Epidural injections for pregnancy
Epidural block - pregnancy: MedlinePlus Medical Encyclopedia
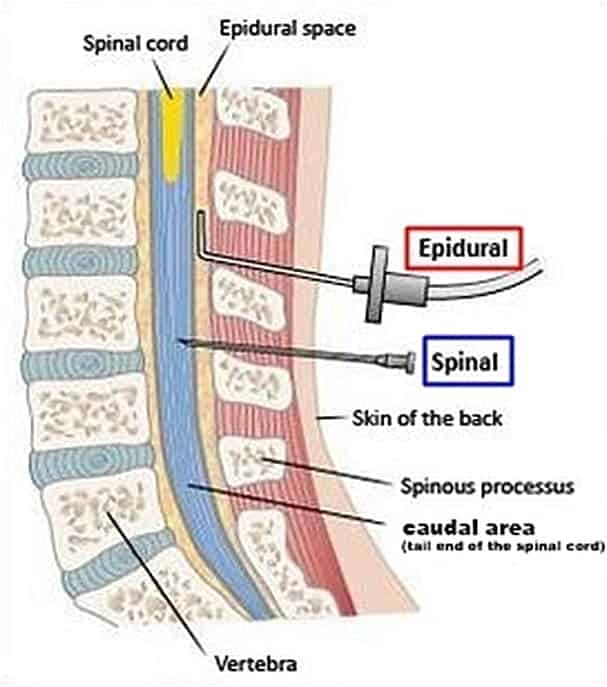
An epidural block is a numbing medicine given by injection (shot) in a specific place in the back. It numbs or causes a loss of feeling in the lower half of your body. This lessens the pain of contractions during childbirth. An epidural block may also be used to reduce pain during surgery on the lower extremities. This article focuses on epidural blocks during childbirth.
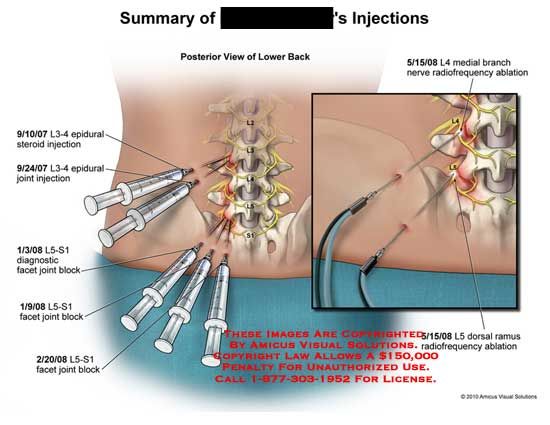
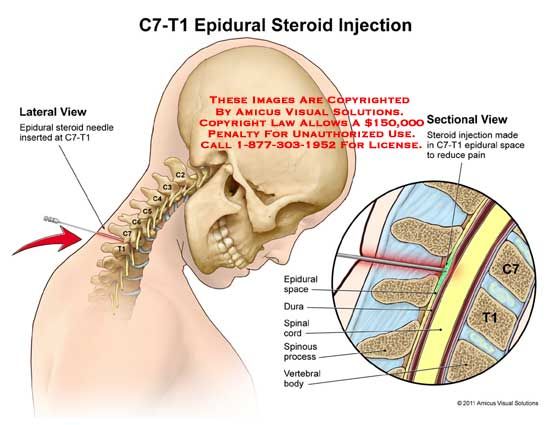
The block or shot is given into an area over your lower back or spine.
- You may be asked to lie on your side, or you may sit up.
- Either way, you will be asked to pull your stomach inward and hunch your back outward.
Your health care provider will wash the area of your back and inject a little medicine to numb the spot where the epidural needle is placed:
- The provider inserts a needle into your lower back.
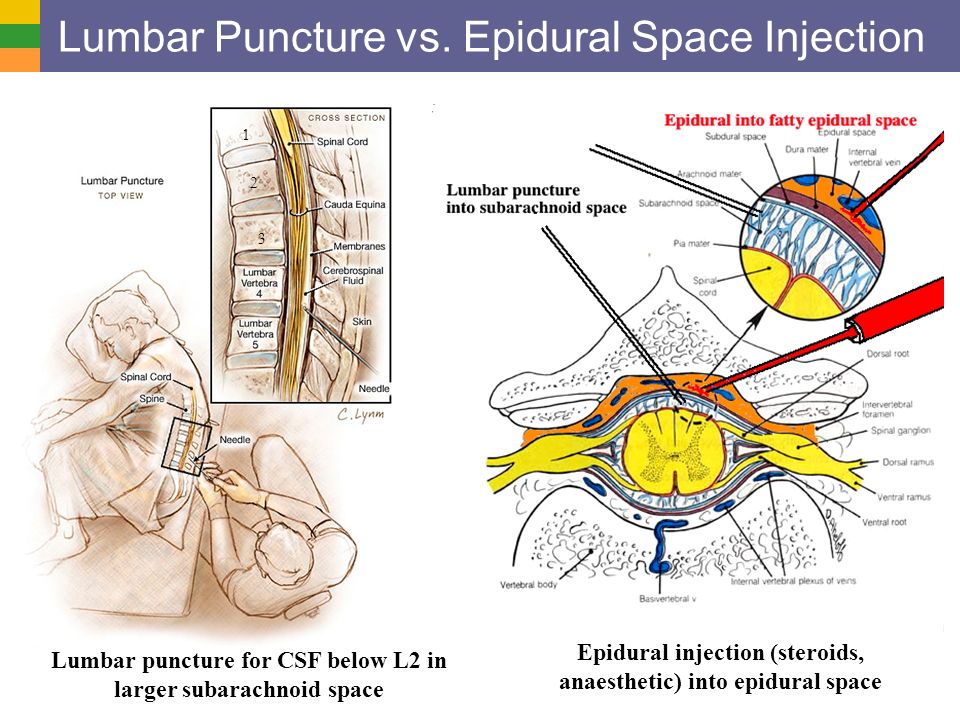
- The needle is placed into a small space outside your spinal cord.
- A small soft tube (catheter) is placed into your back, next to your spine.
- The needle is removed.
The numbing medicine is given through the tube for as long as it is needed.
In most cases, you will receive a low dose because it is safer for you and baby. Once the medicine takes effect (10 to 20 minutes), you should have less pain due to labor. You may still feel some back or rectal pressure during contractions.
You may shiver after an epidural, but this is common. Many women shiver during labor even without an epidural.
Many studies have shown that an epidural is a safe way to manage pain during childbirth. While rare, there are some risks.
Your blood pressure may drop for a short while. This might cause the baby's heart rate to slow down.
- To avoid this, you will receive fluids through an intravenous (IV) line to help keep your blood pressure stable.
- If your blood pressure shows a drop, you may need to lie on your side to keep the blood moving throughout your body.
- Your provider may also give you medicine to raise your blood pressure.

An epidural block may change or alter labor and delivery.
- If you are very numb from the block, you may have a harder time bearing down to push your baby through the birth canal.
- Contractions may lessen or slow down for a little while, but labor will still move along as it should. In some cases, it may even go faster. If your labor slows down, your doctor can give you medicine to speed up your contractions. It is best to wait until you are in active labor to have the epidural placed.
Other rare side effects are:
- You may get a headache after your epidural but this is rare.
- Medicine could enter your spinal fluid. For a short while, it could make you feel dizzy, or you might have a hard time breathing. You could also have a seizure. This is also rare.
There are 2 types:
- "Walking" epidural block. This type of epidural will lessen your pain, but you will still be able to move your legs. Most women are not really able to walk around, but they can move their legs.

- Combined spinal and epidural block. This combines both a spinal and epidural block. It provides pain relief much faster. The combined block is used when women are in very active labor and want relief right away.
Delivery - epidural; Labor - epidural
- Epidural - series
Hawkins JL, Bucklin BA. Obstetric anesthesia. In: Landon MB, Galan HL, Jauniaux ERM, et al, eds. Gabbe's Obstetrics: Normal and Problem Pregnancies. 8th ed. Philadelphia, PA: Elsevier; 2021:chap 16.
Nathan N, Wong CA. Spinal, epidural, and caudal anesthesia: anatomy, physiology, and technique. In: Chestnut DH, Wong CA, Tsen LC, et al, eds. Chestnut's Obstetric Anesthesia: Principles and Practice. 6th ed. Philadelphia, PA: Elsevier; 2020:chap 12.
Sharpe EE, Arendt KW. Anesthesia for obstetrics. In: Gropper MA, ed. Miller's Anesthesia. 9th ed. Philadelphia, PA: Elsevier; 2020:chap 62.
Updated by: John D. Jacobson, MD, Department of Obstetrics and Gynecology, Loma Linda University School of Medicine, Loma Linda, CA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
Browse the Encyclopedia
What is an Epidural | American Pregnancy Association
Epidural anesthesia is the most popular method of pain relief during labor. Women request an epidural by name more than any other method of pain relief. More than 50% of women giving birth at hospitals use epidural anesthesia.
As you prepare yourself for “labor day,” try to learn as much as possible about pain relief options so that you will be better prepared to make decisions during the labor and birth process. Understanding the different types of epidurals, how they are administered, and their benefits and risks will help you in your decision-making during the course of labor and delivery.
Epidural anesthesia is regional anesthesia that blocks pain in a particular region of the body. The goal of an epidural is to provide analgesia, or pain relief, rather than anesthesia, which leads to a total lack of feeling.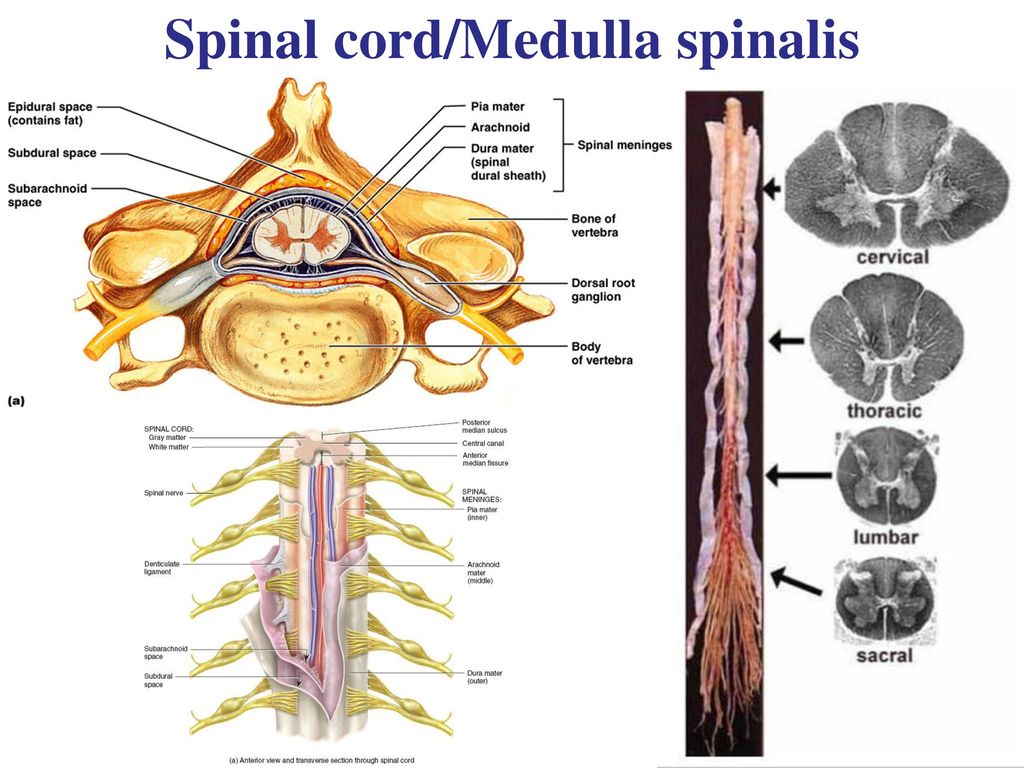 Epidurals block the nerve impulses from the lower spinal segments. This results in decreased sensation in the lower half of the body.
Epidurals block the nerve impulses from the lower spinal segments. This results in decreased sensation in the lower half of the body.
Epidural medications fall into a class of drugs called local anesthetics, such as bupivacaine, chloroprocaine, or lidocaine. They are often delivered in combination with opioids or narcotics such as fentanyl and sufentanil in order to decrease the required dose of local anesthetic.
This produces pain relief with minimal effects. These medications may be used in combination with epinephrine, fentanyl, morphine, or clonidine to prolong the epidural’s effect or to stabilize the mother’s blood pressure.
How is an epidural given?
Intravenous (IV) fluids will be started before active labor begins and prior to the procedure of placing the epidural. You can expect to receive 1-2 liters of IV fluids throughout labor and delivery. An anesthesiologist (specialize in administering anesthesia), an obstetrician or nurse anesthetist will administer your epidural.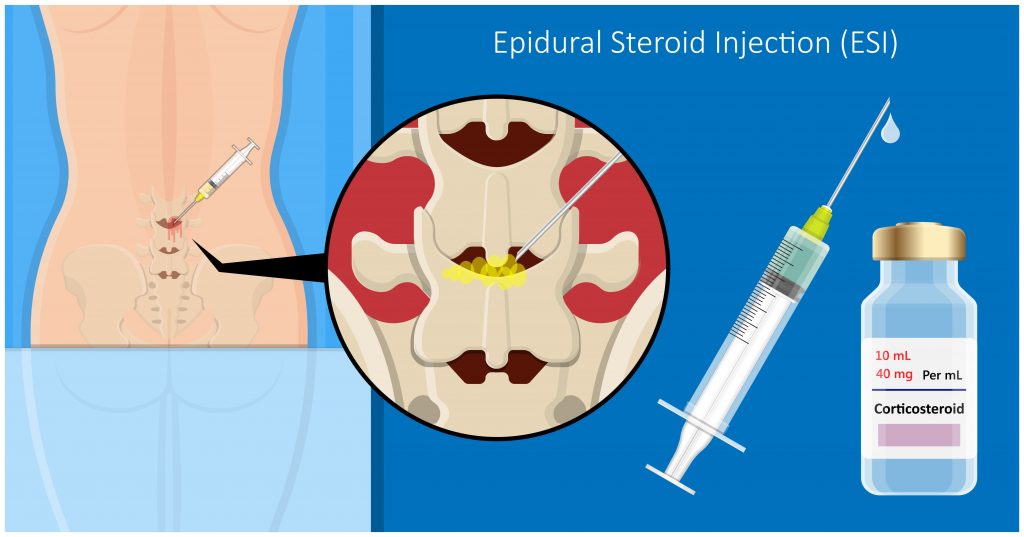
You will be asked to arch your back and remain still while lying on your left side or sitting up. This position is vital for preventing problems and increasing epidural effectiveness.
- An antiseptic solution will be used to wipe the waistline area of your mid-back to minimize the chance of infection. A small area on your back will be injected with a local anesthetic to numb it. A needle is then inserted into the numbed area surrounding the spinal cord in the lower back.
- After that, a small tube or catheter is threaded through the needle into the epidural space. The needle is then carefully removed, leaving the catheter in place to provide medication either through periodic injections or by continuous infusion. The catheter is taped to the back to prevent it from slipping out.
- You’ll start to notice the numbing effect about 10 to 20 minutes after the first dose of medication, though the nerves in your uterus will begin to go numb within a few minutes. You’ll receive continuous doses of medication through the catheter for the rest of your labor.

What are the different types?
There are two basic epidurals in use today. Hospitals and anesthesiologists will differ on the dosages and combinations of medication. You should ask your care providers at the hospital about their practices in this regard.
Regular Epidural
After the catheter is in place, a combination of narcotic and anesthesia is administered either by a pump or by periodic injections into the epidural space. A narcotic such as fentanyl or morphine is given to replace some of the higher doses of anesthetic, like bupivacaine, chloroprocaine, or lidocaine.
This helps reduce some of the adverse effects of the anesthesia. You will want to ask about your hospital’s policies about staying in bed and eating.
Combined Spinal-Epidural (CSE) or “Walking Epidural”
A spinal block is sometimes used in combination with an epidural during labor to provide immediate pain relief. A spinal block, like an epidural, involves an injection in the lower back. While you sit or lie on your side in bed, a small amount of medication is injected into the spinal fluid to numb the lower half of the body. It brings good relief from pain and starts working quickly, but it lasts only an hour or two and is usually given only once during labor. The epidural provides continued pain relief after the spinal block wears off.
While you sit or lie on your side in bed, a small amount of medication is injected into the spinal fluid to numb the lower half of the body. It brings good relief from pain and starts working quickly, but it lasts only an hour or two and is usually given only once during labor. The epidural provides continued pain relief after the spinal block wears off.
What are the benefits of epidural anesthesia?
- An epidural provides a route for very effective pain relief that can be used throughout your labor.
- The anesthesiologist can control the effects by adjusting the type, amount, and strength of the medication. This is important because as your labor progresses and your baby moves down into your birth canal, the dose you’ve been getting might no longer be adequate, or you might suddenly have pain in a different area.
- The medication only affects a specific area, so you’ll be awake and alert during labor and birth. And because you’re pain-free, you can rest (or even sleep!) as your cervix dilates and conserve your energy for when it comes time to push.
- Unlike with systemic narcotics, only a tiny amount of medication reaches your baby.
- Once the epidural is in place, it can be used to provide anesthesia if you need a c-section or if you’re having your tubes tied after delivery.
What are the risks of epidural anesthesia?
- You have to stay still for 10 to 15 minutes while the epidural is put in, and then wait up to 20 minutes before the medication takes full effect.
- Epidurals may cause your blood pressure to suddenly drop. For this reason, your blood pressure will be routinely checked to help ensure adequate blood flow to your baby. If there is a sudden drop in blood pressure, you may need to be treated with IV fluids, medications, and oxygen.
- You may experience a severe headache caused by leakage of spinal fluid. Less than 1% of women experience this side effect. If symptoms persist, a procedure called a “blood patch”, which is an injection of your blood into the epidural space can be performed to relieve a headache.
- After your epidural is placed, you will need to alternate sides while lying in bed and have continuous monitoring for changes in fetal heart rate. Lying in one position can sometimes cause labor to slow down or stop.
- You might experience the following side effects: shivering, a ringing of the ears, backache, soreness where the needle is inserted, nausea, or difficulty urinating.
- You might find that your epidural makes pushing more difficult and additional medications or interventions may be needed, such as forceps or cesarean. Talk to your doctor when creating your birth plan about what interventions he or she generally uses in such cases.
- For a few hours after the birth, the lower half of your body may feel numb. Numbness will require you to walk with assistance.
In rare instances, permanent nerve damage may result in the area where the catheter was inserted. - Though research is somewhat ambiguous, most studies suggest that some babies will have trouble “latching on” causing breastfeeding difficulties.
 Other studies suggest that a baby might experience respiratory depression, fetal malpositioning, and an increase in fetal heart rate variability, thus increasing the need for forceps, vacuum, cesarean deliveries, and episiotomies.
Other studies suggest that a baby might experience respiratory depression, fetal malpositioning, and an increase in fetal heart rate variability, thus increasing the need for forceps, vacuum, cesarean deliveries, and episiotomies.
How Long Does an Epidural Last?
Once the catheter is in place, the anaesthetist can set up an epidural pump. The pump feeds the epidural solution into the catheter continuously, providing pain relief for as long as needed.
The type, amount and strength of the anaesthetic can be adjusted, as necessary. You might also be given the option of having control of the medication pump. This is called patient controlled analgesia. The amount of painkiller is still regulated, so you can’t accidentally overdose.
You can have the dose lowered for second stage pushing, but it takes some time for the pain relief and numbness to wear off, so if this is important to you, discuss it with your care provider early on.
Common Questions About Epidurals
Does the placement of epidural anesthesia hurt?The answer depends on who you ask. Some women describe an epidural placement as creating a bit of discomfort in the area where the back was numbed, and a feeling of pressure as the small tube or catheter was placed.
Some women describe an epidural placement as creating a bit of discomfort in the area where the back was numbed, and a feeling of pressure as the small tube or catheter was placed.
Typically epidurals are placed when the cervix is dilated to 4-5 centimeters and you are in true active labor.
Can an epidural slow labor or lead to a cesarean delivery (C-section)?There is no credible evidence that it does either. When a woman needs a C-section, other factors usually are at play, including the size or position of the baby or slow progression of labor due to other issues. With an epidural, you might be able to feel contractions — they just won’t hurt — and you’ll be able to push effectively. There is some evidence that epidurals can speed the first stage of labor by allowing the mother to relax.
How can an epidural affect my baby?As previously stated, research on the effects of epidurals on newborns is somewhat ambiguous, and many factors can affect the health of a newborn.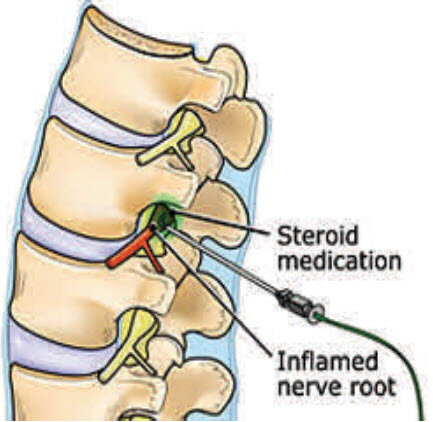 How much of an effect these medications will have is difficult to predetermine and can vary based on dosage, the length of labor, and the characteristics of each individual baby.
How much of an effect these medications will have is difficult to predetermine and can vary based on dosage, the length of labor, and the characteristics of each individual baby.
Since dosages and medications can vary, concrete information from research is currently unavailable. One possible side effect of an epidural with some babies is a struggle with “latching on” in breastfeeding. Another is that while in-utero, a baby might also become lethargic and have trouble getting into position for delivery.
These medications have also been known to cause respiratory depression and decreased fetal heart rate in newborns. Though the medication might not harm these babies, they may have subtle effects on the newborn.
How will I feel after the placement of an epidural?The nerves of the uterus should begin to numb within a few minutes after the initial dose. You will probably feel the entire numbing effect after 10-20 minutes. As the anesthetic dose begins to wear off, more doses will be given–usually every one to two hours.
Depending on the type of epidural and dosage administered, you can be confined to your bed and not allowed to get up and move around.
If labor continues for more than a few hours you will probably need urinary catheterization, because your abdomen will be numb, making urinating difficult. After your baby is born, the catheter is removed and the effects of the anesthesia will usually disappear within one or two hours.
Some women report experiencing an uncomfortable burning sensation around the birth canal as the medication wears off.
Will I be able to push?You might not be able to tell that you are having a contraction because of your epidural anesthesia. If you can not feel your contractions, then pushing may be difficult to control. For this reason, your baby might need additional help coming down the birth canal. This is usually done by the use of forceps.
Does an epidural always work?For the most part, epidurals are effective in relieving pain during labor. Some women complain of being able to feel pain, or they feel that the drug worked better on one side of the body.
Some women complain of being able to feel pain, or they feel that the drug worked better on one side of the body.
An epidural may not be an option to relieve pain during labor if any of the following apply:
- You use blood thinners
- Have low platelet counts
- Are hemorrhaging or in shock
- Have an infection on or in your back
- Have a blood infection
- If you are not at least 4 cm dilated
- Epidural space cannot be located by the physician
- If labor is moving too fast and there is not enough time to administer the d
Questions to ask your healthcare providers now and at the time of delivery in the hospital:
- What combination and dosage of drugs will be used?
- How could the medications affect my baby?
- Will I be able to get up and walk around?
- What liquids and solid foods will I be able to consume?
Want to Know More?
- Nitrous Oxide During Labor
- Stages of Labor: Stage 1
- Inducing Labor
- Cord Blood Banking: Your Three Choices Explained
Compiled using information from the following sources:
1. American Academy of Family Physicians
American Academy of Family Physicians
https://www.aafp.org
2. William’s Obstetrics Twenty-Second Ed. Cunningham, F. Gary, et al, Ch. 19.
3. Mayo Clinic Guide To A Healthy Pregnancy Harms Roger W., M.D., et al, Part 2.
Epidural analgesia in childbirth - REGIONAL PERINATAL CENTER
The use of epidural analgesia during childbirth is becoming popular because of the convenience it provides. An epidural block reduces sensation in the lower parts of the body, but does not affect consciousness. The stage of labor at which an epidural is used may differ from patient to patient. If you need an epidural, your obstetrician and anesthesiologist will need to evaluate you and your baby, history of past anesthesias, and the progress of your labor. The most frequently asked questions when performing epidural analgesia in labor are:
When is epidural analgesia performed?
The time to start epidural analgesia is determined by the obstetrician and anesthesiologist, depending on the needs of the mother and baby during labor.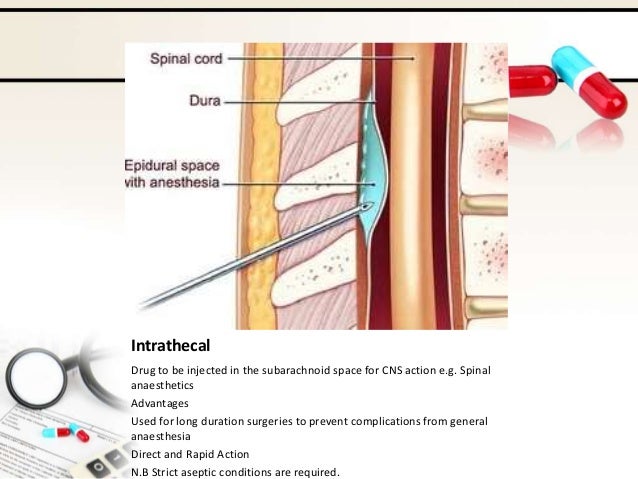
How is an epidural block performed?
Epidural lumbar anesthesia is performed in the lower back with the patient sitting or lying on her side. Anesthesia is performed below the level where the spinal cord ends.
Before performing the block, the skin is treated with an antiseptic solution. The anesthesiologist then performs local anesthesia of the skin at the puncture site. After that, a special needle is inserted into the epidural space of the spine, slightly short of the spinal space. An epidural catheter, which is a thin, flexible tube, is inserted through the needle. Sometimes the catheter can touch a nerve, causing a shooting sensation in the leg. nine0003
Next, the needle is removed and the catheter is attached to the back. Subsequent injections will no longer require a second puncture, but are made through a catheter. An epidurally administered local anesthetic is thought to provide an epidural block by bathing the spinal nerves.
How soon does an epidural block occur and how long does it last?
The start of the block is gradual and slow. Pain relief usually develops 10-20 minutes after epidural administration and may be continued until the end of labor as additional doses of drugs can be administered through the epidural catheter. After delivery, the catheter is removed and after a few hours your sensations return to normal. nine0003
Pain relief usually develops 10-20 minutes after epidural administration and may be continued until the end of labor as additional doses of drugs can be administered through the epidural catheter. After delivery, the catheter is removed and after a few hours your sensations return to normal. nine0003
How does an epidural block feel?
With a significant reduction in pain, there may be a feeling of pressure during contractions and vaginal examination by an obstetrician. There may be transient numbness, weakness, and heaviness in the legs.
Do I need to stay in bed after an epidural?
Usually, during analgesia, you are warned not to get out of bed and lie on your back for more than 10 minutes during labor. However, it is believed that maintaining the vertical position of the body contributes to the favorable course of childbirth. There is a type of epidural analgesia that allows you to sit and walk. This type of analgesia is called "walking epidural" or ambulatory, mobile epidural. nine0003
nine0003
Does epidural analgesia affect the child?
Studies show that epidural analgesia is safe for mother and child.
Will an epidural block slow down labor?
In some patients, during the action of epidural analgesia, contractions may weaken for a short time. Most patients note that epidural analgesia helps them relax, while at the same time, uterine contractility improves.
Will the ability to push remain? nine0005
Epidural analgesia will allow you to relax and maintain strength during the longest part of labor - when the cervix opens. In the pushing period of childbirth, if properly applied, it will not affect the attempts and even make them more pleasant.
What are the possible side effects of epidural analgesia?
Rarely, even with careful monitoring and precautions by the anesthetist, complications or side effects may occur. The most common complications are arterial hypotension and headache. More severe complications are a toxic reaction to local anesthetics, respiratory arrest, and neurological disorders. They are extremely rare. nine0003
They are extremely rare. nine0003
Lowering blood pressure. You will receive intravenous fluids to prevent this complication. In addition, during delivery, you usually need to lie on your side, and after delivery, you need to stay in bed until the block wears off.
Headache occurs infrequently, in about 0.7-1.4% of cases. Maintaining the required position during the puncture helps to prevent its occurrence. When a headache occurs, simple measures are usually effective: bed rest, fluids, and pain medications. If pain persists, additional treatment may be required. nine0003
Chills is a common reaction during childbirth, but may also occur during anesthesia. Warming helps a lot.
Itchy skin is mild in most cases, but if it becomes unbearable, it can be cured by the administration of drugs.
Difficulty breathing , very rarely anesthesia can affect the intercostal muscles and make breathing difficult. In this case, the condition of the woman in labor will facilitate the administration of oxygen. nine0003
In this case, the condition of the woman in labor will facilitate the administration of oxygen. nine0003
Reaction to local anesthetics is rare but can be serious. During pregnancy, the veins passing through the epidural space dilate, and therefore there is a risk of intravascular injection. In order to avoid unwanted reactions, the anesthesiologist initially administers a test dose of the drug and asks the woman in labor to pay attention to the possibility of dizziness, metallic taste, palpitations or numbness.
Insufficient anesthesia. nine0046 Sometimes the effect of the anesthetic is "mosaic" or one-sided. The anesthetist may change your position in bed or pull up your epidural catheter. Rarely, repeat epidural anesthesia may be required.
The anesthesia anesthetist evaluates your condition and takes precautions during the procedure. You can discuss with him the possibilities of pain relief and your concerns about it.
When should epidurals not be used? nine0005
Contraindications to the use of epidural anesthesia are:
- bleeding disorders or the use of anticoagulants,
- generalized infection or infection at the puncture site,
- bleeding,
- patient refusal,
- severe neurological disease,
- heart disease with fixed cardiac output.

The Department of Anesthesiology and Intensive Care provides labor pain relief using epidural analgesia to all patients who need this pain relief. When performing analgesia, modern disposable sets for epidural blockade made in Germany, anesthetic Naropin made in Great Britain are used. All doctors of the department are fluent in this method of labor pain relief. Additional information can be obtained from the head of the department or an anesthesiologist working with obstetric patients. nine0003
Rational anticoagulant therapy in pregnancy
Currently, the treatment of pregnant women with drugs that affect the hemostasis system is widespread. It is difficult to find a patient who would not have been prescribed dipyridamole for 40 weeks of pregnancy. The practice of "correction" of some indicators of the hemostasiogram with anticoagulants is spreading. The duration of treatment, the combination of drugs used are determined differently, often quite arbitrarily, and there are no laboratory methods for monitoring treatment that prove the effectiveness and safety of anticoagulant dosages.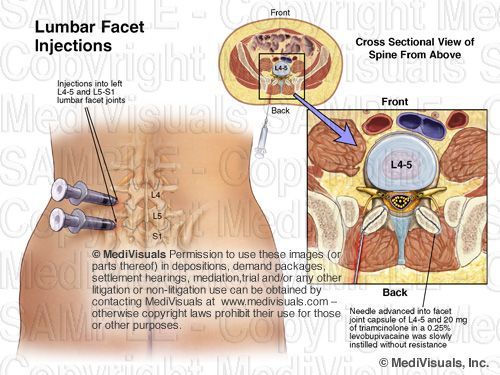 Last but not least is the cost of treatment. The physiological response of the body to pregnancy is hypercoagulation in the procoagulant link of the hemostasis system, probably with an adequate response of the anticoagulant link, which is difficult to assess due to the limited capabilities of modern clinical biology. It is important that the levels of hypercoagulation markers do not correlate with the level of clinical risk of thrombosis in pregnant women at high risk of developing venous thromboembolism (VTE) [7]. nine0003
Last but not least is the cost of treatment. The physiological response of the body to pregnancy is hypercoagulation in the procoagulant link of the hemostasis system, probably with an adequate response of the anticoagulant link, which is difficult to assess due to the limited capabilities of modern clinical biology. It is important that the levels of hypercoagulation markers do not correlate with the level of clinical risk of thrombosis in pregnant women at high risk of developing venous thromboembolism (VTE) [7]. nine0003
Rational anticoagulant therapy of pregnant women seems to us to be a system of treatment according to certain indications with appropriate laboratory control to correct homeostasis in pregnant women and prevent obstetric complications, thrombosis and bleeding. It is supposed to use dosages of drugs, the pharmacological action of which is well known, for the period necessary to realize the therapeutic effect.
Over the past 3 decades, there has been a strong upward trend in maternal mortality from VTE. In addition, in most industrialized countries, the age of women giving birth is increasing, and the proportion of pregnant women suffering from severe extragenital pathology is growing. The successes of modern medicine lead to an increase in the life expectancy of patients and contribute to the onset of pregnancy in women with systemic connective tissue diseases, oncological diseases, pathology of the cardiovascular system, respiratory organs, endocrine pathology, diseases of the blood system, antiphospholipid syndrome, etc. Proper diagnosis and treatment can improve perinatal outcomes in severe pregnancy complications such as recurrent miscarriage, intrauterine growth retardation syndrome, preeclampsia. All of these situations are associated with the intensification of intravascular thrombosis both in the vascular bed of the pregnant woman and in the system of the utero-placental-fetal blood flow, so the use of coagulologically active substances is pathogenetically justified. When prescribing anticoagulants, it should be remembered that the mechanisms of thrombosis are different in the arterial and venous sections of the vascular bed, in macrovessels and in the microcirculation system (distal to the level of the precapillary sphincter).
In addition, in most industrialized countries, the age of women giving birth is increasing, and the proportion of pregnant women suffering from severe extragenital pathology is growing. The successes of modern medicine lead to an increase in the life expectancy of patients and contribute to the onset of pregnancy in women with systemic connective tissue diseases, oncological diseases, pathology of the cardiovascular system, respiratory organs, endocrine pathology, diseases of the blood system, antiphospholipid syndrome, etc. Proper diagnosis and treatment can improve perinatal outcomes in severe pregnancy complications such as recurrent miscarriage, intrauterine growth retardation syndrome, preeclampsia. All of these situations are associated with the intensification of intravascular thrombosis both in the vascular bed of the pregnant woman and in the system of the utero-placental-fetal blood flow, so the use of coagulologically active substances is pathogenetically justified. When prescribing anticoagulants, it should be remembered that the mechanisms of thrombosis are different in the arterial and venous sections of the vascular bed, in macrovessels and in the microcirculation system (distal to the level of the precapillary sphincter). nine0003
Pregnant women eligible for anticoagulant therapy include:
1) deep vein thrombosis and pulmonary embolism during present pregnancy,
2) mechanical heart valves,
3) antiphospholipid syndrome (if correctly diagnosed),
4) in thrombophilia: antithrombin-III defect, combination of hereditary thrombophilias such as protein S and C deficiency, resistance to activated protein C due to FV Leiden mutation, hyperprothrombinemia due to prothrombin G20210A mutation, hyperhomocysteinemia, mutation in plasminogen activator inhibitor I type,
5) manifestation of arterial thrombosis,
6) non-developing pregnancy and a decrease in the number of platelets and / or fibrinogen in preparation for emptying the uterine cavity,
7) fetoplacental insufficiency confirmed by fetometry, Doppler and/or hormonal studies and/or cardiotocography.
The purpose of anticoagulant treatment is to prevent thromboembolic complications, bleeding, improve blood circulation in the mother-placenta-fetus system, ensure an uncomplicated course and prolong pregnancy. nine0003
nine0003
In our opinion, the necessary and sufficient method for the prevention of thromboembolic disease (TED) is the use of a risk assessment point scale and the appointment of anticoagulant prophylaxis, as is practiced in general surgical practice [9].
A score of 1 point is given at age over 40 years, body weight over 80 kg, history of abdominal surgery less than 6 months after, significant varicose veins of the lower extremities, recent immobilization. 2 points are assessed for bed rest for more than 3 days, chronic obstructive pulmonary disease in a severe stage, inflammation of the intestinal tract, severe infection (pneumonia), condition after delivery (within 1 month), use of oral contraceptives or hormone replacement therapy. The presence of oncological disease, heart failure, myocardial infarction less than 3 months ago, and a history of a TEB episode are assessed as 3 points. With a score of 5 or more, enoxaparin is prescribed prophylactically at a dose of 40 mg once subcutaneously until the patient is completely mobilized, the duration of treatment is up to 2 weeks. nine0003
nine0003
VTE risk factors in pregnant women combine 2 groups [14]. The 1st group includes factors related to the patient herself: age over 35 years, obesity (body mass index over 29 kg/m 2 ) in early pregnancy, thrombophilia, history of venous thromboembolism, pronounced varicose veins of the lower extremities, serious extragenital diseases, such as nephrotic syndrome, the presence of an infection or inflammatory process, immobilization, paraplegia, physical inactivity during long journeys, dehydration, intravenous drug use, ovarian hyperstimulation syndrome. The 2nd group includes factors that make pregnancy complications: caesarean section, especially emergency in a woman in labor, operative delivery through the natural birth canal, massive obstetric bleeding, vomiting of pregnant women, preeclampsia. nine0003
More than 12 years ago, a work [23] appeared on significantly greater perinatal losses in patients with such types of thrombophilia as deficiency of antithrombin-III, protein S, protein C, FV Leiden mutation.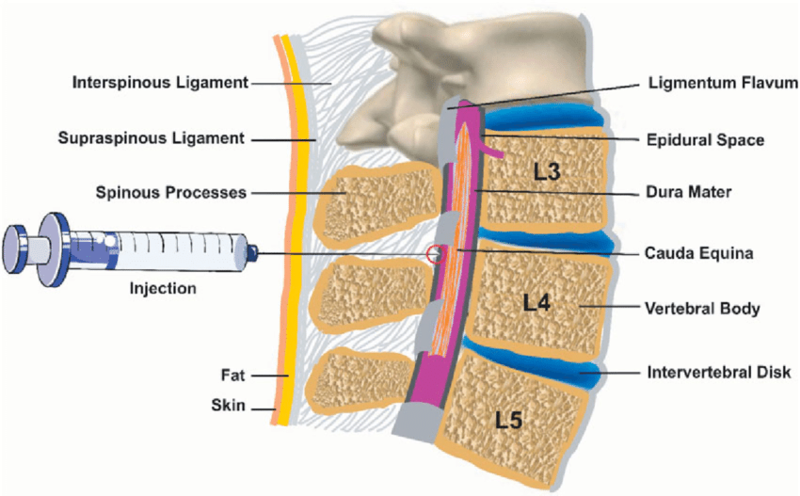
M. de Swiet [29] draws attention to the age of pregnant women and an increase in the frequency of TEB in pregnant women over 40 years old (100 times compared to the group aged 20-25 years). Additional risk factors are overweight and a history of more than 3 pregnancies, operative delivery (caesarean section), suppression of lactation by estrogens. Antenatal risk factors for PE include in vitro fertilization, gestational diabetes, multiple pregnancies, and maternal age over 35, and postnatal risk factors include preeclampsia, eclampsia, placenta previa, placental abruption, and caesarean section [17] . nine0003
The method of confirming the diagnosis of deep vein thrombosis in pregnant women is compression ultrasonography, and pulmonary embolism - ventilation-perfusion scanning of the lungs [13]. The low specificity of D-dimer does not allow the use of this laboratory indicator in pregnant women as a laboratory test for confirmation of PEP [11, 13, 22].
When determining the treatment regimen, the following conditions must be observed: firstly, the safety of the drug for the fetus and mother; secondly, the effectiveness of the applied treatment and/or prophylaxis regimen; thirdly, dosages for the initial course of treatment and maintenance therapy during pregnancy, childbirth and the postpartum period [13].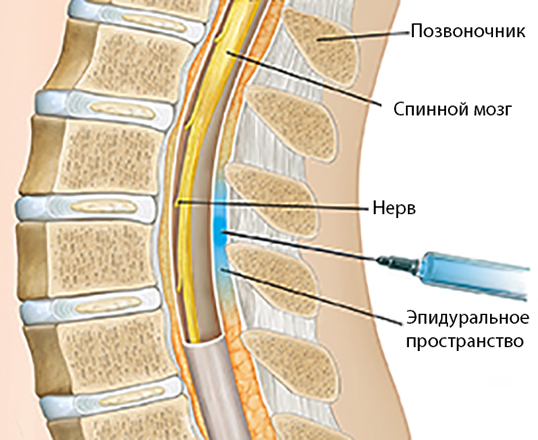 nine0003
nine0003
Consider the most commonly used anticoagulant drugs used in obstetric practice.
Unfractionated heparin (UFH). UFH is obtained from the intestinal mucosa of pigs or from the lungs of cattle. Drugs from different companies have their own characteristics of pharmacodynamics, which, however, is leveled by the fact that the dosage of the drug is selected depending on the reaction of the patient's hemocoagulation system.
A. Continuous intravenous administration.
The success of UFH treatment depends on a sufficient initial dose, which should be at least 30,000-35,000 IU/day [13]. This treatment regimen is used in acute cases with mandatory monitoring of the efficacy and safety of treatment using a laboratory test - an indicator of activated partial thromboplastin time (APTT) [29].
B. Intermittent subcutaneous injection [13]:
nine0002 a) mini-doses of UFH: 5000 IU every 12 hours without laboratory control; b) moderate doses of UFH: subcutaneously every 12 hours with control of changes in the content of antifactor Xa to 0. 1-0.3 U/ml 6 hours after injection;
1-0.3 U/ml 6 hours after injection;
c) adapted doses of UFH: subcutaneously every 12 hours, monitoring changes in the APTT to values exceeding 1.5-2 times normal, 6 hours after injection.
V. Inhalation [1].
Indications for heparin inhalation:
1) prevention of obstetric complications: preeclampsia, fetoplacental insufficiency;
2) presence of preeclampsia of mild or moderate severity;
3) decompensated diabetes mellitus;
4) treatment of fetoplacental insufficiency.
Inhalations are carried out using an ultrasonic inhaler, diluting heparin with distilled water 1:4, inhalations are carried out 2 times a day with an interval of 12 hours. In the prevention of preeclampsia, the daily dose is 300 U / kg, the duration of the course is 7 days, 2-3 courses are required, the interval between courses is 2 days, it is necessary to stop treatment 10 days before delivery; for other indications, the daily dose is 500 U / kg, the duration of the course is 21 days, the number of courses is 1-2, the interval between courses is 2 weeks, it is necessary to stop treatment 14 days before delivery. nine0003
nine0003
Low molecular weight heparins (LMWH). LMWHs (Table 1) are obtained by depolymerization of UFH with nitrous acid, either by induction of a benzyl ring and alkaline hydrolysis, or by depolymerization from amyl nitrate, or by peroxidation and, finally, cleavage with heparinase [26].
In general, rational heparin therapy is presented in Table. 2.
Like UFH, LMWHs do not cross the placental barrier into milk, are safe for the fetus, and are considered the treatment of choice for VTE in pregnant women [10, 13]. nine0003
Prophylactic dose of LMWH tinzaparin, according to K. Khasia et al. [18] should be 4500 IU/day for patients weighing less than 100 kg and 5000 IU/kg for patients weighing more than 100 kg. The authors believe that the final dose of LMWH should be determined taking into account antifactor Xa activity.
In 2001-2005 the main LMWH used during pregnancy in Denmark was tinzaparin - 95.2% of cases, and dalteparin sodium accounted for 4.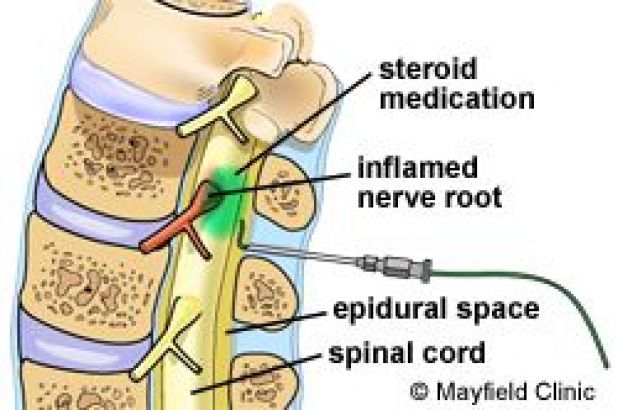 8% [4]. According to A. Andersen et al. [4], indications for treatment of pregnant women with low molecular weight heparins in Denmark were an episode of thromboembolism with/or without thrombophilia - 37.3%, perinatal losses and congenital thrombophilia - 35%, recurrent miscarriage and congenital thrombophilia - 7.2%, other causes - 20 ,five%. nine0003
8% [4]. According to A. Andersen et al. [4], indications for treatment of pregnant women with low molecular weight heparins in Denmark were an episode of thromboembolism with/or without thrombophilia - 37.3%, perinatal losses and congenital thrombophilia - 35%, recurrent miscarriage and congenital thrombophilia - 7.2%, other causes - 20 ,five%. nine0003
Taking into account the poor perinatal outcomes for mother and fetus in patients with antithrombin III deficiency, S. Schulman [27] recommends the administration of UFH in a dosage that can increase the APTT to 1.3-1.5 reference values after 5 years in order to prevent thrombotic complications. -6 hours after injection with three subcutaneous injections or the use of LMWH with an activity index of antifactor Xa equal to 0.1-0.2 U / ml.
Antivitamin K (warfarin). The use of antivitamin K in pregnant women is limited by physicians' fear of possible teratogenic effects of the drugs and the risk of bleeding in both the mother and the fetus. The disadvantages of drugs should also be considered a delayed onset of action and aftereffect of the drug, an unpredictable clinical effect depending on the dose, which requires laboratory monitoring, a narrow "therapeutic corridor", multiple interactions with drugs and foods that change the effect of the drug [5]. Antivitamin K is used in pregnant women with artificial heart valves, with allergic reactions to heparin, in the presence of a high titer of antiphospholipid antibodies [29]. Antivitamin K is not secreted into breast milk and can be used in lactating women [16].
The disadvantages of drugs should also be considered a delayed onset of action and aftereffect of the drug, an unpredictable clinical effect depending on the dose, which requires laboratory monitoring, a narrow "therapeutic corridor", multiple interactions with drugs and foods that change the effect of the drug [5]. Antivitamin K is used in pregnant women with artificial heart valves, with allergic reactions to heparin, in the presence of a high titer of antiphospholipid antibodies [29]. Antivitamin K is not secreted into breast milk and can be used in lactating women [16].
When comparing anticoagulant therapy regimens in pregnant women with an artificial heart valve, the smallest number of thromboembolic and hemorrhagic complications was noted with the tactics of using heparin in early pregnancy and during organogenesis up to 12 weeks, then when transferring pregnant women to indirect anticoagulants with a return to heparin therapy before childbirth [ 24]. nine0003
Many drugs interfere with the effectiveness of antivitamin K; enhance the effect of drugs such as erythromycin, co-trimoxazole, fluconazole, isoniazid, metronidazole, amiodarone, clofibrate, propafenone, propranolol, sulfinperazone, phenylbutazone, piroxicam, ethyl alcohol, cimetidine, omeprazole. Weaken the action of antivitamins K griseofulvin, nafcillin, rifampin, cholestyramine, barbiturates, carbamazepine, chlordiazepoxide, sucralfate [15].
Weaken the action of antivitamins K griseofulvin, nafcillin, rifampin, cholestyramine, barbiturates, carbamazepine, chlordiazepoxide, sucralfate [15].
Aspirin. nine0140 The action of aspirin is the irreversible inhibition of cyclooxygenase, which damages the synthesis of thromboxane A 2 and the metabolism of prostaglandins. At the same time, platelet aggregation induced by collagen, adenosine diphosphate, thrombin, and thromboxane A 2 decreases [6].
Aspirin treatment is usually given in conjunction with heparin therapy. The effectiveness of the use of 75 mg of aspirin with subcutaneous administration of 5000 units of heparin with an interval of 12 hours or in combination with the use of parnaparin LMWH at a dose of 0.3 ml subcutaneously in patients with antiphospholipid antibodies and recurrent miscarriage to improve perinatal parameters has been proven [25]. nine0003
Japanese researchers in 20 confirmed observations of VTE in pregnant women (up to 30 weeks) used UFH with APTT control to select an adequate dose, followed by switching to low doses of aspirin after the disappearance of the thrombus; at the same time, none of the patients used the installation of a filter in the inferior vena cava. The need to continue anticoagulant treatment after the disappearance of thrombosis is absent in the Japanese population due to the fact that there is no resistance to activated protein C [21]. nine0003
The need to continue anticoagulant treatment after the disappearance of thrombosis is absent in the Japanese population due to the fact that there is no resistance to activated protein C [21]. nine0003
A significant issue in clinical practice is the tactics of using anticoagulants during and after childbirth. Most researchers recommend the abolition of heparin 24 hours before labor induction in programmed labor, and in the group of very high risk of developing thromboembolic complications, intravenous administration of UFH is canceled 4-6 hours before labor induction; with an excessive dosage of heparin, it is possible to use a solution of protamine sulfate, the resumption of anticoagulant therapy is possible 12 hours after delivery [13]. In high-risk groups (for example, the first episode of PE during pregnancy, a mechanical heart valve with thrombosis, multiple congenital thrombophilia with venous thrombosis), heparin therapy in childbirth is acceptable, for example, subcutaneously at 7500 IU 2 times a day [29]. In prolonged labor for more than 18 hours and if labor does not occur within the next 3 hours, it is possible to use a prophylactic dose of LMWH [16]. An original system has been developed [19], which provides anticoagulation during childbirth in high-risk patients receiving LMWH at a therapeutic dose, without the risk of hemorrhagic complications.
In prolonged labor for more than 18 hours and if labor does not occur within the next 3 hours, it is possible to use a prophylactic dose of LMWH [16]. An original system has been developed [19], which provides anticoagulation during childbirth in high-risk patients receiving LMWH at a therapeutic dose, without the risk of hemorrhagic complications.
On the eve of a programmed delivery or a planned caesarean section, an infusomat infusion of a solution of UFH 15,000 U / 24 h - 625 U / h is started, and the subcutaneous injection of the drug is canceled in the evening. nine0003
4 hours before delivery (with the onset of the active phase of labor) or epidural analgesia for abdominal delivery, the infusion is stopped and resumed 2-4 hours after delivery.
Laboratory monitoring of anticoagulant treatment.
Use of APTT. With continuous intravenous heparin monitoring, the APTT should be increased 1.5 to 2 times normal after 6 hours of therapy. nine0003
Determination of activity index of antifactor Xa. The difficulty of using LMWH in clinical practice is due to the fact that these drugs can have significant antithrombotic activity in vivo without showing an anticoagulant effect in a laboratory study in vitro [26].
The difficulty of using LMWH in clinical practice is due to the fact that these drugs can have significant antithrombotic activity in vivo without showing an anticoagulant effect in a laboratory study in vitro [26].
Monitoring of treatment with LMWH is carried out monthly, while the level of antifactor Xa should be 0.5-1.2 U / ml (maximum value - 3-4 hours after injection) with a double prescription of the drug and 1.0-2.0 U /ml if the drug is administered once a day [13, 16]. If the level of activity of antifactor Xa is less than 0.4 U / ml, the patient will not experience heparin-induced bleeding [29].
In the presence of artificial mechanical heart valves in pregnant women with two subcutaneous injections of LMWH, peak concentrations of antifactor Xa should be 0.7-0.8 U / ml and echocardiography should be performed in parallel [2].
The prophylactic dose of tinzaparin should be 0.5-0.8 U/ml within 2 hours after injection, and at a small dose, they switch to dose selection according to the above indicator [18].
There is an opinion [28] about the low predictive value of determining the activity of antifactor Xa in relation to the progression of thrombosis and the risk of bleeding. nine0003
Monitoring treatment with indirect anticoagulants-antivitamins K. The international normalized ratio (INR, international normalized ratio ) is currently used to monitor treatment with warfarin. INR is the ratio of the patient's prothrombin time to the control prothrombin time, raised to the power of the international index of sensitivity of the thromboplastin used. These complexities are needed to standardize the laboratory thromboplastin reagent, which makes it possible to compare INR values obtained anywhere in the world. To prevent thrombosis, the INR should be 2–3, with the exception of patients with mechanical heart valves and antiphospholipid syndrome, in whom this indicator should correspond to 3–4 [20]. nine0003
Complications of anticoagulant therapy. Complications of heparin treatment include bleeding, heparin-induced thrombocytopenia, and osteoporosis [13]. M. Damodaran et al. [10] reported more blood loss during childbirth and a significantly greater number of congenital malformations in fetuses of pregnant women treated with LMWH, therefore, according to the authors, LMWH treatment should be based on clear clinical indications.
M. Damodaran et al. [10] reported more blood loss during childbirth and a significantly greater number of congenital malformations in fetuses of pregnant women treated with LMWH, therefore, according to the authors, LMWH treatment should be based on clear clinical indications.
There were no cases of thromboembolic episodes or significant hematomas in 166 observations of long-term use of LMWH, as well as fractures due to osteoporosis with good perinatal parameters, although 96% of cases had increased blood loss after childbirth [4].
Until now, the issue of prophylactic treatment with anticoagulants remains open. They are increasingly being used to improve perinatal pregnancy outcomes in vascular placental complications [8]. To address the issue of prophylactic use of anticoagulants in pregnant women, they are divided into high and low risk groups. In the absence of other risk factors, a recurrent episode of thrombosis or thromboembolism in pregnant women has a probability of occurrence equal to 12%, therefore, observation is either limited or aspirin is prescribed in low (up to 100 mg / day) doses. High-risk patients have more than one episode of VTE per pregnancy, thrombophilia, and a family history of PE. Such patients are given subcutaneous injections of UFH or LMWH from the moment pregnancy is confirmed [29]. The prophylactic use of LMWH and its effectiveness were evaluated by M. Aldea et al. [3] in 14,624 pregnant women. Risk factors were obesity, the presence of varicose veins, uterine fibroids, arterial hypertension, cardiopathy, episodes of venous thrombosis in history. 22% of patients received prophylactic treatment with LMWH, treatment with anticoagulants was canceled 12 hours before and resumed 12 hours after delivery. The authors attribute the ineffectiveness of heparin prophylaxis (4 cases of venous thrombosis against the background of the use of drugs) to the use of a low dose of the drug (once a day) and pay attention to the use of LMWH according to indications - with existing risk factors, so as not to excessively increase the cost of treatment. The question of the dosage of heparin in its prophylactic use in patients with congenital antithrombin deficiency is raised in the publication of I.
High-risk patients have more than one episode of VTE per pregnancy, thrombophilia, and a family history of PE. Such patients are given subcutaneous injections of UFH or LMWH from the moment pregnancy is confirmed [29]. The prophylactic use of LMWH and its effectiveness were evaluated by M. Aldea et al. [3] in 14,624 pregnant women. Risk factors were obesity, the presence of varicose veins, uterine fibroids, arterial hypertension, cardiopathy, episodes of venous thrombosis in history. 22% of patients received prophylactic treatment with LMWH, treatment with anticoagulants was canceled 12 hours before and resumed 12 hours after delivery. The authors attribute the ineffectiveness of heparin prophylaxis (4 cases of venous thrombosis against the background of the use of drugs) to the use of a low dose of the drug (once a day) and pay attention to the use of LMWH according to indications - with existing risk factors, so as not to excessively increase the cost of treatment. The question of the dosage of heparin in its prophylactic use in patients with congenital antithrombin deficiency is raised in the publication of I. Dubedal et al. [12]: total doses of LMWH were 2500-17500 IU/day; at a daily dose of less than 7500 IU / day, more than 50% of pregnant women developed thromboembolic complications, at a higher dose - in 15% (significant difference). nine0003
Dubedal et al. [12]: total doses of LMWH were 2500-17500 IU/day; at a daily dose of less than 7500 IU / day, more than 50% of pregnant women developed thromboembolic complications, at a higher dose - in 15% (significant difference). nine0003
Contraindications for heparin therapy:
1) thrombocytopenia - the content of platelets is less than 100 10 9 /l;
2) arterial hypertension - systolic blood pressure above 160 mm Hg. Art.;
3) vascular or parenchymal bleeding;
4) acidosis - decrease in the expected anticoagulant effect;
5) liver and kidney failure.
Therefore, anticoagulant therapy in pregnant women should be clinically indicated in groups of patients at high risk of VTE or to improve perinatal outcomes in the current pregnancy. Monitoring of treatment with anticoagulants is not carried out in the case of inhalation therapy with heparin, the use of mini-doses of UFH with subcutaneous administration up to 15,000 IU/day, intravenous administration up to 20,000 IU/day, prophylactic treatment of LMWH with one dose per day.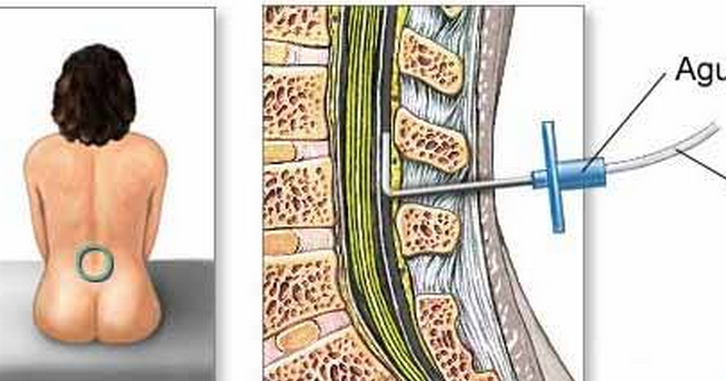 The control is carried out using a certain laboratory test at a certain time with subcutaneous injection of UFH - control over the change in APTT to a level exceeding the norm by 1.5-2 times after 4-6 hours from the moment of injection of the drug, with subcutaneous administration of LMWH, the activity of antifactor Xa is controlled through 4-6 hours after injection to a level of 0.3-0.6 or 0.6-1.2 U / ml, depending on the therapy regimen, warfarin treatment is carried out under the control of INR up to levels of 1.5-2.5, depending on groups of patients. A promising, reliable and convenient method of treating pregnant women is the use of warfarin, except for periods from 5 to 15 weeks of pregnancy (the period of organogenesis) and the period before delivery, given the long half-life of the drug. Treatment with aspirin or chimes at the risk of developing VTE is not pathogenetically justified and should not be used. Anticoagulant therapy should be used when indicated and for a long time, sometimes throughout pregnancy.
The control is carried out using a certain laboratory test at a certain time with subcutaneous injection of UFH - control over the change in APTT to a level exceeding the norm by 1.5-2 times after 4-6 hours from the moment of injection of the drug, with subcutaneous administration of LMWH, the activity of antifactor Xa is controlled through 4-6 hours after injection to a level of 0.3-0.6 or 0.6-1.2 U / ml, depending on the therapy regimen, warfarin treatment is carried out under the control of INR up to levels of 1.5-2.5, depending on groups of patients. A promising, reliable and convenient method of treating pregnant women is the use of warfarin, except for periods from 5 to 15 weeks of pregnancy (the period of organogenesis) and the period before delivery, given the long half-life of the drug. Treatment with aspirin or chimes at the risk of developing VTE is not pathogenetically justified and should not be used. Anticoagulant therapy should be used when indicated and for a long time, sometimes throughout pregnancy.