Headaches and pregnancy first trimester
What Causes Them and What You Can Do
If you’re pregnant and having headaches, you’re not alone. A medical review reports that 39 percent of pregnant and postpartum women have headaches.
Though during pregnancy you may have a different kind of headache than you usually do, most headaches during pregnancy aren’t harmful.
Headache pain during the first trimester of pregnancy may happen for different reasons than headaches in the second or third trimester. In some cases, headache pain may be a sign of other health problems during pregnancy.
Tell your doctor about any headache you have during, before, and after pregnancy. Keep a journal to record how often you have headaches and how serious the pain is. Additionally, record any other symptoms you have.
Most headaches during pregnancy are primary headaches. This means that the headache pain happens by itself. It’s not a sign or symptom of another disorder or a complication in the pregnancy. Primary headaches include:
- tension headaches
- migraine attacks
- cluster headaches
About 26 percent of headaches during pregnancy are tension headaches. Tell your doctor if you have chronic headaches or migraine during pregnancy or if you have a history of migraine.
Some women with a history of migraine get fewer migraine attacks during pregnancy. Migraine has also been linked to complications that happen later in pregnancy or after the birth of your baby.
Secondary headaches are a caused by a complication in the pregnancy, such as high blood pressure.
Headache pain may vary from one person to the next. You may have:
- dull ache
- throbbing or pulsating pain
- severe pain on one or both sides
- sharp pain behind one or both eyes
Migraine pain may also include:
- nausea
- vomiting
- seeing lines or flashes of light
- blind spots
First trimester
Tension headaches are common in the first trimester of your pregnancy. This may happen because your body is undergoing several changes at this time. These changes may trigger headache pain:
- hormonal changes
- higher blood volume
- weight changes
Common causes of headache pain during the first trimester of pregnancy also include:
- dehydration
- nausea and vomiting
- stress
- lack of sleep
- caffeine withdrawal
- poor nutrition
- low blood sugar levels
- too little physical activity
- sensitivity to light
- changes in vision
Some foods may also cause headaches.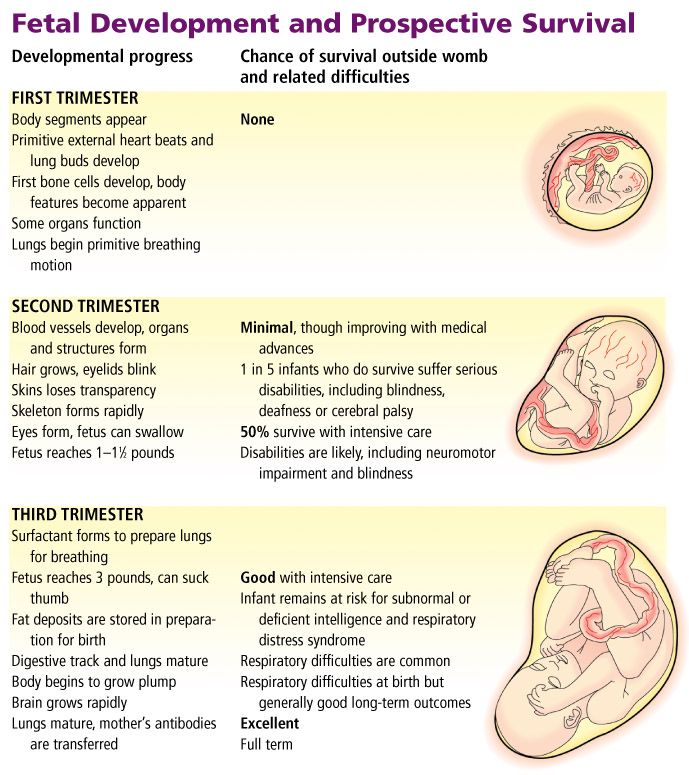 Your trigger foods may change during pregnancy. Common foods that may cause headaches in some people include:
Your trigger foods may change during pregnancy. Common foods that may cause headaches in some people include:
- dairy
- chocolate
- cheese
- yeast
- tomatoes
Second and third trimester
Headaches during your second and third trimester may have different causes. These include:
- extra weight
- posture
- too little sleep
- diet
- muscle strain and tightness
- high blood pressure
- diabetes
High blood pressure
Headaches during your second or third trimester of pregnancy may be a sign that you have high blood pressure. About 6 to 8 percent of pregnant women ages 20 to 44 in the United States have high blood pressure.
The Centers for Disease Control and Prevention (CDC) warns that this treatable condition can cause serious complications for both mother and baby. This is most common after week 20 of pregnancy.
If you’re pregnant, high blood pressure can raise the risk of:
- stroke
- preeclampsia
- eclampsia
- low oxygen flow to the baby
- preterm delivery, before 37 weeks
- placental abruption
- low baby birth weight, which is less than 5 pounds, 8 ounces
Treatment for hypertension during pregnancy
Your doctor may prescribe medication to treat your high blood pressure. You’ll also need to cut down on salt and add more fiber to your daily diet. Regular exercise is also very important to help balance your blood pressure.
You’ll also need to cut down on salt and add more fiber to your daily diet. Regular exercise is also very important to help balance your blood pressure.
Other causes of headache during pregnancy include common infections and more serious illnesses:
- sinus infection
- low blood pressure
- blood clots
- bleeding
- sickle cell anemia
- brain tumor
- aneurysm
- stroke
- heart conditions
- meningitis or encephalitis
Talk to your doctor before taking your regular headache pain medication during pregnancy. Don’t take aspirin and ibuprofen (Advil, Motrin etc.).
The CDC warns that these pain relief drugs can be harmful to your growing baby, especially if taken during the first trimester. Many women may take acetaminophen (Tylenol) during pregnancy. However, some studies suggest there may be effects from taking acetaminophen as well.
Your doctor can recommend alternative medications to treat headache during pregnancy and natural headache remedies, such as:
- drinking plenty of water
- rest
- ice pack
- heating pad
- massage
- exercise and stretching
- essential oils, such as peppermint, rosemary, and chamomile
When to see your doctorSee your doctor if you have any headache pain at all during pregnancy.
Get urgent medical attention if you have:
- fever
- nausea and vomiting
- blurred vision
- severe pain
- headache that lasts longer than a few hours
- frequent headache pain
- fainting
- seizure
Your doctor may recommend tests and scans to find out the cause of your headaches. These include:
- checking your blood pressure
- blood test
- blood sugar test
- vision test
- ultrasound of the head and neck
- heart or head scan
- checking eye health with a scope
- spine puncture
Headache pain during pregnancy is common. You may have tension headaches during your first trimester of pregnancy. This may happen because of the many changes that you’re going through in a short period.
Headache pain may happen in the second and third period of your pregnancy for other reasons. Some causes of headaches in your mid to late pregnancy may be serious.
High blood pressure is a serious cause of headache pain during pregnancy.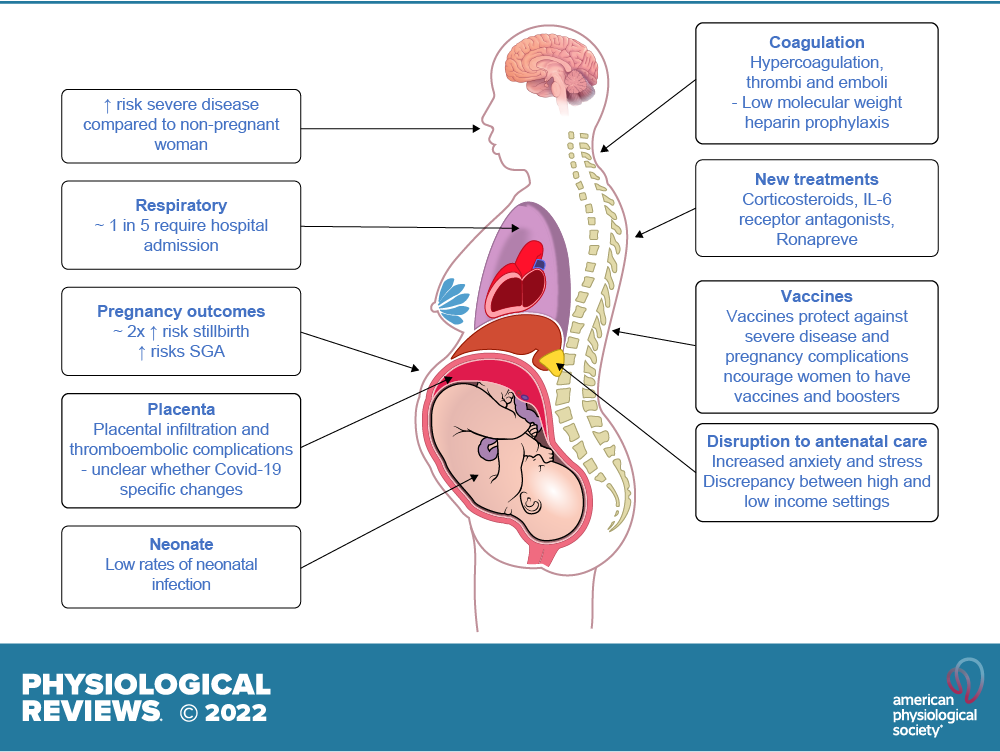 You can have high blood pressure at any time in your pregnancy. You may not have any symptoms at all. Check your blood pressure at least once a day with a home monitor.
You can have high blood pressure at any time in your pregnancy. You may not have any symptoms at all. Check your blood pressure at least once a day with a home monitor.
Tell your doctor if you have headaches at any time in your pregnancy. Let your doctor know right away if you have a personal or family history of migraine, high blood pressure, seizures or diabetes.
Take all medications and treatment exactly as prescribed by your doctor. Follow all diet and exercise advice carefully. See your doctor for all follow-up and regular check-ups. Most causes of headaches during pregnancy are treatable or preventable with the right care.
For more pregnancy guidance and weekly tips tailored to your due date, sign up for our I’m Expecting newsletter.
Headaches during pregnancy | Pregnancy Birth and Baby
Headaches during pregnancy | Pregnancy Birth and Baby beginning of content9-minute read
Listen
If you have a severe headache during pregnancy that is not usual for you, seek medical help immediately.
Key facts
- It’s common to get mild headaches in the first few months of pregnancy because of hormonal changes.
- If you usually suffer from migraines, they may get better, worse, change or stay the same when you’re pregnant.
- Headaches during pregnancy may be triggered by poor sleep, stress, dehydration, low blood sugar or eye strain.
- If your headache doesn’t settle with simple measures (for example, rest and rehydration), you can take paracetamol.
- A headache after 20 weeks can be a sign of pre-eclampsia, which is a serious pregnancy condition that needs medical attention – see your doctor or midwife.
Does pregnancy cause headaches?
Many people get mild headaches when they are pregnant. Headaches can often be triggered by a change in hormones. They are more common in the first few months of pregnancy.
If you usually suffer from migraines, you might notice a change when you’re pregnant.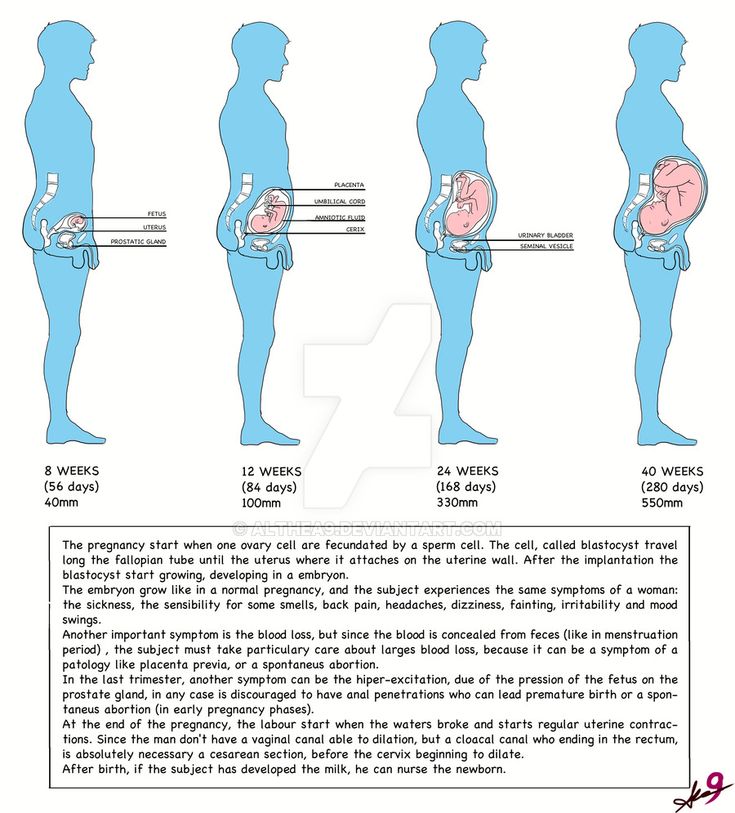 There’s a good chance that your migraines will improve after the first trimester. This may be because your oestrogen level starts to stabilise. However, some people don’t notice a change, or may get worse migraines during pregnancy. You also might notice different changes from one pregnancy to the next.
There’s a good chance that your migraines will improve after the first trimester. This may be because your oestrogen level starts to stabilise. However, some people don’t notice a change, or may get worse migraines during pregnancy. You also might notice different changes from one pregnancy to the next.
Headaches can develop for many different reasons — it’s not always because of pregnancy hormones.
Why else might I get headaches during pregnancy?
Besides hormonal changes, there are many triggers that cause headaches in general, but might occur more often when you’re pregnant, such as:
- not getting enough sleep
- withdrawal from caffeine — such as in coffee, tea or cola drinks
- low blood sugar from not eating regularly
- dehydration
- feeling stressed, anxious or depressed
- eye strain — especially as your eye muscles relax during pregnancy
Many of these triggers can cause tension headaches, which are very common. The pain is usually mild and on both sides of your head.
The pain is usually mild and on both sides of your head.
Some of these triggers can cause migraines, which are more severe and mostly occur on one side of your head. If you have migraines, you might also feel sick or vomit and be sensitive to light or sound.
Pre-eclampsia
If you start getting frequent headaches after 20 weeks of pregnancy, this could be a sign of a more serious pregnancy condition called pre-eclampsia. Pre-eclampsia is when you have high blood pressure that affects your kidneys and sometimes other parts of your body. If you have a pre-eclampsia headache, you may find that simple pain-relieving medicines like paracetamol don’t help.
It’s very important to tell your doctor or midwife if you are getting headaches in the second half of pregnancy, or if your headaches are very severe.
If you have a severe headache during pregnancy, call your doctor or midwife. It could be something more serious.
Health conditions
Just like when you’re not pregnant, a headache can sometimes be a sign of other health conditions, including:
- infections, such as an ear infection or flu
- sinusitis
- problems with your teeth
- an aneurysm or stroke
What can I do to treat a headache when I’m pregnant?
If you have a headache, you could try:
- having a nap, or resting with your eyes closed
- drinking water
- having something to eat
- putting a cold or heat pack on your forehead or the back of your neck
- asking someone to give you a gentle neck massage
If you need to take medicine for pain relief, paracetamol is safe during pregnancy. Pain-relieving medicines can actually cause headaches if you take them too often, so don’t take paracetamol more than 3 times a week.
Pain-relieving medicines can actually cause headaches if you take them too often, so don’t take paracetamol more than 3 times a week.
When you’re pregnant, avoid anti-inflammatories such as ibuprofen or aspirin and medicines that contain caffeine.
What can I do to prevent headaches during pregnancy?
If you find you are getting mild headaches often, it’s a good idea to:
- getting more sleep
- drink at least 8 cups of water a day
- go to pregnancy yoga classes or do some other type of exercise
- learn relaxation or stress management techniques
- don't go more than 4 hours without eating
- avoid processed foods
- see an optometrist for an eye check
What can I do if I suffer from migraines during pregnancy?
If you suffer from migraines, try to avoid things that may trigger migraines for you. People have different triggers for migraines, so it’s important to learn what your personal triggers are. Keep a headache diary, and see if your triggers include:
Keep a headache diary, and see if your triggers include:
- specific foods such as chocolate, or food additives such as caffeine or MSG
- bright or flickering lights, strong smells and loud sounds
- not enough sleep, or too much sleep
- skipping meals
- computer or movie screens
- strenuous exercise
- emotional triggers such as arguments or stress
Check with your doctor, pharmacist or midwife before you take a medicine for your migraine, to make sure it’s safe during pregnancy.
Paracetamol is the safest option for pain relief. If paracetamol doesn’t help and you need something stronger, ask your doctor about if you can take codeine. Try not to take codeine often, as you could become dependent on it and your baby could have withdrawal symptoms after they are born.
Most triptans (migraine medicines) are not considered safe in pregnancy. If you don’t get relief from paracetamol and codeine, you may be able to take sumatriptan occasionally. This medicine is available from a pharmacist and requires a prescription. Speak with your doctor or pharmacist before using it to help you understand the risks and the benefits of this medicine during pregnancy.
This medicine is available from a pharmacist and requires a prescription. Speak with your doctor or pharmacist before using it to help you understand the risks and the benefits of this medicine during pregnancy.
You can take metoclopramide if you suffer from nausea or vomiting with migraines.
Acupuncture can help treat migraines. Talk to your doctor or midwife first to check it’s safe for you. Make sure to tell your acupuncturist that you’re pregnant, so they can avoid certain points that shouldn’t be used in pregnancy.
When should I see a doctor?
See your doctor or midwife if you have symptoms of pre-eclampsia, including:
- a headache that doesn’t get better with paracetamol
- severe pain below your ribs
- heartburn that doesn’t disappear after taking antacids
- sudden swelling in your face, hands or feet
- blurred vision
Headaches can sometimes be a sign of other serious health conditions. Contact your doctor straightaway if you have:
- a sudden severe headache
- a change in your usual headaches
- your first-ever migraine
- a headache together with fever, neck stiffness, sensitivity of your eyes to light, drowsiness or weakness of your arm or leg
- a recent head injury
CHECK YOUR SYMPTOMS — If you are feeling unwell and not sure what to do next, check your symptoms using the healthdirect Symptom Checker tool.
- Speak with your doctor or midwife, particularly if you have any concerns about pre-eclampsia.
- For more information about headaches, visit Migraine and Headache Australia.
- For more information about medicines you can take during pregnancy, talk to your doctor or pharmacist.
Speak to a maternal child health nurse
Call Pregnancy, Birth and Baby to speak to a maternal child health nurse on 1800 882 436 or video call. Available 7am to midnight (AET), 7 days a week.
Sources:
Tommy’s (Headaches in pregnancy – should I be worried?), NSW Government (Having a baby), Migraine & Headache Australia (Adults and headache), Migraine & Headache Australia (Migraine), Migraine & Headache Australia (Headache triggers), Migraine & Headache Australia (Headache treatment – no absolute cure), Migraine & Headache Australia (What is headache?), Migraine & Headache Australia (Tension headache), RANZCOG (Pre-eclampsia and high blood pressure in pregnancy), Royal Women's Hospital (Medicines in pregnancy), NSW Health (Migraine in pregnancy and breastfeeding), RANZCOG (Q&A: severe headache in the third trimester), Migraine & Headache Australia (Self-Care & Trigger Management)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: September 2022
Back To Top
Related pages
- Common discomforts during pregnancy
Need more information?
Treatment of Headache - Migraine & Headache Australia
There is no absolute cure for headache, but many effective treatments exist which can prevent and treat different headache types.
Read more on Migraine and Headache Australia website
Common discomforts during pregnancy
Your body has a great deal to do during pregnancy. Sometimes the changes taking place will cause irritation or discomfort, and on occasions they may seem quite alarming.
Read more on Pregnancy, Birth & Baby website
Adults and Headache - Headache Australia
Studies confirm that tension-type headache and migraine are more common in women while cluster headache, a rare form of headache, is more common in men.
Read more on Migraine and Headache Australia website
Tension-type Headache - Migraine & Headache Australia
Tension-type headache is one of the most common everyday headaches. It causes a dull, non-throbbing pain and can be caused by stress.
Read more on Migraine and Headache Australia website
Migraine Management Tips - Headache Australia
It’s important to be organized and informed about your migraine attacks and how they impact your life. Here are some migraine management tips to assist.
Read more on Migraine and Headache Australia website
Six ways to manage migraine without drugs | The George Institute for Global Health
We’ve all heard of the crushing headache pain that comes with migraine but did you know that one in every seven people experience them, three in every four people with migraine are females, and migraine is the number one cause of disability in young people? With so many people affected worldwide, you’d think modern medicine would have developed a solution by now but unfortunately there’s still no definite cure for migraine.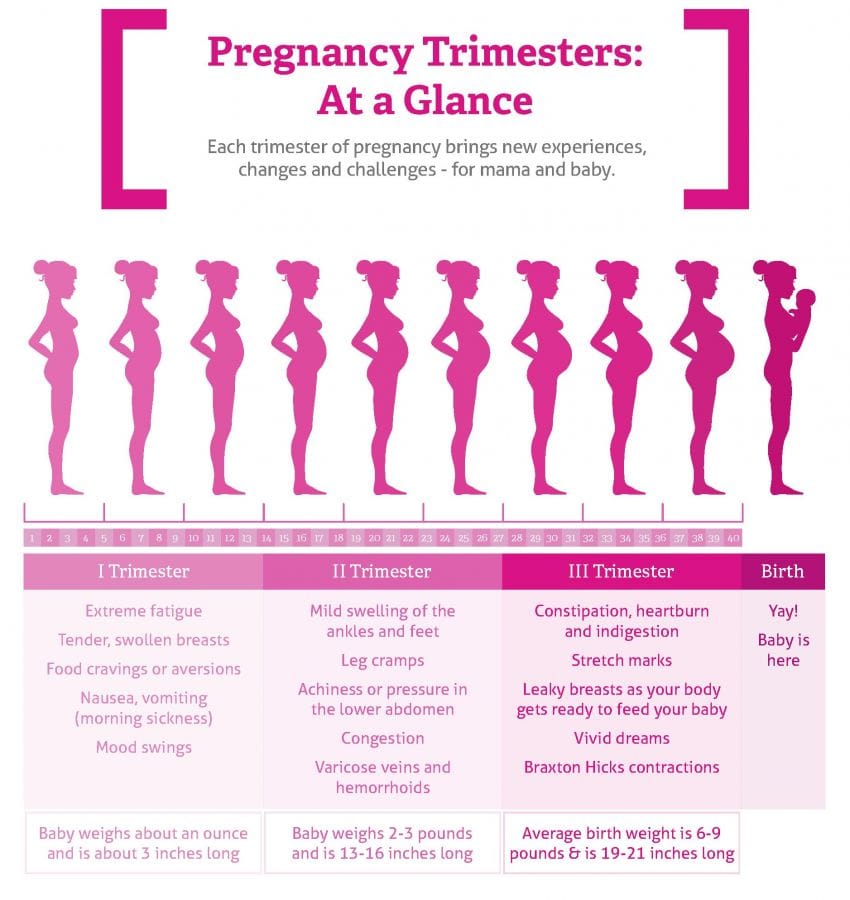
Read more on The George Institute for Global Health website
Stress and pregnancy
Stress is a normal response to major life changes but you can reduce pregnancy-related stress. Learn more about causes and strategies to help.
Read more on Pregnancy, Birth & Baby website
Mumps and pregnancy
Find out about mumps and its symptoms, how it spreads, how to manage it at home, and how to avoid mumps if you’re planning a pregnancy.
Read more on Pregnancy, Birth & Baby website
Toxaemia of pregnancy (pre-eclampsia) - MyDr.com.au
Pre-eclampsia, also known as pre-eclamptic toxaemia, or just toxaemia, occurs in pregnancy, causing problems for the baby and mother.
Read more on myDr website
Warning signs during pregnancy
Most changes in your body are likely to be a normal part of pregnancy, but some signs may indicate things are not going well. Learn how to recognise them and know when you should seek help.
Read more on Pregnancy, Birth & Baby website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Subscribe to newsletters
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.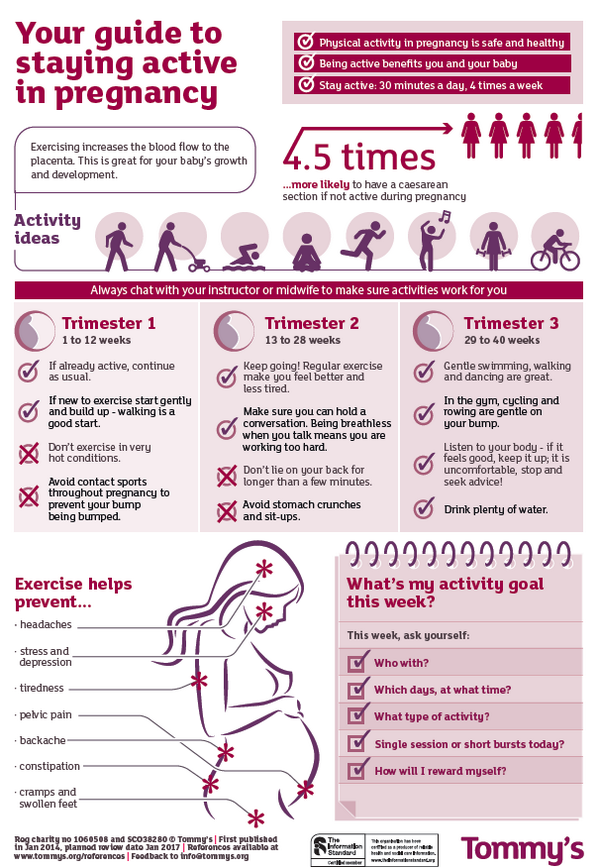
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
Healthdirect Australia acknowledges the Traditional Owners of Country throughout Australia and their continuing connection to land, sea and community. We pay our respects to the Traditional Owners and to Elders both past and present.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care.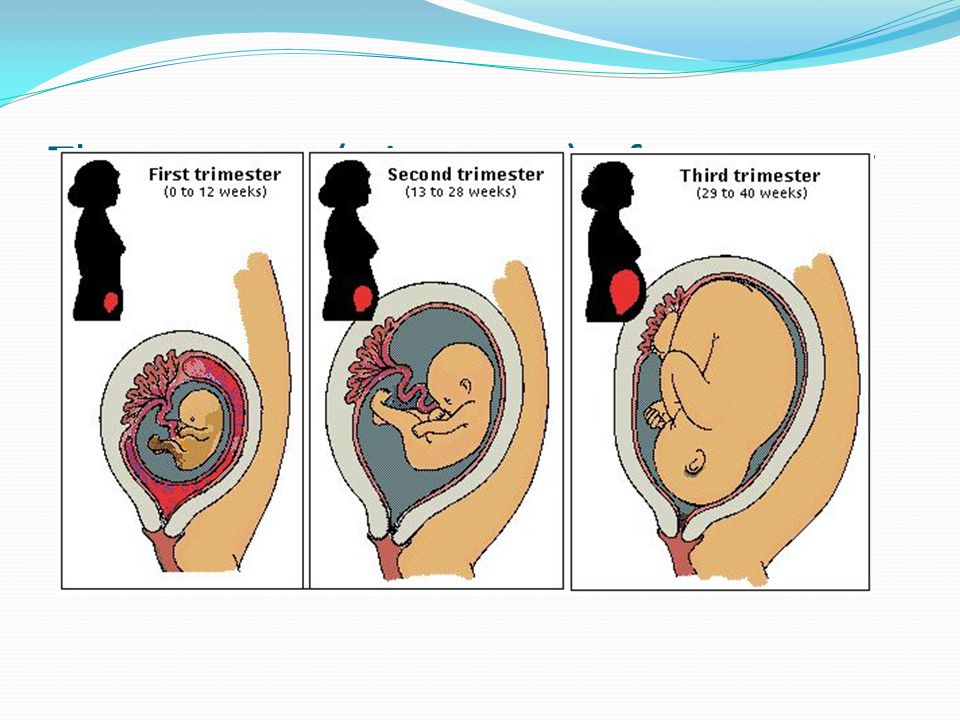 If you have a particular medical problem, please consult a healthcare professional.
If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Migraine during pregnancy: what to do
Migraine is a benign disease, it does not affect the course of pregnancy and fetal development.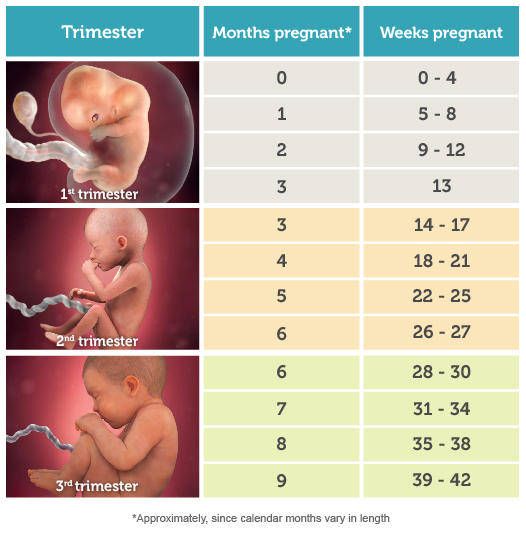 However, migraine and pregnancy is a combination that requires a responsible attitude. Especially with frequent migraines (more than 2 times a week) and migraines with aura, because:
However, migraine and pregnancy is a combination that requires a responsible attitude. Especially with frequent migraines (more than 2 times a week) and migraines with aura, because:
-
medicines approved for use, few,
-
and the approach to the treatment and prevention of migraine during this period is extremely individual: it depends on the frequency, severity and duration of headache, the degree of impact on life.
Our neurologist Daria Korobkova conducted a live broadcast on the clinic's Instagram account, where she told how migraine and pregnancy are connected, why attacks become more frequent or disappear, and answered subscribers' questions. The ether was saved, see “Air recording: migraine during pregnancy and GV.
We will tell about migraine during breastfeeding separately.
The statistics of clinical observations of migraine during pregnancy looks like this:
In 60-70% of pregnant women with migraine, headache attacks become less frequent, milder, or even completely disappear in the second and third trimesters. This is due to the stabilization of estrogen levels. By the beginning of the second trimester, it rises 6 times and its fluctuations stop.
This is due to the stabilization of estrogen levels. By the beginning of the second trimester, it rises 6 times and its fluctuations stop.
In other women, migraines during pregnancy either remain unchanged or worsen. But as the duration of pregnancy increases, the proportion of such women gradually decreases:
If at the end of the first trimester the frequency and intensity of attacks persist, then it is most likely that migraine will disturb the woman throughout the entire period of pregnancy and after childbirth too.
How to manage migraine during pregnancy?
The main thing here is to learn how to control seizures and, if necessary, seek medical help.
-
Follow lifestyle advice:
-
get enough sleep;
-
drink enough fluids;
-
eat fractionally and without long breaks;
-
rest;
-
avoid stressful situations.
 This is one of the main provocateurs of migraine. Psychotherapy, relaxation and stress management are here to help you.
This is one of the main provocateurs of migraine. Psychotherapy, relaxation and stress management are here to help you.
-
Keep a headache diary. This will help you take control of migraine triggers.
Yes, these simple recommendations are sometimes enough to make seizures less frequent! Pregnancy is a special state of a woman. If in other periods of life we do not take such recommendations so seriously, then in this situation it is worth trying to change the philosophy of life and attitude towards ourselves =)
How to relieve an attack?
-
Favor non-drug methods. Sometimes, in order to relieve an attack, it is enough to eliminate an unfavorable factor:
-
dry biscuits, ginger, or applesauce may help with nausea;
-
for dehydration - diluted juice or other liquid;
-
sleep, walking or breathing exercises can also help to cope;
-
If the attacks are severe, interfere with your life, then under the supervision of a specialist, you can resort to drug therapy.

PARACETAMOL is considered the safest and can be taken throughout pregnancy.
All other drugs have nuances. For example:
-
ibuprofen can be taken in the second trimester, and in the first trimester it is better to limit, in the third trimester the drug is contraindicated for use;
-
aspirin is prohibited in the 3rd trimester and is undesirable for taking in the first two, as it can cause extremely undesirable consequences;
-
It is strictly forbidden to use ergotamine and opioid analgesics;
-
triptans are not officially approved for use during pregnancy as no controlled studies have been conducted. However, clinical observations of women around the world who took them on their own showed no adverse effects on the fetus. We discussed this issue in more detail on the air.
!Other than paracetamol, we do not recommend the use of any drug without a doctor's prescription.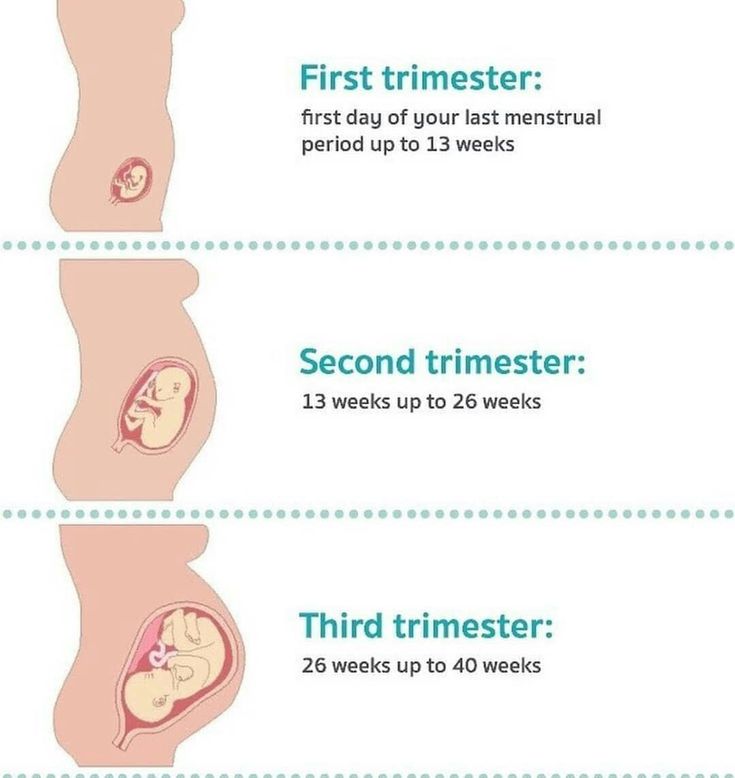
When to see a doctor:
-
migraine occurred for the first time during pregnancy;
-
if migraine attacks suddenly become more frequent and stronger;
-
if the aura became longer or appeared for the first time;
-
if the headache is rapidly increasing and has an unusual character;
-
if the pressure rises during the headache.
Read more articles about headaches in our Telegram channel.
New drugs: jepants and ditans for the treatment of migraine attack Pain 10 out of 10 How to relieve a migraine without medication
which doctor should I contact and how to treat correctly?
- Main
- >Pregnancy
Of course, migraine or chronic tension headache is not a contraindication to pregnancy.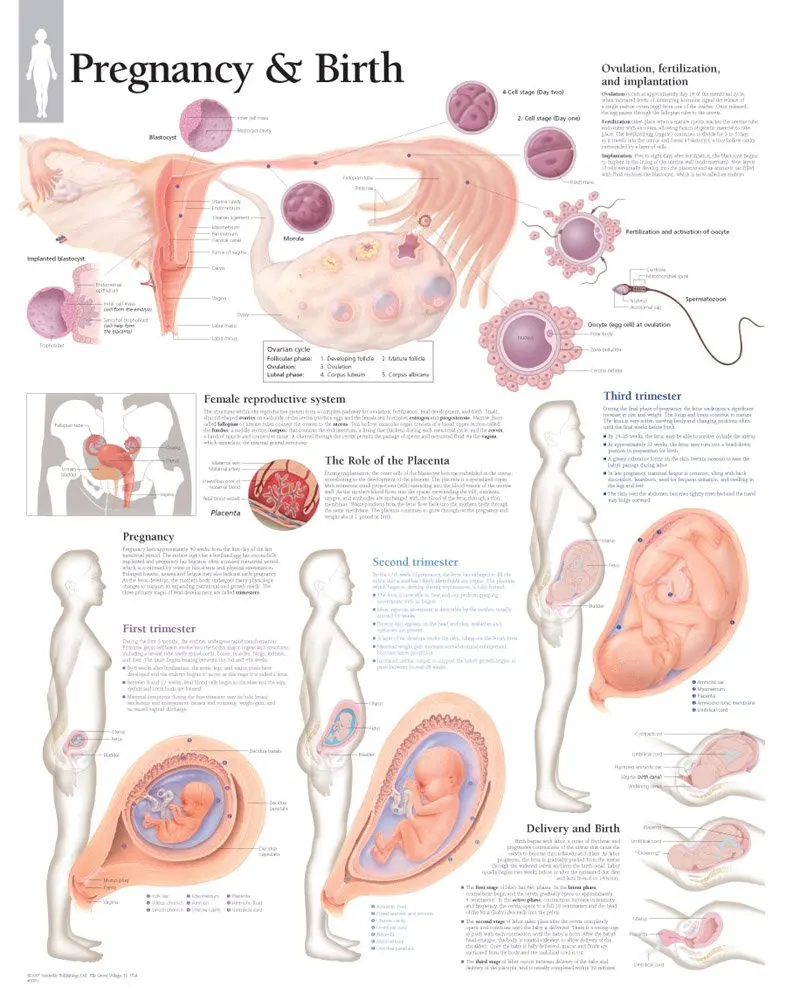 And almost every woman, regardless of the presence of any chronic diseases, wants to become a mother. However, in order to survive the most comfortable period of pregnancy in the presence of chronic migraine or headache, it is necessary to prepare for this period in advance. The better your preparation is, the easier it will be for pregnancy, childbirth and postpartum feeding of the baby. Women with migraines are advised to stop all medications at least two weeks before conception and prepare to avoid severe attacks. Ideally, this stage of preparation takes from 6 to 12 months. Clinic of headache and vegetative disorders. Veina in Moscow specializes in the treatment of migraines, headaches and other types of pain syndrome. For a long time of work under the supervision of our doctors, many pregnancies have come and gone successfully, even in difficult patients. Effective assistance was provided to expectant mothers with such diseases as:
And almost every woman, regardless of the presence of any chronic diseases, wants to become a mother. However, in order to survive the most comfortable period of pregnancy in the presence of chronic migraine or headache, it is necessary to prepare for this period in advance. The better your preparation is, the easier it will be for pregnancy, childbirth and postpartum feeding of the baby. Women with migraines are advised to stop all medications at least two weeks before conception and prepare to avoid severe attacks. Ideally, this stage of preparation takes from 6 to 12 months. Clinic of headache and vegetative disorders. Veina in Moscow specializes in the treatment of migraines, headaches and other types of pain syndrome. For a long time of work under the supervision of our doctors, many pregnancies have come and gone successfully, even in difficult patients. Effective assistance was provided to expectant mothers with such diseases as:
- migraine,
- headache,
- panic attacks and anxiety during pregnancy,
- insomnia,
- attacks of vegetovascular dystonia during pregnancy,
- pain in the neck, back, lower back during pregnancy,
- diseases during pregnancy.

Pregnancy and breastfeeding has many restrictions in taking medicines. However, some schemes for taking drugs to relieve headaches and migraines during pregnancy still exist. It is better to clarify and select them in advance together with the attending physician, and also to develop a clear algorithm of actions in case of an impending attack. Enduring pain during pregnancy with migraine is still not recommended, with the exception of the first trimester and the last weeks of the third trimester. But most importantly, non-drug methods of relieving headaches come to the aid of pregnant women, such as:
- biofeedback therapy,
- manual therapy,
- massage,
- acupuncture,
- psychotherapy.
botulinum therapy - prevention of migraine and headache during pregnancy
The most interesting and promising method of treating headache during pregnancy and migraine is botulinum therapy. The essence of this method is prevention.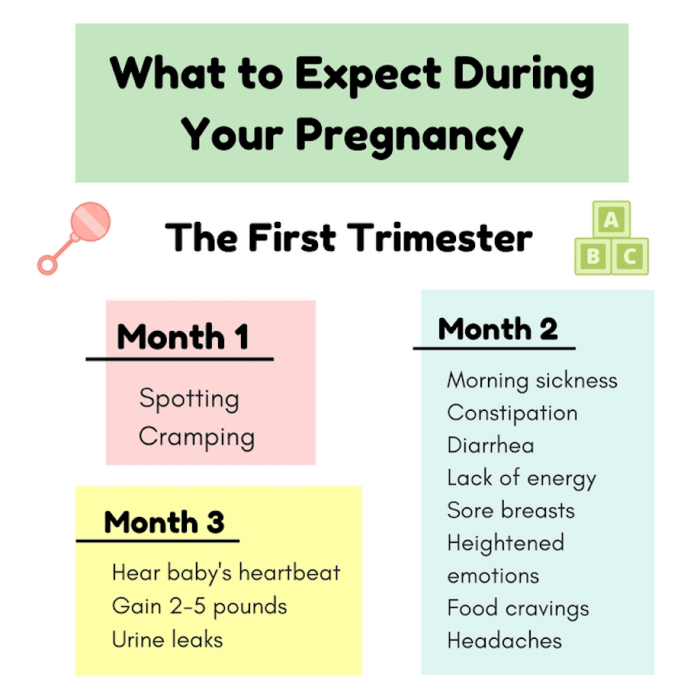 Before becoming pregnant, a woman is given injections of one of the botulinum toxin preparations (multiple injections during the year are possible). Such prophylactic treatment can significantly reduce the frequency and intensity of migraine attacks for up to six months. Thus, it is possible to minimize the frequency and severity of attacks in the most important first trimester. Then, when the laying of the organs and systems of the baby occurs, it is risky to take painkillers. To select the optimal timing and methods of treating your type of headache, it is best to contact a headache specialist a year, six months before the planned pregnancy.
Before becoming pregnant, a woman is given injections of one of the botulinum toxin preparations (multiple injections during the year are possible). Such prophylactic treatment can significantly reduce the frequency and intensity of migraine attacks for up to six months. Thus, it is possible to minimize the frequency and severity of attacks in the most important first trimester. Then, when the laying of the organs and systems of the baby occurs, it is risky to take painkillers. To select the optimal timing and methods of treating your type of headache, it is best to contact a headache specialist a year, six months before the planned pregnancy.
Authorized medicines for migraine and headache
Still, migraine and headache often take pregnant women by surprise. What painkillers are still allowed for pregnant women? During the entire period of pregnancy, you can take paracetamol at a dose of 325-500 mg up to 4 times a day. Caffeine is also allowed. So, you can drink migraine, panadol extra or solpadein fast. Of course, these painkillers are not very strong. And at the usual time, taking them to relieve a migraine attack is not recommended. But during pregnancy, they can be drunk absolutely fearlessly. It is effective to take aspirin, naproxen and ibuprofen during pregnancy for migraine. But they can be drunk without fear only during the first and second trimesters. When planning a pregnancy, they are undesirable. And in the third trimester it is generally prohibited.
Of course, these painkillers are not very strong. And at the usual time, taking them to relieve a migraine attack is not recommended. But during pregnancy, they can be drunk absolutely fearlessly. It is effective to take aspirin, naproxen and ibuprofen during pregnancy for migraine. But they can be drunk without fear only during the first and second trimesters. When planning a pregnancy, they are undesirable. And in the third trimester it is generally prohibited.
DRUGS FOR MIGRAINES AND HEADACHES IN PREGNANCY
There are drugs that are strictly prohibited during pregnancy. These are painkillers with phenobarbital, codeine, old tranquilizers like phenazepam and ergotamines.
Headache and migraine treatment during pregnancy
Dear expectant mothers! If you suffer from migraines, chronic headaches or other types of pain syndrome, experience a feeling of constant anxiety, panic attacks, we invite you to spend your pregnancy under the supervision of our specialists! Our doctors have harmless, but effective methods of treatment.