Test milk allergy
Milk allergy - Diagnosis and treatment
Diagnosis
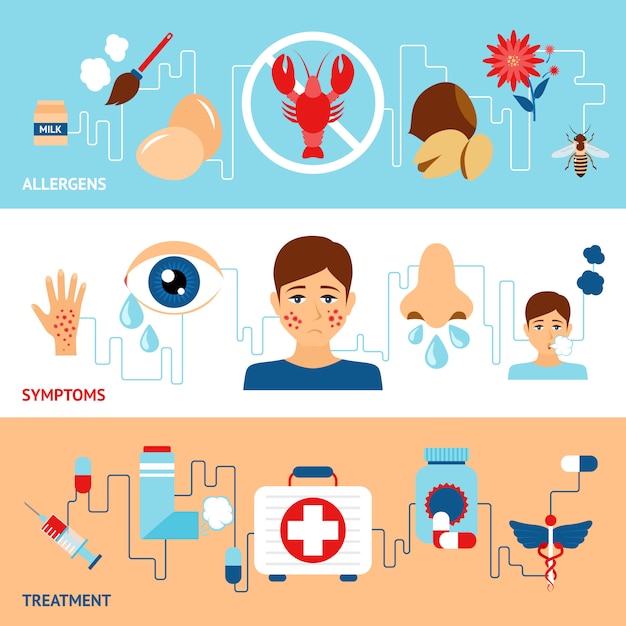
When food causes an allergic reaction, it isn't always easy to find out what food is to blame. To evaluate whether you or your child has milk allergy, your health care provider may:
- Ask detailed questions about signs and symptoms
- Perform a physical exam
- Have you keep a detailed diary of the foods you or your child eats
- Have you eliminate milk from your diet or your child's diet (elimination diet) — and then have you add back the food to see if it causes a reaction
He or she may also recommend one or both of the following tests:
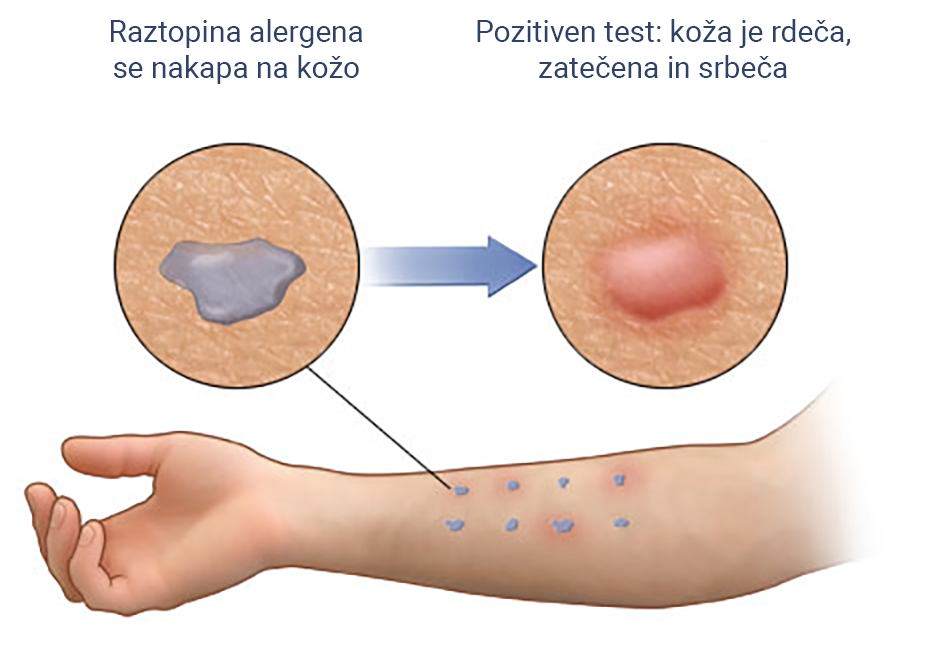
- Skin test. In this test, your skin is pricked and exposed to small amounts of the proteins found in milk. If you're allergic, you'll likely develop a raised bump (hive) at the test location on your skin. Allergy specialists usually are best equipped to perform and interpret allergy skin tests. Keep in mind that this type of test isn't completely accurate for detecting milk allergy.
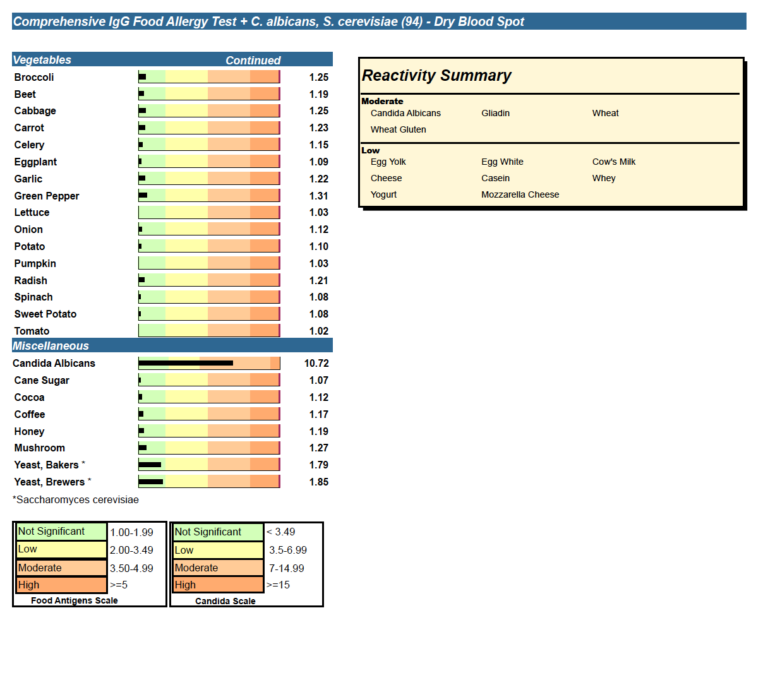
- Blood test. A blood test can measure your immune system's response to milk by measuring the amount of immunoglobulin E (IgE) antibodies in your blood. But this test isn't completely accurate in identifying milk allergy.
If your examination and test results can't confirm milk allergy, your health care provider might administer an oral challenge, in which you are fed different foods that may or may not contain milk in increasing amounts to see if you react to the ones that contain milk. It's a good idea to have allergy tests administered by an allergist who's been trained to manage serious reactions.
If your provider suspects that your symptoms are caused by something other than a food allergy, you may need other tests to identify — or rule out — other medical problems.
More Information
- Allergy skin tests
Treatment
The only way to prevent an allergic reaction is to avoid milk and milk proteins. This can be difficult because milk is a common ingredient in many foods. Also, some people with milk allergy can tolerate milk in some forms, such as milk that's heated in baked goods, or in some processed foods, such as yogurt. Talk to your health care provider about what to avoid.
Also, some people with milk allergy can tolerate milk in some forms, such as milk that's heated in baked goods, or in some processed foods, such as yogurt. Talk to your health care provider about what to avoid.
If you or your child has a serious allergic reaction (anaphylaxis), you may need an emergency injection of epinephrine (adrenaline) and a trip to the emergency room. If you're at risk of having a severe reaction, you or your child may need to carry injectable epinephrine (EpiPen, Adrenaclick, others) at all times. Have your provider or pharmacist demonstrate how to use this device so that you're prepared for an emergency.
Request an Appointment at Mayo Clinic
Clinical trials
Explore Mayo Clinic studies testing new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.
Coping and support
Having a serious allergy or being the parent of a child with a potentially life-threatening allergy can be stressful. Talking to others in similar situations can be helpful. Besides offering support and encouragement, they may also provide useful coping tips, such as how to deal effectively with school officials to ensure your child's medical needs are met. Ask your health care provider if there are any support groups in your area, or contact the Asthma and Allergy Foundation of America.
Talking to others in similar situations can be helpful. Besides offering support and encouragement, they may also provide useful coping tips, such as how to deal effectively with school officials to ensure your child's medical needs are met. Ask your health care provider if there are any support groups in your area, or contact the Asthma and Allergy Foundation of America.
Preparing for your appointment
You're likely to start by seeing your family health care provider or your child's pediatrician. However, you may then be referred to a doctor who specializes in allergic disorders (allergist-immunologist).
Here's some information to help you get ready for your appointment and to know what to expect.
What you can do
- Be aware of any pre-appointment restrictions. When you make the appointment, ask if there's anything you need to do in advance. For example, if you're going to have allergy testing done, your provider will want you or your child to stop taking antihistamine medications for a certain time period before the test.
- Write down any symptoms you or your child has experienced, including any that may seem unrelated to milk allergy.
- Make a list of any medications, vitamins and supplements you or your child is taking.
- Write down questions to ask your provider.
Preparing a list of questions can help you make the most of your time with your provider. For milk allergy, some basic questions to ask include:
- Do you think this is milk allergy or lactose intolerance?
- Are there tests to diagnose milk allergy? Do these tests require preparation?
- Is it possible to outgrow this allergy?
- Are there treatments?
- Is it necessary to avoid milk and milk products?
- What foods are likely to contain milk products?
- Is it necessary to stay away from others who are drinking milk?
- What do I need to tell people at my child's school about this allergy?
- How can milk allergy best be managed with other conditions?
- Are there brochures or other printed materials that I can take? What websites do you recommend?
- Do I need to carry injectable epinephrine at all times?
Don't hesitate to ask any other questions you may have.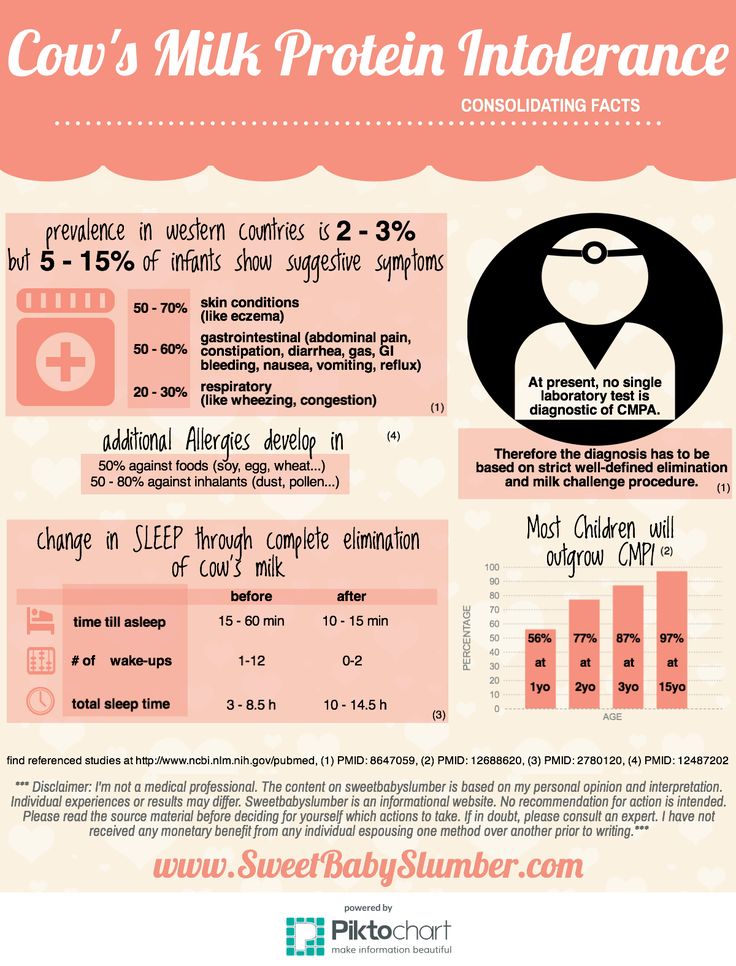
What to expect from your doctor
Your provider is likely to ask you a number of questions, including:
- When did you or your child first react to milk?
- Can you describe the reaction?
- Does this happen every time you or your child drinks milk or eats something made with milk?
- How soon after consuming milk or milk products do symptoms begin?
- How severe are the symptoms?
- Does anything seem to improve the symptoms, such as allergy medication or milk avoidance?
- What, if anything, appears to worsen the symptoms?
- Have you or your child tried any of the products made for people with lactose intolerance? If yes, did those help?
- Is anyone else in your family allergic to milk?
What you can do in the meantime
If you're having mild allergy symptoms from eating something that contained milk, taking an antihistamine medication may lessen your discomfort. Watch for more-severe symptoms that might require medical attention. If you or your child has symptoms of anaphylaxis, seek emergency medical care.
If you or your child has symptoms of anaphylaxis, seek emergency medical care.
By Mayo Clinic Staff
Related
Associated Procedures
Products & Services
Milk Allergy | Causes, Symptoms & Treatment
Symptoms
Milk is one of the most common food allergens. People with an allergy to cow’s milk may also be allergic to milk from other animals, including sheep and goats.
Within a short period of time after consuming milk or a milk protein, you may experience the following symptoms:
- Hives
- Stomach upset
- Vomiting
- Bloody stools, especially in infants
- Anaphylaxis, a rare, potentially life-threatening reaction that impairs breathing and can send the body into shock
Take back control of your life. If you or your child experiences any of these symptoms, see an allergist to find a solution.
Diagnosis
At your appointment, your allergist will take a detailed history, including asking what you ate, what symptoms you experienced, how long the symptoms lasted and what you did to alleviate them.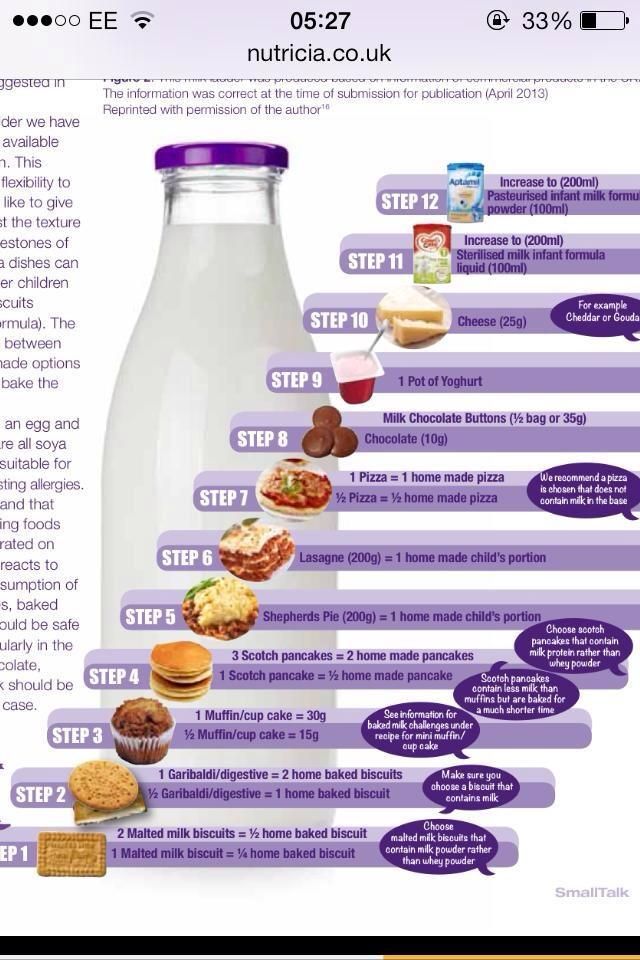 The most common allergy tests are a skin-prick test or a blood test; both look for the presence of immunoglobulin E (IgE) antibodies, which develop when your body is exposed to a substance to which it is sensitive. These antibodies trigger the release of chemicals that cause allergic symptoms.
The most common allergy tests are a skin-prick test or a blood test; both look for the presence of immunoglobulin E (IgE) antibodies, which develop when your body is exposed to a substance to which it is sensitive. These antibodies trigger the release of chemicals that cause allergic symptoms.
In the skin-prick test, a liquid containing milk or a milk protein extract is placed on your forearm or back. Your skin is pricked with a small, sterile probe, allowing the liquid to seep into your skin. If you develop a raised, reddish welt, typically within 15 to 20 minutes, that can indicate an allergy. In a blood test, a blood sample is tested for the presence of IgE antibodies. The results are reported as a numerical value.
Research suggests that some types of milk proteins (casein and two proteins found in whey, alpha-lactalbumin and beta-lactalbumin) are more likely to cause serious reactions. A newer type of blood test, known as a component test, can help the allergist determine your risk for a serious reaction by looking for allergies to those specific proteins.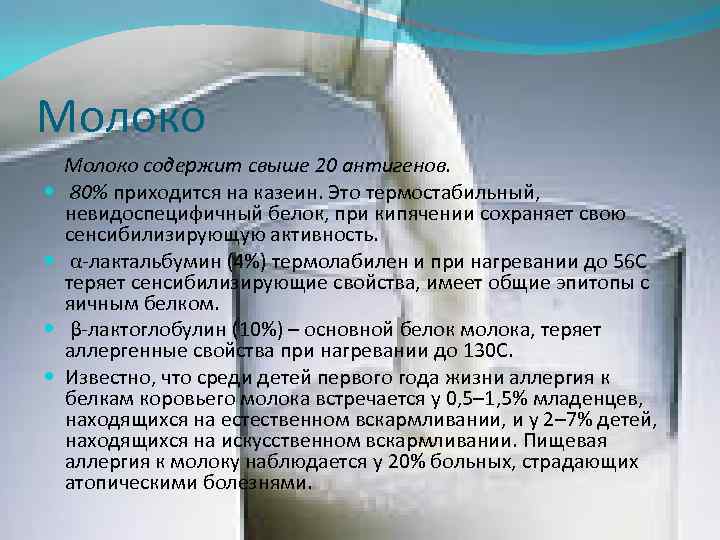
Another test your allergist may order is an oral food challenge. Under medical supervision, you’ll eat small amounts of a substance containing milk or a milk powder to see if a reaction develops. Because of the possibility that a reaction could be severe, this test is conducted in your allergist’s office or at a food challenge center with emergency equipment and medication on hand.
Management and Treatment
Avoidance of milk or items containing milk products is the only way to manage a milk allergy. People who are allergic to milk and the parents of children who have this allergy must read ingredient labels very carefully.
Milk is one of eight allergens with specific labeling requirements under the Food Allergen Labeling and Consumer Protection Act of 2004. That law requires manufacturers of packaged food products sold in the U.S. and containing milk as an ingredient to include the presence of milk or milk products, in clear language, on the ingredient label.
There are two main types of milk protein — casein and whey. Casein, the “solid” part of milk, comprises about 80 percent of milk protein. Whey proteins, found in the liquid part of milk, make up the other 20 percent. Milk proteins are found in many foods, including all dairy products, and in many places where they might not be expected. For example, some canned tuna, sausage, meats and other nondairy products may contain casein. Beverage mixes and body-building and energy drinks commonly contain whey. Milk protein has also been found in some chewing gum.
Casein, the “solid” part of milk, comprises about 80 percent of milk protein. Whey proteins, found in the liquid part of milk, make up the other 20 percent. Milk proteins are found in many foods, including all dairy products, and in many places where they might not be expected. For example, some canned tuna, sausage, meats and other nondairy products may contain casein. Beverage mixes and body-building and energy drinks commonly contain whey. Milk protein has also been found in some chewing gum.
Some companies may voluntarily include information that their food products “may contain traces of milk” or that they are manufactured in a facility that also processes milk, though such advisory statements are not required by law.
Allergies to food (including milk) are the most common causes of anaphylaxis, a potentially life-threatening allergic reaction. Symptoms include swelling of the airways, impairing the ability to breathe, and a sudden drop in blood pressure, causing dizziness and fainting. An allergist will advise patients with a food allergy to carry an auto-injector containing epinephrine (adrenaline), which is the only treatment for anaphylactic shock, and will teach the patient how to use it. If a child has the allergy, teachers and caregivers should be made aware of his or her condition as well.
Some people with this allergy can tolerate foods containing milk that has been extensively heated, such as a baked muffin. Still, people with an allergy to milk protein should consult an allergist before determining whether they should completely avoid milk and other dairy products.
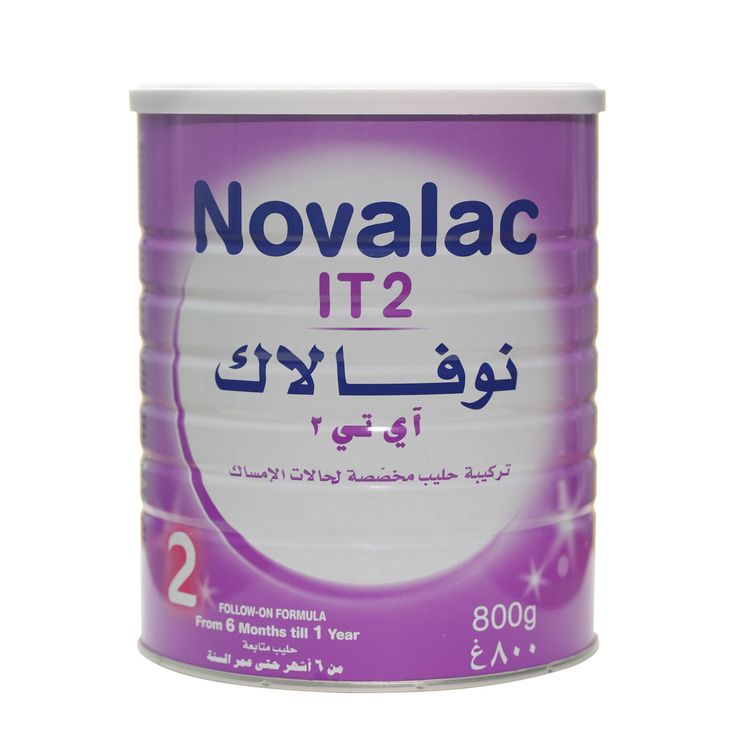
Milk is a fairly easy ingredient to substitute in recipes.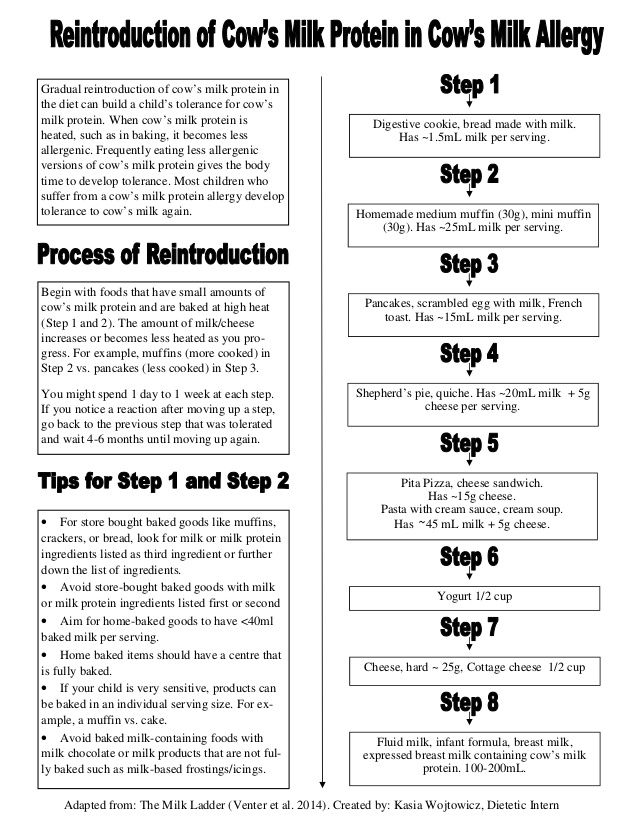 Most recipes calling for milk can be just as successful by substituting the equivalent in water, juice, or soy or rice milk. If your infant is allergic to milk, talk to your pediatrician about which formula to use. Often, an extensively hydrolyzed elemental formula or a casein-hydrolysate formula is recommended for milk allergy in infants, as the proteins in these formulas have been extensively broken down. Alternatively, your infant’s doctor may recommend a soy-based formula.
Most recipes calling for milk can be just as successful by substituting the equivalent in water, juice, or soy or rice milk. If your infant is allergic to milk, talk to your pediatrician about which formula to use. Often, an extensively hydrolyzed elemental formula or a casein-hydrolysate formula is recommended for milk allergy in infants, as the proteins in these formulas have been extensively broken down. Alternatively, your infant’s doctor may recommend a soy-based formula.
Milk Allergy or Lactose Intolerance?
Milk or dairy allergies and lactose intolerance are not related.
People with a milk or dairy allergy experience symptoms because their immune system reacts as though milk and other dairy products are a dangerous invader. This reaction can cause hives, an upset stomach, vomiting, bloody stools and even anaphylactic shock — a life-threatening allergic response.
Individuals who are lactose intolerant cannot digest the sugar in milk (lactose) because they have a deficiency of lactase, an enzyme produced by cells in the lining of the small intestine. Lactase is required to metabolize lactose. The lack of this enzyme — which sometimes can just be temporary, due to infection — causes symptoms such as abdominal gas, diarrhea or abdominal cramps.
Lactase is required to metabolize lactose. The lack of this enzyme — which sometimes can just be temporary, due to infection — causes symptoms such as abdominal gas, diarrhea or abdominal cramps.
If you suffer digestive problems after eating or drinking dairy products, try tracking your diet and noting how your body reacts to the items you consume. You may also try temporarily cutting dairy products — milk, cheese and yogurt, for example — from your diet and see if your symptoms improve. Report the results to your allergist, who can do testing — typically, skin testing — to confirm a diagnosis.
Cow's milk (F2), allergen-specific IgG
I confirm More
- Invitro
- Analyzes
- Allergological ...
- IgG, ...
- Specific IgG K ...
- Corny Milk (F2), ...
-
- COVID-19 9000
- Program program surveys for office workers
- Household staff screening
- Cardiovascular risk assessment
- Antiphospholipid syndrome (APS) diagnosis
- Liver function assessment
- Kidney and genitourinary system diagnosis
- Gastrointestinal tract diagnosis 909 909
- Diabetes mellitus diagnostics
- Anemia diagnostics
- Oncology
- Diagnostics and control of osteoporosis therapy
- Biathly blood biochemistry
- Diagnostics of the thyroid state
- Hospital profiles
- Healthy are healthy Country ,
- Gynecology, Reproduction
- Healthy child: for children from 0 to 14 years old
- infections, transmitted perishable by (STI)
- Weight problems
- VIP examinations
- Respiratory diseases
- Allergies
- Determination of microelement reserves in the body
- Laboratory assessment of the endocrine function of the pancreas and diagnosis of diabetes
- Biogenic amines
- Laboratory assessment of the state of the renin-angiotensin-aldosterone system
- Factors involved in the regulation of appetite and fat metabolism
- Laboratory assessment of the state of the gastrointestinal tract 60 Laboratory assessment of hormonal regulation of erythropoiesis
- Laboratory assessment of pineal gland function
- Interferon status, assessment of sensitivity to immunotherapeutic drugs:
- IgE - allergen-specific (allergy tests), mixtures, panels, total IgE.
- IgG, allergen-specific
- ImmunoCAP technology
- AlcorBio technology
- Systemic connective tissue diseases
- Articular rheumatoid lesions
- Antiphospholipid syndrome
- Vasculitis and kidney lesions
- Autoimmune lesions of the gastrointestinal tract. Celiac disease
- Autoimmune liver lesions
- Neurological autoimmune diseases
- Autoimmune endocrinopathy
- Autoimmune skin diseases
- Diseases of the lungs and heart
- Immune thrombocytopenes 9000
- Micromemoramic Micromemas0006
- Life and genetic factors
- Immunogenetics 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 Rules and blood vessels
- Diseases of the gastrointestinal tract
- Diseases of the central nervous system
- Oncological diseases
- metabolic disorders
- Description of the results of genetic studies by the geneticist
- Pharmacogenetics
- Detoxification of xenobiotics and carcinogens 9,000,000 9000
- Ruzas-factor
- Hereditary metabolic diseases
- Examination of newborns to detect hereditary metabolic diseases
- Additional studies (after screening and consultation with a specialist)
- Determination of biological relationship: paternity and motherhood
- Determination of biological relationship in the family: paternity and motherhood
- Water and soil quality study water quality study
- Soil quality testing
- Venous blood for analysis
- Tumor markers.
 View of a practical oncologist. Laboratory justifications.
View of a practical oncologist. Laboratory justifications. - Testosterone: diagnostic threshold, method-dependent reference values
- Laboratory assessment of lipid parameters in INVITRO
- Lipid profile: fasting or not fasting
Description
Method of determination Chemiluminescent immunoassay.
Test material Blood serum
Home visit available
Online check-in
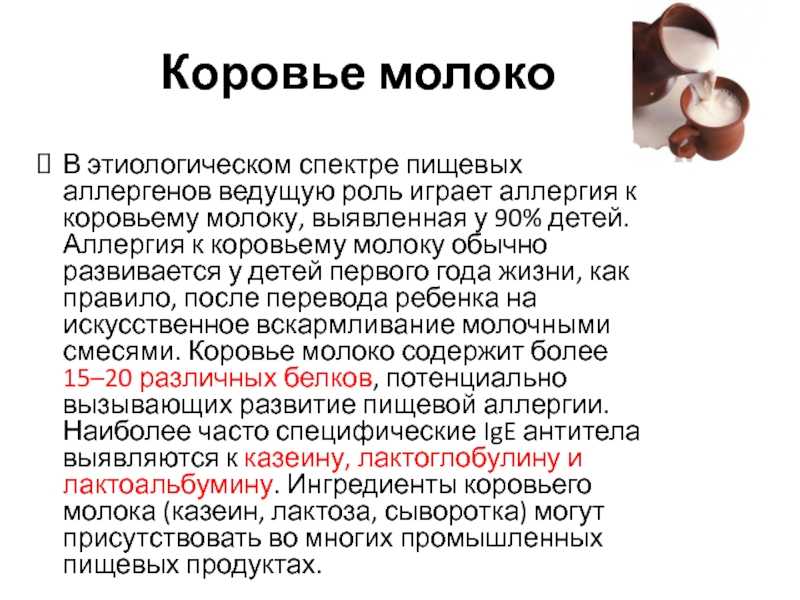
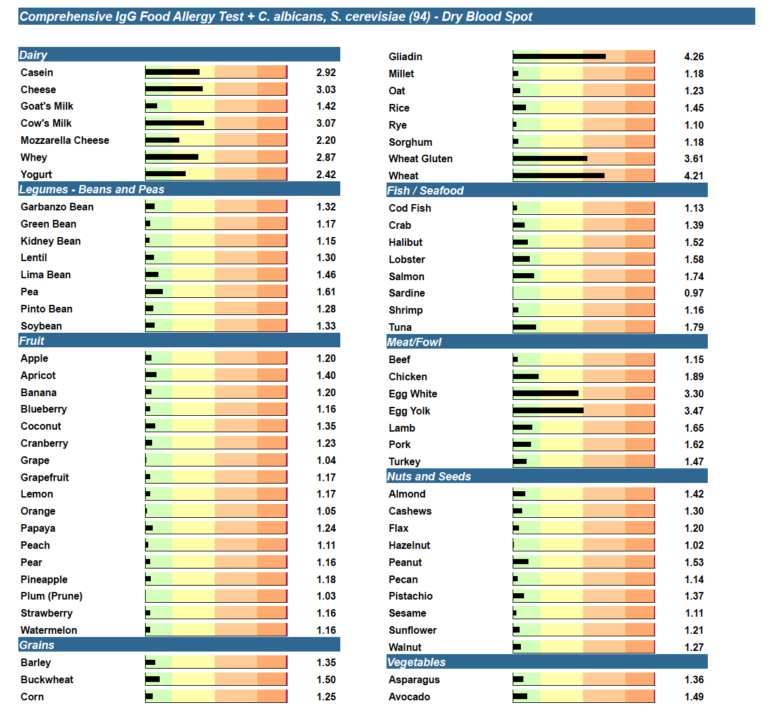
Determination of IgG class immunoglobulins to cow's milk antigens. See also test No. 608 - Cow's milk IgE. Cow's milk is one of the most common causes of allergic reactions in children. Sensitization to cow's milk occurs in 75% of children with food allergies. Milk allergens can be divided into caseins (curdling proteins) and whey proteins.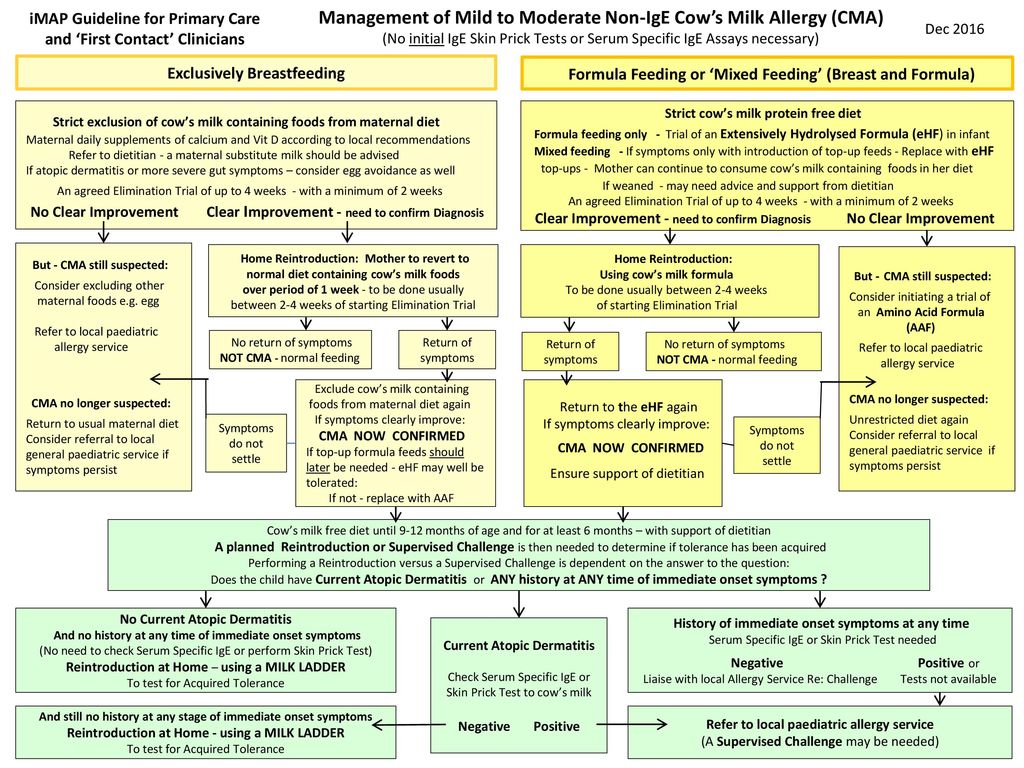 Caseins (see tests Nos. 650, 6602 - Casein IgE, IgG) quantitatively account for about 80% of all proteins in cow's milk (there are about 40% in breast milk). About 20% of the proteins in raw milk are whey proteins. The main milk whey allergens are beta-lactalbumin, beta-lactoglobulin (the main milk allergen, see tests no. 649, 6601 - beta-lactoglobulin IgE, IgG), bovine serum albumin, immunoglobulins. Due to the deficiency of digestive enzymes and the permeability of the intestinal wall in children, milk proteins can enter the bloodstream unchanged. Sensitization to cow's milk proteins can occur even in the womb or during breastfeeding against the background of intensive consumption of dairy products by the mother. The most common clinical manifestations of milk allergy can be skin manifestations (itchy rash, eczema, dermatitis), gastrointestinal symptoms (abdominal pain, vomiting, diarrhea, flatulence, constipation). Sometimes - respiratory phenomena (cough, asthma attacks, rhinitis).
Caseins (see tests Nos. 650, 6602 - Casein IgE, IgG) quantitatively account for about 80% of all proteins in cow's milk (there are about 40% in breast milk). About 20% of the proteins in raw milk are whey proteins. The main milk whey allergens are beta-lactalbumin, beta-lactoglobulin (the main milk allergen, see tests no. 649, 6601 - beta-lactoglobulin IgE, IgG), bovine serum albumin, immunoglobulins. Due to the deficiency of digestive enzymes and the permeability of the intestinal wall in children, milk proteins can enter the bloodstream unchanged. Sensitization to cow's milk proteins can occur even in the womb or during breastfeeding against the background of intensive consumption of dairy products by the mother. The most common clinical manifestations of milk allergy can be skin manifestations (itchy rash, eczema, dermatitis), gastrointestinal symptoms (abdominal pain, vomiting, diarrhea, flatulence, constipation). Sometimes - respiratory phenomena (cough, asthma attacks, rhinitis).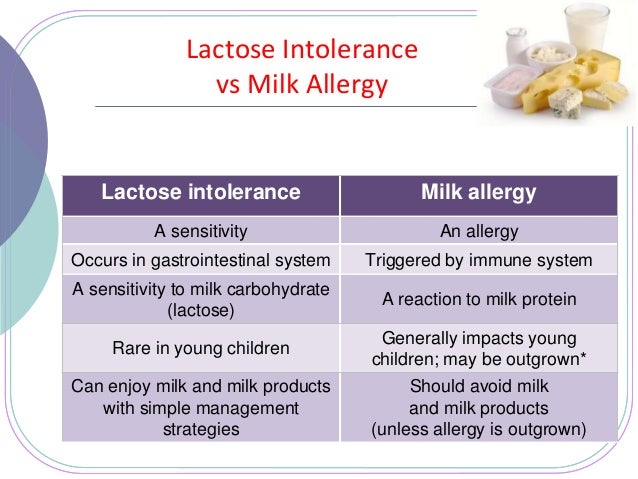 If you are allergic to cow's milk, you can cross-react with beef. An allergic reaction to milk proteins should be distinguished from milk intolerance associated with an enzyme (lactase) deficiency (see test No. 236 - Carbohydrates in feces). The vast majority of food allergies are IgE-mediated allergic reactions. Basic laboratory diagnostic allergy tests are based on the presence of specific IgE antibodies in the blood (see definition of specific IgE). IgG antibodies are often found in food allergies, detectable IgG are not necessarily reactive to the same proteins as IgE, their role is not completely clear. Potentially, they can participate in food hypersensitivity reactions: it has been shown that degranulation of mast cells and basophils can be induced not only by the complex of IgE and antigen, but also by other stimuli, for example, anaphylotoxins C3a and C5a, which are produced during the alternative (IgG4 is involved) or classical ( involved IgG1, IgG2, IgG3) complement activation pathways.
If you are allergic to cow's milk, you can cross-react with beef. An allergic reaction to milk proteins should be distinguished from milk intolerance associated with an enzyme (lactase) deficiency (see test No. 236 - Carbohydrates in feces). The vast majority of food allergies are IgE-mediated allergic reactions. Basic laboratory diagnostic allergy tests are based on the presence of specific IgE antibodies in the blood (see definition of specific IgE). IgG antibodies are often found in food allergies, detectable IgG are not necessarily reactive to the same proteins as IgE, their role is not completely clear. Potentially, they can participate in food hypersensitivity reactions: it has been shown that degranulation of mast cells and basophils can be induced not only by the complex of IgE and antigen, but also by other stimuli, for example, anaphylotoxins C3a and C5a, which are produced during the alternative (IgG4 is involved) or classical ( involved IgG1, IgG2, IgG3) complement activation pathways. But it is also known that IgG antibodies to the allergen can also perform the function of blocking antibodies, which reduce the severity of allergic reactions that occur with the participation of specific IgE. IgG antibodies to food allergens can be found in healthy people as evidence of increased consumption of certain foods without being allergic to them. The diagnostic value of the fact of detecting an increased amount of IgG to food allergens in the patient's blood is debatable. The study of IgG to food allergens is usually carried out in addition to the study of IgE, in order to select the optimal change in diet with the exclusion or rotation of individual food components, which can significantly improve the patient's condition. The appointment and interpretation of the test results should be carried out by a specialist who represents the limitations of this study and considers it in combination with clinical and anamnestic data and the results of other tests.
But it is also known that IgG antibodies to the allergen can also perform the function of blocking antibodies, which reduce the severity of allergic reactions that occur with the participation of specific IgE. IgG antibodies to food allergens can be found in healthy people as evidence of increased consumption of certain foods without being allergic to them. The diagnostic value of the fact of detecting an increased amount of IgG to food allergens in the patient's blood is debatable. The study of IgG to food allergens is usually carried out in addition to the study of IgE, in order to select the optimal change in diet with the exclusion or rotation of individual food components, which can significantly improve the patient's condition. The appointment and interpretation of the test results should be carried out by a specialist who represents the limitations of this study and considers it in combination with clinical and anamnestic data and the results of other tests. nine0003
nine0003
Preparation
Preferably 4 hours after the last meal, no requirement. It is undesirable to conduct a study against the background of the use of glucocorticoid hormone preparations (you should consult with your allergist regarding the advisability of canceling). Antihistamines do not affect the result.
Indications for prescribing
- In a complex of studies to identify the potential pathogenetic role of individual allergens (in addition to the study of IgE antibodies). nine0006
- For dietary management in patients with food sensitivities.
Interpretation of results
Interpretation of test results contains information for the attending physician and is not a diagnosis. The information in this section should not be used for self-diagnosis or self-treatment. An accurate diagnosis is made by the doctor, using both the results of this examination and the necessary information from other sources: history, results of other examinations, etc.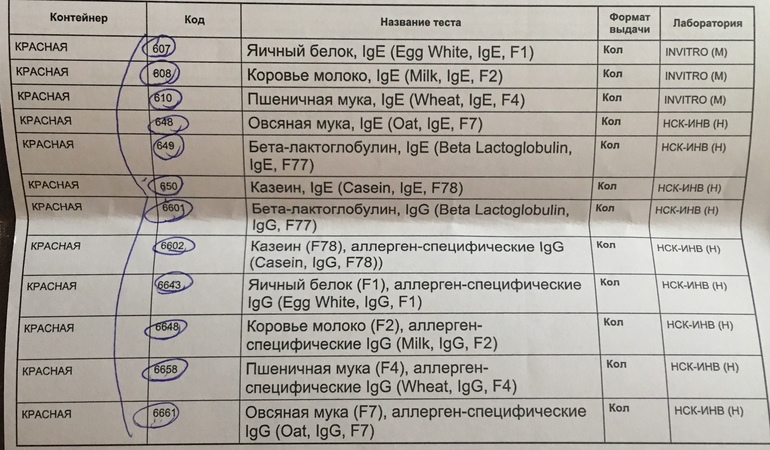 nine0538
nine0538
Units of measurement in the INVITRO laboratory: mg/l. Interpretation of results:
| Concentration specific IgG, mg/l | Interpretation of the result | |
| Negative - Norma | ||
| 50 - 100 | Little amount | |
| 100 - 200 | ||
| > 200 | High |
Reference values:
In this section you can find out how much it costs to perform this study in your city, read the description of the test and the table of interpretation of the results. When choosing where to take the analysis "Cow's milk (F2), allergen-specific IgG" in Moscow and other cities of Russia, do not forget that the price of the analysis, the cost of the procedure for taking biomaterial, methods and terms for performing studies in regional medical offices may differ. nine0003
nine0003
Subscribe to our newsletters
Enter e-mail
I consent to processing of personal data nine0003
Subscribe
Component diagnosis of milk allergy
Quantification in the blood of specific class E immunoglobulins to casein and whole cow's milk, which allows to differentiate sensitization to thermostable and thermolabile fractions of milk proteins and to resolve the issue of the possibility of eating some dairy and fermented milk products by patients with allergies for milk.
Synonyms Russian
Class E specific immunoglobulins to casein and whole cow's milk .
Synonyms English
Component diagnostics of milk allergy, Cow’s Milk and Casein, IgE (ImmunoCAP).
Test method
Solid phase immunofluorescence (ImmunoCAP).
Units
kU/l (kilo unit per litre).
What biomaterial can be used for research?
Venous blood.
How to properly prepare for an examination?
- Do not smoke for 30 minutes before the test.
General information about the study
Milk is an important component of baby food. Milk and dairy products are a valuable source of protein, calories, vitamins and minerals, especially calcium. At the same time, milk is one of the most common food allergens. In developed countries, according to various sources, the frequency of sensitization to it is 0.5-7.5%. Food allergy to milk is more often observed in children of the first years of life, mainly up to 5-6 years of age.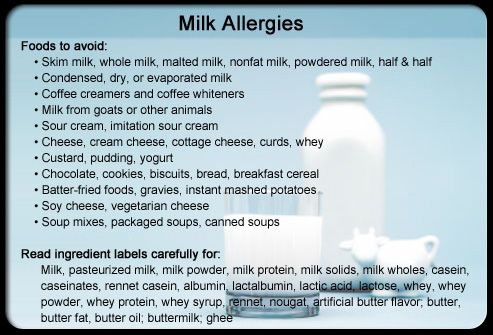 nine0003
nine0003
In people sensitized to cow's milk, allergy can manifest itself as skin symptoms in the form of urticaria, angioedema and exacerbations of atopic dermatitis, damage to the digestive tract (abdominal pain, nausea, vomiting, diarrhea), rhinitis, exacerbation of bronchial asthma, anaphylactic reactions. Allergic reactions can also occur when consuming products that are not considered dairy, but contain some milk proteins or their traces that have fallen into production. Therefore, with allergies, it is very important to carefully read the composition of the products before eating. Hypersensitivity to cow's milk does not always disappear in childhood and may persist for many years into adulthood or for life, depending to some extent on the type of protein to which the sensitization occurs. nine0003
Cow's milk contains about 40 proteins that can act as allergens. Taking into account the physicochemical properties, they are divided into caseins (80% of milk proteins) and whey proteins (20%).
Casein is a thermostable protein and retains its allergenic properties after heat treatment of milk. It is found in large quantities in cheese, cottage cheese, and in the food industry it is used as additives in sausages and confectionery, sauces, soups, stews, drinks, ice cream, glazes. This protein is often a latent allergen, and reactions to it are usually associated with a more severe course of allergy and prolonged persistence of sensitization to milk and dairy products in any form. nine0003
Bovine whey contains predominantly globular proteins, beta-lactoglobulin and alpha-lactalbumin, and to a lesser extent bovine whey protein, lactoferrin, immunoglobulins. Whey proteins reduce or lose allergenicity after heat treatment, for example, during baking, boiling, and also during fermentation, fermentation. Therefore, patients sensitized only to whole milk and insensitive to casein can in most cases consume fermented milk products (cottage cheese, kefir, fermented baked milk, curdled milk, yogurt), melted butter, and baked goods containing milk without developing allergic reactions. nine0003
nine0003
Cow's milk proteins are 80% similar in structure to goat's and sheep's milk proteins, which causes their allergic cross-reactivity. Therefore, the replacement of cow's milk with goat's milk is not possible in all patients with an allergy to cow's milk, but only in about a third of those sensitized.
However, the complete exclusion of dairy products without their adequate replacement with other types of milk or special mixtures can adversely affect the growth and development of the child's body. The selection of mixtures for young children should be carried out under the supervision of a physician, taking into account the individual patient's sensitization profile. Possible blends include partial or total milk protein hydrolysates, goat's milk formulas, soy or rice formulas, and in cases of severe allergies, amino acid blends. Additional medications and vitamin and mineral supplements may be recommended for patients. nine0003
With age, many children become tolerant to milk allergens. However, if the level of specific IgE antibodies to milk exceeds 60 IU / ml (EC / L), then the likelihood of persistent allergies is high - the persistence of reactions until adolescence or adulthood, and in some cases for life.
However, if the level of specific IgE antibodies to milk exceeds 60 IU / ml (EC / L), then the likelihood of persistent allergies is high - the persistence of reactions until adolescence or adulthood, and in some cases for life.
The main therapeutic measure for allergy to cow's milk proteins is the complete exclusion of this product from the diet, and in case of sensitization only to whey proteins - the exclusion of whole thermally unprocessed milk. The possibility of sublingual and oral immunotherapy for the treatment of allergy to cow's milk proteins is currently being studied. nine0003
What is research used for?
- Diagnosis of allergy to cow's milk proteins;
- addressing the issue of the possibility of including heat-treated dairy and sour-milk products in the diet;
- selection of hydrolyzed or alternative formulas for feeding young children.
When is the test scheduled?
- If cow's milk sensitization is suspected; nine0006
- when a reaction to milk is detected according to the results of skin tests;
- when selecting infant formula;
- when examining children with atopic dermatitis, urticaria, angioedema, bronchial asthma, allergic rhinitis / conjunctivitis, gastrointestinal disorders, anaphylactic shock and other manifestations of allergic diseases.

What do the results mean?
Reference values
For each indicator included in the complex:
- [21-627] Allergen f2 - cow's milk, IgE (ImmunoCAP)
- [21-630] Allergic component f78 – casein nBos d8, IgE (ImmunoCAP)
| IgE to whole blood milk + | IgE to casein + | Casein sensitization with or without whey protein sensitization (possible reactions to any kind of dairy products, traces of milk protein) |
| IgE to whole blood milk + | IgE to casein - | Sensitization to whey proteins only (possible consumption of fermented milk products, as well as pastries containing milk) |
| IgE to whole blood milk - | IgE to casein - | nine0701
Important Notes
- The test results should not be used to formulate a patient's diet without the advice of a physician.
 The absence of antibodies to cow's milk proteins does not exclude other possible reactions of the gastrointestinal tract to milk consumption, for example, in lactase deficiency, non-IgE-related hypersensitivity mechanisms in eosinophilic esophagitis. nine0006
The absence of antibodies to cow's milk proteins does not exclude other possible reactions of the gastrointestinal tract to milk consumption, for example, in lactase deficiency, non-IgE-related hypersensitivity mechanisms in eosinophilic esophagitis. nine0006 - Performing this study is safe for the patient compared to skin tests (in vivo), as it eliminates the patient's exposure to the allergen. Taking antihistamines and age characteristics do not affect the quality and accuracy of the study.
Also recommended
[02-029] CBC with leukocyte formula and ESR
[08-017] Total immunoglobulins E (IgE) in serum
[21-673] Allergochip ISA component1 nine0003
[40-443] Eczema
[21-713] Allergic component f77 - Beta-lactoglobulin nBos d 5, IgE (ImmunoCAP)
[21-636] Allergen f79 - gluten (gluten), IgE (ImmunoCAP)
[21-622] Allergen f245 - egg, IgE (ImmunoCAP)
[42-018] Lactose intolerance (adults and children over 3 years )
+ determination of class E specific immunoglobulins to other allergens
Who orders the test?
Allergist, gastroenterologist, pediatrician, dermatologist, internist, general practitioner.