Hcg beta chart
The BetaBase
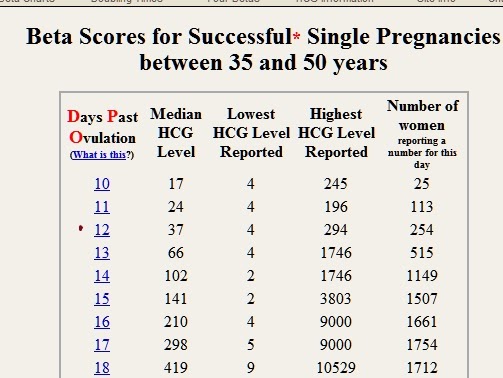
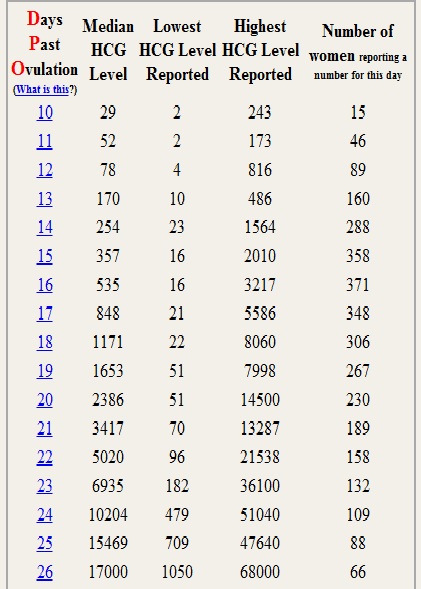
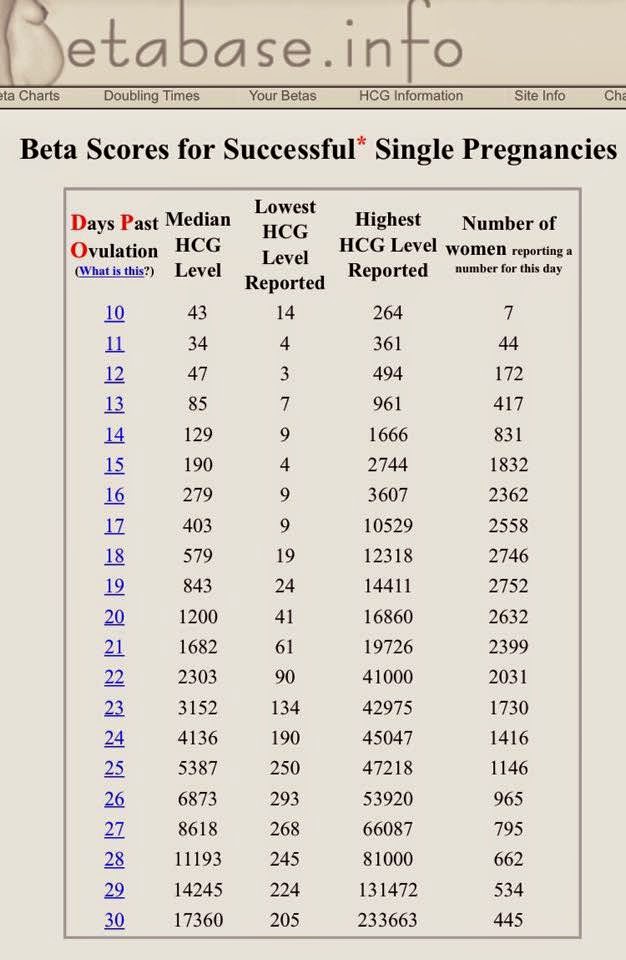
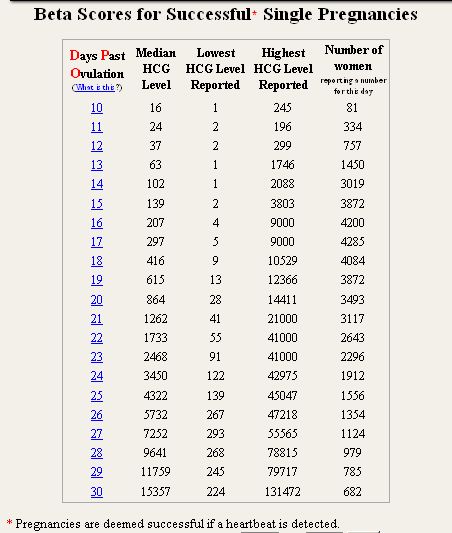
The BetaBaseBeta Scores for Successful* Single Pregnancies
| Days Past Ovulation (What is this?) | Median HCG Level | Lowest HCG Level Reported | Highest HCG Level Reported | Number of women reporting a number for this day |
|---|---|---|---|---|
| 10 | 37 | 3 | 617 | 22 |
| 11 | 31 | 4 | 361 | 105 |
| 12 | 50 | 3 | 494 | 332 |
| 13 | 87 | 7 | 961 | 782 |
| 14 | 133 | 5 | 1666 | 1557 |
| 15 | 200 | 4 | 2744 | 3440 |
| 16 | 299 | 6 | 3607 | 4525 |
| 17 | 431 | 9 | 10529 | 4853 |
| 18 | 630 | 14 | 12802 | 5067 |
| 19 | 922 | 18 | 17072 | 5000 |
| 20 | 1320 | 13 | 22766 | 4785 |
| 21 | 1862 | 11 | 30360 | 4375 |
| 22 | 2545 | 9 | 41000 | 3777 |
| 23 | 3473 | 46 | 53991 | 3293 |
| 24 | 4598 | 53 | 72000 | 2786 |
| 25 | 5876 | 45 | 55521 | 2309 |
| 26 | 7397 | 39 | 69865 | 1943 |
| 27 | 9096 | 37 | 87915 | 1630 |
| 28 | 11598 | 36 | 89387 | 1417 |
| 29 | 14521 | 20 | 131472 | 1200 |
| 30 | 17288 | 12 | 233663 | 1027 |
* Pregnancies are deemed successful if a heartbeat is detected.
Beta hCG doubling time calculator and charts
First β-hCG level
mIU/mL
Second β-hCG level
mIU/mL
Time between tests
Days
Hours
We don’t collect, process, or store any of the data that you enter while using this tool. All calculations are done exclusively in your browser, and we don’t have access to the results. All data will be permanently erased after leaving or closing the page.
Difference
Doubling time
One day increase
Two day increase
Start over
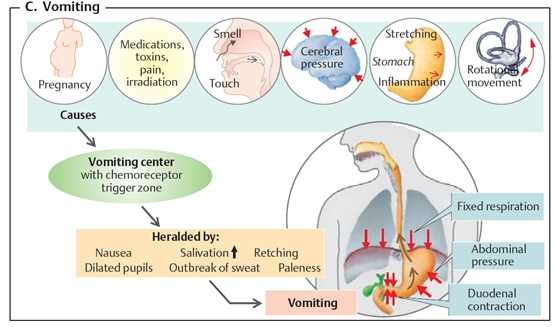
Human chorionic gonadotropin, or hCG, is the hormone your body produces when you are pregnant. In fact, hCG showing up in your blood or urine is one of the earliest signs of pregnancy, which is why lots of people are eager to know more about normal hCG levels.
In fact, hCG showing up in your blood or urine is one of the earliest signs of pregnancy, which is why lots of people are eager to know more about normal hCG levels.
Get started with our hCG calculator now (above) to work out your hCG levels at home by entering the results of two blood tests and the time between those tests. Then scroll down for everything you need to know about hCG levels in early pregnancy.
Remember that hCG calculator tools and hCG level charts can help you learn more about the part hCG plays in pregnancy. But they are for informational purposes only, not a replacement for medical advice nor a self-diagnosis tool. Your doctor should always be your first port of call when it comes to tracking and explaining hCG progression.
Medically reviewed by
Dr. Angela Jones
Obstetrician and gynecologist, attending physician, Jersey Shore University Medical Center, New Jersey, US
When does hCG start?First up, you might be wondering when hCG starts to show up.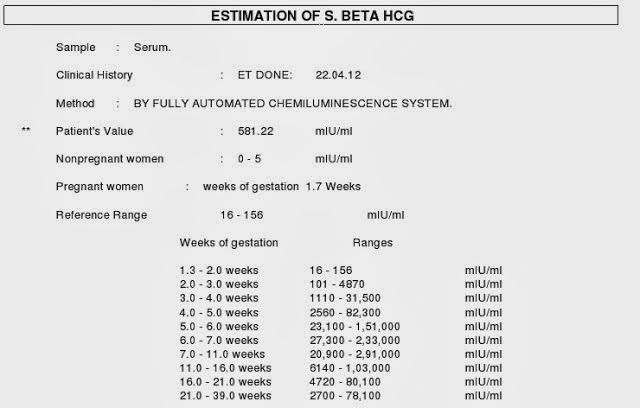 The pregnancy hormone can be picked up in your urine and your blood once the embryo attaches itself to the uterine wall (between days 6 and 14 after the sperm has fertilized the egg).
The pregnancy hormone can be picked up in your urine and your blood once the embryo attaches itself to the uterine wall (between days 6 and 14 after the sperm has fertilized the egg).
A positive test confirms you’re pregnant. At-home pregnancy tests work by detecting hCG in your pee — normally from days 5 to 10 after your expected period, but some sensitive tests can detect it as early as 10 days after conception.
Dr. Sara Matthews, consultant gynecologist and fertility specialist at London’s Portland Hospital, says, “Home pregnancy tests using urine are very accurate. A positive result pretty much means you are pregnant, but before you celebrate or panic, make sure you are reading the test correctly — always check the instructions! A negative result may mean it’s simply too early to test, so if a period is delayed, the test should be repeated 2 to 3 days later.”
Your doctor can request an in-clinic blood test to check for hCG. “This can be useful if there has been bleeding and a miscarriage is possible,” Dr. Matthews explains. “It can also help the doctor if an ectopic pregnancy is suspected (a pregnancy that has implanted outside the womb).”
Matthews explains. “It can also help the doctor if an ectopic pregnancy is suspected (a pregnancy that has implanted outside the womb).”
We now know that hCG in your urine and blood can show you’re pregnant, but that’s not all. Your health care provider can also learn more about how your pregnancy might be progressing from the hCG levels in your blood.
“A pregnancy cannot be detected reliably by ultrasound until six weeks of pregnancy, so sometimes blood levels are monitored before then,” explains Dr. Matthews.
Beta hCG calculator: What if hCG levels are low?Let’s look at what different hCG levels can mean with a little help from Dr. Matthews:
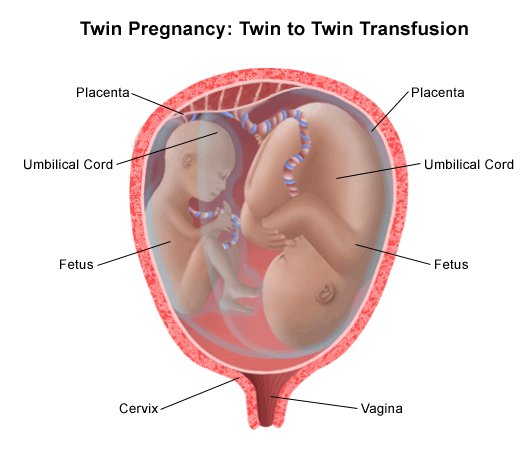
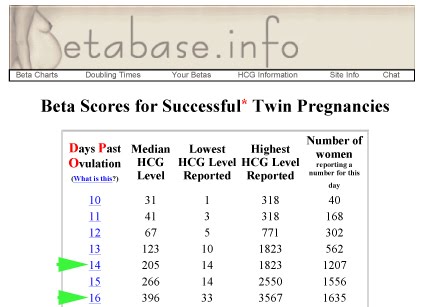
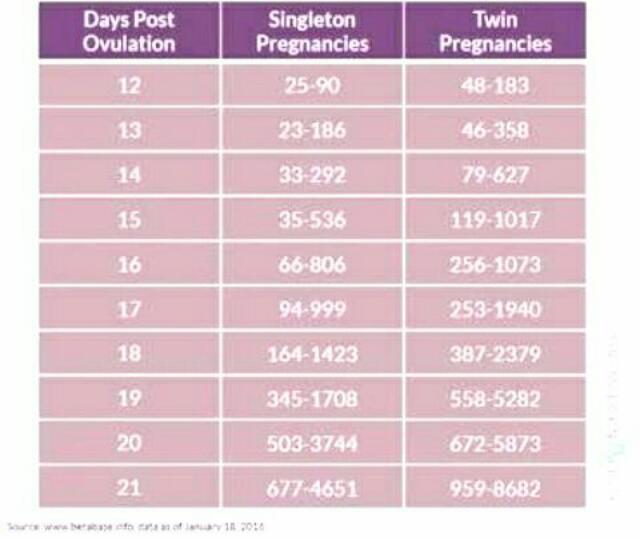
- Higher than average hCG levels might indicate that you’re having twins or triplets, but you’ll need an ultrasound scan to confirm this. “A normal blood level for hCG on the day a period is due (14 days after ovulation) is 40 to 120 mIU/mL, but levels are up to 400 in multiple pregnancies!” she says.
 Higher than average hCG levels could also suggest your due date is wrong (you’re further along in your pregnancy than you thought!). Sadly, they can also indicate a molar pregnancy (when the placenta grows abnormally). “[Molar] pregnancy always ends in miscarriage, and careful monitoring of the hCG levels may be required for up to six months,” says Dr. Matthews.
Higher than average hCG levels could also suggest your due date is wrong (you’re further along in your pregnancy than you thought!). Sadly, they can also indicate a molar pregnancy (when the placenta grows abnormally). “[Molar] pregnancy always ends in miscarriage, and careful monitoring of the hCG levels may be required for up to six months,” says Dr. Matthews. - Falling hCG levels within the first six weeks could mean you’re at higher risk of having a miscarriage. If you’re worried about your hCG levels, then speak to your doctor right away.
- Lower than average hCG levels “might indicate that the pregnancy implanted a day or two later than expected,” Dr. Matthews says. It could also mean an ectopic pregnancy or a “biochemical” pregnancy. A biochemical pregnancy is a very early miscarriage where the embryo implants, but only for a few days, and a late period happens before a scan to confirm a pregnancy can be done. Again, speak to your doctor if you think this might apply to you.
.jpg)
It’s important to remember that hCG levels are not a diagnosis on their own. They are just a sign that your doctor might need to do more tests. The tool above is designed for informational purposes only; you should always reach out to your health care provider for early pregnancy advice and support.
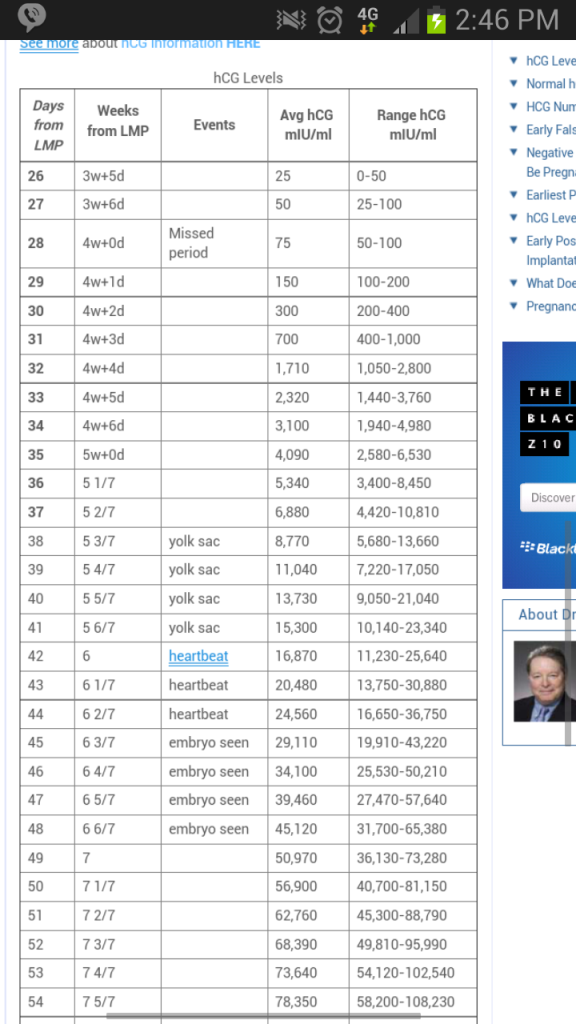
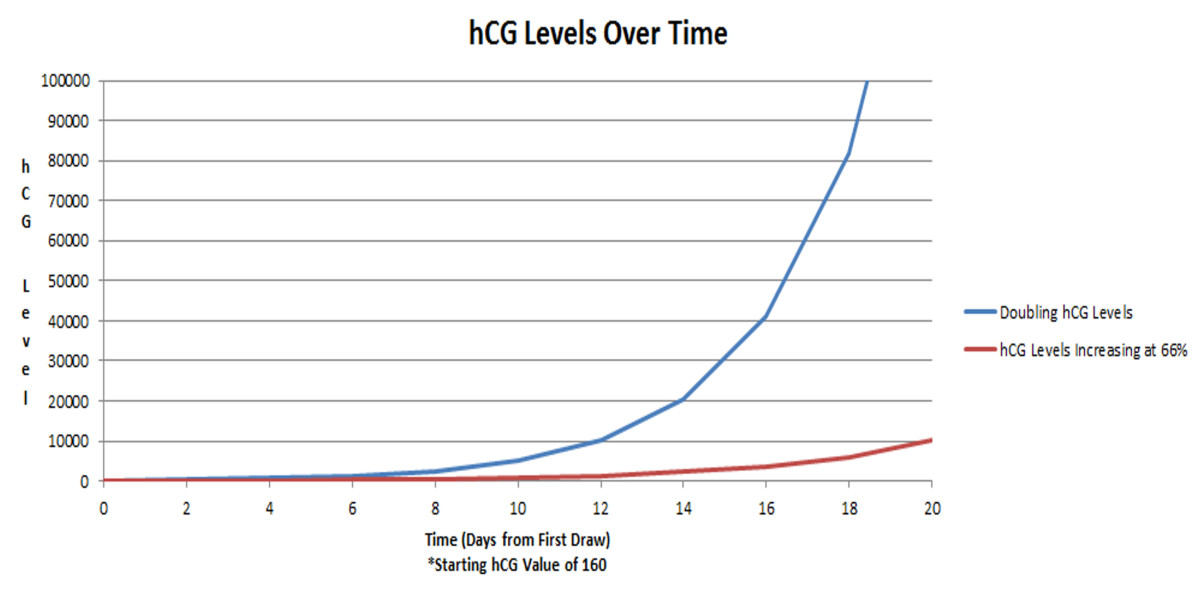
hCG progression: What is a normal hCG level in pregnancy? When do hCG levels stop doubling?hCG levels in our blood change during the first trimester, rising rapidly.
Nonpregnant women have less than 5 milli-international units per milliliter (mIU/mL). “A normal blood level for hCG on the day a period is due (14 days after ovulation) is 40 to 120 mIU/mL,” Dr. Matthews says.
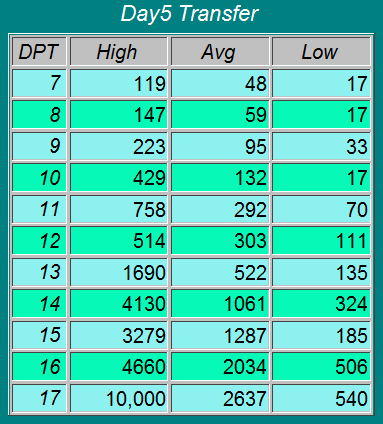
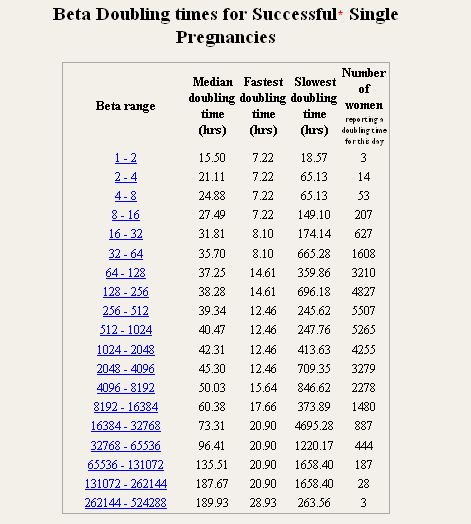
Levels should then double every 48 hours from weeks four to six, but that isn’t the case for everyone. hCG can vary from person to person and still mean a pregnancy is normal. In fact, a 2017 study into hCG found that “the slowest or minimal rise for a normal viable intrauterine pregnancy was 24% at one day and 53% at two days.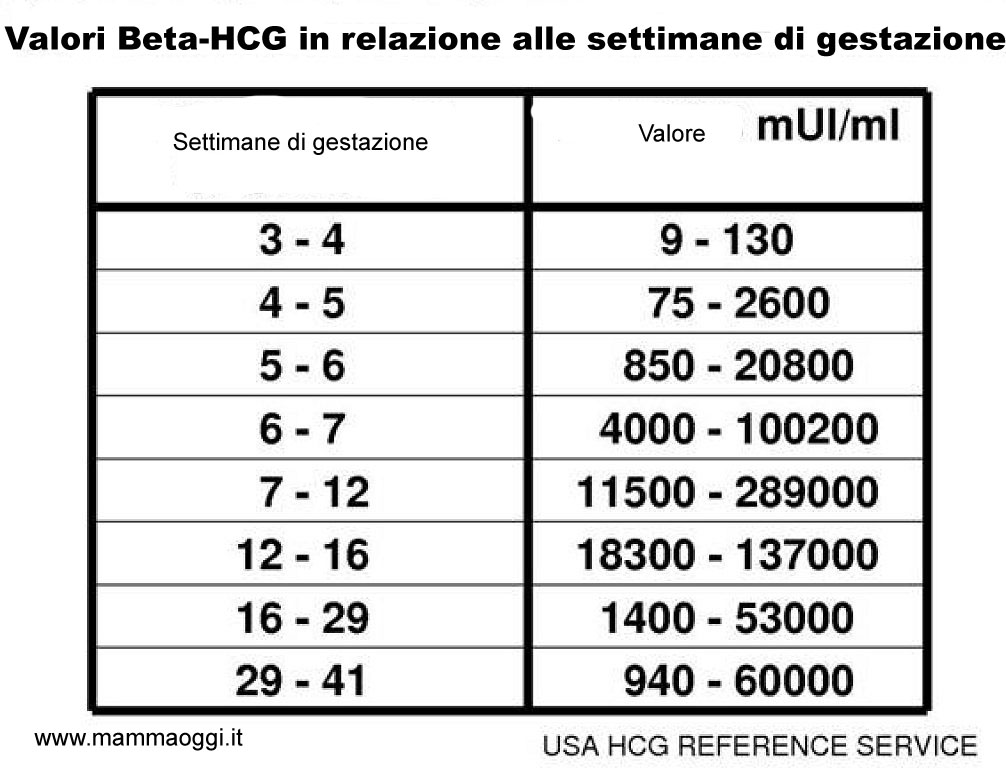 More recently, a rise of 35% over 48 hours was proposed as the minimal increase consistent with a viable intrauterine pregnancy.”
More recently, a rise of 35% over 48 hours was proposed as the minimal increase consistent with a viable intrauterine pregnancy.”
Dr. Matthews adds that “hCG levels peak at around eight [to ten] weeks of pregnancy. [They] are unreliable after that, but at that stage, ultrasound is used [anyway].”
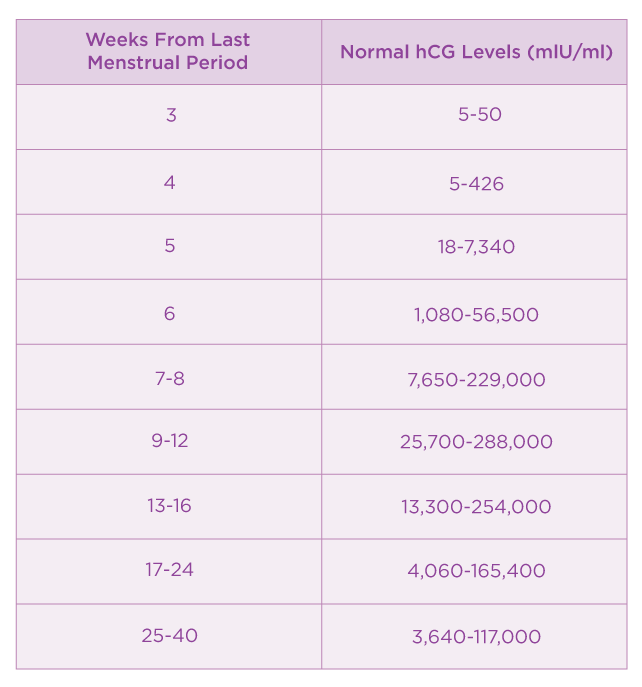
hCG levels in early pregnancyRemember that hCG levels vary from person to person and can be lower than average, so the above beta hCG chart should only be used as a rough guide.
hCG doubling time: What does it mean?It’s important not to get fixated on hCG doubling time because, as we’ve learned, every pregnancy is different. That means your hCG levels might not double but are totally normal for you.
That said, it’s useful to know how hCG doubling time works in theory. Over to Dr. Matthews again: “An hCG level should double every 48 hours from four to six weeks [of pregnancy]. A level that does not double should be rechecked after another two days as it might indicate a failing pregnancy or a PUO (pregnancy of unknown origin).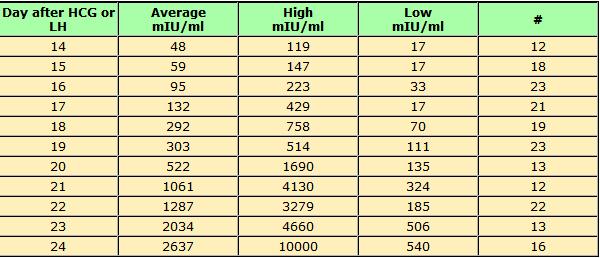
“But an initially high level can also fall in a multiple pregnancy when one baby stops growing. In this situation, the other baby is not affected by that unless twins or triplets are identical (they come from one embryo that split when it’s implanted).”
Speak to your doctor to put your hCG levels into context.
At what hCG level will I miscarry?“A miscarriage is likely if the hCG level falls in the first six weeks of pregnancy, but don’t forget that it can also fall from a high level with an early ‘vanishing twin,’ so if no bleeding has happened by six weeks, then always scan to find more information,” Dr. Matthews says.
“That is also of course an essential way to diagnose an ectopic pregnancy, commonly called a PUO (pregnancy of unknown origin), in the early stages that might be resolving itself without the need for an operation.
“A negative urine hCG pregnancy test is registered when the level of hormone drops below 4 mIU/mL [or the test sensitivity threshold]. A period will inevitably start within 1 to 2 days.”
A period will inevitably start within 1 to 2 days.”
In the early stages of pregnancy? We’ve got plenty of personalized information to help you track your baby’s development and changes to your body, week by week. Download the app now to get started.
References
Updated November 28 2022
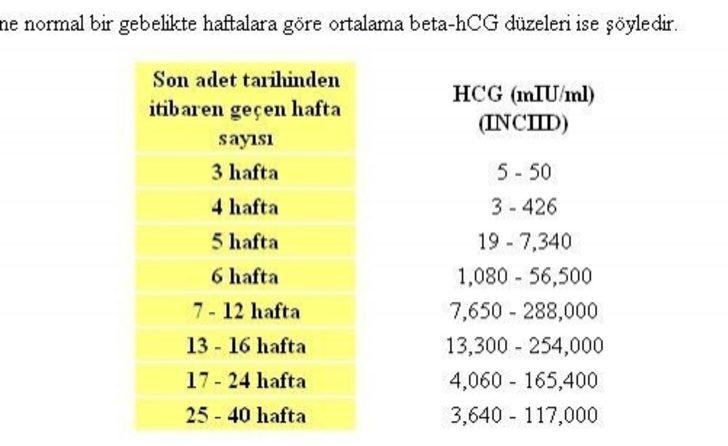
HCG norms by weeks of pregnancy
HCG norms by weeks of pregnancy - Private maternity hospital Ekaterininskaya Clinics
Content
- Table of average hCG norms
- Table of average hCG norms for carrying twins
- Table of average hCG values after IVF with engrafted twins
- Guidelines for free β-hCG subunit
- Norm РАРР-А
- What if I am at high risk? nine0008
- How to confirm or deny the results of screening?
- The doctor says I need an abortion.
 What to do?
What to do?
One of the main tests during pregnancy is the study of the level of pregnancy hormone - hCG or human chorionic gonadotropin. If future mothers want to know if the hormone level is normal, we made a summary table of values
Table of average hCG norms:
| Gestation period | nine0031 HCG in honey/mlHCG in mIU/ml | HCG in ng/ml | |
| 1-2 weeks | 25-156 | 5-25 (doubtful result) | - |
| 2-3 weeks | 101-4870 | 5-25 (doubtful result) | - |
| 3-4 weeks | 1100 – 31500 | 25-156 | - |
| 4-5 weeks | 2560 – 82300 | nine0031 101-4870- | |
| 5-6 weeks | 23100 – 151000 | 1110 -31500 | - |
| 6-7 weeks | 27300 – 233000 | 2560 -82300 | - |
| 7-11 weeks | 20900 – 2 | 23100 -233000 | 23.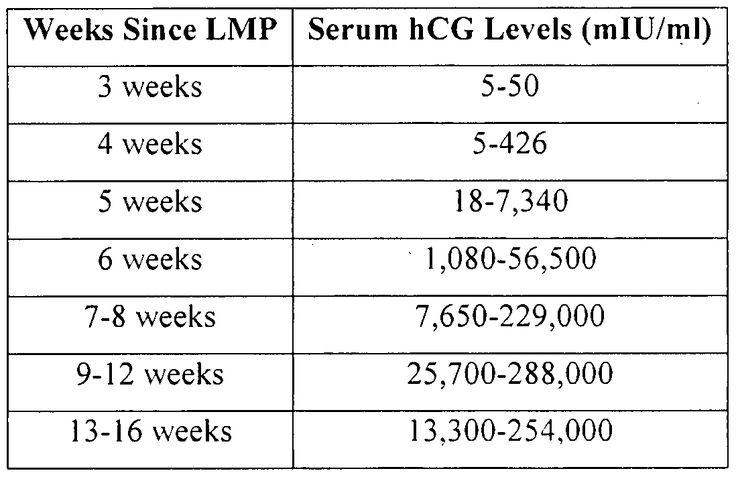 7 - 130.4 7 - 130.4 |
| 11-16 weeks | 6140 – 103000 | 20900 -103000 | 17.4 - 50.0 | nine0039
| Weeks 16-21 | 4720 – 80100 | 6140 – 80100 | 4.67 - 33.3 |
| 21-39 weeks | 2700 – 78100 | 2700 -78100 | - |
Table of average hCG norms for carrying twins:
| Gestation period, weeks | Average range of hCG concentration (mU/ml) |
| 1-2 weeks | 50 - 112 |
| 2-3 weeks | 209 – 9740 |
| 3-4 weeks | 2220 – 63000 |
| 4-5 weeks | 5122 – 164600 |
| 5-6 weeks | 46200 – 302000 |
| 6-7 weeks | 54610 – 466000 |
| 7-11 weeks | 41810 – 582000 |
| 11-16 weeks | 12280 – 206000 |
| 16-21 weeks | 9440 – 160210 |
| 21-39 weeks | 5400 – 156200 |
Table of average hCG values after IVF with engrafted twins:
| Gestational age, weeks | HCG range, mU/ml |
| 1-2 weeks | 50 – 600 |
| 2-3 weeks | 3000 – 10000 |
| 3-4 weeks | 20000 – 60000 |
| 4-5 weeks | 40000 – 200000 |
| 5-6 weeks | 100000 – 400000 |
| 6-7 weeks | 100000 – 400000 |
| 7-11 weeks | 40000 – 200000 |
| 11-16 weeks | 40000 – 120000 |
| 16-21 weeks | 20000 – 70000 |
| 21-39 weeks | 20000 – 120000 |
Free hCG β-subunit limits
Free hCG β-subunit measurement is more accurate in determining the risk of Down syndrome in an unborn child than measuring total hCG.
Norms for free β-hCG subunit in the first trimester:
| Gestational period, weeks | HCG in ng/ml |
|---|---|
| 9 weeks | 23.6 - 193.1 ng/mL or 0.5 - 2 MoM |
| 10 weeks | 25.8 - 181.6 ng/mL or 0.5 - 2 MoM |
| 11 weeks | 17.4 - 130.4 ng/mL or 0.5 - 2 MoM |
| 12 weeks | 13.4 - 128.5 ng/mL or 0.5 - 2 MoM |
| 13 weeks | 14.2 - 114.7 ng/mL or 0.5 - 2 MoM |
Norms in ng / ml may vary in different laboratories, therefore the data indicated is not final, and in any case you should consult your doctor. If the result is indicated in MoM, then the norms are the same for all laboratories and for all analyzes: from 0.5 to 2 MoM. nine0349If hCG is abnormal, then:
- If the free β-subunit of hCG is higher than normal for your gestational age, or more than 2 MoM, then the child has an increased risk of Down syndrome.
- If the free hCG β-subunit is below normal for your gestational age, or is less than 0.5 MoM, then the baby is at increased risk of Edwards syndrome.
PAPP-A norm
PAPP-A, or "pregnancy-associated plasma protein A" as it is called, is the second indicator used in biochemical screening of the first trimester. The level of this protein constantly increases during pregnancy, and deviations in the indicator may indicate various diseases in the unborn child. nine0003
Norm for PAPP-A depending on the duration of pregnancy:
Gestational period, weeks HCG in ng/ml 8-9 weeks 0.17 - 1.54 mU/ml, or 0.5 to 2 MoM 9-10 weeks 0.32 - 2.42 mU/ml or 0.5 to 2 MoM 10-11 weeks 0.46 - 3.73 mU/ml, or 0.5 to 2 MoM 11-12 weeks 0.79– 4.76 mU/ml, or 0.5 to 2 MoM 12-13 weeks 1. 03 - 6.01 mU/ml, or 0.5 to 2 MoM
13-14 weeks 1.47 - 8.54 mU/ml, or 0.5 to 2 MoM
Norms in ng / ml may vary in different laboratories, therefore the data indicated is not final, and in any case you should consult your doctor. If the result is indicated in MoM, then the norms are the same for all laboratories and for all analyzes: from 0.5 to 2 MoM. nine0349If PAPP-A is abnormal:
- If PAPP-A is lower for your gestational age, or less than 0.5 MoM, your baby is at increased risk of Down syndrome and Edwards syndrome.
- If PAPP-A is higher than normal for your gestational age, or more than 2 MoM, but other screening values are normal, then there is no cause for concern.
Studies have shown that women with elevated PAPP-A levels during pregnancy are not at greater risk of fetal disease or pregnancy complications than other women with normal PAPP-A. nine0003
What if I am at high risk?
If your screening reveals an increased risk of having a baby with Down syndrome, then this is not a reason to terminate the pregnancy.
You will be referred for a consultation with a geneticist who, if necessary, will recommend examinations: chorionic villus biopsy or amniocentesis
How to confirm or refute the screening results?
If you think that the screening was not done correctly, then you should be re-examined at another clinic, but for this you need to retake all the tests and undergo an ultrasound. This method is possible only if the gestational age at the time of the examination does not exceed 13 weeks and 6 days. nine0003
The doctor says I need an abortion. What to do?
Unfortunately, there are times when a doctor strongly recommends or even forces an abortion based on the screening results. Remember: no doctor has the right to such actions. Screening is not a definitive method for diagnosing Down syndrome and, based on poor results alone, a pregnancy should not be terminated.
Say that you want to consult a geneticist and undergo diagnostic procedures for Down syndrome (or other disease): chorionic villus biopsy (if you are 10-13 weeks pregnant) or amniocentesis (if you are 16-17 weeks pregnant).
nine0003
The author of the article:
Ananyina Anna Alexandrovna
Obstetrician-gynecologist
Work experience since 2010
Sign upEat more foods rich in iron: beef tongue, liver, buckwheat and oatmeal, prunes, dried apricots, green apples, etc. But diet alone will not work to raise hemoglobin. nine0455 Medical therapy with iron supplements is required. If the problem is associated with insufficient intake of iron into the body, one set of drugs is needed, if with absorption, another. The doctor must select drugs.
Injection therapy may be required for more severe anemia.If there are no contraindications, natural childbirth is possible. Only an obstetrician-gynecologist should decide on the possibility of EP.
Get tested
- Chest X-ray
- KSR
- Hepatitis B HBsAg
- Hepatitis C Anti-HCV
- Rubella IgM
- Rubella IgG
- HIV
- B/P for flora and senses.
- from throat
Specialist consultation:
- General practitioner consultation
With an increase in the duration of pregnancy and the growth of the baby, the uterus increases - this can lead to increased tone. Sometimes tension arises in response to the movements of the child. Strong physical exertion, stress, overwork of a pregnant woman can also lead to increased tone. nine0455 In early pregnancy, uterine tone may be associated primarily with reduced progesterone production. In this case, the doctor prescribes the patient treatment with progesterone preparations.
Symptoms of increased tone
All pregnant women experience tone differently. Someone - like heaviness and tension in the lower abdomen. Others - as a pulling pain in the lumbar region. In the 2nd and 3rd trimesters of pregnancy, a woman can feel the tone by putting her hand on her stomach: the uterus becomes "stone", then relaxes. nine0003Obstetrician-gynecologist
Doctor of the first category
Specify the cost of admission
in the Call-centerObstetrician-gynecologist nine0451
Doctor of the first category
Admission fee
2500 ₽Obstetrician-gynecologist
Doctor of the highest category
Candidate of Medical SciencesCheck the cost of admission
in the Call-centerObstetrician-gynecologist
Doctor of the first category
Check the cost of admission
in Call-centerObstetrician-gynecologist
Doctor of the highest category
Specify the cost of admission
nine0495 Obstetrician-gynecologist / Gynecologist
in the Call-centerDoctor of the highest category
Candidate of Medical SciencesAdmission fee
2500 ₽Obstetrician-gynecologist nine0451
Doctor of the highest category
Admission fee
2500 ₽Obstetrician-gynecologist
Doctor of the second category
Check the cost of admission
in Call-centerMobile application of the clinic
You can make an appointment with a doctor, get tests
and much more...
Fill out the form to make an appointment or order a call back
I agree with personal data processing policy and user agreement I also give my consent to the processing of personal data.
Sign up for a consultation
I agree with personal data processing policy and user agreement I also give my consent to the processing of personal data.
By continuing to use rd.clinic23.ru, you agree to the use of cookies. How to ban the use of certain cookies can be found in Politics
hCG, human chorionic gonadotropin, indications for the appointment, rules for preparing for the test, interpretation of the results and norm indicators. nine0001
I confirm More
- INVITRO
- Library
- Laboratory...
- HCG, Chorionic...
ECO
Miscarriage
nine0002 Pregnancy3841 July 29
IMPORTANT!
The information in this section should not be used for self-diagnosis or self-treatment. In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor. nine0455 For a correct assessment of the results of your analyzes in dynamics, it is preferable to do studies in the same laboratory, since different laboratories may use different research methods and units of measurement to perform the same analyzes.
We remind you that independent interpretation of the results is unacceptable, the information below is for reference only.
Human chorionic gonadotropin (hCG, β-hCG, beta-hCG, Human Chorionic Gonadotropin): indications for prescribing, rules for preparing for the test, interpretation of the results and norm indicators. nine0601
Chorionic gonadotropin is a hormone produced by the outer shell of the embryo, and is normally determined in the blood and urine of a woman only when pregnancy occurs.
Chorionic gonadotropin consists of two subunits - alpha and beta. The beta subunit (β-hCG) used for the immunometric determination of the hormone is unique. To monitor the course of pregnancy, the determination of the beta subunit of hCG is used. The level of beta-hCG in the blood as early as 6-8 days after conception makes it possible to diagnose pregnancy (the concentration of β-hCG in the urine reaches the diagnostic level 1-2 days later than in the blood serum).
nine0003
HCG has a multifaceted effect on the body of a pregnant woman: it affects the development of the embryo and fetus, stimulates the synthesis of estrogens and androgens by ovarian cells, promotes the functional activity of the chorion and placenta, and ensures the successful course of pregnancy.
The introduction of hCG into the body of non-pregnant women stimulates ovulation and the synthesis of sex hormones necessary for conception. In men, this hormone enhances the formation of seminal fluid, activates the production of gonadosteroids. nine0003
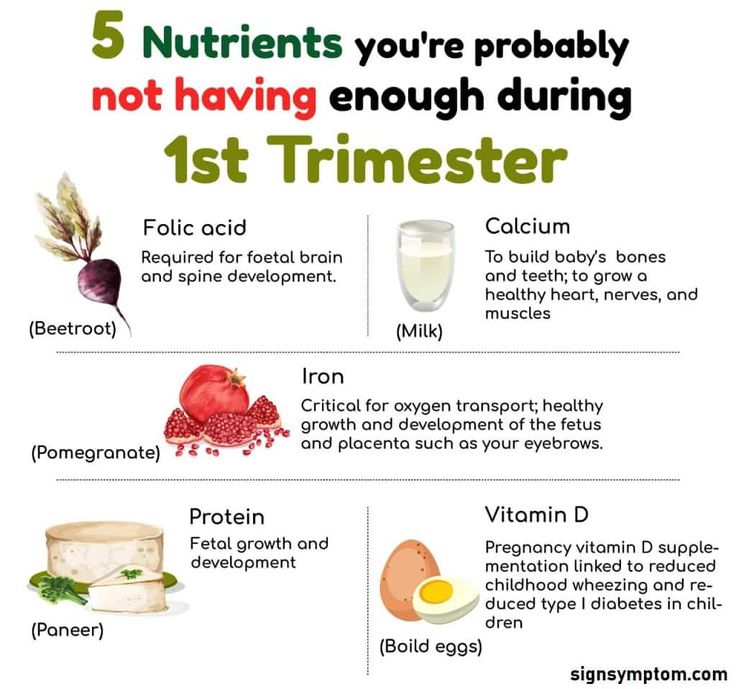
In early pregnancy and up to the 2nd trimester, β-hCG supports the production of hormones necessary to maintain pregnancy, and in male fetuses it stimulates cells responsible for the formation and development of the male reproductive system.
Human chorionic gonadotropin (hCG, beta-hCG, b-hCG, Human Chorionic)
Synonyms: Beta-hCG general.
Human Chorionic Gonadotropin; hCG; Pregnancy Quantitative hCG; Beta hCG; Total beta hCG. Brief description of the analyte Human chorionic gonadotropin ...
Up to 1 business day
Available with house call
RUB 685
In garbage
Indications for determining the level of hCG in women
- Absence of menstruation (amenorrhea).
- Exclusion/confirmation of pregnancy, including ectopic (ectopic). nine0008
- Diagnosis of the state of the fetus at different stages of pregnancy.
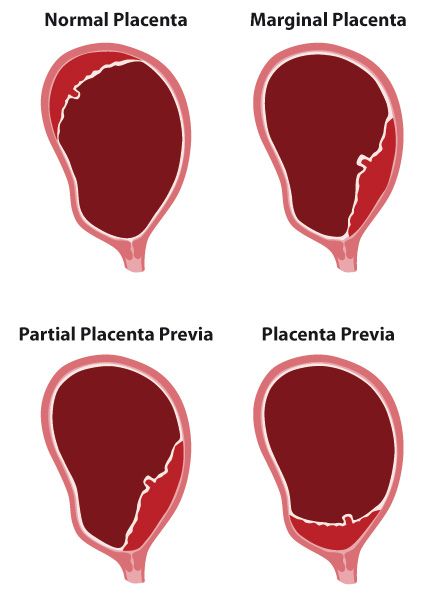
- Assessment of the state of the placenta at different stages of pregnancy.
- Dynamic monitoring of fetal development during pregnancy, including in the diagnosis of malformations.
- Suspicion of the presence of neoplastic diseases of the reproductive system, such as hydatidiform mole (a rare pathology of the fetal egg, in which instead of developing the embryo, chorionic villi grow), chorionepithelioma (a malignant tumor that develops from the epithelium of the villi of the fetal egg). nine0008
- Performing artificial termination of pregnancy.
Indications for determining the level of hCG in men:
The presence of suspicion of tumors of the testicles.
Deadline for this test is 1 working day, excluding the day of taking the biomaterial.
Rules for preparing for a blood test to determine the level of hCG
non-specific: it is enough to refrain from smoking and drinking alcohol on the eve of the procedure, limit stress and intense physical activity for a week; blood donation is carried out on an empty stomach.
nine0003
The determination of hCG in the blood is possible already on the 6-8th day after conception. The use of urinary test systems (rapid pregnancy tests) will be informative starting from the 7th day after the fertilization of the egg. To confirm the result, it is recommended to re-determine the level of the hormone a few days after the first analysis.
You can take a blood test for hCG (thyroid-stimulating hormone, thyrotropin, Thyroid StimulatingHormone, TSH) at the nearest INVITRO medical office. The list of offices where biomaterial for laboratory testing is accepted is presented in the "Addresses" section. nine0003
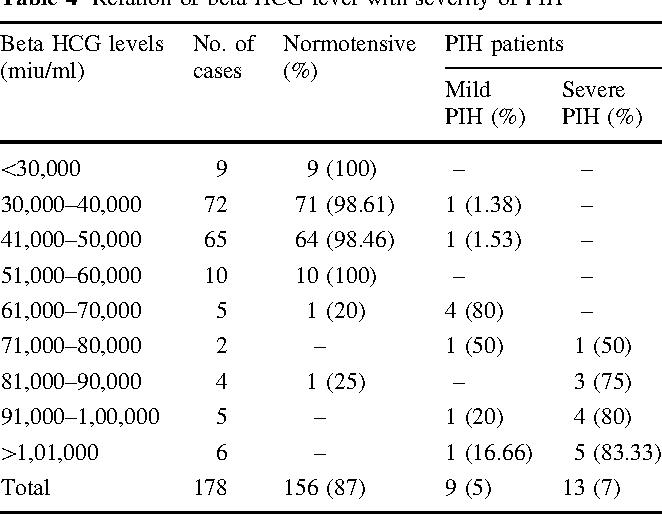
Reasons leading to high levels of β-hCG
- Multiple pregnancy.
- Incorrect timing of pregnancy.
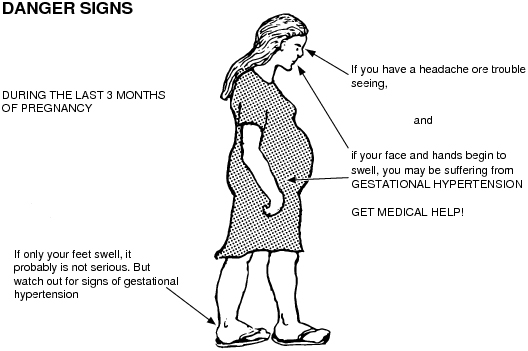
- Pathological pregnancy: the appearance of edema, increased blood pressure, loss of protein in the urine (preeclampsia), convulsions (eclampsia), toxicosis.

- The presence of a pregnant woman with chronic diseases (for example, diabetes mellitus). nine0008
- Multiple fetal malformations (in such a situation, the determination of the level of β-hCG is used together with other indicators, the so-called "triple test". This study is used as a screening, and not for diagnosis.).
Reasons for fixing a decrease in the level of β-hCG
- Incorrectly established terms of pregnancy.
- Ectopic pregnancy.
- Frozen pregnancy. nine0008
- Threat of miscarriage.
- Fetal or placental disorders (including placental insufficiency).
- Intrauterine fetal death (in this case, it is informative to determine the level of the hormone in the first and second trimesters).
During abortions, the level of β-hCG is also monitored, the dynamics of growth / fall of which can be used to judge the completeness of the manipulation.
Determining the level of hCG, in addition to establishing the fact of pregnancy in the early stages, is part of the screening examination of pregnant women in the first trimester, along with ultrasound. nine0003
1st trimester prenatal screening for trisomies, PRISCA-1 (1st trimester biochemical screening - 1st trimester “double test”, risk calculation using PRISCA software)
Synonyms: Prenatal Screening Markers for Down Syndrome; PRISCA-1. Brief description of the study "Prenatal screening for trisomies of the 1st trimester of pregnancy, PRISCA-1)" Test run...
Up to 1 business day
Available with house call
2 040 RUB
In garbage
Screening ultrasound 1st trimester of pregnancy (11-13 weeks 6 days)
Examination necessary to monitor the growth and development of the fetus in the first trimester of pregnancy.
RUB 2,790 Sign up nine0003
In gynecological practice, human chorionic gonadotropin is used to treat infertility, stimulate ovulation, and synthesize sex steroids. In urology, it is used in the treatment of cryptorchidism (undescended testicles) and infertility associated with impaired spermatogenesis.
Quantitatively, β-hCG is determined in the blood, for a qualitative determination, special test systems (pregnancy tests) are used, and in this case, urine serves as a biomaterial.
Quantitative determination of the level of hCG allows you to monitor the course of pregnancy in dynamics. To do this, obstetrician-gynecologists have developed tables for increasing the level of hCG, depending on the duration of pregnancy in weeks. The sensitivity of the determination is in the range of 1.2-1125000 mU/ml. nine
Pregnancy (weeks from conception) HCG level (mU / ml) 2 25–300 3 1500–5000 nine00394 10000–30000 five 20000–100000 6–11 20000–>225000 12 19000–135000 13 18000–110000 nine0039fourteen 14000–80000 fifteen 12000–68000 16 10000–58000 17–18 8000–57000 nineteen 7000–49000 nine003920–28 1600–49000 Men and non-pregnant women 0–<5 mU/ml Values ranging from 5 to 25 mU / ml do not allow unambiguous confirmation or denial of pregnancy, therefore, a second study is required after two days.
Since the hormone is produced by the placenta, during normal pregnancy, with placental pathology (for example, with fetoplacental insufficiency - a violation of the development of the fetus and placenta), with multiple pregnancies, the values of β-hCG will differ. With a normal pregnancy until the fifth week, the level of the hormone rises exponentially: every two days its concentration doubles, reaching a peak by the 11th week of gestation. Accordingly, in a multiple pregnancy, the level of β-hCG will be even higher than in a single pregnancy. nine0003
If the indicator deviates from the norm, additional ultrasound of the pelvic organs (uterus, appendages) is required.
US examination of pelvic organs (uterus, adnexa)
Ultrasound scanning of the female reproductive system to assess the shape and size, as well as exclude pathology.
RUB 2,390 Sign up nine0003
However, with a normal hCG value, additional examinations may also be needed:
- Ultrasound diagnosis of pregnancy (required to confirm pregnancy, clarify the term).
Ultrasound diagnosis of pregnancy
Examination to confirm pregnancy and determine the place of attachment of the ovum (to exclude ectopic pregnancy).
RUB 2,290 Sign up nine0003
- Screening ultrasound of the 1st trimester of pregnancy (11-13 weeks 6 days) - to assess the characteristics and confirm the normal development of the fetus.
Screening ultrasound of the 1st trimester of pregnancy (11-13 weeks 6 days)
Examination necessary to monitor the growth and development of the fetus in the first trimester of pregnancy.
RUB 2,790 Sign up nine0003
- Screening ultrasound of the 1st trimester of multiple pregnancy (11-13 weeks 6 days) - to confirm the presence of several fetuses, determine their characteristics; It is necessary for planning the subsequent actions of the doctor and the management of pregnancy.
Screening ultrasound of the 1st trimester of multiple pregnancy (11-13 weeks 6 days)
Examination to assess the growth and development of fetuses, their position in the uterus, and make a plan for further pregnancy management. nine0003
RUB 3,840 Sign up
- Fetal ultrasound according to indications (before the 20th week) - performed in case of suspected ectopic pregnancy.
Fetal ultrasound according to indications (before the 20th week)
Additional ultrasound, which is prescribed in the presence of concomitant pathologies to monitor the condition of the fetus.
RUB 2,540 Sign up nine0003
- Laboratory tests to be performed in the first trimester are collected in the Pregnancy: 1st trimester (1-13 weeks) profile.
For professional assistance in interpreting the results, contact
obstetrician-gynecologist
.
Sources:
- www.invitro.ru
- Clinical guidelines "Ectopic (ectopic) pregnancy". Developed by: Russian Society of Obstetricians-Gynecologists, Association of Obstetric Anesthesiologists-Resuscitators. – 2021.
- Clinical guidelines "Premature birth". Developed by: Russian Society of Obstetricians-Gynecologists, Association of Obstetric Anesthesiologists-Resuscitators. – 2020.
IMPORTANT!
The information in this section should not be used for self-diagnosis or self-treatment. In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor. nine0455 For a correct assessment of the results of your analyzes in dynamics, it is preferable to do studies in the same laboratory, since different laboratories may use different research methods and units of measurement to perform the same analyzes.

Recommendations
nine0002 Show more
PSA (prostate specific antigen) test
9070 may 13 nine0003
Human papillomavirus
13230 04 May
Alkaline phosphatase
4578 16 April
Similar articles
ECO
Hypogonadism
Menopause
Climax
nine0590 Anti-Mullerian hormone (AMH, AMH, anti-Mullerian hormone)Anti-Mullerian hormone: indications for prescription, rules for preparing for the test, interpretation of the results and indicators of the norm.
More
ECO
Thrombophilia
nine0002 PregnancyThrombosis: extended panel 114ГП
Thrombosis, extended panel: indications for prescribing, rules for preparing for an analysis, interpretation of results and norm indicators.
More
Infertility
Varicocele
nine0002 ECOSpermogram in INVITRO
Sperm analysis is an integral part of infertility diagnostics and monitoring of diseases of the male genital area.
The analysis of the ejaculate includes the determination of the quantitative and qualitative morphological composition of spermatozoa using visual counting in the Goryaev chamber and special staining.
More
nine0002 ECOBlood transfusion
Pregnancy
Rh-affiliation (Rh-factor, Rh)
Rh-affiliation: indications for the appointment, rules for preparing for the analysis, interpretation of the results and norm indicators.
More nine0003
ECO
Thrombophilia
Stroke
Obesity
COVID-19
nine0002 Nephrotic syndromePregnancy
Propensity to thrombosis during pregnancy - minimal panel
Propensity to thrombosis during pregnancy: indications for prescribing, rules for preparing for the test, interpretation of the results and indicators of the norm.