Hormone changes before labor
Hormones of pregnancy and labour
Introduction
The correct balance of hormones is essential for a successful pregnancy. Hormones act as the body’s chemical messengers sending information and feeding back responses between different tissues and organs. Hormones travel around the body, usually via the blood, and attach to proteins on the cells called receptors – much like a key fits a lock or a hand fits a glove. In response to this, the target tissue or organ functions in a way that ensures pregnancy is maintained. Initially, the ovaries, and then later, the placenta, are the main producers of pregnancy-related hormones that are essential in creating and maintaining the correct conditions required for a successful pregnancy.
The early stages of pregnancy
Following conception, a new embryo must signal its presence to the mother, allowing her body to identify the start of pregnancy. When an egg is fertilised, it travels though the female reproductive tract and implants into the womb around 9 days after it was fertilised, releasing a hormone called human chorionic gonadotrophin in the process. This hormone enters the maternal circulation and allows the mother to recognise the embryo and begin to change her body to support a pregnancy. This hormone continues to be produced in large quantities during pregnancy.
Human chorionic gonadotrophin can be detected in the urine as early as 7-9 days after fertilisation and is used as an indicator of pregnancy in most over-the-counter pregnancy tests. It is partly responsible for the frequent urination often experienced by pregnant women during the first trimester. This is because rising levels of human chorionic gonadotrophin causes more blood to flow to the pelvic area and kidneys, which causes the kidneys to eliminate waste quicker than before pregnancy. Human chorionic gonadotrophin passes through the mother’s blood to the ovaries to regulate the levels of the pro-pregnancy hormones, oestrogen and progesterone.
The role of progesterone and oestrogen during pregnancy
High levels of progesterone are required throughout pregnancy with levels steadily rising until the birth of the baby.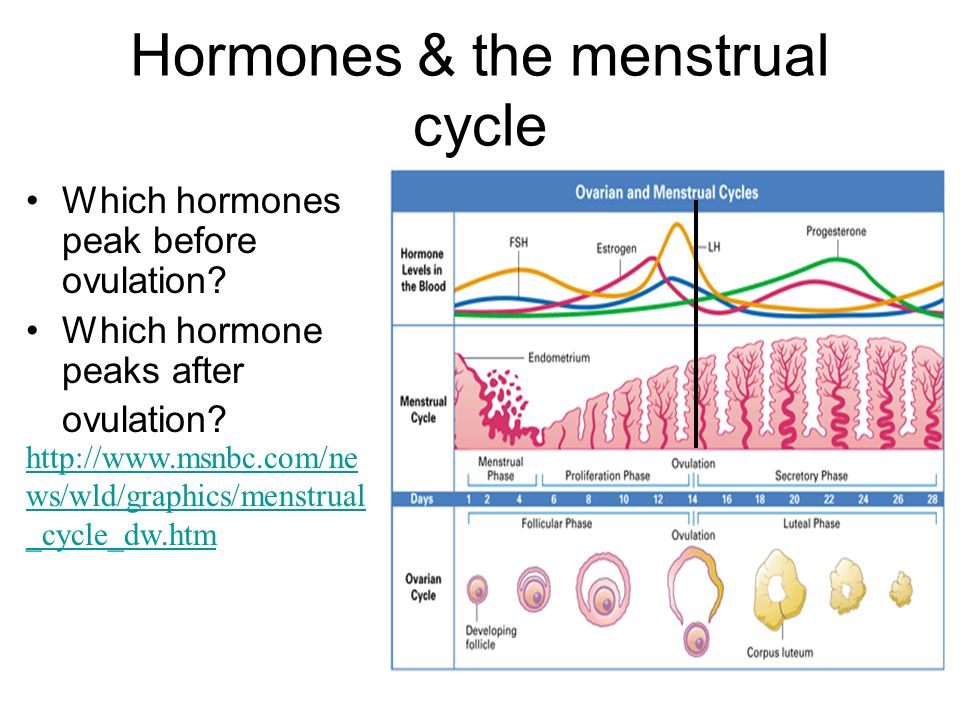 During the first few weeks of pregnancy, progesterone produced from the corpus luteum (a temporary endocrine gland of the ovaries) is sufficient to maintain pregnancy. At this early stage, progesterone has many different functions which are vital to the establishment of pregnancy, including:
During the first few weeks of pregnancy, progesterone produced from the corpus luteum (a temporary endocrine gland of the ovaries) is sufficient to maintain pregnancy. At this early stage, progesterone has many different functions which are vital to the establishment of pregnancy, including:
- Increasing blood flow to the womb by stimulating the growth of existing blood vessels.
- Stimulating glands in the lining of the womb (the endometrium) to produce nutrients that sustain the early embryo.
- Stimulating the endometrium to grow and become thickened, producing the decidua (a unique organ that supports the attachment of the placenta) and allowing implantation of the embryo.
- Helping to establish the placenta.
As the placenta forms and grows, it develops the ability to produce hormones. The cells that make up the placenta, known as trophoblasts, are able to convert cholesterol from the mother’s bloodstream into progesterone. Between weeks 6-9 of pregnancy, the placenta takes over from the ovaries as the main producer of progesterone. As well as being vital to the establishment of pregnancy, progesterone also has many functions during mid- to late pregnancy, including:
As well as being vital to the establishment of pregnancy, progesterone also has many functions during mid- to late pregnancy, including:
- Being important for correct foetal development.
- Preventing the muscles of the womb contracting until labour starts.
- Preventing lactation (breastfeeding) until after pregnancy.
- Strengthening the muscles of the pelvic wall in preparation for labour.
Although progesterone dominates throughout pregnancy, oestrogen is also very important. Many of the functions of progesterone require oestrogen and in fact, progesterone production from the placenta is stimulated by oestrogen. Initially, oestrogen is made and released by the corpus luteum of the ovaries. As the pregnancy develops, the foetal adrenal glands produce androgens that are then passed to the placenta and converted to the hormone oestriol (an oestrogen often used to determine foetal wellbeing in pregnancy) and other oestrogens. Levels of oestriol increase steadily until birth and have a wide range of effects, including:
- Maintaining, controlling and stimulating the production of other pregnancy hormones.
- Ensuring the correct development of many foetal organs including the lungs, liver and kidneys.
- Stimulating the growth and correct function of the placenta.
- Promoting growth of maternal breast tissue (along with progesterone) and preparing the mother for lactation (breastfeeding).
Other hormones produced by the placenta
The placenta also produces several other hormones including human placental lactogen and corticotrophin-releasing hormone. The function of human placental lactogen is not completely understood, although it is thought to promote the growth of the mammary glands in preparation for lactation. It is also believed to help regulate the mother’s metabolism by increasing maternal blood levels of nutrients for use by the foetus. Corticotrophin-releasing hormone is thought to regulate the duration of pregnancy and foetal maturation. For example, when pregnant women experience stress, particularly in the first trimester of pregnancy, the placenta increases the production of corticotrophin-releasing hormone.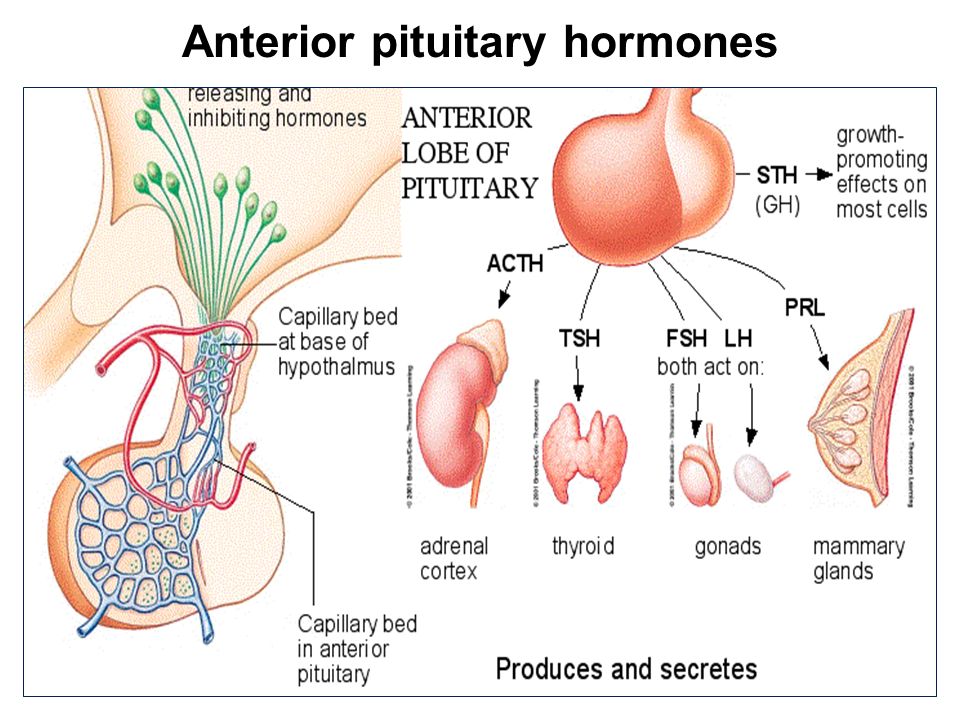 There is a good reason for this. In the first days of pregnancy, corticotrophin-releasing hormone suppresses the mother’s immune system, preventing the mother’s body from attacking the foetus. Later in pregnancy, it improves the blood flow between the placenta and foetus. In the last weeks of pregnancy corticotrophin-releasing hormone levels climb even higher – a rise which coincides with a major spike in cortisol levels. The rise in corticotrophin-releasing hormone and cortisol may help the foetal organs mature just before labour begins, and influence the timing of birth, through production of a ‘late-term cortisol surge’. This prenatal cortisol surge has also been linked to more attentive mothering in both animals and women. It is thought to be an adaptive response that induces an increased liking for their infant’s body odours, strengthening the bond between mother and baby.
There is a good reason for this. In the first days of pregnancy, corticotrophin-releasing hormone suppresses the mother’s immune system, preventing the mother’s body from attacking the foetus. Later in pregnancy, it improves the blood flow between the placenta and foetus. In the last weeks of pregnancy corticotrophin-releasing hormone levels climb even higher – a rise which coincides with a major spike in cortisol levels. The rise in corticotrophin-releasing hormone and cortisol may help the foetal organs mature just before labour begins, and influence the timing of birth, through production of a ‘late-term cortisol surge’. This prenatal cortisol surge has also been linked to more attentive mothering in both animals and women. It is thought to be an adaptive response that induces an increased liking for their infant’s body odours, strengthening the bond between mother and baby.
Side-effects of pregnancy hormones
High levels of progesterone and oestrogen are important for a healthy pregnancy but are often the cause of some common unwanted side-effects in the mother, especially as they act on the brain. Until the mother’s body has adapted to the higher levels of these hormones, mood swings can be very common. The majority of women will experience morning sickness – a feeling of nausea, any time of day, which may lead to vomiting. The exact cause of morning sickness is unknown but it is likely to be because of the rapid increase in oestrogen, progesterone and human chorionic gonadotrophin, or a decrease in thyroid stimulating hormone (which has a similar structure to human chorionic gonadotrophin). Although it is probably caused by a combination of all these hormonal changes. Morning sickness usually starts around week 5-6 of pregnancy and often subsides by week 12-16, although some women suffer throughout pregnancy and/or have very severe forms of morning sickness.
Until the mother’s body has adapted to the higher levels of these hormones, mood swings can be very common. The majority of women will experience morning sickness – a feeling of nausea, any time of day, which may lead to vomiting. The exact cause of morning sickness is unknown but it is likely to be because of the rapid increase in oestrogen, progesterone and human chorionic gonadotrophin, or a decrease in thyroid stimulating hormone (which has a similar structure to human chorionic gonadotrophin). Although it is probably caused by a combination of all these hormonal changes. Morning sickness usually starts around week 5-6 of pregnancy and often subsides by week 12-16, although some women suffer throughout pregnancy and/or have very severe forms of morning sickness.
Many women experience pain and discomfort in the pelvis and lower back during the first trimester. This is mostly due to a hormone called relaxin. Relaxin becomes detectable by week 7-10 and is produced throughout pregnancy.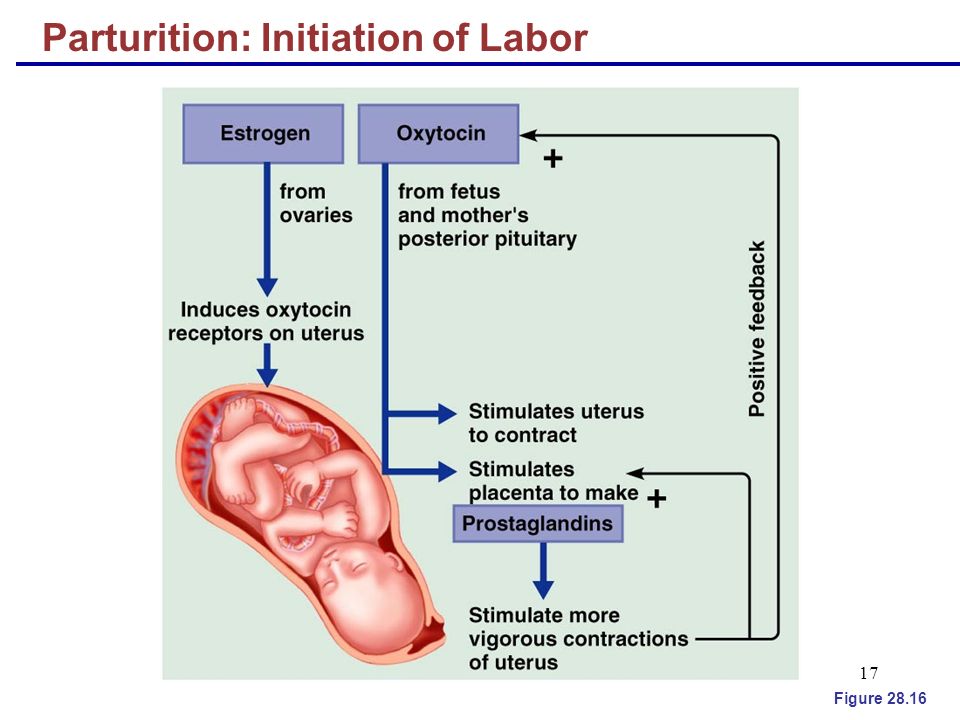 This hormone relaxes the mother’s muscles, joints and ligaments to make room for the growing baby. The effects of relaxin are mostly concentrated around the pelvic region, and softening the joints of the pelvis can often lead to pain in the area. Softer pelvic joints can also decrease stability and some women may notice it is harder to balance.
This hormone relaxes the mother’s muscles, joints and ligaments to make room for the growing baby. The effects of relaxin are mostly concentrated around the pelvic region, and softening the joints of the pelvis can often lead to pain in the area. Softer pelvic joints can also decrease stability and some women may notice it is harder to balance.
Although uncomfortable and frustrating at times, all these side-effects will usually lessen or even subside by the end of the first trimester.
Hormones and labour
The exact events leading up to the onset of labour are still not fully understood. For the baby to arrive, two things must happen: the muscles in the womb and abdominal wall have to contract and the cervix needs to soften, or ripen, allowing passage of the baby from the womb to the outside world.
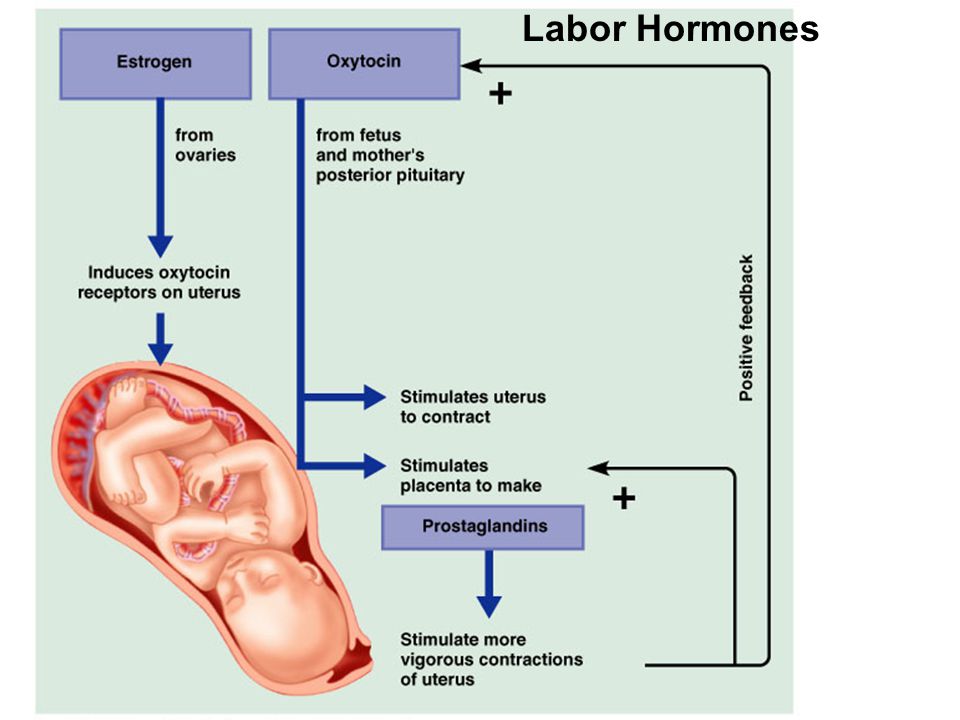
The hormone oxytocin plays a key role in labour. Often called the ‘love hormone’, oxytocin is associated with feelings of bonding and motherhood. This is also true of another hormone released during labour called prolactin. If labour needs to be induced (brought on artificially), oxytocin or a synthetic oxytocin equivalent is often administered to ‘kick-start’ the process. Oxytocin levels rise at the onset of labour, causing regular contractions of the womb and abdominal muscles.
If labour needs to be induced (brought on artificially), oxytocin or a synthetic oxytocin equivalent is often administered to ‘kick-start’ the process. Oxytocin levels rise at the onset of labour, causing regular contractions of the womb and abdominal muscles.
The cervix must dilate (open) to around 10cm for the baby to pass through. Oxytocin, along with other hormones, stimulates softening of the cervix leading to successive dilation during labour. Oxytocin, with the help of the high levels of oestrogen, causes the release of a group of hormones, known as prostaglandins, which may play a role in softening of the cervix. Levels of relaxin also increase rapidly during labour. This aids the lengthening and softening of the cervix and the softening and expansion of the mother’s lower pelvic region, thereby further aiding the baby’s arrival.
As labour contractions become more intense, natural pain relief hormones are released. Known as beta-endorphins, they are similar to drugs like morphine and act on the same receptors in the brain. As well as pain relief, they can also induce feelings of elation and happiness in the mother. As birth becomes imminent, the mother’s body releases large amounts of adrenaline and noradrenaline - so-called ‘fight or flight’ hormones. A sudden rush of these hormones just before birth causes a surge of energy in the mother and several very strong contractions, which help to deliver the baby.
As well as pain relief, they can also induce feelings of elation and happiness in the mother. As birth becomes imminent, the mother’s body releases large amounts of adrenaline and noradrenaline - so-called ‘fight or flight’ hormones. A sudden rush of these hormones just before birth causes a surge of energy in the mother and several very strong contractions, which help to deliver the baby.
Hormones after labour
When the baby is born, oxytocin continues to contract the womb in order to limit blood flow to the womb and reduce the risk of bleeding, and to help detach the placenta (which is delivered shortly afterwards). Blood levels of oxytocin and prolactin are very high, which supports bonding between the mother and baby. Skin-to-skin and eye contact between the mother and baby also stimulate the release of oxytocin and prolactin, further encouraging bonding. Many mothers describe being in a euphoric state just after labour; this is due to the effects of oxytocin, prolactin and beta-endorphins.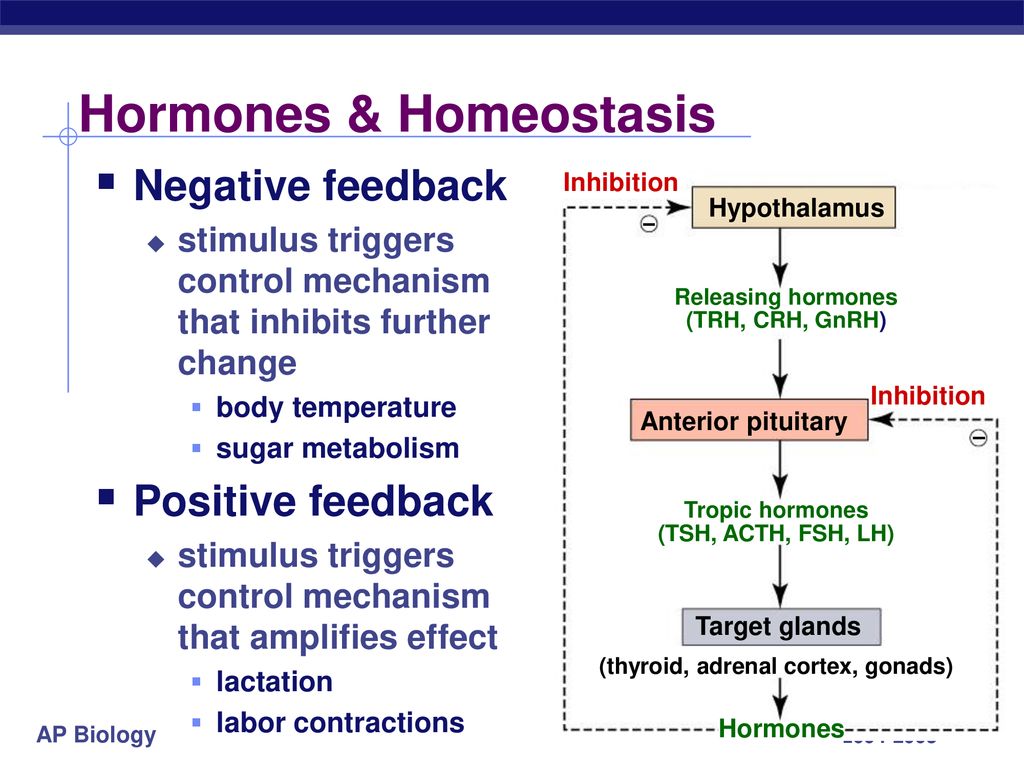
Women are actually able to breastfeed at around four months of pregnancy but high levels of progesterone and oestrogen during this time prevent milk production. After the placenta is delivered during birth, the blood levels of progesterone and oestrogen fall, allowing the mother to produce the first meal of colostrum, a high density milk that contains more protein, minerals and fat-soluble vitamins (A and K) than mature milk, which is produced later. When the baby suckles, oxytocin and prolactin are released from the pituitary gland, and pass through the mother’s blood to the breast, where prolactin stimulates milk production and oxytocin stimulates milk delivery to the nipple. As well as stimulating bonding, these hormones also aid milk release and further milk production. Mature milk that nourishes the baby and induces sleep starts to be produced about four days after birth.
Last reviewed: Mar 2021
Patient factsheet: SfE position statement on male hypogonadism and ageing
Hormones and fetal growth
Stanford researchers identify blood markers that indicate labor is approaching | News Center
About three weeks before delivery, a pregnant woman’s body shifts into a pre-labor phase characterized by changes in immune, hormonal and blood-clotting signals.
May 5, 2021 - By Erin Digitale
For the first time, researchers have found a way to predict when a pregnant woman will go into labor by analyzing immune and other biological signals in a blood sample, according to a study from the Stanford University School of Medicine.
The study, which was published online May 5 in Science Translational Medicine, sheds light on how labor begins, a biological process that until now has been a mystery. The findings lay the groundwork for a clinical blood test that could tell women with healthy, full-term pregnancies how close they are to delivery. Current estimates are imprecise, with anything in a five-week window — from three weeks before to two weeks after the due date — considered a normal delivery time.
The researchers expect their findings to yield a test within the next two to three years that doctors can use to predict labor onset in healthy pregnancies. The method narrows the predicted delivery time to a two-week window, and the researchers expect it will become even more precise as the technique is refined.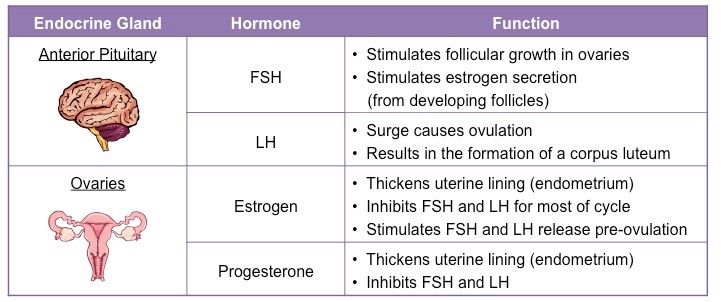
“We found a transition from ‘progressing pregnancy’ to a ‘pre-labor’ phase that happens two to four weeks before the mom goes into labor,” said Ina Stelzer, PhD, the study’s lead author and a postdoctoral scholar in anesthesiology, perioperative and pain medicine at Stanford. “We’ve identified a novel way to use the maternal blood to predict when a mother will go into labor. This prediction is independent from the duration of pregnancy.”
The shift from ongoing pregnancy to the pre-labor phase was detected both in women who had full-term pregnancies and in women who delivered prematurely. The change to pre-labor maternal biology is characterized by changes in levels of steroid hormones, factors that control blood vessel growth and blood coagulation, and immune regulatory signals, the study found.
“The mom’s body and physiology start to change about three weeks before the actual onset of labor,” said co-author Virginia Winn, MD, PhD, associate professor of obstetrics and gynecology at Stanford.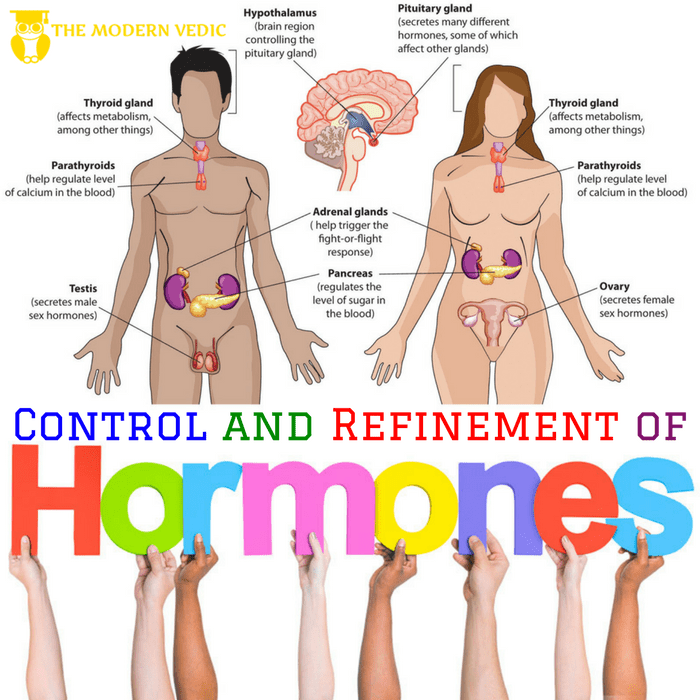 “It’s not a single switch; there’s this preparation that the body has to go through.”
“It’s not a single switch; there’s this preparation that the body has to go through.”
Getting mother and baby ready for birth
Clinicians currently estimate a woman’s due date by counting 40 weeks from the first day of her last menstrual period and taking into account ultrasound data about the baby’s size.
“Clinicians are good at estimating gestational age, which measures the development of the fetus. But there is a disconnect between this timing and when labor starts, because whether the baby is ready is only one factor in the onset of labor,” said Brice Gaudilliere, MD, PhD, the study’s senior author and associate professor of anesthesiology, perioperative and pain medicine. “The other part of the equation is the mother.”
The study is one of many findings about the biology of pregnancy to come out of Stanford’s Prematurity Research Center.
Although women deliver around 40 weeks of pregnancy on average, going into labor at anywhere from 37 to 42 weeks’ gestational age is considered normal. More precise prediction of when the baby will arrive could be helpful, for both planning and medical reasons. For instance, being able to test whether a woman with preterm contractions is in the pre-labor phase could help doctors decide whether to administer steroids, which mature the fetus’s lungs before birth.
More precise prediction of when the baby will arrive could be helpful, for both planning and medical reasons. For instance, being able to test whether a woman with preterm contractions is in the pre-labor phase could help doctors decide whether to administer steroids, which mature the fetus’s lungs before birth.
The study followed 63 women through the last 100 days of their pregnancies. They gave blood samples for analysis two to three times before delivery. All of them went into labor spontaneously, meaning none were artificially induced.
Each blood sample was analyzed for 7,142 metabolic, protein and single-cell immune features. The data was plotted against the number of days before labor that each blood sample had been taken, ensuring that the analysis would be sensitive to signals of impending labor, as opposed to signals tied primarily to pregnancy duration or the baby’s growth. The researchers identified, via mathematical modeling, which features in the blood best predicted labor onset.
Whether the baby is ready is only one factor in the onset of labor.
Fifty-eight of the women gave birth after full-term pregnancies, meaning the baby did not arrive more than three weeks before the due date, and five gave birth after spontaneous preterm labor.
As they moved into the pre-labor phase, the women’s blood showed surges in steroid hormones such as progesterone and cortisol, confirming prior findings about the biology of late pregnancy. The blood also showed decreasing levels of factors that help blood-vessel formation, likely a first step toward weakening the connection between the placenta and uterus, as well as increasing levels of factors needed for blood coagulation, which help prevent blood loss after delivery. Some placental proteins surged as well.
The study also found a fine-tuning of immune responses in the shift to labor preparation. The top predictive feature in the model was a regulatory immune protein, IL-1R4, that inhibits an inflammatory molecule called IL-33, the researchers said.
“We were really interested in and excited about the finding that IL-33 seems to play a role in pregnancy and impending labor,” Stelzer said. Near the end of pregnancy, placental material and fetal cells reach the mom’s blood, potentially causing an immune response. The body needs to carefully tailor the amount of inflammation that will occur during labor, Stelzer said.
“The hypothesis has been that labor is an inflammatory reaction, and yes, there are signs of that, but we also found that aspects of this inflammation are toned down before labor starts, which we think may prepare the mother’s immune system for the next phase, when the baby is born and healing and immune resolution begins,” Gaudilliere said. “It needs to be a regulated process.”
The next steps in the research are to validate the findings in more pregnant women and to narrow the number of biological markers needed to predict labor onset, Stelzer said, adding that the team has already made progress on the latter.
The findings could have other important clinical implications, Winn said. “If we understand what’s regulating labor, we might be able to do a better job of inducing labor,” she said.
Other Stanford co-authors of the paper are former postdoctoral scholars Mohammad Ghaemi, PhD, Kristen Rumer, MD, PhD, Natalie Stanley, PhD, Xiaoyuan Han, PhD, Benjamin Choisy, MD, and Lea Gaigne, MD; Kazuo Ando, MD, PhD, clinical assistant professor of anesthesiology, perioperative and pain medicine; research data analysts Julien Hedou and Anthony Culos; postdoctoral scholars Dorien Feyaerts, PhD, Franck Verdonk, MD, PhD, Martin Becker, PhD, and Ramin Fallahzadeh, PhD; Laura Peterson, MD, instructor in pediatrics; research scientist Edward Ganio, PhD; Dyani Gaudilliere, DMD, MPH, clinical assistant professor of plastic and reconstructive surgery; life science researchers Eileen Tsai, Amy Tsai and Danielle Jacobsen; Sonia Gavasso, PhD, former visiting professor in anesthesiology, perioperative and pain medicine; life science technicians Gavin Traber and Mathew Ellenberger; senior research scientist Ronald Wong; Gary Darmstadt, MD, professor of pediatrics; Maurice Druzin, MD, professor of obstetrics and gynecology; Ronald Gibbs, MD, clinical professor of obstetrics and gynecology; Xuefeng Ling, PhD, assistant professor of pediatric surgery; Karl Sylvester, MD, professor of surgery; Brendan Carvalho, MD, professor of anesthesiology, perioperative and pain medicine; Michael Snyder, PhD, professor of genetics; Gary Shaw, PhD, professor of pediatrics; David Stevenson, MD, professor of pediatrics and director of the Stanford Prematurity Research Center; Kevin Contrepois, PhD, scientific director in genetics; Martin Angst, MD, professor of anesthesiology, perioperative and pain medicine; and Nima Aghaeepour, PhD, assistant professor of anesthesiology, perioperative and pain medicine.
Stelzer, Feyaerts, Becker, Darmstadt, Druzin, Winn, Ling, Sylvester, Carvalho, Snyder, Shaw, Stevenson, Aghaeepour and Brice Gaudilliere are members of the Stanford Maternal and Child Health Research Institute. Darmstadt, Winn, Ling, Sylvester, Snyder, Shaw, Stevenson, Angst and Aghaeepour are members of Stanford Bio-X. Darmstadt is a faculty affiliate of the Institute for Human-Centered Artificial Intelligence. Sylvester and Snyder are members of the Stanford Cancer Institute. Winn, Snyder and Angst are members of the Stanford Cardiovascular Institute. Snyder, Angst and Brice Gaudilliere are members of the Wu Tsai Neurosciences Institute at Stanford. Stevenson is an affiliate of the Stanford Woods Institute for the Environment.
The study was supported by the Doris Duke Charitable Foundation, the Burroughs Wellcome Fund, the German Research Foundation, the Stanford Maternal and Child Health Research Institute, the Prematurity Research Fund, the March of Dimes Prematurity Research Center at Stanford University, a pilot seed grant from the Bill & Melinda Gates Foundation and Center for Human Systems Immunology, the Charles B. and Ann L. Johnson Research fund, the Christopher Hess Research Fund, the Providence Foundation Research Fund, the Roberts Foundation Research Fund, the Charles and Mary Robertson Foundation, the National Institutes of Health (grants R01AG058417, R01HL13984401, R21DE02772801, R61NS114926, R01HL13984403, 2RM1HG00773506, R35GM138353 and R35GM137936), the American Heart Association, the Stanford Maternal and Child Health Research Institute Harmon Faculty Scholar Award, the H&H Evergreen Faculty Scholar Award, and the Stanford Metabolic Health Center.
and Ann L. Johnson Research fund, the Christopher Hess Research Fund, the Providence Foundation Research Fund, the Roberts Foundation Research Fund, the Charles and Mary Robertson Foundation, the National Institutes of Health (grants R01AG058417, R01HL13984401, R21DE02772801, R61NS114926, R01HL13984403, 2RM1HG00773506, R35GM138353 and R35GM137936), the American Heart Association, the Stanford Maternal and Child Health Research Institute Harmon Faculty Scholar Award, the H&H Evergreen Faculty Scholar Award, and the Stanford Metabolic Health Center.
Media Contacts
About Stanford Medicine
Stanford Medicine is an integrated academic health system comprising the Stanford School of Medicine and adult and pediatric health care delivery systems. Together, they harness the full potential of biomedicine through collaborative research, education and clinical care for patients. For more information, please visit http://mednews.stanford.edu.
Harbingers of childbirth - How to understand that it is time to go to the hospital?
January 10, 2017
Alekseeva Inna
Obstetrician-gynecologist, Doctor of the highest category
Subscribe to our Instagram! Useful information about pregnancy and childbirth from leading obstetricians and gynecologists in Moscow and foreign experts: https://www. instagram.com/roddompravda/
instagram.com/roddompravda/
nine0009 Tips and opinions from leading children's specialists: https://www.instagram.com/emc.child/
Every pregnant woman with excitement and joy awaits the upcoming birth. The closer the cherished date, the more attentively the expectant mother listens to the changes taking place in her body and in the behavior of the baby. Of course, the expectant mother wants to know by what signs it is possible to understand that childbirth is just around the corner.
It is customary to call the harbingers of childbirth external, really tangible changes in the body, which are direct preparation for the onset of labor. The tissues of the birth canal - the cervix, vagina, vulva, perineum - become quite elastic, extensible, but at the same time - very strong and resistant to tearing. The cervix is located in the center of the vaginal vault, shortens by almost half its normal length and softens significantly. The cervical canal - the lumen of the cervix connecting the uterine cavity with the vagina - opens slightly, as a result, the diameter of the cervical canal is approximately 2-2. 5 cm. Of course, such a significant "perestroika" takes more than one day. nine0003
5 cm. Of course, such a significant "perestroika" takes more than one day. nine0003
Female sex hormones are responsible for preparing for childbirth. During the nine months of pregnancy, progesterone "reigns" in the body of the expectant mother. It ensures the normal tone of the uterus (relaxed state of the muscles), the production of cervical mucus - a mucous plug in the cervix that protects the fetus from infection. The amount of progesterone during pregnancy largely determines the normal development and growth of the fetus, the necessary concentration of nutrients and oxygen in the mother's blood, as well as their timely and uninterrupted delivery to the baby. nine0003
Shortly before childbirth, the production of progesterone decreases markedly, it is replaced by estrogens - female sex hormones. The increase in estrogen in the blood is caused by the need to prepare the body for the upcoming birth. It is these hormones that are responsible for the elasticity and patency of the birth canal. The rate of cervical dilatation in the first stage of labor depends on them. In the second period, when the cervix is fully opened and the fetus passes through the birth canal, it is also very important how elastic and extensible the walls of the vagina are - this will largely determine the duration of the straining period. Finally, the onset of labor itself depends on the level of estrogen: contractions occur as a result of a nerve impulse that is caused by a certain level (“peak”) of estrogen accumulation. nine0003
The rate of cervical dilatation in the first stage of labor depends on them. In the second period, when the cervix is fully opened and the fetus passes through the birth canal, it is also very important how elastic and extensible the walls of the vagina are - this will largely determine the duration of the straining period. Finally, the onset of labor itself depends on the level of estrogen: contractions occur as a result of a nerve impulse that is caused by a certain level (“peak”) of estrogen accumulation. nine0003
These changes are normal and do not require an unscheduled visit to the doctor or hospitalization. Harbingers of childbirth are manifestations of a planned restructuring in the body of a future mother, the “finishing touches” of preparation for the upcoming joyful event.
The absence of clearly perceptible changes on the eve of the expected date of birth is also not a pathology. Not all expectant mothers note those changes in well-being that are commonly called harbingers.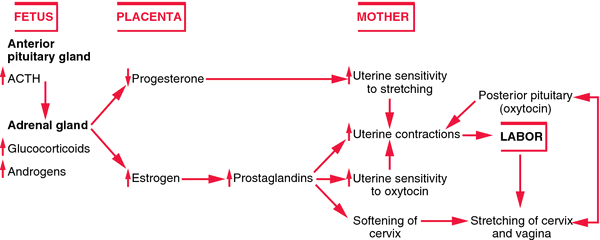 However, this does not mean that there is no preparation. In some cases, the “final preparations” go unnoticed by the pregnant woman. Therefore, do not worry or urgently contact a specialist. nine0003
However, this does not mean that there is no preparation. In some cases, the “final preparations” go unnoticed by the pregnant woman. Therefore, do not worry or urgently contact a specialist. nine0003
The appearance of any of the "harbingers" indicates the likelihood of the development of regular labor activity over the next two hours - two weeks. None of the sensations described gives a 100% guarantee that a woman will become a mother within the next 24 hours. Hormonal changes before childbirth begin approximately two weeks before the expected birth. Theoretically, during these two weeks, at any time, a pregnant woman can notice certain changes in her state of health. Consequently, the absence of labor activity an hour, a day, or even a week after the first noted changes is not a pathology and does not require special medical advice. nine0003
- Scarlet discharge from the genital tract in any amount.
- Severe abdominal pain.
- Increased blood pressure (above 130/80 mmHg).

- An increase in body temperature to 37.5 ° C and above.
- Increased heart rate (more than 100 beats per minute).
- Severe headache, vomiting, blurred vision.
- Significant increase in edema. nine0035 Absence, sharp decrease, sharp increase in fetal movements.
- Suspicion of amniotic fluid leakage.
Weight loss . Shortly before the expected date of delivery, the expectant mother may notice some “weight loss”. Weight loss during this period is associated with the removal of excess fluid from the body, that is, a general decrease in edema. The more pronounced the fluid retention during pregnancy, the more mass the pregnant woman will “lose” on the eve of childbirth. During pregnancy, water is retained in the body of all expectant mothers to a greater or lesser extent. The reason is progesterone - a hormone whose main function is to support the processes of pregnancy. Before childbirth, progesterone is replaced by estrogen. It is estrogen that removes excess fluid from the body. The first results are visible on the hands, feet and legs. Depending on the severity of edema, weight loss before childbirth varies from 0.5 to 2.5 kg. nine0003
Before childbirth, progesterone is replaced by estrogen. It is estrogen that removes excess fluid from the body. The first results are visible on the hands, feet and legs. Depending on the severity of edema, weight loss before childbirth varies from 0.5 to 2.5 kg. nine0003
Change of stool. Increased frequency and change in the consistency of physiological functions on the eve of childbirth is also associated with an increase in estrogen levels and the removal of fluid from the body of the future mother. Similar changes in the body of a non-pregnant woman are observed during menstruation. The chair can become more frequent up to 2-3 times a day, at the same time there may be some liquefaction of the feces. More frequent urge to defecate, a sharp change in the color and smell of feces, combined with nausea and vomiting, is a reason for consulting a doctor - food poisoning can be masked under such "harbingers". nine0003
Fundal prolapse.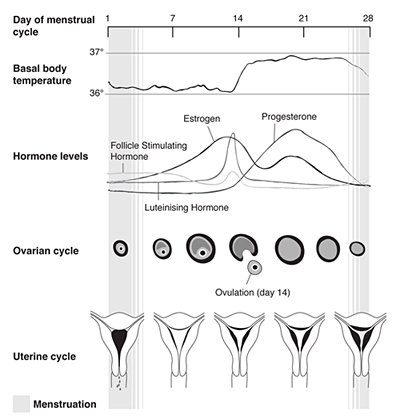 Shortly before delivery, the baby presses the presenting part (most often the head) against the lower segment of the uterus and pulls it down, pressing against the entrance to the small pelvis. The fetus "groups", taking the most advantageous position for itself at the time of the onset of contractions. As a result of such "preparations" from the side of the fetus, the uterus "sags", and its upper part - the bottom - ceases to exert pressure on the internal organs. After lowering the bottom of the uterus, the pregnant woman has no shortness of breath (it becomes easier to breathe, there is a feeling of a full breath). If in the last month the expectant mother had belching, heartburn, a feeling of heaviness in the stomach after eating, these phenomena disappear when the bottom of the uterus descends. However, lowering down to the pelvic area, the uterus will put more pressure on the internal organs located there. The pelvic organs, in particular, include the bladder. It is located directly in front of the uterus, in its lower part.
Shortly before delivery, the baby presses the presenting part (most often the head) against the lower segment of the uterus and pulls it down, pressing against the entrance to the small pelvis. The fetus "groups", taking the most advantageous position for itself at the time of the onset of contractions. As a result of such "preparations" from the side of the fetus, the uterus "sags", and its upper part - the bottom - ceases to exert pressure on the internal organs. After lowering the bottom of the uterus, the pregnant woman has no shortness of breath (it becomes easier to breathe, there is a feeling of a full breath). If in the last month the expectant mother had belching, heartburn, a feeling of heaviness in the stomach after eating, these phenomena disappear when the bottom of the uterus descends. However, lowering down to the pelvic area, the uterus will put more pressure on the internal organs located there. The pelvic organs, in particular, include the bladder. It is located directly in front of the uterus, in its lower part.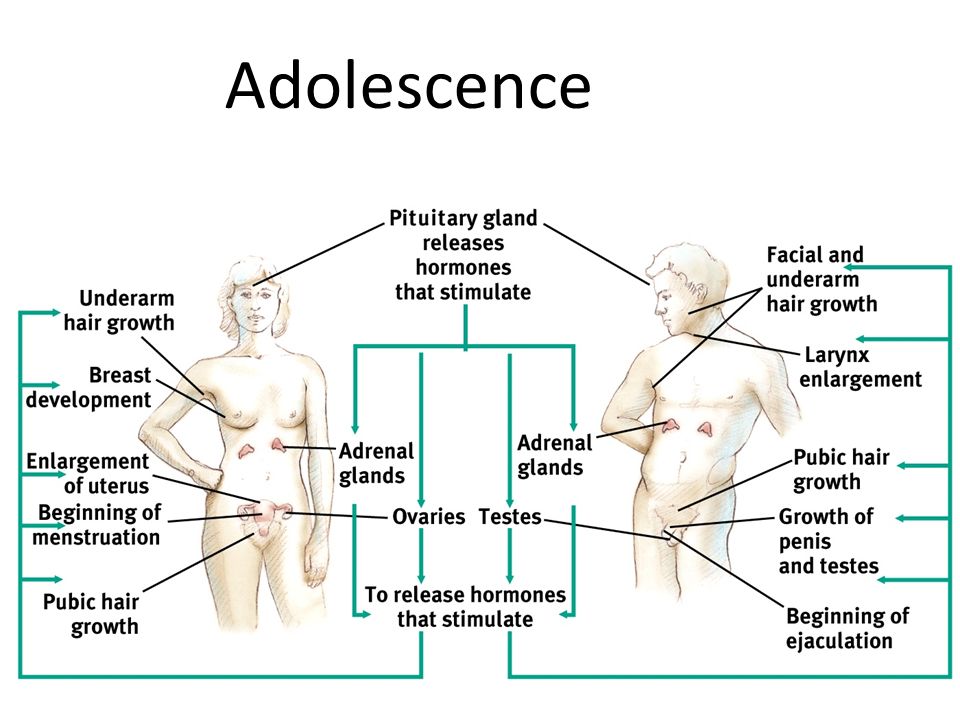 Behind the uterus, at a distance of several centimeters, there is an ampulla of the rectum - the output section of the intestine. It is not difficult to guess what the result of pressure on the bladder and rectum will be: the urge to go to the toilet before childbirth can become noticeably more frequent. nine0003
Behind the uterus, at a distance of several centimeters, there is an ampulla of the rectum - the output section of the intestine. It is not difficult to guess what the result of pressure on the bladder and rectum will be: the urge to go to the toilet before childbirth can become noticeably more frequent. nine0003
Isolation of the mucous plug. During pregnancy, the glands of the mucous membrane of the cervical canal (the lumen of the cervix) secrete a special secret. It is a thick, sticky, jelly-like mass that forms a kind of cork. The mucous plug completely fills the cervical canal, preventing the penetration of bacterial flora from the vagina into the uterine cavity. Thus, cervical mucus, or the mucous plug of the cervix, protects the fetus from ascending infection. Before childbirth, when the cervix begins to soften under the influence of estrogen, the cervical canal opens slightly and the cervical mucus contained in it can be released. In this case, the expectant mother may find small clots of yellowish-brownish mucus, transparent, jelly-like, odorless. The mucous plug can stand out at once or depart in parts during the day. In the latter case, slight discomfort is sometimes noted in the form of "sipping" in the lower abdomen, reminiscent of sensations before or during menstruation. However, most often, the release of the mucous plug is not accompanied by tangible changes in the well-being of the expectant mother. After the discharge of the mucous plug, it is not recommended to visit the pool, swim in the reservoirs and in the bath. When immersed in water, it fills the vagina; thus, in the absence of a mucous plug, the risk of infection of the fetus and membranes through the ajar cervix increases. nine0003
The mucous plug can stand out at once or depart in parts during the day. In the latter case, slight discomfort is sometimes noted in the form of "sipping" in the lower abdomen, reminiscent of sensations before or during menstruation. However, most often, the release of the mucous plug is not accompanied by tangible changes in the well-being of the expectant mother. After the discharge of the mucous plug, it is not recommended to visit the pool, swim in the reservoirs and in the bath. When immersed in water, it fills the vagina; thus, in the absence of a mucous plug, the risk of infection of the fetus and membranes through the ajar cervix increases. nine0003
Training contractions. Training or false contractions are called such contractions that appear shortly before childbirth and are not actually labor activity, since they do not lead to the opening of the cervix. A contraction is essentially a single contraction of the uterine wall; this contraction usually lasts a few seconds.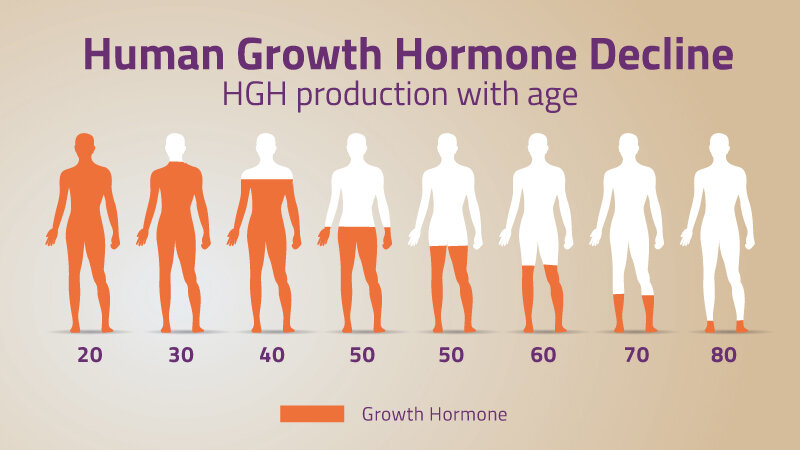 At the time of the contraction, the expectant mother feels a gradually increasing and then gradually decreasing tension in the abdomen. If at this moment you put your hand on your stomach, you can notice that the stomach becomes very hard, but after the contraction it completely relaxes and becomes soft again. In addition to involuntary tension of the uterus, other changes in the well-being of the expectant mother during false contractions are usually not noted. It is not difficult to distinguish training fights from real ones. In most cases, false contractions are weak, painless, irregular or alternating at a significant interval (30 minutes or more). Labor pains, on the contrary, are distinguished by regularity and a gradual increase in intensity. Unlike false contractions, real contractions lead to a visible result - the opening of the cervix. In doubtful cases, a simple obstetric examination will be enough to make an accurate diagnosis. In other cases, training contractions, like all harbingers of childbirth, do not require a visit to a doctor or hospitalization.
At the time of the contraction, the expectant mother feels a gradually increasing and then gradually decreasing tension in the abdomen. If at this moment you put your hand on your stomach, you can notice that the stomach becomes very hard, but after the contraction it completely relaxes and becomes soft again. In addition to involuntary tension of the uterus, other changes in the well-being of the expectant mother during false contractions are usually not noted. It is not difficult to distinguish training fights from real ones. In most cases, false contractions are weak, painless, irregular or alternating at a significant interval (30 minutes or more). Labor pains, on the contrary, are distinguished by regularity and a gradual increase in intensity. Unlike false contractions, real contractions lead to a visible result - the opening of the cervix. In doubtful cases, a simple obstetric examination will be enough to make an accurate diagnosis. In other cases, training contractions, like all harbingers of childbirth, do not require a visit to a doctor or hospitalization. False contractions may recur for several hours and then stop. Most often, they disturb a pregnant woman in the evening and morning hours for several days. nine0003
False contractions may recur for several hours and then stop. Most often, they disturb a pregnant woman in the evening and morning hours for several days. nine0003
Discomfort. In the last weeks before giving birth, many pregnant women report discomfort in the lower abdomen and in the area of the sacrum (the area slightly below the waist). Such changes in
the well-being of the expectant mother is caused by sprain of the pelvic ligaments and increased blood flow to the pelvic organs. Usually these minor sensations, described as a feeling of "light languor" in the lower abdomen, are comparable to similar phenomena in the period before or during menstruation. Discomfort, like training contractions, more often disturbs the expectant mother in the morning and evening hours. The level of discomfort is minimal, it should not worry the expectant mother and does not require medical intervention. nine0003
All harbingers of childbirth can appear during the last two weeks before childbirth, their presence, as well as their absence, is the norm and does not require a visit to a doctor.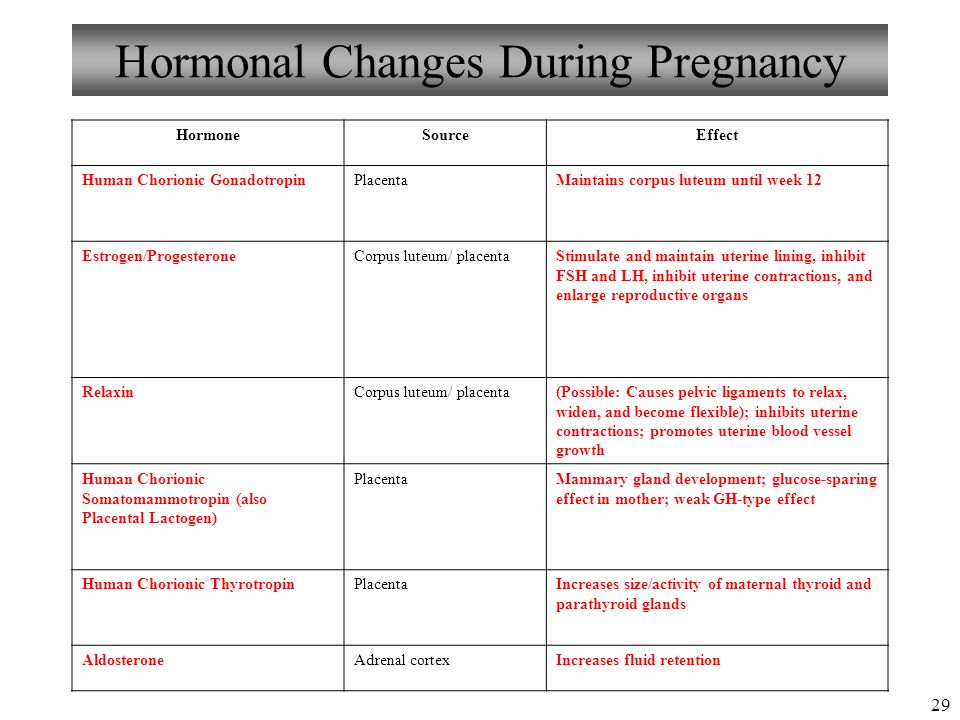 It is important to learn to listen to changes in your body, not to be afraid of changes in well-being associated with prenatal preparation, and most importantly, to have time to mentally and physically prepare for the most important event - the birth of a baby.
It is important to learn to listen to changes in your body, not to be afraid of changes in well-being associated with prenatal preparation, and most importantly, to have time to mentally and physically prepare for the most important event - the birth of a baby.
Subscribe to our Instagram. You will find useful information about pregnancy and childbirth from leading EMC obstetricians and gynecologists. nine0003
10 little helpers: what hormones are involved in childbirth - Parents.ru
Pregnancy
- Photo
- becon/Getty Images/E+
obstetrician-gynecologist
obstetrician-gynecologist doctor
put forward many theories and mechanisms of childbirth. The most interesting one is from the Dutch neuroscientist Dick Swaab. In his opinion, the signal for the onset of labor is given by a decrease in the level of glucose in the blood of the unborn baby.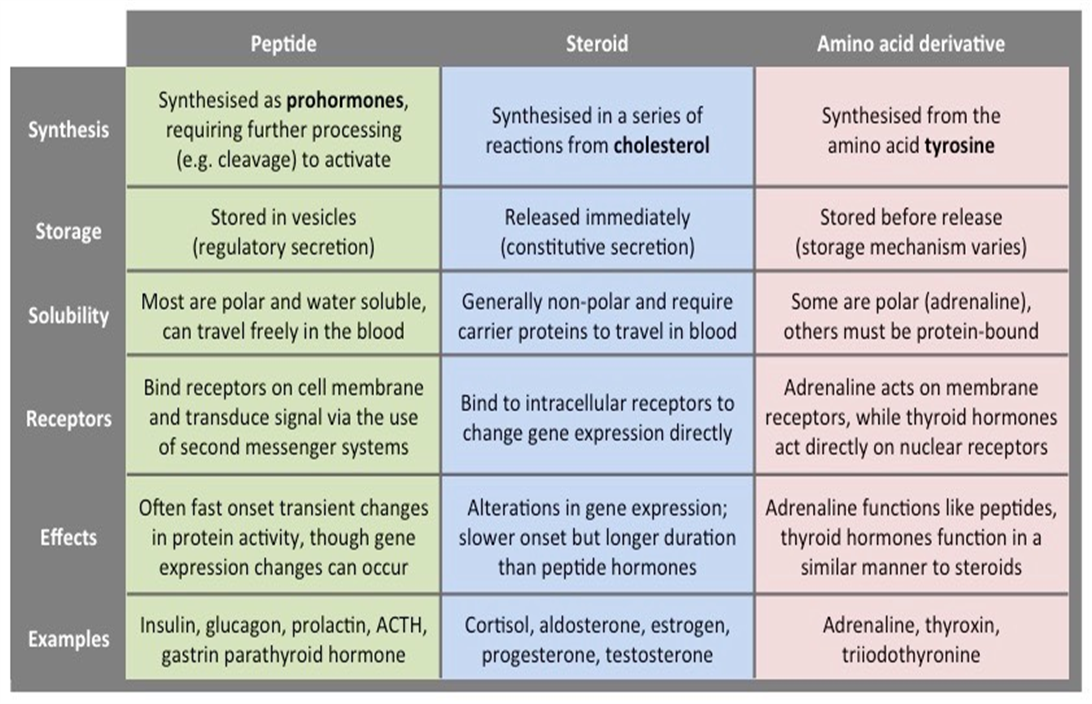 As the mother's body is no longer able to provide adequate nutrition to the growing baby, a series of hormonal changes occur that cause uterine contractions. But recently, another hypothesis has been gaining more and more supporters. The main reason for timely delivery, she calls the genetic program, which provides for the completion of pregnancy as soon as the unborn baby is ready for autonomous existence. In any case, mother and baby cannot do without helpers. They become hormones. nine0003
As the mother's body is no longer able to provide adequate nutrition to the growing baby, a series of hormonal changes occur that cause uterine contractions. But recently, another hypothesis has been gaining more and more supporters. The main reason for timely delivery, she calls the genetic program, which provides for the completion of pregnancy as soon as the unborn baby is ready for autonomous existence. In any case, mother and baby cannot do without helpers. They become hormones. nine0003
First Aid
Childbirth begins with "forerunners". At this point, the level of progesterone in the woman's body begins to decrease. This hormone is produced by the placenta. He is the "guardian" of pregnancy, suppressing the contractility of the uterus and maintaining the tone of the cervix. As the level of progesterone decreases, the uterus, which for the time being was relaxed, becomes sensitive and tense. Mom feels the movements of the baby more and more sharply, at times tension arises in the lower abdomen, slight contractions of the uterus are felt.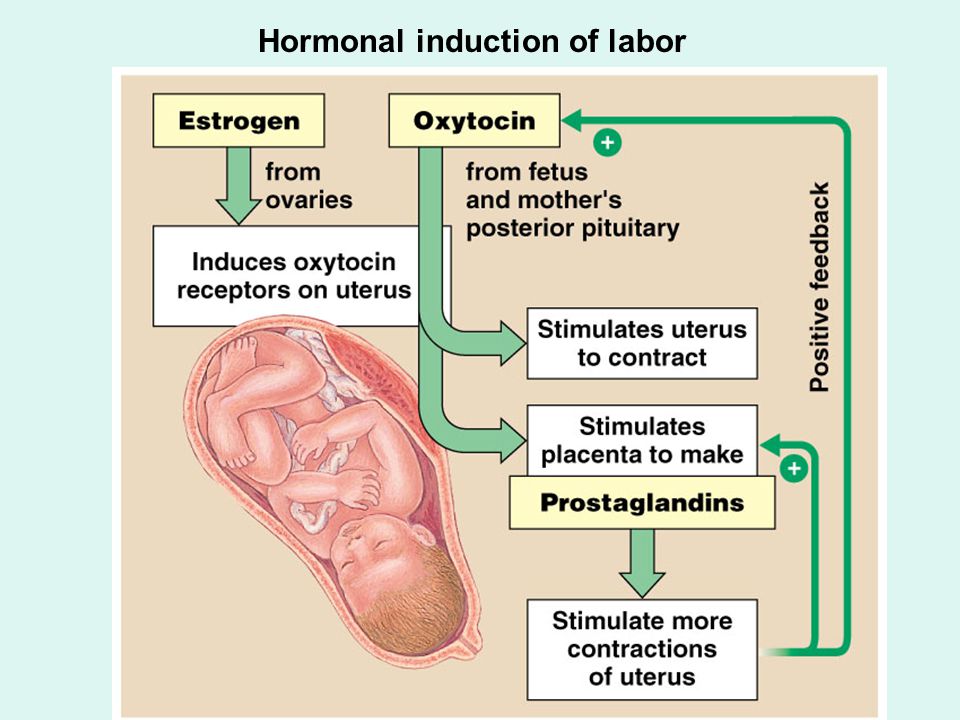 nine0003
nine0003
At the same time, the level of estrogen in a woman increases - this is how the female sex hormones estradiol, estrone and estriol are generally called. They contribute to the maturation of the cervix. Under their influence, it softens, shortens and begins to gradually open up. Thanks to estrogen, the tone of the uterus also increases and the preparation of the soft birth canal begins for the birth of the baby. In addition, female sex hormones inhibit the activity of specific enzymes that destroy oxytocin. He is called the "king of childbirth". And not in vain. This hormone is the strongest stimulator of uterine contractions. At the same time, prostaglandins are formed in the tissues of the placenta, the walls of blood vessels, ovaries, intestines, lungs, in the fallopian tubes, in the wall of the stomach and even in the muscle of the heart, but most of them are produced in the tissues of the uterus. Interestingly, these biologically active substances, close to hormones, were first discovered in the male gonads (“prostaglandins” - a derivative of the word “prostate”). They also cause uterine contractions, soften the cervix and start labor. nine0003
They also cause uterine contractions, soften the cervix and start labor. nine0003
Serotonin is also involved in the regulation of labor activity. It acts directly on the receptors located in the myometrium (one of the layers of the uterus), activating them, plus through the central nervous system increases the production of oxytocin. The concentration of serotonin in the blood, uterus and placenta increases with increasing gestational age and reaches a maximum by the time of delivery.
- Photo
- Getty Images/Brand X
Developments
So, prostaglandins “trigger” the mechanism of contractions, and oxytocin helps to keep them normal. Its powerful release into the blood occurs at the very beginning of childbirth, then another one, after which the cervix begins to open faster. As soon as it opens completely, the third surge of this hormone will make the woman push, "pushing" the child to the "exit". And, finally, “at the end” of the process, oxytocin is needed so that the contractions do not fade away and the separated placenta, along with the fetal membranes, leaves the body of a young mother. nine0003
And, finally, “at the end” of the process, oxytocin is needed so that the contractions do not fade away and the separated placenta, along with the fetal membranes, leaves the body of a young mother. nine0003
Natural pain relief
But this is not all the hormones and biologically active substances that help a woman cope with a difficult task and give birth to a baby. In the reserves of our body there is a whole arsenal of tools that reduce pain and tension. We are talking about the so-called pleasure hormones - endorphins. The adrenal hormones cortisol and catecholamines, the production of which is stimulated by adrenocorticotropic hormone, also help to cope with the difficulties of childbirth. Together with endorphins, they “balance” the stress hormones adrenaline and norepinephrine. The last substances during childbirth also do not remain behind the scenes. Before the start of the attempts, when the woman has already spent a lot of energy to survive the contractions, and is rather tired, thanks to a sharp release of adrenaline, she has a “second wind” and the strength to push.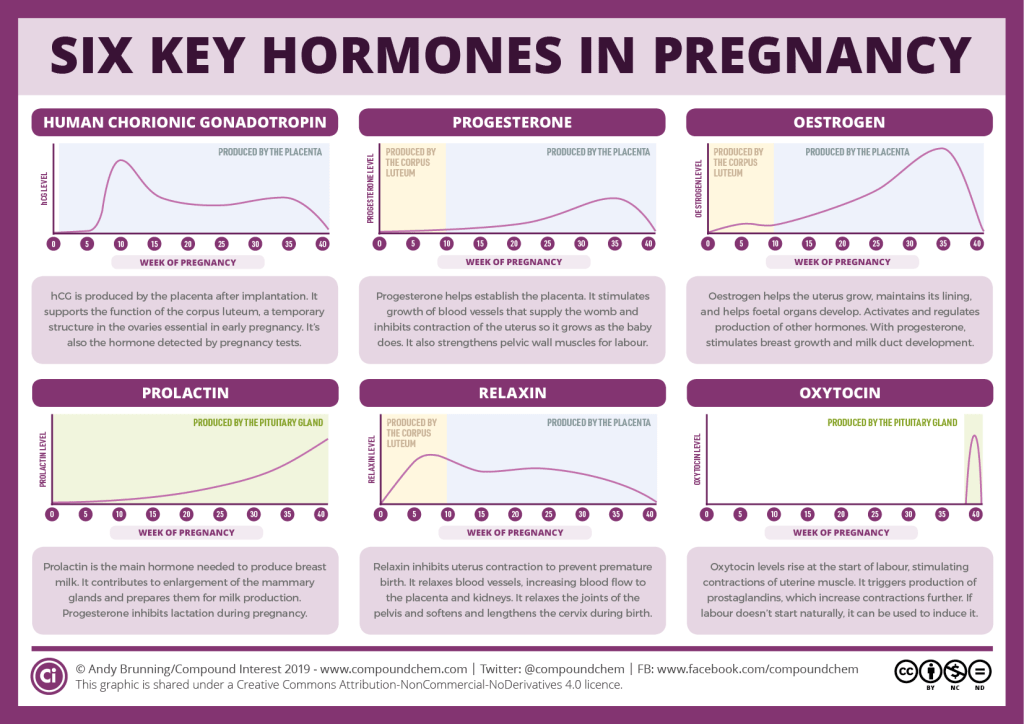 nine0003
nine0003
It is believed that the signal for the onset of labor is given by the unborn baby. In his blood, the level of corticosteroids increases, which, in turn, stimulate the production of estrogens and prostaglandins.
- Photo
- mustafagull/Getty Images/E+
Difficulties are overcome
Childbirth will take place as prescribed by nature, only when each of the hormones starts working at the right time and its concentration is sufficient. Even the smallest failure in this system can disrupt the normal course of events. For example, due to a lack of estrogen, the process of preparing for childbirth and maturation of the cervix may be delayed. In this case, doctors talk about a "post-term" pregnancy, and childbirth begins after 41 weeks. nine0003
With a deficiency of prostaglandins, difficulties begin with the maturation of the cervix. If for some reason this has not yet happened by the time of birth, synthetic analogues of these biologically active substances are used. In Russia, a vaginal gel is registered, which is allowed to be used in such cases. Also, with a deficiency of prostaglandins, the preparatory stage of childbirth is lengthened. It usually lasts up to 6 hours. During this period, a woman feels light, almost imperceptible irregular contractions. But if her body produces few necessary hormones, the process is delayed, the woman in labor gets very tired. nine0003
If for some reason this has not yet happened by the time of birth, synthetic analogues of these biologically active substances are used. In Russia, a vaginal gel is registered, which is allowed to be used in such cases. Also, with a deficiency of prostaglandins, the preparatory stage of childbirth is lengthened. It usually lasts up to 6 hours. During this period, a woman feels light, almost imperceptible irregular contractions. But if her body produces few necessary hormones, the process is delayed, the woman in labor gets very tired. nine0003
Deficiency of oxytocin complicates not only the preparatory period, but also the very process of the birth of a child. With this turn of events, the muscles contract weakly, the cervix opens slowly. Because of this, the child moves through the birth canal for a very long time. Doctors talk about the weakness of labor and can introduce a synthetic analogue of oxytocin into the woman's body. You should not be afraid of such manipulations: everything is done only with the written consent of the future mother, and the goal is the same - to help the baby be born healthy.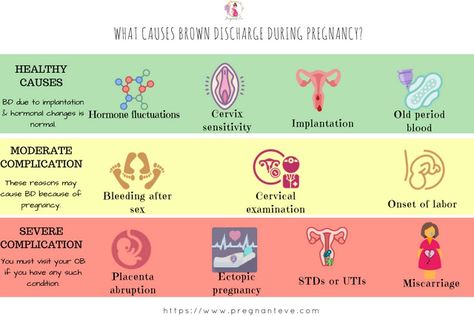 Moreover, in this way, the most formidable complication is prevented, which is very rare, but can occur at the last stage of childbirth - hypotonic bleeding. nine0003
Moreover, in this way, the most formidable complication is prevented, which is very rare, but can occur at the last stage of childbirth - hypotonic bleeding. nine0003
There is also a situation when oxytocin is produced in excess. Childbirth then takes place too rapidly, the baby moves very quickly towards the “exit”. As a result, he, having no time to prepare, can get injured, and his mother can get soft tissue ruptures.
Take a look at your plate
Hormone levels are adjusted during childbirth with the help of drips or injections. It is possible to speak about the prevention of such troubles with a certain degree of conventionality, because often the problem does not manifest itself until X hour. But if you eat right, the chances that pregnancy and childbirth will pass without complications increase dramatically. After all, the prostaglandins needed during childbirth are synthesized in the body from polyunsaturated fatty acids (PUFAs). Their sources are vegetable oils: linseed, olive, almond.