Threatened abortion meaning
Miscarriage - threatened Information | Mount Sinai
Threatened miscarriage; Threatened spontaneous abortion; Abortion - threatened; Threatened abortion; Early pregnancy loss; Spontaneous abortion
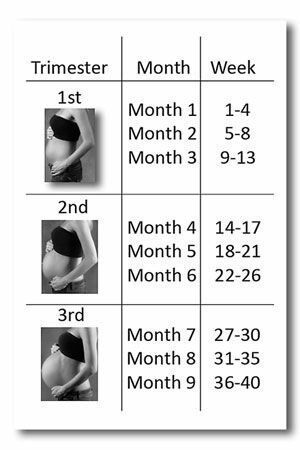
A threatened miscarriage is a condition that indicates the potential for a miscarriage or early pregnancy loss. It might take place before the 20th week of pregnancy.
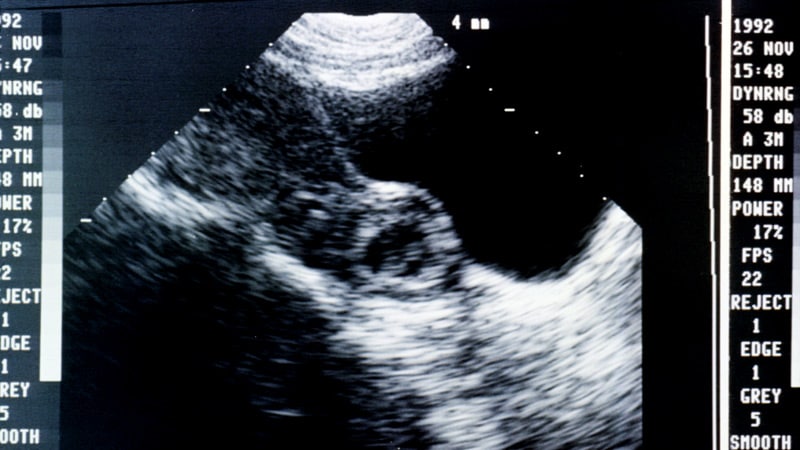
This image shows a human embryo implanted in the uterine wall in the early stages of pregnancy.
A threatened miscarriage is a condition that suggests a miscarriage might take place before the 20th week of pregnancy. Symptoms include vaginal bleeding and abdominal cramps.
Causes
Some pregnant women have some vaginal bleeding during the first 3 months of pregnancy. Bleeding may occur with or without abdominal cramps. When the symptoms indicate a miscarriage is possible, the condition is called a "threatened abortion." (This refers to a natural event that is not due to a medical or surgical abortion.)
Miscarriage is common. Small falls, injuries or stress during the first trimester of pregnancy can cause threatened miscarriage. It occurs in almost one half of all pregnancies. The chance of miscarriage is higher in older women. About one half of women who have bleeding in the first trimester will have a miscarriage.
Symptoms
Symptoms of a threatened miscarriage include:
- Vaginal bleeding during the first 20 weeks of pregnancy (last menstrual period was less than 20 weeks ago).
 Vaginal bleeding occurs in almost all threatened miscarriages.
Vaginal bleeding occurs in almost all threatened miscarriages. - Abdominal cramps may also occur. If abdominal cramps occur in the absence of significant bleeding, consult your health care provider to check for other problems besides threatened miscarriage.
Note: During a miscarriage, low back pain or abdominal pain (dull to sharp, constant to intermittent) can occur. Tissue or clot-like material may pass from the vagina.
Exams and Tests
Your provider may perform an abdominal or vaginal ultrasound to check the baby's development and heartbeat, and the amount of bleeding. A pelvic exam may also be done to check your cervix.
Blood tests done may include:
- Beta HCG (quantitative) test (pregnancy test) over a period of days or weeks to confirm whether the pregnancy is continuing
- Complete blood count (CBC) to determine the presence of anemia
- Progesterone level
- White blood count (WBC) with differential to rule out infection
Treatment
Apart from controlling the blood loss, you may not need any particular treatment. If you are Rh Negative, then you may be given immune globulin. You may be told to avoid or restrict some activities. Not having sexual intercourse is often recommended until the warning signs have disappeared.
If you are Rh Negative, then you may be given immune globulin. You may be told to avoid or restrict some activities. Not having sexual intercourse is often recommended until the warning signs have disappeared.
Outlook (Prognosis)
Most women with a threatened miscarriage go on to have a normal pregnancy.
Women who have had two or more miscarriages in a row are more likely than other women to miscarry again.
Possible Complications
Complications may include:
- Anemia from moderate to heavy blood loss, which may require a blood transfusion.

- Infection.
- Miscarriage.
- The health care provider will want to ensure that the symptoms are not due to an ectopic pregnancy. This is a potentially life-threatening complication.
When to Contact a Medical Professional
If you know you are (or are likely to be) pregnant and you have any symptoms of threatened miscarriage, contact your prenatal provider right away.
Prevention
Most miscarriages cannot be prevented. The most common cause of a miscarriage is a random genetic abnormality in the developing pregnancy. If you have two or more repeated miscarriages, you should consult a specialist to look for an underlying condition that is causing the problem. Women who get prenatal care have better pregnancy outcomes for themselves and their babies.
The most common cause of a miscarriage is a random genetic abnormality in the developing pregnancy. If you have two or more repeated miscarriages, you should consult a specialist to look for an underlying condition that is causing the problem. Women who get prenatal care have better pregnancy outcomes for themselves and their babies.
A healthy pregnancy is more likely when you avoid things that are harmful to your pregnancy, such as:
- Alcohol
- Infectious diseases
- High caffeine intake
- Recreational drugs
- X-rays
Taking a prenatal vitamin or folic acid supplement before becoming pregnant and throughout your pregnancy can lower your chance of miscarriage and improve the chance of delivering a healthy baby.
It is better to treat health problems before you get pregnant than to wait until you are already pregnant. Miscarriages caused by diseases that affect your whole body, such as high blood pressure, are rare. But you can prevent these miscarriages by detecting and treating the disease before becoming pregnant.
Other factors that can increase your risk for miscarriage include:
- Obesity
- Thyroid problems
- Uncontrolled diabetes
Keyhan S, Muasher L, Muasher SJ. Spontaneous abortion and recurrent pregnancy loss: etiology, diagnosis, treatment. In: Lobo RA, Gershenson DM, Lentz GM, Valea FA, eds. Comprehensive Gynecology. 7th ed. Philadelphia, PA: Elsevier; 2017:chap 16.
Richards DS. Obstetric ultrasound: imaging, dating, growth, and anomaly. In: Landon MB, Galan HL, Jauniaux ERM, et al, eds. Gabbe's Obstetrics: Normal and Problem Pregnancies. 8th ed. Philadelphia, PA: Elsevier; 2021:chap 9.
Salhi BA, Nagrani S. Acute complications of pregnancy. In: Walls RM, Hockberger RS, Gausche-Hill M, eds. Rosen's Emergency Medicine: Concepts and Clinical Practice. 9th ed. Philadelphia, PA: Elsevier; 2018:chap 178.
9th ed. Philadelphia, PA: Elsevier; 2018:chap 178.
Last reviewed on: 12/2/2020
Reviewed by: LaQuita Martinez, MD, Department of Obstetrics and Gynecology, Emory Johns Creek Hospital, Alpharetta, GA. Also reviewed by David Zieve, MD, MHA, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
Threatened Abortion - StatPearls - NCBI Bookshelf
Continuing Education Activity
A threatened abortion is vaginal bleeding during pregnancy that does not meet diagnostic criteria for spontaneous abortion. In a threatened abortion, the cervical os remains closed. The World Health Organization (WHO) defines a threatened abortion as pregnancy-related bloody vaginal discharge or frank bleeding during the first half of pregnancy without cervical dilatation. A threatened abortion can present during early pregnancy with lower abdominal pain, and/or vaginal bleeding. Nearly 25 percent of pregnant women have some degree of vaginal bleeding during the first two trimesters and about 50 percent of these progress to an actual abortion. The bleeding in a threatened abortion is mild to moderate. The abdominal pain may present as intermittent cramps, suprapubic pain, pelvic pressure, or lower back pain. This activity examines when this condition should be considered on differential diagnosis and how to properly evaluate it. This activity highlights the role of the interprofessional team in caring for patients with this condition.
The bleeding in a threatened abortion is mild to moderate. The abdominal pain may present as intermittent cramps, suprapubic pain, pelvic pressure, or lower back pain. This activity examines when this condition should be considered on differential diagnosis and how to properly evaluate it. This activity highlights the role of the interprofessional team in caring for patients with this condition.
Objectives:
Outline threatened abortion.
Summarize the differences between threatened abortion and other abortion types including elective, inevitable, incomplete, complete, or missed.
Explain how to manage a patient presenting with a threatened abortion.
Describe how the facilitation of interprofessional team education and discussion can optimize the effective detection of a threatened abortion and inform the need for subsequent evaluations.
Access free multiple choice questions on this topic.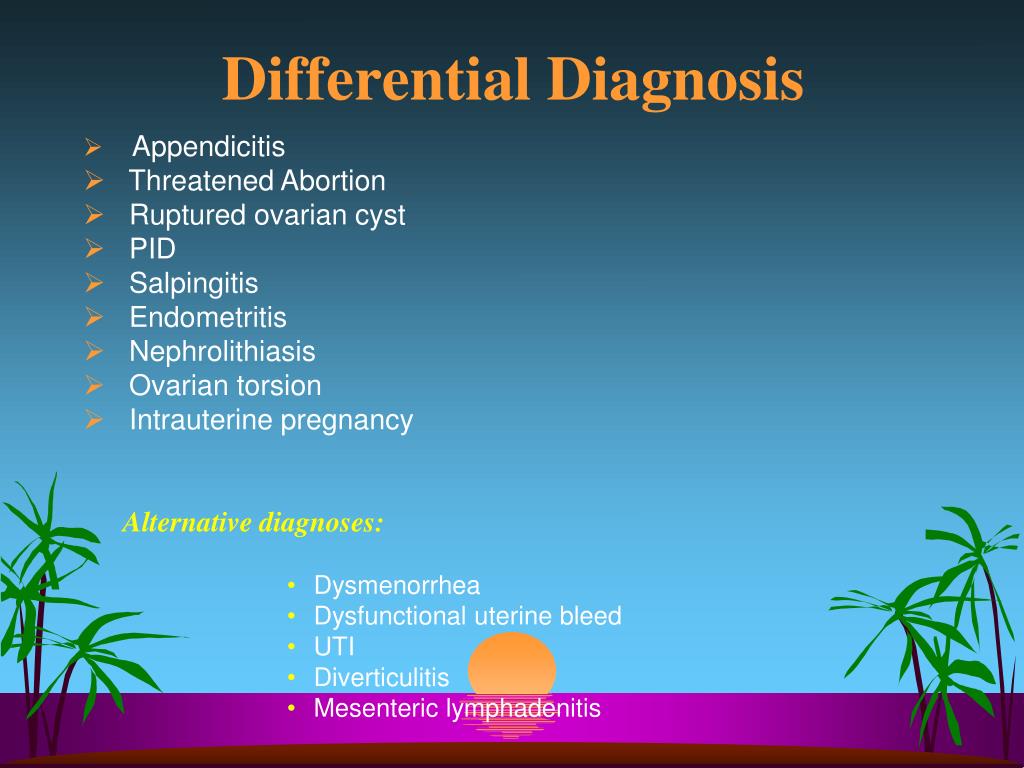
Introduction
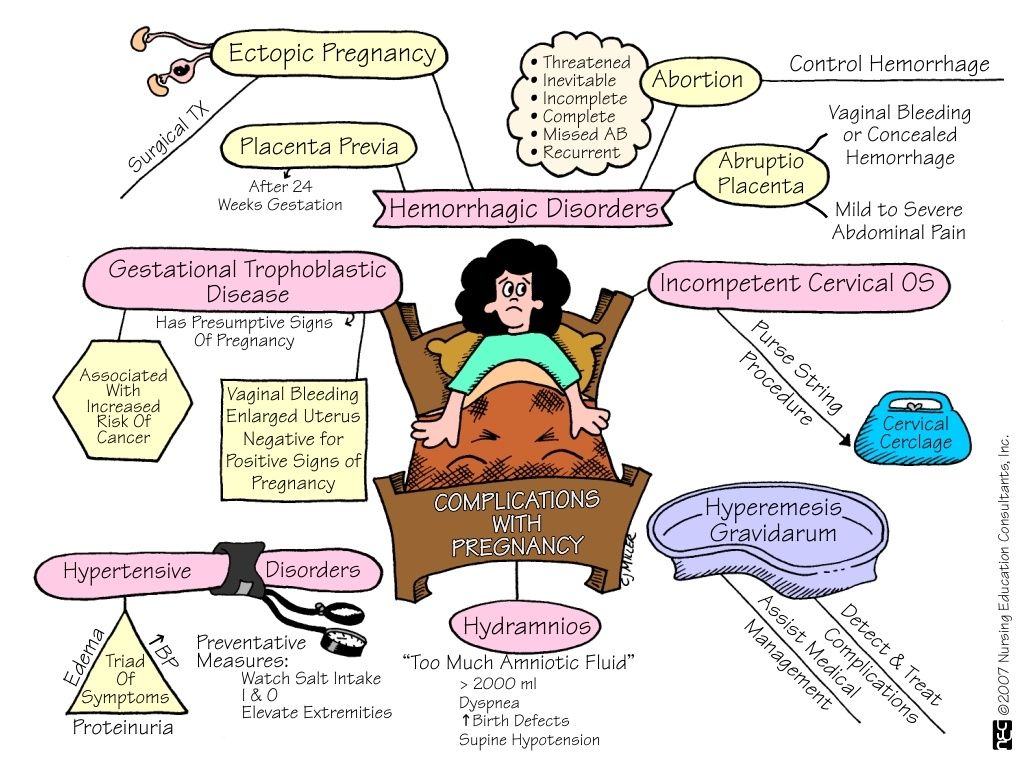
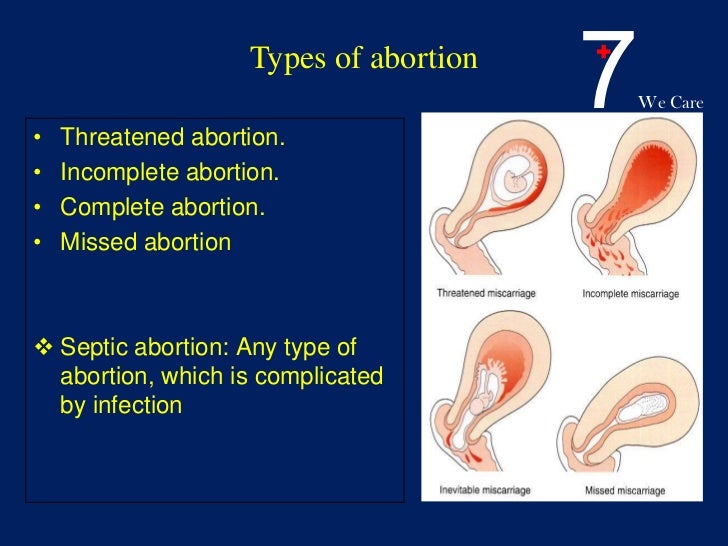
Abortion is the medical term for a pregnancy loss before 20 weeks of gestational age. The types of spontaneous abortion include threatened, inevitable, incomplete, complete, septic, and missed abortion[1].
A threatened abortion is defined as vaginal bleeding before 20 weeks gestational age in the setting of a positive urine and/or blood pregnancy test with a closed cervical os, without passage of products of conception and without evidence of a fetal or embryonic demise. The definition of a threatened abortion by the World Health Organization (WHO) is pregnancy-related bloody vaginal discharge or frank bleeding during the first half of pregnancy without cervical dilatation[2].
Other types of abortion should be considered if the cervical os is open, if there is determined to be an extrauterine pregnancy, if there is determined to be an intrauterine pregnancy without a fetal heartbeat, or if there is evidence of the passage of products of conception[3].
Nearly 25% of pregnant women have some degree of vaginal bleeding during the first two trimesters and about 50% of these progress to loss of the pregnancy. The bleeding during a threatened abortion is typically mild to moderate. The abdominal pain may present as intermittent cramps, suprapubic pain, pelvic pressure, or lower back pain. [4][5][6][7]
Etiology
The exact etiology of a threatened or spontaneous abortion is not always known. It is widely accepted that the vast majority of spontaneous abortions cannot be prevented or modified likely because they are due to chromosomal abnormalities in at least half of all cases[8]. For pregnancy losses that are determined to have a normal chromosomal makeup, termed euploid abortions, maternal and paternal factors play a more significant role[9]. Optimization of maternal health before pregnancy, correcting structural abnormalities of the uterus, and minimizing exposure to teratogens or infections during early pregnancy can reduce the risks for spontaneous abortion[10].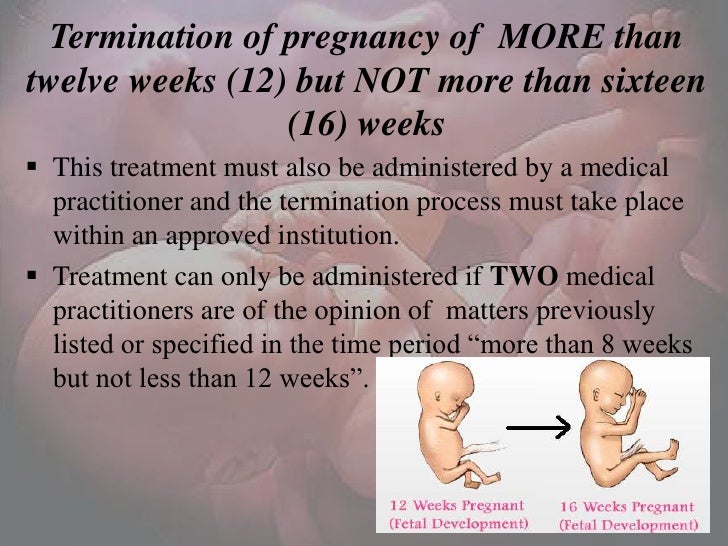 When optimizing maternal health, special consideration should be given to chronic illnesses such as diabetes and thyroid disease, as well as extremes of weight and use of tobacco products, alcohol, or illicit drugs. Some studies have shown that folic acid supplementation immediately before and during early pregnancy may reduce the risk of spontaneous abortionf[11]. It has also been shown in several studies that increasing paternal age is associated with increased risk for pregnancy loss, likely due to increased chromosomal abnormalities[12]. Women should also be educated about reducing the risk of traumatic events and should be screened for risk for intimate partner violence. It is reasonable to recommend preconception counseling to modify these risk factors. [6][13][14][15]
When optimizing maternal health, special consideration should be given to chronic illnesses such as diabetes and thyroid disease, as well as extremes of weight and use of tobacco products, alcohol, or illicit drugs. Some studies have shown that folic acid supplementation immediately before and during early pregnancy may reduce the risk of spontaneous abortionf[11]. It has also been shown in several studies that increasing paternal age is associated with increased risk for pregnancy loss, likely due to increased chromosomal abnormalities[12]. Women should also be educated about reducing the risk of traumatic events and should be screened for risk for intimate partner violence. It is reasonable to recommend preconception counseling to modify these risk factors. [6][13][14][15]
Epidemiology
Threatened abortion can occur in any pregnancy regardless of maternal age, race, comorbidities, lifestyle, or socioeconomic status[10]. If a woman has previously had bleeding in the first trimester of pregnancy, her risk of bleeding in the first trimester of subsequent pregnancies does appear to be increased.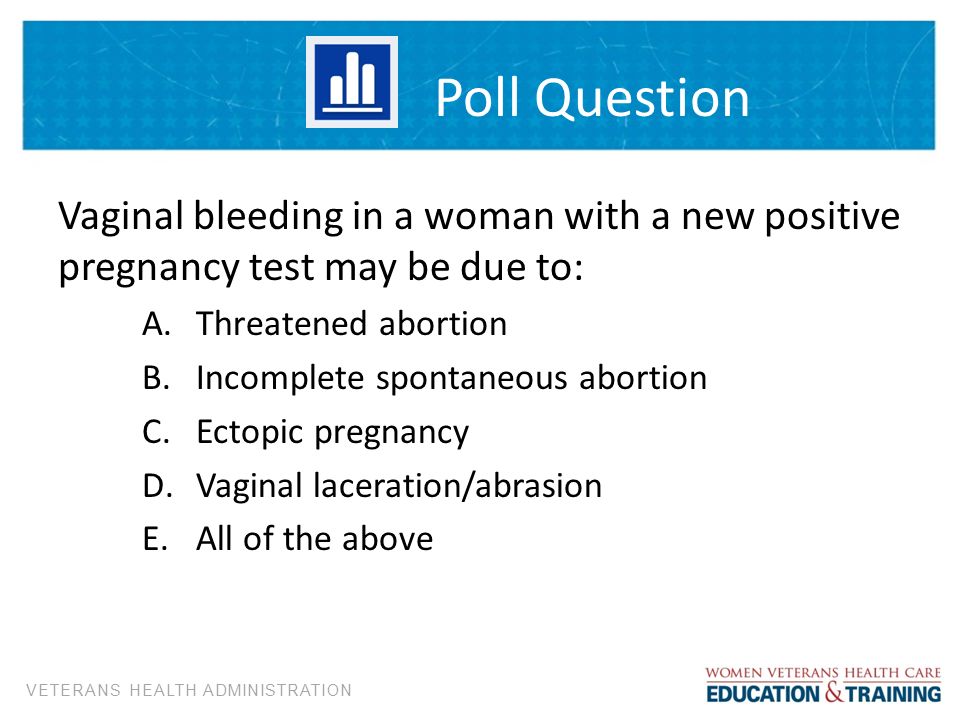 Risk factors for any type of miscarriage include advanced maternal age, advanced paternal age, prior history of pregnancy loss, TORCH infections, uncontrolled hyperglycemia, obesity, uncontrolled thyroid disease, significant stressors, use of teratogenic medications, and presence of a subchorionic hemorrhage[12].
Risk factors for any type of miscarriage include advanced maternal age, advanced paternal age, prior history of pregnancy loss, TORCH infections, uncontrolled hyperglycemia, obesity, uncontrolled thyroid disease, significant stressors, use of teratogenic medications, and presence of a subchorionic hemorrhage[12].
Pathophysiology
A threatened abortion occurs when a pregnant patient at less than 20 weeks gestation presents with vaginal bleeding. The cervical os is closed on a physical exam. The patient may also experience abdominal cramping, pelvic pain, pelvic pressure, and/or back pain. Vaginal bleeding usually begins first followed by cramping abdominal pain hours to days later. Bleeding is the most predictive risk factor for pregnancy loss. More than half of threatened abortions will abort. The risk of spontaneous abortion, in a patient with threatened abortion, is less if fetal cardiac activity is present[1].
Histopathology
It is strongly recommended that all products of conception from any type of abortion are considered for histopathological examination. For patients with repeat pregnancy loss, karyotyping should be given as an option for products of conception to rule in or rule out chromosomal abnormalities as likely cause of spontaneous abortion. This information can help patients determine the best options for moving forward if they desire future pregnancies[16].
For patients with repeat pregnancy loss, karyotyping should be given as an option for products of conception to rule in or rule out chromosomal abnormalities as likely cause of spontaneous abortion. This information can help patients determine the best options for moving forward if they desire future pregnancies[16].
History and Physical
A pelvic exam is mandatory to determine the type of abortion. Determining factors include the amount and site of bleeding, whether the cervix is dilated, and whether fetal tissue has passed. In a threatened abortion, the vaginal exam may reveal a closed cervical os with no tissue. There is usually no cervical motion tenderness[17]. In rare cases, the pelvic exam will reveal uterine and bilateral adnexal tenderness. It is important to note that in a threatened abortion there is no passage of tissue and the cervical os is, by definition, closed[2]. These observations differentiate the condition from an inevitable or incomplete abortion. Women with a threatened abortion usually have stable vital signs, but if hypovolemia is present, one should suspect bleeding or sepsis.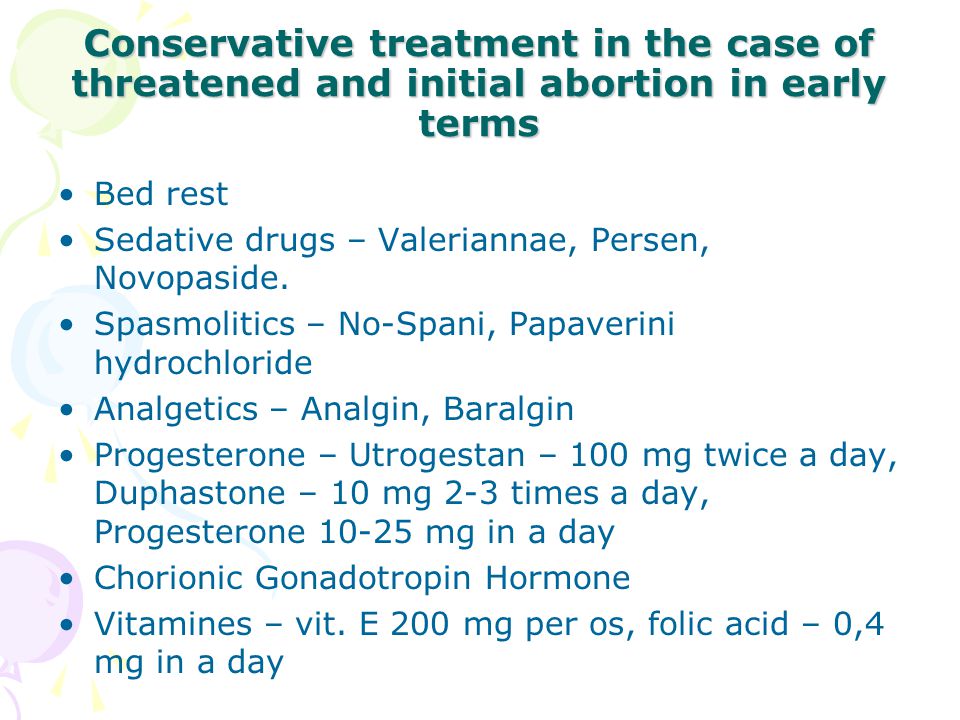 The abdomen in most cases is non-tender and soft. If it is confirmed that there is no viable fetus, a discussion concerning expectant management or induction of abortion should occur with the patient. The method of inducing abortion is either surgical with a suction dilation and curettage or medical with a medication like misoprostol[18][19].
The abdomen in most cases is non-tender and soft. If it is confirmed that there is no viable fetus, a discussion concerning expectant management or induction of abortion should occur with the patient. The method of inducing abortion is either surgical with a suction dilation and curettage or medical with a medication like misoprostol[18][19].
Evaluation
The diagnosis is made by history, physical exam, measurement of beta-human chorionic gonadotropin (beta-hCG), and an ultrasound[10].
A thorough history should be obtained including pregnancy history, medical history, and history of present illness. History of present illness should include when and how symptoms/bleeding began, modifying factors, any treatments trialed up to the point of evaluation, and helping the patient to describe and quantify the bleeding[20][5].
Transvaginal ultrasound may be used to locate the pregnancy and determine if the fetus is viable. The ultrasound can also help rule out ectopic pregnancy and to evaluate for retained products of conception. A yolk sac is typically seen at 36 days, and a heartbeat is seen on ultrasound at approximately 45 days after the last menstruation[21].
A yolk sac is typically seen at 36 days, and a heartbeat is seen on ultrasound at approximately 45 days after the last menstruation[21].
A beta-hCG level of 1500 lU/mL to 2000 lU/mL is associated with a gestational sac on ultrasound. Beta-hCG doubles in 48 hours in 85% of intrauterine pregnancies. Beta-hCG is usually detectable the first nine to 11 days following ovulation and reaches 200 IU/mL at the expected time of menses[22].
Rh factor will also determine if Rhogam should be administered to prevent hemolytic disease of the newborn in this pregnancy and subsequent pregnancies[23].
Hemoglobin and hematocrit levels help monitor the degree of blood loss.
A urinalysis can also be obtained. Urinary tract infection (UTI) has been associated with signs and symptoms of threatened abortion[24].
During the pelvic exam, suction or cotton swabs may be needed to remove blood and products of conception to allow for better visualization of the cervix. Ringed forceps can also be used to remove tissue that may be protruding from the cervical os. All tissue must be examined to determine if it is a clot or products of conception. Evidence of products of conception protruding from the cervix or within the vagina changes the diagnosis from a threatened abortion to a complete or incomplete abortion. Evaluation of the amount of bleeding/blood loss should be performed through a thorough history, as well as during the pelvic examination[25].
All tissue must be examined to determine if it is a clot or products of conception. Evidence of products of conception protruding from the cervix or within the vagina changes the diagnosis from a threatened abortion to a complete or incomplete abortion. Evaluation of the amount of bleeding/blood loss should be performed through a thorough history, as well as during the pelvic examination[25].
Treatment / Management
Alloimmunization prevention by the administration of Rh(D) immunoglobulin should be considered for patients who have vaginal bleeding in the setting of pregnancy in a patient who is Rh-[26]. It has been determined that a 50 mcg dose of immunoglobulin is effective at alloimmunization prevention up to and through the 12th week of gestation, however, it is considered acceptable to give the standard 300 mcg dose due to availability or provider preference[23].
Patients with a threatened abortion should be managed expectantly without any medical or surgical interventions.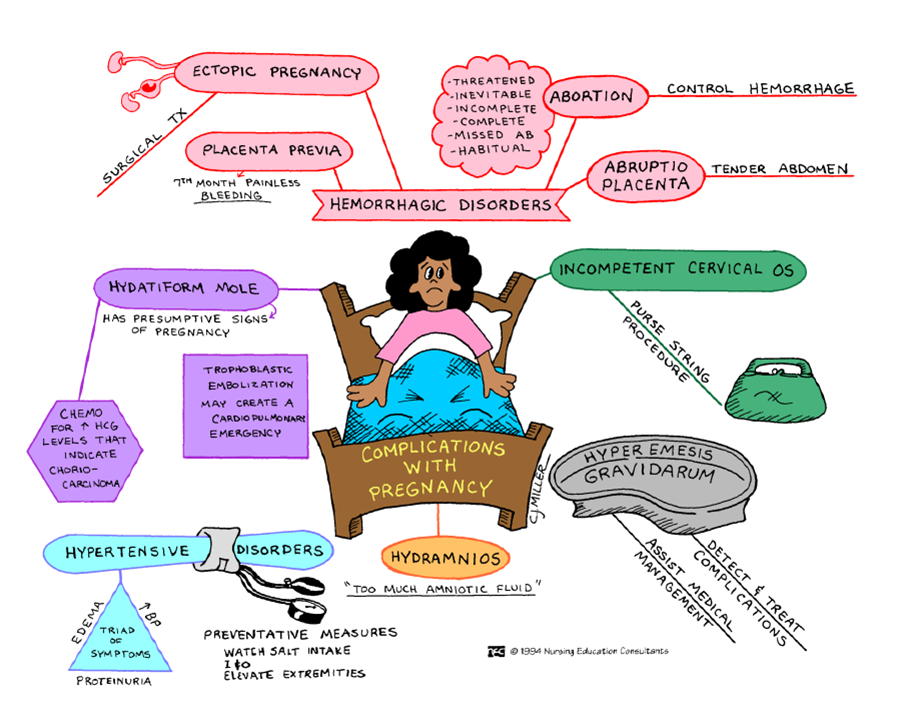 However, patients should be given strict return precautions concerning excessive vaginal bleeding, abdominal pain, or fever and patients should be educated on the importance of follow-up. Analgesia can be provided to help relieve discomfort from cramping. NSAIDs should be avoided in the setting of a threatened abortion, as the pregnancy may continue to progress to viability[27]. Follow-up is recommended with serial transvaginal ultrasounds until a viable intrauterine pregnancy is confirmed or until progression to an inevitable, incomplete, or complete abortion occurs. Clinicians can consider serial quantitative beta hCG testing as recommended for a pregnancy of unknown origin to continue to monitor for the viability of the pregnancy, especially in the setting where an intrauterine pregnancy with cardiac activity has not been confirmed by ultrasound[28]. In these cases, it is possible that the pregnancy has not reached the gestational age by which cardiac activity would be expected on ultrasound or it is possible that the pregnancy will not be viable[22].
However, patients should be given strict return precautions concerning excessive vaginal bleeding, abdominal pain, or fever and patients should be educated on the importance of follow-up. Analgesia can be provided to help relieve discomfort from cramping. NSAIDs should be avoided in the setting of a threatened abortion, as the pregnancy may continue to progress to viability[27]. Follow-up is recommended with serial transvaginal ultrasounds until a viable intrauterine pregnancy is confirmed or until progression to an inevitable, incomplete, or complete abortion occurs. Clinicians can consider serial quantitative beta hCG testing as recommended for a pregnancy of unknown origin to continue to monitor for the viability of the pregnancy, especially in the setting where an intrauterine pregnancy with cardiac activity has not been confirmed by ultrasound[28]. In these cases, it is possible that the pregnancy has not reached the gestational age by which cardiac activity would be expected on ultrasound or it is possible that the pregnancy will not be viable[22].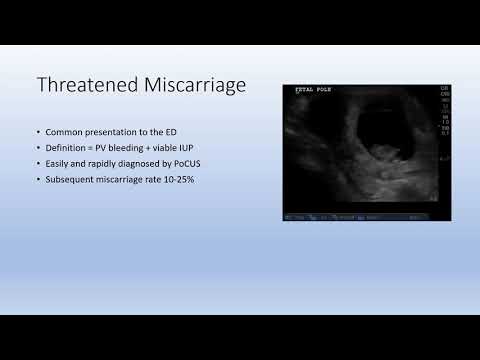 The patient should be counseled about the possibility of spontaneous abortion of the pregnancy, as well as the possibility that the pregnancy may continue to progress towards viability. Several trials have shown that progesterone supplementation does not improve outcomes for patients with threatened abortion and progesterone is not currently recommended as treatment or prevention for patients with threatened abortion.[29] Bedrest and other activity restrictions have not been found to be efficacious in the prevention of a threatened abortion progressing to spontaneous abortion and have been shown to increase the risk of other complications including deep vein thrombosis and/or pulmonary embolism and therefore should not be recommended[30]. Some providers do prefer to advise patients to avoid strenuous activities and to maintain pelvic rest at least until the cessation of vaginal bleeding. Clinicians should recommend that patients start or continue to take prenatal vitamins with folic acid supplementation.
The patient should be counseled about the possibility of spontaneous abortion of the pregnancy, as well as the possibility that the pregnancy may continue to progress towards viability. Several trials have shown that progesterone supplementation does not improve outcomes for patients with threatened abortion and progesterone is not currently recommended as treatment or prevention for patients with threatened abortion.[29] Bedrest and other activity restrictions have not been found to be efficacious in the prevention of a threatened abortion progressing to spontaneous abortion and have been shown to increase the risk of other complications including deep vein thrombosis and/or pulmonary embolism and therefore should not be recommended[30]. Some providers do prefer to advise patients to avoid strenuous activities and to maintain pelvic rest at least until the cessation of vaginal bleeding. Clinicians should recommend that patients start or continue to take prenatal vitamins with folic acid supplementation.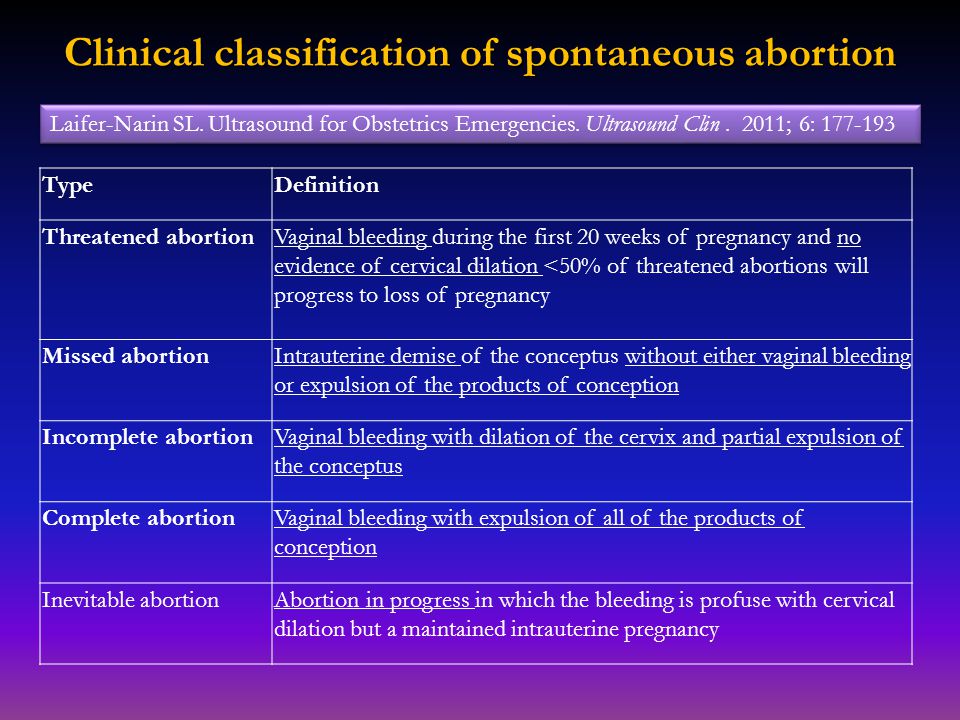 [31][32][33][34]
[31][32][33][34]
Differential Diagnosis
Clinicians should consider several differential diagnoses when encountering vaginal bleeding in the setting of pregnancy. Vulvar, vaginal, cervical trauma should be ruled out during a pelvic examination. Cervical friability can lead to vaginal bleeding which can be caused by cervicitis from an infection or due to premalignant or malignant changes on the cervix. Clinical judgment should determine whether or not the patient should undergo a Pap smear and/or cultures for infection at the time of examination. Other types of abortion should be considered including elective, inevitable, incomplete, complete, septic, and missed abortion[25].
Prognosis
Studies have shown that about 20% of women experience vaginal bleeding before 20 weeks of pregnancy. Furthermore, about 50% of those patients who experience a threatened abortion progress to a pregnancy loss. Studies have shown that there may be an increased risk of adverse outcomes later in pregnancy if there was vaginal bleeding during the first trimester of that pregnancy. For example, there may be a greater risk of placenta previa, placental abruption, necessitation for manual removal of the placenta after delivery, cesarean delivery, preterm premature ruptured membranes, preterm birth, low-birthweight infant, fetal-growth restriction, and fetal or neonatal death. [2]
Complications
Pregnancy loss (progression to inevitable, incomplete, complete, missed abortion)
Heavy bleeding
Retained products of conception
Endometritis
Septic abortion
Complications later in pregnancy as discussed in "Prognosis" [20]
Consultations
Patients with recurrent pregnancy loss or recurrent bleeding during pregnancy should be offered evaluation by a reproductive endocrinology and infertility specialist and/or by a maternal-fetal medicine specialist. If a patient is determined to have a coagulopathy, a hematology consult should be considered[10].
Deterrence and Patient Education
Patient education should be provided as both verbal and written explanations and instructions.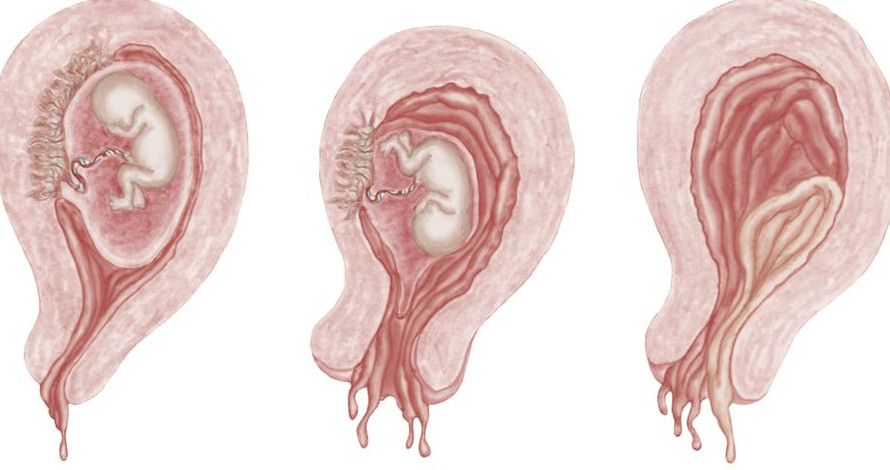 It should be explained to the patient that it is possible her pregnancy will continue and it is also possible that she will undergo a miscarriage. The patient needs to understand that the vast majority of miscarriages are not preventable and that she is not at fault for the loss of the pregnancy if a loss does occur[35]. Providers should explain to the patient that mild to moderate bleeding and cramping can be expected, but uncontrolled pain or heavy bleeding should be evaluated by an obstetric care provider or in the emergency department. Many providers explain that saturating more than 1-2 pads per hour for 2 hours is considered to be heavy bleeding and should be promptly evaluated[36]. Patients can be instructed to take acetaminophen as directed for pain relief. Patients should avoid ibuprofen for pain control during a threatened abortion as it is contraindicated in pregnancy and the patient's pregnancy may progress to viability. Patients who undergo threatened abortion should be evaluated for mood disorders including depression and anxiety.
It should be explained to the patient that it is possible her pregnancy will continue and it is also possible that she will undergo a miscarriage. The patient needs to understand that the vast majority of miscarriages are not preventable and that she is not at fault for the loss of the pregnancy if a loss does occur[35]. Providers should explain to the patient that mild to moderate bleeding and cramping can be expected, but uncontrolled pain or heavy bleeding should be evaluated by an obstetric care provider or in the emergency department. Many providers explain that saturating more than 1-2 pads per hour for 2 hours is considered to be heavy bleeding and should be promptly evaluated[36]. Patients can be instructed to take acetaminophen as directed for pain relief. Patients should avoid ibuprofen for pain control during a threatened abortion as it is contraindicated in pregnancy and the patient's pregnancy may progress to viability. Patients who undergo threatened abortion should be evaluated for mood disorders including depression and anxiety. Especially if a threatened abortion proceeds to pregnancy loss, the patient should be allowed to grieve as appropriate for each individual and should be offered grief counseling[37].
Especially if a threatened abortion proceeds to pregnancy loss, the patient should be allowed to grieve as appropriate for each individual and should be offered grief counseling[37].
Pearls and Other Issues
Most patients with a threatened abortion can be observed from home with close follow-up. Repeat ultrasounds and beta-hCG levels will help to determine progression to a viable pregnancy or to an inevitable, complete, incomplete, or missed abortion. Patients with increased vaginal bleeding require evaluation for hemorrhagic anemia and may be candidates for a blood transfusion or pregnancy evacuation[38].
Enhancing Healthcare Team Outcomes
The diagnosis and management of a threatened abortion involve an interprofessional team that can include an emergency department physician, obstetrician, radiologist, midlevel providers, and nursing staff. For patients to be safely monitored expectantly, good communication between clinicians and the patient is key. All members of the care team need to be on the same page regarding the possibility of pregnancy loss and the importance of return precautions[39].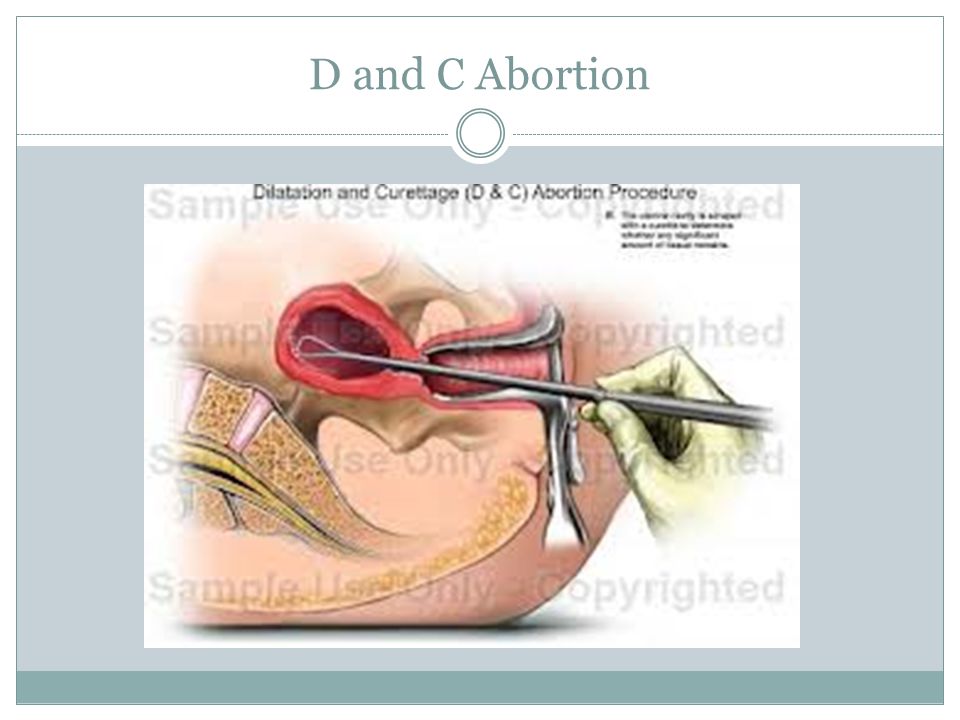
Review Questions
Access free multiple choice questions on this topic.
Comment on this article.
References
- 1.
Alves C, Rapp A. StatPearls [Internet]. StatPearls Publishing; Treasure Island (FL): Jul 18, 2022. Spontaneous Abortion. [PubMed: 32809356]
- 2.
Redinger A, Nguyen H. StatPearls [Internet]. StatPearls Publishing; Treasure Island (FL): Jun 27, 2022. Incomplete Abortions. [PubMed: 32644497]
- 3.
de Codt M, Balza C, Jadoul P, Forget P, Squifflet JL, Bernard P, Luyckx M. Hysteroscopic Resection for Missed Abortion: Feasibility, Operative Technique and Potential Benefit Compared to Curettage. Front Surg. 2020;7:64. [PMC free article: PMC7505996] [PubMed: 33102514]
- 4.
Karataşlı V, Kanmaz AG, İnan AH, Budak A, Beyan E. Maternal and neonatal outcomes of adolescent pregnancy. J Gynecol Obstet Hum Reprod. 2019 May;48(5):347-350. [PubMed: 30794955]
- 5.
Hendriks E, MacNaughton H, MacKenzie MC. First Trimester Bleeding: Evaluation and Management. Am Fam Physician. 2019 Feb 01;99(3):166-174. [PubMed: 30702252]
- 6.
Goodarzi P, Falahzadeh K, Aghayan H, Payab M, Larijani B, Alavi-Moghadam S, Tayanloo-Beik A, Adibi H, Gilany K, Arjmand B. Therapeutic abortion and ectopic pregnancy: alternative sources for fetal stem cell research and therapy in Iran as an Islamic country. Cell Tissue Bank. 2019 Mar;20(1):11-24. [PubMed: 30535614]
- 7.
Boiko VI, Nikitina IM, Babar TV, Boiko AV. The problem of miscarriage in multiple pregnancy. Wiad Lek. 2018;71(7):1195-1199. [PubMed: 30448784]
- 8.
Yang J, Chen M, Ye X, Chen F, Li Y, Li N, Wu W, Sun J. A cross-sectional survey of pregnant women's knowledge of chromosomal aneuploidy and microdeletion and microduplication syndromes. Eur J Obstet Gynecol Reprod Biol. 2021 Jan;256:82-90. [PubMed: 33176246]
- 9.
Weghofer A, Barad DH, Darmon SK, Kushnir VA, Albertini DF, Gleicher N.
 Euploid miscarriage is associated with elevated serum C-reactive protein levels in infertile women: a pilot study. Arch Gynecol Obstet. 2020 Mar;301(3):831-836. [PMC free article: PMC7060953] [PubMed: 32107607]
Euploid miscarriage is associated with elevated serum C-reactive protein levels in infertile women: a pilot study. Arch Gynecol Obstet. 2020 Mar;301(3):831-836. [PMC free article: PMC7060953] [PubMed: 32107607]- 10.
Devall AJ, Coomarasamy A. Sporadic pregnancy loss and recurrent miscarriage. Best Pract Res Clin Obstet Gynaecol. 2020 Nov;69:30-39. [PubMed: 32978069]
- 11.
Wierzejska R, Wojda B. Folic acid supplementation in pregnancy and prevention of fetal neural tube defects. Przegl Epidemiol. 2020;74(2):362-369. [PubMed: 33115226]
- 12.
du Fossé NA, van der Hoorn MP, van Lith JMM, le Cessie S, Lashley EELO. Advanced paternal age is associated with an increased risk of spontaneous miscarriage: a systematic review and meta-analysis. Hum Reprod Update. 2020 Sep 01;26(5):650-669. [PMC free article: PMC7456349] [PubMed: 32358607]
- 13.
Carp HJA. Progestogens and pregnancy loss. Climacteric. 2018 Aug;21(4):380-384.
 [PubMed: 29565684]
[PubMed: 29565684]- 14.
Wahabi HA, Fayed AA, Esmaeil SA, Bahkali KH. Progestogen for treating threatened miscarriage. Cochrane Database Syst Rev. 2018 Aug 06;8:CD005943. [PMC free article: PMC6513446] [PubMed: 30081430]
- 15.
Pillai RN, Konje JC, Richardson M, Tincello DG, Potdar N. Prediction of miscarriage in women with viable intrauterine pregnancy-A systematic review and diagnostic accuracy meta-analysis. Eur J Obstet Gynecol Reprod Biol. 2018 Jan;220:122-131. [PubMed: 29207325]
- 16.
Xu J, Chen M, Liu QY, Hu SQ, Li LR, Li J, Ma RM. Detecting trisomy in products of conception from first-trimester spontaneous miscarriages by next-generation sequencing (NGS). Medicine (Baltimore). 2020 Jan;99(5):e18731. [PMC free article: PMC7004681] [PubMed: 32000376]
- 17.
Curry A, Williams T, Penny ML. Pelvic Inflammatory Disease: Diagnosis, Management, and Prevention. Am Fam Physician. 2019 Sep 15;100(6):357-364.
 [PubMed: 31524362]
[PubMed: 31524362]- 18.
Stewart KT, Lee JS, Pan K, Albert AY, Fisher S. Outcome of using vaginal misoprostol for treatment of retained products of conception after first trimester miscarriage: a retrospective cohort study. Eur J Contracept Reprod Health Care. 2020 Dec;25(6):474-479. [PubMed: 32869658]
- 19.
Long Y, Zhu H, Hu Y, Shen L, Fu J, Huang W. Interventions for non-tubal ectopic pregnancy. Cochrane Database Syst Rev. 2020 Jul 01;7:CD011174. [PMC free article: PMC7389314] [PubMed: 32609376]
- 20.
Storey A, White K, Treder K, Woodhams E, Bell S, Cannon R. First-Trimester Abortion Complications: Simulation Cases for OB/GYN Residents in Sepsis and Hemorrhage. MedEdPORTAL. 2020 Oct 16;16:10995. [PMC free article: PMC7566226] [PubMed: 33094159]
- 21.
Mj G, K B, R M, G D. Abdominal ectopic pregnancy with implantation on the rectum. Ulster Med J. 2020 Sep;89(2):101-102. [PMC free article: PMC7576386] [PubMed: 33093695]
- 22.

Pereira PP, Cabar FR, Gomez ÚT, Francisco RPV. Pregnancy of unknown location. Clinics (Sao Paulo). 2019;74:e1111. [PMC free article: PMC6784610] [PubMed: 31618321]
- 23.
Yoham AL, Casadesus D. StatPearls [Internet]. StatPearls Publishing; Treasure Island (FL): May 23, 2022. Rho(D) Immune Globulin. [PubMed: 32491807]
- 24.
Gágyor I, Strube-Plaschke S, Rentzsch K, Himmel W. Management of urinary tract infections: what do doctors recommend and patients do? An observational study in German primary care. BMC Infect Dis. 2020 Nov 09;20(1):813. [PMC free article: PMC7650164] [PubMed: 33167875]
- 25.
Milman T, Walker M, Thomas J. Pregnancy of unknown location. CMAJ. 2020 Sep 28;192(39):E1132. [PMC free article: PMC7532014] [PubMed: 32989026]
- 26.
Mayekar RV, Paradkar GV, Bhosale AA, Sachan R, Beeram S, Anand AR, Mundle SR, Trivedi Y, Md R, Patole KP, Sambarey PW, Daftary GV, John J, Divekar GH. Recombinant anti-D for prevention of maternal-foetal Rh(D) alloimmunization: a randomized multi-centre clinical trial.
 Obstet Gynecol Sci. 2020 May;63(3):315-322. [PMC free article: PMC7231934] [PubMed: 32489976]
Obstet Gynecol Sci. 2020 May;63(3):315-322. [PMC free article: PMC7231934] [PubMed: 32489976]- 27.
Zafeiri A, Mitchell RT, Hay DC, Fowler PA. Over-the-counter analgesics during pregnancy: a comprehensive review of global prevalence and offspring safety. Hum Reprod Update. 2021 Jan 04;27(1):67-95. [PubMed: 33118024]
- 28.
Grenache DG. Current Practices When Reporting Quantitative Human Chorionic Gonadotropin Test Results. J Appl Lab Med. 2020 Sep 01;5(5):850-857. [PubMed: 32761058]
- 29.
Ali S, Majid S, Niamat Ali M, Taing S, El-Serehy HA, Al-Misned FA. Evaluation of etiology and pregnancy outcome in recurrent miscarriage patients. Saudi J Biol Sci. 2020 Oct;27(10):2809-2817. [PMC free article: PMC7499272] [PubMed: 32994741]
- 30.
Walsh CA. Maternal activity restriction to reduce preterm birth: Time to put this fallacy to bed. Aust N Z J Obstet Gynaecol. 2020 Oct;60(5):813-815. [PubMed: 32691407]
- 31.
Morin L, Cargill YM, Glanc P. Ultrasound Evaluation of First Trimester Complications of Pregnancy. J Obstet Gynaecol Can. 2016 Oct;38(10):982-988. [PubMed: 27720100]
- 32.
Huchon C, Deffieux X, Beucher G, Capmas P, Carcopino X, Costedoat-Chalumeau N, Delabaere A, Gallot V, Iraola E, Lavoue V, Legendre G, Lejeune-Saada V, Leveque J, Nedellec S, Nizard J, Quibel T, Subtil D, Vialard F, Lemery D., Collège National des Gynécologues Obstétriciens Français. Pregnancy loss: French clinical practice guidelines. Eur J Obstet Gynecol Reprod Biol. 2016 Jun;201:18-26. [PubMed: 27039249]
- 33.
Mellerup N, Sørensen BL, Kuriigamba GK, Rudnicki M. Management of abortion complications at a rural hospital in Uganda: a quality assessment by a partially completed criterion-based audit. BMC Womens Health. 2015 Sep 20;15:76. [PMC free article: PMC4576397] [PubMed: 26388296]
- 34.
Schindler AE, Carp H, Druckmann R, Genazzani AR, Huber J, Pasqualini J, Schweppe KW, Szekeres-Bartho J.
 European Progestin Club Guidelines for prevention and treatment of threatened or recurrent (habitual) miscarriage with progestogens. Gynecol Endocrinol. 2015 Jun;31(6):447-9. [PubMed: 25976550]
European Progestin Club Guidelines for prevention and treatment of threatened or recurrent (habitual) miscarriage with progestogens. Gynecol Endocrinol. 2015 Jun;31(6):447-9. [PubMed: 25976550]- 35.
Diamanti A, Papadakis S, Schoretsaniti S, Rovina N, Vivilaki V, Gratziou C, Katsaounou PA. Smoking cessation in pregnancy: An update for maternity care practitioners. Tob Induc Dis. 2019;17:57. [PMC free article: PMC6770622] [PubMed: 31582946]
- 36.
Shamsi S, Mirza TT, Shejuti TR, Nigar K, Nahar S, Begum S, Sharmin T, Panna LK, Islam N, Jahan T. An Overview of Unsafe Abortion: Patterns and Outcomes in a Tertiary Level Hospital. Mymensingh Med J. 2020 Jul;29(3):523-529. [PubMed: 32844789]
- 37.
Smith C, Hashmi SS, Czerwinski J, Wagner VF, Promecene P, Milentijevic I, Ramdaney A. The impact of genetic counseling on women's grief and coping following termination of pregnancy for fetal anomaly. J Genet Couns. 2021 Apr;30(2):522-532.
 [PubMed: 33103308]
[PubMed: 33103308]- 38.
Bondick CP, M Das J, Fertel H. StatPearls [Internet]. StatPearls Publishing; Treasure Island (FL): Nov 22, 2021. Subchorionic Hemorrhage. [PubMed: 32644443]
- 39.
Ogunyemi D, Haltigin C, Vallie S, Ferrari TM. Evolution of an obstetrics and gynecology interprofessional simulation-based education session for medical and nursing students. Medicine (Baltimore). 2020 Oct 23;99(43):e22562. [PMC free article: PMC7581067] [PubMed: 33120744]
ᐈ Threatened miscarriage - Reproductive medicine, gynecology, pregnancy monitoring, urology
Laser treatment and vaginal rejuvenation
Read more
Once again about hormones or the list of must-haves for the week
Read more
A visit to the urologist. For or Against?
Read more
Preservation of reproductive health
Read more
Pregnancy with uterine fibroids
Read more
Practical skills in examining infertile couples
Read more
Pregnancy with endometriosis: Modern view
Read more
Control against breast cancer
Read more
varicocele and violation of spermatogenesis
Read more
Secretary and obstructive infertility in men
Read more (KOS)
More
Miscarriage.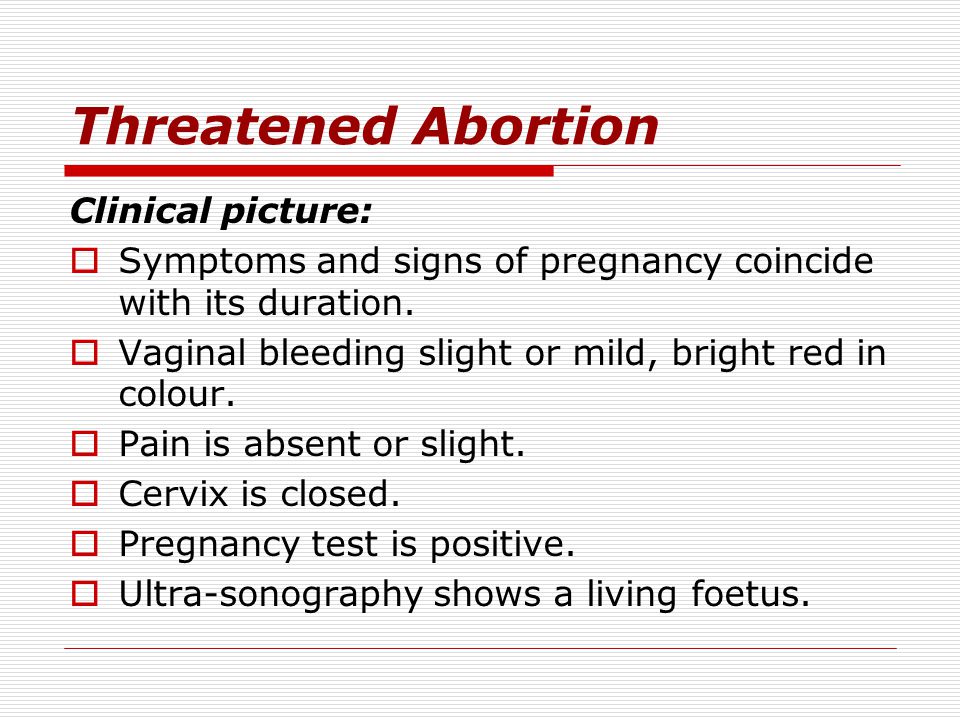 What is the reason?
What is the reason?
More
Hysteroscopy and its role in the treatment of infertility
Read more
Why you can’t get pregnant
Read more
How to calculate the gender of the child before conception
Read more
The obstruction of the uterine pipes
Read ovary hypermostimulation syndrome: modern views on the problem
Read more
Pregnancy with endometriosis - a modern view
Read more
Immunological infertility and the role of antisperm antibodies in it
More
What is cervical pathology?
Read more
Natural cycle IVF: pros and cons
Read more
Practical skills in the examination of infertile couples
Read more
Artificial insemination
Skin whitening and laser removal Read more
Read more
Unable to get pregnant. Where to run? Where to begin?
Where to run? Where to begin?
More
What prospective parents need to know (most popular questions)
More
Endometriosis. Some important questions
Read more
Prolactin increase. Should I be afraid?
Read more
Obstruction of the fallopian tubes, what to do next?
More
Human papillomavirus. Basic information
Read more
KAMALIYA: “I consider Vladimir Kotlik the godfather of my children”
Read more
Infertility and cancer: why men should definitely visit a reproductive specialist
Read more
Sex, children, rock and roll: reproductive specialists on what can increase the chances of IVF
Read more
Portrait of a female doctor: 5 signs of good gynecologist
Read more
Is sex during IVF a good idea?
Read more
Never say never.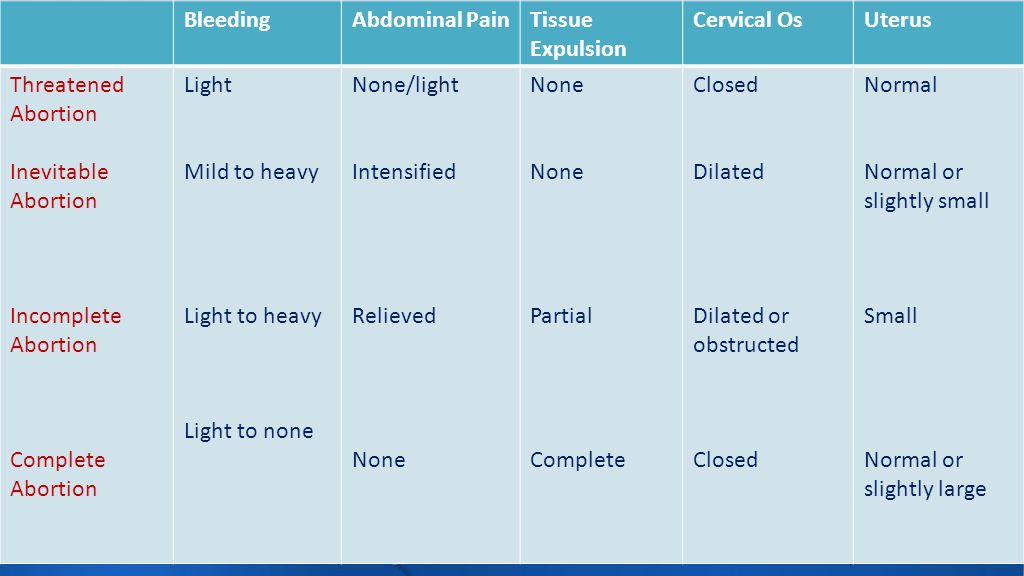 Why childfree is dangerous and why it is worth leaving a “part of yourself” in a cryobank
Why childfree is dangerous and why it is worth leaving a “part of yourself” in a cryobank
More details
How to plan health, longevity and parenthood: practical advice from doctors for 2020
More details
From virus to cancer: hidden threats to women's health
More details
Threatened abortion
Reproductive health of teenage girls: what children and their parents need to knowRead more
Life is like magic: how to believe in a miracle if you are a pragmatist - a doctor's story
Read more
Beautiful skin in youth is the key to happy motherhood
Read more
Charged for success. What determines the effectiveness of ART
More
Why do not all eggs become embryos?
More details
Maxim Gapchuk in "Mother and child" ambitious future
More details
Unsuccessful IVF, how to survive? Expert advice
Read more
What should an Rh-negative woman know?
Read more
9 tips for future parents
Read more
Eco: Modern methods and approaches in the treatment of female infertility
Read more
icSI: Men's infertility - NOT a sentence
Read more
Laparoscopy: Advantages over traditional surgery
Read more
Uterine examination: what you need to know about hysteroscopy
Read more
Artificial intrauterine insemination: the essence of the method, stages and results
Read more
Infertility Diagnostics in men
Read more
10 reasons to contact a man to andrologist
more — what kind of technology is this
More
Premature menopause in men: how to recognize and what is dangerous
More
Why visit a gynecologist for preventive examinations
More details
Laser therapy in gynecology: without anesthesia and pain
More details
Outpatient gynecology - timely seeking qualified help
More details
examinationMore details
Causes and prevention of female infertility
More details
One-day surgery: a modern approach to treatment
3
More details
Pregnancy management: to keep the baby healthy and mother's well-being
More details
Pregnancy after IVF: what future parents need to remember
More details
Anomalies of the uterus and their impact on the onset and carrying of pregnancy.
Read more
Scar on the uterus after caesarean section
Read more
The most common mistakes during pregnancy
Read more
Varicose veins and hemorrhoids during pregnancy
More details
Pregnancy planning (lifestyle)
More details
First aid kit for pregnant women during the war
More details
Periods disappeared during the war. What to do?
More details
Freezing of husband's sperm before the war
More details
A visit to a reproductive specialist during the war
More details
I learned that I was pregnant before the war. What to do?
Read more
What does vaginal discharge mean
Read more
Why can't I get pregnant?
Read more
How to get pregnant if you don't ovulate?
Read more
Diagnosis of male infertility
Read more
When to see a gynecologist
Read more
Infertility treatment program guide
Read more
What you need to know0003
Read more
You are given a chance.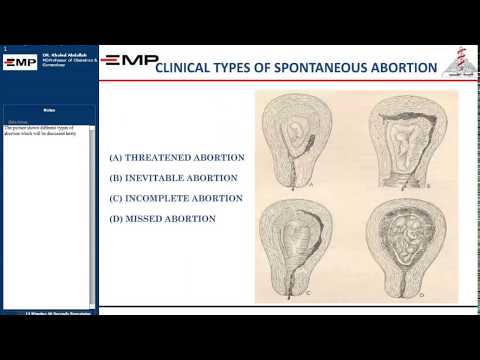 What you need to know about artificial insemination
What you need to know about artificial insemination
Read more
What causes thrush and why it comes back
Read more
Threatened miscarriage – MOSITALMED
If the threat of miscarriage occurs before 22 weeks, then this condition is called a threatened miscarriage. After the 22nd and before the 37th week, the threat of premature birth develops. Pathology can be suspected by the appearance of pain in the lower abdomen, bloody discharge from the vagina and an increase in the tone of the uterus.
The Mositalmed clinic has top-class diagnostic equipment, thanks to which it is possible to determine the cause of the threat of termination of pregnancy, as well as to diagnose even minimal deviations in the health of the mother and fetus.
Causes of a threatened miscarriage
The cause of a threatened miscarriage may be a pathology of the endocrine system in the mother. These include progesterone deficiency, androgen imbalance, thyroid disease, and the presence of a hormone-producing tumor.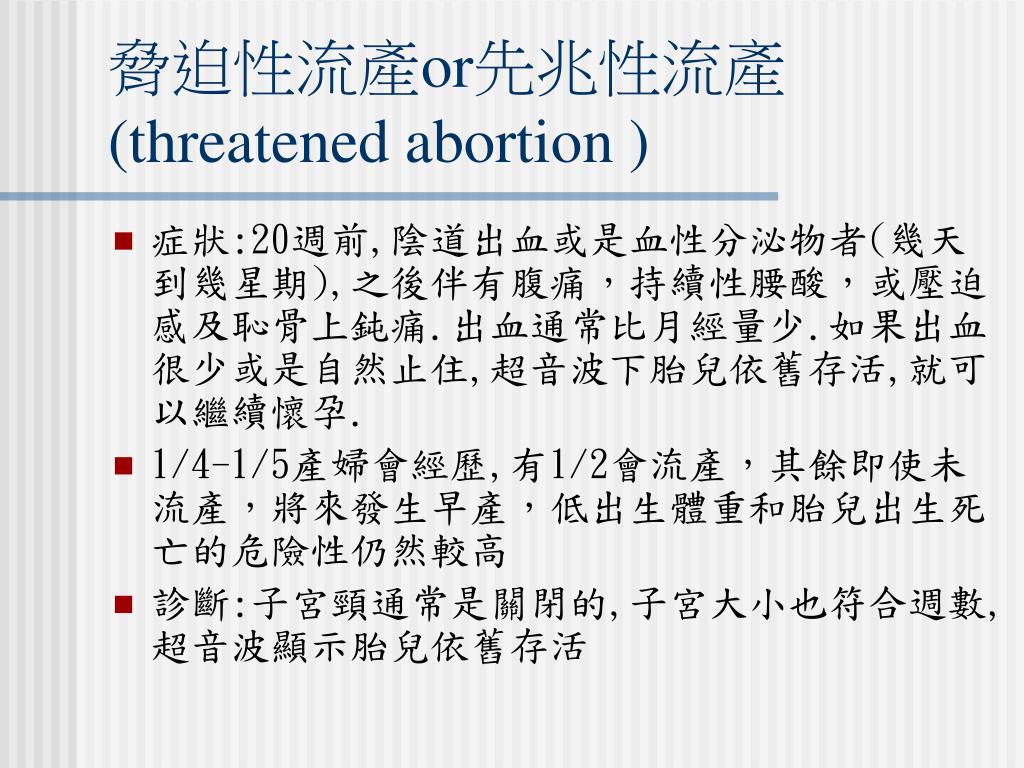
Miscarriage or premature birth can occur when there is insufficient nutrition to the fetus, which leads to its hypoxia. The development of this condition is facilitated by the pathology of the cardiovascular system in a pregnant woman, abruption or placenta previa, preeclampsia and polyhydramnios.
Other reasons for termination of pregnancy include:
- isthmic-cervical insufficiency;
- injuries;
- frequent abortions;
- viral, bacterial or parasitic infections;
- genetic mutations;
- obesity;
- smoking and alcohol abuse;
- taking certain medications;
- autoimmune diseases;
- anomalies in the development of the genital organs in a pregnant woman
Symptoms of a threatened miscarriage
Warning signs of a threatened miscarriage or premature birth are the discharge of blood from the vagina, an increase in the tone of the uterus and pain in the lower abdomen.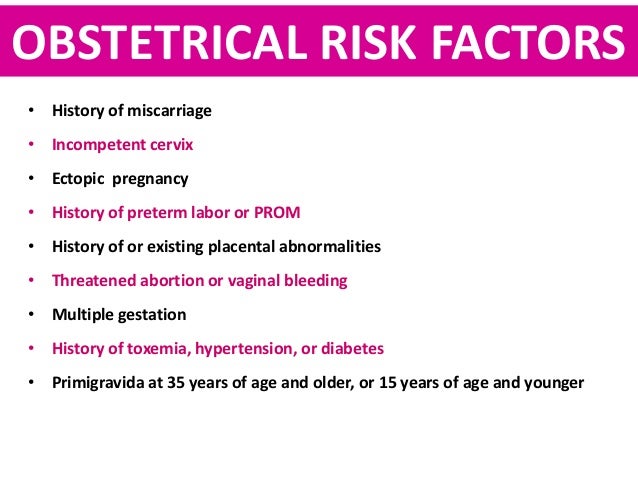 The latter may be aching, pulling or cramping in nature. The pain syndrome is most often localized above the pubis and radiates to the sides or lower back.
The latter may be aching, pulling or cramping in nature. The pain syndrome is most often localized above the pubis and radiates to the sides or lower back.
The amount of bleeding changes with progression from spotting and scanty to copious with clots. This sign is the most dangerous in relation to the life and health of the expectant mother and child. Therefore, with spotting during pregnancy, you should immediately contact a specialist.
Uterine hypertonicity can be suspected by an increase in the abdomen, its induration, and a feeling of fullness in the projection of the uterus.
Diagnosis and treatment of threatened miscarriage
To determine the cause of the threat of termination of pregnancy, an examination on a gynecological chair, laboratory tests and ultrasound of the small pelvis are carried out. At the Mositalmed clinic, based on the results of the examination, our specialists will draw up an individual treatment regimen, taking into account the characteristics of the body of the pregnant woman and the fetus.