Group b streptococcus screening in pregnancy
Group B Strep and Pregnancy (for Parents)
What Is Group B Strep?
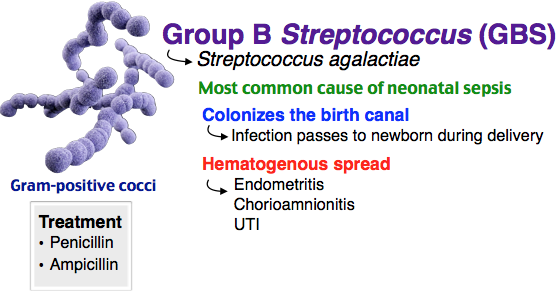
Group B Streptococcus (group B strep, GBS) is a type of
bacteriaoften found in the urinary tract, digestive system, and reproductive tracts. The bacteria come and go from our bodies, so most people who have it don't know that they do. GBS usually doesn't cause health problems.
What Problems Can Group B Strep Cause?
Health problems from GBS are not common. But it can cause illness in some people, such as the elderly and those with some medical conditions. GBS can cause infections in such areas of the body as the blood, lungs, skin, or bones.
About 1 out of every 4 women have GBS. In pregnant women, GBS can cause infection of the urinary tract, placenta, womb, and amniotic fluid.
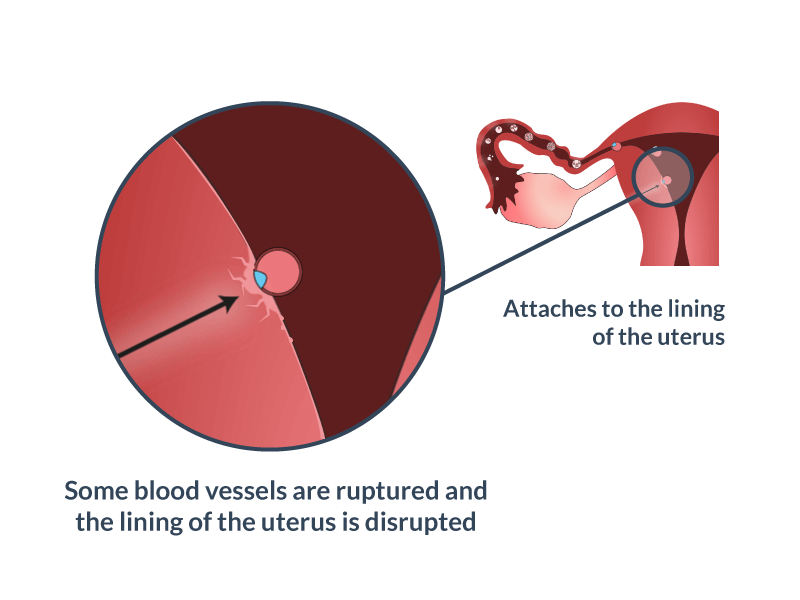
Even if they haven't had any symptoms of infection, pregnant women can pass the infection to their babies during labor and delivery.
How Does Group B Strep Affect Babies?
When women with GBS are treated with antibiotics during labor, most of their babies do not have any problems. But some babies can become very sick from GBS. Premature babies are more likely to be infected with GBS than full-term babies because their bodies and immune systems are less developed.
The two types of GBS disease in babies are:
- Early-onset infections, which happen during the first week of life. Babies often have symptoms within 24 hours of birth.
- Late-onset infections, which develop weeks to months after birth. This type of GBS disease is not well understood.
What Are the Signs & Symptoms of GBS Disease?
Newborns and infants with GBS disease might show these signs:
- a fever
- feeding problems
- breathing problems
- irritability or fussiness
- inactivity or limpness
- trouble keeping a healthy body temperature
Babies with GBS disease can develop serious problems, such as:
- pneumonia
- sepsis
- meningitis (infection of the fluid and lining around the brain).
 Meningitis is more common with late-onset GBS disease and, in some cases, can lead to hearing loss, vision loss, learning disabilities, seizures, and even death.
Meningitis is more common with late-onset GBS disease and, in some cases, can lead to hearing loss, vision loss, learning disabilities, seizures, and even death.
How Is Group B Strep Diagnosed?
Pregnant women are routinely tested for GBS late in the pregnancy, usually between weeks 35 and 37. The test is simple, inexpensive, and painless. Called a culture, it involves using a large cotton swab to collect samples from the vagina and rectum. These samples are tested in a lab to check for GBS. The results are usually available in 1 to 3 days.
If a test finds GBS, the woman is said to be "GBS-positive." This means only that she has the bacteria in her body — not that she or her baby will become sick from it.
GBS infection in babies is diagnosed by testing a sample of blood or spinal fluid. But not all babies born to GBS-positive mothers need testing. Most healthy babies are simply watched to see if they have signs of infection.
How Is Group B Strep Treated?
Doctors will test a pregnant woman to see if she has GBS.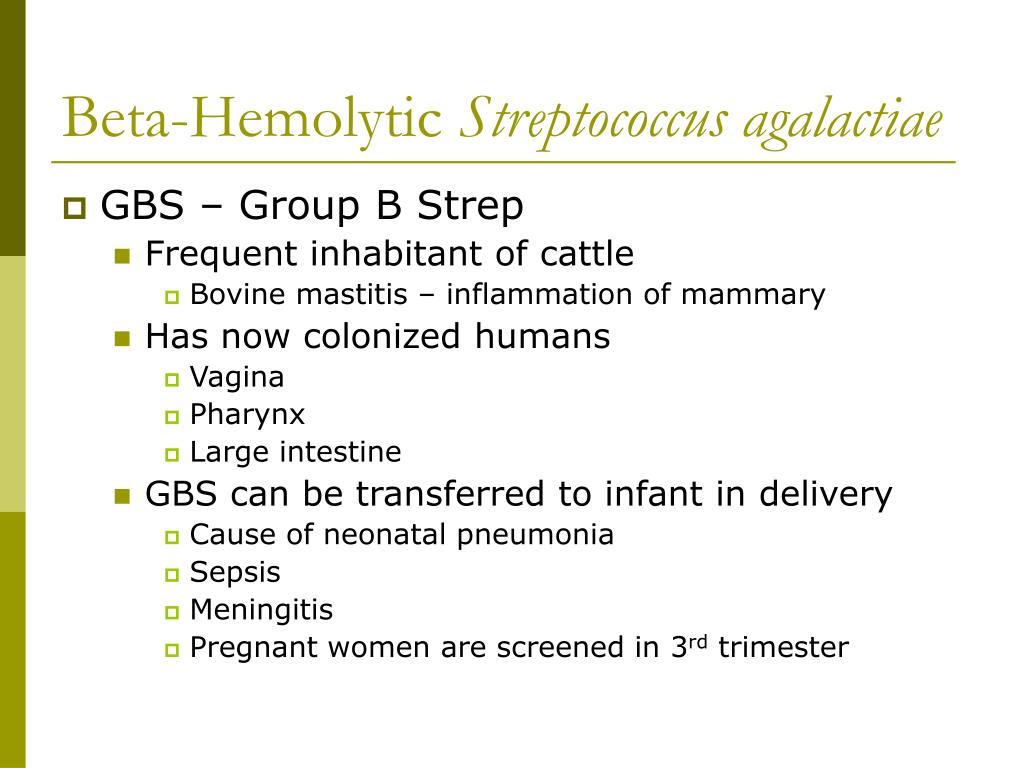 If she does, she will get intravenous (IV) antibiotics during labor to kill the bacteria. Doctors usually use penicillin, but can give other medicines if a woman is allergic to it.
If she does, she will get intravenous (IV) antibiotics during labor to kill the bacteria. Doctors usually use penicillin, but can give other medicines if a woman is allergic to it.
It's best for a woman to get antibiotics for at least 4 hours before delivery. This simple step greatly helps to prevent the spread of GBS to the baby.
Doctors also might give antibiotics during labor to a pregnant woman if she:
- goes into labor prematurely, before being tested for GBS
- hasn't been tested for GBS and her water breaks 18 or more hours before delivery
- hasn't been tested for GBS and has a fever during labor
- had a GBS bladder infection during the pregnancy
- had a baby before with GBS disease
Giving antibiotics during labor helps to prevent early-onset GBS disease only. The cause of late-onset disease isn't known, so no method has yet been found to prevent it. Researchers are working to develop a vaccine to prevent GBS infection.
Babies who get GBS disease are treated with antibiotics. These are started as soon as possible to help prevent problems. These babies also may need other treatments, like breathing help and IV fluids.
How Can I Help Prevent Group B Strep Infection?
Because GBS comes and goes from the body, a woman should be tested for it during each pregnancy. Women who are GBS-positive and get antibiotics at the right time during labor do well, and most don't pass the infection to their babies.
If you are GBS-positive and begin to go into labor, go to the hospital rather than laboring at home. By getting IV antibiotics for at least 4 hours before delivery, you can help protect your baby against early-onset GBS disease.
Reviewed by: Thinh Phu Nguyen, MD
Date reviewed: July 2022
Group B strep test | Pregnancy Birth and Baby
Group B strep test | Pregnancy Birth and Baby beginning of content8-minute read
Listen
If your baby suddenly develops very high fever with vomiting, call triple zero (000) and ask for an ambulance or go to the nearest hospital emergency department.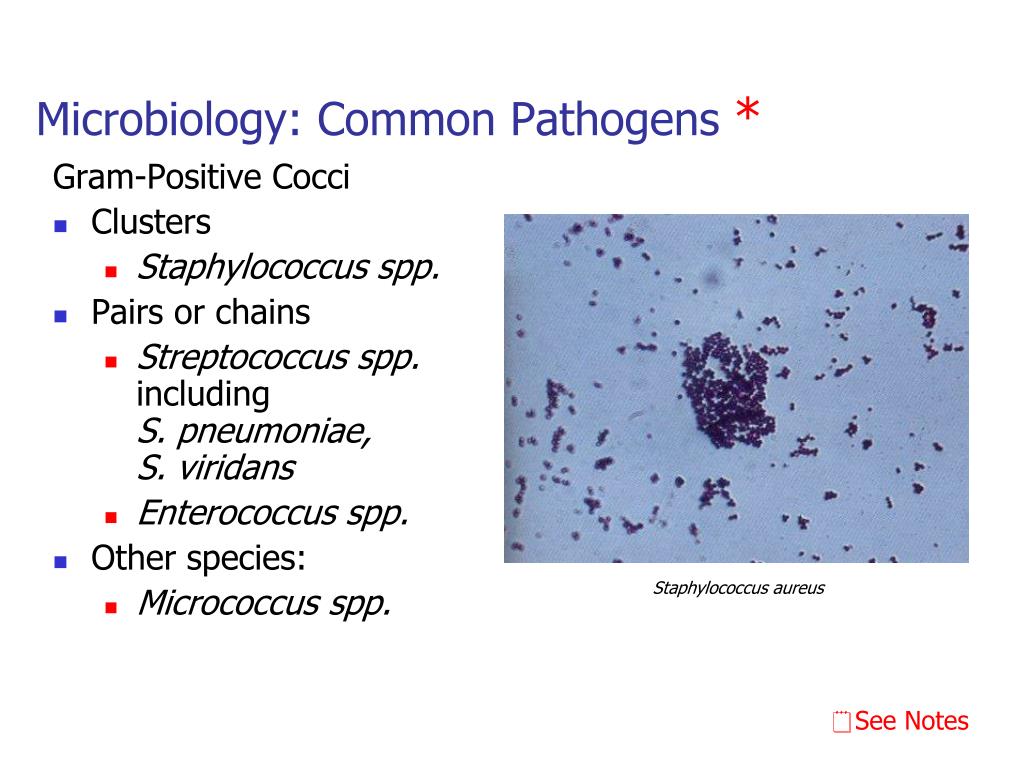
Key facts
- Group B streptococcus (GBS) is part of the normal bacteria that lives in our body. It is most commonly found in the intestines, rectum, urethra or vagina.
- It usually causes no health concerns or symptoms.
- If you are pregnant and have GBS, bacteria can pass to your baby before or during a vaginal birth. In a small number of cases, this may make your baby sick.
- You may be offered a test to check if you have GBS, which involves taking a swab of your vagina at around 35 to 37 weeks of pregnancy.
- If you are a GBS carrier or if you develop risk factors for GBS infection, intravenous antibiotics during labour can reduce the risk of GBS colonisation and an early GBS infection in your baby.
- Testing and treatment for GBS is your choice and should be done in consultation with your care provider.
What is GBS?
Group B streptococcus (GBS) is one of many bacteria that normally live in our bodies. GBS is commonly found in the intestines, rectum, urethra, or vagina.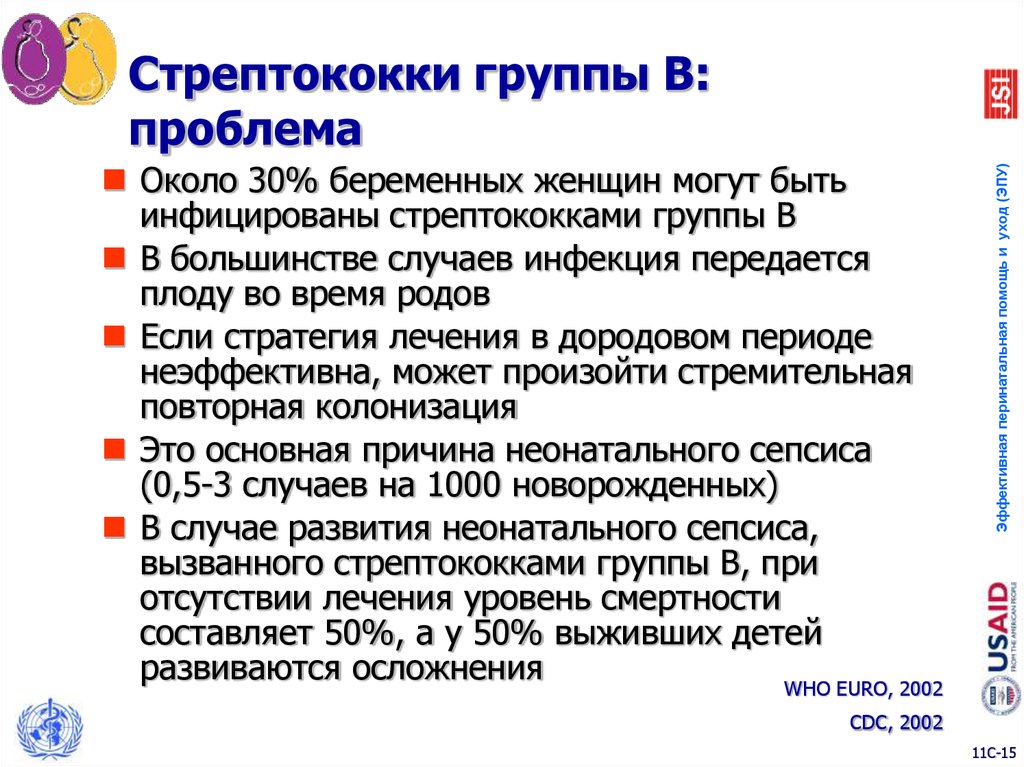 Many people have it, and it usually causes no health concerns or symptoms. This bacterium is transient, meaning that it comes and goes from your body. GBS is not sexually transmitted. Being a carrier of GBS in pregnancy is not usually harmful to you but it can cause infection in some babies.
Many people have it, and it usually causes no health concerns or symptoms. This bacterium is transient, meaning that it comes and goes from your body. GBS is not sexually transmitted. Being a carrier of GBS in pregnancy is not usually harmful to you but it can cause infection in some babies.
Carrying GBS, also known as GBS colonisation is not the same as having a GBS infection.
What could GBS mean for my baby?
Many babies come into contact with GBS during labour or around the time of birth. Most of these babies won’t become unwell. However, if you carry GBS, there is a small chance (about 1 in 1000) that your baby will develop GBS infection in the first week after birth. This is known as ‘early onset GBS infection’.
GBS can cause infections such as pneumonia, blood poisoning (septicaemia), or meningitis (an infection around the brain) in babies. However, with early detection and treatment using intravenous antibiotics, most babies fully recover. A very small number of babies who become infected may have long-term disability and some don’t survive.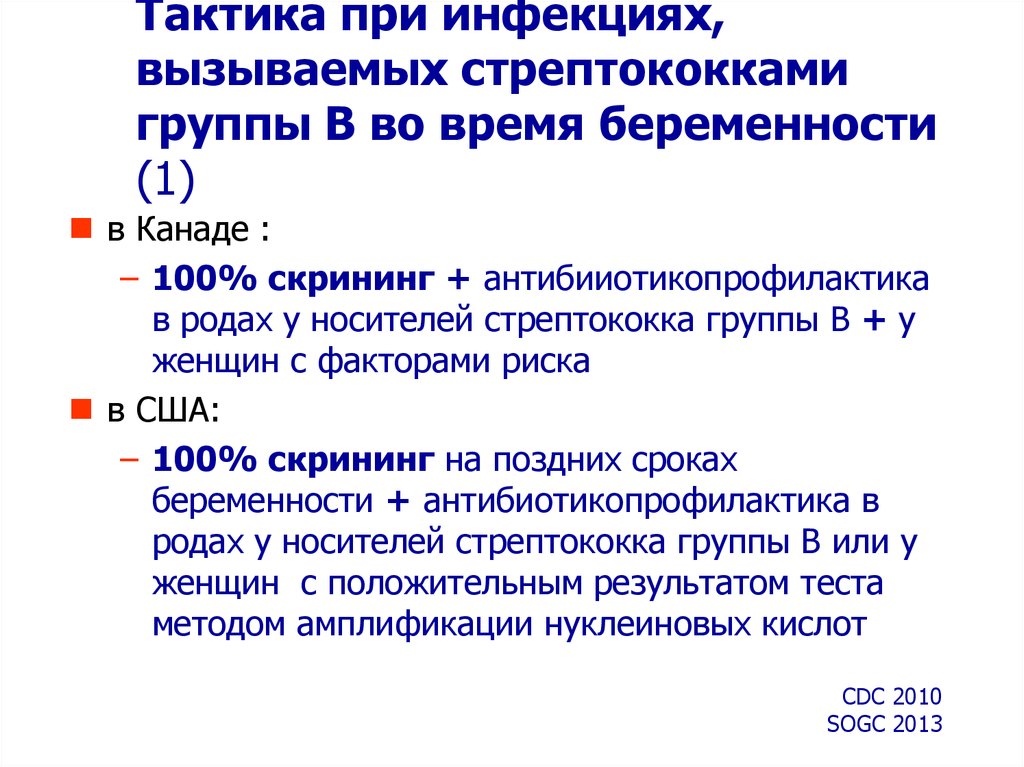
Can GBS infection be prevented?
Unfortunately, there is no way to completely prevent GBS infection in babies. However, early detection and treatment with antibiotics can reduce the chance of your baby becoming very unwell.
How is GBS found?
GBS may be found during a routine antenatal test. It can be found in urine or more commonly, when you have a vaginal or rectal swab testing specifically for this bacterium.
There is no standard practice for testing for GBS in Australia, but universal screening for the GBS bacteria is most common. This means that all women will be offered to test for GBS bacteria during pregnancy. Some healthcare providers may only test for GBS if you have risk factors that make GBS infection more likely.
The test can only find GBS if the bacteria is there at the time of testing. Because GBS bacteria comes and goes from your body, routine screening for this bacteria may not detect GBS in everyone who has it during pregnancy.
Testing for GBS involves taking a swab of the inside of the vagina and/or rectum.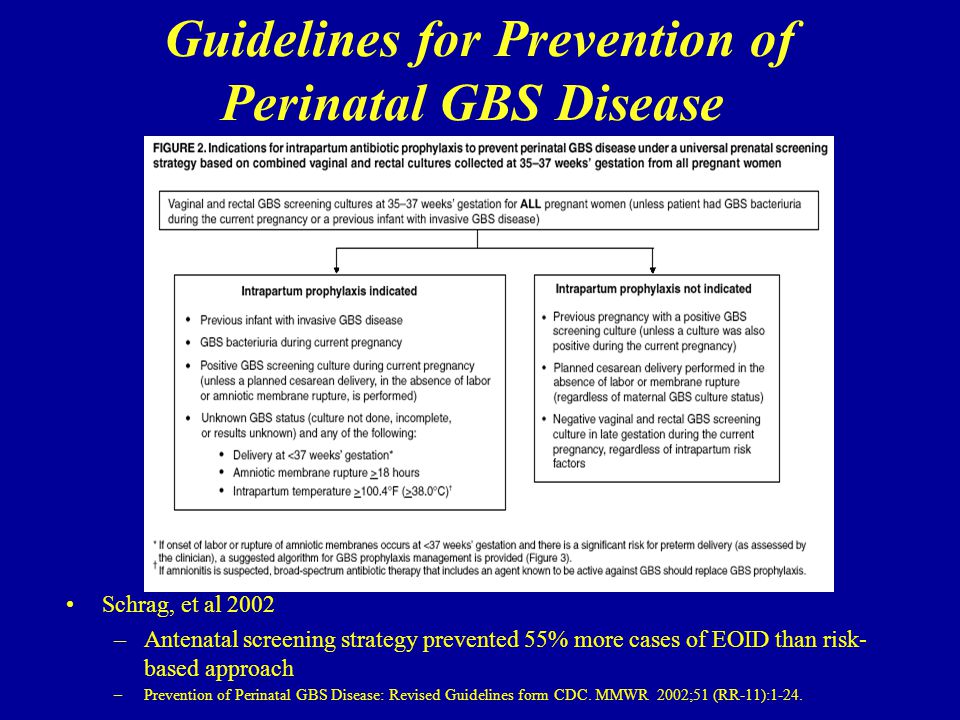 You can usually do this test yourself, but if you prefer your doctor or midwife can do this for you. The swab is usually taken between 35 to 37 weeks of pregnancy.
You can usually do this test yourself, but if you prefer your doctor or midwife can do this for you. The swab is usually taken between 35 to 37 weeks of pregnancy.
Speak to your doctor or midwife to understand how GBS is tested and managed at your care provider. They can help you to decide if this test is right for you.
Questions you may want to ask your doctor
- What are the risks and benefits to me and my baby if I test for GBS?
- If I have GBS, what does this mean for my pregnancy and birth?
- What is the rate of GBS infection in newborn babies?
- Can my baby become unwell if my test is negative?
What are the risk factors for early onset GBS infection?
Babies are more likely to become infected with GBS if:
- they are born prematurely
- your waters break before 37 weeks of pregnancy
- you give birth more than 18 hours after your waters break
- you have a fever (over 38°C) while in labour
- you've had a previous child with severe GBS infection
- a urine test during pregnancy detected GBS
- a swab taken no more than 5 weeks earlier detected GBS
How is GBS treated?
If your GBS test is positive, or if you have risk factors as listed above, your doctor or midwife will probably recommend that you have intravenous antibiotics when your waters break or when labour starts. If your waters break before your labour starts your healthcare team may recommend inducing labour.
If your waters break before your labour starts your healthcare team may recommend inducing labour.
The antibiotic given is usually penicillin, but other options are available if you are allergic to penicillin. The antibiotics pass through the placenta and into your baby’s blood. This reduces your baby's chances of GBS colonisation and infection.
There is usually no need for screening or treatment with antibiotics for GBS before a planned caesarean, because the baby will not pass through your vagina.
What happens after the birth?
All babies are monitored for the first couple of days for signs of infection. Your baby’s health team will monitor their heart rate, breathing and temperature to check they are well. The chance of your baby being infected with GBS is very low.
Signs that your baby is not well may include:
- abnormal breathing sounds, such as ‘grunting’ with each breath out
- difficulty breathing or breathing too fast or slow
- sleepiness and not interested in feeding
- vomiting
- having trouble keeping their temperature at the right level (being too hot or too cold)
- looking pale or blotchy
- floppy arms and legs
If you notice any of these signs in hospital or at home, it’s important that you contact your healthcare provider straight away.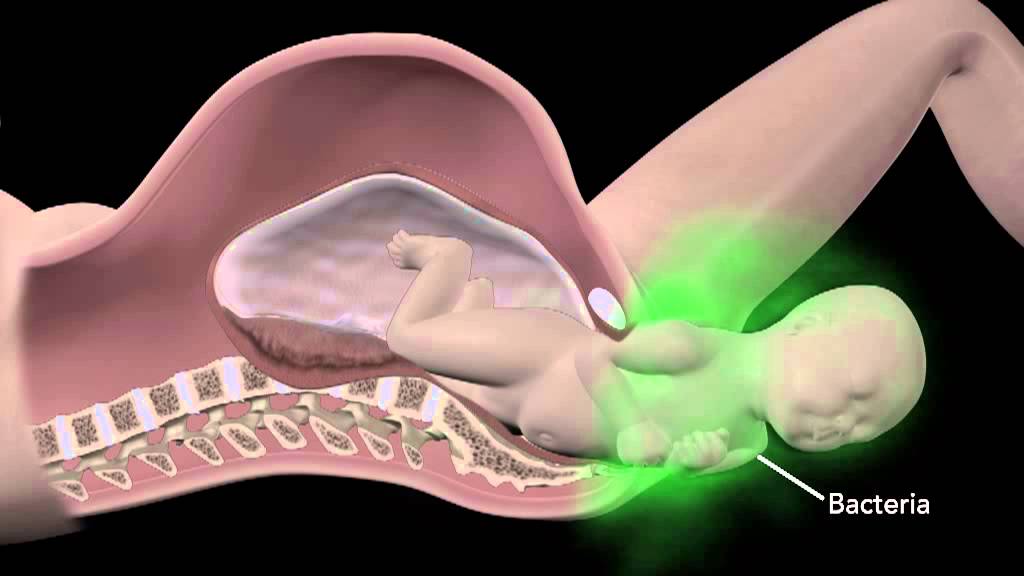
What is late-onset group B strep?
Rarely, babies can develop GBS infection weeks or months after birth. This is called ‘late onset group B strep'. They become seriously unwell quite quickly with fevers, vomiting and difficulty feeding. Unfortunately, the group B strep test and use of antibiotics during labour doesn’t prevent a baby developing late-onset group B strep infection.
If your baby's condition deteriorates quickly, call triple zero (000) and ask for an ambulance or go to the nearest hospital emergency department.
If you want more information about GBS, or if you have any concerns about your baby, call Pregnancy, Birth and Baby on 1800 882 436 to speak to a maternal child health nurse, or talk to your midwife or doctor.
Speak to a maternal child health nurse
Call Pregnancy, Birth and Baby to speak to a maternal child health nurse on 1800 882 436 or video call. Available 7am to midnight (AET), 7 days a week.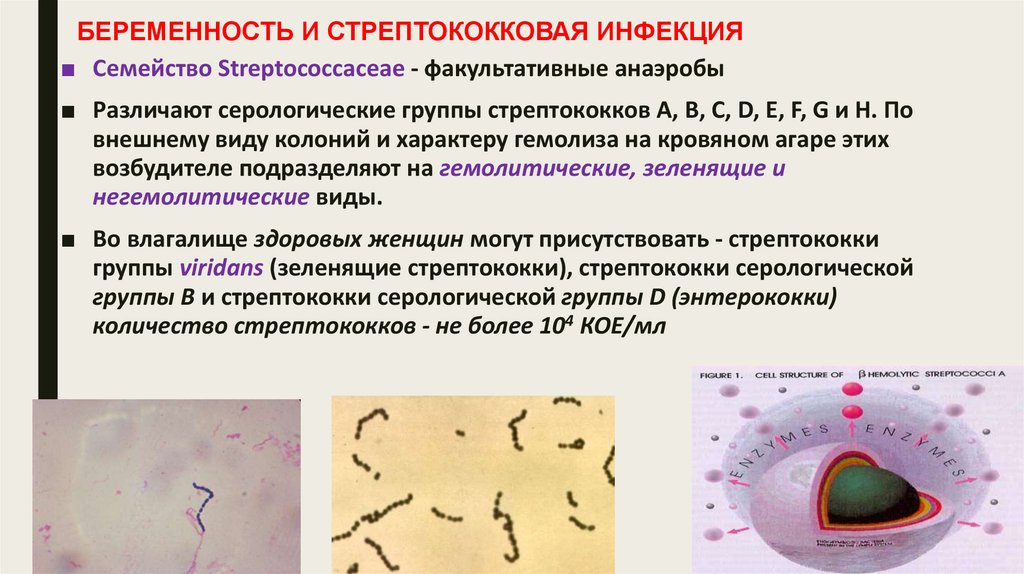
Sources:
Department of Health (Pregnancy Care Guidelines, Group B streptococcus), RANZCOG (Group B Streptococcus), Mater Mothers Hospital (Group B streptococcus and pregnancy), Safer Care Victoria (Group B streptococcus (GBS) – screening and management), Monash Women's (Group B streptococcus (GBS) screening)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: September 2022
Back To Top
Related pages
- Pregnancy checkups, screenings and scans
- Routine antenatal tests
Need more information?
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
Need further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.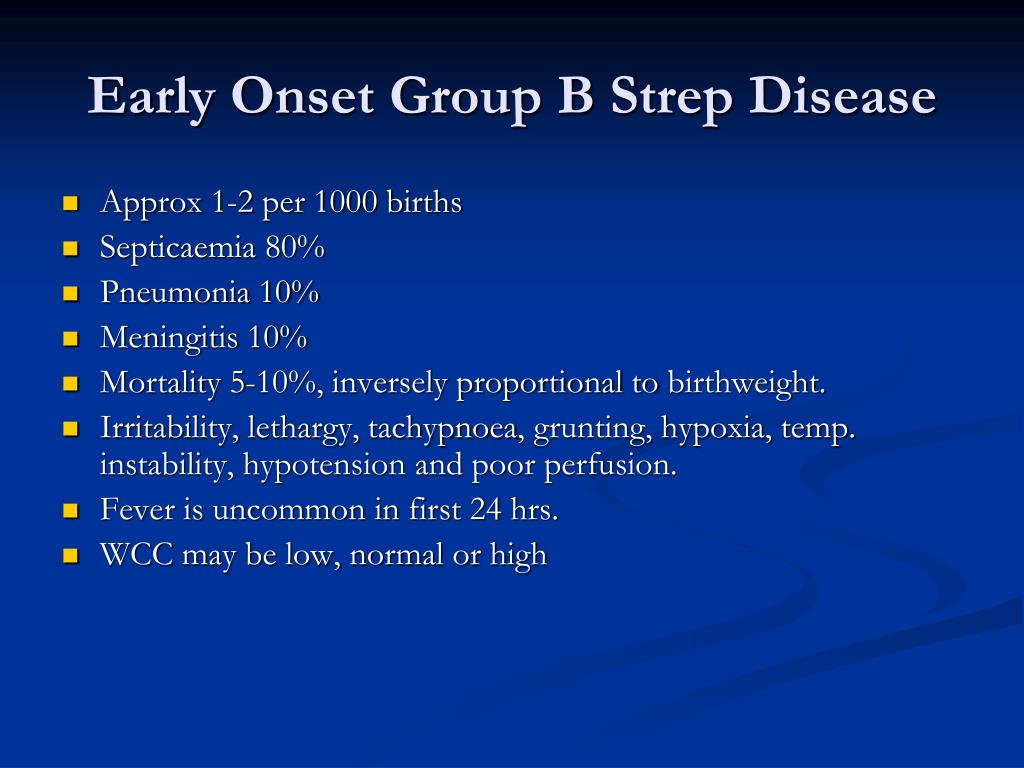
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
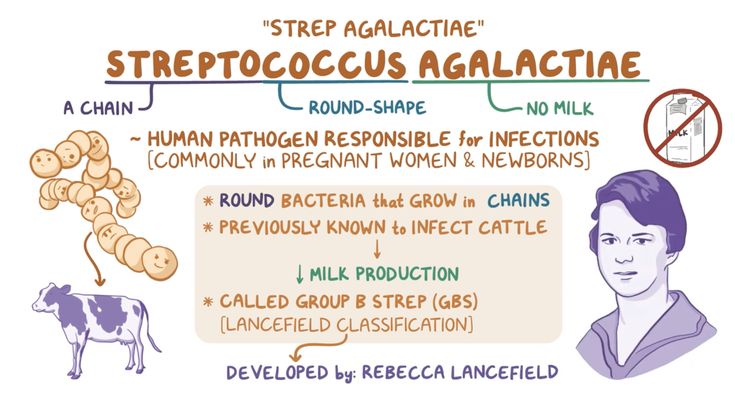
Culture for group B beta-hemolytic streptococcus (Streptococcus group B, S. agalactiae)
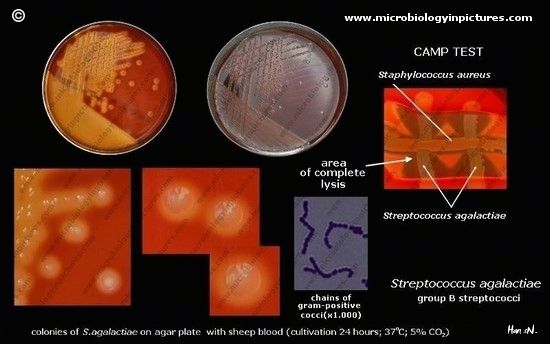
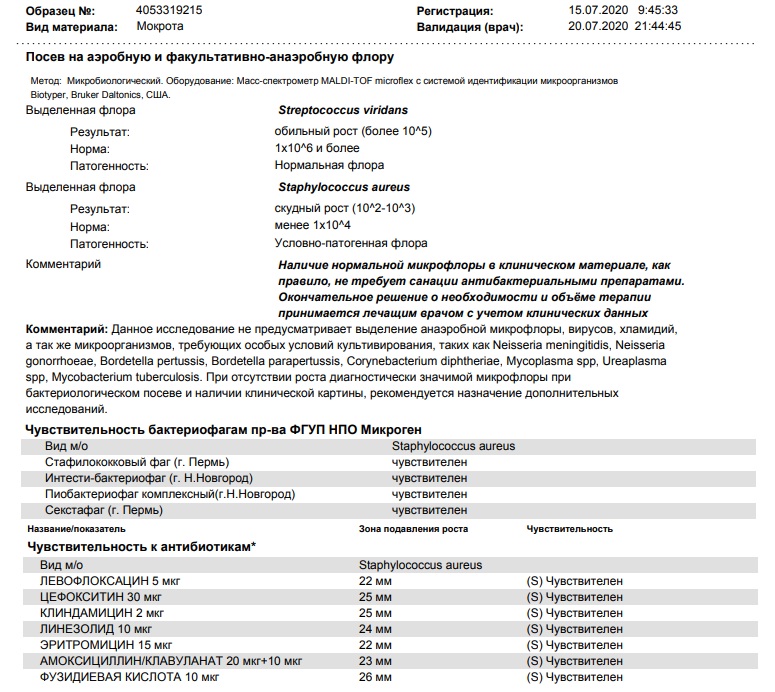
Method of determination The study is carried out by the method of sowing on dense nutrient media. The identification of microorganisms is carried out by mass spectrometry using a Microflex Brucker Daltonik MALDI Biotyper, BRUKER, Germany.
Test material A swab from the entrance to the vagina or anorectal area; vaginal discharge, cervical discharge
Home visit available
Synonyms: Streptococcus group B (S. agalactiae) Culture.
Brief description of the study "Culture for group B beta-hemolytic streptococcus (Streptococcus group B, S.
 agalactiae)"
agalactiae)" Group B streptococcus (GBS, Streptococcus agalactiae) causes severe illness in newborns and is dangerous for certain patients other age groups.
In the vast majority of cases, newborns become infected with GBS during maternal deliveries, with a higher incidence during vaginal delivery. GBS causes early neonatal infections such as sepsis, meningitis, pneumonia, osteomyelitis, arthritis, and pyelonephritis, with rates ranging from 0.2 to 5 or more per 1,000 live births in different countries. In obstetric practice, group B streptococcus is associated with bacteremia, urinary tract infections, chorioamnionitis, premature rupture of amniotic fluid, preterm labor, postpartum endometritis, etc.
GBS in the human body can colonize the oropharynx, anal area of the rectum, vagina (usually vestibule), urogenital tract, skin.
It has been established that GBS in 5-35% of women can be detected in the vagina and often in the urethra of their sexual partners A significant association of carriage of GBS in the vagina has been shown not only with early septicemia of newborns, but also with spontaneous miscarriages, premature birth, premature rupture of amniotic fluid , urinary infection in pregnant women, the birth of children with low body weight, the development of chorioamnionitis in childbirth, endometritis and sepsis in puerperas.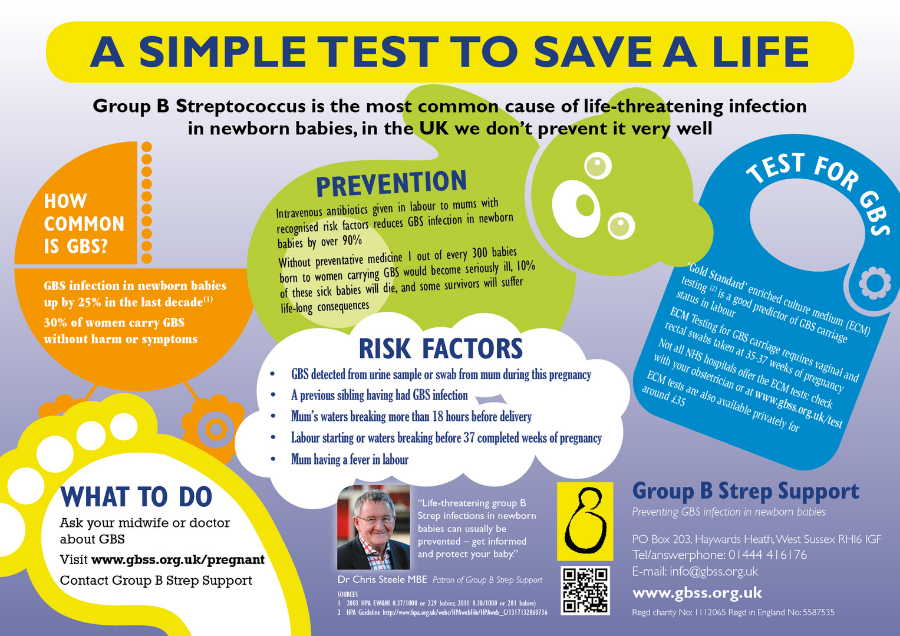 The highest level of colonization in women of reproductive age and pregnant women. In pregnant women, GBS is isolated from the listed areas in 7-30% of cases (more often in young people who have high sexual activity or use intrauterine contraceptives). Of these, 60-75% remain GBS carriers until the end of pregnancy. nine0003
The highest level of colonization in women of reproductive age and pregnant women. In pregnant women, GBS is isolated from the listed areas in 7-30% of cases (more often in young people who have high sexual activity or use intrauterine contraceptives). Of these, 60-75% remain GBS carriers until the end of pregnancy. nine0003
Vaginal-rectal swabs are collected to detect colonization of the vagina of pregnant women with group B streptococcus. In all other cases, the biomaterial is taken only if there are clinical signs of infection.
GBS has a natural sensitivity to beta-lactam antibiotics, including penicillins. Determination of sensitivity is necessary in cases where the patient has an individual intolerance to drugs of this group. nine0003
Isolateable microorganisms and pathogens:
- Streptococcus agalactiae.
What is the purpose of culture for group B beta-hemolytic streptococcus (Streptococcus group B, S. agalactiae)? in order to identify bacteriocarrier and determine the need for antibiotic prophylaxis during childbirth, to prevent neonatal complications (septicemia, pneumonia and neonatal meningitis).
 nine0003
nine0003 What can affect the result of the test "Culture for beta-hemolytic streptococcus group B (Streptococcus group B, S. agalactiae)"
Failure to follow the rules for preparing for the study may affect the result of the test.
Infections during pregnancy. Detection of group B streptococcus
05/16/2017
Infections during pregnancy that can be transmitted from mother to fetus deserve great attention, as they carry a potential risk of infection of the fetus or newborn and may lead to undesirable consequences. In addition, the diagnosis of infections during pregnancy has certain characteristics due to the asymptomatic course of most maternal infections or non-specific signs and symptoms. nine0003
Group B Streptococcus (GBS, Streptococcus agalactiae ) - Causes severe neonatal illness and poses a risk to certain patients in other age groups.
It has been estimated that GBS in 30% of pregnant women can be found in the vagina and often in the urethra of their sexual partners.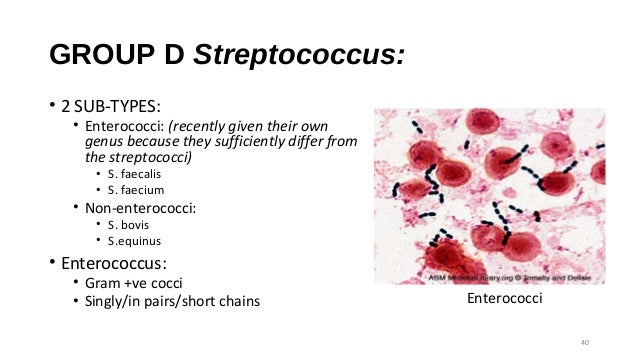 Despite the fact that GBS can occur as part of the normal intestinal microflora of a woman, their colonization of the urogenital tract of a pregnant woman poses a significant risk to the fetus due to the possibility of ascending infection. There is a significant relationship between the carriage of GBS in the vagina, not only with early infection of newborns (sepsis, pneumonia and meningitis), but also with premature birth, premature discharge of amniotic fluid, urinary infection in pregnant women, development of chorioamnionitis during childbirth, endometritis. nine0003
Despite the fact that GBS can occur as part of the normal intestinal microflora of a woman, their colonization of the urogenital tract of a pregnant woman poses a significant risk to the fetus due to the possibility of ascending infection. There is a significant relationship between the carriage of GBS in the vagina, not only with early infection of newborns (sepsis, pneumonia and meningitis), but also with premature birth, premature discharge of amniotic fluid, urinary infection in pregnant women, development of chorioamnionitis during childbirth, endometritis. nine0003
In the USA, Canada and European countries, regulated National programs for the prevention and treatment of GBS infections have been adopted, which are mandatory for all medical institutions.
From 01.05.17, DILA ML introduces a new study “Identification of group B streptococcus (streptococcus agalactiae) with sensitivity to antibiotics”.
| Prompt identification of pregnant women who are positive for group B streptococcus and who have risk factors for an increased chance of infection in the newborn allows to conduct intravenous antibiotic prophylaxis with the onset of labor and prevent early infection of the newborn with group B streptococcus:
|
Rules for preparation : 24 hours before the use of intravaginal and rectal medications should be excluded, before taking the biomaterial, do not wash the external genital organs.
The biomaterial is taken from two points: the lower third of the vagina and the next - the rectum, the overall result is evaluated. nine0099 Detection of group B streptococcus is carried out by a cultural method with the determination of sensitivity to antibiotics.
Research period: 6 days (Kyiv), 7.5 days (Regions).
Adequate assessment of the risk of infection of the newborn with group B streptococcus will significantly reduce the possibility of complications and ensure a favorable pregnancy outcome.
Literature:
1. Australasian society for infectious diseases, 2014
2. Antibiotic Prevention for Maternal Group B Streptococcal Colonization on Neonatal GBS-Related Adverse Outcomes: A Meta-Analysis, Shunming Li, Jingya Huang, 2017.