Grade 1 posterior placenta
Placenta praevia | Pregnancy Birth and Baby
Placenta praevia | Pregnancy Birth and Baby beginning of content4-minute read
Listen
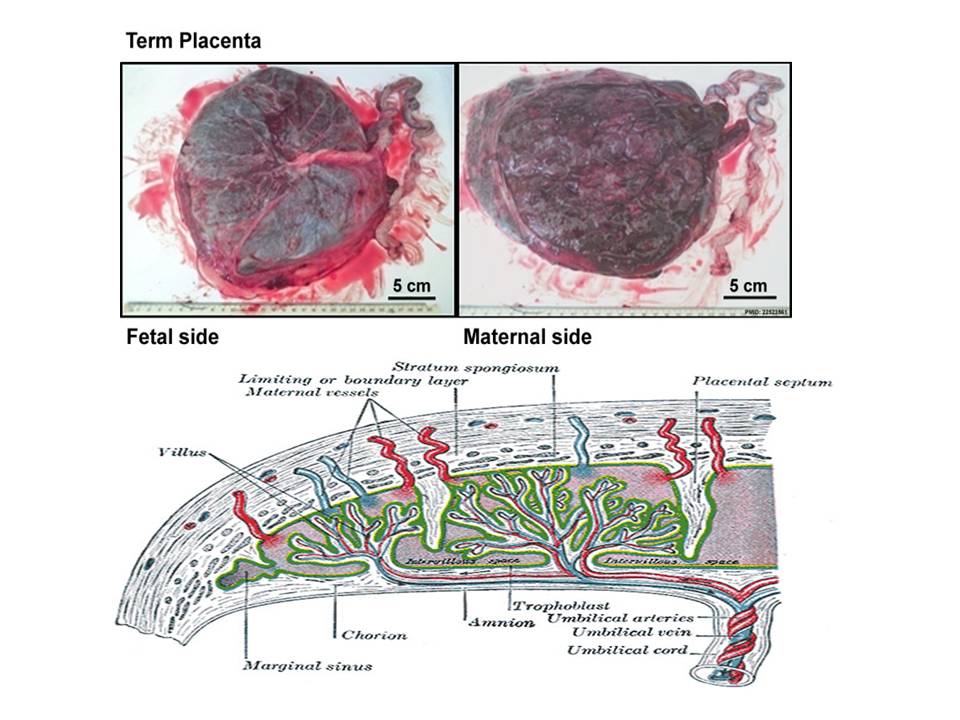
The placenta develops at the same time as your baby and is attached to the lining of your uterus (womb) during pregnancy. It allows for oxygen and nutrients to pass from you to your baby as well as producing hormones that support your pregnancy.
The fertilised ovum (egg) implants into the lining of your uterus and the placenta grows from there. As your pregnancy progresses and your baby and placenta increase in size, your womb expands and this affects the placenta's position. The area where the placenta is usually attached stretches upwards, moving the placenta away from your cervix.
If the placenta stays low in your womb, near to or covering your cervix, it may block the baby's way out. This is called 'low-lying placenta' or 'placenta praevia'.
The position of your placenta will be recorded at your 18-22 week ultrasound scan. If your placenta is significantly low, you'll be offered an extra ultrasound scan later in your pregnancy (usually at about 32 weeks) to check its position again. For most women, the placenta will have moved into the upper part of the womb by this stage.
What causes placenta praevia?
There is no obvious cause for placenta praevia. It may be that there is a larger placenta area (such as, if you are having twins) or there could be scar tissue from a previous caesarean or curette. There are several factors that can increase your risk of placenta praevia, including having had a caesarean section in the past (especially if your last baby was born by caesarean), and older age in the mother.
There is nothing you can do to prevent placenta praevia.
Placenta praevia symptoms
Signs that the placenta could be low-lying include painless, bright red bleeding from the vagina (either spontaneously or after sex) any time after 20 weeks of pregnancy. Placenta praevia is the most common cause of painless bleeding in the last trimester of pregnancy.
Placenta praevia is the most common cause of painless bleeding in the last trimester of pregnancy.
You may also experience:
- cramping in your uterus with bleeding
- bleeding during labour
If you experience bleeding during your pregnancy, contact your midwife or doctor immediately.
Placenta praevia treatment
Placenta praevia is graded into 4 categories from minor to major. If you have grade 1 or 2 it may still be possible to have a vaginal birth, but grade 3 or 4 will require a caesarean section.
Any grade of placenta praevia will require you to live near or have easy access to the hospital in case you start bleeding. Heavy bleeding may mean you need to be admitted to hospital for the remainder of your pregnancy.
When you are in hospital, your blood will be taken to make sure an exact donor blood match is available in case you need a blood transfusion. You may also need to take iron tablets if you have anaemia (low blood haemoglobin level).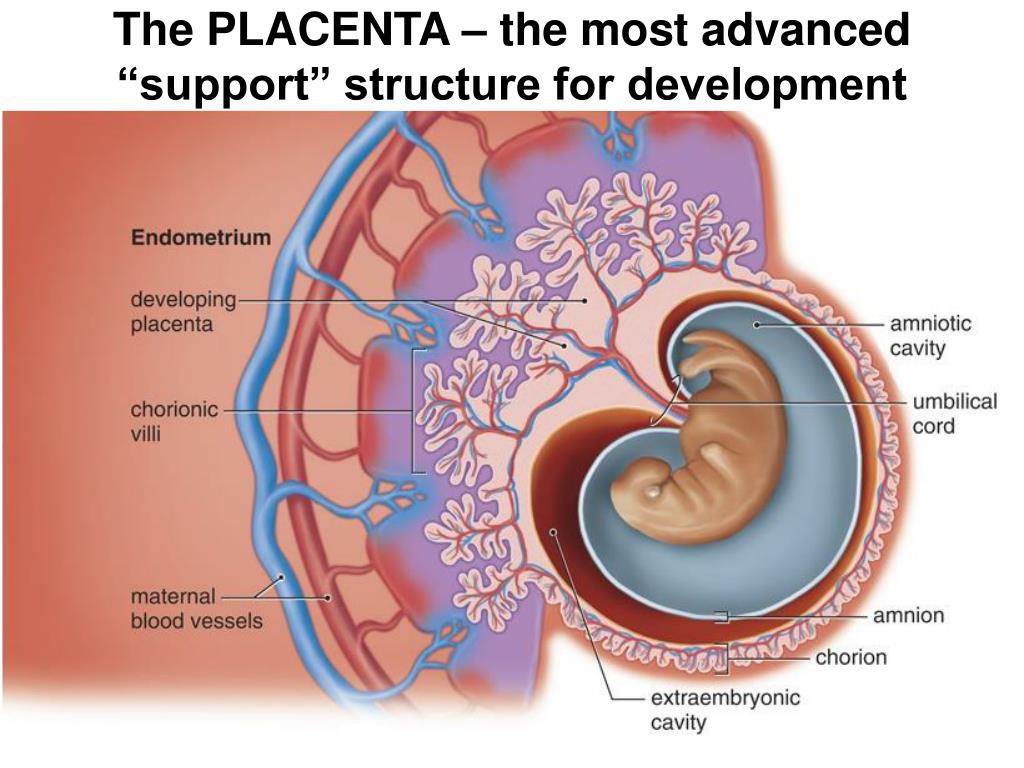
If you have bleeding during your pregnancy and have Rh negative blood, you will need an injection of Anti D so your baby is not affected by the bleeding.
Your baby may also be monitored with a cardiotocograph (CTG) to make sure they are not distressed. The CTG records your baby's heart rate and response to movements and contractions.
Being in hospital doesn't stop you from bleeding, but your baby can be delivered more quickly if needed. Your doctor or midwife will discuss any test results with you and what steps may be needed to ensure you and your baby's wellbeing.
As well as speaking to your doctor or midwife for advice, you can get help and information from:
- Pregnancy, Birth and Baby — call 1800 882 436 to speak to a maternal child health nurse (7 days a week, 7am to midnight AET).
- The Australian Birth Trauma Association offers advice, resources and a peer-to-peer support service.
- The Centre of Perinatal Excellence (COPE) provides information and a list of support services.

- Perinatal Anxiety & Depression Australia (PANDA) — call 1300 726 306 to speak with a counsellor (Mon to Fri, 9am to 7.30pm AET).
Sources:
RANZCOG (Placenta praevia, placenta praevia accreta and vasa praevia: diagnosis and management), Women's and Children's Health Network (Placenta praevia), March of Dimes (Placenta previa)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: October 2019
Back To Top
Related pages
- Placenta complications in pregnancy
- What is the placenta?
Need more information?
Placenta previa - Better Health Channel
betterhealth.vic.gov.au
Read more on Better Health Channel website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.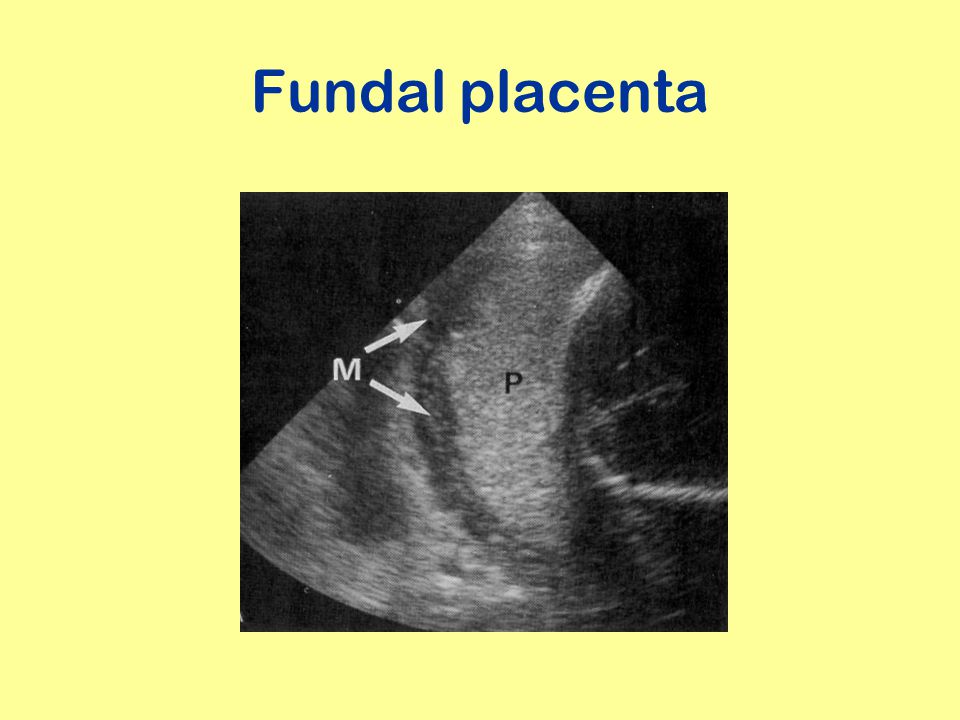
Need further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari.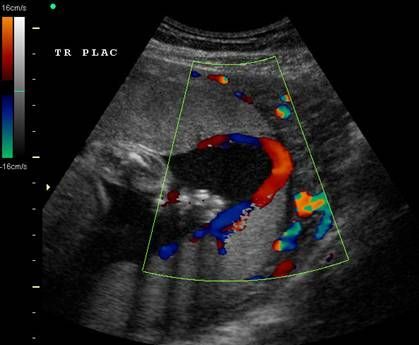 For more information, please visit the links below:
For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Is Posterior Positioning Good for the Baby?
The placenta is a temporary organ that attaches itself to the uterus and to the fetus’s umbilical cord. It’s through the placenta that the growing fetus is able to get oxygen and nutrients.
The positioning of the placenta is very important and determines whether you will be able to give birth vaginally or if a cesarean section will be safer.
Placental development stages
By attaching itself to the fetus’s umbilical cord, the placenta provides the fetus with nourishment and oxygen while also eliminating the fetus’s waste.
How does the placenta develop?
The placenta begins to grow when the blastocyst implants itself into your uterus.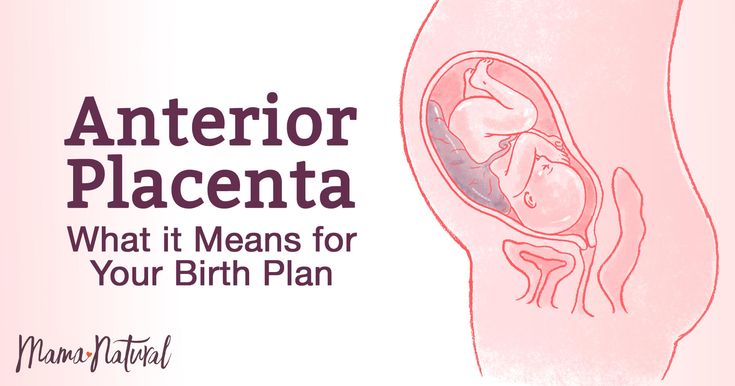 The blastocyst is the bunch of cells, referred to as the inner cell mass, that develops into the embryo. The outer cluster of cells, known as the trophoblast, forms the placenta.
The blastocyst is the bunch of cells, referred to as the inner cell mass, that develops into the embryo. The outer cluster of cells, known as the trophoblast, forms the placenta.
The trophoblast grows quickly, and its cells split into two layers: cytotrophoblasts, which are the inner cells, and syncytiotrophoblasts, which are the outer cells.
The inner cells of the placenta reshape blood vessels in your uterus. This is how the placenta receives blood to provide the fetus with nutrients.
The placenta develops wherever the fertilized egg embeds itself in your uterus:
- Anterior position — on the front wall of your uterus, closest to the belly
- Posterior position — on the back wall of your uterus, closest to the spine
- Fundal position — on the top wall of your uterus
- Lateral position — on the right or left side of your uterus
These are all normal places for the placenta to implant and grow.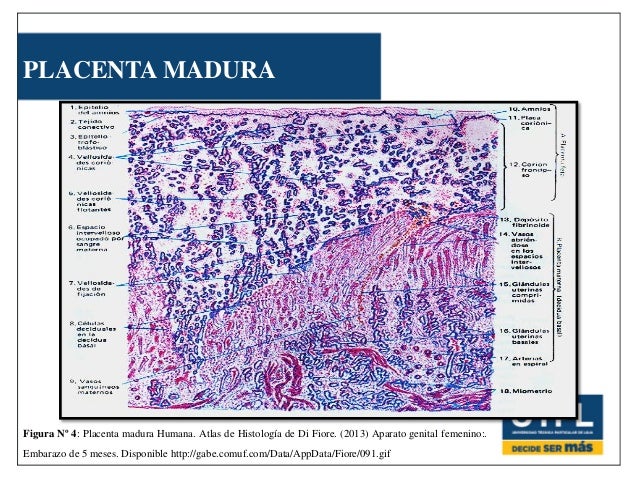
When the placenta attaches itself to the back of the uterus, it is called a posterior placenta. When it attaches itself to the front of the uterus, it is known as an anterior placenta.
The placenta undergoes numerous changes from conception to birth. As the fetus grows, the placenta grows to accommodate their development. By the time you give birth, the placenta may weigh as much as a pound (500 grams) and measure 9 inches in length. After the baby is born, your uterus will also contract to expel the placenta.
Take a quiz
Find out what you can do with our Health Assistant
What is it?
The term posterior placenta describes the placenta’s attachment to the back wall of the uterus.
If your health care provider determines that you have a posterior placenta, there’s no need to worry. It’s completely normal. The upper (or fundal) portion of the uterine back wall is one of the best locations for the fetus to be in. It allows them to move into the anterior position just before birth.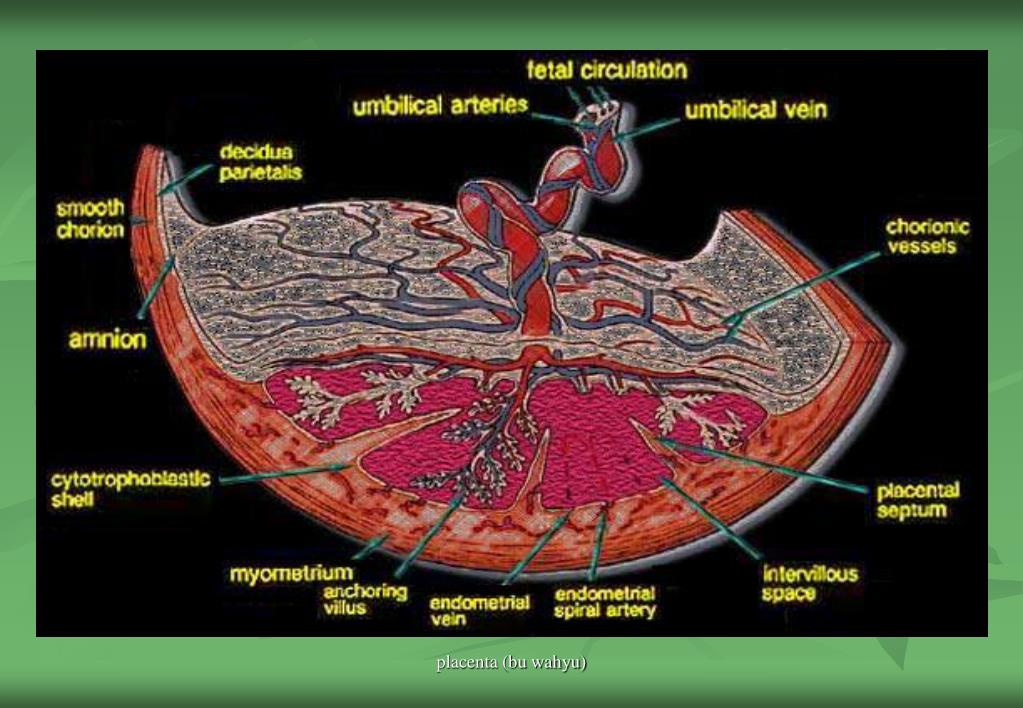
Furthermore, a posterior placenta does not affect or interfere with the growth and development of the fetus.
How does placenta positioning affect delivery?
During pregnancy, the placenta location can change. This is why your health care provider may perform an ultrasound scan in the second trimester of pregnancy (roughly 18 to 21 weeks). Another scan may be necessary in the third trimester to double-check placenta positioning before delivery.
One placental location that might be problematic is when the placenta grows toward the cervix. This is called placenta previa. In this position, the placenta could detach from the uterine wall and cause premature labor or internal bleeding.
Another condition, known as placenta accreta, happens when parts of the placenta attach too deeply into the uterine wall. Instead of completely detaching itself after delivery, some or all of the placenta remains in the uterus, sometimes resulting in bleeding.
In such cases, your health care provider may recommend a caesarian section and a post-delivery hysterectomy.
In some rare instances, the placenta remains in the uterus after the baby has been delivered. This is called a retained placenta, and when left untreated, it can lead to complications including infections and heavy vaginal bleeding.
Anterior vs. posterior placenta
To recap, a posterior placenta is one that attaches itself to the back of the uterus, while an anterior placenta attaches itself to the front. Both placental positions are considered normal. Aside from being an ideal location for delivery, the other benefit of a posterior placenta is being able to feel your baby’s movements early on.
This is not the case with an anterior placenta because the placenta may create more space between the baby and your abdomen. Neither posterior or anterior placental location will affect the development or growth of a strong and healthy baby.
0, 1, 2, 3 by week of pregnancy. Calculator
Degree of maturity of the placenta - 0
Degree of maturity of the placenta 0 (zero degree) is normally observed up to 30 weeks of pregnancy.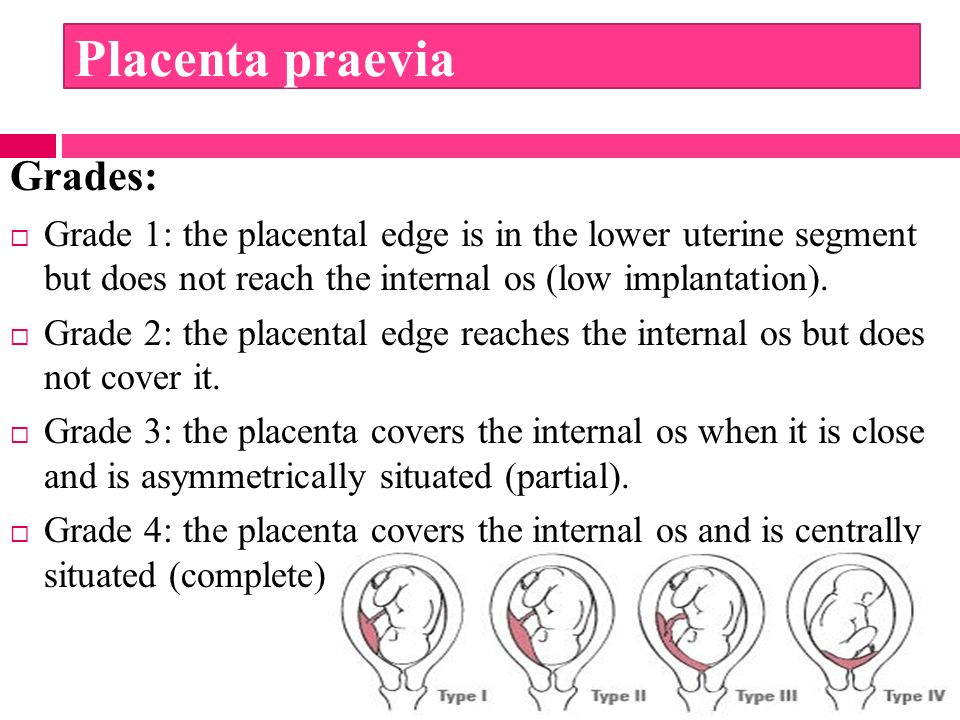
The chorionic membrane at grade 0 is a smooth, straight, echogenic line without dimples. The parenchyma is homogeneous (homogeneous), low echo density. The basal layer is not identified.
Zero placenta
Placenta 1
The degree of maturity of the placenta 1 (first degree) is normally observed from 27 to 34 weeks of pregnancy. Basically, the first degree is noted for the period from the thirtieth to the thirty-second week of pregnancy.
Grade 1 is characterized by a slightly wavy chorionic plate. Randomly distributed individual echogenic inclusions of various shapes appear in the tissue. The basal layer is not identified.
First stage of placental maturity
Placental stage of maturity - 2
The degree of maturity of the placenta 2 (second degree) is normally observed from 34 to 39 weeks of pregnancy.
At grade 2, the waviness of the chorionic plate increases.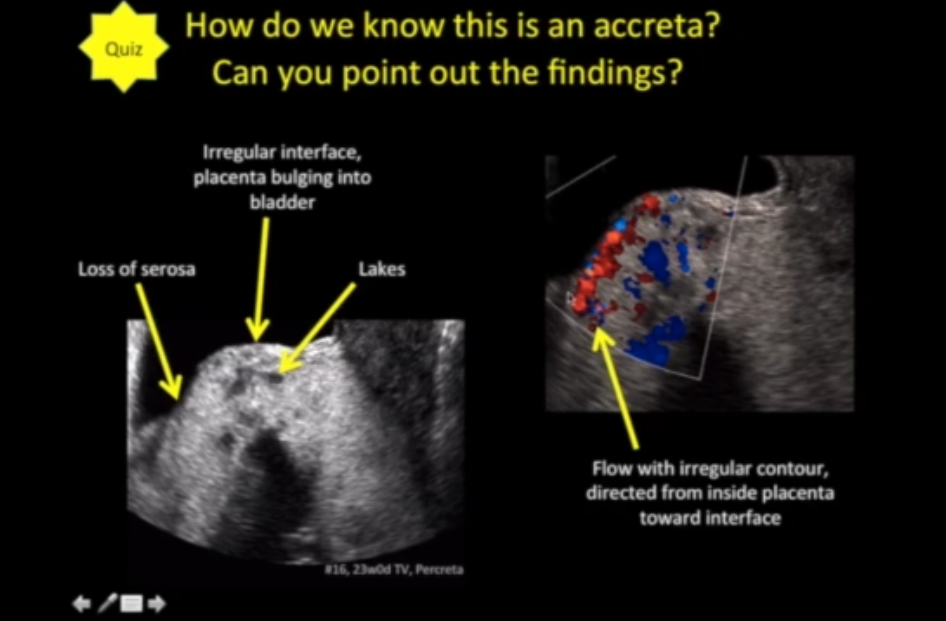 Depressions appear on the chorionic plate, turning into perpendicular linear seals, but not reaching the basal layer. Multiple small echopositive inclusions in the form of lines and dots are visible, the so-called "dot-dash-dot" configuration.
Depressions appear on the chorionic plate, turning into perpendicular linear seals, but not reaching the basal layer. Multiple small echopositive inclusions in the form of lines and dots are visible, the so-called "dot-dash-dot" configuration.
Placenta II
The degree of maturity of the placenta - 3
The third degree of maturity of the placenta is observed after 37 weeks of gestation and is typical for full-term pregnancy. The onset of stage 3 before 37 weeks of pregnancy is usually regarded as premature maturation - one of the indicators of placental insufficiency, which requires constant careful monitoring of the fetus.
Grade 3 of maturity is characterized by pronounced tortuosity of the chorionic membrane, the presence of depressions in the chorionic plate, turning into perpendicular linear seals that reach the basal layer. The placenta acquires a lobular structure. Visible significant calcification of the basal plate (rounded areas of increased echo density are determined).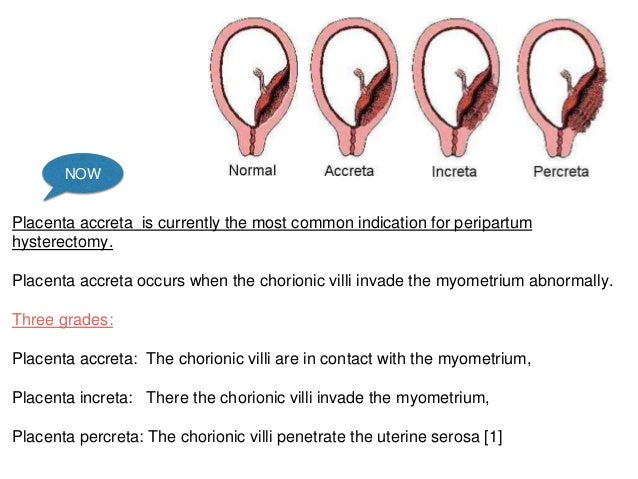
Third degree of placental maturity
Inconsistency with the gestational age (premature or early maturation of the placenta)
At the end of pregnancy, the so-called physiological aging of the placenta occurs, accompanied by a decrease in the area of its exchange surface, the appearance of areas of salt deposition.
If the placenta changes structure prematurely (for example, the appearance of 1 degree of maturity before 27 weeks of pregnancy, 2 degrees before 32 weeks, and 3 degrees of maturity before 36 weeks), then this indicates about its premature maturation and talk about premature aging - one of the indicators of placental insufficiency, which requires constant careful monitoring of the fetus.
There are various reasons for premature maturation of the placenta: impaired blood flow, intrauterine infections, preeclampsia, spotting in the first trimester of pregnancy, hormonal disorders (for example, maternal diabetes mellitus), threatened miscarriage, twin pregnancy, and others.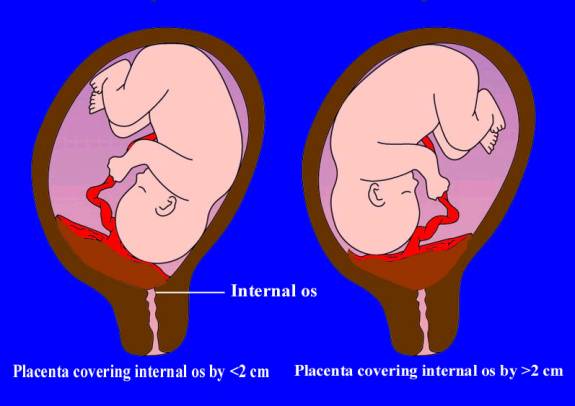
Therefore, when determining the 1, 2, 3 degree of placental maturity before the established dates, the ultrasound doctor at the end of the study makes a diagnosis of "premature maturation of the placenta".
If premature maturation of the placenta is detected, the attending physician prescribes complex treatment with drugs to improve the function of the placenta and prevent fetal hypoxia. It is also recommended dopplerometry (monitoring the state of blood circulation in the mother-placenta-fetus system), fetal CTG (cardiomonitor study) - at 33-34 weeks and repeated ultrasound after 1 month. Drugs are prescribed that improve blood circulation in the placenta (for example, chimes), vitamins, rest and good nutrition.
Delayed maturation of the placenta is less common and most often associated with congenital malformations of the fetus. However, risk factors may be the presence of diabetes in the expectant mother, Rh conflict, smoking during pregnancy. With a delay in the maturation of the placenta, the risk of having a dead baby increases.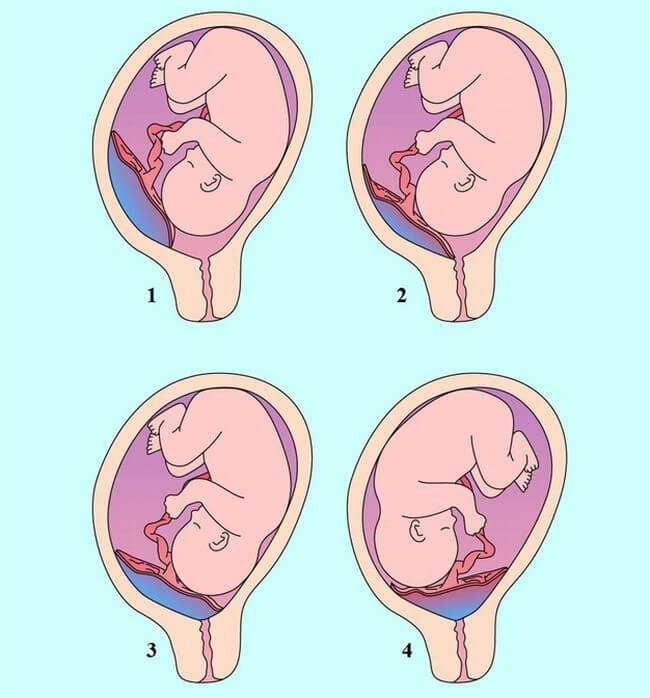
Determining the degree of maturity of the placenta plays an important role in the management of pregnancy. However, the degree of maturity is a subjective factor, it is established only with an ultrasound examination, and since the assessment of this indicator is determined “by eye”, the degree of maturity may differ for each diagnostician.
Criteria for evaluating the maturity of the placenta are very subjective and may differ for each ultrasound doctor.
If there is a slight discrepancy between the degree of maturity of the placenta and the gestational age, then there is nothing to worry about. Most likely, its early maturation is a feature of a pregnant woman. If the aging of the placenta began much earlier than the due date, then this is one of the important diagnostic signs of placental insufficiency.
With premature aging, a decrease or increase in the thickness of the placenta is manifested. So a “thin” placenta (less than 20 mm in the 3rd trimester of pregnancy) is characteristic of late toxicosis, a threat of abortion, fetal malnutrition, while with hemolytic disease and diabetes mellitus, a “thick” placenta (50 mm or more) indicates placental insufficiency .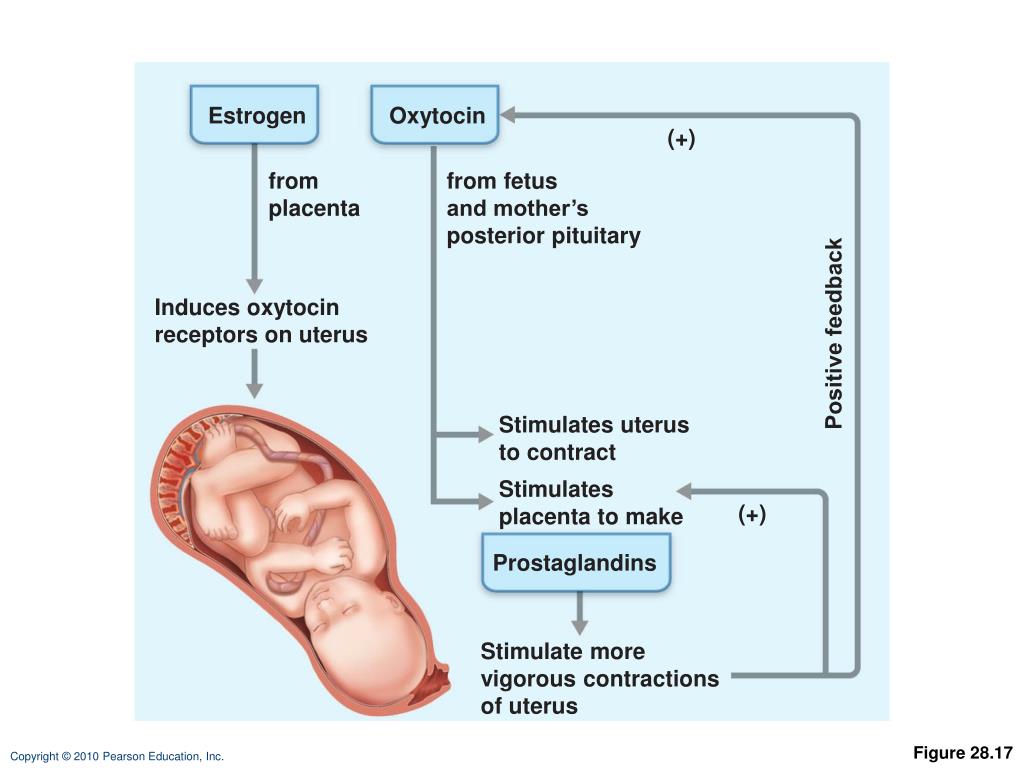 Thinning or thickening of the placenta indicates the need for therapeutic measures and requires a second ultrasound examination.
Thinning or thickening of the placenta indicates the need for therapeutic measures and requires a second ultrasound examination.
Late maturation of the placenta (prolonged immaturity) is rare, more often in pregnant women with diabetes mellitus, Rhesus conflict, and also with congenital malformations of the fetus. The delay in the maturation of the placenta leads to the fact that it does not properly perform its functions. Often late maturation leads to stillbirths and mental retardation in the fetus.
Makarov I.O. • Placenta previa
Ultrasound scanner HS70
Accurate and confident diagnosis. Multifunctional ultrasound system for examinations with expert diagnostic accuracy.
In the normal course of pregnancy, the placenta is usually located in the area of the fundus or body of the uterus, along the back wall, with the transition to the side walls, i.e. in those areas where the walls of the uterus are best supplied with blood. On the anterior wall, the placenta is located somewhat less frequently, since the anterior wall of the uterus undergoes significantly more changes than the posterior one.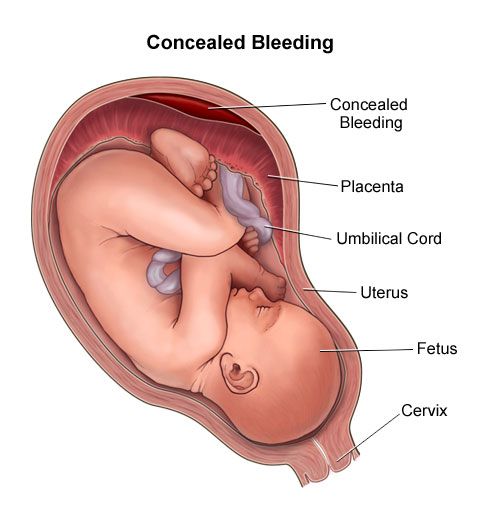 In addition, the location of the placenta on the back wall protects it from accidental injury.
In addition, the location of the placenta on the back wall protects it from accidental injury.
Placenta previa is a pathology in which the placenta is located in the lower parts of the uterus along any wall, partially or completely blocking the area of the internal os. The incidence of placenta previa averages from 0.1% to 1% of the total number of births.
If the placenta only partially covers the area of the internal pharynx, then this is an incomplete presentation, which occurs with a frequency of 70-80% of the total number of presentations. If the placenta completely covers the area of the internal os, then this is a complete placenta previa. This option occurs with a frequency of 20-30%.
There is also a low location of the placenta, when its edge is at a lower level than it should be in the norm, but does not cover the area of the internal os.
Causes of low or low placenta
There are several causes of low or low placenta. The most common causes are pathological changes in the inner layer of the uterus (endometrium) due to inflammation, surgical interventions (curettage, caesarean section, removal of myomatous nodes, etc. ), multiple complicated births. In addition, violations of the attachment of the placenta can be caused by uterine fibroids, endometriosis, underdevelopment of the uterus, isthmicocervical insufficiency, inflammation of the cervix, multiple pregnancy. It should be noted that placenta previa is more common in re-pregnant women than in primiparas. Due to these factors, the fetal egg that enters the uterine cavity after fertilization cannot be implanted in the upper sections of the uterus in a timely manner, and this process is carried out only when the fetal egg has already descended into its lower sections.
), multiple complicated births. In addition, violations of the attachment of the placenta can be caused by uterine fibroids, endometriosis, underdevelopment of the uterus, isthmicocervical insufficiency, inflammation of the cervix, multiple pregnancy. It should be noted that placenta previa is more common in re-pregnant women than in primiparas. Due to these factors, the fetal egg that enters the uterine cavity after fertilization cannot be implanted in the upper sections of the uterus in a timely manner, and this process is carried out only when the fetal egg has already descended into its lower sections.
The most common manifestation in placenta previa is recurrent bleeding from the genital tract. Bleeding can occur during various periods of pregnancy, starting from its earliest terms. However, most often they are observed already in the second half of pregnancy due to the formation of the lower segment of the uterus. In the last weeks of pregnancy, when uterine contractions become more intense, bleeding may increase.
Bleeding is caused by repeated abruption of the placenta, which is unable to stretch following the stretching of the uterine wall as pregnancy progresses or labor begins. In this case, the placenta partially exfoliates, and bleeding occurs from the vessels of the uterus. The fetus does not shed blood. However, he is threatened by oxygen starvation, since the exfoliated part of the placenta is not involved in gas exchange.
Provoking factors for bleeding during pregnancy can be: physical activity, sudden coughing, vaginal examination, sexual intercourse, increased intra-abdominal pressure with constipation, thermal procedures (hot bath, sauna).
With complete placenta previa, bleeding often occurs suddenly, without pain, and can be very heavy. Bleeding may stop, but reappear after some time, or may continue in the form of scanty discharge. In the last weeks of pregnancy, bleeding resumes and / or increases.
With incomplete placenta previa, bleeding may begin at the very end of pregnancy.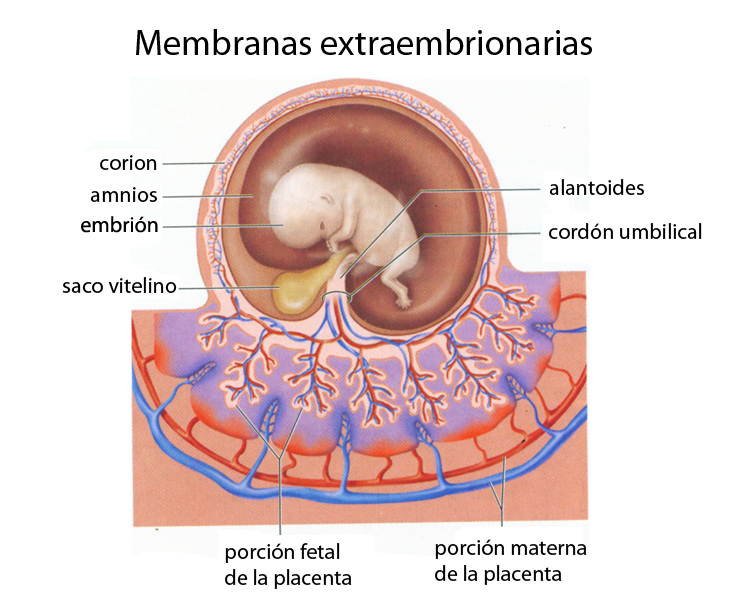 However, more often it occurs at the beginning of labor. The amount of bleeding depends on the size of the placenta previa. The more placental tissue is present, the earlier and more bleeding begins.
However, more often it occurs at the beginning of labor. The amount of bleeding depends on the size of the placenta previa. The more placental tissue is present, the earlier and more bleeding begins.
Recurrent bleeding during pregnancy complicated by placenta previa in most cases leads to the development of anemia.
Pregnancy with placenta previa is often complicated by the threat of miscarriage, which is due to the same reasons as the occurrence of an incorrect location of the placenta. Preterm labor most often occurs in patients with complete placenta previa.
Pregnant women with placenta previa are characterized by low blood pressure, which occurs in 25%-34% of cases.
Preeclampsia (nephropathy, late toxicosis) is also no exception for pregnant women with placenta previa. This complication, which occurs against the background of dysfunction of a number of organs and systems, as well as with symptoms of blood clotting disorders, significantly worsens the nature of recurrent bleeding.
Placenta previa is often accompanied by fetal placental insufficiency, lack of oxygen for the fetus and delayed development. The exfoliated part of the placenta is switched off from the general system of the uteroplacental circulation and does not participate in gas exchange. With placenta previa, an incorrect position of the fetus (oblique, transverse) or breech presentation is often formed, which in turn are accompanied by certain complications.
In obstetric practice, the term "migration of the placenta" is widely rooted, which, in fact, does not reflect the real essence of what is happening. The change in the location of the placenta is carried out due to a change in the structure of the lower segment of the uterus during pregnancy and the direction of growth of the placenta towards a better blood supply to the sections of the uterine wall (towards the bottom of the uterus) compared to its lower sections. A more favorable prognosis in terms of placental migration is noted when it is located on the anterior wall of the uterus. Usually the process of "migration of the placenta occurs within 6-10 weeks and is completed by the middle of 33-34 weeks of pregnancy.
Usually the process of "migration of the placenta occurs within 6-10 weeks and is completed by the middle of 33-34 weeks of pregnancy.
Diagnosis of placenta previa
Placenta previa is not difficult to detect. The presence of placenta previa may be indicated by complaints of a pregnant woman about bleeding. In this case, recurrent bleeding from the second half of pregnancy, as a rule, is associated with complete placenta previa. Bleeding at the end of pregnancy or at the beginning of labor is more often associated with incomplete placenta previa.
In the presence of bleeding, carefully examine the walls of the vagina and cervix using speculums to exclude trauma or pathology of the cervix, which may also be accompanied by the presence of bloody discharge.
A vaginal examination of a pregnant woman also easily reveals clear diagnostic signs indicating an abnormal location of the placenta. However, such a study must be performed as carefully as possible, in compliance with all the necessary rules to prevent possible bleeding.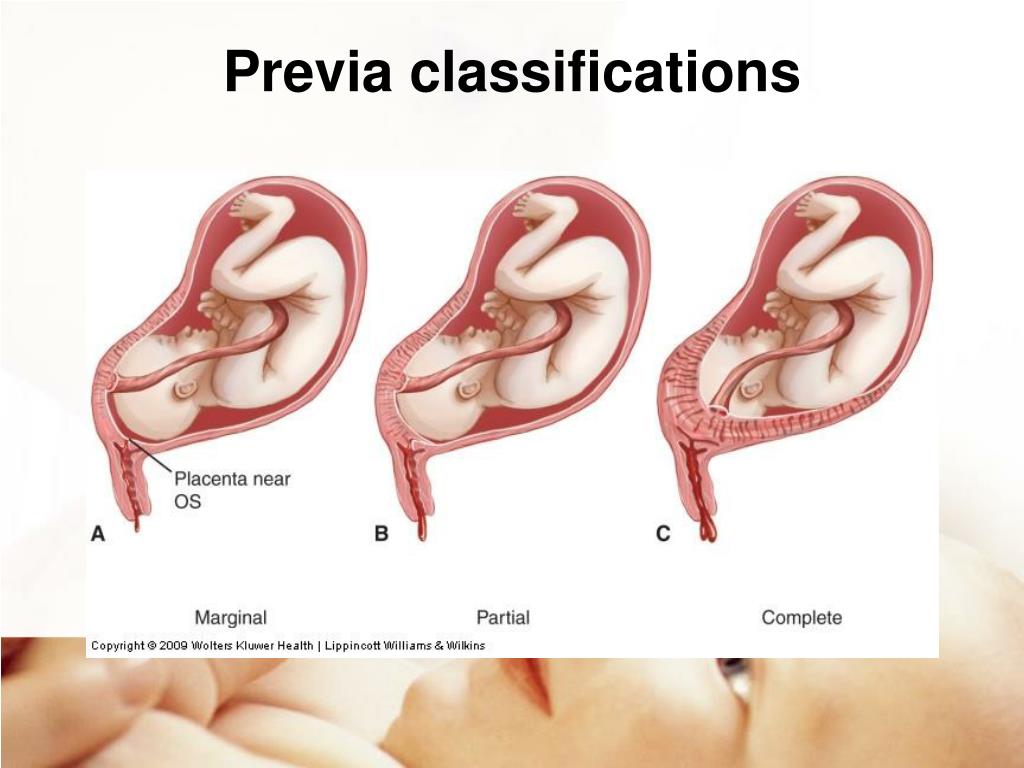
Currently, the most objective and safest method for diagnosing placenta previa is ultrasound, which allows you to establish the fact of placenta previa and the variant of placenta previa (complete, incomplete), determine the size, structure and area of the placenta, assess the degree of detachment, as well as get an accurate picture of the migration of the placenta.
If the ultrasound revealed complete placenta previa, then a vaginal examination should not be performed at all. The criterion for the low location of the placenta in the III trimester of pregnancy (28 - 40 weeks) is the distance from the edge of the placenta to the area of the internal os 5 cm or less. Placenta previa is indicated by the presence of placental tissue in the area of the internal os.
The nature of the localization of the placenta in the II and III trimesters of pregnancy (up to 27 weeks) is judged by the ratio of the distance from the edge of the placenta to the area of the internal os, with the diameter value (BDP) of the fetal head.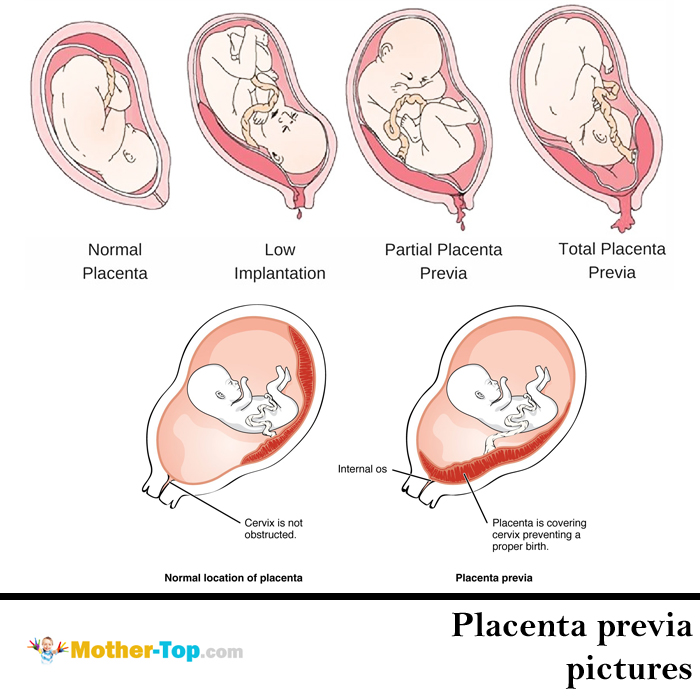
If an abnormal location of the placenta is detected, a dynamic study should be carried out to monitor its "migration". For these purposes, it is advisable to perform at least three echographic controls during pregnancy at 16, 24-26 and 34-36 weeks.
Ultrasound should be done when the bladder is moderately full. With the help of ultrasound, it is also possible to determine the presence of an accumulation of blood (hematoma) between the placenta and the wall of the uterus during placental abruption (in the event that there was no outflow of blood from the uterine cavity). If the site of placental abruption occupies no more than 1/4 of the area of the placenta, then the prognosis for the fetus is relatively favorable. In the event that the hematoma occupies more than 1/3 of the area of the placenta, then most often this leads to the death of the fetus.
Medical support for pregnant women with placenta previa
The nature of management and treatment of pregnant women with placenta previa depends on the severity of bleeding and the amount of blood loss.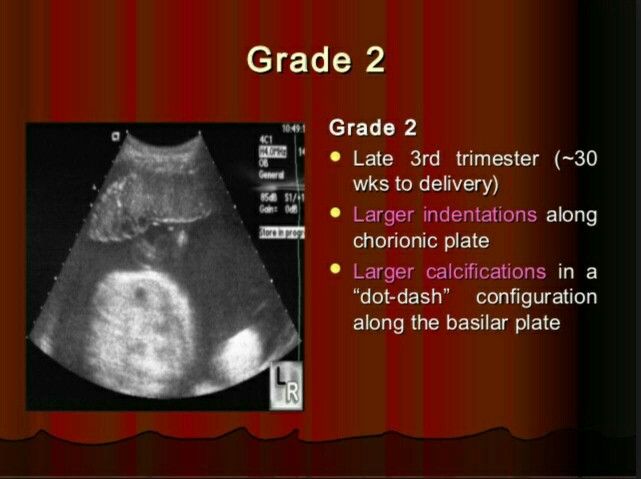
In the first half of pregnancy, if there are no blood discharges, then the pregnant woman can be at home under outpatient control in compliance with the regime that excludes the action of provoking factors that can cause bleeding (restriction of physical activity, sexual activity, stressful situations, etc.)
Observation and treatment for more than 24 weeks of pregnancy is carried out only in an obstetric hospital.
Treatment aimed at continuing the pregnancy up to 37-38 weeks is possible if the bleeding is not heavy, and the general condition of the pregnant woman and the fetus is satisfactory. Even despite the cessation of bloody discharge from the genital tract, pregnant women with placenta previa can under no circumstances be discharged from the hospital before delivery.
Management of pregnant women in an obstetric hospital includes: observance of strict bed rest; the use of drugs that ensure the optimization of the normalization of contractile activity; treatment of anemia and fetal placental insufficiency.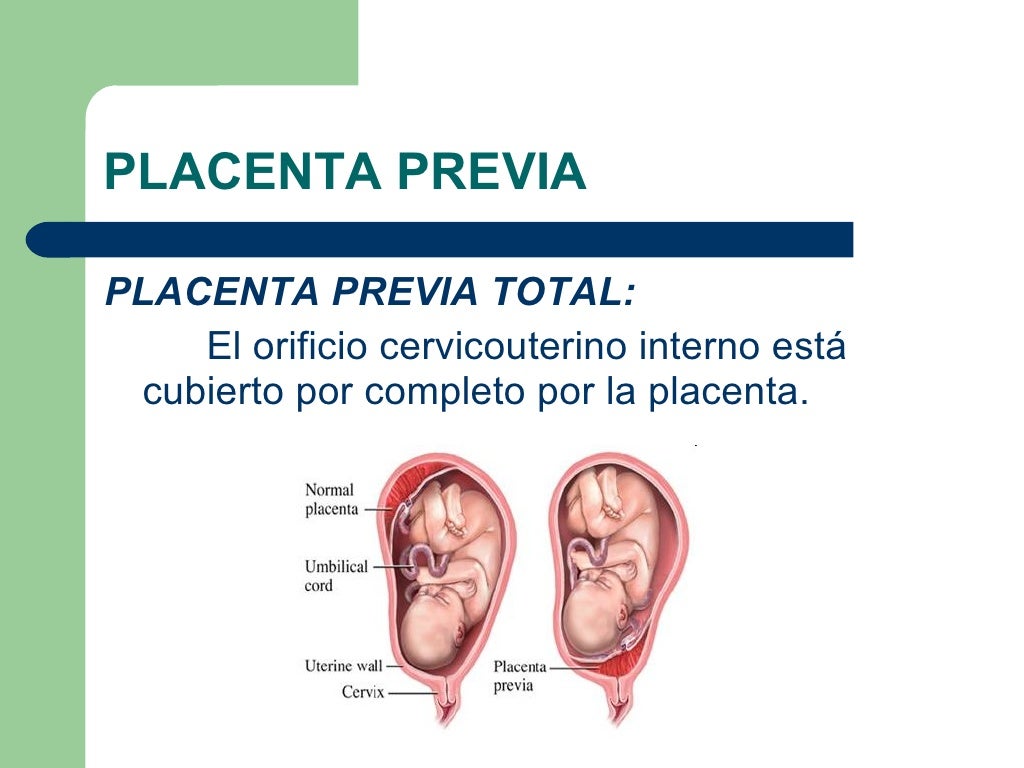
Emergency caesarean section, regardless of gestational age, is indicated for: recurrent bleeding; a combination of small blood loss with anemia and a decrease in blood pressure; simultaneous profuse blood loss; complete placenta previa and bleeding.
The operation is performed according to vital indications on the part of the mother, regardless of the duration of pregnancy and the condition of the fetus.
In the event that the pregnancy was carried out to 37-38 weeks and placenta previa persists, depending on the situation, the most optimal method of delivery is chosen on an individual basis.
The absolute indication for elective caesarean section is complete placenta previa. Childbirth through the natural birth canal in this situation is impossible, since the placenta that covers the internal os does not allow the presenting part of the fetus (fetal head or pelvic end) to be inserted into the pelvic inlet. In addition, in the process of increasing uterine contractions, the placenta will exfoliate more and more, and the bleeding will increase significantly.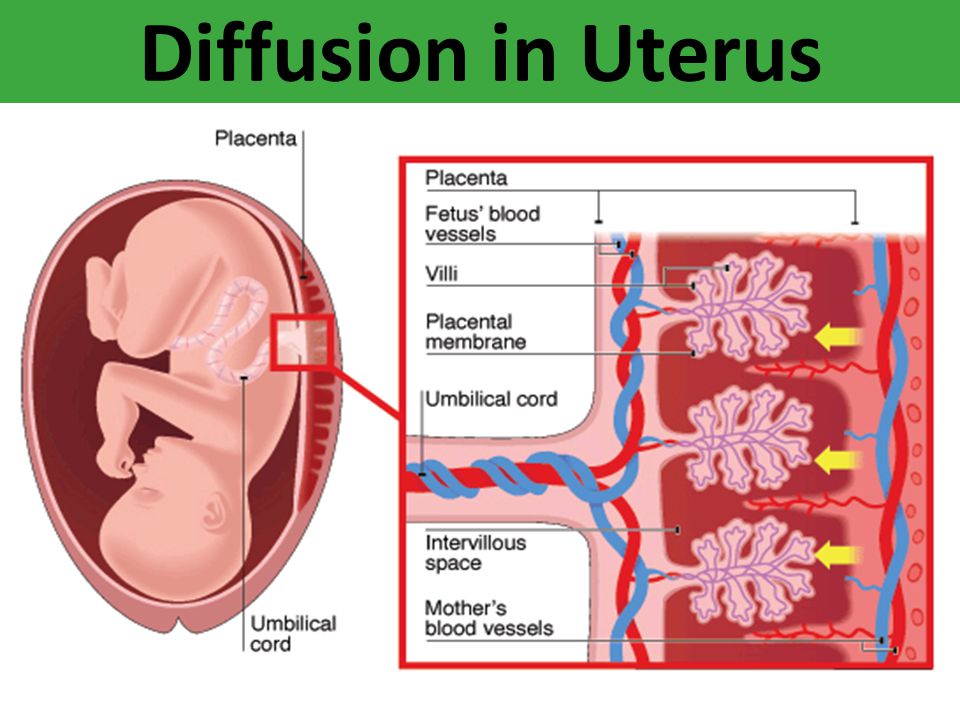
In case of incomplete placenta previa and in the presence of concomitant complications (breech presentation, malposition of the fetus, uterine scar, multiple pregnancy, severe polyhydramnios, narrow pelvis, age of the primiparous over 30 years, etc.), a caesarean section should also be performed in a planned manner.
If the above associated complications are absent and there is no blood discharge, then you can wait until the onset of independent labor activity, followed by early opening of the fetal bladder. In the event that after opening the fetal bladder, bleeding nevertheless began, then it is necessary to resolve the issue of performing a caesarean section.
If, with incomplete placenta previa, bleeding occurs before the onset of labor, then the fetal bladder is opened. The necessity and expediency of this procedure is due to the fact that when the membranes are opened, the fetal head is inserted into the entrance to the pelvis and presses the exfoliated part of the placenta against the wall of the uterus and pelvis, which helps to stop further placental abruption and stop bleeding.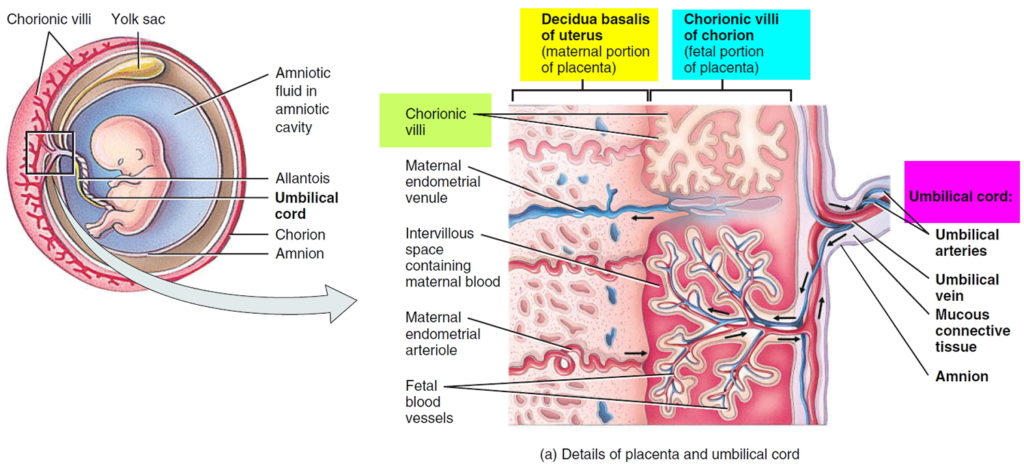 If bleeding after opening the fetal bladder continues and / or the cervix is immature, then a caesarean section is performed. In the case of stopping bleeding, it is possible to conduct labor through the natural birth canal (with a favorable obstetric situation).
If bleeding after opening the fetal bladder continues and / or the cervix is immature, then a caesarean section is performed. In the case of stopping bleeding, it is possible to conduct labor through the natural birth canal (with a favorable obstetric situation).
Bleeding can also start in the early stages of labor, from the moment of the first contractions. In this case, early opening of the fetal bladder is also shown.
Thus, the management of childbirth with incomplete placenta previa through the natural birth canal is possible if: the bleeding stopped after opening the fetal bladder; mature cervix; labor activity is good; there is a cephalic presentation of the fetus.
However, caesarean section is one of the most frequently chosen methods of delivery by obstetricians in placenta previa and is performed with a frequency of 70% -80% in this pathology.
Other typical complications in childbirth with incomplete placenta previa are weakness of labor and insufficient oxygen supply to the fetus (fetal hypoxia).