Blood screening pregnancy
Common Tests During Pregnancy | Johns Hopkins Medicine
-
Genetic Screening
-
First Trimester
-
Second Trimester
-
Ultrasound
-
Amniocentesis
-
Chorionic Villus Sampling
-
Fetal Monitoring
-
Glucose
-
Group B Strep Culture
Your health care provider may recommend a variety of screenings, tests and imaging techniques during your pregnancy. These tests are designed to provide information about the health of your baby and may help you optimize your child’s prenatal care and development.
Genetic Screening
Many genetic abnormalities can be diagnosed before birth. Your doctor or midwife may recommend genetic testing during pregnancy if you or your partner has a family history of genetic disorders. You may also choose to have genetic screening if you have had a fetus or baby with a genetic abnormality.
Examples of genetic disorders that can be diagnosed before birth include:
-
Cystic fibrosis
-
Duchenne muscular dystrophy
-
Hemophilia A
-
Polycystic kidney disease
-
Sickle cell disease
-
Tay-Sachs disease
-
Thalassemia
The following screening methods are available during pregnancy:
-
Alpha-fetoprotein (AFP) test or multiple marker test
-
Amniocentesis
-
Chorionic villus sampling
-
Cell-free fetal DNA testing
-
Percutaneous umbilical blood sampling (withdrawing a small sample of the fetal blood from the umbilical cord)
-
Ultrasound scan
First Trimester Prenatal Screening Tests
First trimester screening is a combination of fetal ultrasound and maternal blood testing. This screening process can help determine the risk of the fetus having certain birth defects. Screening tests may be used alone or with other tests.
This screening process can help determine the risk of the fetus having certain birth defects. Screening tests may be used alone or with other tests.
First trimester screening includes:
-
Ultrasound for fetal nuchal translucency. Nuchal translucency screening uses an ultrasound to examine the area at the back of the fetal neck for increased fluid or thickening.
-
Ultrasound for fetal nasal bone determination. The nasal bone may not be visualized in some babies with certain chromosome abnormalities, such as Down syndrome. This screen is performed using an ultrasound between 11 and 13 weeks gestation.
-
Maternal serum (blood) tests. These blood tests measure two substances found in the blood of all pregnant women:
-
Pregnancy-associated plasma protein A. A protein produced by the placenta in early pregnancy. Abnormal levels are associated with an increased risk of chromosomal abnormality.
-
Human chorionic gonadotropin. A hormone produced by the placenta in early pregnancy. Abnormal levels are associated with an increased risk of chromosomal abnormality.
-
When used together as first trimester screening tests, nuchal translucency screening and maternal blood tests have a greater ability to determine if the fetus might have a birth defect, such as Down syndrome (trisomy 21) and trisomy 18.
If the results of these first trimester screening tests are abnormal, genetic counseling is recommended. Additional testing, such as chorionic villus sampling, amniocentesis, cell-free fetal DNA or other ultrasounds, may be needed for an accurate diagnosis.
Second Trimester Prenatal Screening Tests
Second trimester prenatal screening may include several blood tests called multiple markers. These markers provide information about your potential risk of having a baby with certain genetic conditions or birth defects.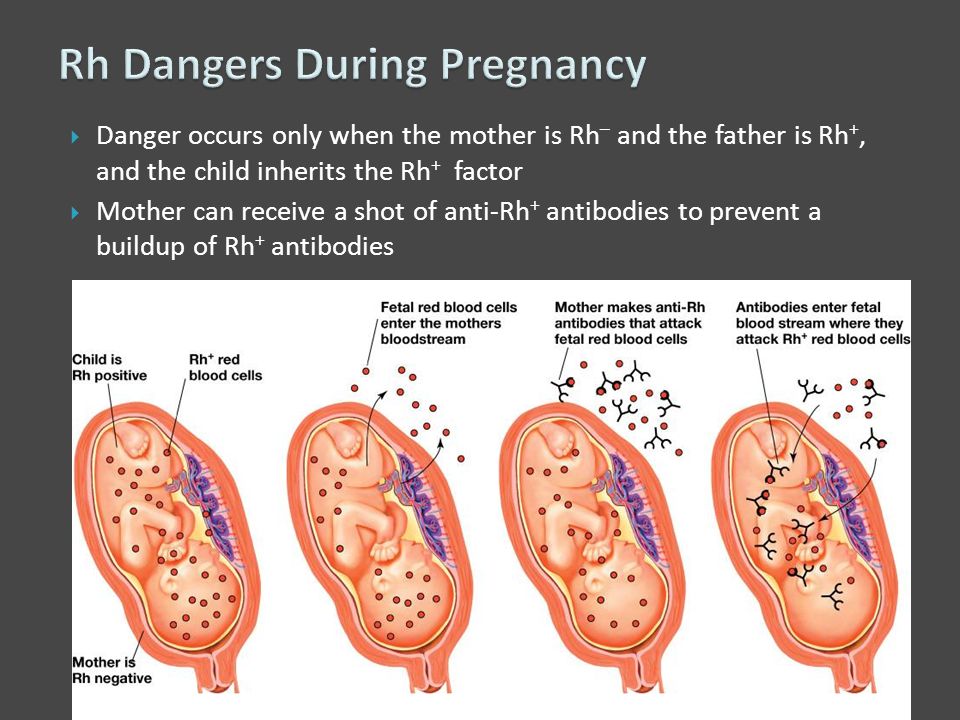 Screening is usually done by taking a sample of your blood between 15 and 20 weeks of pregnancy (16 to 18 weeks is ideal). The multiple markers include:
Screening is usually done by taking a sample of your blood between 15 and 20 weeks of pregnancy (16 to 18 weeks is ideal). The multiple markers include:
-
AFP screening. Also called maternal serum AFP, this blood test measures the level of AFP in your blood during pregnancy. AFP is a protein normally produced by the fetal liver that is present in the fluid surrounding the fetus (amniotic fluid). It crosses the placenta and enters your blood. Abnormal levels of AFP may indicate:
-
A miscalculated due date, as the levels vary throughout pregnancy
-
Defects in the abdominal wall of the fetus
-
Down syndrome or other chromosomal abnormalities
-
Open neural tube defects, such as spina bifida
-
Twins (more than one fetus is producing the protein)
-
-
Estriol.
 This is a hormone produced by the placenta. It can be measured in maternal blood or urine to be used to determine fetal health.
This is a hormone produced by the placenta. It can be measured in maternal blood or urine to be used to determine fetal health. -
Inhibin. This is a hormone produced by the placenta.
-
Human chorionic gonadotropin. This is also a hormone produced by the placenta.
Abnormal test results of AFP and other markers may mean that additional testing is needed. An ultrasound is used to confirm the milestones of your pregnancy and to check the fetal spine and other body parts for defects. An amniocentesis may be needed for an accurate diagnosis.
Since multiple marker screening is not diagnostic, it is not 100 percent accurate. It helps determine who in the population should be offered additional testing during pregnancy. False-positive results may indicate a problem when the fetus is actually healthy. On the other hand, false-negative results indicate a normal result when the fetus actually does have a health problem.
When you have both first and second trimester screening tests performed, the ability of the tests to detect an abnormality is greater than using just one screening independently. Most cases of Down syndrome can be detected when both first and second trimester screenings are used.
Ultrasound
An ultrasound scan is a diagnostic technique that uses high-frequency sound waves to create an image of the internal organs. A screening ultrasound is sometimes done during the course of your pregnancy to check normal fetal growth and verify the due date.
When are ultrasounds performed during pregnancy?
Ultrasounds may be done at various times throughout pregnancy for several reasons:
First Trimester
-
To establish the due date (this is the most accurate way of determining the due date)
-
To determine the number of fetuses and identify placental structures
-
To diagnose an ectopic pregnancy or miscarriage
-
To examine the uterus and other pelvic anatomy
-
To detect fetal abnormalities (in some cases)
Midtrimester (also called the 18- to 20-week scan)
-
To confirm the due date (a due date set in the first trimester is rarely changed)
-
To determine the number of fetuses and examine the placental structures
-
To assist in prenatal tests, such as an amniocentesis
-
To examine the fetal anatomy for abnormalities
-
To check the amount of amniotic fluid
-
To examine blood flow patterns
-
To observe fetal behavior and activity
-
To measure the length of the cervix
-
To monitor fetal growth
Third Trimester
-
To monitor fetal growth
-
To check the amount of amniotic fluid
-
To conduct the biophysical profile test
-
To determine the position of the fetus
-
To assess the placenta
How is an ultrasound scan performed?
Two types of ultrasounds can be performed during pregnancy:
-
Abdominal ultrasound.
 In an abdominal ultrasound, gel is applied to your abdomen. The ultrasound transducer glides over the gel on the abdomen to create the image.
In an abdominal ultrasound, gel is applied to your abdomen. The ultrasound transducer glides over the gel on the abdomen to create the image. -
Transvaginal ultrasound. In a transvaginal ultrasound, a smaller ultrasound transducer is inserted into your vagina and rests against the back of the vagina to create an image. A transvaginal ultrasound produces a sharper image than an abdominal ultrasound and is often used in early pregnancy.
Which ultrasound imaging techniques are available?
There are several types of ultrasound imaging techniques. As the most common type, the 2-D ultrasound provides a flat picture of one aspect of the baby.
If more information is needed, a 3-D ultrasound exam can be done. This technique, which provides a 3-D picture, requires a special machine and special training. The 3-D image allows the health care provider to see the width, height and depth of the images, which can be helpful during the diagnosis. The 3-D images can also be captured and saved for later review.
The 3-D images can also be captured and saved for later review.
The latest technology is 4-D ultrasound, which allows the health care provider to visualize the unborn baby moving in real time. With 4-D imaging, a three-dimensional image is continuously updated, providing a “live action” view. These images often have a golden color, which helps show shadows and highlights.
Ultrasound images may be captured in still photographs or on video to document findings.
What are the risks and benefits of ultrasound imaging?
Fetal ultrasound has no known risks other than mild discomfort due to pressure from the transducer on your abdomen or in your vagina. No radiation is used during the procedure.
Transvaginal ultrasound requires covering the ultrasound transducer in a plastic or latex sheath, which may cause a reaction in women with a latex allergy.
Ultrasound imaging is constantly being improved and refined. As with any test, the results may not be completely accurate.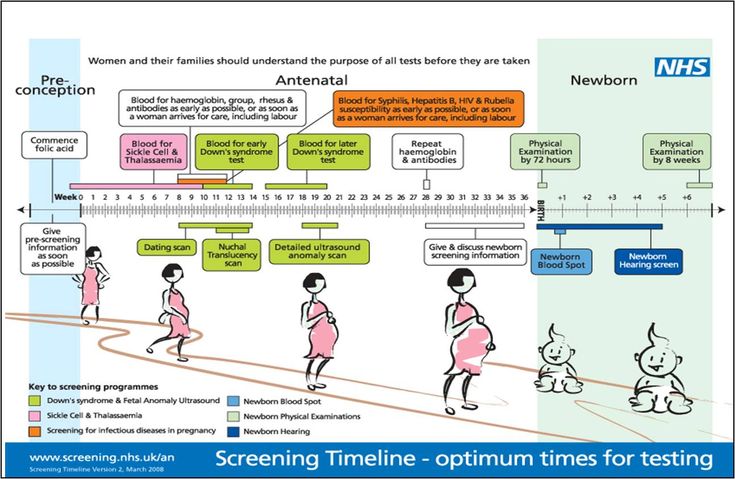 However, an ultrasound can provide valuable information to parents and health care providers, helping them manage and care for the pregnancy and the baby. In addition, ultrasound imaging gives parents a unique opportunity to see their baby before birth, helping them to bond and establish an early relationship.
However, an ultrasound can provide valuable information to parents and health care providers, helping them manage and care for the pregnancy and the baby. In addition, ultrasound imaging gives parents a unique opportunity to see their baby before birth, helping them to bond and establish an early relationship.
Fetal ultrasound is sometimes offered in nonmedical settings to provide keepsake images or videos for parents. While the ultrasound procedure itself is considered safe, it is possible that untrained personnel may miss an abnormality or give parents false assurances about their baby’s well-being. It is best to have an ultrasound performed by trained medical personnel who can correctly interpret the results. Talk with your doctor or midwife if you have questions.
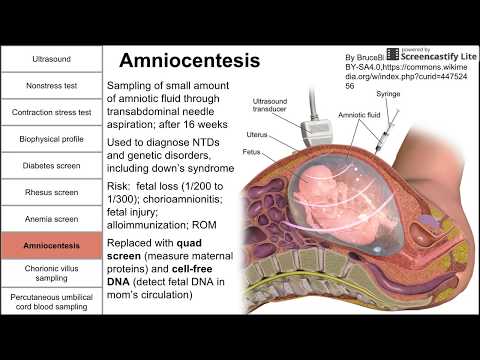
Amniocentesis
An amniocentesis involves taking a small sample of the amniotic fluid that surrounds the fetus. It is used to diagnose chromosomal disorders and open neural tube defects, such as spina bifida. Testing is available for other genetic defects and disorders depending on your family history and the availability of lab testing at the time of the procedure.
Testing is available for other genetic defects and disorders depending on your family history and the availability of lab testing at the time of the procedure.
Who is an ideal candidate for amniocentesis?
An amniocentesis is generally offered to women between the 15th and 20th week of pregnancy who have an increased risk of chromosomal abnormalities. Candidates include women who will be over age 35 at the time of delivery or those who have had an abnormal maternal serum screening test.
How is an amniocentesis performed?
An amniocentesis involves inserting a long, thin needle through your abdomen into the amniotic sac to withdraw a small sample of amniotic fluid. The amniotic fluid contains cells shed by the fetus, which contain genetic information. Although specific details of each procedure may vary, a typical amniocentesis follows this process:
-
Your abdomen will be cleansed with an antiseptic.
-
Your doctor may or may not give a local anesthetic to numb the skin.

-
Your doctor will use ultrasound technology to help guide a hollow needle into the amniotic sac. He or she will withdraw a small sample of fluid for lab analysis.
You may feel some cramping during or after the amniocentesis. Strenuous activities should be avoided for 24 hours following the procedure.
Women who are pregnant with twins or other higher-order multiples need sampling from each amniotic sac to study each baby. Depending on the position of the baby and placenta, amount of fluid, and woman’s anatomy, sometimes the amniocentesis cannot be done. The fluid is then sent to a genetics lab so that the cells can grow and be analyzed. AFP is also measured to rule out an open neural tube defect. Results are usually available in about 10 days to two weeks, depending on the lab.
Chorionic Villus Sampling (CVS)?
CVS is a prenatal test that involves taking a sample of some of the placental tissue. This tissue contains the same genetic material as the fetus and can be tested for chromosomal abnormalities and some other genetic problems. Testing is available for other genetic defects and disorders, depending on your family history and the availability of lab testing at the time of the procedure. Unlike amniocentesis, CVS does not provide information on open neural tube defects. Therefore, women who undergo CVS also need a follow-up blood test between 16 and 18 weeks of pregnancy to screen for these defects.
Testing is available for other genetic defects and disorders, depending on your family history and the availability of lab testing at the time of the procedure. Unlike amniocentesis, CVS does not provide information on open neural tube defects. Therefore, women who undergo CVS also need a follow-up blood test between 16 and 18 weeks of pregnancy to screen for these defects.
How is CVS performed?
CVS may be offered to women with an increased risk of chromosomal abnormalities or who have a family history of a genetic defect that is testable from the placental tissue. CVS is usually performed between the 10th and 13th week of pregnancy. Although exact methods may vary, the procedure involves the following steps:
-
Your doctor will insert a small tube (catheter) through your vagina and into your cervix.
-
Using ultrasound technology, your doctor will guide the catheter into place near the placenta.
-
Your doctor will remove some tissue using a syringe on the other end of the catheter.

Your doctor may also choose to perform a transabdominal CVS, which involves inserting a needle through your abdomen and into your uterus to sample the placental cells. You may feel some cramping during and after either type of CVS procedure. The tissue samples are sent to a genetic lab for growth and analysis. Results are usually available in about 10 days to two weeks, depending on the lab.
What if CVS is not possible?
Women with twins or other higher-order multiples usually need sampling from each placenta. However, because of the complexity of the procedure and the positioning of the placentas, CVS is not always feasible or successful with multiples.
Women who are not candidates for CVS or who did not get accurate results from the procedure may require a follow-up amniocentesis. An active vaginal infection, such as herpes or gonorrhea, will prohibit the procedure. In other cases, the doctor may take a sample that does not have enough tissue to grow in the lab, generating incomplete or inconclusive results.
Fetal Monitoring
During late pregnancy and labor, your doctor may want to monitor the fetal heart rate and other functions. Fetal heart rate monitoring is a method of checking the rate and rhythm of the fetal heartbeat. The average fetal heart rate is between 120 and 160 beats per minute. This rate may change as the fetus responds to conditions in the uterus. An abnormal fetal heart rate or pattern may mean that the fetus is not getting enough oxygen or indicate other problems. An abnormal pattern also may mean that an emergency cesarean delivery is needed.
How is fetal monitoring performed?
Using a fetoscope (a type of stethoscope) to listen to the fetal heartbeat is the most basic type of fetal heart rate monitoring. Another type of monitoring is performed with a hand-held Doppler device. This is often used during prenatal visits to count the fetal heart rate. During labor, continuous electronic fetal monitoring is often used. Although the specific details of each procedure may vary, standard electronic fetal monitoring follows this process:
-
Gel is applied to your abdomen to act as a medium for the ultrasound transducer.

-
The ultrasound transducer is attached to your abdomen with straps so it can transmit the fetal heartbeat to a recorder. The fetal heart rate is displayed on a screen and printed onto special paper.
-
During contractions, an external tocodynamometer (a monitoring device that is placed over the top of the uterus with a belt) can record the pattern of contractions.
When is internal fetal monitoring needed?
On occasion, internal fetal monitoring is needed to provide a more accurate reading of the fetal heart rate. Your bag of waters (amniotic fluid) must be broken and your cervix must be partially dilated to use internal monitoring. Internal fetal monitoring involves inserting an electrode through the dilated cervix and attaching the electrode to the scalp of the fetus.
Glucose Testing
Glucose testing is used to measure the level of sugar in your blood.
A glucose challenge test is usually conducted between 24 and 28 weeks of pregnancy. Abnormal glucose levels may indicate gestational diabetes.
Abnormal glucose levels may indicate gestational diabetes.
What is involved in a glucose challenge test?
The initial one-hour test is a glucose challenge test. If the results are abnormal, a glucose tolerance test is needed.
How is a glucose tolerance test performed?
You may be asked to only drink water on the day the glucose tolerance test is given. Although the specific details of each procedure may vary, a typical glucose tolerance test includes the following steps:
-
An initial fasting sample of blood will be drawn from your vein.
-
You will be given a special glucose solution to drink.
-
Blood will be drawn at various times over the course of several hours to measure the glucose levels in your body.
Group B Strep Culture
Group B streptococcus (GBS) is a type of bacteria found in the lower genital tract of about 20 percent of all women. While a GBS infection does not usually cause problems in women before pregnancy, it can cause serious illness in mothers during pregnancy. GBS may cause chorioamnionitis (a severe infection of the placental tissues) and postpartum infection. Urinary tract infections caused by GBS can lead to preterm labor and birth or pyelonephritis and sepsis.
GBS may cause chorioamnionitis (a severe infection of the placental tissues) and postpartum infection. Urinary tract infections caused by GBS can lead to preterm labor and birth or pyelonephritis and sepsis.
GBS is the most common cause of life-threatening infections in newborns, including pneumonia and meningitis. Newborn babies contract the infection during pregnancy or from the mother’s genital tract during labor and delivery.
The Centers for Disease Control and Prevention recommends screening all pregnant women for vaginal and rectal GBS colonization between 35 and 37 weeks gestation. The treatment of mothers with certain risk factors or positive cultures is important to reduce the risk of transmission of GBS to the baby. Babies whose mothers receive antibiotic treatment for a positive GBS test are 20 times less likely to develop the disease than those without treatment.
Prenatal tests | March of Dimes
Prenatal tests help your health care provider find out how you and your baby are doing during pregnancy.

Some prenatal tests, such as a blood pressure check and a urine test, are done several times during pregnancy.
Other prenatal tests, such as an ultrasound or special blood tests, are done less often.
Some prenatal tests check to see if your baby has certain health problems, like birth defects or genetic conditions.
Talk to your provider about which prenatal tests are right for you.
What are prenatal tests and why are they important?
Prenatal tests are medical tests you get during pregnancy. They help your health care provider find out how you and your baby are doing.
You get some prenatal tests several times during pregnancy at your prenatal care checkups. These tests make sure you and your baby are staying healthy. There are other tests that are done at certain times during your pregnancy. These prenatal tests check to see if your baby has any health problems, including:
- Birth defects.
 These are health conditions that are present at birth. They change the shape or function of one or more parts of the body. Birth defects can cause problems in overall health, how the body develops or how the body works.
These are health conditions that are present at birth. They change the shape or function of one or more parts of the body. Birth defects can cause problems in overall health, how the body develops or how the body works. - Genetic and chromosomal conditions. These conditions are caused by changes in genes and chromosomes. A gene is part of your body's cells that stores instructions for the way your body grows and works. A chromosome is the structure in cells that holds genes. Genetic conditions include cystic fibrosis (also called CF), sickle cell disease and heart defects. A common chromosomal condition is Down syndrome. Sometimes these conditions are passed from parent to child, and sometimes they happen on their own.
If there is a history of certain health conditions in your family, you may want to talk with a genetic counselor. A genetic counselor has training to help you understand about birth defects and other medical conditions that run in families and how they can affect your health and your baby's health.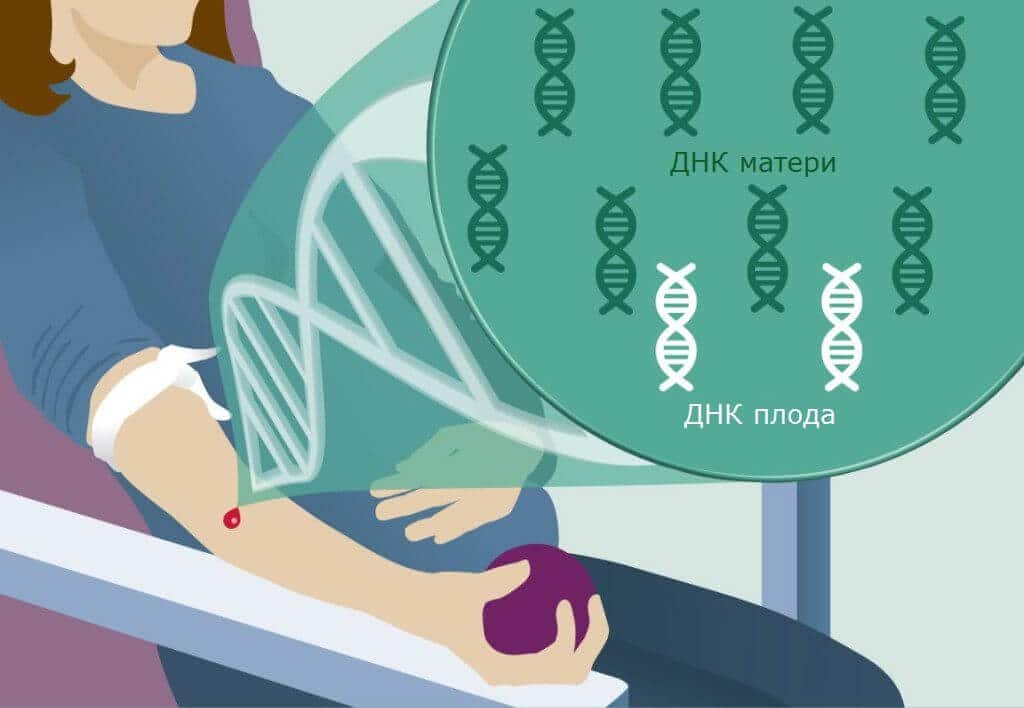
What are screening tests and diagnostic tests?
Screening tests check to see if your baby is more likely to have a health condition, but they don’t tell you for sure if you baby has a condition. There are no risks to you or your baby when you have a screening test.
Diagnostic tests tell you for sure if your baby has a health condition. If a screening test shows your baby is at high risk of a health condition, your provider may recommend a diagnostic test to confirm the results. Some diagnostic tests may have some risks for your baby, like miscarriage. Miscarriage is when a baby dies in the womb before 20 weeks of pregnancy.
Screening test results can help you decide if you want to have a diagnostic test. You may or may not want to know if your baby has a health condition. If you decide to have a diagnostic test, you can learn more about your baby’s condition and how to care for your baby after he’s born. You also can make plans to give birth in a hospital that can give your baby special medical care.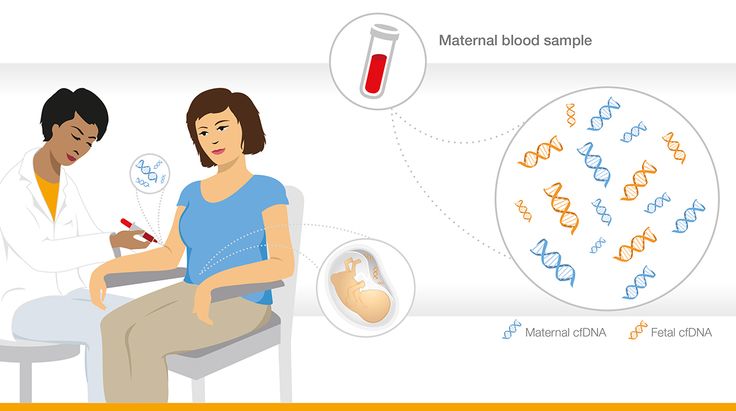
What prenatal tests do you get all through pregnancy?
You can get these prenatal tests several times during pregnancy:
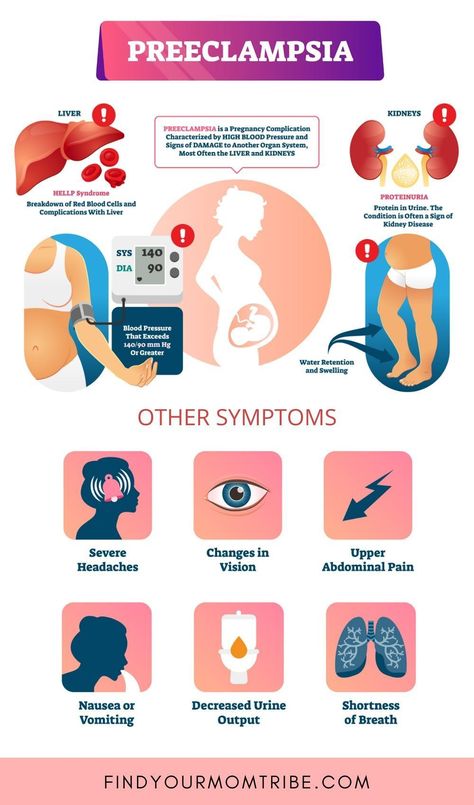
- Blood pressure check. Your provider checks your blood pressure to make sure you don’t have preeclampsia. Preeclampsia is high blood pressure that can happen after the 20th week of pregnancy. Preeclampsia can cause serious problems during pregnancy.
- Urine test. Your provider checks your urine for infections, like a bladder or kidney infection, and other conditions, like preeclampsia. Having protein in your urine may be a sign of preeclampsia.
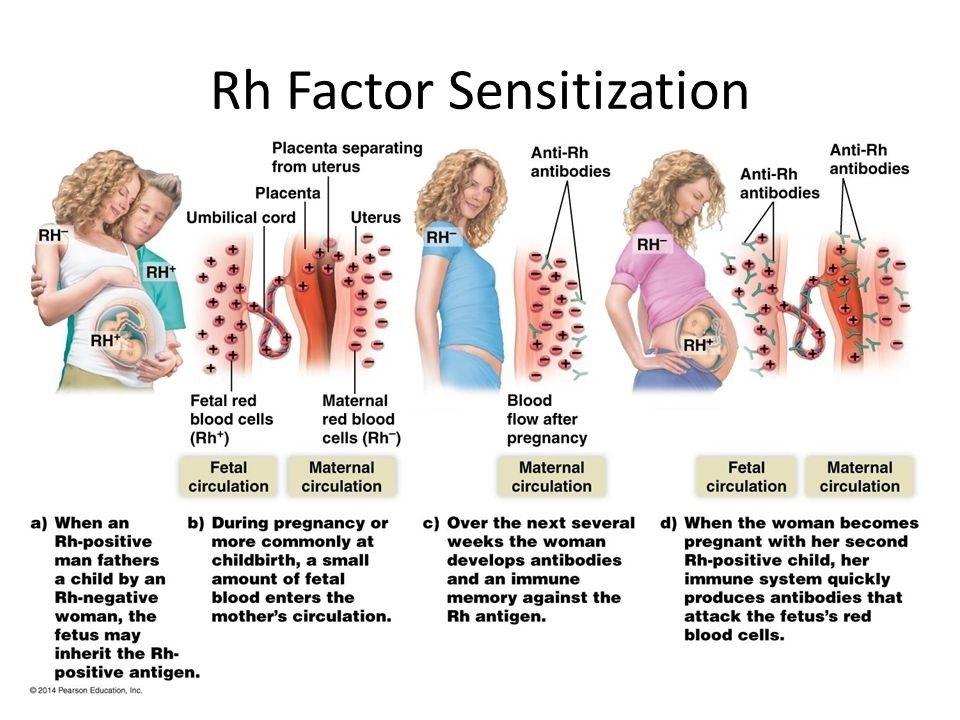
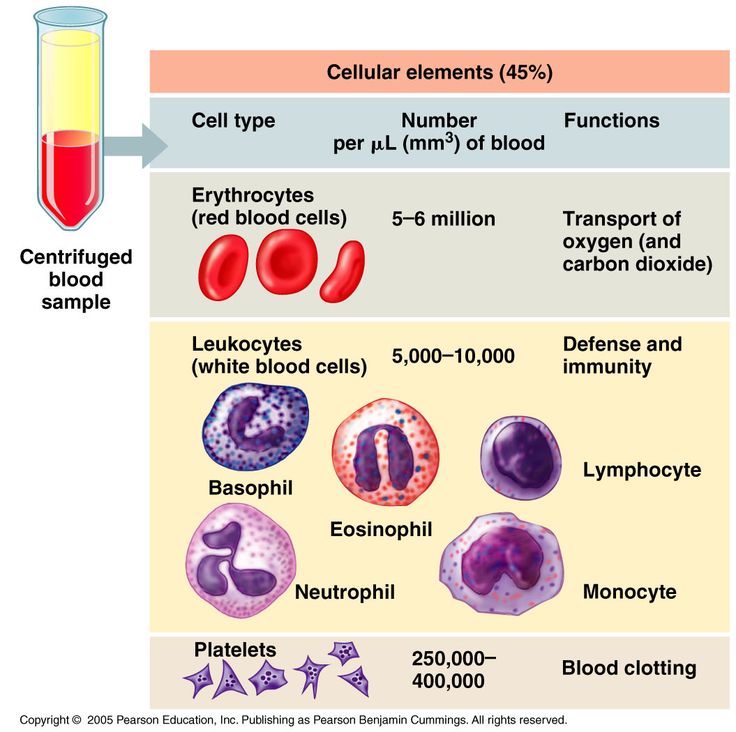
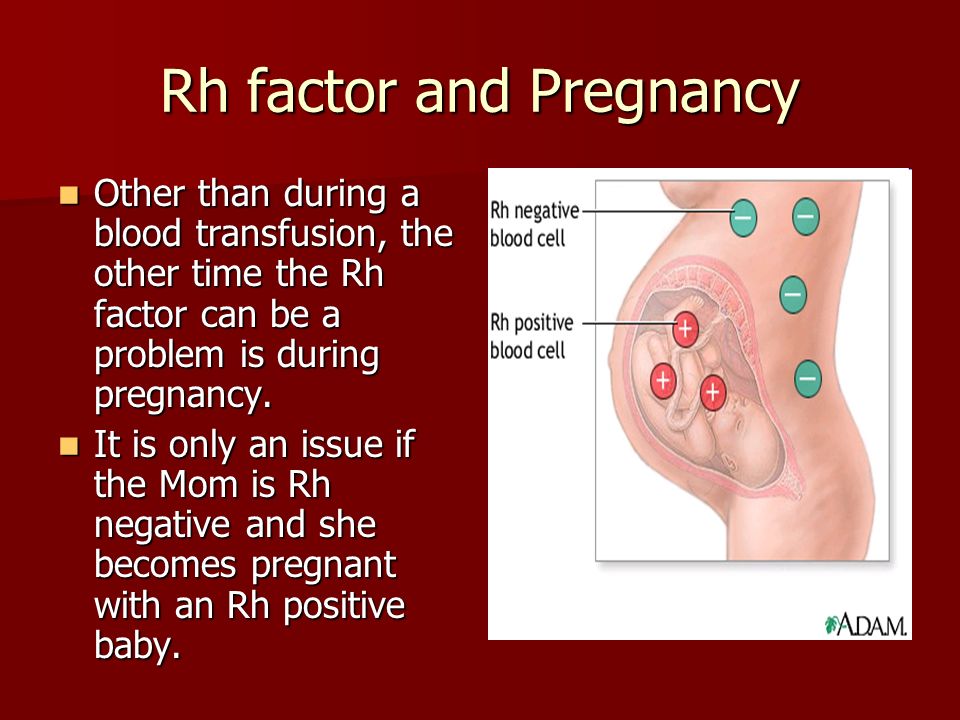
- Blood tests. Your provider checks your blood for certain infections, like syphilis, hepatitis B and HIV. Your blood test is also used to find out your blood type and Rh factor and to check for anemia. Anemia is when you don't have enough healthy red blood cells to carry oxygen to the rest of your body. Rh factor is a protein that most people have on their red blood cells.
 If you don’t have it and your baby does, it can cause Rh disease in your baby. Treatment during pregnancy can prevent Rh disease.
If you don’t have it and your baby does, it can cause Rh disease in your baby. Treatment during pregnancy can prevent Rh disease.
Your provider also checks your weight at each prenatal care checkup to make sure you’re gaining the right amount.
What prenatal tests are done in the first trimester?
You may have several tests in your first trimester (months 1, 2 and 3). Talk to your provider to find out which tests are right for you.
- Carrier screening for genetic conditions. This screening test checks your blood or saliva to see whether you’re a carrier of certain genetic conditions that could affect your baby. If you’re a carrier, it means you don’t have the condition yourself but you do have a genetic change that you can pass to your baby. If both you and your partner are carriers of the same condition, there is a greater risk that your baby will have the condition. Carrier screening can be done before pregnancy or during the early weeks of pregnancy.
 If results show that you or your partner is a carrier, you may be able to find out if your baby has the condition or is a carrier of the condition. Talk to your health care provider about what carrier screening tests might be right for you.
If results show that you or your partner is a carrier, you may be able to find out if your baby has the condition or is a carrier of the condition. Talk to your health care provider about what carrier screening tests might be right for you. - Cell-free fetal DNA testing (also called noninvasive prenatal screening or testing). This screening test checks your blood for your baby’s DNA. The DNA is examined for certain genetic conditions, such as Down syndrome. This test is done after 9 weeks of pregnancy. Your provider may recommend the test if an ultrasound shows your baby may have a birth defect or if you've already had a baby with a birth defect. If you have this test, your provider may recommend you have a diagnostic test, like amniocentesis, to confirm the results.
- Chorionic villus sampling (also called CVS). This diagnostic test checks tissue from the placenta to see if your baby has a genetic condition. CVS is done at 10 to 13 weeks of pregnancy.
 Your provider may want you to have CVS if you’re older than 35, if there’s a history of genetic conditions in your family or if your first-trimester screening shows that your baby is at increased risk for birth defects.
Your provider may want you to have CVS if you’re older than 35, if there’s a history of genetic conditions in your family or if your first-trimester screening shows that your baby is at increased risk for birth defects. - Early ultrasound (also called first-trimester ultrasound). Ultrasound uses sound waves and a computer screen to make a picture of your baby inside the womb. Your provider may use early ultrasound to make sure that you’re pregnant or to date your pregnancy so you know how far along in pregnancy (how many weeks) you are.
- First-trimester screening. This screening test includes a blood test and an ultrasound to see if your baby may be at risk for some birth defects, like Down syndrome and heart defects. The test usually is done at 11 to 13 weeks of pregnancy.
What tests are done in the second trimester?
Your provider may offer you these prenatal tests in your second trimester (months 4, 5 and 6 of pregnancy):
- Maternal blood screening (also called quad screen).
 This screening test checks your blood to see if your baby may be at risk for some birth defects, such as Down syndrome. It’s called a quad screen because it measures 4 substances in your blood: alpha-fetoprotein (AFP), estriol, human chorionic gonadostropin (hCG) and inhibin A. The test is done at 15 and 22 weeks of pregnancy.
This screening test checks your blood to see if your baby may be at risk for some birth defects, such as Down syndrome. It’s called a quad screen because it measures 4 substances in your blood: alpha-fetoprotein (AFP), estriol, human chorionic gonadostropin (hCG) and inhibin A. The test is done at 15 and 22 weeks of pregnancy. - Ultrasound. Your health care provider will perform an ultrasound between 18 and 22 weeks of pregnancy. The ultrasound will check your baby’s growth and development and check for any birth defects.
- Amniocentesis. During amniocentesis, a sample of amniotic fluid is taken from around the baby. The fluid is tested to see if your baby has a birth defect or genetic condition. The test usually is done at 15 to 20 weeks of pregnancy. Your provider may want you to have amniocentesis if you’re older than 35, if there is a history of genetic conditions in your family, or if your first-trimester screening shows that your baby is at increased risk for birth defects.

- Glucose screening. This screening test checks to see if you may have gestational diabetes. This is a kind of diabetes that some women get during pregnancy. You get this test at 24 to 28 weeks of pregnancy.
What tests are done during the third trimester?
In your last trimester (months 7, 8 and 9 of pregnancy), your provider does a test for group B strep (also called GBS). Group B strep is an infection you can pass to your baby during birth. The test checks fluid from your cervix to see if you have GBS. You get this test at 35 to 37 weeks of pregnancy.
What are kick counts and how do you do them?
Kick counts (also called fetal movement counts) is a way for you to track how often your baby moves. By about 5 months (20 weeks) of pregnancy, you should start to feel your baby move in your belly. Your baby can turn from side to side and sometimes head over heels. Tell your provider if:
- You’re at about 20 weeks of pregnancy and haven’t felt your baby move.
- You’re worried that your baby isn’t moving.
- You notice a change in how often your baby moves, especially if movement decreases.
Your provider may ask you to do kick counts to see when and how often your baby moves. Here are 2 ways to do kick counts:
- Every day, time how long it takes for your baby to move 10 times. If it takes longer than 2 hours, tell your provider.
- See how many movements you feel in 1 hour. Do this 3 times each week. If the number changes, tell your provider.
You can do kick counts even into your third trimester. If your provider is concerned about your baby’s movements, they may do other tests to check on your baby’s health.
More information
- Einstein Victor Center for the Prevention of Jewish Genetic Diseases
- Genetic Alliance
- JScreen at Emory University
- National Organization for Rare Disorders (NORD)
- National Society of Genetic Counselors
Last reviewed: September, 2020
Screening for the detection of congenital diseases of the fetus during pregnancy
Category: Reminders for the population .
Pregnancy screening is a whole range of studies that allows parents and doctors to get the most complete information about the health of an unborn baby. Screening reveals many congenital and physical characteristics. How and when is pregnancy screening done?
What is pregnancy screening and why is it done
Screening during pregnancy is a complex of examinations, which includes ultrasound and biochemical analysis of venous blood for hormones. As a rule, screening is carried out three times - in the first, second and third trimester.
Early detection of pathologies is very important. This makes it possible to start treating genetic diseases as early as possible and, if not completely cure them, then at least stop the symptoms as much as possible. If the doctor notices any abnormalities during the examination, the pregnancy is monitored especially carefully, which makes it possible to prevent the development of complications or premature birth.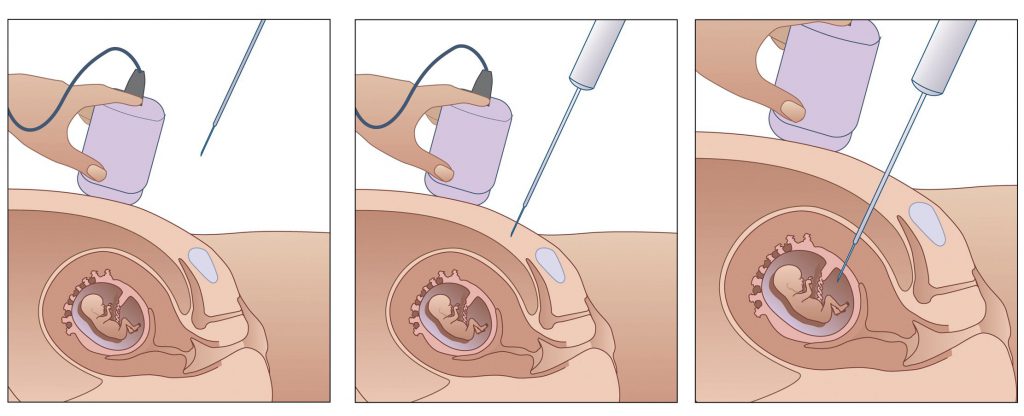 If the detected pathologies turn out to be too severe and incompatible with life, the doctor will refer the patient to terminate the pregnancy for medical reasons. nine0003
If the detected pathologies turn out to be too severe and incompatible with life, the doctor will refer the patient to terminate the pregnancy for medical reasons. nine0003
Pregnancy screening is harmless for both mother and baby. This is a fairly accurate study, although it should be clearly understood that it does not give a 100% guarantee. The accuracy of screening depends on many factors - the professionalism of the researchers, the woman's compliance with the rules for preparing for the examination, and other factors.
First pregnancy screening
The first screening during pregnancy is carried out between the 11th and 13th weeks. It makes no sense to undergo this examination earlier - before the 11th week of pregnancy, many indicators are practically indeterminate. nine0003
The study includes two medical tests - an ultrasound and a blood test.
ultrasound
With the help of ultrasound, the doctor determines the exact gestational age, evaluates the baby's physique, its dimensions (head circumference, limb length, height), the work of the heart muscle, the symmetry of the brain, the volume of amniotic fluid, the structure and size of the placenta, as well as the condition and tone of the uterus. For each of these parameters, there are normal indicators with which the doctor will compare the results. For an 11-13 week pregnancy, these rates are:
For each of these parameters, there are normal indicators with which the doctor will compare the results. For an 11-13 week pregnancy, these rates are:
- KTP (coccygeal-parietal size, that is, the length of the fetus from the crown to the tailbone) is 43–65 mm. If this figure is more than normal, then the child will be large. A downward deviation indicates slow development (the reason for this state of affairs is often a hormonal imbalance or infectious diseases suffered by the expectant mother), genetic pathologies or fetal death (in this case, the heart will not be auscultated). However, this may also be due to a banal mistake in determining the timing of pregnancy. nine0030
- BDP (biparietal size, that is, the distance from the temple to the temple) - 17-24 mm. A high BDP means a large fetus, but only on the condition that all other indicators say the same. Otherwise, we can talk about a herniated brain or hydrocephalus. Low BDP indicates slow brain development.
- TVP (collar space thickness) - 1.6–1.7 mm. Deviation from this norm (TVP above 3 mm) is considered a sign of some severe chromosomal pathologies - Down syndrome, Edwards syndrome, etc. However, one should not panic ahead of time - no one will make such a serious diagnosis only on the basis of TVP. To confirm, you need to take a blood test for hormones and take a biopsy of the outer dense shell of the embryo for further research. nine0030
The length of the nasal bone is 2–4.2 mm. Too small a nose bone can indicate pathology or simply that the baby's nose will be snub-nosed. HR (heart rate) - 140-160 beats per minute. A small (up to 40 beats per minute) deviation in one direction or another is considered a variant of the norm.
The size of the chorion, amnion and yolk sac. The chorion is the outer shell of the fetus, which will eventually become the placenta. If it is located on the lower wall of the uterus, they speak of chorion previa. This is a potentially dangerous situation, fraught with miscarriage, and in this case, bed rest is recommended for the pregnant woman. nine0003
nine0003
The amnion is the inner membrane that holds the amniotic fluid. The normal volume of amniotic fluid at 11–13 weeks is 50–100 ml.
The yolk sac is an embryonic organ that, in the first weeks of a fetus's life, plays the role of some internal organs that will be formed later. By the time of the first screening, the yolk sac should practically disappear (then the examination form will indicate “not visualized”). If its size is about 6 mm, then the fetus may have certain pathologies. nine0003
Cervix. Normally, its length by the time of the first screening is 35–40 mm. A shorter cervix means a risk of preterm labor.
Ultrasound is performed in two ways - transabdominal, in which the sensor of the ultrasound machine is located on the abdomen, and transvaginal, in which it is inserted into the vagina. Transvaginal ultrasound provides more complete and accurate information, but it is usually performed only in the first trimester. This method is usually used when examining overweight women, since the fat layer in the abdomen does not allow the fetus and uterus to be examined in detail. nine0003
nine0003
It is necessary to properly prepare for an ultrasound. Before a transabdominal ultrasound, it is advised to drink about a liter of water so that the bladder is full at the time of the examination - then the uterus will shift slightly towards the abdomen and the picture will be clearer. With transvaginal ultrasound, the degree of fullness of the bladder does not matter, however, before the examination, it is better to go to the toilet - it will be more comfortable. Before the examination, you need to take a shower or freshen up with wet wipes. The accumulation of gases can distort the results of ultrasound, no matter what method it is carried out. Therefore, expectant mothers suffering from flatulence are advised the day before the examination to take remedies for flatulence and not eat anything that produces gas. nine0003
Blood test
Biochemical screening, also called a dual test, is done to determine the level of two hormones (hence the name) - free b-hCG and PAPP-A.
- b-hCG (human chorionic gonadotropin) begins to be produced from the first days of pregnancy. Its amount gradually increases until about the 9th week, and then begins to gradually decrease. On average, for a period of 11–13 weeks, 50,000–55,000 mIU / ml is considered the norm. An elevated level of hCG may indicate a multiple pregnancy, or, in the worst case, genetic pathologies of the fetus or the presence of diabetes in the mother. Reduced hCG is typical of miscarriage, ectopic pregnancy, fetal death, or certain malformations (Patau syndrome and Edwards syndrome). nine0030
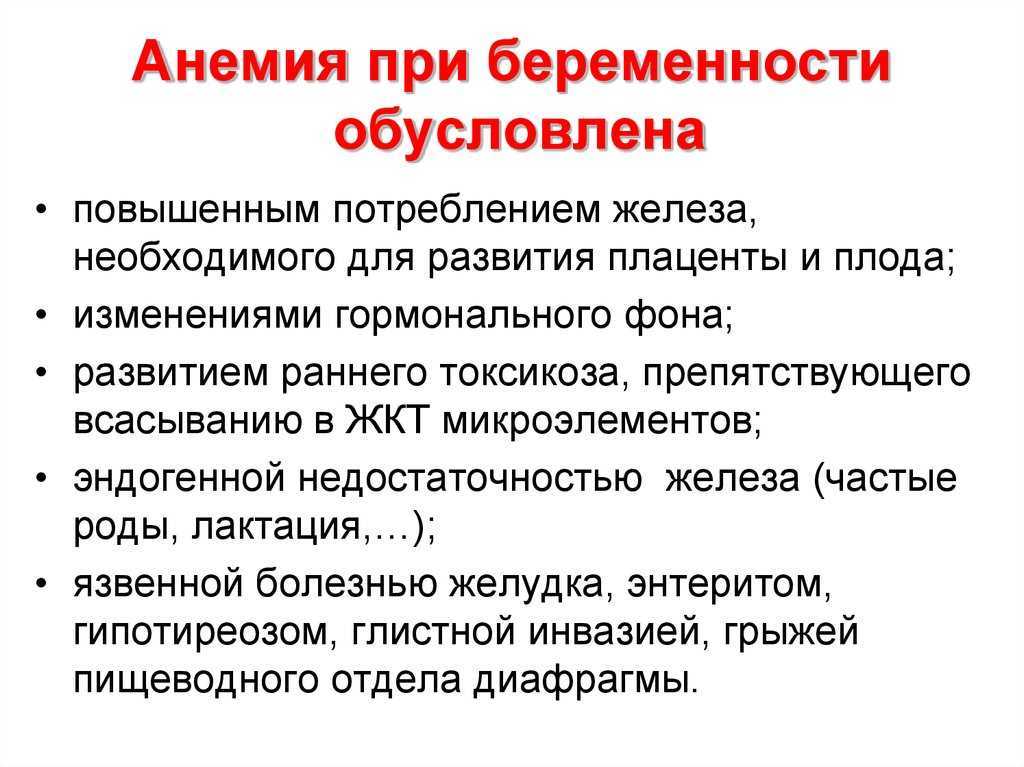
- PAPP-A is an A-plasma protein. The content rate for a period of 11–13 weeks is 0.79–6.01 mU / l. Low PAPP-A is a sign of chromosomal pathologies such as Down syndrome and Edwards syndrome, fetal death and miscarriage, fetal malnutrition (underweight) and preeclampsia.
- A high PAPP-A is a sign of multiple pregnancies, large fetuses, or a low placenta.
In order for the blood test to give the most accurate information, it must be taken on an empty stomach, at least 8 hours after the last meal.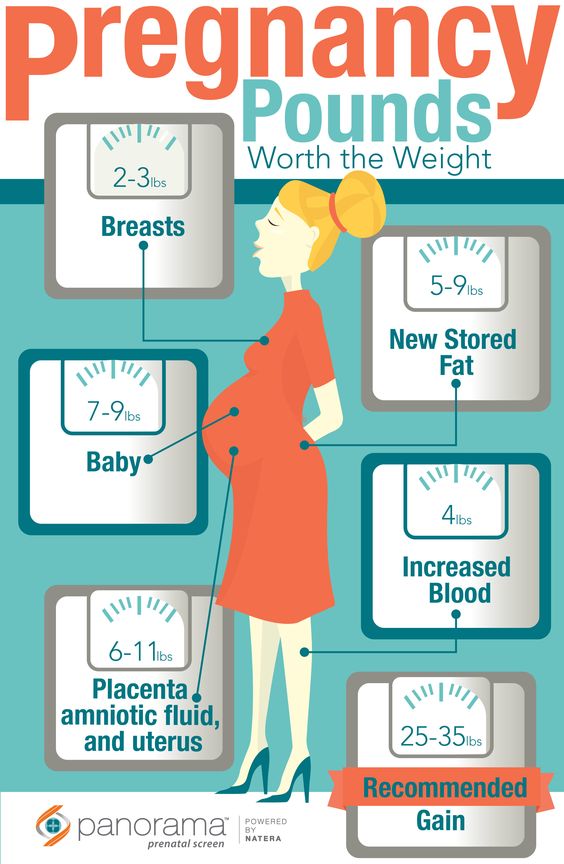 2-3 days before the analysis, you should refrain from fried, fatty, spicy, smoked foods, chocolate, nuts, seafood. It is also recommended not to have sexual intercourse. All this is not so significant, but it can affect the result in one way or another. nine0003
2-3 days before the analysis, you should refrain from fried, fatty, spicy, smoked foods, chocolate, nuts, seafood. It is also recommended not to have sexual intercourse. All this is not so significant, but it can affect the result in one way or another. nine0003
Second pregnancy screening
The second screening during pregnancy is carried out at 16-20 weeks. Like the first one, it consists of the same two stages - ultrasound and blood test.
ultrasound
This time, the doctor determines not only the size, but also the position of the fetus and its bone structure, the condition of the internal organs and the place of attachment of the umbilical cord, as well as the volume of amniotic fluid. Here are the approximate main indicators of the norm for a period of 16-20 weeks:
- BPR - 26–56 mm.
- DBK (length of the femur) - 13-38 mm.
- DPC (length of the humerus) - 13-36 mm.

- OG (head circumference) - 112-186 mm.
IAF (amniotic fluid index, that is, the volume of amniotic fluid) - 73-230 mm. Oligohydramnios can adversely affect the condition of the child's bone structure and the development of his nervous system.
Localization of the placenta. There is some risk only when the placenta is located on the anterior wall of the uterus - with such localization, detachment of the placenta is possible. nine0003
Umbilical cord. One of the most important parameters is the place of attachment of the umbilical cord. Marginal, split or sheath attachment is fraught with fetal hypoxia and difficulties during childbirth, often it becomes an indication for caesarean section. The umbilical cord is fed through 2 arteries and 1 vein, although sometimes only one artery is available. This can cause fetal hypoxia, heart disease, disorders in the child’s cardiovascular system, and cause a baby’s low body weight. However, if all other analyzes and examinations do not show deviations from the norm, you should not worry. nine0003
nine0003
Cervix. The length of the cervix at this time should be 40–45 mm. A short cervix means a threatened miscarriage.
Visualization. Unsatisfactory visualization can be caused both by the peculiarities of the position of the fetus or the excess weight of the expectant mother, and by edema or hypertonicity of the uterus.
Blood test
As during the first screening, during the second, a blood test for b-hCG is taken, the level of free estriol and AFP is also checked. Here are the norms for their content at the 16th-20th weeks of pregnancy:
- b-hCG - 4.67-5-27 ng / ml.
- Free estriol is a hormone whose level can be used to judge the state of the placenta. The norm is 1.17–3.8 ng / ml. Elevated estriol is characteristic of multiple pregnancy or a large fetus. Reduced - for threatened miscarriage, placental insufficiency, anencephaly and Down's syndrome.
- AFP is a protein that is produced in the gastrointestinal tract of the fetus.
 Norm - 15-27 U / ml. A slightly lower AFP may mean that the gestational age was determined incorrectly (slightly underestimated). If the AFP is very low, the cause may be Edwards or Down syndrome, the threat of miscarriage or fetal death. High AFP is characteristic of neural tube pathologies, esophageal atresia, Meckel's syndrome. High AFP is also possible in women who have had an infectious disease during pregnancy. nine0030
Norm - 15-27 U / ml. A slightly lower AFP may mean that the gestational age was determined incorrectly (slightly underestimated). If the AFP is very low, the cause may be Edwards or Down syndrome, the threat of miscarriage or fetal death. High AFP is characteristic of neural tube pathologies, esophageal atresia, Meckel's syndrome. High AFP is also possible in women who have had an infectious disease during pregnancy. nine0030
Third pregnancy screening
The third screening during pregnancy is carried out at the 30th-43rd week. Based on the results of this screening, the doctor decides on the need for a caesarean section or the possibility of a natural birth. The basis of the third screening is the same ultrasound. Sometimes dopplerography is prescribed - a study of the work of blood vessels. Here are the approximate norms for a given gestational age:
ultrasound
nine0028 The thickness of the placenta is 23. 9–43.8. Too thin placenta is not a particularly dangerous deviation from the norm. The reason may be the miniature physique of a woman, her infectious diseases, hypertension. An excessively thick placenta is a sign of anemia, diabetes, Rh conflict. Such an indicator as the degree of maturity of the placenta is also taken into account - at a period of 30–35 weeks, the 1st degree of maturity is considered normal. With too rapid thickening and aging of the placenta, premature birth, fetal hypoxia and its slow development are possible. nine0003
9–43.8. Too thin placenta is not a particularly dangerous deviation from the norm. The reason may be the miniature physique of a woman, her infectious diseases, hypertension. An excessively thick placenta is a sign of anemia, diabetes, Rh conflict. Such an indicator as the degree of maturity of the placenta is also taken into account - at a period of 30–35 weeks, the 1st degree of maturity is considered normal. With too rapid thickening and aging of the placenta, premature birth, fetal hypoxia and its slow development are possible. nine0003
Prenatal screening is very important and should not be neglected. Timely detected pathologies and deviations from the norm can save the life and health of your child. This is worth remembering, especially for those parents who refuse to be examined out of fear of learning that the development of the baby is not going according to plan.
Frequently asked questions about biochemical screening of pregnant women
What tests are performed on pregnant women?
Currently, two main types of examinations are recommended to pregnant women in St.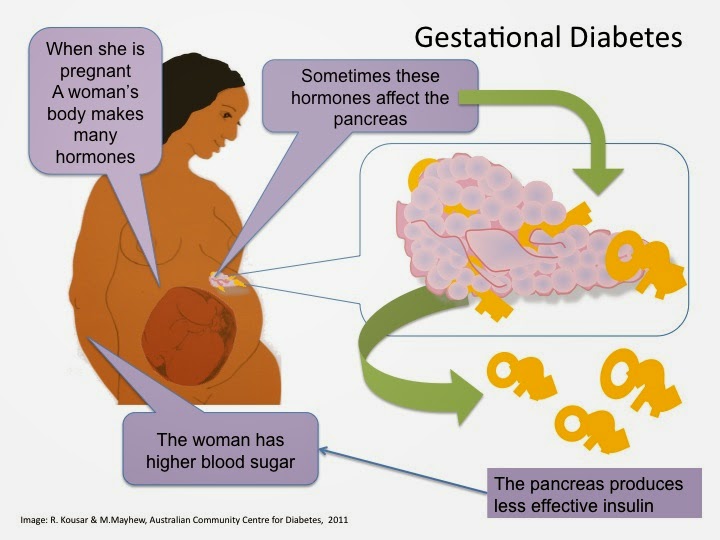 Petersburg:
Petersburg:
- analysis for PAPP-A and beta-hCG in the period of 9-13 weeks
- analysis for AFP and hCG.
Should I do a “triple test”?
Some private laboratories use the so-called "triple test", using kits that, in addition to AFP and hCG, have added the determination of the concentration of another hormone - unconjugated estriol. According to modern data, its assessment for clarifying the risks of fetal chromosomal pathology has too little weight and is highly dependent on many other factors of the woman's condition, which is not significant for calculating risks for fetal chromosomal pathology. If the results of the “double” test reveal an increased risk for you, it is better to contact a geneticist and understand the situation, taking into account a professional clinical assessment of the test results. nine0003
How important is it to accurately indicate the weight of a pregnant woman when taking blood for “fetal proteins”?
Each woman's weight must be recorded on the examination referral. In the absence of such information, the risk can be calculated "according to the average" weight of pregnant women in this period - 60 kg.
In the absence of such information, the risk can be calculated "according to the average" weight of pregnant women in this period - 60 kg.
All women are different - there are pregnant women weighing 45 and 145 kg. For a more accurate assessment of the results, an amendment is introduced in accordance with the "weight category". But absolute accuracy is not required here - individual grams will not change the calculations. An individual approach is important. Therefore, we always measure a woman's weight before taking tests. nine0003
I took a blood test for fetal proteins, as the doctor prescribed them immediately after taking them, now I'm worried, so I had a hearty breakfast in the morning. Will this affect the outcome of the study? Can I retake blood on an empty stomach?
Don't worry! Unlike most "adult" tests that are sensitive to food intake, the measurement of the amount of any proteins entering the mother's blood from the fetus is not dependent on the time of the meal. The most important thing here is to know exactly the gestational age established by ultrasound. It makes no sense to retake the analysis. And it is very important for pregnant women to eat breakfast and continue to eat more often during the day than usual. nine0003
The most important thing here is to know exactly the gestational age established by ultrasound. It makes no sense to retake the analysis. And it is very important for pregnant women to eat breakfast and continue to eat more often during the day than usual. nine0003
In clinics where an individual approach to the examination of pregnant women is possible, and of course, in our Fetal Medicine Center, blood for screening tests can be donated throughout the working day.
Which test is better - PAPP-A and beta-hCG or AFP and hCG?
At present, the first one has the absolute advantage. It has been proven that it is more specific for assessing risks for chromosomal pathology, including Down syndrome. Its important advantage is that it is carried out in the first trimester, you can donate blood from the age of 9weeks of pregnancy (determined by the size of the fetus on ultrasound). The most optimal terms for this analysis are 9-12 weeks. A study period of up to almost 14 (13 weeks 6 days) is allowed, but the reliability of the risk assessment will be lower.
If you have completed a full first trimester test, performed an ultrasound and received a conclusion from a geneticist that the fetus is at low risk for chromosomal abnormalities, testing for AFP and hCG is not worth it.
In special cases, after the first screening, a test for AFP and hCG is prescribed as an additional test on the recommendation of a geneticist. nine0003
If you missed the first screening test, then, of course, you need to donate blood at least for the second one within 15-18 weeks.
I would like to emphasize that, on the recommendation of international experts in prenatal diagnostics, analysis for PAPP-A and beta-hCG in a period of 9-12 weeks is recommended for all pregnant women at any age.
I went through the IVF procedure and used a donor cell, since my cells do not mature at 46 years old. Now 12 weeks. How do I correctly pass a biochemical test? nine0016
You urgently need to donate blood for PAPP-A and beta-hCG and perform an ultrasound. From your age, the IVF procedure itself does not change the amount of proteins. And the risk "by proteins" will be assessed depending on certain concentrations.
From your age, the IVF procedure itself does not change the amount of proteins. And the risk "by proteins" will be assessed depending on certain concentrations.
But the computer program calculates the "combined" risks - by proteins, by ultrasound and by the age of the woman, more precisely, by the "age of the egg." Accordingly, for this analysis, the age of the egg donor must be indicated in the calculation referral. If you do not know it exactly, you can calculate by low age risk, since all donors have age restrictions for participating in the IVF program. If you have already been calculated according to your age, don't worry, we can reassess the risks taking into account real data and issue you a Medical Genetic Conclusion based on the results of prenatal studies. nine0003
Doctors of the Fetal Medicine Center are one of the leading specialists in prenatal diagnostics, candidates of medical sciences, doctors of the highest categories with a narrow specialization and extensive experience in prenatal medicine.