Endo pain during pregnancy
Pelvic Pain During Pregnancy in Endometriosis
Pelvic pain is one of the most common symptoms of endometriosis. Women with endometriosis may experience painful periods, severe cramping, chronic pelvic pain (pain even outside of periods), pain while passing gas, urine, or stool, and pain during sex.
The cause of pain in endometriosis is unclear. In endometriosis, tissue resembling the lining of the uterus grows elsewhere in the body, forming lesions. These lesions most frequently occur in the pelvis, but in some cases can also develop on the appendix, bowels, and even the diaphragm.
Researchers think that the swelling and breakdown of the misplaced endometrial tissue in response to hormones may cause the pain. Think of it as a micro-period, possibly in multiple different locations. Since the body cannot expel the endometriosis lesions, they may cause inflammation and pain. The lesions may also form nodules on the surface of pelvic organs over time causing even further pain.
Some endometrial lesions may develop a nerve within them. Or they may form near a nerve, pressing against it, thereby also causing pain.
What may cause pelvic pain during pregnancy?
The most common causes of pelvic pain during pregnancy include uterine muscle stretching due to fetus growth spurts, inflammation, the movement of pelvic joints during and after pregnancy, pressure from the fetus’ increasing weight, and the secretion of the relaxin hormone that helps in the softening of the ligaments and loosening of the joints for delivery.
In some cases, pregnancy complications can also cause pelvic pain. These include ectopic pregnancy (when the fetus develops outside the uterus), preterm labor (onset of contractions and labor before 37 weeks of gestation), miscarriage (loss of pregnancy), or placental abruption (placental detachment from the uterine wall). Endometriosis may increase the risk of these complications in some cases.
In women with endometriosis, the profile of experienced pain may change during pregnancy. While some women with the disease may get relief from pelvic pain, for others pregnancy may make the pain worse. Some women may see no change in their symptoms.
While some women with the disease may get relief from pelvic pain, for others pregnancy may make the pain worse. Some women may see no change in their symptoms.
Why does the pain subside in some women?
In some women with endometriosis, pregnancy may provide temporary relief from pelvic pain, particularly during the later months. One reason may be the absence of the menstrual cycle and the monthly hormonal fluctuations.
Another reason may be the increased levels of the hormone progesterone during pregnancy. This progesterone may suppress the growth of endometrial tissue. Research has shown that progestin, a synthetic version of progesterone can, in fact, reduce pelvic pain due to endometriosis in approximately 90% of the patients. In fact, doctors sometimes prescribe progestin hormone therapy for women with the disease. This further supports the idea that high levels of progesterone may reduce pelvic pain during pregnancy in some women with endometriosis.
Pregnancy may provide temporary relief from pelvic pain in some cases. However, the symptom will often return after the birth of the baby when the monthly cycle resumes. Pregnancy should, therefore, not be a strategy to manage the symptoms of endometriosis.
However, the symptom will often return after the birth of the baby when the monthly cycle resumes. Pregnancy should, therefore, not be a strategy to manage the symptoms of endometriosis.
Breastfeeding may delay the return of painful symptoms associated with having a period. This is because breastfeeding inhibits the release of the hormone estrogen by the ovaries. This suppresses both ovulation and the growth of endometrial tissues.
Why does the pain sometimes worsen during pregnancy?
Some women with endometriosis may not see any improvement. Some may even see their symptoms worsen during pregnancy, particularly during the earlier months. This may be because the uterus expands to accommodate the growing fetus. This expansion may pull and stretch the endometrial lesions and cause pain.
An increase in the level of estrogen may also worsen pelvic pain during pregnancy.
Pelvic pain due to complications in endometriosis
A Danish study found that pregnant women with endometriosis have a higher risk of complications such as pre-eclampsia and preterm birth. Both complications are associated with pelvic pain.
Both complications are associated with pelvic pain.
Another study suggests that endometriosis may slightly increase the risk of miscarriage, which is characterized by lower back pain, cramping, or bleeding.
Management of pelvic pain during pregnancy
It is crucial that women with endometriosis are closely followed during pregnancy to avoid complications and provide the necessary treatment if necessary.
Surgery and hormonal therapy (the standard treatments for endometriosis) cannot be implemented during pregnancy. Doctors may, however, prescribe pain relievers that are safe to use during pregnancy.
Other measures that may alleviate pelvic pain during pregnancy include taking warm baths, getting enough rest, and eating fiber-rich foods to avoid constipation. Prenatal stretching exercises, prenatal massage, avoiding sharp movements at the waist, and regular exercise may also help. Finally, heat pads, a pelvic support garment that provides support to the uterus, and wearing comfortable shoes with good support, can alleviate pelvic pain during pregnancy.
Ready for a Consultation?
Our endometriosis specialists are dedicated to providing patients with expert care. Whether you have been diagnosed or are looking to find a doctor, they are ready to help.
Our office is located on 872 Fifth Avenue New York, NY 10065.
You may call us at (212) 988-1444 or have your case reviewed by clicking here.
Review My Case
What to Expect, Risks, and More
Endometriosis is a disorder in which tissue similar to what normally lines the uterus, called the endometrium, grows outside of the uterine cavity. It can adhere to the outside of the uterus, the ovaries, and the fallopian tubes.
When any of these organs are damaged, blocked, or irritated by this endometrium-like tissue, it can become more difficult to get and stay pregnant. Your age, health, and the severity of your condition will also affect your chances of carrying a baby to term.
One 2014 study found that while 15 to 20 percent of fertile couples attempting to become pregnant will be successful each month, that number drops to 2 to 10 percent for couples affected by endometriosis.
Pregnancy may temporarily halt the painful periods and heavy menstrual bleeding that are often characteristic of endometriosis. It might provide some other relief as well.
Some people benefit by the increased levels of progesterone during pregnancy. It’s thought that this hormone suppresses and perhaps even shrinks endometrial growths. In fact, progestin, a synthetic form of progesterone, is often used to treat those with endometriosis.
Other people, however, will find no improvement. You may even find that your symptoms worsen during pregnancy. That’s because, as the uterus expands to accommodate the growing fetus, it can pull and stretch misplaced tissue. That can cause discomfort. An increase in estrogen can also feed endometrial growths.
Your experience during pregnancy may be different from other pregnant people with endometriosis. The severity of your condition, your body’s hormone production, and the way your body responds to pregnancy will all affect how you feel.
The severity of your condition, your body’s hormone production, and the way your body responds to pregnancy will all affect how you feel.
Even if your symptoms do improve during pregnancy, they can resume after the birth of your baby. Breastfeeding may delay the return of symptoms, but once your period returns, your symptoms will likely return.
Endometriosis may increase your risk for pregnancy and delivery complications. This may be caused by the inflammation, structural damage to the uterus, and hormonal influences endometriosis causes.
Miscarriage
Several studies have documented that miscarriage rates are higher in those with endometriosis than in those without the condition. This holds true even for people with mild endometriosis.
One retrospective analysis from 2017 concluded that people with endometriosis had a 35.8 percent chance of miscarriage versus 22 percent in those without the disorder. More research is needed to determine if endometriosis is a significant risk factor for miscarriage.
There’s nothing you or your doctor can do to stop a miscarriage from happening, but it’s important to recognize the signs so you can seek medical and emotional help to properly recover.
If you’re fewer than 12 weeks pregnant, miscarriage symptoms resemble those of a menstrual period:
- bleeding
- cramping
- low back pain
You might also notice the passage of some tissue.
Symptoms after 12 weeks are mostly the same, but bleeding, cramping, and tissue passage might be more severe.
Preterm birth
According to an analysis of studies, pregnant people with endometriosis are 1.5 times more likely than other expectant moms to deliver before 37 weeks of gestation. A baby is considered preterm if he or she is born before 37 weeks of gestation.
Babies born prematurely tend to have a low birth weight and are more likely to experience health and developmental problems. Symptoms of early labor include:
- Regular contractions: Contractions are a tightening around your midsection, which may or may not hurt.

- Change in vaginal discharge: It may become bloody or the consistency of mucus.
- Pressure in your pelvis
If you’re experiencing any of these symptoms, speak with your doctor. Early labor can sometimes cause, or be a symptom of your baby being in distress, and should be investigated to see if medical intervention is needed.
Placenta previa
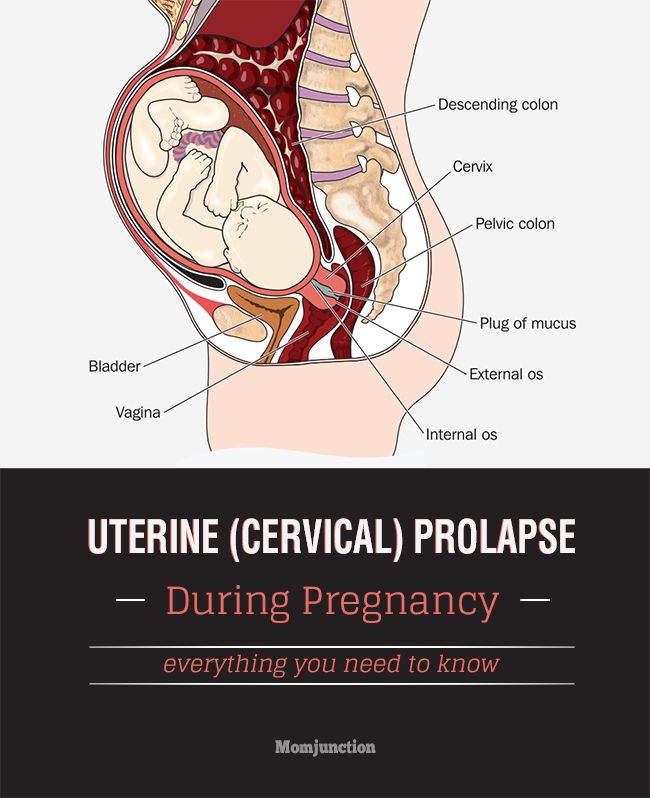
During pregnancy, a fetus and placenta will develop. The placenta supplies oxygen and nourishment to your growing fetus through your blood.
Most placentas attach to the uterine walls, away from the cervix. However, in some, the placenta may be close to or directly on the opening to the cervix. This is known as placenta previa.
Placenta previa can increase your risk for significant bleeding and placenta abruption — a premature and dangerous separation of the placenta from the uterus.
People with endometriosis may be at increased risk for this life-threatening condition. The main symptom is bright red vaginal bleeding. If the bleeding is minimal, you may be advised to limit your activities, including sex and exercise. If bleeding is heavy, you may need a blood transfusion and an emergency C-section.
The main symptom is bright red vaginal bleeding. If the bleeding is minimal, you may be advised to limit your activities, including sex and exercise. If bleeding is heavy, you may need a blood transfusion and an emergency C-section.
Surgery and hormonal therapy, the standard treatments for endometriosis, are generally not recommended while pregnant.
Over-the-counter pain relievers may help reduce endometriosis discomfort, but it’s important to work with your doctor to determine which ones can be safely used during pregnancy, and for how long. Never take any medication, even over the counter, without consulting with your doctor first.
Some self-help measures include:
- taking warm baths
- eating fiber-rich foods to help reduce your risk for constipation
- walking gently or doing prenatal yoga to stretch the back and relieve endometriosis-related back pain
Getting pregnant and having a healthy baby are possible and common with endometriosis.
Having endometriosis may make it more difficult to conceive, and may also increase your risk for serious pregnancy complications.
Pregnant people with the condition are considered higher risk. Depending on the severity, you could expect to have more frequent and careful monitoring throughout your pregnancies, so that your doctor can quickly identify complications if they do arise.
Pain in the pubic region during pregnancy
Subscribe to our Instagram! Useful information about pregnancy and childbirth from leading obstetricians and gynecologists in Moscow and foreign experts: https://www.instagram.com/roddompravda/
Tips and opinions from leading child professionals: https://www.instagram.com/emc.child/
The pubic bone is one of the three bones that make up the pelvic bone. Two pubic bones, forming the pubic articulation (symphysis), form the anterior wall of the pelvis. The pubic bone in women with a regular physique has the form of a roller about the thickness of the thumb, which is curved and forms a pubic eminence. This bone hangs in a kind of arch over the entrance to the vagina.
This bone hangs in a kind of arch over the entrance to the vagina.
The main cause of pain in the pubic bone is the divergence and increased mobility of the pubic symphysis. To refer to pathological changes in the pubic symphysis of the pelvis during pregnancy and after childbirth, the following terms are used: symphysiopathy, symphysitis, arthropathy of pregnant women, divergence and rupture of the pubic symphysis, dysfunction of the pubic symphysis. The most commonly used terms are "symphysitis" or "symphysiopathy".
So, symphysiopathy is a disease associated with a pronounced softening of the pubic joint under the influence of the hormone relaxin, which is produced during pregnancy. The process of softening the interosseous joints is natural, it helps the child to pass more easily through the bone pelvis during childbirth. The diagnosis of "symphysiopathy" is made when severe pain appears, the pubic joint swells, greatly stretches, becomes mobile, and the pubic bones diverge excessively. One of the striking, characteristic symptoms of this pathology is that it is impossible to raise the leg in the prone position. In addition to acute pain in the pubis, there are difficulties when walking up the stairs, it becomes difficult to turn from side to side on the bed and get up from the sofa, and the gait changes and becomes like a "duck". According to most doctors, the cause of symphysiopathy is a lack of calcium, an increased concentration of the hormone relaxin, and increased physical activity on the bones of the pelvic region. In addition, the development of symphysiopathy can be provoked by a serious sports injury or a fracture of the pelvic bones.
One of the striking, characteristic symptoms of this pathology is that it is impossible to raise the leg in the prone position. In addition to acute pain in the pubis, there are difficulties when walking up the stairs, it becomes difficult to turn from side to side on the bed and get up from the sofa, and the gait changes and becomes like a "duck". According to most doctors, the cause of symphysiopathy is a lack of calcium, an increased concentration of the hormone relaxin, and increased physical activity on the bones of the pelvic region. In addition, the development of symphysiopathy can be provoked by a serious sports injury or a fracture of the pelvic bones.
At what stage of pregnancy do they occur?
The disease begins gradually or suddenly during pregnancy, childbirth or after childbirth. Most often, women begin to feel pain in the area of the pubic joint in the third trimester of pregnancy. This is due to the fact that the places of adhesions of the pubic bones, their ligaments and cartilage, soften under the influence of the hormone relaxin. This hormone of pregnancy naturally softens the bony joints, which is necessary to facilitate the passage of the child's bone pelvis and birth canal at the time of childbirth.
This hormone of pregnancy naturally softens the bony joints, which is necessary to facilitate the passage of the child's bone pelvis and birth canal at the time of childbirth.
Some women begin to complain of pain in the pelvic bones some time after giving birth. This may be the result of traumatic childbirth (imposition of obstetrical forceps, shoulder dystocia, excessive separation of the hips during childbirth, etc.) or physical exertion (lifting a heavy baby stroller up the stairs, prolonged motion sickness in the arms of a well-fed baby, etc.). It is recommended to limit physical activity, wear an orthopedic bandage, consult a traumatologist. Complaints usually recur after the next pregnancy. In a small proportion of patients, pain persists for a long time.
When can this be considered the norm, and when not?
Obstetricians-gynecologists do not consider a slight soreness of the pubic joint to be a pathology, but if the pain is acute, restricting the movements of the pregnant woman, accompanied by edema, then we can talk about pathology. Pain can be quite strong and especially manifest itself while walking, turning the body to the right and left in a sitting position and even lying down. In this case, you need to urgently consult a doctor and undergo an ultrasound diagnosis (ultrasound) to determine the size of the divergence of the pubic bones. Magnetic resonance imaging (MRI) is also used, which allows assessing the state of the symphysis, the state of the bone tissue, as well as soft tissues.
Pain can be quite strong and especially manifest itself while walking, turning the body to the right and left in a sitting position and even lying down. In this case, you need to urgently consult a doctor and undergo an ultrasound diagnosis (ultrasound) to determine the size of the divergence of the pubic bones. Magnetic resonance imaging (MRI) is also used, which allows assessing the state of the symphysis, the state of the bone tissue, as well as soft tissues.
With ultrasound, the degree of divergence (diastasis) of the pubic bones is determined. The severity of the clinical picture largely depends on the degree of divergence of the pubic bones, and therefore there are three degrees of divergence of the pubic branches: in the first degree - by 6-9 mm, in the second - by 10-20 mm, in the third - more than 20 mm. The severity of the symptoms of the disease varies from mild discomfort to unbearable pain.
How can pain be relieved?
There are some recommendations that will help reduce bone pain during pregnancy, if the cause of its occurrence is the divergence of the pubic bones. Be sure to wear a bandage, especially in later pregnancy. The bandage takes on most of the load, thereby releasing pressure from the pubic joint. Limitation of heavy physical exertion is indicated for any manifestations of pain, lying down more often, walking less and being in a sitting position for no longer than 30-40 minutes. In severe cases, before and sometimes after childbirth, a woman may be shown strict bed rest. Moreover, the bed should not be hard and flat.
Be sure to wear a bandage, especially in later pregnancy. The bandage takes on most of the load, thereby releasing pressure from the pubic joint. Limitation of heavy physical exertion is indicated for any manifestations of pain, lying down more often, walking less and being in a sitting position for no longer than 30-40 minutes. In severe cases, before and sometimes after childbirth, a woman may be shown strict bed rest. Moreover, the bed should not be hard and flat.
Since the appearance of symphysiopathy is associated not only with a large production of the hormone relaxin, but also with a lack of calcium in the body, the expectant mother is prescribed calcium preparations and complex vitamins for pregnant women, which contain all the necessary vitamins and trace elements in the right amount and proportions. There is evidence that pain is reduced during acupuncture and physiotherapy.
In especially severe cases of symphysiopathy, the pregnant woman is hospitalized.
What is the danger of this condition?
The occurrence of symphysiopathy is due to several reasons. This is a lack of calcium in the body of the future mother, and an excess amount of the hormone relaxin, and the individual structural features of the woman's body, and possible hereditary or acquired problems of the musculoskeletal system.
With an unexpressed clinical picture of the disease, with an expansion of the pubic fissure up to 10 mm, normal pelvic sizes, a small fetus, childbirth can be carried out through the birth canal, avoiding the use of physical force, such as the Christeller maneuver. With a pronounced stretching of the pubic symphysis, pain syndrome, especially with anatomical narrowing of the pelvis, a large fetus, there is a danger of rupture of the pubic symphysis, and the method of choice in this case is caesarean section. This is due to the fact that during natural delivery, the bones can disperse even more and the woman subsequently will not be able to walk at all.
Prevention
The body of a healthy woman is able to independently cope with all the difficulties of the pregnancy period. First of all, the expectant mother should include enough foods containing calcium in her diet, as well as take vitamins for pregnant women.
For the prevention of symphysiopathy, the use of a prenatal bandage is recommended, which supports the abdomen and prevents excessive stretching of the ligaments and muscles. Prophylactic antenatal bandage is usually recommended from 25 weeks of gestation, when the abdomen begins to actively grow.
In order to ensure the plasticity of the ligaments and muscles, as well as the flexibility of the joints, special exercises must be done even during the planning of pregnancy. Yoga gives good results.
Pregnancy with endometriosis: a modern view
Laser treatment and vaginal rejuvenation
Read more
Once again about hormones or a must-buy list for the week
Read more
Visit to the urologist. For or Against?
Read more
Preservation of reproductive health
Read more
Pregnancy with uterine fibroids
more
Practical skills when examining barren steam
Read more
9000Read more
Varicocele and impaired spermatogenesis
Read more
Secretory and obstructive infertility in men
Read more
Protocols for controlled ovarian stimulation (COS)
Read more
Miscarriage. What is the reason?
Read more
Hysteroscopy and its role in the treatment of infertility
Read more
Why you can’t get pregnant
more
How to calculate the gender of the child before the conception of
Read more
Loveliness of the fallopian tubes
more than
Syndrome of ovary hypertension syndrome look at problem
More
Pregnancy with endometriosis - a modern view
More
Immunological infertility and the role of antisperm antibodies in it
More
What is cervical pathology?
Read more
IVF in the natural cycle: pros and cons
Read more
Practical skills in examining infertile couples
Read more
Artificial insemination
Read more
Laser removal of scars and scars, skin whitening.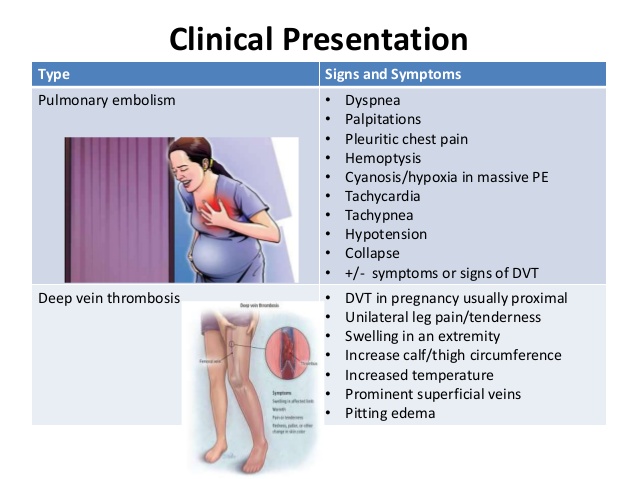
Read more
Unable to get pregnant. Where to run? Where to begin?
Read more
What future parents need to know (most popular questions)
Read more
Endometriosis. Some important questions
Read more
Prolactin increase. Should I be afraid?
Read more
Obstruction of the fallopian tubes, what to do next?
Read more
Human papillomavirus. Basic information
Read more
KAMALIYA: “I consider Vladimir Kotlik the godfather of my children”
Read more
Infertility and cancer: why men should definitely visit a reproductive specialist
Read more
Sex, children, rock-roll about what can increase the chances of IVF
More
Portrait of a female doctor: 5 signs of a good gynecologist
More
Is sex during IVF a good idea?
Read more
Never say never. Why childfree is dangerous and why it is worth leaving a “piece of yourself” in a cryobank
Why childfree is dangerous and why it is worth leaving a “piece of yourself” in a cryobank
More details
How to plan health, longevity and parenthood: practical advice from doctors for 2020
More details
From virus to cancer: hidden threats to women's health
Read more
Threatened miscarriage
Read more
Reproductive health of adolescent girls: what children and their parents need to know
Read more
Life is like magic: how to believe in a miracle if you are a pragmatist - the story of a doctor
Read more
Beautiful skin in youth is the key to happy motherhood
Read more
Charged for success. What determines the effectiveness of ART
More
Why do not all eggs become embryos?
Read more
Maxim Gapchuk in "Mother and child" ambitious future
Read more
Unsuccessful IVF, how to survive? Expert advice
Read more
What should an Rh-negative woman know?
Read more
9 tips for future parents
Read more
Eco: Modern methods and approaches in the treatment of female infertility
more
ICSI: Men's infertility - NOT a sentence
more
Laparoscopy: Advantages over traditional surgery
Read more
Uterine examination: what you need to know about hysteroscopy
Read more
Artificial intrauterine insemination: The essence of the method, stages and results of
Read more
Infertility Diagnostics in men
Read more
10 reasons to contact a man to andrologist
more
Cryutotechnology as a method of family planning
How to become a mother: psychological and physical preparation
Read more
Monalisa Touch – what is this technology
Read more
Premature menopause in men: how to recognize and how dangerous is
Read more
Why go to a preventive inspection for a gynecologist
Read more
Laser therapy in gynecology: without anesthesia and pain
Read more
Ambulant gynecology. seeking qualified help
seeking qualified help
More details
Pregnancy after 35: why additional tests and examinations are needed
Read more
Causes and prevention of female infertility
Read more
One-day surgery: a modern approach to treatment
Read more
Pregnancy management: keep the baby healthy and mother feel good
Read more future parents to remember
More details
Anomalies of the uterus and their influence on the onset and gestation of pregnancy.
Read more
Rubts on the uterus after cesarean section
Read more
The most common mistakes during pregnancy
Read more
Varicosis and hemorrhoids during pregnancy
Read more
Read more
Periods disappeared during the war.