Breast infections not breastfeeding
Breast Infection (Mastitis): Symptoms, Causes, Treatments
Written by WebMD Editorial Contributors
In this Article
- How the Breast Is Built
- Breast Infection Causes
- Breast Infection Symptoms
- When to Seek Medical Care
- Breast Infection Exams and Tests
- Breast Infection Treatment
- Breast Infection Home Remedies
- Medications for Mastitis
- Surgery for an Abscess
- Next Steps
- Follow-Up Care After a Breast Infection
- Mastitis Prevention
- Outlook for Breast Infections
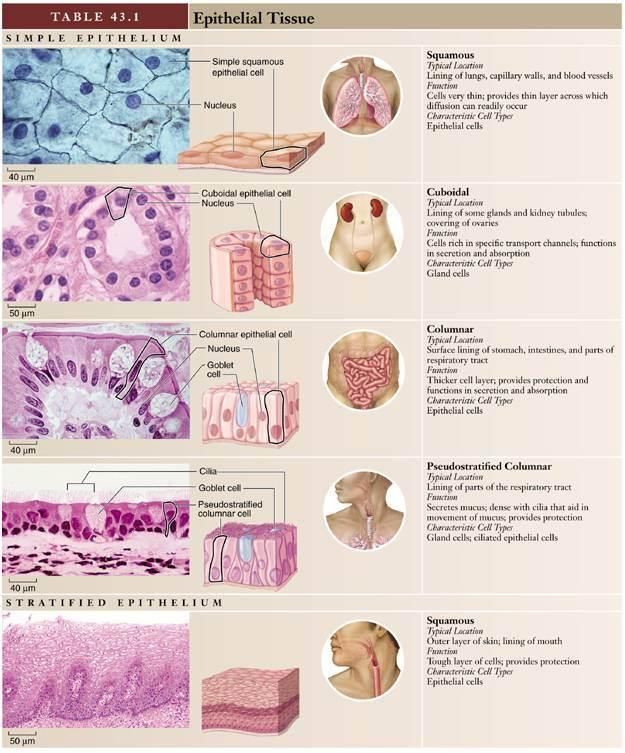
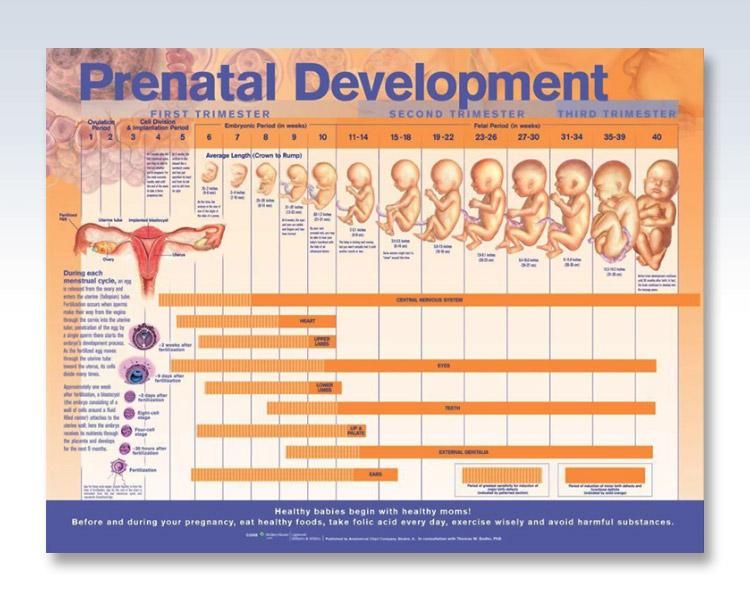
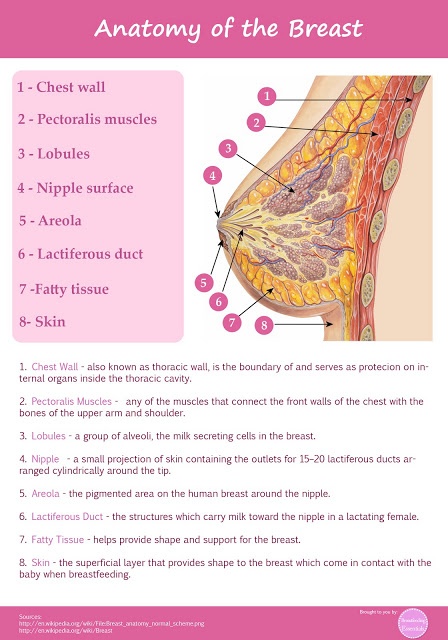
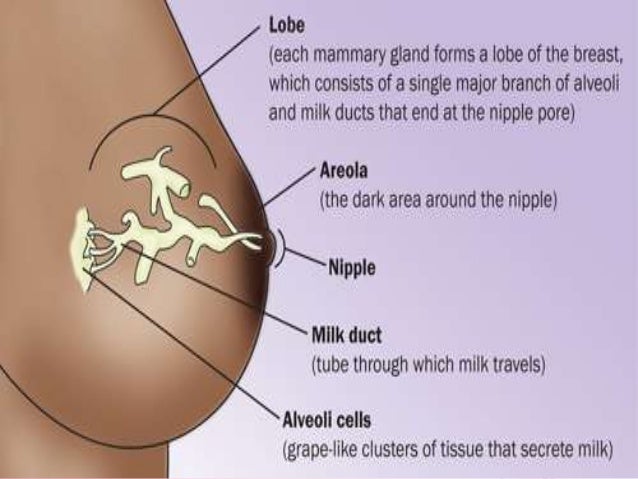
How the Breast Is Built
The breast is composed of several glands and ducts that lead to the nipple and the surrounding colored area called the areola. The milk-carrying ducts extend from the nipple into the underlying breast tissue like the spokes of a wheel. Under the areola are lactiferous ducts. These fill with milk during lactation after a woman has a baby. When a girl reaches puberty, changing hormones cause the ducts to grow and cause fat deposits in the breast tissue to increase. The glands that produce milk (mammary glands) that are connected to the surface of the breast by the lactiferous ducts may extend to the armpit area.
Breast Infection Causes
Mastitis is an infection of the tissue of the breast that occurs most frequently during the time of breastfeeding. It can occur when bacteria, often from the baby's mouth, enter a milk duct through a crack in the nipple.
Breast infections most commonly occur one to three months after the delivery of a baby, but they can occur in women who have not recently delivered and in women after menopause. Other causes of infection include chronic mastitis and a rare form of cancer called inflammatory carcinoma.
In healthy women, mastitis is rare. However, women with diabetes, chronic illness, AIDS, or an impaired immune system may be more susceptible.
About 1%-3% of breastfeeding mothers develop mastitis. Engorgement and incomplete breast emptying can contribute to the problem and make the symptoms worse.
Chronic mastitis occurs in women who are not breastfeeding. In postmenopausal women, breast infections may be associated with chronic inflammation of the ducts below the nipple. Hormonal changes in the body can cause the milk ducts to become clogged with dead skin cells and debris. These clogged ducts make the breast more open to bacterial infection. Infection tends to come back after treatment with antibiotics.
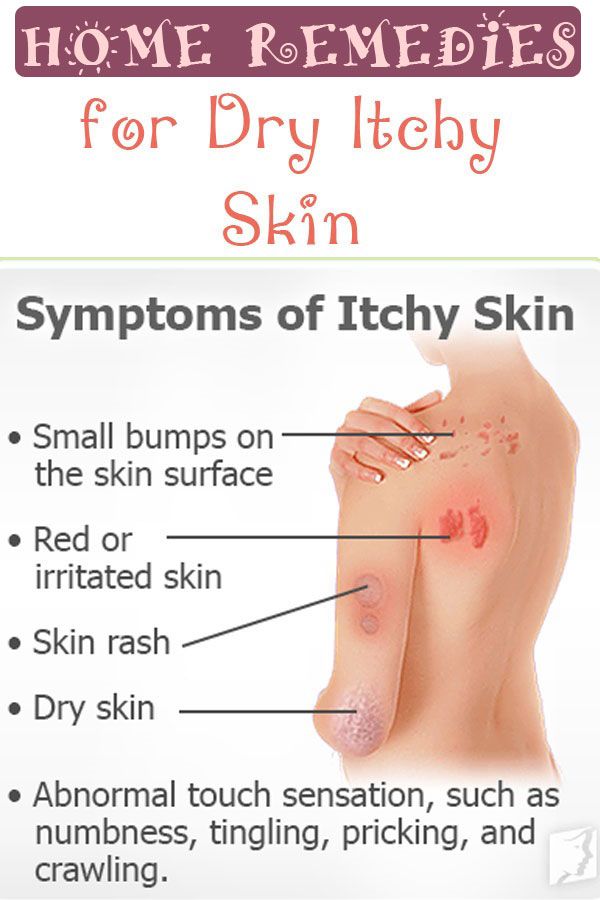
Breast Infection Symptoms
Breast infections may cause pain, redness, and warmth of the breast along with the following symptoms:
- Tenderness and swelling
- Body aches
- Fatigue
- Breast engorgement
- Fever and chills
- Abscess: A breast abscess can be a complication of mastitis. Noncancerous masses such as abscesses are more often tender and frequently feel mobile beneath the skin. The edge of the mass is usually regular and well defined. Indications that this more serious infection has occurred include the following:
- Tender lump in the breast that does not get smaller after breastfeeding a newborn (If the abscess is deep in the breast, you may not be able to feel it.
 )
) - Pus draining from the nipple
- Persistent fever and no improvement of symptoms within 48-72 hours of treatment
- Tender lump in the breast that does not get smaller after breastfeeding a newborn (If the abscess is deep in the breast, you may not be able to feel it.
When to Seek Medical Care
Call your health care provider as soon as you feel any suspicious lump, whether you are breastfeeding or not. Call for an appointment if:
- You have any abnormal discharge from your nipples.
- Breast pain is making it difficult for you to function each day.
- You have prolonged, unexplained breast pain.
- You have any other associated symptoms such as redness, swelling, pain that interferes with breastfeeding, a mass or tender lump in the breast that does not disappear after breastfeeding.
- If you are breastfeeding, call your doctor if you develop any symptoms of breast infection so that treatment may be started promptly.
You may need to be evaluated in a hospital's emergency department if the breast pain is associated with other signs of an infection (such as a fever, swelling, or redness to the breast) and if your health care provider cannot see you promptly.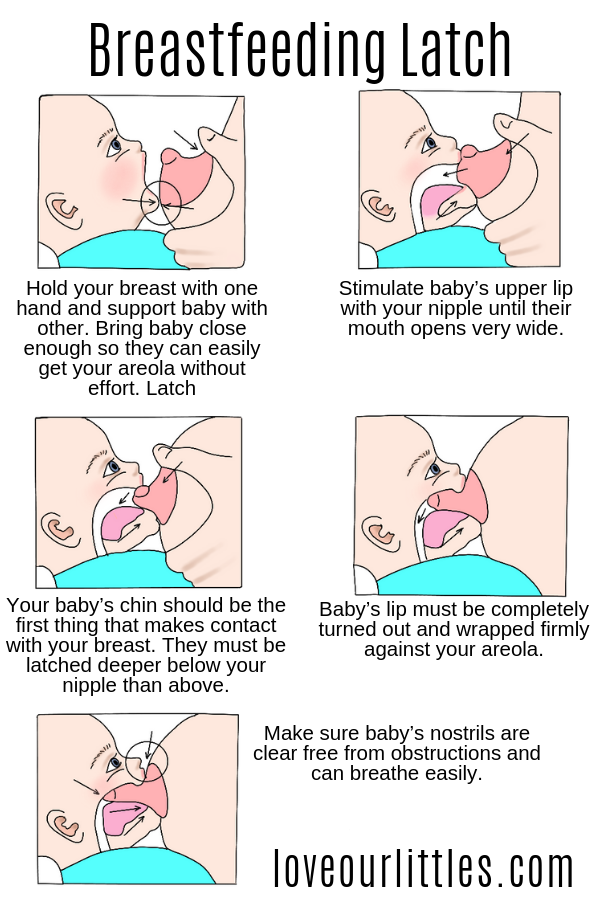 The below symptoms require emergency treatment:
The below symptoms require emergency treatment:
- A persistent high fever greater than 101.5°F
- Nausea or vomiting that is preventing you from taking the antibiotics as prescribed
- Pus draining from the breast
- Red streaks extending toward your arm or chest
- Dizziness, fainting, or confusion
Breast Infection Exams and Tests
The diagnosis of mastitis and a breast abscess can usually be made based on a physical exam.
- If it is unclear whether a mass is due to a fluid-filled abscess or to a solid mass such as a tumor, a test such as an ultrasound may be done. An ultrasound may also be helpful in distinguishing between simple mastitis and abscess or in diagnosing an abscess deep in the breast. This noninvasive test allows your doctor to directly visualize the abscess by placing an ultrasound probe over your breast. If an abscess is confirmed, aspiration or surgical drainage, and IV antibiotics, are often required.
- Cultures may be taken, either of breast milk or of material taken out of an abscess through a syringe, to determine the type of organism causing the infection.
 This information can help your doctor decide what kind of antibiotic to use.
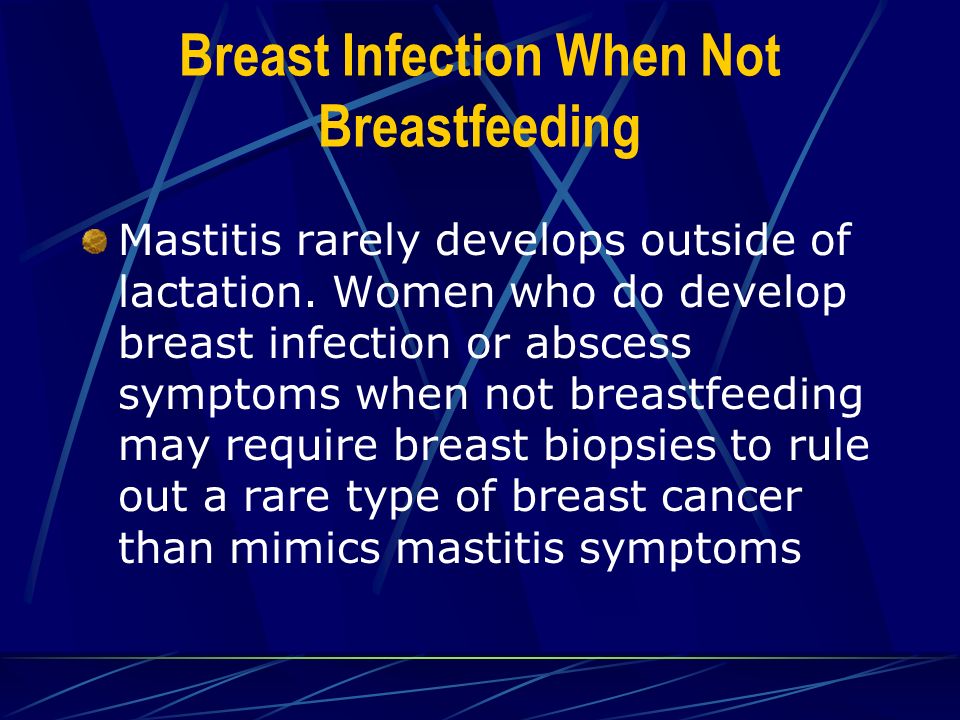
This information can help your doctor decide what kind of antibiotic to use. - Nonbreastfeeding women with mastitis, or those who do not respond to treatment, may have a mammogram or breast biopsy. This is a precautionary measure because a rare type of breast cancer can produce symptoms of mastitis.
Breast Infection Treatment
Breast infections require treatment by a health care provider.
Breast Infection Home Remedies
After you see a doctor, try the following to help your breast infection heal.
- Pain medication: Take acetaminophen (Tylenol) or ibuprofen (such as Advil) for pain. These drugs are safe while breastfeeding and will not harm your baby. Your doctor may prescribe a prescription strength pain reliever if your pain is severe and not relieved with over-the-counter medication.
- In mild cases of mastitis, antibiotics may not be prescribed at all. If you are prescribed antibiotics, finishing the prescription even if you feel better in a few days is very important.
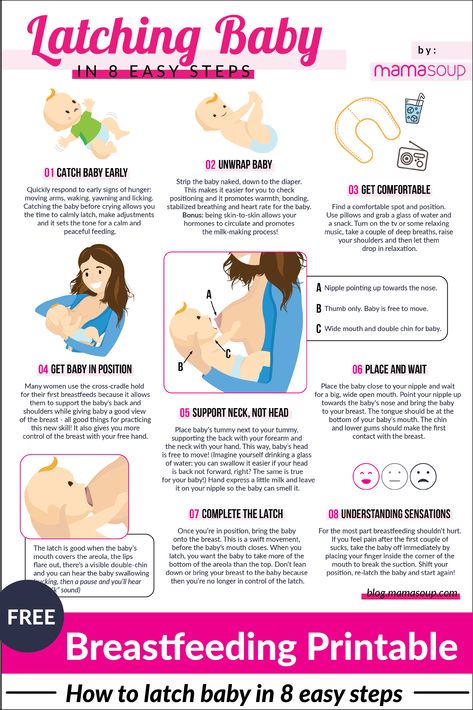
- Frequent feedings: Do not stop breastfeeding from the affected breast, even though it will be painful and you may be taking antibiotics. Frequent emptying of the breast prevents engorgement and clogged ducts that can only make mastitis worse.
- If needed, use a breast pump to relieve pressure and completely empty the breast.
- You can also breastfeed from the unaffected side and supplement with infant formula as needed.
- The infection will not harm the baby because the germs that caused the infection probably came from the baby’s mouth in the first place.
- Breastfeeding should be avoided in the infected breast when an abscess is present.
- Pain relief: A warm compress applied before and after feedings can often provide some relief. A warm bath may work as well.
- If heat is ineffective, ice packs applied after feedings may provide some comfort and relief.
- Avoid using ice packs just before breastfeeding because it can slow down milk flow.
- Drink plenty of water -- at least 10 glasses a day. Eat well-balanced meals and add 500 extra calories a day while breastfeeding. Dehydration and poor nutrition can decrease milk supply and make you feel worse.
Medications for Mastitis
For simple mastitis without an abscess, oral antibiotics are prescribed. Cephalexin (Keflex) and dicloxacillin (Dycill) are two of the most common antibiotics chosen, but a number of others are available. The antibiotic prescribed will depend on your specific situation, your doctor’s preference, and any drug allergies you may have. This medicine is safe to use while breastfeeding and will not harm the baby.
Chronic mastitis in nonbreastfeeding women can be complicated. Recurrent episodes of mastitis are common. Occasionally, this type of infection responds poorly to antibiotics. Therefore, close follow-up with your doctor is mandatory.
If the infection worsens in spite of oral antibiotics or if you have a deep abscess requiring surgical treatment, you may be admitted to the hospital for IV antibiotics.
Surgery for an Abscess
If an abscess is present, it must be drained. After injection of a local anesthetic, the doctor may drain an abscess near the surface of the skin either by aspiration with a needle and syringe or by using a small incision. This can be done in the doctor’s office or emergency department.
If the abscess is deep in the breast, however, it may require surgical drainage in the operating room. This procedure is usually done under general anesthesia to minimize pain and completely drain the abscess. Antibiotics and heat on the area are also used to treat abscesses.
Next Steps
Mastitis does not cause cancer, but cancer can mimic mastitis in appearance. If a breast infection is slow to go away, your health care provider may recommend a mammogram or other tests to rule out cancer.
Follow-Up Care After a Breast Infection
If you have a breast infection, you may be seen for a recheck in 24-48 hours.
- Take all antibiotics as prescribed.
- Take your temperature three times a day for the first 48 hours after treatment begins. Watch for fever.
- Call your doctor if you develop a high fever, vomiting, or increasing redness, swelling, or pain in the breast.
- Follow up with your doctor in one to two weeks to make sure that the infection has gone away. If the infection spreads or an abscess develops, you may require IV antibiotics or surgical treatment.
Mastitis Prevention
Sometimes mastitis is unavoidable. Some women are more susceptible than others, especially those who are breastfeeding for the first time. In general, good habits to prevent mastitis include the following:
- Breastfeed equally from both breasts.
- Empty breasts completely to prevent engorgement and blocked ducts.
- Use good breastfeeding techniques to prevent sore, cracked nipples.
- Allow sore or cracked nipples to air dry.
- Prevent moisture from accumulating in breast pads or bras.
- Avoid dehydration by drinking plenty of fluids.

- Practice careful hygiene: Handwashing, cleaning the nipples, keeping your baby clean.
Outlook for Breast Infections
When treated promptly, the majority of breast infections go away quickly and without serious complications. Most women can and should continue to breastfeed despite an episode of uncomplicated mastitis. With proper treatment, symptoms should begin to resolve within one to two days.
A breast abscess may require surgical drainage, IV antibiotics, and a short hospital stay. A small incision is made and usually heals quite well. Prognosis for complete recovery is also good.
Postmenopausal women with breast abscesses have a high rate of return after simple drainage and frequently need to follow up with a surgeon for more definitive treatment. Chronic infection can result if an abscess is not completely drained, and this can result in a poor cosmetic outcome.
Women's Health Guide
- Screening & Tests
- Diet & Exercise
- Rest & Relaxation
- Reproductive Health
- Head to Toe
Symptoms, causes, types, and treatment
A breast infection occurs when bacteria invade the breast, resulting in inflammation. This is called mastitis.
This is called mastitis.
Although mastitis is often associated with lactation, people who are not lactating can also get breast infections.
This article explores breast infections in more detail, including their symptoms, risk factors, and treatment options.
In some cases, a person with a breast infection may notice an infected lesion on the surface of the breast. Additionally, a breast infection can cause pain deep in the breast.
Other breast infection symptoms can include:
- the breast feeling hot to the touch
- a fever
- flu-like symptoms, including body aches and feeling tired
- nausea
- sores on the nipple or breast that do not heal
Some people may develop ulcers on their skin, which may leak pus or blood.
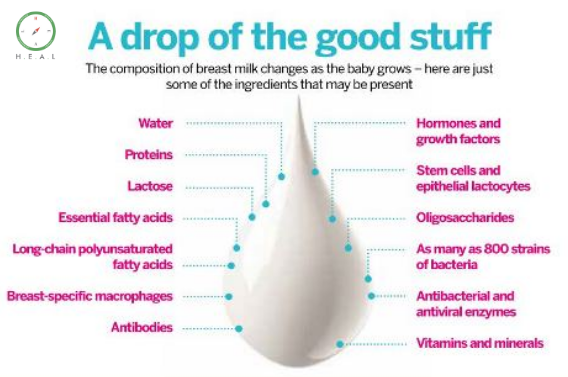
Mastitis is a common type of breast infection. It is particularly prevalent during lactation because the nipples can crack, allowing bacteria to enter the breast.
A milk duct can also become clogged due to incomplete breast emptying or excess pressure on the breast.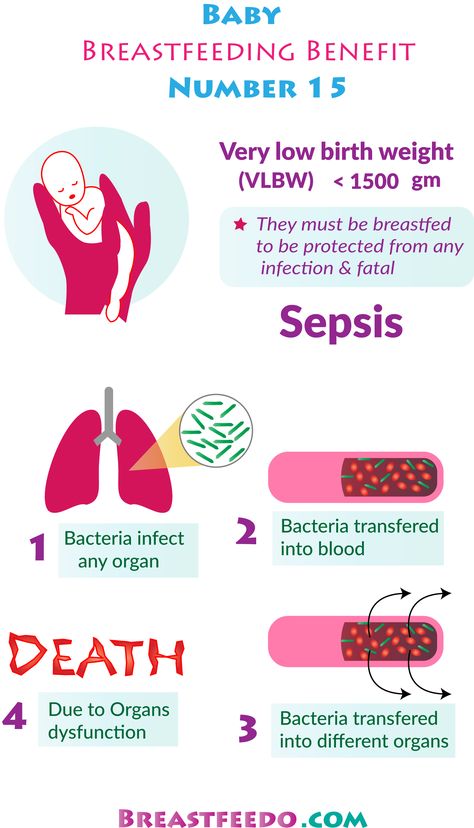 Clogged milk ducts allow bacteria to multiply, which can lead to an infection.
Clogged milk ducts allow bacteria to multiply, which can lead to an infection.
There are several types of breast infections, including:
- Central or subareolar infection: This occurs when the milk ducts become infected or inflamed. It is most likely to develop in people who smoke. It can cause nipple changes, such as nipple retraction or unusual discharge.
- Granulomatous lobular mastitis: This causes a painful but noncancerous mass to develop in the breast.
- Peripheral, nonlactating infection: This type of infection often leads to inflammation or a visible abscess on the breast. It commonly occurs in people with diabetes or those who smoke.
- Cellulitis: This is a skin infection more common in people with large breasts or those with a history of breast surgery or radiotherapy. It can cause a rash that can spread quickly if not treated.
- Inflammatory carcinoma: This cancer is rare, accounting for just 1–5% of all breast cancers diagnosed in the United States.
 It can cause the breast to become swollen and discolored, and sometimes the skin can appear dimpled, like an orange peel. As this cancer is very aggressive, a person who has any symptoms should contact a doctor.
It can cause the breast to become swollen and discolored, and sometimes the skin can appear dimpled, like an orange peel. As this cancer is very aggressive, a person who has any symptoms should contact a doctor.
To make a diagnosis, a doctor needs to know about a person’s symptoms. They may ask whether a person is breastfeeding, has a history of breast trauma, or has had surgery or treatments on the breast. Additionally, they may ask if a person has fever, chills, or fatigue.
The individual may also need a physical examination of the breast and nipple.
In some instances, a doctor may take a swab of breast discharge. They can send this for tests to determine the type of bacteria growing in the breast. Knowing the type of bacteria can help a doctor prescribe the right medication.
Depending on a person’s symptoms, a doctor may order the following tests:
- Mammogram: This test uses low dose X-rays to look for breast cancer and other changes in the tissue.
- Ultrasound: A breast ultrasound uses high frequency sound waves and makes a computer image of the breast tissue. It can show breast changes, such as fluid-filled cysts, that are difficult to see on mammograms.
- Breast biopsy: The biopsy procedure takes a small sample of tissue from the breast using a needle or minor surgery, then sends it for examination in a laboratory.
It is important to note that a healthcare professional should evaluate any breast infection. Usually, if a person is breastfeeding, the infection is caused by lactation and is relatively simple to treat. However, in people who are not lactating, an infection may be more serious. If they experience symptoms that do not resolve, they should contact a doctor.
Treatment for a breast infection often depends on the underlying cause and the severity of symptoms. However, it is important to receive early treatment to prevent complications.
If a bacteria is causing the infection, a doctor usually prescribes antibiotics. People should always take the full course of antibiotics, even if they start to feel better before completing treatment.
People should always take the full course of antibiotics, even if they start to feel better before completing treatment.
Some people with breast infections have an abscess, a tender lump containing pus. A doctor can drain the abscess, which will reduce pain. They will likely then prescribe antibiotics to treat the infection.
Warm compresses can help relieve mastitis pain. People can also take medications, which may include antibiotics to treat the infection and ibuprofen to relieve pain and inflammation.
Breast abscesses are more common in lactating people than nonlactating people.
Incision and drainage can treat breast abscesses. A doctor uses a scalpel blade to create a small opening in the skin. They may then insert a drain into the wound or leave it open for natural drainage.
However, if an abscess is small, a doctor may attempt needle aspiration instead. The procedure involves using a needle to draw out the infected material.
Home remedies
A person can use a variety of home remedies to minimize the pain and discomfort of an infection, including:
- drinking plenty of fluids
- wearing loose-fitting clothing and avoiding tight bras
- using warm or cold compresses after breastfeeding to reduce pain
Milk stasis, when the milk is no longer flowing freely, is the main cause of mastitis. The milk can block milk ducts, creating a clogged duct. The area of the clog will often look inflamed or swollen and feel tender to the touch. Milk stasis can also create a sore, white spot on the nipple opening. Doctors call this a bleb.
Clearing the plugged duct or removing the bleb can prevent mastitis. A person can gently remove a bleb at home with a warm compress, or they can contact a doctor.
Additionally, the following may reduce discomfort and minimize the likelihood of the infection returning:
- continuing to breastfeed or pump frequently, unless the doctor says otherwise
- using the infected breast first when breastfeeding to ensure that it empties
- applying warm, moist compresses to the painful breast, especially right before nursing or pumping
- trying to adopt different positions during breastfeeding so that all areas of the breast can empty fully
- while breastfeeding or pumping, massaging the areas of the breast that feel hard with gentle pressure
If bacteria enter the breast, it can cause an infection, leading to painful inflammation. It can cause tenderness, pain, and flu-like symptoms.
It can cause tenderness, pain, and flu-like symptoms.
Doctors usually treat these infections with antibiotics. People can take OTC medications and use home remedies to manage their symptoms.
An individual can reduce their chances of developing mastitis while breastfeeding by nursing or pumping often to ensure their milk can flow freely.
Read this article in Spanish.
Treatment of infections and inflammation of the mammary glands in the Vyborgsky district of St. Petersburg
In this article, we have described the most common diseases of the mammary glands. The material is for informational purposes only. If you are worried about any tightness in the chest or pain, be sure to contact a mammologist to conduct a diagnostic study.
Orthopedist
Appointment online
Phones:
+7 (812) 30-888-03
+7 (812) 242-53-50
Clinic address: St. Petersburg, Vyborgsky district, Parnas metro station, st. Asafiev, 9, building 2, lit. А
Asafiev, 9, building 2, lit. А
Our doctors
Kasyanova Marina Nikolaevna
Surgeon, oncologist, mammologist, proctologist, doctor of ultrasound diagnostics, Ph.D.
Borisov Sergey Vladimirovich
Surgeon, pediatric surgeon, oncologist, mammologist, doctor of ultrasound diagnostics (children, adults)
Prices for services
- Mammologist's consultation
- Procedures
Please note! Prices are for adult patients. Please see the Pediatrics section for the cost of children's appointments.
| Reception (inspection, consultation) Mammologist primary | 2 200 |
| Reception (examination, consultation) of a mammologist repeated | 1 800 |
| Reception (examination, consultation) ) Ph.D. primary | 2 500 |
Appointment (examination, consultation) with an oncologist (mammologist), Ph. D. Repeated D. Repeated | 2 100 |
| Opening and drainage of purulent mastitis (1 square) without the cost of anesthesia | 5 100.00 | 550.00
| Dressing after opening for purulent mastitis | 1000.00 |
| Small -iginal aspiration biopsy (Tab) of breast cysts (1 cyst), without the cost of histology | 2 100.00 |
Lactation mastitis
The most common type mastitis. With this condition, which occurs when a woman is breastfeeding, women's nipples become cracked and sore, allowing bacteria from the baby's mouth to enter the ducts and multiply rapidly in the milk. Sometimes the infection comes from a blocked milk duct. In both cases, the chest becomes hard, reddened, hot and sore. nine0003
The doctor may also prescribe antibiotics and painkillers. In some cases, lactational mastitis progresses and forms an abscess, a more serious condition that may require drainage.
Non-lactational mastitis
Non-lactational mastitis is similar to lactational mastitis but occurs in non-breastfeeding women. In some cases, this condition occurs after a lumpetomy followed by radiation therapy in women with diabetes or in those who have reduced immune functions in the body. nine0003
Although rare, this condition is usually accompanied by high fever and headache and is treated with antibiotics. Consult your doctor for diagnosis and treatment.
Chronic subarreal abscess
Is a common infection of the breast, although it is uncommon. If an infection is found before an abscess develops, it can often be treated with antibiotics. Most often it is necessary to make an incision and drain the abscess.
Mastalgia (chest pain)
Classified as cyclic pain (associated with menstrual periods) or non-cyclic. The latter may come from the chest or may come from somewhere else, such as near the muscles or joints, felt in the chest. In some cases, pain can range from minor discomfort to severe. Many women with mastalgia worry more about the fear of cancer than the pain itself.
Cyclic chest pain
The most common type of chest pain is associated with the menstrual cycle and is almost always hormonal. Some women begin to experience pain during ovulation, which continues until the start of the menstrual cycle. The pain may be subtle or so severe that the woman cannot wear tight clothing or endure close contact of any kind. The pain may be felt in only one breast or in the area under the arm.
Doctors continue to study the role of hormones in cyclic mastalgia. One study showed that some women with cyclic mastalgia experienced a decrease in the ratio of progesterone to estrogen in the second half of their menstrual cycle. Other studies have shown that an abnormality in the hormone prolactin can affect breast pain. Hormones can also influence cyclical stress-related chest pain - sensations can increase or change in texture with hormone changes that occur during times of stress. nine0003
Hormones can also influence cyclical stress-related chest pain - sensations can increase or change in texture with hormone changes that occur during times of stress. nine0003
Hormones cannot give a general response to cyclic breast pain because the pain is often more severe in one breast than the other (steroids tend to affect both breasts equally).
Treatment includes:
- avoiding caffeine
- vitamin E
- low fat diet
- In some cases, various additional hormones and hormone blockers are also prescribed. These may include:
- birth control pills
- BROMOKRIPTINE (which blocks prolactin in the hypothalamus)
- Danazole, male hormone
- thyroid hormones
- Tamoxifen, estrogen blocker
The pectoral pain in the sternum
7
does not change during the menstrual cycle. As a rule, the pain is present all the time and is located only in one specific place.
One of the causes of non-cyclic chest pain is trauma or impact. Other causes may include arthritic pain in the chest cavity and in the area of the neck that reaches the chest. nine0003
Other causes may include arthritic pain in the chest cavity and in the area of the neck that reaches the chest. nine0003
Doctors usually do a physical examination and a mammogram. In some cases, a biopsy is also needed. If the pain is determined to be caused by a cyst, it will be aspirated. Depending on where the pain occurs, treatment may include analgesics, anti-inflammatory drugs, and compresses.
Orthopedist
Online appointment
Phones:
+7 (812) 30-888-03
+7 (812) 242-53-50
Clinic address: St. Petersburg, metro Vyborgsky district Parnassus, st. Asafiev, 9, to 2, lit. A
How to identify breast disease | Directory of medical laboratory Optimum (Sochi, Adler)
- Home
- How to recognize the disease
- Diseases of the breast
More about the doctor
How to recognize breast diseases?
Breast diseases is a group of pathological conditions of a polyetiological nature. Men and women are subject to their development. Most often they are faced by women of reproductive age.
Men and women are subject to their development. Most often they are faced by women of reproductive age.
Types of breast diseases
All breast diseases can be divided into two main groups. These are pathologies of an inflammatory nature and of a tumor nature .
Inflammatory conditions include lactational or non-lactational mastitis. nine0003
All neoplastic conditions can be divided into benign and malignant diseases. These include:
- Fibroadenomas.
- Breast cysts.
- Glandular, fibrous, cystic, mixed mastopathy.
- Lipoma.
- Intraductal papilloma.
- Malignant tumor.
Causes of the development of pathologies
The most common cause of the development of breast diseases is a hormonal disorder. Changes in hormonal levels can develop in patients at different ages. These include pathologies from the work of the ovaries, thyroid gland or other endocrine organs. Increase the risk of developing hormonal disorders:
Increase the risk of developing hormonal disorders:
- Termination of pregnancy.
- Tumors in the pituitary, ovaries or adrenal glands.
- Uncontrolled intake of hormonal drugs.
- Bad habits such as smoking, drinking alcohol or drugs.
- Traumatic effects.
Mastitis can develop as a result of lactostasis, infection through injured nipples, the spread of pathogenic pathogens from foci of chronic infection with a natural decrease in immune forces. nine0003
Symptoms and first signs
Symptoms of breast diseases are characterized by a variety of clinical picture.
The inflammatory process is characterized by an acute onset of the disease. The patient complains of pain in the chest area, its redness, swelling. Lymph nodes may be enlarged. As the pathological process progresses, there is a deterioration in general well-being with an increase in body temperature, weakness and general malaise.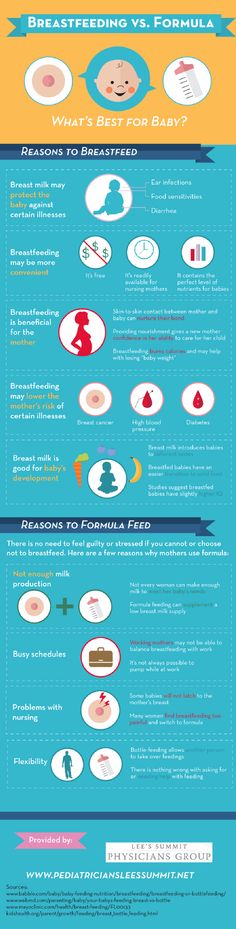 nine0003
nine0003
Tumor processes are characterized by engorgement of the mammary glands, the appearance of a volumetric formation. The mammary gland is deformed, the skin may resemble a "lemon peel". In some cases, palpation determines the soreness of the site. When the duct is involved in the pathological process, milky, serous, sanious or purulent contents are released from the nipple.
Methods of diagnosis
Initially, to clarify the disease of the breast, a conversation between the doctor and the patient is held. Find out complaints, the dynamics of the pathological process, the presence of concomitant pathologies and the nature of the menstrual function. nine0003
The specialist performs palpation of the mammary gland with an assessment of the skin, pain and condition of the surrounding tissues. Lymph nodes are also palpable.
Based on the information received, additional diagnostic methods are prescribed, such as:
- Mammography .
 This method is the most common and available in clinical practice. It is rarely prescribed for patients under 40 years of age. Because of the X-ray load, mammography is prohibited during pregnancy and breastfeeding. nine0040
This method is the most common and available in clinical practice. It is rarely prescribed for patients under 40 years of age. Because of the X-ray load, mammography is prohibited during pregnancy and breastfeeding. nine0040 - Ultrasound. A common technique is highly accessible and highly informative. Due to the absence of radiation exposure, it is allowed to be used by pregnant and lactating women.
- Pathological site puncture . If there is a suspicious area, a biopsy is performed. After a histological examination, the nature of the formation is determined and treatment tactics are selected.
- Cytological examination of the discharge (punctate) of the breast. The method determines a malignant breast tumor in the early stages of development. nine0040
Treatment
Therapy for breast pathology is selected based on the diagnosis.
Drug treatment includes:
- Antibiotics.
 Means are indicated for mastitis as part of complex therapy. Preference is given to broad-spectrum drugs.
Means are indicated for mastitis as part of complex therapy. Preference is given to broad-spectrum drugs. - Non-steroidal anti-inflammatory drugs. This group is used for a complex effect on the inflammatory process, reducing the severity of edema. Also, against the background of the application, there is a decrease in temperature and pain. nine0040
- Herbal products. They help to normalize the hormonal background in the initial stages of the disease.
- Hormonal preparations.
If conservative therapy is ineffective, surgical intervention is indicated, which involves resection of the pathological focus or removal of the mammary gland with lymph nodes.
In order to prevent breast diseases, exposure to various risk factors must be excluded. Also, patients are advised to visit a doctor regularly and undergo an additional examination.