Dairy face rash
4 Unexpected Signs You May Have a Dairy Allergy
A dairy allergy is one of the most common food allergies, and it is particularly prevalent in young children. Up to three percent of children in western populations are estimated to be allergic to dairy, and while many children grow out of the affliction, 6.1 million adults in America reported dairy allergy symptoms in 2019. Symptoms can range from very severe life-threatening anaphylaxis to less serious reactions such as hives. You deserve to feel your best every day. Read on to learn more about dairy allergy symptoms, its causes, and its cures.
What Is a Dairy Allergy?
A dairy allergy is an immunological reaction to the proteins in milk (casein and whey). When an individual with a milk allergy consumes dairy of any kind, the body triggers an immune response to fight off what it sees as a harmful substance. Individuals can experience an array of symptoms that are a result of this immune response.
Signs and Symptoms of a Dairy Allergy
A dairy or milk allergy reaction can be immediate or occur up to three days after consuming dairy. These delayed responses make the allergy difficult to diagnose, as people may not associate their symptoms with the bowl of cows’ milk ice cream they ate three days prior. Symptoms range from mild and uncomfortable to severe and life-threatening.
Immediate Allergic Reactions to Milk and Dairy
Those who experience immediate allergic reactions to dairy are generally aware of their allergy. These symptoms include wheezing, rash, lip-swelling, and anaphylaxis.
4 Delayed Allergic Reactions to Milk and Dairy
Delayed allergies (called non-IgE mediated) may take up to three days for symptoms to manifest. Those who experience delayed allergic reactions often report ‘thick note syndromes’ (patients with long medical history files that no doctors have been able to help). The symptoms triggered by a dairy allergy may often look like disease and can seem elusive given their delayed response. The unifying mechanism underlying all these symptoms is inflammation. A dairy (or other food) allergy can lead to an overworked immune system and chronic inflammation in the body.
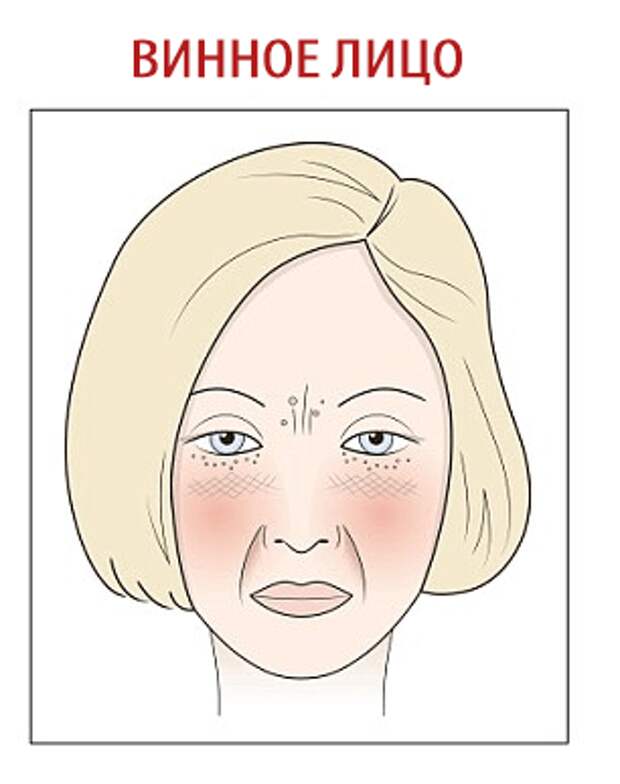
1. Eczema, Acne, and Other Skin Complaints
There are now multiple studies that support a link between acne and dairy consumption. A dairy allergy can also cause a delayed reaction manifesting as eczema. While more research is needed, those with chronic skin issues tend to report clearer skin after eliminating dairy from their diets.
2. Joint pains
Studies as far back as 1986 have illustrated improvements in joint symptoms (and even rheumatoid arthritis) with an elimination diet. Participants who suffered from joint pain and permanently eliminated dairy from their diets experienced pain relief, while those who reintroduced milk and dairy reported a return of their joint pain symptoms.
3. Asthma, Sinus Issues, and Other Respiratory Problems
The casein in dairy can cause increased mucus production in the airways and lungs. Over time, this excess mucus may lead to asthma symptoms and recurrent sinus problems like chronic sinusitis.
4. Fatigue and Weight Loss Resistance
Fatigue is such a common symptom of a dairy allergy, and while there are many other causes (issues with your thyroid or hormonal imbalance), if a full medical workup has been conducted and no cause for fatigue can be identified, it is advisable to discuss the possibility of a dairy allergy or other food sensitivity with your medical provider.
I Think I Have a Dairy Allergy, What Do I Do?
If you experience any of these symptoms, eliminate dairy from your diet for three weeks to determine if dairy may be the culprit. Monitor your symptoms and keep a diary. At the end of the three weeks, reintroduce dairy and take note if your symptoms start to reappear. If so, it’s a good indication that dairy is the cause of your symptoms. Once you permanently eliminate dairy from your diet, you should experience significant relief.
Don’t think you have a dairy allergy, but still suffer symptoms? You might be lactose intolerant. Take our Lactose Intolerance Test to find out
Take our Lactose Intolerance Test to find out
This content is for informational or educational purposes only. Please consult your healthcare provider in regard to recommendations and treatments as this material cannot be used as medical advice.
Cow’s milk allergy - Better Health Channel
About cow's milk allergy
An allergy to cow’s milk and related dairy products affects one in 50 in babies and is different to lactose intolerance. Very few adults are allergic to cow’s milk. People who are allergic to cow’s milk can also be allergic to milk from other animals such as goats, sheep and buffalo.
Symptoms of milk allergy vary and range from mild reactions to a severe allergic reaction (anaphylaxis). Some people experience symptoms immediately, but in others, the symptoms can take time to develop.
If you think you, or someone in your care, have a cow’s milk allergy, visit your doctor for a diagnosis. To manage a cow’s milk allergy, all food containing milk must be avoided (under strict medical supervision).
Exclusion and reintroduction of cow's milk and other dairy foods should only be undertaken with advice from a medical specialist (and in many cases, a dietitian), particularly in cases of anaphylaxis. If long-term exclusion is required, an alternative source of calcium and protein is needed, to ensure adequate nutrition and growth.
Do not change your child’s diet without consulting a doctor or your child could suffer from nutritional deficiencies.
Food allergies can be life threatening. If you, or someone in your care, have a severe allergic reaction (anaphylaxis), call triple zero (000) for an ambulance. Do not stand or walk. Administer adrenaline (epinephrine) via injector (EpiPen® or Anapen®), if available.
Causes of cow’s milk allergy
Milk allergy is most commonly caused by an allergy to cow’s milk, although some people are allergic to milk from other animals such as goats, sheep and buffalo.
In all allergies, the immune system reacts to triggers, also known as allergens.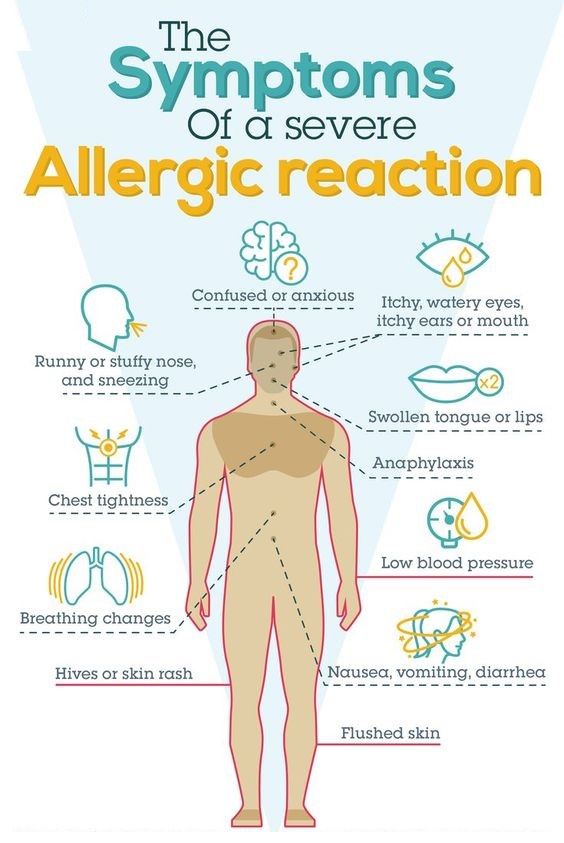 Your immune system produces antibodies that detect the allergen, causing inflammatory reactions and the release of chemicals, including histamine, which cause allergic symptoms.
Your immune system produces antibodies that detect the allergen, causing inflammatory reactions and the release of chemicals, including histamine, which cause allergic symptoms.
In the case of milk, the triggers are milk proteins including whey and casein. You or your child may be allergic to either one of these proteins, or both.
More research is needed into the causes, diagnosis and treatment of food allergy.
Some reactions to milk are not caused by allergies
Some people can have a physical reaction to milk that is not due to an allergy. If you lack an enzyme called lactase, which breaks down the milk sugar lactose, you can experience symptoms that seem similar to an allergy (diarrhoea, vomiting, stomach pain and gas). This is called lactose intolerance and is different from milk allergy, because it does not involve your immune system reacting to a trigger.
Some people also experience excess thick mucus in their throat after eating or drinking dairy products, but this is not caused by an allergy. The Australasian Society of Clinical Immunology and Allergy (ASCIA) advises that this mucus production is not a health risk.
The Australasian Society of Clinical Immunology and Allergy (ASCIA) advises that this mucus production is not a health risk.
Symptoms of cow’s milk allergy
Symptoms of a cow’s milk allergy can appear within minutes or several days of consuming cow’s milk or dairy products. The severity of the symptoms will depend on the person and the amount of cow’s milk they consume.
Symptoms that can appear within minutes of having a small amount of milk include:
- raised red bumps of skin – hives (urticaria)
- itchy, red, weeping or crusty rash of the skin – dermatitis or eczema
- swelling of the face
- wheeze or persistent cough
- vomiting
- diarrhoea.
If your child is prone to a severe allergic reaction to milk, these symptoms can also appear very rapidly.
Symptoms that can appear within hours include:
- vomiting
- diarrhoea
- rashes or eczema.
Symptoms that can appear within days include:
- eczema
- diarrhoea
- asthma.

Severe allergic reaction – anaphylaxis
Cow’s milk is one of the most common foods to cause severe allergic reactions. Severe allergic reaction (anaphylaxis) is life threatening.
Symptoms of a severe allergic reaction include:
- difficult or noisy breathing
- swelling of the tongue
- swelling or tightness of the throat
- difficulty talking or hoarse voice
- wheeze or persistent cough
- persistent dizziness or collapse
- paleness and floppiness in young children
If you, or someone your care, have a severe allergic reaction (anaphylaxis), call triple zero (000) for an ambulance.
- Do not stand or walk.
- Administer adrenaline (epinephrine) via injector (EpiPen® or Anapen®), if available.
- Further adrenaline may be given if there is no response after 5 minutes.
- Give adrenaline first, then asthma reliever puffer, if required.
Keep a record of your symptoms
Keep a diary that describes your symptoms or your child’s symptoms and when and where they occur.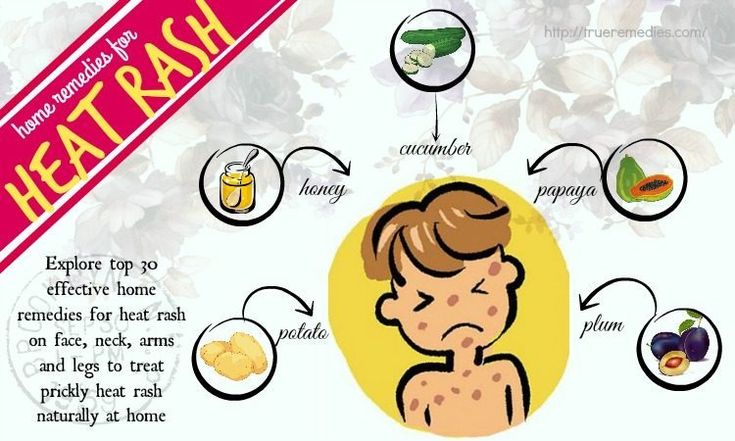 Your diary could include information about whether the symptoms occur:
Your diary could include information about whether the symptoms occur:
- inside your home, outside or both
- for a short time or longer
- at night, during the day or when you wake up
- after you have had a particular food or drink
- after you have taken a particular medication, either prescription or over the counter from a pharmacy or supermarket
- after you have taken a herbal medicine.
Diagnosis of cow’s milk allergy
If you or your child have allergic symptoms, visit your family doctor who will ask some questions about your reactions. You can also discuss your record of your symptoms. To diagnose your allergy, your doctor may refer you to a clinical immunology/allergy specialist.
If your symptoms appear rapidly after eating or drinking milk or dairy products, the allergy may be easier to diagnose, whereas symptoms that take longer to appear make diagnosis more difficult.
Allergists can test for allergies using a number of methods depending on the type of potential allergy.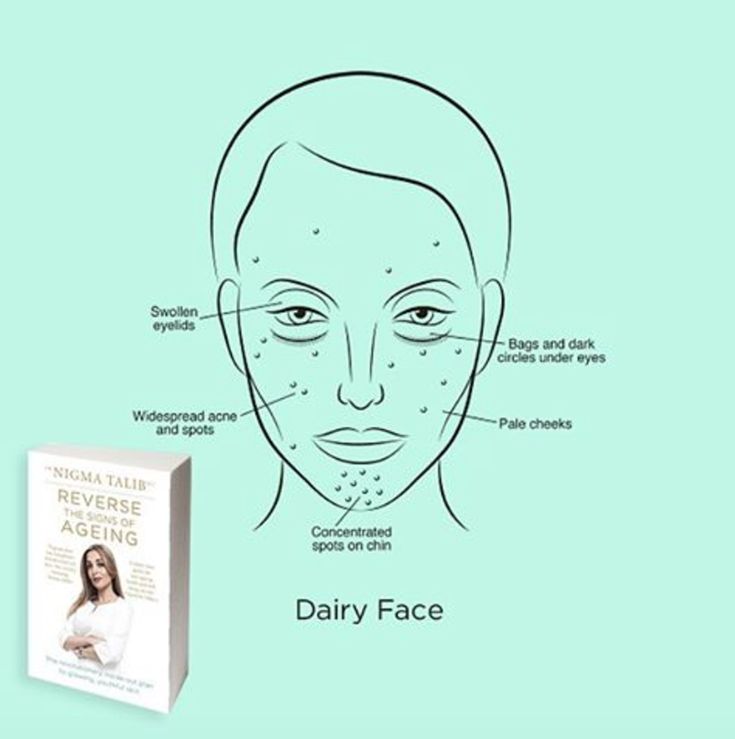 To test for an allergy, the allergist may:
To test for an allergy, the allergist may:
- do a skin prick test
- do a blood test
- ask you to temporarily avoid all milk or products containing milk (elimination diet), then follow up with the introduction of milk back into your diet (food challenge) under strict medical supervision.
A number of methods claim to test for allergies but have not been medically or scientifically proven. They can be costly and could lead to dangerous avoidance of certain foods. The Australasian Society of Clinical Immunology and Allergy (ASCIA) recommends that you do not use certain methods to have potential allergies tested, including:
- cytotoxic food testing
- electrodermal testing
- hair analysis
- iridology
- kinesiology
- pulse testing
- reflexology
- Vega testing.
Always speak with your doctor if you are thinking of using a complementary medicine or therapy for allergies.
Treatment for cow’s milk allergy
If you or your child have been diagnosed with milk allergy, treatment involves total avoidance of milk or products containing milk.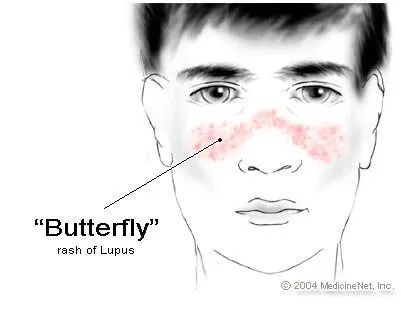 This can be difficult to achieve.
This can be difficult to achieve.
The Australasian Society of Clinical Immunology and Allergy (ASCIA) advises that children who are allergic to cow’s milk are often allergic to goat’s milk, and so substitution with a milk of animal origin may not be possible.
To avoid milk and milk products, read food labels and avoid foods that contain milk or milk products such as:
- butter
- buttermilk
- casein and caseinate
- cheese
- chocolate
- cow's or goat's milk – including ‘A2 milk’
- cream
- crème fraiche
- ghee
- ice cream
- margarines that contain milk products
- milk powder
- nougat
- whey
- yoghurt.
ASCIA has more information about dietary avoidance of cow’s milk for food allergy.
Eliminate milk and milk products from your baby or young child’s diet only under strict medical supervision. Your doctor will need to advise on replacement sources of calcium and protein, which are especially important nutrients for children.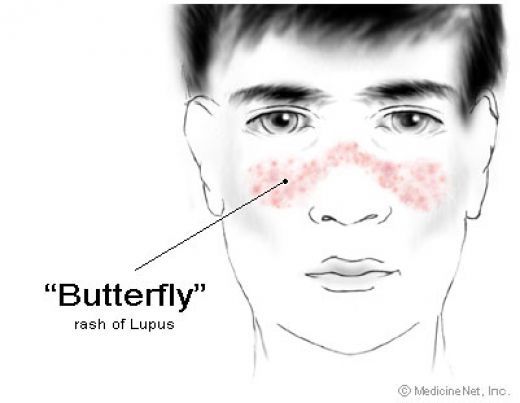 Replacement formulas for babies also needs to be carefully supervised. For example, some children with cow’s milk allergy will not be able to tolerate soy milk products.
Replacement formulas for babies also needs to be carefully supervised. For example, some children with cow’s milk allergy will not be able to tolerate soy milk products.
Emergency treatment for severe allergic reactions (anaphylaxis)
If you are at risk of a severe allergic reaction (anaphylaxis), carry an adrenaline injector such as an EpiPen® or Anapen®, an Australasian Society of Clinical Immunology and Allergy (ASCIA) Action Plan for Anaphylaxis and a means of calling for medical assistance, such as a mobile telephone.
Emergency responses for a severe allergic reaction are:
- Lay the person flat – do not allow them to stand or walk.
- Administer adrenaline with an injector into the outer mid-thigh.
- Always dial triple zero (000) to call an ambulance in a medical emergency.
- Further doses of adrenaline may be given if there is no response after 5 minutes.
- Give adrenaline first, then asthma reliever puffer, if required.
If you are at risk of a severe allergic reaction (anaphylaxis) make sure you:
- Have an ASCIA Action Plan for Anaphylaxis.
- Carry an adrenaline injector (such as an EpiPen® or Anapen®) to treat a severe allergic reaction.
- Consider wearing medical identification jewellery – this increases the likelihood that adrenaline will be administered in an emergency.
- Avoid medication (where possible) that may increase the severity of allergic reaction or complicate its treatment such as beta blockers.
- Avoid the food which causes your allergic reaction.
- Tell food staff about your allergy when eating out.
- Seek medical advice from a doctor or clinical immunology/allergy specialist.
Adrenaline injectors are also available over the counter from a pharmacy.
Where to get help
- In an emergency, always call triple zero (000)
- Emergency department of your nearest hospital
- Your GP (doctor)
- NURSE-ON-CALL Tel.
 1300 60 60 24 – for health information and advice (24 hours, 7 days)
1300 60 60 24 – for health information and advice (24 hours, 7 days) - St John Ambulance Australia Tel. 1300 360 455
- Australasian Society of Clinical Immunology and Allergy (ASICA)
- Cow’s milk allergy
- Locate a specialist
- Allergy and Anaphylaxis Australia
Rashes in infants | Rassvet Clinic
Babies are generous with various rashes. According to the "good" tradition, most of them are considered allergic with all the consequences - a strict diet for a nursing mother, transfer to artificial feeding, prescription of therapeutic mixtures, etc. In fact, true allergic rashes in infants are not so common. Allergic diseases affecting the skin in infants include: atopic dermatitis, acute urticaria and angioedema. Acute urticaria is extremely rare in infants - this is an acute allergic reaction in the form of peculiar rashes like blisters (as with a nettle burn, hence the name), which suddenly appear on the skin and just as suddenly disappear without leaving any trace, usually do not exist on the skin for longer than a day and are accompanied by severe itching, which manifests itself in the general anxiety of the child. The most common causes are dietary proteins (such as cow's milk), viral infections, insect bites, and drugs (such as antibiotics). In severe cases, it may be accompanied by swelling and redness of the soft tissues of the face, neck, larynx, arms, legs, genitals or abdominal cavity - Quincke's edema, which requires immediate medical attention.
The most common causes are dietary proteins (such as cow's milk), viral infections, insect bites, and drugs (such as antibiotics). In severe cases, it may be accompanied by swelling and redness of the soft tissues of the face, neck, larynx, arms, legs, genitals or abdominal cavity - Quincke's edema, which requires immediate medical attention.
Let's look at what is most often undeservedly called an allergy:
Toxic erythema newborns - a transient benign rash, the exact cause of the appearance is unknown (possibly due to skin irritation by environmental factors).
Appears at birth or in the first 24-48 hours of life. Localization - face, trunk, limbs, except for the palms and soles. Disappears on its own within 5-7 days, sometimes 3 weeks. Does not require treatment.
Neonatal acne (acne infancy, neonatal pustulosis) is caused by androgen stimulation of the baby's sebaceous glands.
Peak rash falls on the 3rd week of life. It is localized more often on the face, sometimes spreads to the scalp, less often to the collar zone. They resolve spontaneously. The skin needs cleansing and moisturizing, in some cases, the application of
It is localized more often on the face, sometimes spreads to the scalp, less often to the collar zone. They resolve spontaneously. The skin needs cleansing and moisturizing, in some cases, the application of
treatment creams may be required.
Sweating rash , which occurs in poorly "ventilated" areas as a result of blockage of the sweat glands. May occur at any age.
Localization - skin folds, buttocks and back surface of the body, sometimes the face (after sleep). Depending on the depth of the lesion, it happens - crystal prickly heat, prickly heat, deep prickly heat (superficial).
The duration of the rash is from several hours to several days.
Treatment - cool water baths, air baths, prevention of overheating. Lotions containing calamine and creams with corticosteroids and antibiotics may be used to treat some cases of red and deep prickly heat.
Seborrheic dermatitis is a skin disorder that develops in areas rich in sebum. The exact cause is unknown (a certain role is assigned to the skin saprophyte - the Malassezia fungus, which grows well and multiplies in the sebaceous secretion).
The exact cause is unknown (a certain role is assigned to the skin saprophyte - the Malassezia fungus, which grows well and multiplies in the sebaceous secretion).
It can be foci or widespread, dermatitis with bran-like scales, which can form a crust (“bonnet”, gneiss) on the scalp.
Favorite localization - scalp, face, folds (!).
May begin at 1-2 weeks of age or later, resolve spontaneously within weeks or months.
Treatment consists of softening the crusts with oil or cream and then removing them, moisturizing the skin and, in some cases, applying antifungal and anti-inflammatory creams.
Simple contact dermatitis is a non-specific skin injury due to prolonged or repeated exposure to a variety of substances - saliva, fruit juices, foaming bath products, detergents (their residues on the walls of the bath), etc. In infants, saliva is often causes dermatitis in the area of contact with the nipple and in the folds of the neck.
Usually, removal of the damaging agent and short-term use of anti-inflammatory creams will quickly lead to recovery, but some children are so sensitive that it is almost impossible to identify the causative factor.
Diaper dermatitis (contact dermatitis prototype) is a skin lesion that occurs under the influence of physical (overheating), chemical, enzymatic (contact with sweat, urine and feces) and microbial factors. Localization - the area of the diaper or diaper fit.
Treatment is carried out using the abbreviation ABCDE (air, barrier, cleansing, diaper, education) - air, barrier, cleansing, diaper and parent education. Frequent diaper changes, washing the skin and drying it thoroughly help. Dermatitis is effectively prevented by the application to clean skin of products that completely cover it (Vaseline, zinc paste). In stubborn cases, medicated creams containing corticosteroids, antibiotics, or antifungals may be recommended.
And now a few words about AD:
Atopic dermatitis is a chronic allergic inflammation of the skin, genetically determined, associated with the loss of the skin barrier and, therefore, accompanied by dryness, itching and various rashes. In a third (!) of cases, it is combined with food allergies (the most common "culprits" are cow's milk, chicken eggs, wheat, fish, soy, nuts).
Starts more often not earlier than 3 months of life.
The most common localization up to 2-3 years is the face (cheeks, forehead, chin), convex parts of the limbs (extensor surfaces) and trunk, never in babies in folds (!).
Exacerbations are provoked by various factors - stress, dry air, sweat, food (histamine liberators), infections, contact with tobacco smoke, animal hair, rough fabrics, detergent residues on clothes, etc.
Treated with careful skin care and using anti-inflammatory creams.
There are also:
Pseudo-allergic reactions are reactions that look similar to allergic reactions (for example, various rashes), but are not such, due to the non-immune mechanism of their development.
The reason is an increased content of histamine (tyramine, serotonin) in foods, or the ability of foods to increase the release of these substances in the body, or their increased absorption, due to the pathology of the gastrointestinal tract (fermentopathy, inflammation in the intestinal wall, etc.). ). Such products include chocolate, cocoa, strawberries, citrus fruits, honey, sauerkraut, marinades and spices, seafood, fish, caviar, pork, mushrooms, cheeses, nuts, smoked meats, preservatives, dyes and flavor enhancers.
Treatment includes dietary advice, skin care, and in some cases, antihistamines and anti-inflammatory creams.
Clinical manifestations of atopic dermatitis, simple contact dermatitis in highly sensitive children and the manifestation of pseudo-allergic reactions are very similar to each other, so the main task remains to create a "skin barrier" by constantly moisturizing the skin with the help of emollients, stopping exacerbation with anti-inflammatory creams and eliminating exacerbation-provoking factors .
And the last:
Skin infections - herpesvirus, staphylococcal pemphigus, candidiasis also occurs in infants, do not forget about them. It is worth contacting a doctor immediately if the child is lethargic, has a fever, refuses to breast or bottle, skin rashes are accompanied by pus or are covered with purulent crusts, there are blisters or a group of bubbles, erosion (violation of the integrity of the skin), severe swelling and redness of the skin.
Author:
Eroshkina Maria Sergeevna
pediatrician
Causes of a rash in children
Naturally, only a pediatrician, dermatologist or allergist can correctly determine the cause of rash , diagnose and prescribe treatment for a child. But parents themselves can provide initial assistance, relieve itching and help the baby, knowing the main signs and causes of the rash . At the first stage, it is important to determine the nature of the rash - infectious , allergic or none of the above.
Causes of rashes in children:
1. Newborn acne . For the first time may occur in newborns at the age of 1 - 2 months. As a rule, such rashes are hormonal in nature, are not contagious and are not allergies . A rash in the form of pimples, sometimes with a white dot in the middle, appears on the head, body of the baby. If there are no purulent compartments, then the rash goes away on its own and does not require treatment. Acne can also occur in teenagers. They most often appear on the face as black dots and are associated with hormonal changes in the body of a teenager and increased work of the sebaceous glands. To prevent acne, there are cosmetic lotions, washing gels and other products. In case of inflammation, it is better to seek advice from a pediatric dermatologist or cosmetologist, because. antibiotic treatment may be needed;
2. Urticaria is an allergic reaction on the skin of a child, accompanied by itching and blisters on various parts of the body, in some cases fever and disturbed chair child.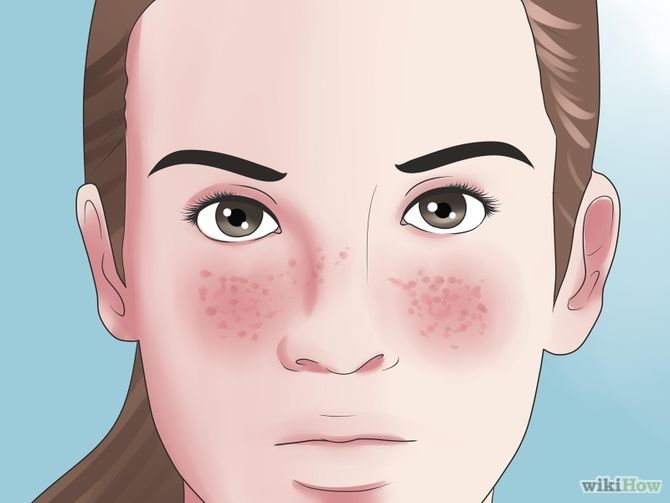 The blisters appear suddenly and can disappear just as quickly, but sometimes they disappear only after a few days. The causes of urticaria can be various factors: hormonal disorders, malfunctions of the liver, kidneys, consumption of foods that caused an allergic reaction (fish, eggs, citrus fruits, etc.), insect bites, reaction to sunlight, temperature changes, emotional stress etc. Urticaria can be chronic and not go away for a long time, and acute - disappearing after a few hours. For the treatment of urticaria, it is important to identify the underlying cause that caused it;
The blisters appear suddenly and can disappear just as quickly, but sometimes they disappear only after a few days. The causes of urticaria can be various factors: hormonal disorders, malfunctions of the liver, kidneys, consumption of foods that caused an allergic reaction (fish, eggs, citrus fruits, etc.), insect bites, reaction to sunlight, temperature changes, emotional stress etc. Urticaria can be chronic and not go away for a long time, and acute - disappearing after a few hours. For the treatment of urticaria, it is important to identify the underlying cause that caused it;
3. Food allergy manifests itself as spots pinkish red. It is slightly convex, edematous in places of scratching and is accompanied by itching. It is localized, as a rule, on the baby's cheeks, but can also appear on other parts of the body. It can occur in both infants and adolescents. If the baby is breastfed, then the allergy that has arisen is associated with the products consumed by the mother. If the newborn is artificially fed, then an allergic reaction may appear on the mixture. In older children, food allergies can be caused by fish, eggs, nuts, chocolate, strawberries, and other foods;
If the newborn is artificially fed, then an allergic reaction may appear on the mixture. In older children, food allergies can be caused by fish, eggs, nuts, chocolate, strawberries, and other foods;
Allergy, as a rule, is accompanied by edema, which, in turn, in case of improper treatment and untimely assistance, cause suffocation . If an allergy of any nature occurs, a pediatrician's consultation is required to help in choosing the optimal mixture for the baby, or a pediatric dermatologist - allergist to refer older children to laboratory tests ;
4. Household allergies . It can occur in both newborns and older children. It usually appears as pimples all over the body and is accompanied by lachrymation, sneezing. The causes of such a reaction of the body can be washing powder and other detergents, dust, plants, animal hair, etc. An allergic rash differs from an infectious rash in that the child does not have a temperature with it, he does not have general ailments, there is no loss of appetite, drowsiness;
5. Prickly heat . It occurs mainly in infants. It manifests itself in the form of red pimples all over the body, especially in the inguinal zone. The affected areas must be smeared with a special baby cream, air baths more often for the baby and a diaper change;
Prickly heat . It occurs mainly in infants. It manifests itself in the form of red pimples all over the body, especially in the inguinal zone. The affected areas must be smeared with a special baby cream, air baths more often for the baby and a diaper change;
6. Roseola (erythema infectiosum) is an acute childhood viral disease affecting only children under 2 years of age. Very often, roseola is confused with SARS or rubella . At the beginning of the illness, the baby's temperature rises sharply, which lasts 3-5 days, and after that the child becomes covered with a red-pink rash that disappears in 5-7 days. This is not a dangerous disease, it does not require treatment, and if it occurs, the child should be given only antipyretic drugs;
7. Windmill . This is a common childhood infectious disease that requires treatment. The incubation period of this disease can last from 11 to 21 days. Occurs at any age. It is accompanied by a rash on the skin and mucous membranes in the form of red spots, in the center of which blisters with a yellowish liquid are localized. Accompanied by itching. As the disease progresses, the blisters burst, crusts form, leaving scars if the child has scratched the blister and brought the infection. The disease can also cause fever and headache;
It is accompanied by a rash on the skin and mucous membranes in the form of red spots, in the center of which blisters with a yellowish liquid are localized. Accompanied by itching. As the disease progresses, the blisters burst, crusts form, leaving scars if the child has scratched the blister and brought the infection. The disease can also cause fever and headache;
8. Measles is an acute infectious disease that is quite rare due to the use of vaccinations. In addition, this virus is rarely activated in babies under 8 months old, because. they are protected by their mother's immunity. The disease begins with symptoms of a common cold - coughing, lacrimation, sneezing and fever up to 40 C. Then the child develops white spots on the mucous surface of the cheeks, nasal discharge, severe headache, photophobia. Then, within a few days, red spots of various shapes appear on the face, neck, near the head and further throughout the body. The disease is contagious within a week of the onset of the first symptoms. The virus is dangerous with complications such as: meningitis pneumonia development of deafness, brain damage and even death;
The virus is dangerous with complications such as: meningitis pneumonia development of deafness, brain damage and even death;
9. Scarlet fever is an acute infectious streptococcal disease. Begins with sore throat, high fever, enlarged tonsils , in some cases with plaque. Then a small dotted rash appears on the back, chest, knees, armpits, groin and quickly spreads throughout the body and face. Only the area around the mouth remains white. Throat and tongue become very red. By the end of the disease, peeling of the skin on the toes and hands begins;
10. Rubella is an acute infectious disease . The disease begins with a slight increase in temperature and swollen lymph nodes in the parotid and cervical region. A small rash also appears on the face and behind the ears, and then all over the body. Rubella is very dangerous for pregnant women, and complications can occur in older children and adolescents. In children, the disease proceeds in a fairly mild form;
In children, the disease proceeds in a fairly mild form;
11. Meningitis is an inflammation of the membranes of the brain and spinal cord. Rash in meningitis is not the main symptom. However, with this disease, rashes appear on the back of the throat, as well as on the hips, back, buttocks in the form of a red rash of various shapes. Symptoms of meningitis include very high fever, severe headache, vomiting, photophobia, and neck muscle tension. At the slightest suspicion of meningitis, parents should immediately consult a doctor. Timely help with this disease will save the child's life;
12. Streptoderma is a skin infection caused by Staphylococcus aureus. The disease affects, as a rule, the paranasal and perioral region. In the beginning, redness appears around the nose and mouth, then small bubbles with liquid. When they burst, yellow crusts remain. The disease may be accompanied by fever;
13. Herpes is an infectious disease accompanied by the appearance of blisters on the skin and mucous membranes, in children it is most often located on the lips. This disease is extremely rare in newborns, because. they are given maternal immunity. It affects children from 3 to 4 years of age. In addition to a rash, the disease may be accompanied by a sore throat, fever.
This disease is extremely rare in newborns, because. they are given maternal immunity. It affects children from 3 to 4 years of age. In addition to a rash, the disease may be accompanied by a sore throat, fever.
There are a lot of skin rashes and diseases in children, they can be very similar, but some are completely harmless to your child's health, while others pose a threat not only to the general condition, but also to the child's life! Do not take risks, and if you have any doubts, if any spots, rashes and other symptoms appear, contact your pediatrician, who, if necessary, will refer you and your child to a pediatric dermatologist, allergist, neurologist or other highly specialized specialist, depending on the nature of the rash and the severity of the skin disease.
Our clinics in St. Petersburg
Structural subdivision
Polikarpova
Alley Polikarpova 6k2
Primorsky district
- Pioneer
- Specific
- Komendantskiy
Structural subdivision
Zhukov
Marshal Zhukov Ave.