Anus pressure during pregnancy
Causes, in Pregnancy, Home Remedies, Treatment
We include products we think are useful for our readers. If you buy through links on this page, we may earn a small commission. Here’s our process.
Healthline only shows you brands and products that we stand behind.
Our team thoroughly researches and evaluates the recommendations we make on our site. To establish that the product manufacturers addressed safety and efficacy standards, we:
- Evaluate ingredients and composition: Do they have the potential to cause harm?
- Fact-check all health claims: Do they align with the current body of scientific evidence?
- Assess the brand: Does it operate with integrity and adhere to industry best practices?
We do the research so you can find trusted products for your health and wellness.
Read more about our vetting process.Overview
Anus pain is known as proctalgia and can have many causes. The anus is where your large intestine opens into your buttocks at the rectum. The anus is the last passageway of the gastrointestinal (GI) tract.
The anus is surrounded by muscles known as sphincter muscles. These tighten and relax the anus when you pass waste. Your tailbone (coccyx), the last bone in your spine, and many nerves are also near your anus.
Read on to learn what causes anus pain, how you can treat it at home, what medical treatments are available, and how you can help prevent this type of pain.
Anal pain can have a variety of causes.
1. Sitting for a long time
Sitting down for a long time, especially on a hard surface, can cause temporary anal pain by putting pressure on anal nerves and muscles. Even sitting for a short time on a hard surface can cause anal pain that lasts for hours after you get up.
You don’t need to see your doctor for this kind of pain.
If the pain persists for a few days after a long period of sitting, see your doctor. They can diagnose any injury to your anus muscles, tailbone, or the surrounding structures.
They can diagnose any injury to your anus muscles, tailbone, or the surrounding structures.
2. Diarrhea
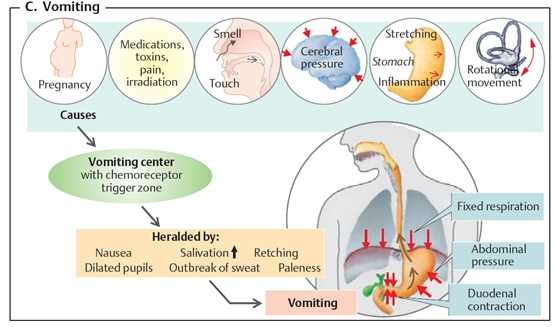
Diarrhea happens when you pass watery, loose stool more than three times in a day. Diarrhea can have many causes, such as dietary changes (being dehydrated or not eating enough fiber), and infections like gastroenteritis, colitis, or diverticulitis.
Frequently passing stool can make your anus sore. This can get worse from wiping or cleaning. Your anal tissue can become raw and bleed, too.
Other diarrhea symptoms include:
- feeling bloated or gassy
- cramping in your lower abdomen
- feeling nauseous
- not being able to hold in your stool
Diarrhea often goes away on its own. Seek emergency medical attention if you have any of the following symptoms, though:
- diarrhea for more than two days
- fever
- blood in your stool
- black or discolored stool
- loss of consciousness
3. Injury
Falling on your butt can injure the muscles, bones, or nerves around the anus. The sudden impact of a hard surface can bruise or damage your skin, muscles, or nerve endings as well as potentially fracture bones.
The sudden impact of a hard surface can bruise or damage your skin, muscles, or nerve endings as well as potentially fracture bones.
This type of injury is most common during activities like contact sports, such as football and soccer, or activities like skateboarding, rollerblading, or gymnastics.
Depending on how severe the injury is, pain may radiate up from your anus to your lower back and feel like a constant ache or throb. You may notice bruises on your buttocks.
Seek immediate medical attention if:
- the pain is sharp and constant
- you can’t walk or get up without severe pain
- you lose sensation in your lower back or in one or both legs
4. Fissures
Anal fissures happen when your anal tissues tear. Passing especially hard or large stool is the most common culprit. The pain is often sudden and sharp at first. Your anus may ache for hours or days afterward until the fissure heals.
Symptoms of an anal fissure include:
- feeling sudden, unusual pain in or around your anus when you pass stool
- bleeding from your anus, especially when you wipe
- pain that lasts for hours after you pass stool
Fissures don’t always require immediate medical treatment.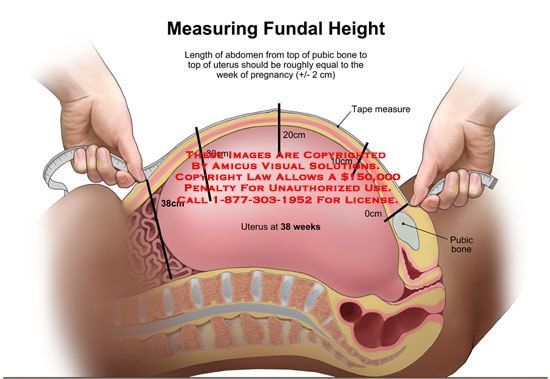 See your doctor if the pain persists or gets significantly worse when you sit down, pass stool, or walk.
See your doctor if the pain persists or gets significantly worse when you sit down, pass stool, or walk.
5. Hemorrhoids
Hemorrhoids happen when anal blood vessels are swollen. Straining to pass stool or being constipated are often the causes of hemorrhoids.
When you have a hemorrhoid, you may feel a lump near your anus. The pain may be generally dull but sharp when you sit down. You may not feel comfortable sitting without a special cushion or pillow. In some cases, you may not notice any symptoms.
Common symptoms of hemorrhoids include:
- constant pain, soreness, or itching around your anus
- bleeding from your anus when you pass stool
- sharp anal pain if blood in the hemorrhoid becomes clotted
Hemorrhoids can go away on their own, but severe hemorrhoids may require medical treatment. See your doctor right away if you:
- have trouble passing stool
- can’t sit without sharp or severe pain
- notice blood in your stool
6.
 Menstruation
MenstruationMenstruation can cause anal pain along with other symptoms related to your digestive tract.
Your rectum and anus may be more sensitive during this time. This can make your anus feel tender, sore, or uncomfortable. Common period symptoms, such as diarrhea and bloating, can make anal pain even more pronounced.
You don’t need to see your doctor to treat these symptoms. They usually go away once your period is over.
7. Anal spasms (proctalgia fugax)
Anal spasms happen when you get sharp, unexpected anal pain due to anal sphincter muscle contractions. It’s relatively common. A 2013 review estimates it affects between 8 and 18 percent of people.
The cause of this condition isn’t well known. It’s more likely to occur if you have irritable bowel syndrome (IBS) or anxiety as well as after hemorrhoid surgery or a hysterectomy.
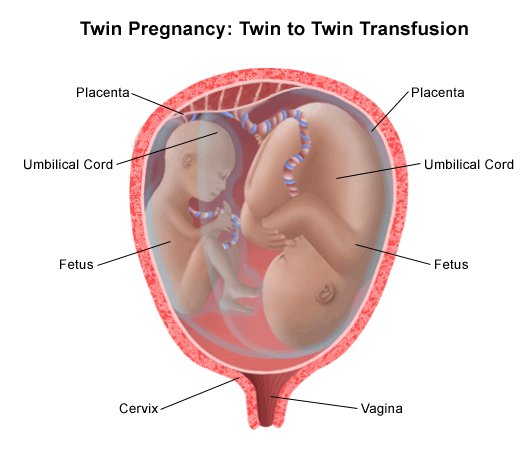
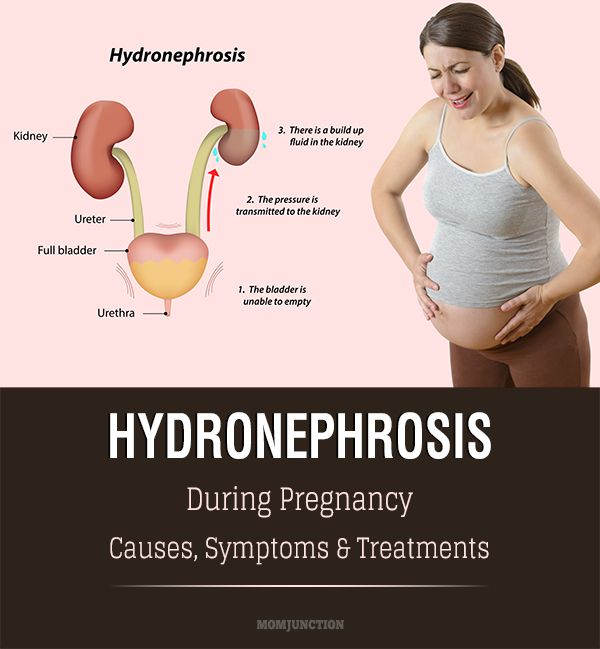
When you’re pregnant, your uterus becomes enlarged, which puts pressure on your anus. That can lead to discomfort or pain.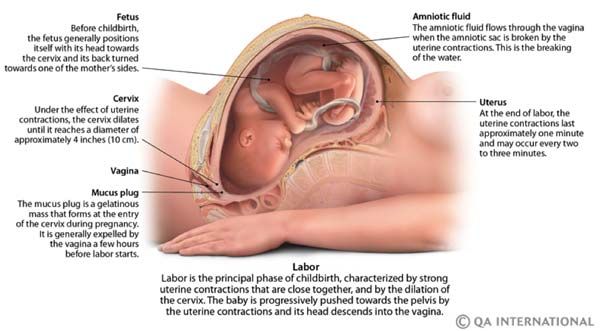 This extra pressure can also cause hemorrhoids, which can make your anus uncomfortable.
This extra pressure can also cause hemorrhoids, which can make your anus uncomfortable.
Anal pain during pregnancy is most common during the third trimester, when your baby is larger and may put more pressure on your anal nerves. Contractions during labor can also cause pain in your anus.
In many cases, you should be able to treat anal pain at home. Here are some home remedies to try:
- Take a sitz bath. Buy a sitz bath at your local drugstore or online and mount it in your toilet bowl. Fill it with warm water and Epsom salt, then sit on top of the sitz bath with the water immersing your anus. Soak for 15 to 20 minutes.
- Use over-the-counter (OTC) creams or ointments. Apply a small amount of cream or ointment, such as lidocaine or cortisone, to reduce pain and speed up the healing process of irritated skin.
- Use a cold compress. You can make your own cold compress at home by wrapping an ice pack or bag of frozen vegetables in a towel.
 Press it against your anal area to help relieve pain. Do this 20 minutes at a time, three to four times daily.
Press it against your anal area to help relieve pain. Do this 20 minutes at a time, three to four times daily. - Take OTC pain medicine for pain relief. Ibuprofen (Advil, Motrin) or acetaminophen (Tylenol) can temporarily relieve anal pain until any cuts or injuries heal.
Seek emergency medical treatment if:
- Your anal pain makes you unable to walk, pass waste, stand, or sit.
- You notice blood in your stool.
- You have a fever.
- You’re severely dehydrated.
- You can’t eat or pass stool.
Medical treatment depends on the cause of pain and the severity of your symptoms.
Treatment for injuries
You may need X-rays or other imaging tests to see the extent of any damage to your tailbone or spine. Severe spinal injuries may require surgery or long-term rehabilitation to restore any lost mobility.
Treatment for diarrhea
If you’re severely dehydrated, you may need intravenous fluids (IV) to replenish your body fluids. If a bowel disorder is causing diarrhea, such as IBS or Crohn’s disease, your doctor may prescribe you medication or a treatment plan to help reduce symptoms.
If a bowel disorder is causing diarrhea, such as IBS or Crohn’s disease, your doctor may prescribe you medication or a treatment plan to help reduce symptoms.
Treatment for a fissures
Chronic anal fissures may require surgery so that you can pass stool without injuring your sphincter muscles. Your doctor may also recommend adding fiber to your diet to help you pass stool more easily.
Treatment for hemorrhoids
Your doctor may wrap the hemorrhoid with a rubber band until it shrinks. Surgery to cut or freeze the hemorrhoid are also possible treatment options. In severe cases, your doctor may need to remove the hemorrhoid tissues and blood vessels in a hemorrhoidectomy procedure.
It may not always be possible to prevent anal pain. But there are things you can do to reduce your risk:
- Stay hydrated. Drink at least 64 ounces of water per day to make your stool easier to pass.
- Sit with good posture.
 When sitting,straighten your back and keep your knees bent at a 90-degree angle.
When sitting,straighten your back and keep your knees bent at a 90-degree angle. - Get up and walk around at least once every 30 to 50 minutes. This reduces long-term pressure on muscles and nerves in your anus and lower spine.
- Don’t strain when you pass stool. Straining can cause discomfort, hemorrhoids, and anal fissures.
- Eat a healthy diet. Eat plenty of fiber so that you regularly pass stool and prevent constipation.
- Wear loose, breathable underwear. Wear 100 percent cotton underwear to prevent your anus from becoming moist with sweat, which could lead to irritation.
- Consider using moist wipes or jets of water instead of toilet paper. Toilet paper can scratch and cut your anal skin, making you more prone to infections. Moist wipes and bidets are gentler on your skin.
- Don’t eat raw, uncooked, or untrustworthy food.
 Food and unfiltered water can contain bacteria or other microbes that can lead to diarrhea. Make sure your food is properly cooked and that your water is clean.
Food and unfiltered water can contain bacteria or other microbes that can lead to diarrhea. Make sure your food is properly cooked and that your water is clean.
Many things can lead to anal pain, some serious and others not.
If the pain is bearable and starts to fade quickly after it starts, there’s no need for concern. If pain persists for more than a few days and accompanies other painful or disruptive symptoms, see your doctor for immediate treatment.
Butt Pain During Pregnancy: How to Cope
Butt Pain During Pregnancy: How to CopeMedically reviewed by Janine Kelbach, RNC-OB — By Rachel Nall, MSN, CRNA on November 6, 2018
We include products we think are useful for our readers. If you buy through links on this page, we may earn a small commission. Here’s our process.
Healthline only shows you brands and products that we stand behind.
Our team thoroughly researches and evaluates the recommendations we make on our site. To establish that the product manufacturers addressed safety and efficacy standards, we:
To establish that the product manufacturers addressed safety and efficacy standards, we:
- Evaluate ingredients and composition: Do they have the potential to cause harm?
- Fact-check all health claims: Do they align with the current body of scientific evidence?
- Assess the brand: Does it operate with integrity and adhere to industry best practices?
We do the research so you can find trusted products for your health and wellness.
Read more about our vetting process.Overview
If you’re pregnant, you probably expected to experience some back pain and abdominal discomfort. But what you didn’t count on was butt pain.
As your pregnancy progresses, there are common conditions like sciatica that can cause you a great deal of discomfort. You might feel pain in the buttocks area as a result.
Luckily, as you continue to wait for your little one to enter the world, there are several steps you can take to reduce butt pain.
Here’s how to make the next few months more comfortable before your baby makes their arrival.
Causes of butt pain during pregnancy
Butt pain during pregnancy can be pain caused by an abnormality on the buttocks itself (like hemorrhoids). It can also be referred pain that radiates from the lower back to the buttocks.
Some common causes of butt pain during pregnancy include the following.
Hemorrhoids
Hemorrhoids are enlarged, swollen veins in the anus or rectum. Pregnant women are more likely to experience hemorrhoids because the uterus creates extra pressure on the anus and rectum.
If you have to stand for long periods of time because of your job or hobbies, the pain may get worse.
Labor pains/Contractions
Women experience contractions differently. Some have abdominal cramping and back cramping that can extend to the buttocks. The nature of the pain can vary, too. Some people feel a cramping sensation while others may feel pressure, throbbing, or shooting pain.
Braxton-Hicks contractions may cause discomfort, but they aren’t usually painful. If the contractions are causing your buttocks pain, call your doctor.
Pelvic girdle pain
Pelvic girdle pain affects 1 in 5 pregnant woman. This pain occurs when the extra weight of the baby and pregnancy-related movements in the pelvis start to add up and cause pelvic pain.
Many women also experience this pain in their buttocks. Other symptoms can include feeling a grinding or clicking in the pelvic area, and pain that gets worse with movement.
Although pelvic girdle pain is very uncomfortable, it isn’t harmful to your baby. It won’t keep you from having a vaginal birth.
Sciatica
Sciatica is a condition that happens when there’s pressure on the sciatic nerve that runs from the buttocks down the leg. Pregnancy can cause the nerve to become irritated or inflamed. Your expanding uterus can place extra pressure on the sciatic nerve.
As you reach your third trimester, your baby’s change in positioning can rest on the nerve directly in your buttocks area.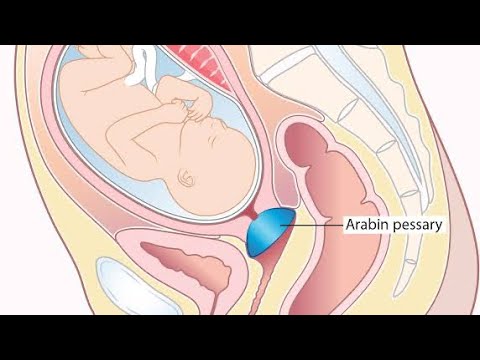 This can cause butt pain.
This can cause butt pain.
You also might feel a burning sensation in your back, buttocks, and leg. Some women also report shooting pain that extends down the leg.
When to call your doctor
Whatever the cause, butt pain can make it difficult to complete your daily activities comfortably. (As if it wasn’t hard enough already with your pregnancy!)
If you experience the following symptoms, it’s time to call your doctor:
- the pain is so severe that it is making you feel ill
- you are experiencing a significant amount of blood loss (bigger than typical hemorrhoids, which may cause only a smear of blood)
- you have experienced a rush of fluid from your vagina or your “water breaking”
- you lose control of your bladder/bowels
- the pain never subsides
Medical treatments
An estimated 14 percent of pregnant women take an opioid pain medication while they’re pregnant. Examples of these prescription medications include oxycodone and hydrocodone.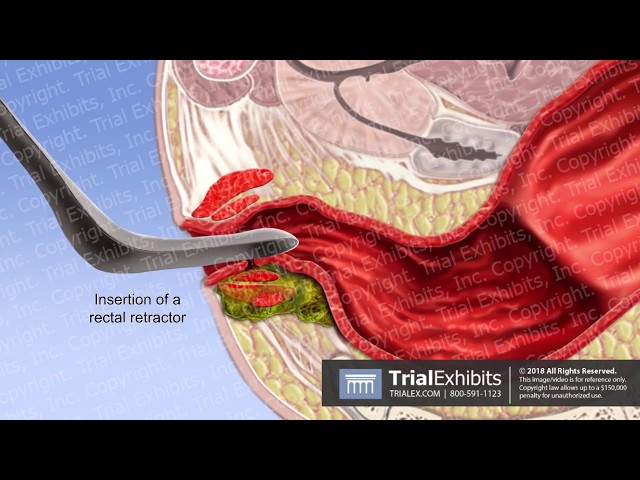
Typically, women take them for a week or less. Back pain’s the most common reason doctors prescribe these medications.
If your buttocks pain does not respond to over-the-counter and at-home treatments, your doctor may consider prescribing a pain medicine.
But the fewer medications you can take during pregnancy, the better. This will reduce the likelihood the medications could affect your baby’s growth and/or development.
At-home treatments
If your pain is the result of hemorrhoids, you can try the following at-home treatments to reduce discomfort:
- Soak in a warm water bath or a sitz bath. A sitz bath is a plastic bath that can fit over your toilet. You can fill it with warm water, sit, and soak without having to draw a bath. Shop for sitz baths.
- Try witch hazel. Place a few drops of witch hazel on a sanitary pad that you can wear to reduce inflammation. You can change the witch hazel pads throughout the day to reduce inflammation.
 Also try freezing them for more relief. Shop for witch hazel.
Also try freezing them for more relief. Shop for witch hazel. - Don’t sit or stand too long. Refrain from sitting or standing for extended time periods. This puts extra pressure on your anus. Lying on your side can reduce pressure.
- Drink up. Drink plenty of fluids each day. This can help reduce your risk for constipation, which makes your stool harder to pass.
- Eat fiber. Eat a diet that has plenty of fiber with whole-grain foods, fruits, and vegetables.
You can also ask your doctor if there are creams and/or stool softeners you could take to reduce hemorrhoid-related pain and strain.
Shop for stool softeners.
Sciatica treatments
For pain related to sciatica and/or pelvic pain, you can take the following steps:
- Take an over-the-counter pain reliever like acetaminophen to reduce discomfort.
- Take a warm bath and/or shower to soothe tight muscles.
- Wear a supportive pelvic belt (also called a girdle) to reduce the pressure on your lower back and pelvis.
 Shop for pelvic belts.
Shop for pelvic belts. - Avoid performing activities that aggravate your pain, like lifting heavy objects, standing on only one leg at a time, and keeping your legs together when you turn in bed and/or get out of the car.
- Place a pillow under your belly and one between your legs when you sleep. This can help promote proper body positioning.
You can also ask your doctor if you can apply cold and/or heat packs to painful areas.
The takeaway
Pregnancy-related butt pain will typically resolve after you deliver. But some women may continue to experience hemorrhoids post-delivery. You can ask your doctor if there are other treatments you can use to reduce the frequency of butt pain.
Share on Pinterest
Last medically reviewed on November 7, 2018
- Parenthood
- Pregnancy
- Pregnancy Health
How we reviewed this article:
Healthline has strict sourcing guidelines and relies on peer-reviewed studies, academic research institutions, and medical associations. We avoid using tertiary references. You can learn more about how we ensure our content is accurate and current by reading our editorial policy.
We avoid using tertiary references. You can learn more about how we ensure our content is accurate and current by reading our editorial policy.
- Giannoudis, P. V., Kanakaris, N. K., & Roberts, C. S. (2011, February 15)
ncbi.nlm.nih.gov/pmc/articles/PMC3050758/ - Hemorrhoids. (2009, August)
marchofdimes.org/pregnancy/hemorrhoids.aspx - How do you treat pregnancy hemorrhoids and constipation. (2013, January)
kidshealth.org/parent/pregnancy_center/q_a/piles.html - How to handle sciatica during your pregnancy. (2014, December 17)
health.clevelandclinic.org/2014/12/how-to-handle-sciatica-during-your-pregnancy/ - More than 14 percent of pregnant women prescribed opioids, study says. (2014, February 12)
asahq.org/about-asa/newsroom/news-releases/2014/02/opioids-in-pregnancy - Pelvic girdle pain and pregnancy. (2015)
rcog.org.uk/globalassets/documents/patients/patient-information-leaflets/pregnancy/pi-pelvic-girdle-pain-and-pregnancy.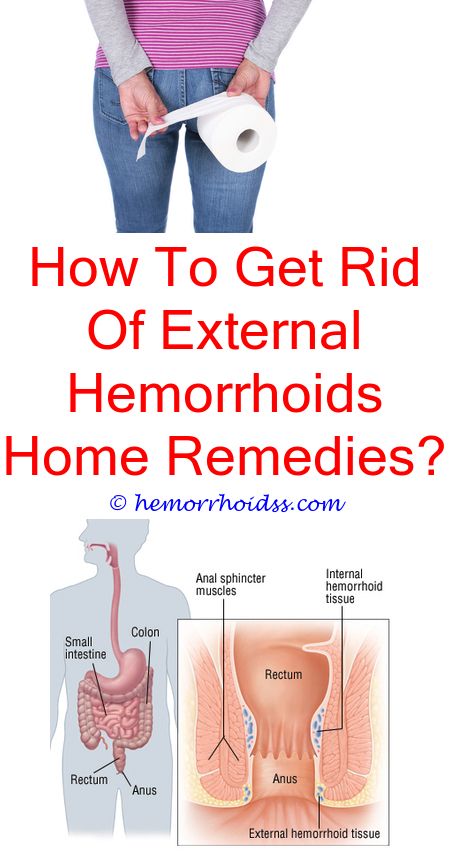 pdf
pdf - Types of back pain in pregnancy. (2009, December 3)
spine-health.com/conditions/pregnancy-and-back-pain/types-back-pain-pregnancy - What can I do to treat hemorrhoids during pregnancy? (2014, November 11)
mayoclinic.org/healthy-lifestyle/pregnancy-week-by-week/expert-answers/hemorrhoids-during-pregnancy/faq-20058149
Our experts continually monitor the health and wellness space, and we update our articles when new information becomes available.
Current Version
Nov 7, 2018
Written By
Rachel Nall, MSN, CRNA
Edited By
Frank Crooks
Medically Reviewed By
Janine Kelbach, RNC-OB
Share this article
Medically reviewed by Janine Kelbach, RNC-OB — By Rachel Nall, MSN, CRNA on November 6, 2018
related stories
How to Identify Lightning Crotch Pain During Pregnancy
How to Manage Back Spasms During Pregnancy
First Trimester Pregnancy Back Pain: Causes and Treatments
Sciatica During Pregnancy: Symptoms, Causes, Treatments
13 Home Remedies for Swollen Feet During Pregnancy
Read this next
How to Identify Lightning Crotch Pain During Pregnancy
Medically reviewed by Deborah Weatherspoon, Ph.
 D., MSN
D., MSNIn your third trimester and having some shooting pain “down there”? In general, lightning crotch pain is a normal part of pregnancy and nothing to get…
READ MORE
How to Manage Back Spasms During Pregnancy
Medically reviewed by Debra Rose Wilson, Ph.D., MSN, R.N., IBCLC, AHN-BC, CHT
One of the most common complaints during pregnancy is back pain and, specifically, back spasms. Learn why this happens and how you can treat it.
READ MORE
First Trimester Pregnancy Back Pain: Causes and Treatments
Medically reviewed by Kimberly Dishman, MSN, WHNP-BC, RNC-OB
Back pain during the first trimester might be one of the first pregnancy symptoms you experience. Here’s what’s causing it and how to treat it safely.
READ MORE
Sciatica During Pregnancy: Symptoms, Causes, Treatments
Medically reviewed by Beth Holloway, RN, MEd
Many pregnant women experience sciatic pain.
 Here's a look at the causes, symptoms, and ways to find relief.
Here's a look at the causes, symptoms, and ways to find relief. READ MORE
13 Home Remedies for Swollen Feet During Pregnancy
Medically reviewed by Meredith Wallis, MS, APRN, CNM, IBCLC
Swollen feet during pregnancy is very common, but that doesn't mean you have to be uncomfortable. We'll cover some effective ways to deal with the…
READ MORE
Causes of Hemorrhoids and Tips for Prevention
Medically reviewed by Lauren Castiello, MS, AGNP-C
Hemorrhoids, also known as piles, are swollen veins located around the anus or in the lower rectum.
READ MORE
The Best Pregnancy Apps of 2020
These are the best iPhone and Android apps to find information, answers, tools, and tracking during your pregnancy. From scheduling doctor’s visits…
READ MORE
14 Recipes to Ease Morning Sickness
Medically reviewed by Natalie Butler, R.
 D., L.D.
D., L.D.Morning sickness got you down? Get over your nausea with one of these 14 delicious, easy recipes.
READ MORE
Hemorrhoid Surgery Types: Outpatient and Inpatient
Medically reviewed by Saurabh Sethi, M.D., MPH
Hemorrhoids are swollen veins that appear near the rectum. If you have a severe case that doesn't resolve with home treatment, there are a number of…
READ MORE
7 Books That Shine a Light on Pregnancy
For everything from what to eat during pregnancy to how to plan for birth and what comes after, check out these best pregnancy books!
READ MORE
Hemorrhoids during pregnancy - what symptoms to recognize and how to treat
Hemorrhoids during pregnancy - cure the mother, do not harm the baby
Pregnant women always think about the health of the unborn baby, forgetting to pay due attention to their body.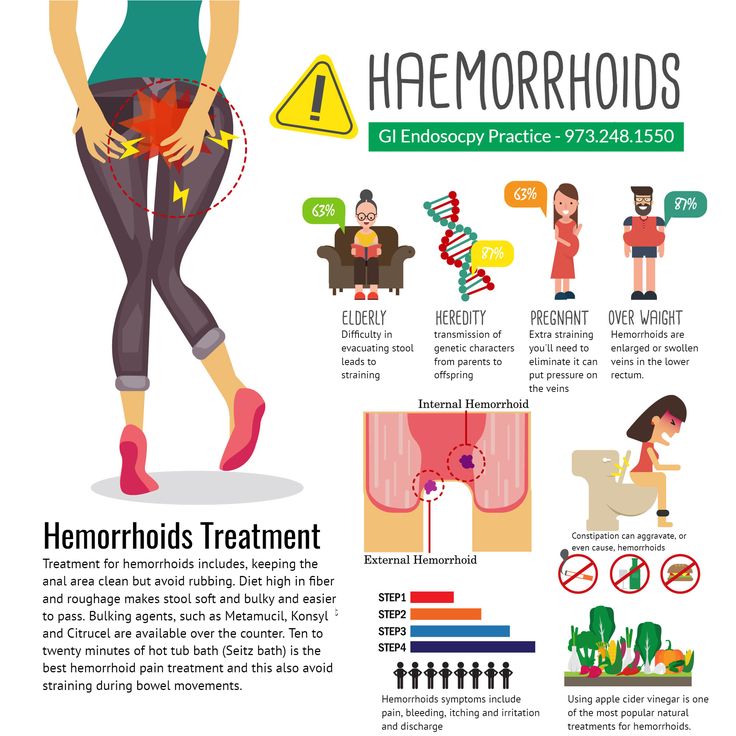 One of the most common diseases during this period is hemorrhoids. And it is very important to cure the mother, not harm the child and forget about this problem forever.
One of the most common diseases during this period is hemorrhoids. And it is very important to cure the mother, not harm the child and forget about this problem forever.
Symptoms of hemorrhoids and several stages of development
Hemorrhoids in pregnant women are hard to miss. It develops gradually. If the disease is detected at the first stage, then the treatment will not take much time, and the discomfort will disappear on the second day. There are several stages of hemorrhoids, and you need to focus immediately on the signs of the initial stage:
- pulling pain in the anus;
- discomfort and discomfort that does not go away after emptying;
- mild and non-systematic bleeding; nine0015
- appearance of nodules;
- the beginning of the inflammatory process in the mucosa.
When contacting a doctor at this stage, properly prescribed treatment and prevention, hemorrhoids will disappear forever, without causing trouble to the expectant mother.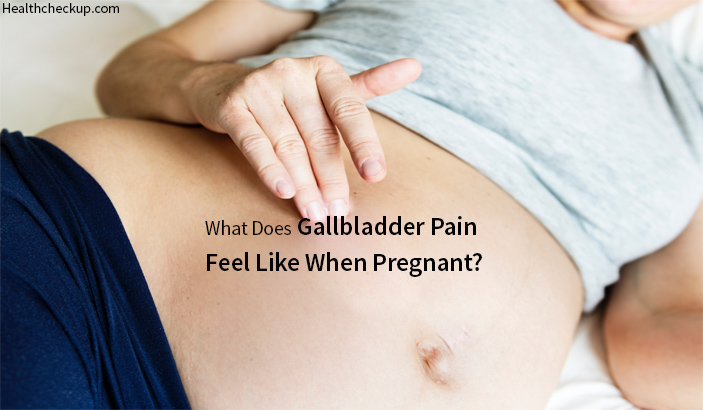 The second stage is itching in the anus, increased pain, growth and prolapse of nodes.
The second stage is itching in the anus, increased pain, growth and prolapse of nodes.
Attention! It is not recommended to self-medicate at any stage of the disease. This is especially true for women who are expecting a baby. Incorrectly selected drugs or traditional medicine can forever deprive a woman of the joys of motherhood. nine0005
The third stage requires intervention: the knots already have to be adjusted by hand, and the pain in the anus is getting worse. Hemorrhoids during pregnancy at the fourth stage are very difficult and dangerous for mom and baby. Thrombosis and heavy bleeding may appear, requiring serious medical and surgical intervention.
The development of hemorrhoids in expectant mothers - the main factors
As soon as the blood supply to the rectum is disturbed and the vessels become inelastic, weak, begin to stretch, there is a risk of inflammatory processes. To cure hemorrhoids in pregnant women, the doctor needs to find out the reasons that led to it. There are four main factors that provoke the onset of a serious illness. nine0005
There are four main factors that provoke the onset of a serious illness. nine0005
Chronic constipation. During pregnancy, bowel tone is weakened, constipation is common, and stretching of the intestinal walls increases. Also, tension increases during emptying - nodules, cracks, bleeding appear.
Low activity and sedentary lifestyle. Before treating hemorrhoids in pregnant women, the doctor conducts a survey. If a woman moves little, blood stagnation occurs in the small pelvis, which results in thrombosis of the venous vessels. nine0011
Circulatory disturbance due to pressure of the enlarged uterus on the vena cava. This leads not only to inflammation in the rectum, but also to stagnation of blood in the legs.
Nutrition. Spicy, highly salty and smoked food causes blood to rush to the organs of the small pelvis. If you eat such food often, the blood stagnates, and seals form.
If hemorrhoids occur during pregnancy, treatment should only be under medical supervision. These risk factors, often combined with hormonal changes in the body of a pregnant woman, without prevention and timely medical intervention, will lead to a serious disease that can develop into a chronic one. nine0005
If time was lost during pregnancy, hemorrhoids after childbirth can become a chronic disease. It is important not to miss the moment and turn to a good specialist who will quickly put the mother's body in order.
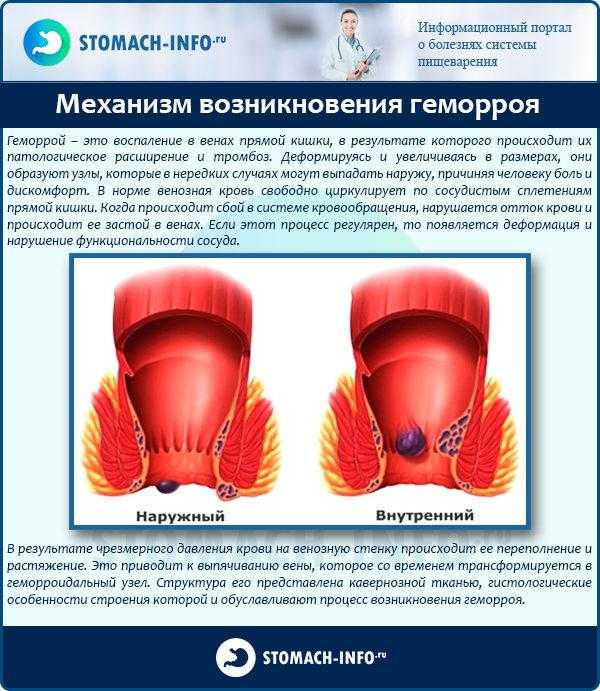
Types of hemorrhoids in pregnant women
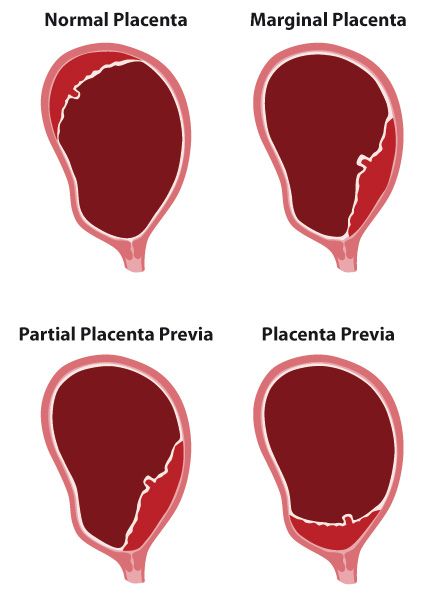
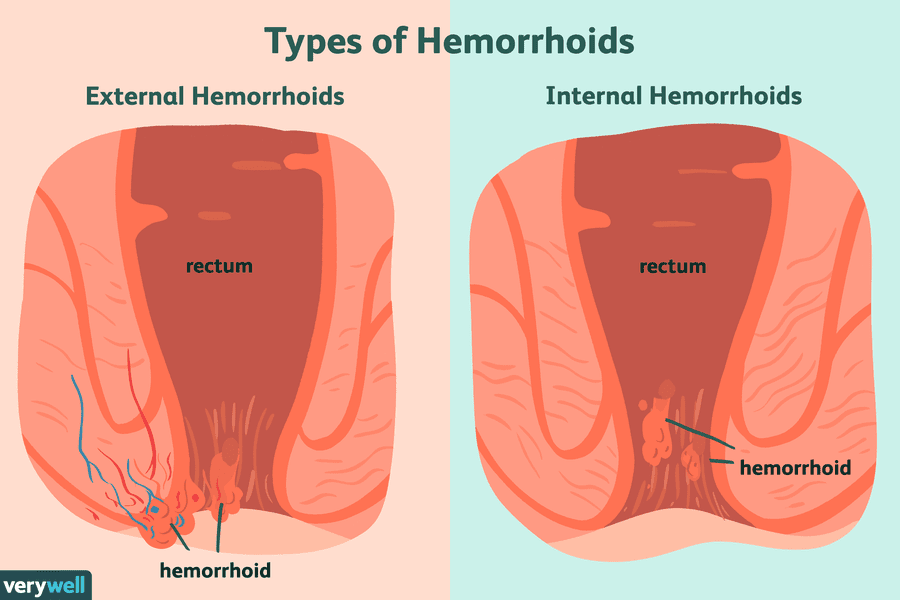
Hemorrhoids are of several types. If the nodes are located inside - internal. They are located in the middle of the intestine, but can sometimes, with strong tension, fall out. When external nodules are placed around the anus. They are well palpable and visible to the naked eye. nine0005
Treatment of hemorrhoids after childbirth or during pregnancy also depends on whether it is congenital or acquired, acute or chronic. The chronic form lasts several months or years if the woman does not see a doctor. During a relapse, unpleasant sensations and pulling pains appear in the lower abdomen, in the region of the anus. Minor or severe bleeding may occur with constipation. In the intervals between exacerbations, the pain subsides, the discomfort disappears. There comes a period of remission, which can also last a very long time. nine0005
The chronic form lasts several months or years if the woman does not see a doctor. During a relapse, unpleasant sensations and pulling pains appear in the lower abdomen, in the region of the anus. Minor or severe bleeding may occur with constipation. In the intervals between exacerbations, the pain subsides, the discomfort disappears. There comes a period of remission, which can also last a very long time. nine0005
Chronic hemorrhoids after pregnancy or in pregnant women can develop in four stages.
- Discharge of blood during bowel movements.
- Nodes falling out.
- Knots have to be adjusted, they do not hide themselves.
- With any slight load - coughing, sneezing, lifting the child into the arms, the knots fall out and it is impossible to set them back on their own.
In order to prevent the last stage of the disease and permanently cure hemorrhoids after childbirth, treatment should be carried out by qualified doctors on the basis of a licensed medical institution. nine0005
nine0005
Medical and surgical treatment of hemorrhoids
As soon as the first signs of the disease are detected, a diagnosis is made and the condition of the mother and fetus is examined, treatment is prescribed. While a woman is carrying a baby, she can be prescribed gels, suppositories, ointments and special creams. The following types of treatment can also be used according to the doctor's prescription:
- phlebotropic drugs that improve lymph outflow, increase the elasticity of blood vessels; nine0014 microclysters to soften the stool and relieve intestinal inflammation;
- vitamin complexes to improve blood circulation;
- natural laxatives;
- suppositories and ointments that eliminate pain, relieve inflammation.
In case of neglect of the disease and impossibility of treatment during pregnancy, an experienced proctologist knows how to cure hemorrhoids after childbirth, using surgery. During gestation, surgical methods are used in extreme cases and with the obligatory use of anesthesia. This is the hemming and removal of knots or their pulling with the help of special latex rings. If you need to achieve complete death of the nodes, do sclerotherapy or photocoagulation. nine0005
This is the hemming and removal of knots or their pulling with the help of special latex rings. If you need to achieve complete death of the nodes, do sclerotherapy or photocoagulation. nine0005
A woman who is expecting a child or a young mother after childbirth should not be afraid to go to the clinic. The doctor will select such methods of treatment that will be successful in eliminating a serious disease, without harming either the mother or the baby.
Hemorrhoids during pregnancy - symptoms, diagnosis, treatment methods
Contents
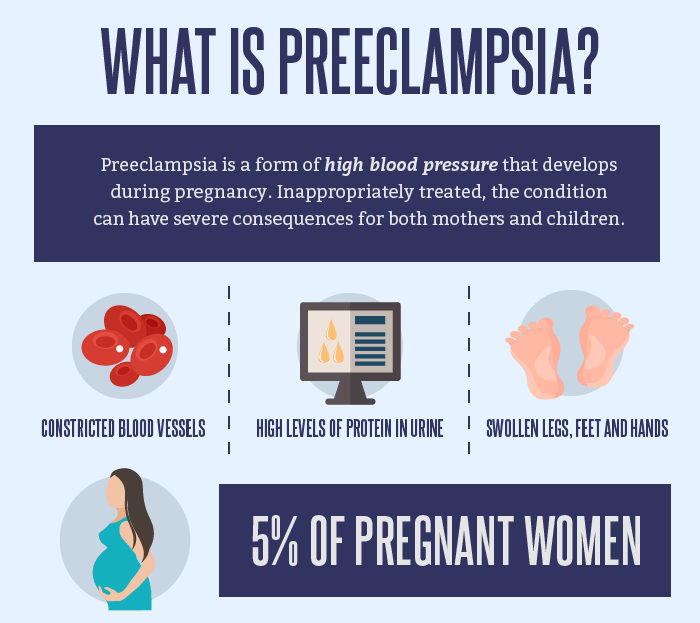
1. Introduction 2. Diagnostics 2.1. Diagnosis of anal fissure 2.2. Digital rectal examination 2.3. Instrumental diagnostics 2.4. Laboratory diagnostics 3. Features of the treatment of hemorrhoids in pregnant women 3.1. Lifestyle change 3.2. Medical therapy 3.3. Surgical intervention 4. Complications 5. Prevention 5.1. Nutrition and drinking regimen 5.2. Personal hygiene 5.3. Physical activity nine0005 According to statistics, hemorrhoids during pregnancy occur in 40% of cases. Most often in the II - III trimesters.
Most often in the II - III trimesters.
In the initial stages, the disease does not pose a danger to either the patient or the fetus. But it negatively affects the psycho-emotional state of the pregnant woman and causes a lot of discomfort.
The problem is complicated by limitations in the patient's treatment methods - not all drugs and procedures can be used during gestation and lactation without a threat to the child. nine0005
If hemorrhoids occur during pregnancy and do not progress, then after childbirth, the nodes, most often, retract on their own.
Causes
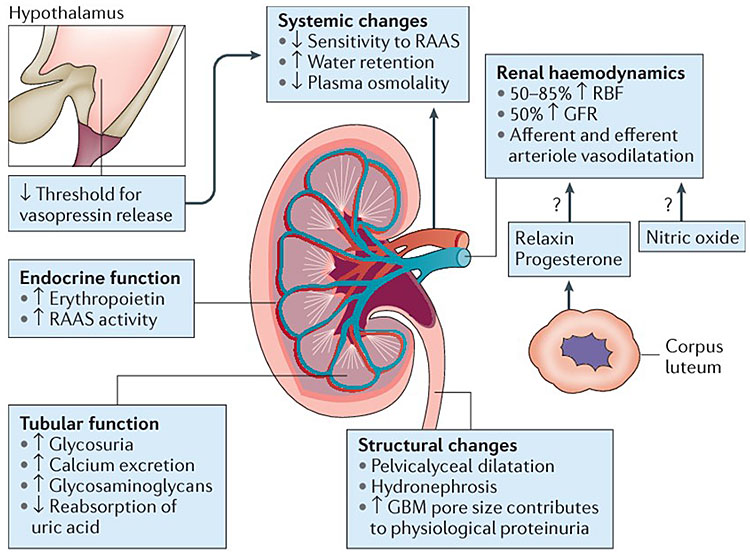
The main reason for the development of hemorrhoids during gestation is physiological changes in the functioning of the whole organism.
During this period, both chronic pathologies can become aggravated, and new ones can appear. The development of nodes during pregnancy is facilitated by: nine0005
- Lifestyle. Some women begin to neglect physical exercises or, due to poor health, severely limit themselves in them.
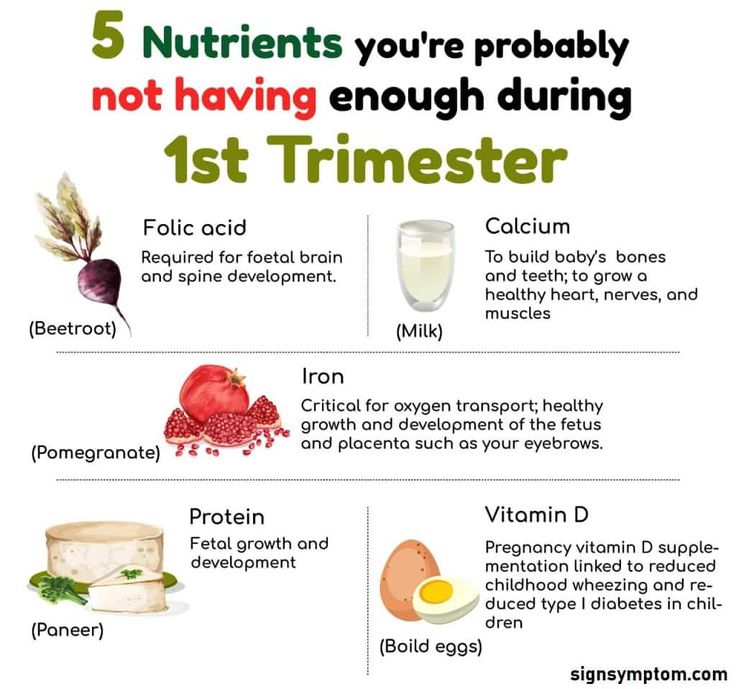
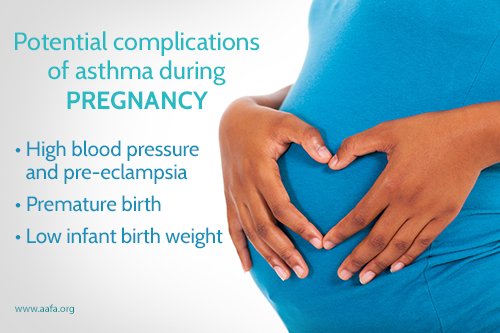 Against the background of physical inactivity and actively produced progesterone, intestinal motility worsens. With improper nutrition and fluid deficiency, an increase in progesterone synthesis leads to constipation. An enlarged uterus puts extra pressure on the rectum. When straining during bowel movements, intra-abdominal pressure rises even more, which causes overflow of blood into the cavernous sinuses of the rectum. nine0015
Against the background of physical inactivity and actively produced progesterone, intestinal motility worsens. With improper nutrition and fluid deficiency, an increase in progesterone synthesis leads to constipation. An enlarged uterus puts extra pressure on the rectum. When straining during bowel movements, intra-abdominal pressure rises even more, which causes overflow of blood into the cavernous sinuses of the rectum. nine0015 - Stagnation. An enlarged uterus leads to compression of the inferior vena cava. Blood circulation in the pelvic organs and the digestive system worsens. This provokes a poor outflow of blood from the lower extremities and the formation of congestion. Due to the increased pressure on the walls of the vessels, they do not withstand and are deformed.
- Childbirth. When pushing, the body is put under enormous stress. Especially strongly the pressure rises in the intra-abdominal space. When the child's head descends into the small pelvis, the rectal vein is compressed.
 During this period, hemorrhoids may be displaced and ruptured, which leads to additional hemorrhage. nine0015
During this period, hemorrhoids may be displaced and ruptured, which leads to additional hemorrhage. nine0015 - The effect of progesterone on the body. Under the influence of the hormone, loosening of the connective tissue and a decrease in the tone of smooth muscle fibers occur. As a result, blood is deposited in the hemorrhoidal plexuses and typical cavernous bodies are formed.
- Improper nutrition and non-compliance with the drinking regimen. Deficiencies of fiber and fluid lead to compaction of feces, which increases the need for straining during the act of defecation. Overeating and plentiful rare meals are also considered harmful. In such a situation, the feces are unevenly distributed throughout the intestines, which leads to their tamping and complications during the act of defecation. nine0015
Additional factors in the development of hemorrhoids are: chronic constipation or diarrhea, heredity, changes in blood volume, coagulation process, intensive synthesis of mediators, long stay in the toilet, excessive straining, weight gain.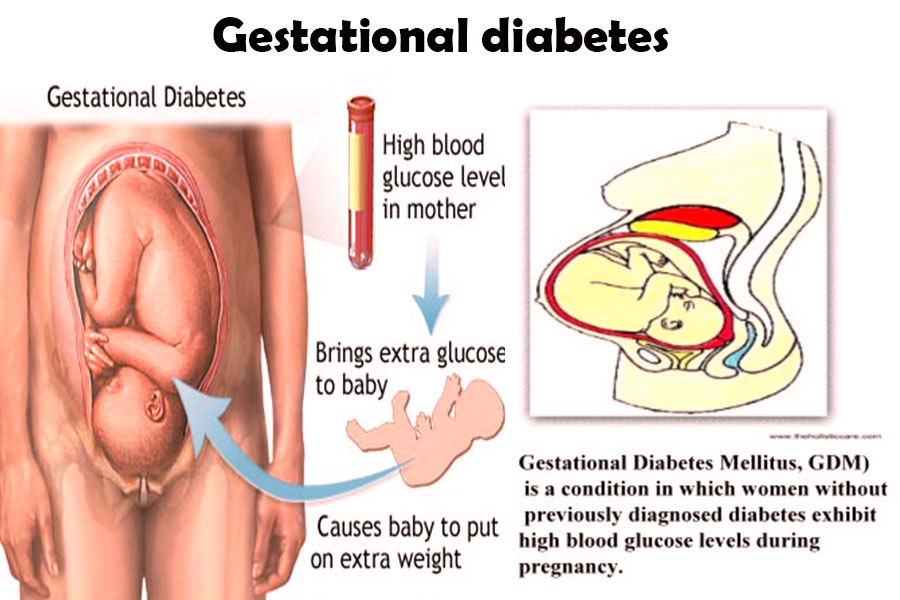
Diagnostics
At the slightest suspicion of a pathology, it is urgent to contact a proctologist. The most competent treatment is to prevent the development of the disease. nine0005
Diagnosis consists of several stages: a survey, examination, instrumental and laboratory examination.
Poll
The proctologist asks a number of questions in order to clarify the lifestyle, nutrition, genetic predisposition to the patient's varicose veins. The doctor is also interested in the frequency and nature of the symptoms that provoke them.
An important role is played by concomitant diseases, occupation, allergies, etc. nine0005
After collecting an anamnesis, the doctor makes a preliminary diagnosis. It is possible to confirm or refute it according to the results of further examinations.
Digital rectal examination
With hemorrhoids in a mild form, the examination is painless. The proctologist studies the structure of the anus (closeness, symmetry of the valves, deformities), the condition of the mucous membranes and the adjacent dermis, the presence of inflammation and discharge, etc. If the procedure is painful for the patient, then the question of transferring it is raised. nine0005
The proctologist studies the structure of the anus (closeness, symmetry of the valves, deformities), the condition of the mucous membranes and the adjacent dermis, the presence of inflammation and discharge, etc. If the procedure is painful for the patient, then the question of transferring it is raised. nine0005
Examination is necessary to make a differential diagnosis. Symptoms similar to hemorrhoids appear with anal fissures, condyloma, oncology, benign neoplasms, rectal prolapse.
In addition to visiting the proctologist, the patient is examined by a gynecologist. The doctor evaluates the condition of the vagina, rectovaginal septum and tissues adjacent to the anus.
Instrumented Diagnostics
If your doctor suspects other bowel disease, an anoscopy may be done. This is a technique in which a tube with a flashlight is inserted into the rectum. If necessary, during the procedure, tissues of the intestinal mucosa are taken for a biopsy.
Anoscopy during pregnancy is possible, since it does not require anesthesia. It does not cause pain to the patient, only a slight discomfort during the introduction of the instrument and the sampling of the biomaterial. nine0005
Before carrying out instrumental diagnostics by the method under consideration, cleaning of the lower intestine with microclysters is required.
If oncology or intestinal bleeding is suspected, a colonoscopy is performed. In other cases, during the period of preeclampsia, colonoscopy is strictly not recommended, as it can cause the onset of premature birth.
Laboratory diagnostics
nine0002 Due to the fact that during pregnancy a woman systematically donates biomaterials for research, when examining hemorrhoids, they can not be taken additionally. However, this rule applies to cases where the clinical picture is clear and there are no reasons for additional laboratory diagnostics.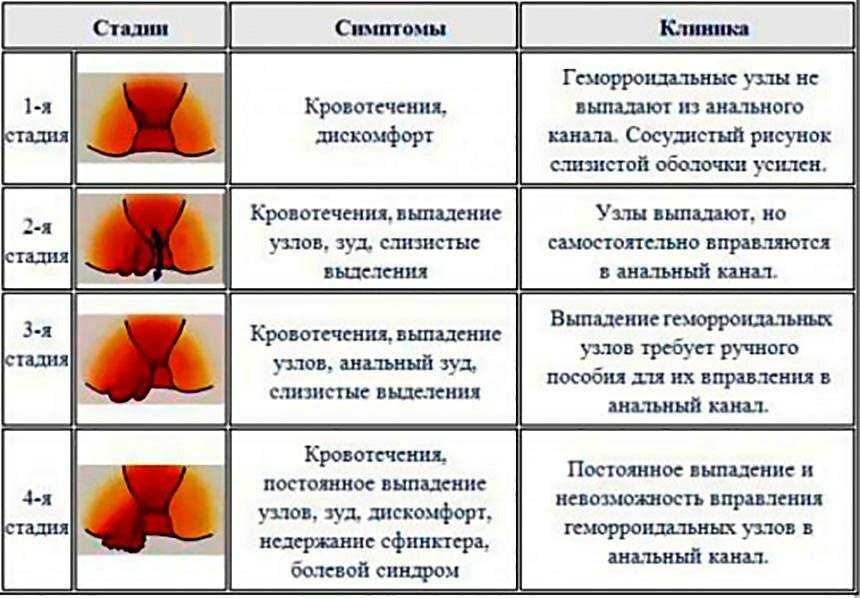
If there is anal bleeding, especially in the postpartum period, then the patient must donate blood for hemoglobin and feces to determine the latent blood in it. nine0005
Features of the treatment of hemorrhoids in pregnant women
Treatment of hemorrhoids in pregnant women consists of several stages. First of all, the patient is prescribed a lifestyle change and drug therapy. If necessary, it is possible to carry out minimally invasive techniques to remove the hemorrhoid.
Lifestyle change
After collecting information about the patient and her habits, the doctor may recommend: nine0005
1. Stick to a diet:
- avoid spicy and salty foods;
- eat foods rich in fiber;
- if there are no diseases of the cardiovascular system and kidneys, then drink at least 1.5 liters of water per day.
2. Carry out the act of defecation correctly:
- do not push;
- sit no longer than 5 minutes, even if it was not possible to defecate; nine0015
- use microclysters.
3. Moderate physical activity. It can be a complex of exercise therapy, light physical exercises without weights, long walks at a calm pace.
If it is necessary to use laxatives, castor oil is recommended to be replaced with medicines allowed during gestation. Preparations containing magnesium can lead to premature stimulation of the uterus. It is better to give preference to vaseline oil, preparations with lactulose or foods rich in dietary fiber (plums, prunes, for example). The introduction of drugs in any trimester is permissible only after agreement with the supervising physician. nine0005
Compliance with simple rules allows you to eliminate the disease completely or significantly reduce its manifestations in 70% of cases.
Medical therapy
Due to the limited list of permitted medications, the scheme and course of taking medications should be developed by a doctor.
As a general rule, patients in position are prohibited from taking analgesics. However, there are a number of drugs, which include local anesthetics. They are not absorbed into the bloodstream, so they are absolutely safe for the fetus. These can be: suppositories, ointments and gels with benzocaine and lidocaine. nine0005
However, there are a number of drugs, which include local anesthetics. They are not absorbed into the bloodstream, so they are absolutely safe for the fetus. These can be: suppositories, ointments and gels with benzocaine and lidocaine. nine0005
To eliminate the processes of thrombus formation in the hemorrhoid, let's take drugs with diosmin. They relieve swelling and inflammation in the “bump” and tissues adjacent to the anus. But during lactation, this group of drugs is prohibited, since proper clinical studies in the field of the effect of diosmin on the development of a child during breastfeeding have not been conducted. During lactation, local hormonal rectal suppositories and ointments are prescribed to relieve swelling, inflammation and itching.
When self-medicating, remember that even the safest medicines for an adult can be extremely dangerous for the fetus and newborn. Therefore, the appointment of drugs should be handled by a doctor.
Surgery
Milligan-Morgan operations or Ferguson hemorrhoidectomy during pregnancy are used extremely rarely and in situations that threaten the life and health of the patient. They can be carried out after childbirth, when the hemorrhoids have not returned to normal on their own or there is no effect from drug therapy or minimally invasive techniques. nine0005
They can be carried out after childbirth, when the hemorrhoids have not returned to normal on their own or there is no effect from drug therapy or minimally invasive techniques. nine0005
Pregnant women may be offered a thrombectomy. This is a minimally invasive procedure that uses a local anesthetic. It takes only 10 minutes and does not require a long rehabilitation. The operation is painless.
For recurrent bleeding, the method of ligation with latex rings is used. The essence of the method is to pinch the leg of the hemorrhoid and stop the flow of blood into it. Over time, the knot dries out and falls off on its own. It is used only for internal hemorrhoids using local anesthesia. nine0005
Complications
Not running hemorrhoids does not affect the course of gestation. It only causes discomfort to the pregnant woman and worsens the quality of life of the patient.
In advanced situations, it can cause the development of anemia, anal bleeding with attempts, paraproctitis, thrombophlebitis of the rectal veins, pinching. Complications lead to the launch of necrotic processes and infection of the patient's tissues, as well as intrauterine infection of the fetus. nine0005
Complications lead to the launch of necrotic processes and infection of the patient's tissues, as well as intrauterine infection of the fetus. nine0005
There is an opinion that hemorrhoids lead to oncology. However, it is not. It can affect the quality of sleep, cause an increase in blood pressure and cause anxiety, thereby worsening the physical and psycho-emotional state of the patient.
Prophylaxis
Timely diagnosis and therapy can slow down the development of pathology in the early stages or eliminate it completely. With surgery, the problem can be completely eliminated. However, minimally invasive techniques used during pregnancy do not exclude relapses. nine0005
To avoid the re-development of hemorrhoids or prevent its occurrence during gestation, experts recommend following simple rules.
Food and drink regimen
Patients are advised:
- eat often and in small portions;
- , depending on the trimester and the state of the body, consume the amount of calories recommended by the doctor;
- consume enough water, fiber and dietary fiber; nine0015
- Eliminate alcohol completely.
Depending on the type of constipation, a diet may be suggested.
So, with spastic constipation caused by irritation of the intestinal receptors, onions, legumes, mustard, unripe berries and fruits, black bread should be excluded from the diet. Add broccoli, honey (if there is no allergy), raisins, ripe apples, corn, potatoes, carrots, cauliflower, dried apricots, cereals (oatmeal and pearl barley), sour-milk products, vegetable fats to the diet. Vegetables and fruits need to be boiled, steamed or baked, they can be mashed. nine0005
With atonic constipation, on the contrary, it is necessary to increase intestinal motility. The patient is recommended to diversify the menu with beets, prunes, berry and fruit decoctions, fresh salads, fresh fruits, juices and compotes.
An indicator of the correctness of the action is the normalization of the stool and a comfortable bowel movement.
Personal care
In addition to morning and evening hygiene, patients are advised to carry out additional procedures after each act of defecation. To do this, you can use wet wipes without alcohol, as well as a cool hygienic shower. nine0005
To do this, you can use wet wipes without alcohol, as well as a cool hygienic shower. nine0005
If hemorrhoids still appear, you should abandon toilet paper, even the softest, and give preference to a hygienic shower with soap. For a hygienic shower, you can use herbal infusions and decoctions, a weak solution of potassium permanganate or other available antiseptic.
Physical activity
During pregnancy, moderate gentle physical activity is extremely important to normalize blood circulation in the lower extremities and pelvic organs. nine0005
Pregnant women benefit from gymnastics (for example, according to Kegel), an individual set of exercises, exercise therapy, yoga (for pregnant women). A set of exercises designed for 10 - 15 minutes a day is enough.
Recently, hygienic gymnastics has been gaining popularity. The essence of the exercise is to lie on your back with a raised pelvis. For convenience, a pillow can be placed under the pelvis. For the day you need to do 3 sets of 15 minutes.
For the day you need to do 3 sets of 15 minutes.
Pregnant women are also advised to avoid prolonged static standing and sitting. It is strongly not recommended to supercool and walk for a long time in wet weather. nine0005
Running hemorrhoids during pregnancy is a danger not only to the mother, but also to the fetus. Complications can force doctors to resort to radical measures to stop bleeding, which is fraught with premature birth with all the ensuing consequences for the child.
Like any disease, hemorrhoids are easier to prevent by using prevention recommendations and consulting a doctor in a timely manner. Call +7 (4842) 20-70-20!
FAQ
Of course NO! Hemorrhoids are not a tumor, as many people think, it is associated with deformation of the vessels of the lower rectum.
The danger of late treatment for hemorrhoids lies in the risk of bleeding. But discomfort and bruising also occur with rectal cancer.
As soon as there is discomfort in the anus, you should immediately contact a proctologist for an examination.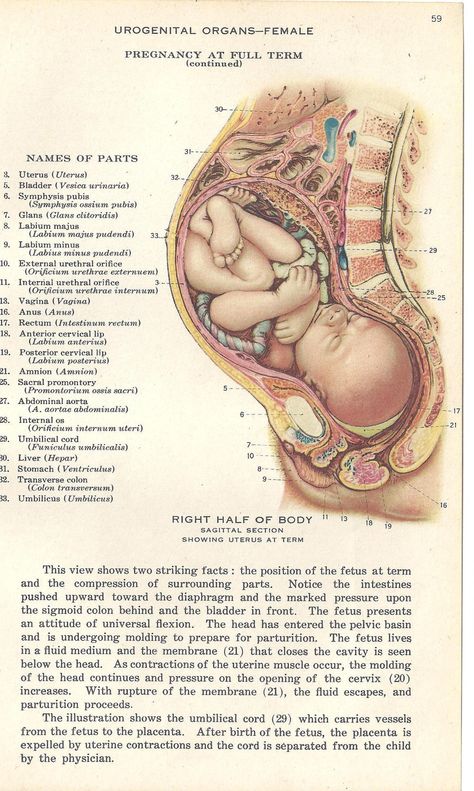
You can't say yes or no. In the large intestine, the processes of fecal formation take place. Further movement of feces is facilitated by wave-like contractions of the walls of the rectum, which depend on our nutrition and activity. These contractions are called peristalsis. The walls of the large intestine simultaneously absorb minerals and water. If there is no proper level of peristalsis, even with the consumption of large amounts of water, pathology can develop! nine0005
Hemorrhoids are considered a chronic disease. By identifying symptoms in the early stages and the correct behavior of the patient, it is possible to avoid exacerbation for a long period of time. But the disease tends to aggravate and progress if left untreated.
Most often, complications of hemorrhoids are manifested in the form of hemorrhoidal bleeding and thrombosis of the node. All this is accompanied by intense pain and causing significant discomfort. Frequent heavy bleeding leads to anemia, which may necessitate a blood transfusion procedure.