Failed newborn hearing screen
Newborn Hearing Screening FAQs - HealthyChildren.org
Before you bring your newborn home from the hospital, your baby needs to have a hearing screening.
From birth, one important way babies can learn is through listening and hearing. Although most infants can hear fine, 1 to 3 of every 1,000 babies born in the U.S. have hearing levels outside the typical range.
Newborn screening and diagnosis helps ensure all babies who are deaf or hard of hearing are identified as soon as possible. Then, they can receive early intervention services that can make a big difference in their communication and language development.
The American Academy of Pediatrics (AAP) recommends hearing screenings for all newborns. The goal is for all babies to have a newborn hearing screening by one month of age, ideally before they go home from the hospital; identified by 3 months of age and enrolled in early intervention or treatment, if identified as deaf or hard of hearing, by the age of 6 months. |
Why do newborns need hearing screening?
The hearing screening is a first and important step in helping understand if your baby may be deaf or hard of hearing. Without newborn hearing screening, it is hard to know when there are hearing changes in the first months and years of your baby's life.
Babies may respond to noise by startling or turning their heads toward the sound, for example. But this doesn't necessarily mean they can hear all the sounds around them and everything we say. Babies who are deaf or hard of hearing may hear some sounds but still not hear enough to understand spoken language.
Infants who are deaf or hard of hearing need the right supports, care, and early intervention services to promote healthy development. If the hearing status is not identified, it may have negative effects on the baby's communication and language skills. Longer term, a missed hearing loss can also impact the child's academic achievement and social-emotional development.
How is the newborn hearing screening done?
According to the most recent Centers for Disease Control and Prevention (CDC) data, over 98% of newborns in the United States receive newborn hearing screening.
There are two screening methods that may be used:
-
Automated Auditory Brainstem Response (AABR)—This screen measures how the hearing nerve and brain respond to sound. Clicks or tones are played through soft earphones into the baby's ears. Three electrodes placed on the baby's head measure the hearing nerve and brain's response.
-
Otoacoustic Emissions (OAE)—This screen measures sound waves produced in the inner ear. A tiny probe is placed just inside the baby's ear canal. It measures the response (echo) when clicks or tones are played into the baby's ears.
Both screens are quick (about 5 to 10 minutes), painless, and may be done while your baby is sleeping or lying still. One or both screens may be used.
One or both screens may be used.
What if my baby does not pass the initial hearing screening?
If your baby does not pass the hearing screening at birth, it does not necessarily mean that she is deaf or hard of hearing. Fluid or vernix inside the baby's ear, for example, or too much noise in the room can affect results. In fact, most babies who do not pass the newborn screening have typical hearing. But to be sure, it is extremely important to have further testing done.
About 1 or 2 in every 100 babies will not pass the initial hearing screening at birth and will need tests with an audiologist who has experience working with babies. This testing should include a more thorough hearing and medical evaluation.
Be sure to talk with your baby's pediatrician about scheduling further tests if your baby does not pass the initial hearing screening at birth.
The additional testing should be done as soon as possible, but before your baby is 3 months old.
Follow-up testing may start with one more screening similar to the type done in the hospital. Some hospitals or clinics may complete a diagnostic test at the time of follow-up, instead of re-screening. In young infants, the follow-up testing may be able to be completed while the baby naps.
If my baby is identified as deaf or hard of hearing, what are the treatment and intervention options?
If your baby's audiologist confirms hearing changes, treatment and early intervention with a team of providers should start as soon as possible. Just like hearing children, children who are deaf or hard of hearing can achieve many things. Studies show your baby will have the best chance for spoken language development―on par with that of hearing peers―if any hearing changes are discovered, and support and intervention begins by 6 months of age. The earlier, the better.
In addition to your pediatrician and audiologist, every baby who is deaf or hard of hearing should be seen by a pediatric
otolaryngologist who specializes in the mechanics of the ear.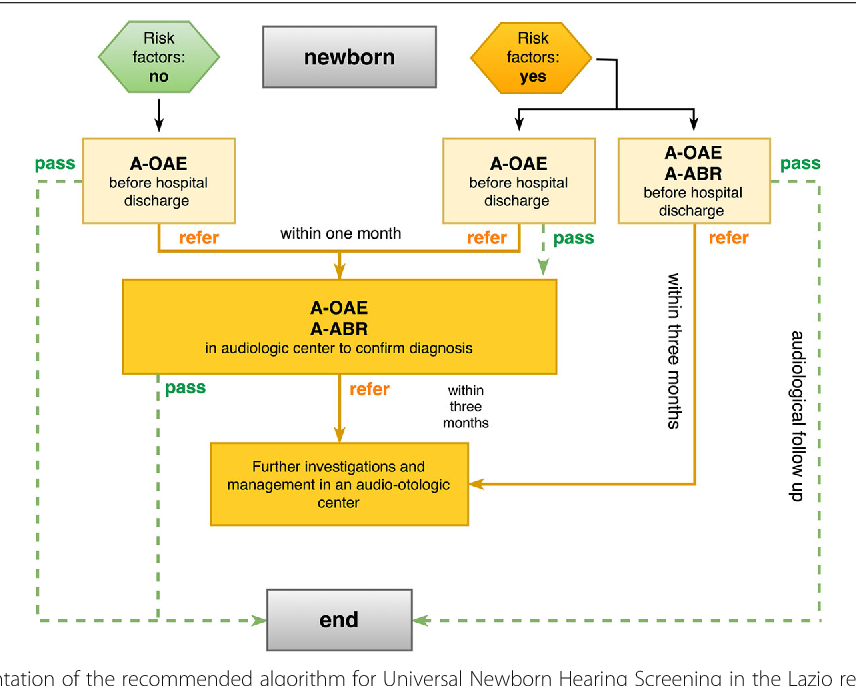 Your pediatrician should also recommend seeing a pediatric
ophthalmologist, because some children can also have problems with their vision, and children who are deaf or hard of hearing are dependent on their vision for language input. Many children are also seen by a
geneticist to determine if there is a hereditary cause of hearing changes.
Your pediatrician should also recommend seeing a pediatric
ophthalmologist, because some children can also have problems with their vision, and children who are deaf or hard of hearing are dependent on their vision for language input. Many children are also seen by a
geneticist to determine if there is a hereditary cause of hearing changes.
Your state Early Hearing Detection and Intervention (EHDI) program can help provide you and your pediatrician with more information. Babies who are deaf or hard of hearing should be referred to Early Intervention for evaluation and services. Additionally, the Individuals with Disabilities Education Act (IDEA) supports intervention programs for children who are deaf or hard of hearing within early intervention and school programming.
The audiologist, together with the otolaryngologist, can tell you the
type and degree of hearing change and what the next steps are. These next steps can vary depending on your family's choices, as well as the type and degree of hearing change.
If my baby passes the newborn hearing screening, does it mean he or she will not have hearing loss later?
Unfortunately, no. Some babies may develop
hearing loss later in childhood. Causes of late onset or progressive hearing loss in children can include genetics,
frequent ear infections, other infections like
measles or
meningitis, a head injury, exposure to damaging levels of
loud noises, and secondhand
smoke. Newborns who need an extended period of neonatal intensive care may also be at an increased risk for hearing loss later.
Even if your baby passes the newborn hearing screening, you should still watch for possible signs of hearing loss as your child grows. Talk with your pediatrician if your child:
|
If my baby passes the first hearing test, why is more screening needed?
Even if your child shows no signs of hearing changes, the AAP recommends they be screened again at ages 4, 5, 6, 8 and 10. Additional screenings are recommended sometime between ages 11-14, 15-17, and 18-21--or any time there is a concern. More frequent follow-up screenings may be recommended for children who have a higher risk for hearing loss.
Hearing loss sometimes is gradual and hard to notice at first. Routine screenings can catch hearing changes early, when providing support and resources can have the most impact on the child's development.
Additional screenings are recommended sometime between ages 11-14, 15-17, and 18-21--or any time there is a concern. More frequent follow-up screenings may be recommended for children who have a higher risk for hearing loss.
Hearing loss sometimes is gradual and hard to notice at first. Routine screenings can catch hearing changes early, when providing support and resources can have the most impact on the child's development.
Remember:
Timing is everything. The sooner hearing changes are identified in a baby, the more likely interventions can help her reach her full potential. Talk with your pediatrician if you have any concerns about your child's hearing.
Additional Information & Resources:
Newborn Screening Tests
Early Hearing Detection and Intervention - A Program of the American Academy of Pediatrics
Centers for Disease Control and Prevention (CDC) National Center on Birth Defects and Developmental Disabilities (NCBDDD) - Provides research, basic information and statistics regarding hearing loss, screening and diagnosis, as well as current articles and educational materials for clinicians and families.

The information contained on this Web site should not be used as a substitute for the medical care and advice of your pediatrician. There may be variations in treatment that your pediatrician may recommend based on individual facts and circumstances.
Why follow-up care is crucial when a newborn fails ABR hearing screening | ENT | Pediatrics | Your Pregnancy Matters
If a baby fails their newborn ABR hearing screening test, follow-up care is crucial to their future language development.Your baby will receive many tests and treatments in their first days of life, from Apgar scoring to measure their reflexes and eye drops that eliminate germs to their first series of vaccinations.
Among the most important of these is the newborn hearing screening. From birth, babies use information from their surroundings to access early language – the foundation for a lifetime of communication.
Babies who are born deaf or hard of hearing need additional support to access language. Knowing early whether a newborn has hearing loss gives families the best chance to improve their hearing and language development.
There are two types of hearing screenings for newborns. Both are painless and work by introducing sound into the baby’s ear and analyzing the ear’s function:
- Otoacoustic emissions (OAE) – the standard that many hospitals use. OAE measures activity from the hair cells in the inner ear that bring sound vibrations to the cochlea, a structure that transforms the vibrations into signals that travel up the brainstem.
- Auditory brainstem response (ABR) – an advanced technology that UT Southwestern and Parkland Health use. ABR assesses more of the auditory pathway, recording neural impulses from the cochlea and all the way through the upper levels of the brainstem.
OAE screening is sufficient for most newborns, but ABR screening reduces the number of vulnerable babies who might get left behind. For example, preemies may have underdeveloped auditory nerves, causing hearing loss. Babies with auditory neuropathy spectrum disorder may have a cochlear response, but sound vibrations don’t make it to their brains.
For example, preemies may have underdeveloped auditory nerves, causing hearing loss. Babies with auditory neuropathy spectrum disorder may have a cochlear response, but sound vibrations don’t make it to their brains.
Using ABR offers parents two layers of confidence in their newborn’s results. A trained technician performs the screening. At some institutions, including Parkland Hospital, if the baby does not pass, they get a second ABR with an audiologist – a doctor who specializes in hearing – before they go home from the hospital.
Angela Shoup, Ph.D., previously Chief of the Division of Communicative and Vestibular Disorders at UT Southwestern Medical Center, and now Executive Director of the Callier Center for Communication Disorders, Professor at UT Dallas and Clinical Professor at UT Southwestern was a champion in developing this advanced process. Learn more below about Dr. Shoup’s 25-year passion for universal newborn hearing screening.
Newborns that do not pass the hospital hearing screening may have acute or chronic hearing loss. These babies need advanced follow-up within two weeks. At that visit, we can determine whether the problem is temporary or chronic – and what the baby needs in order to access early language development.
These babies need advanced follow-up within two weeks. At that visit, we can determine whether the problem is temporary or chronic – and what the baby needs in order to access early language development.
What causes babies to fail their hearing screening?
Deafness and hearing loss can be caused by genetic abnormalities, birth defects, or maternal infections during pregnancy. In some cases, the baby will immediately show signs of hearing loss, such as not responding to sounds or failing their hearing screening.
Rarely, a baby who can hear and process sound might nonetheless fail their newborn hearing screening. Some of these include babies who:
- Stayed in the NICU: Babies go to the neonatal intensive care unit (NICU) for high-risk health issues, some of which can damage hearing. For example, serious breathing problems can decrease oxygen to the brain, resulting in inner ear or auditory nerve damage. Maternal health complications such as diabetes or substance use disorder can also negatively impact hearing.

- Had fluid in their ears: Some newborns get fluid in their middle or inner ears during the birth process, and it can take a few days for the fluid to clear. Approximately 10 percent of babies with fluid in their ears may develop lasting hearing loss that requires treatment, according to the American Academy of Otolaryngology – Head and Neck Surgery Foundation [PDF].
- Had jaundice: Jaundice is a temporary condition that causes approximately 60 percent of newborns to temporarily have yellowed skin and eyes. The baby’s liver must adapt to filtering out the chemical bilirubin – which is handled by the mother’s liver during pregnancy. Short-term elevations of bilirubin levels, as well as severe and untreated jaundice, can cause hearing loss.
- Had a CMV infection: Congenital cytomegalovirus (CMV) is a viral infection that can cause severe disease if a baby is infected before birth. In the U.S., 0.5-0.7 percent of babies are born with CMV, and approximately 90 percent of those have no symptoms at birth.
 However, 10-15 percent of asymptomatic babies develop hearing loss over time. Visit the National CMV Foundation to learn more.
However, 10-15 percent of asymptomatic babies develop hearing loss over time. Visit the National CMV Foundation to learn more. - Aspirated meconium: Occasionally, a baby swallows their own feces (poop) during birth. With quick treatment, breathing complications generally resolve quickly. However, some antibiotics used to treat meconium-related infections, such as gentamicin, can damage the sense organ of hearing.
If your baby experienced these issues and passed their newborn hearing screening, they still will likely need follow-up screenings throughout childhood. Hearing loss can develop over time, and your baby may need close monitoring and screening for hearing loss through young adulthood.
If the baby did not pass the newborn hearing screening, it’s important that the baby receive an advanced follow-up screening within 10-12 days for the best chance at receiving early intervention and unlocking their early language development.
The advanced follow-up visit is crucial
Because UT Southwestern uses highly sensitive ABR screening for all newborns, many babies who are referred for advanced follow-up screening have some level of hearing impairment. Keeping the advanced follow-up visit is crucial to give your newborn a healthy start in language development.
Keeping the advanced follow-up visit is crucial to give your newborn a healthy start in language development.
We understand that attending another appointment with a newborn takes extra work. But there are serious health consequences for infants who do not get the advanced care they need, including delayed speech, social isolation, and lifelong communication problems at school, at work, and in interpersonal relationships.
What to expect at the advanced follow-up visit
Your baby will get an outpatient ABR screening.
- If the baby passes this advanced screening, we will give you important information about hearing and speech development milestones. We’ll also refer you for regular follow-up screening if your baby has a risk factor for delayed onset of hearing loss, which can develop later in childhood.
- If the baby does not pass, we will refer you to Children’s Health for a diagnostic evaluation by a pediatric audiologist and otolaryngologist (ear, nose, and throat doctor).
 At the appointment, the audiologist will complete a diagnostic ABR evaluation that helps us determine at which volumes, pitches, and frequencies the baby can receive sound.
At the appointment, the audiologist will complete a diagnostic ABR evaluation that helps us determine at which volumes, pitches, and frequencies the baby can receive sound.
We will guide and support you through every step of evaluation, diagnosis, and treatment. With early diagnosis, there are many options to improve how your baby accesses sound, develops language, and learns to communicate.
Treatment options for babies with hearing loss
With proper support, deaf or hard of hearing babies can grasp language and develop on track with their peers. Our goal is to maximize any hearing they have and supplement language development with multichannel support.
Depending on the type and severity of hearing loss, babies through young adults can benefit from:
- Getting cochlear implants – surgically implanted devices that stimulate the auditory nerves to improve sound transmission
- Using amplification devices or hearing aids
- Learning American Sign Language (ASL)
- Some types of ear surgeries, if the part of the ear behind the eardrum is not fully developed or the bones in that part of the ear have congenital abnormalities
- Accessing accommodations at school, such as sitting closer to the teacher or getting written notes
- Connecting with other deaf or hard of hearing people, socially or in support groups
 Knowing early whether a newborn has hearing loss gives families the best chance to improve their hearing and language development.
Knowing early whether a newborn has hearing loss gives families the best chance to improve their hearing and language development. Children’s Health Family-Focused Center for Deaf and Hard of Hearing Children can connect you with community resources to keep your child’s development on track, as well as offer emotional support for children and parents.
Universal hearing screening and early intervention for infants who are deaf or hard of hearing can generate positive impacts on society as a whole. Citizens who learn to communicate – with speech, ASL, or both – can enjoy interacting with their peers and contribute more productively to society than if their hearing loss was left untreated.
Early hearing loss intervention offers parents a chance to bond with their baby and help them thrive. And pediatric intervention services can spare children from the stress and depression that can arise from potentially isolating disabilities such as hearing loss.
When it comes to hearing difficulties, time is of the essence. The quicker we identify and quantify your child’s hearing abilities, the sooner we can help get them the advanced care they need.
The quicker we identify and quantify your child’s hearing abilities, the sooner we can help get them the advanced care they need.
Innovation spotlight: How UT Southwestern faculty, affiliates led the Texas journey to universal newborn hearing screening
Dr. Shoup and her colleagues have been instrumental in the movement for universal newborn hearing screening for Texas newborns. She has dedicated more than 25 years to improving early language access and community strategies for enhancing follow-up for infants who do not pass newborn hearing screening. Her overarching goal is for hearing screening, early intervention, and language development support to be the standard of care for all newborns.Angela Shoup, Ph.D., is a champion for newborn hearing screening. She was Chief of the Division of Communicative and Vestibular Disorders at UT Southwestern Medical Center and is currently the Executive Director of the Callier Center for Communication Disorders at UT Dallas, a professor at UT Dallas and a clinical professor in the department of Otolaryngology at UT Southwestern.
Evolution of Hearing Screening in Texas
- 1960s: National advocates begin working toward universal newborn hearing screening.
- 1970s: The Joint Committee on Infant Hearing recommends developing a high-risk registry for screening, inclusive of factors we still use today in determining a child’s chances for delayed onset or progressive hearing loss, such as infections or premature birth.
- 1986: Supported by the National Council of Jewish Women, Parkland begins newborn hearing screenings for all babies at high risk for hearing loss, as well as all babies in special care nurseries, regardless of known risk factors.
- 1993: The National Institutes of Health recommends that all infants need an ABR or OAE hearing screening by three months of age, and that appropriate follow-up should be established for babies who do not pass.
- 1996: Dr. Shoup joins the UT Southwestern faculty with a passion for newborn hearing and early language access.

- 1997: Dr. Shoup and Kristine Owen, Au.D., a UT Southwestern audiologist, work with a multidisciplinary team including representatives from the Parkland nursery nurse and nurse practitioner leadership, physician leadership, and Women and Children’s Health leadership to plan for universal newborn hearing screening at Parkland. Pablo J. Sanchez, M.D., an infectious disease neonatologist, advocated for the addition of hearing-targeted congenital cytomegalovirus screening to the protocol.
- 1999: The team earns a grant from the Hoblitzelle Foundation to equip Parkland with the necessary equipment to launch universal newborn hearing screening – one year before it is required by the passing of Texas House Bill 714.
- 2000-present: Dr. Shoup works with organizations involving multiple stakeholders, including physicians, audiologists, early intervention specialists, educators, speech-language pathologists, and others, to ensure providers and families understand the importance of newborn hearing screening for lifelong health and communication.

- 2008: Drs. Stehel, Shoup, Sanchez, and Owen, et al., publish a study in Pediatrics associating the discovery of CMV infections in infants based on abnormal newborn hearing screening results.
- 2016: Dr. Shoup receives the UT Dallas Distinguished Alumni Award.
- 2018 & 2019: Dr. Shoup is named a D Magazine Best Doctor and inducted into the National Academies of Practice Audiology Academy as a Distinguished Scholar and Fellow.
- 2020: Parkland Health maintains a strong follow-up program, with nearly 100% of infants that do not pass hearing screening returning for follow-up visits.
- 2021: Dr. Shoup currently serves as President of the American Academy of Audiology and Vice Chair of the National Academies of Practice Audiology Academy.
Schedule a visit with a pediatric hearing expert. Call 214-645-8300 or request an appointment online.
Audiology at the Central Clinical Hospital of the Russian Academy of Sciences - where to check the hearing of a child in Moscow
Hearing screening for newborns and children in the first year of life
To detect congenital hearing impairments and effective hearing and speech rehabilitation (starting from the first months of life), since 2008, universal audiological screening has been carried out in our country, which consists in conducting an otoacoustic emission registration test for all children not at risk on the 4th day of life in the maternity hospital. If for some reason (technical condition of the device in the maternity hospital, the impossibility of conducting the study due to the restless behavior of the child, etc.) the study was not carried out, you can have your child's hearing screened by our audiologists. If a child has congenital causes (risk factors) of hearing loss, then it is necessary to register the auditory potentials of the brain - a method that allows you to assess the degree of potential hearing loss. These reasons include:
If for some reason (technical condition of the device in the maternity hospital, the impossibility of conducting the study due to the restless behavior of the child, etc.) the study was not carried out, you can have your child's hearing screened by our audiologists. If a child has congenital causes (risk factors) of hearing loss, then it is necessary to register the auditory potentials of the brain - a method that allows you to assess the degree of potential hearing loss. These reasons include:
- rubella, syphilis and certain other maternal infections during pregnancy,
- low birth weight,
- asphyxia at birth (lack of oxygen during childbirth),
- misuse of drugs (such as aminoglycosides, cytotoxic drugs, antimalarial drugs and diuretics) during pregnancy,
- severe jaundice in the neonatal period, which can lead to damage to the auditory nerve of the newborn.
Appointment for a hearing test by phone: +7 (985) 413-34-75
+7 (985) 413-34-75
Hearing diagnostics
The main study, on the basis of which a conclusion is made about the state of hearing, is tonal threshold audiometry - registration of sound perception thresholds at various frequencies. The limitation of this method is the age of the patient (from 6 years old) and the need to focus on test signals, which can be problematic, for example, for patients with concomitant neurological pathology.
The limitation of this method is the age of the patient (from 6 years old) and the need to focus on test signals, which can be problematic, for example, for patients with concomitant neurological pathology.
To determine hearing in patients in whom it is impossible to conduct audiometry, the so-called. “objective” techniques that do not depend on the reaction of the patient. The most informative group of tests is the registration of various classes of auditory evoked potentials of the brain - recording the responses of the auditory analyzer (by means of electrodes fixed on the patient's head) to acoustic stimuli. The main condition for such a study is the state of sleep of the child.
Other commonly used objective tests for assessing the organ of hearing are acoustic impedancemetry (assessment of the state of the middle ear) and registration of otoacoustic emissions (OAE) - recording the responses of the hair cells of the cochlea to acoustic stimulation (with normal cochlear function, the OAE is recorded).
A brief description of all the most common audiological tests is presented in the table below:
Appointment for hearing diagnostics for children under 5 years of age (in conditions of natural sleep) and hearing test (children of any age) under anesthesia, as well as setting up the processor of cochlear implant systems (Advanced Bionics, Cochlear, Med-El, Oticon-Neurelec) by phone. +7 (985) 413 3475.
Cochlear Implant
The operation of cochlear implantation - the installation of an electrode in the cochlea of the inner ear, which produces electrical stimulation of the auditory nerve, is performed in patients with bilateral sensorineural deafness. With congenital deafness, it is critically important to perform this operation and start hearing and speech rehabilitation as early as possible - in this case, the potential effect will be maximum. The audiological indication for cochlear implantation is the state of sound perception thresholds corresponding to severe hearing loss and deafness.
To diagnose hearing, an extended audiological study is carried out, on the basis of which the type and degree of hearing loss are determined; patients with identified sensorineural deafness undergo hearing aids - the installation of hearing aids. 6 months after hearing aid, on the basis of deaf pedagogical testing, a conclusion is made about the advisability of cochlear implantation.
Advantages of the Clinic of the Research Institute of Pediatrics of the Central Clinical Hospital of the Russian Academy of Sciences
- Advanced diagnostic and laboratory equipment for fast and accurate diagnosis of various diseases in children.
- Individual approach to each child, taking into account age characteristics, personal preferences and wishes of parents.
- Clear and precise answers to all questions related to the child's health.
Management of cochlear implant patients
Hearing-speech rehabilitation after cochlear implantation is a long process, the result of which depends on the constancy of classes with a deaf teacher to develop hearing-speech skills. Audiological support consists in regular adjustments of the processor of the cochlear implantation system. The specialists of the Institute have developed original methods for setting up the processor based on the registration of the responses of the auditory analyzer, which allows the rehabilitation of young children to be most effective.
Audiological support consists in regular adjustments of the processor of the cochlear implantation system. The specialists of the Institute have developed original methods for setting up the processor based on the registration of the responses of the auditory analyzer, which allows the rehabilitation of young children to be most effective.
Practical advice for parents
Can my child have hearing loss? Your child may be suffering from hearing loss if he or she:
- Does not respond to sounds
- Recently had a serious illness, such as meningitis
- He/she has a delay or impairment of speech/language development that does not correspond to age norms
- Does not understand what you say to him or often asks to repeat what was said
- Responds incorrectly to questions or instructions
- Turns up the volume when watching TV or is hard of hearing what is said to him on the phone
- Does not study well at school or has behavioral problems
- He/she often has ear discharge or wax plugs
- Often complains of pain or stuffiness in the ear.

When should the child be examined?
- The sooner the better!
- Infants who are diagnosed with hearing loss three months after birth and begin rehabilitation six months later may develop speech and language similar to those of children with normal hearing.
- Even if your child is older, any delay can negatively impact their language development and learning ability.
The child is hard of hearing. How to help him?
Follow these rules when talking to a child:
- look him in the face
- talk in a well-lit area where your child can see your lips and facial expressions
- Keep background noise low - or move to a quieter place speak clearly and slowly
- don't shout!
Don't hide your child's hearing problems
- Inform your child's teachers about the hearing loss problem and ask them to seat the child at the first table in the class.
 Ask teachers to look the child in the face while talking
Ask teachers to look the child in the face while talking - Tell friends and family about your child's needs and teach them how to communicate effectively
- Involve your child in all family and social activities.
Service your child's hearing aid or cochlear implant, including:
- change batteries regularly
- monitor the technical condition of the device
- Store the device in a drying box at night.
Follow your audiologist's advice
- Get a scheduled hearing test as recommended by
- Have your hearing aid or cochlear implant processor fitted regularly by an audiologist.
REMEMBER
Every 20th person suffers from hearing loss. Nothing to be ashamed of. Don't hide your child's hearing problems!
* in the section "Practical advice to parents" materials of the World Health Organization (WHO) and the National Medical Association of Audiologists are used.
Hearing tests for children
The hearing test helps to determine if there is a hearing loss, whether it affects one or both ears, what degree and type of hearing loss, and whether the hearing loss can be treated or corrected by technical means (for example, hearing aids, cochlear implants and assistive devices). technologies) and how this hearing loss will affect the child and their ability to communicate.
Different types of hearing tests
Audiological screening
Audiological screening usually only detects a child's hearing loss. Screening procedures are fast, reliable and painless. If the child does not pass the screening test, they are referred to a specialist for a more detailed examination.
Objective hearing tests
These tests do not require the child to react or participate when they hear a sound. They are usually performed on infants and young children, children with developmental disabilities or non-contact children; in cases where the results of other tests are inconsistent or unreliable, as well as to confirm the results of behavioral testing.
- Acoustic stem evoked potential (ASEP): the sound is reproduced through headphones, the reaction to sound stimuli is recorded. The analysis of the obtained recordings makes it possible to assess the sensitivity of hearing.
- Otoacoustic Emission Method (OAE): The OAE method provides information on the functioning of sensory hair cells inside the organ of hearing (cochlea). Sound signals are fed into the already through a miniature speaker, and the microphone records the reaction of the snail to the sound.
- Tympanometry: This test method provides information on the functional state of the tympanic membrane and middle ear. An air jet is directed into the ear under a small pressure, and the intensity of the tympanic membrane vibrations is recorded in response to a change in air pressure. This test helps to determine if there is a hole in the eardrum, as well as to detect the presence of fluid in the middle ear.
Behavioral hearing tests
Behavioral tests provide information about how a child hears sounds of different frequencies and reacts to them. Sound signals are given through headphones or speakers. The audiologist monitors and records the child's reaction to the quietest of the reproduced sounds and, based on the data obtained, builds a graph called an audiogram.
Sound signals are given through headphones or speakers. The audiologist monitors and records the child's reaction to the quietest of the reproduced sounds and, based on the data obtained, builds a graph called an audiogram.
How hearing loss is measured
Sounds have different pitches, called frequency, and different volume levels, called sound intensity. The unit of sound frequency is hertz (Hz), the unit of sound intensity is decibel (dB). The range of frequencies we hear includes both low (250 Hz) and high frequencies (8000 Hz). The range of sound intensity levels we perceive ranges from 0 dB (very quiet sound) to 120 dB (very loud sound). A hearing test is a determination of how quiet sounds in each frequency range we can hear.
Audiogram
The results of a hearing test are recorded on a graph called an audiogram (a visual representation of a child's hearing sensitivity). An audiogram shows the quietest sounds a child hears. Sounds are quiet and loud, as well as low-frequency and high-frequency. The graph shows both the volume and the frequency of the sound. The area of very quiet sounds is at the top of the graph, and the area of very loud sounds is at the bottom of the graph. Low frequencies are located on the graph on the left, high frequencies on the right.
The graph shows both the volume and the frequency of the sound. The area of very quiet sounds is at the top of the graph, and the area of very loud sounds is at the bottom of the graph. Low frequencies are located on the graph on the left, high frequencies on the right.
Degrees of hearing loss
Degree of hearing loss refers to the severity of hearing loss. In children, hearing sensitivity is usually described as an average.
- Normal hearing: 0 to 20 dB
- Mild hearing loss: 21 to 40 dB
- Moderate hearing loss: 41 to 65 dB
- Severe hearing loss: 66 to 90 dB
- Profound hearing loss: 91 dB or more
Hearing loss often affects the ability to understand speech. In particular, a person stops hearing consonant sounds /p/, /k/, /f/, /x/ or all sounds like /t/, /sh/ and /s/.
Frequently Asked Questions about Hearing Tests
Why does my child need a hearing test?
Your child may need a hearing test for several reasons:
- Your child did not receive an audiological newborn screening or an audiological screening at school
- You, your loved ones, or your child's teacher are concerned that your child is having trouble hearing or following directions
- Your child reported hearing problems
- Your child is having ear surgery
- Your child is about to undergo medication that could affect hearing
How often should my child have a hearing test?
Your child's hearing may change over time.