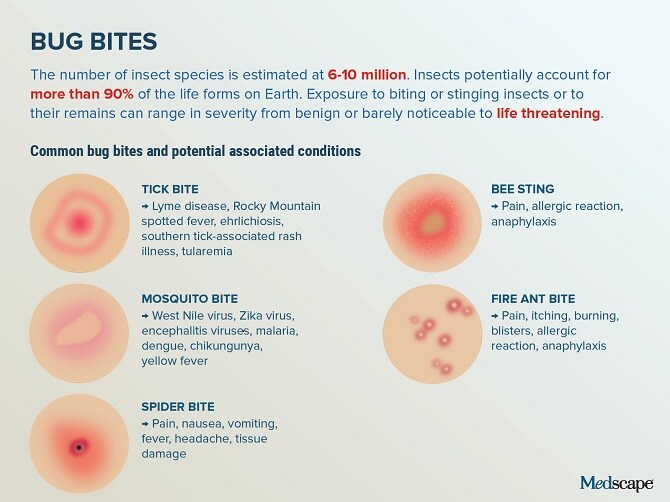
Doctors can treat actinic keratoses in the office with liquid nitrogen. Other treatment options include topical chemotherapy creams, such as aminolevulinic acid HCl (Levulan), which doctors might use alongside blue light therapy.
Basal cell carcinoma
The most common type of skin cancer is basal cell carcinoma (BCC), with doctors diagnosing more than 3 million cases every year in the United States. BCC can look like an open sore, a papule or growth that does not heal or bleeds easily on its own, a shiny bump, or a discolored scaly patch.
BCC usually results from intense sun exposure and very rarely spreads to other areas of the body. However, it is important to get treatment for BCC to prevent it from destroying the surrounding skin and potentially invading nerve tissue.
Various treatment options are available for BCC. Although the most common recommendation is excision, Mohs surgery might be a better option if the skin cancer affects thinner tissue, such as the face.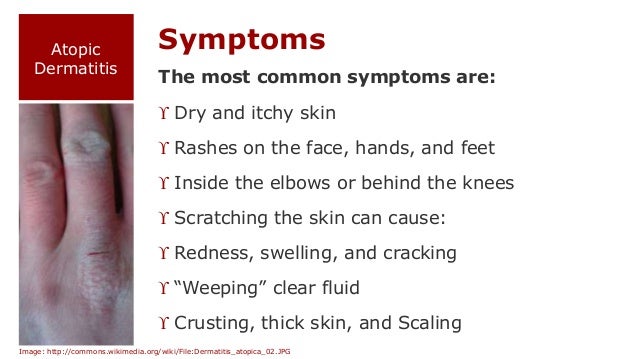
If the lesions are more superficial, doctors may recommend either a topical chemotherapy cream or electrocautery and desiccation in the office. They are unlikely to use radiation therapy to treat a superficial skin cancer unless the person is older in age or the skin cancer is difficult to treat with surgery.
Squamous cell carcinoma
Squamous cell carcinoma is the second most common type of skin cancer. Squamous cells are present throughout the body, as they line the throat, skin, lungs, and organs.
Squamous cell carcinoma can develop anywhere these cells are present. It often presents as a rough, scaly patch, but it can also look like a wart, dark brown mole, or open sore.
Before the cancer develops, some people may notice signs of skin damage, such as age spots or patches of discolored skin. In some cases, actinic keratosis develops into squamous cell carcinoma.
This type of skin cancer is more common in people with fair skin, but People of Color can also develop it. When they do, the cancerous spots tend to be in areas that do not commonly have exposure to the sun, such as the mouth, genitals, or anus.
When they do, the cancerous spots tend to be in areas that do not commonly have exposure to the sun, such as the mouth, genitals, or anus.
Squamous cell carcinoma is not usually life threatening, but the tumor can grow large enough to injure nerves and blood vessels.
A doctor will likely take a biopsy of the spot to determine whether it is a squamous cell carcinoma or another type of skin cancer or lesion.
The treatment options include surgical removal, liquid nitrogen, and radiation therapy.
Melanoma
The most aggressive type of skin cancer is melanoma.
Melanoma can affect any area of the body. It can grow deep into the skin and may also affect the lymph nodes and blood vessels. Without treatment, melanoma can spread to the bones and organs.
Experts estimate that doctors will diagnose 197,700 new cases of melanoma in 2022 in the U.S. Of these, 97,920 will be noninvasive, and 99,780 will be invasive.
Despite only accounting for about 5% of all skin cancer diagnoses in the U.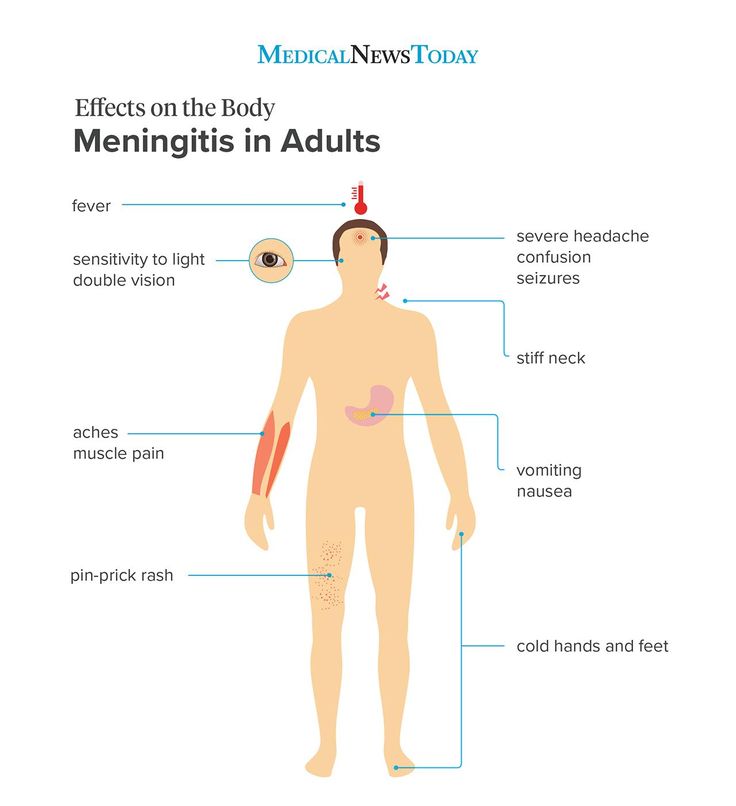 S., melanoma is responsible for the majority of deaths from skin cancer.
S., melanoma is responsible for the majority of deaths from skin cancer.
Melanomas are typically dark brown, pink, or black with an irregular border, although they can also be multicolored. They may sometimes arise from a large or atypical mole. In rare cases, they appear as growths with no melanin, which are known as amelanotic melanoma. These are faint and can be difficult to detect, increasing the risk of the cancer spreading.
It is important to adopt sun-safety habits to protect the skin. People should avoid direct sunlight for prolonged periods, especially between the hours of 10 a.m. and 4 p.m.
The advice is to apply 1 ounce of sunscreen with an SPF of 15 or higher to the entire body 30 minutes before going outside. Those who plan on being outside for a long time should use a broad-spectrum sunscreen with an SPF of 30 or higher. They should reapply the sunscreen every 2 hours.
A sunscreen with a physical blocker, such as zinc oxide or titanium dioxide, might provide better protection. People with sensitive skin should look for noncomedogenic products.
People with sensitive skin should look for noncomedogenic products.
Many different sunscreen products are available for purchase online.
It is also important to avoid using tanning beds, which increase the risk of skin cancer.
People should check their skin once a month and contact a doctor if they notice any new or changing lesions, or anything that itches, bleeds on its own, or does not heal.
People should examine their skin at home each month and let a doctor know if they notice any new or changing skin symptoms. It is important for the doctor to carry out a physical examination to rule out potentially severe conditions, such as skin cancer.
The doctor might also need to carry out tests to confirm a diagnosis. For example, carcinomas can often resemble other skin conditions, such as psoriasis or eczema, so a biopsy may be necessary.
Once the doctor has the results of the biopsy, they can decide on the most effective treatments.
Rubella in children and adults: symptoms, treatment methods
Author
Zurnadzhi Elena Vyacheslavovna
Leading physician
Pediatrician
Creation date: 2016. 03.30
03.30
Cashback 1000 rub for all services for a visit in January More All promotions
Rubella is an acute viral disease predominantly of childhood. A typical manifestation: a pink-red rash that appears first on the face, and then spreads throughout the body within a few hours. nine0005
The susceptibility of children to rubella is high. Usually, children under the age of 6 months have innate immunity received from their mother, but if the child does not have specific antibodies, he can get sick even in the first months of life.
Rubella most often affects children aged 2 to 9 years.
Immunity after the transferred rubella is persistent, lifelong.
Any questions?
Leave the phone -
and we will call you back
Causes of rubella
Rubella is transmitted by airborne droplets. Although the virus is considered non-persistent, contact transmission of the disease (for example, through children's toys) is also possible.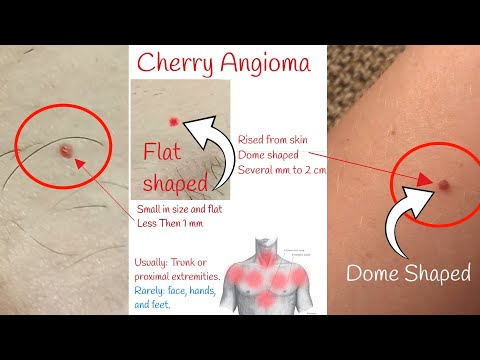
The incubation period for rubella is from 11 to 24 days (in most cases - from 16 to 20 days). The patient is contagious already a week before the rash appears. After the rash, the risk of infection persists for another 5-7 days.
Another option for transmission of infection is during pregnancy, from mother to fetus. With such congenital rubella, the virus is secreted for a long time - within 1.5-2 years after birth (with sputum, urine, feces). nine0005
Rubella risk
The main danger of the disease lies in its effect on the fetus in the early stages of pregnancy. Up to 11 weeks, the probability of infection of the fetus upon contact with the source of infection is 90%. The consequences can be serious: various pathologies and fetal death. Therefore, rubella is included in the number of ToRCH infections (a group of infections that pose a particular danger to the fetus and the health of the unborn child).
Rubella symptoms
The main symptoms of rubella are:
Rash
Rubella is manifested primarily by a rash.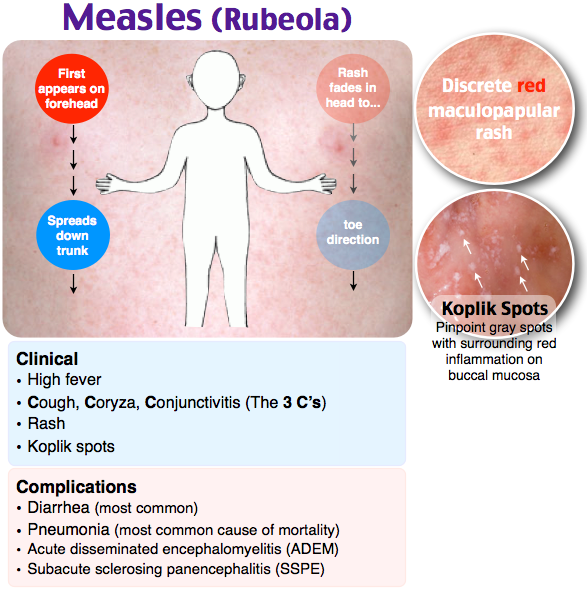 The rubella rash looks like small pink-red spots of a round or oval shape.
The rubella rash looks like small pink-red spots of a round or oval shape.
In children, the rash lasts 2-4, occasionally 5-7 days, then disappears - without pigmentation and peeling.
More about the symptom
Swollen lymph nodes
There is enlargement of the lymph nodes, especially those located on the back of the head and back of the neck. nine0005
Catarrhal phenomena
Sometimes in children with rubella, catarrhal phenomena are observed: a slight runny nose, sore throat, dry cough.
Symptoms of rubella in adults
In adults, rubella is much more severe: headache, general weakness, fever (up to 38-39 ° C), muscles hurt. The disease can affect the joints (primarily the small joints of the hands).
Methods for diagnosing rubella
Do not assume that you or your child is already immune because you have experienced symptoms that fit the description of rubella. Other viral diseases can have similar symptoms. Absolute certainty can only be given by a blood test for specific antibodies.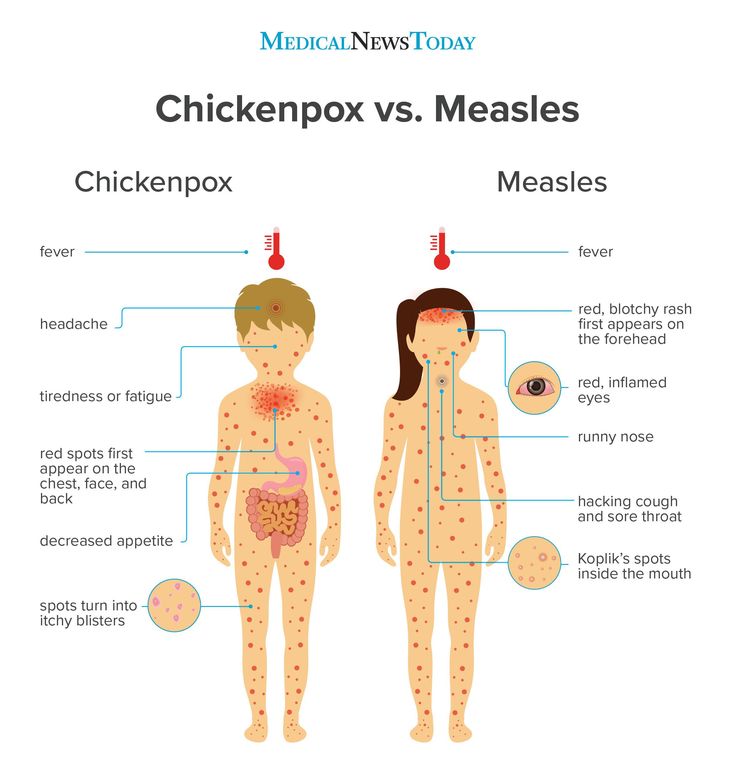
Serological blood test
Serological analysis detects the presence of antibodies to the rubella virus in the blood. Such an analysis can be done separately, or you can use the "Diagnostics of ToRCH infections" profile. nine0005
More about the diagnostic method
To accurately diagnose the disease, make an appointment with the specialists of the Family Doctor network.
Rubella treatments
If symptoms appear that suggest rubella, the child should be shown to the pediatrician, and the adult should consult a general practitioner.
Symptomatic treatment
Rubella is treated with bed rest and symptomatic treatment. The patient should receive enough vitamins (in the form of vitamin preparations or in kind). nine0005
Vaccination
Vaccination is a simple and effective way to avoid the danger of getting sick already in adulthood. It is especially important to exclude the threat of rubella disease to the expectant mother. The prevention of this disease is so significant that rubella vaccination is included in the National and Regional immunization schedules.
The prevention of this disease is so significant that rubella vaccination is included in the National and Regional immunization schedules.
The vaccine is administered subcutaneously or intramuscularly. Vaccination is carried out at the age of 12 months, repeated immunization (revaccination) - at 6 years. For girls who have not had rubella and have not previously been vaccinated, the vaccine is administered at the age of 18 to 25 years. Specific immunity is provided in almost 100% of cases. It develops 15-20 days after vaccination and persists for more than 20 years. nine0005
More about the treatment
Do not self-medicate. Contact our specialists who will correctly diagnose and prescribe treatment.
Rate how useful the material was
Thank you for rating
Similar diseases
Measles
Read completely
Chicken pox
Read completely
Dermatitis nine0107
Read completely
Herpes
Read completely
Allergy
Read completely
All diseases
Rash in a child on the body, legs, back
We treat children according to the principles of evidence-based medicine: we choose only those diagnostic and treatment methods that have proven their effectiveness.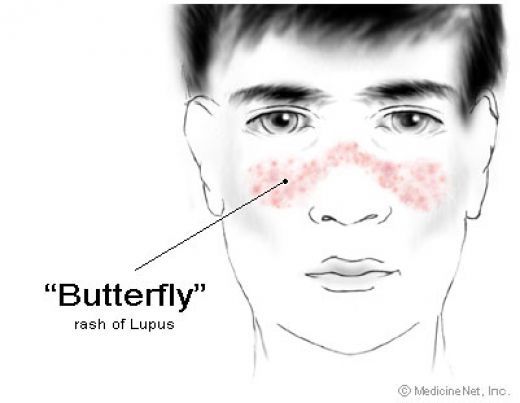 We will never prescribe unnecessary examinations and medicines! nine0005
We will never prescribe unnecessary examinations and medicines! nine0005
Make an appointment via WhatsApp
Prices Doctors
The first children's clinic of evidence-based medicine in Moscow
No unnecessary examinations and drugs! We will prescribe only what has proven effective and will help your child.
Treatment according to world standards
We treat children with the same quality as in the best medical centers in the world. nine0005
Fantasy has the best team of doctors!
Pediatricians and subspecialists Fantasy - highly experienced doctors, members of professional societies. Doctors constantly improve their qualifications, undergo internships abroad.
Ultimate safety of treatment
We have made children's medicine safe! All our staff work according to the strictest international standards JCI
We have fun, like visiting best friends
Game room, cheerful animator, gifts after the reception.