Fused skull baby
Facts about Craniosynostosis | CDC
Craniosynostosis is a birth defect in which the bones in a baby’s skull join together too early. This happens before the baby’s brain is fully formed. As the baby’s brain grows, the skull can become more misshapen.
Click here to view a larger image
Click here to view a larger image
What is Craniosynostosis?
Craniosynostosis is a birth defect in which the bones in a baby’s skull join together too early. This happens before the baby’s brain is fully formed. As the baby’s brain grows, the skull can become more misshapen. The spaces between a typical baby’s skull bones are filled with flexible material and called sutures. These sutures allow the skull to grow as the baby’s brain grows. Around two years of age, a child’s skull bones begin to join together because the sutures become bone. When this occurs, the suture is said to “close.” In a baby with craniosynostosis, one or more of the sutures closes too early. This can limit or slow the growth of the baby’s brain.
When a suture closes and the skull bones join together too soon, the baby’s head will stop growing in only that part of the skull. In the other parts of the skull where the sutures have not joined together, the baby’s head will continue to grow. When that happens, the skull will have an abnormal shape, although the brain inside the skull has grown to its usual size. Sometimes, though, more than one suture closes too early. In these instances, the brain might not have enough room to grow to its usual size. This can lead to a build-up of pressure inside the skull.
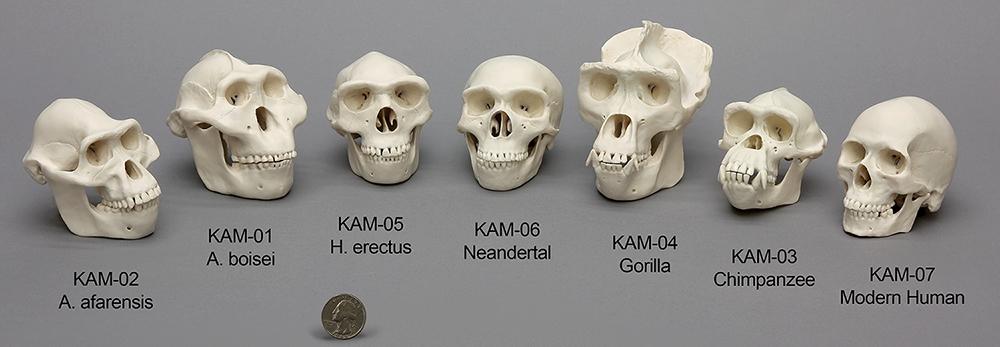
Types of Craniosynostosis
The types of craniosynostosis depend on what sutures join together early.
- Sagittal synostosis– The sagittal suture runs along the top of the head, from the baby’s soft spot near the front of the head to the back of the head. When this suture closes too early, the baby’s head will grow long and narrow (scaphocephaly).
 It is the most common type of craniosynostosis.
It is the most common type of craniosynostosis. - Coronal synostosis – The right and left coronal sutures run from each ear to the sagittal suture at the top of the head. When one of these sutures closes too early, the baby may have a flattened forehead on the side of the skull that closed early (anterior plagiocephaly). The baby’s eye socket on that side might also be raised up and his or her nose could be pulled toward that side. This is the second most common type of craniosynostosis.
- Bicoronal synostosis – This type of craniosynostosis occurs when the coronal sutures on both sides of the baby’s head close too early. In this case, the baby’s head will grow broad and short (brachycephaly).
- Lambdoid synostosis – The lambdoid suture runs along the backside of the head. If this suture closes too early, the baby’s head may be flattened on the back side (posterior plagiocephaly). This is one of the rarest types of craniosynostosis.

- Metopic synostosis – The metopic suture runs from the baby’s nose to the sagittal suture at the top of the head. If this suture closes too early, the top of the baby’s head shape may look triangular, meaning narrow in the front and broad in the back (trigonocephaly). This is one of the rarest types of craniosynostosis.
Other Problems
Many of the problems a baby can have depend on:
- Which sutures closed early
- When the sutures closed (was it before or after birth and at what age)
- Whether or not the brain has room to grow
Sometimes, if the condition is not treated, the build-up of pressure in the baby’s skull can lead to problems, such as blindness, seizures, or brain damage.
How Many Babies are Born with Craniosynostosis?
Researchers estimate that about 1 in every 2,500 babies is born with craniosynostosis in the United States.1
Causes and Risk Factors
The causes of craniosynostosis in most infants are unknown. Some babies have a craniosynostosis because of changes in their genes. In some cases, craniosynostosis occurs because of an abnormality in a single gene, which can cause a genetic syndrome. However, in most cases, craniosynostosis is thought to be caused by a combination of genes and other factors, such as things the mother comes in contact with in her environment, or what the mother eats or drinks, or certain medications she uses during pregnancy.
Some babies have a craniosynostosis because of changes in their genes. In some cases, craniosynostosis occurs because of an abnormality in a single gene, which can cause a genetic syndrome. However, in most cases, craniosynostosis is thought to be caused by a combination of genes and other factors, such as things the mother comes in contact with in her environment, or what the mother eats or drinks, or certain medications she uses during pregnancy.
CDC, like the many families of children with birth defects, wants to find out what causes these conditions. Understanding the factors that are more common among babies with a birth defect will help us learn more about the causes. CDC funds the Centers for Birth Defects Research and Prevention, which collaborate on large studies such as the National Birth Defects Prevention Study (NBDPS; births 1997-2011), to understand the causes of and risks for birth defects, such as craniosynostosis.
Recently, CDC reported on important findings from research studies about some factors that increase the chance of having a baby with craniosynostosis:
- Maternal thyroid disease ― Women with thyroid disease or who are treated for thyroid disease while they are pregnant have a higher chance of having an infant with craniosynostosis, compared to women who don’t have thyroid disease.
 2
2 - Certain medications ― Women who report using clomiphene citrate (a fertility medication) just before or early in pregnancy are more likely to have a baby with craniosynostosis, compared to women who didn’t take this medicine.3
CDC continues to study birth defects, such as craniosynostosis, and how to prevent them. If you are pregnant or thinking about becoming pregnant, talk with your doctor about ways to increase your chances of having a healthy baby.
Diagnosis
Craniosynostosis usually is diagnosed soon after a baby is born. Sometimes, it is diagnosed later in life.
Usually, the first sign of craniosynostosis is an abnormally shaped skull. Other signs may include:
- No “soft spot” on the baby’s skull
- A raised firm edge where the sutures closed early
- Slow growth or no growth in the baby’s head size over time
Doctors can identify craniosynostosis during a physical exam. A doctor will feel the baby’s head for hard edges along the sutures and unusual soft spots. The doctor also will look for any problems with the shape of the baby’s face. If he or she suspects the baby might have craniosynostosis, the doctor usually requests one or more tests to help confirm the diagnosis. For example, a special x-ray test, such as a CT or CAT scan, can show the details of the skull and brain, whether certain sutures are closed, and how the brain is growing.
The doctor also will look for any problems with the shape of the baby’s face. If he or she suspects the baby might have craniosynostosis, the doctor usually requests one or more tests to help confirm the diagnosis. For example, a special x-ray test, such as a CT or CAT scan, can show the details of the skull and brain, whether certain sutures are closed, and how the brain is growing.
Treatments
Many types of craniosynostosis require surgery. The surgical procedure is meant to relieve pressure on the brain, correct the craniosynostosis, and allow the brain to grow properly. When needed, a surgical procedure is usually performed during the first year of life. But, the timing of surgery depends on which sutures are closed and whether the baby has one of the genetic syndromes that can cause craniosynostosis.
Babies with very mild craniosynostosis might not need surgery. As the baby gets older and grows hair, the shape of the skull can become less noticeable. Sometimes, special medical helmets can be used to help mold the baby’s skull into a more regular shape.
Each baby born with craniosynostosis is different, and the condition can range from mild to severe. Most babies with craniosynostosis are otherwise healthy. Some children, however, have developmental delays or intellectual disabilities, because either the craniosynostosis has kept the baby’s brain from growing and working normally, or because the baby has a genetic syndrome that caused both craniosynostosis and problems with how the brain works. A baby with craniosynostosis will need to see a healthcare provider regularly to make sure that the brain and skull are developing properly. Babies with craniosynostosis can often benefit from early intervention services to help with any developmental delays or intellectual problems. Some children with craniosynostosis may have issues with self-esteem if they are concerned with visible differences between themselves and other children. Parent-to-parent support groups also can be useful for new families of babies with birth defects of the head and face, including craniosynostosis.
Other Resources
The views of these organizations are their own and do not reflect the official position of CDC.
- Children’s Craniofacial Association (CCA)
CCA addresses the medical, financial, psychosocial, emotional, and educational concerns relating to craniofacial conditions. - The National Craniofacial Association (FACES)
FACES is dedicated to assisting children and adults who have craniofacial disorders resulting from disease, accident, or birth.
References
- Boulet SL, Rasmussen SA, Honein MA. A population-based study of craniosynostosis in metropolitan Atlanta, 1989-2003. Am J Med Genet Part A. 2008;146A:984–991.
- Rasmussen SA, Yazdy MM, Carmichael SL, Jamieson DJ, Canfield MA, Honein MA. Maternal thyroid disease as a risk factor for craniosynostosis. Obstet Gynecol. 2007;110:369-377.
- Reefhuis J, Honein MA, Schieve LA, Rasmussen SA, and the National Birth Defects Prevention Study. Use of clomiphene citrate and birth defects, National Birth Defects Prevention Study, 1997–2005.
 Hum Reprod. 2011;26:451–457.
Hum Reprod. 2011;26:451–457.
The images are in the public domain and thus free of any copyright restrictions. As a matter of courtesy we request that the content provider (Centers for Disease Control and Prevention, National Center on Birth Defects and Developmental Disabilities) be credited and notified in any public or private usage of this image.
The images are in the public domain and thus free of any copyright restrictions. As a matter of courtesy we request that the content provider (Centers for Disease Control and Prevention, National Center on Birth Defects and Developmental Disabilities) be credited and notified in any public or private usage of this image.
Craniosynostosis - Symptoms and causes
Overview
Cranial sutures and fontanels
Cranial sutures and fontanels
Joints made of strong, fibrous tissue (cranial sutures) hold the bones of your baby's skull together. The sutures meet at the fontanels, the soft spots on your baby's head. The sutures remain flexible during infancy, allowing the skull to expand as the brain grows. The largest fontanel is at the front (anterior).
The sutures remain flexible during infancy, allowing the skull to expand as the brain grows. The largest fontanel is at the front (anterior).
Children's Center
At Mayo Clinic, medical and surgical specialists from over 70 areas are available to discuss and develop a personal treatment plan for your child.
- Children's CenterChildren's Center
Craniosynostosis (kray-nee-o-sin-os-TOE-sis) is a disorder present at birth in which one or more of the fibrous joints between the bones of your baby's skull (cranial sutures) close prematurely (fuse), before your baby's brain is fully formed. Brain growth continues, giving the head a misshapen appearance.
Usually, during infancy the sutures remain flexible, allowing a baby's skull to expand as the brain grows. In the front of the skull, the sutures meet in the large soft spot (fontanel) on top of the head. The anterior fontanel is the soft spot felt just behind a baby's forehead. The next largest fontanel is at the back (posterior).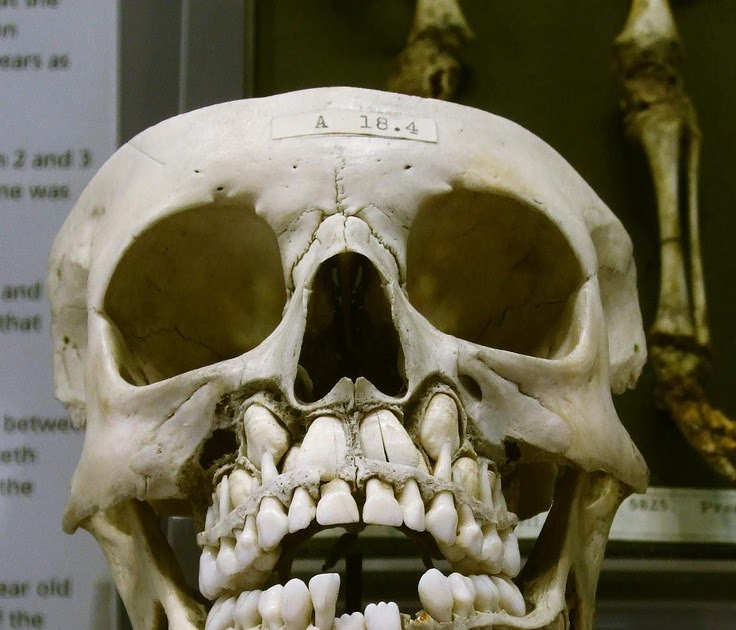 Each side of the skull has a tiny fontanel.
Each side of the skull has a tiny fontanel.
Craniosynostosis usually involves premature fusion of a single cranial suture, but it can involve more than one of the sutures in a baby's skull (multiple suture craniosynostosis). In rare cases, craniosynostosis is caused by certain genetic syndromes (syndromic craniosynostosis).
Treating craniosynostosis involves surgery to correct the shape of the head and allow for brain growth. Early diagnosis and treatment allow your baby's brain adequate space to grow and develop.
Although neurological damage can occur in severe cases, most children develop as expected in their ability to think and reason (cognitive development) and have good cosmetic results after surgery. Early diagnosis and treatment are key.
Products & Services
- Book: Mayo Clinic Family Health Book, 5th Edition
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Symptoms
The signs of craniosynostosis are usually noticeable at birth, but they become more apparent during the first few months of your baby's life. Signs and severity depend on how many sutures are fused and when in brain development the fusion occurs. Signs and symptoms can include:
Signs and severity depend on how many sutures are fused and when in brain development the fusion occurs. Signs and symptoms can include:
- A misshapen skull, with the shape depending on which of the sutures are affected
- Development of a raised, hard ridge along affected sutures, with a change in the shape of the head that's not typical
Types of craniosynostosis
There are several types of craniosynostosis. Most involve the fusion of a single cranial suture. Some complex forms of craniosynostosis involve the fusion of multiple sutures. Multiple suture craniosynostosis is usually linked to genetic syndromes and is called syndromic craniosynostosis.
The term given to each type of craniosynostosis depends on what sutures are affected. Types of craniosynostosis include:
- Sagittal (scaphocephaly). Premature fusion of the sagittal suture that runs from the front to the back at the top of the skull forces the head to grow long and narrow.
 This head shape is called scaphocephaly. Sagittal craniosynostosis is the most common type of craniosynostosis.
This head shape is called scaphocephaly. Sagittal craniosynostosis is the most common type of craniosynostosis. - Coronal. Premature fusion of one of the coronal sutures (unicoronal) that run from each ear to the top of the skull may cause the forehead to flatten on the affected side and bulge on the unaffected side. It also leads to turning of the nose and a raised eye socket on the affected side. When both coronal sutures fuse prematurely (bicoronal), the head has a short and wide appearance, often with the forehead tilted forward.
- Metopic. The metopic suture runs from the top of the bridge of the nose up through the midline of the forehead to the anterior fontanel and the sagittal suture. Premature fusion gives the forehead a triangular appearance and widens the back part of the head. This head shape is also called trigonocephaly.
- Lambdoid. Lambdoid synostosis is a rare type of craniosynostosis that involves the lambdoid suture, which runs along the back of the head.
 It may cause one side of a baby's head to appear flat, one ear to be higher than the other ear and tilting of the top of the head to one side.
It may cause one side of a baby's head to appear flat, one ear to be higher than the other ear and tilting of the top of the head to one side.
Other reasons for a misshapen head
A misshapen head doesn't always indicate craniosynostosis. For example, if the back of your baby's head appears flattened, it could be the result of spending too much time lying on one side of the head. This can be treated with regular position changes, or if significant, with helmet therapy (cranial orthosis) to help reshape the head to a more balanced appearance.
When to see a doctor
Your health care provider will routinely monitor your child's head growth at well-child visits. Talk to your pediatrician if you have concerns about your baby's head growth or shape.
Request an Appointment at Mayo Clinic
Causes
Often the cause of craniosynostosis is not known, but sometimes it's related to genetic disorders.
- Nonsyndromic craniosynostosis is the most common type of craniosynostosis.
 Its cause is unknown, although it's thought to be a combination of genes and environmental factors.
Its cause is unknown, although it's thought to be a combination of genes and environmental factors. - Syndromic craniosynostosis is caused by certain genetic syndromes, such as Apert syndrome, Pfeiffer syndrome or Crouzon syndrome, which can affect a baby's skull development. These syndromes usually also include other physical features and health problems.
Complications
If untreated, craniosynostosis may cause, for example:
- Permanently misshapen head and face
- Poor self-esteem and social isolation
The risk of increased pressure inside the skull (intracranial pressure) from simple craniosynostosis is small if the suture and head shape are fixed surgically. But babies with an underlying syndrome may develop increased intracranial pressure if their skulls don't expand enough to make room for their growing brains.
If untreated, increased intracranial pressure can cause:
- Developmental delays
- Cognitive impairment
- Blindness
- Seizures
- Headaches
By Mayo Clinic Staff
Related
Associated Procedures
Products & Services
Plagiocephaly in a child - an irregular shape of the skull in an infant
The disease is cured by:
Children's osteopath
Article content
- Causes of
- Types of plagiocephaly in children
- Signs of disease
- Diagnostics of plagiocephaly in children
Plagiocephaly is an abnormally shaped skull, or flat head syndrome, in infants. Its signs are detected to some extent in every fifth child, and only every tenth of them needs specific treatment. Deformation becomes distinct noticeable by 2 months (sometimes earlier). Treatment started on time is usually effective.
Its signs are detected to some extent in every fifth child, and only every tenth of them needs specific treatment. Deformation becomes distinct noticeable by 2 months (sometimes earlier). Treatment started on time is usually effective.
Causes
- Postpartum - permanent position with emphasis on the bones of the skull (mainly lying on the back) or premature fusion of the sutures of the skull.
- Intrauterine - in most cases caused by the anatomical position during gestation - with twin pregnancy and / or pressing the fetus to the mother's ribs, large fetus or uterine abnormalities, premature prolapse during childbirth.
- Pathological conditions - torticollis, or torticollis - shortening of the neck muscles on one side, other neuromuscular diseases.
Previously, the disease was diagnosed less frequently - due to the fact that pediatricians recommended laying newborns on their side. To date, it has been proven that this position increases the risk of sudden infant death syndrome in a dream, therefore, since 1992, it has been recommended to lay children on their backs during sleep, which becomes a frequent cause of deformation of the skull bones that have not yet been fully formed.
To date, it has been proven that this position increases the risk of sudden infant death syndrome in a dream, therefore, since 1992, it has been recommended to lay children on their backs during sleep, which becomes a frequent cause of deformation of the skull bones that have not yet been fully formed.
Types of plagiocephaly in children
According to etiological types, plagiocephaly is distinguished:
- Positional - acquired, caused by mechanical deformations - intrauterine or perinatal. Occurs in the vast majority of cases. Source:
https://www.ncbi.nlm.nih.gov/pubmed/25382999
Mawji A, Vollman AR, Fung T, Hatfield J, McNeil DA, Sauvé R
Risk factors for positional plagiocephaly and appropriate time frames for prevention messaging
// Pediatric Child Health. 2014 Oct;19(8):423-7 - Deformation - caused by congenital diseases - progressive deformity due to early fusion of the cranial bones.
 It occurs extremely rarely - in 1 out of 2,000 patients. Source:
It occurs extremely rarely - in 1 out of 2,000 patients. Source:
https://www.ncbi.nlm.nih.gov/pubmed/30151193
Renz-Polster H, De Bock
Deformational plagiocephaly: The case for an evolutionary mismatch
// Evol Med Public Health. 2018 Aug 8;2018(1):180-185. doi: 10.1093/emph/eoy019. eCollection 2018
According to localization, it happens:
- frontal;
- occipital;
- side.
Signs of disease
Atypical skull shape - flattened in the occipital region. Rarely - elongated in the frontal direction or squeezed from the sides. Characteristic frontal or temporal bulges, protrusions of the parietal region are possible.
If the asymmetry of the head is caused by congenital anomalies, then without treatment, the pathology progresses. Over time, it can cause negative consequences in the child - increased intracranial pressure and the symptoms caused by it . Source:
Source:
E.V. Mammadov
Plagiocephaly. II. Synostotic, deformation and compensatory
// Children's surgery, 2003, No. 5, p. 45-50
Diagnosis of plagiocephaly in a child
In accordance with modern recommendations, the diagnosis is made on the basis of a clinical examination. For differential diagnosis - identifying the cause of the pathology - ultrasound, radiography or CT of the skull are optionally prescribed.
Methods of treatment
The main treatment for positional plagiocephaly in infants is the repositioning method : multiple changes in body position during the day. The child should lie on his back as little as possible when he is awake. Minimize wearing in a sling and carrier, transport in a car seat. An effective technique is to change the position of the child relative to the light source (stimulates turning over).
Children older than 7 weeks also indicated exercise therapy. It is aimed at:
It is aimed at:
- stimulation of motor development and correction of positional preferences;
- stretching of the neck muscles with torticollis - an increase in the range of motion in the cervical spine.
Includes laying out the child on the stomach during wakefulness under the supervision of adults.
With moderate and severe deformities, as well as with the ineffectiveness of conservative treatment, orthotics are indicated - helmet therapy. The orthosis is made according to individual measurements in an orthopedic workshop. The child wears it 23 hours a day until it heals or needs to change the size of the helmet.
Conservative treatment and orthotics last for several months. The bones of the skull gradually assume a physiological position, while no damage is done to the brain, and neurological diseases do not develop.
If the deformity is due to a congenital anomaly, surgery is indicated. As a rule, it is done at the age of ~7-9 years. The use of orthopedic pillows for newborns is contraindicated, as they sometimes cause infant death.
The use of orthopedic pillows for newborns is contraindicated, as they sometimes cause infant death.
Sources:
- https://www.ncbi.nlm.nih.gov/pubmed/25382999 Mawji A, Vollman AR, Fung T, Hatfield J, McNeil DA, Sauvé R. Risk factors for positional plagiocephaly and appropriate time frames for prevention messaging // Paediatr child health. 2014 Oct;19(8):423-7.
- https://www.ncbi.nlm.nih.gov/pubmed/30151193 Renz-Polster H, De Bock. Deformational plagiocephaly: The case for an evolutionary mismatch // Evol Med Public Health. 2018 Aug 8;2018(1):180-185. doi: 10.1093/emph/eoy019. eCollection 2018.
- E.V. Mammadov. Plagiocephaly. II. Synostotic, deformation and compensatory // Children's surgery, 2003, No. 5, pp. 45-50.
The information in this article is provided for reference only and does not replace the advice of a qualified professional. Do not self-medicate! At the first signs of the disease, you should consult a doctor.
All pediatric osteopaths
- All doctors
- Malaya Balkanskaya, 23
- Udarnikov, 19k1
Make an appointment
Registration through the site is preliminary.
Our employee will contact you to confirm the appointment with a specialist.
Specify time
Time9:009:3010:0010:3011:0011:3012:0012:3013:0013:3014:0014:3015:0015:3016:0016:3017:0017:3018:0018:3019:0019:3020: 0020:3021:0021:30
Specify specialist
Specialist-I don’t know-a pediatrician allergist of the Gastroenter gynecologist of the dermatologist Immunology Cardiology, Logo-Pedious Neurology of the Oncologist of the Orthradeda Orthodox, Pulmonary Dermon, Rheumen Dermon, Rheumen Dermon, Rheumen Dermon, Rheumen Dermon, Rheumen Dermon, Cardiocratic District.
More about the quality assurance of medical services
Deformation of the skull in a child.
 Plagiocephaly. Osteopath in Kyiv
Plagiocephaly. Osteopath in Kyiv During childbirth, the baby's head is deformed, the bones move, and immediately after birth, the baby's skull can be deformed. In the coming days (most often 3-7 days), the skull straightens itself out, without any outside interference. This happens if the seams are loose. It is also important that the brain itself is not damaged. A healthy brain grows and this is what leads to the growth of the skull, and not vice versa. That is, the child's head grows, as the brain grows and develops.
Now about deformities:
⠀ ⠀ Plagiocephaly - a deformed skull - is different in that the brain is not initially damaged, but in one way or another the process of growth and transformation of the bones and sutures of the skull is disrupted, which can subsequently affect the brain. Microcephaly - "small skull" - the skull does not grow as the brain is seriously damaged. The volume of the brain does not increase, and this does not stimulate the growth of the bones of the skull. ⠀
⠀
⠀ With plagiocephaly, it is important to understand the difference between two conditions: craniostenosis is a structural fusion and is subject to surgical treatment, and functional suture blocks are a restriction of mobility / micromotion in the sutures while maintaining their correct structure, and this is what osteopaths work with. In both of these cases, there is a "twisting" of the entire skull around the axis of the affected suture.
⠀⠀When parents come to us with a child and show his asymmetrical, uneven head, it is important for us to differentiate and understand what the nature of this asymmetry is.
Treatment tactics will depend on this understanding and it can radically differ in different cases: in some cases, a course of osteopathic treatment will be the best solution, and sometimes it is impossible to delay and it is worth contacting neurosurgeons for surgical treatment, reconstructive operations. ⠀⠀
⠀⠀If divided by causes of deformity, one can distinguish craniostenosis and functional blocks of sutures (cause - damage to the structure of the skull) and microcephaly (cause - damage to the brain), as well as head deformity due to a condition of the neck (torticollis), or prolonged lying on one side (primary - cervical dysfunction).
⠀⠀ What to do if you notice a skull deformity in a child?
- Assess the range of motion in the neck: does the child turn his head equally in both directions, does he have a “favorite” side, does he sleep more often on one side or with his head turned to one side? ⠀⠀
- Evaluate if the change in the shape of the skull is the only symptom? If there are other symptoms (restless sleep, profuse regurgitation, tone in the limbs and body) - you need to contact a pediatrician or neurologist without postponing this visit.
- If there are no concomitant symptoms, (now about a newborn baby) observe how the deformity behaves over time, during 3-4 weeks of the child's life. ⠀
⠀I would recommend contacting an osteopath as soon as possible, as soon as you notice the deformity. This is due to the fact that the bones and sutures are the most pliable and it can be much easier to correct violations. It is important to say that in some cases (provided that the brain was not damaged, there was no hypoxia and other factors, and also if the suture block is light), the skull can straighten itself out without external influences, including without the help of an osteopath.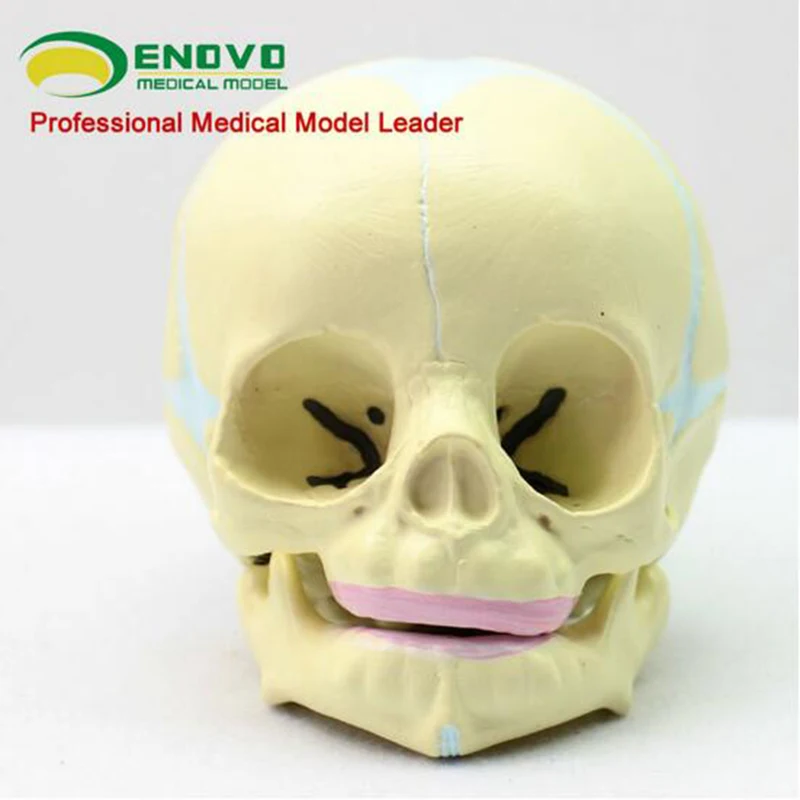 But we cannot predict this in advance. ⠀⠀ ⠀
But we cannot predict this in advance. ⠀⠀ ⠀
⠀ What else is important to do?
If there are no concomitant symptoms and the deformity does not disappear during the observation period (3-4 weeks), but worsens, you should contact a neurosurgeon and, on his recommendation, do a CT scan to exclude craniosynostosis, suture fusion. In cases of craniosynostosis, surgical treatment shows the best results and it is important to carry it out before the child is 1 year old. ⠀⠀
At the same time, the osteopath can also work with the child, but rather as a support, and not as the main specialist (the osteopath can help speed up the recovery process, work with the tension of the meninges, which are always affected during such operations).
⠀⠀⠀⠀⠀⠀⠀⠀⠀⠀ In case of suture fusion, I would recommend contacting an osteopath, and here his work will be very important. This can be a whole course of appointments over several months or 3-4 visits: it all depends on the specific situation, the severity of the suture block, the age of the child, the body's response to treatment, etc.