Early screening for down syndrome
First trimester screening - Mayo Clinic
Overview
Nuchal translucency measurement
Nuchal translucency measurement
First trimester screening includes an ultrasound exam to measure the size of the clear space in the tissue at the back of a baby's neck (nuchal translucency). In Down syndrome, the nuchal translucency measurement is abnormally large — as shown on the left in the ultrasound image of an 11-week fetus. For comparison, the ultrasound image on the right shows an 11-week fetus with a normal nuchal translucency measurement.
First trimester screening is a prenatal test that offers early information about a baby's risk of certain chromosomal conditions, specifically, Down syndrome (trisomy 21) and extra sequences of chromosome 18 (trisomy 18).
First trimester screening, also called the first trimester combined test, has two steps:
- A blood test to measure levels of two pregnancy-specific substances in the mother's blood — pregnancy-associated plasma protein-A (PAPP-A) and human chorionic gonadotropin (HCG)
- An ultrasound exam to measure the size of the clear space in the tissue at the back of the baby's neck (nuchal translucency)
Typically, first trimester screening is done between weeks 11 and 14 of pregnancy.
Using your age and the results of the blood test and the ultrasound, your health care provider can gauge your risk of carrying a baby with Down syndrome or trisomy 18.
If results show that your risk level is moderate or high, you might choose to follow first trimester screening with another test that's more definitive.
Products & Services
- Book: Mayo Clinic Guide to a Healthy Pregnancy
- Book: Obstetricks
Why it's done
First trimester screening is done to evaluate your risk of carrying a baby with Down syndrome. The test also provides information about the risk of trisomy 18.
Down syndrome causes lifelong impairments in mental and social development, as well as various physical concerns. Trisomy 18 causes more severe delays and is often fatal by age 1.
First trimester screening doesn't evaluate the risk of neural tube defects, such as spina bifida.
Because first trimester screening can be done earlier than most other prenatal screening tests, you'll have the results early in your pregnancy.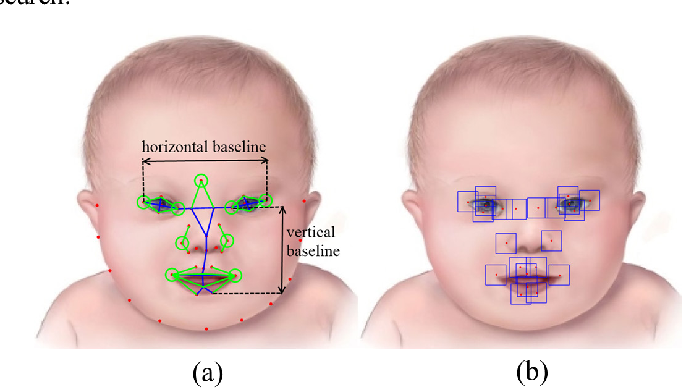 This will give you more time to make decisions about further diagnostic tests, the course of the pregnancy, medical treatment and management during and after delivery. If your baby has a higher risk of Down syndrome, you'll also have more time to prepare for the possibility of caring for a child who has special needs.
This will give you more time to make decisions about further diagnostic tests, the course of the pregnancy, medical treatment and management during and after delivery. If your baby has a higher risk of Down syndrome, you'll also have more time to prepare for the possibility of caring for a child who has special needs.
Other screening tests can be done later in pregnancy. An example is the quad screen, a blood test that's typically done between weeks 15 and 20 of pregnancy. The quad screen can evaluate your risk of carrying a baby with Down syndrome or trisomy 18, as well as neural tube defects, such as spina bifida. Some health care providers choose to combine the results of first trimester screening with the quad screen. This is called integrated screening. This can improve the detection rate of Down syndrome.
First trimester screening is optional. Test results indicate only whether you have an increased risk of carrying a baby with Down syndrome or trisomy 18, not whether your baby actually has one of these conditions.
Before the screening, think about what the results will mean to you. Consider whether the screening will be worth any anxiety it might cause, or whether you'll manage your pregnancy differently depending on the results. You might also consider what level of risk would be enough for you to choose a more invasive follow-up test.
More Information
- Prenatal testing: Quick guide to common tests
Request an Appointment at Mayo Clinic
Risks
First trimester screening is a routine prenatal screening test. The screening poses no risk of miscarriage or other pregnancy complications.
How you prepare
You don't need to do anything special to prepare for first trimester screening. You can eat and drink normally before both the blood test and the ultrasound exam.
What you can expect
First trimester screening includes a blood draw and an ultrasound exam.
During the blood test, a member of your health care team takes a sample of blood by inserting a needle into a vein in your arm. The blood sample is sent to a lab for analysis. You can return to your usual activities immediately.
The blood sample is sent to a lab for analysis. You can return to your usual activities immediately.
For the ultrasound exam, you'll lie on your back on an exam table. Your health care provider or an ultrasound technician will place a transducer — a small plastic device that sends and receives sound waves — over your abdomen. The reflected sound waves will be digitally converted into images on a monitor. Your health care provider or the technician will use these images to measure the size of the clear space in the tissue at the back of your baby's neck.
The ultrasound doesn't hurt, and you can return to your usual activities immediately.
Results
Your health care provider will use your age and the results of the blood test and ultrasound exam to gauge your risk of carrying a baby with Down syndrome or trisomy 18. Other factors — such as a prior Down syndrome pregnancy — also might affect your risk.
First trimester screening results are given as positive or negative and also as a probability, such as a 1 in 250 risk of carrying a baby with Down syndrome.
First trimester screening correctly identifies about 85 percent of women who are carrying a baby with Down syndrome. About 5 percent of women have a false-positive result, meaning that the test result is positive but the baby doesn't actually have Down syndrome.
When you consider your test results, remember that first trimester screening indicates only your overall risk of carrying a baby with Down syndrome or trisomy 18. A low-risk result doesn't guarantee that your baby won't have one of these conditions. Likewise, a high-risk result doesn't guarantee that your baby will be born with one of these conditions.
If you have a positive test result, your health care provider and a genetics professional will discuss your options, including additional testing. For example:
- Prenatal cell-free DNA (cfDNA) screening. This is a sophisticated blood test that examines fetal DNA in the maternal bloodstream to determine whether your baby is at risk of Down syndrome, extra sequences of chromosome 13 (trisomy 13) or extra sequences of chromosome 18 (trisomy 18).
 Some forms of cfDNA screening also screen for other chromosome problems and provide information about fetal sex. A normal result might eliminate the need for a more invasive prenatal diagnostic test.
Some forms of cfDNA screening also screen for other chromosome problems and provide information about fetal sex. A normal result might eliminate the need for a more invasive prenatal diagnostic test. - Chorionic villus sampling (CVS). CVS can be used to diagnose chromosomal conditions, such as Down syndrome. During CVS, which is usually done during the first trimester, a sample of tissue from the placenta is removed for testing. CVS poses a small risk of miscarriage.
- Amniocentesis. Amniocentesis can be used to diagnose both chromosomal conditions, such as Down syndrome, and neural tube defects, such as spina bifida. During amniocentesis, which is usually done during the second trimester, a sample of amniotic fluid is removed from the uterus for testing. Like CVS, amniocentesis poses a small risk of miscarriage.
Your health care provider or a genetic counselor will help you understand your test results and what the results mean for your pregnancy.
By Mayo Clinic Staff
Related
Products & Services
First trimester screening - Mayo Clinic
Overview
Nuchal translucency measurement
Nuchal translucency measurement
First trimester screening includes an ultrasound exam to measure the size of the clear space in the tissue at the back of a baby's neck (nuchal translucency). In Down syndrome, the nuchal translucency measurement is abnormally large — as shown on the left in the ultrasound image of an 11-week fetus. For comparison, the ultrasound image on the right shows an 11-week fetus with a normal nuchal translucency measurement.
First trimester screening is a prenatal test that offers early information about a baby's risk of certain chromosomal conditions, specifically, Down syndrome (trisomy 21) and extra sequences of chromosome 18 (trisomy 18).
First trimester screening, also called the first trimester combined test, has two steps:
- A blood test to measure levels of two pregnancy-specific substances in the mother's blood — pregnancy-associated plasma protein-A (PAPP-A) and human chorionic gonadotropin (HCG)
- An ultrasound exam to measure the size of the clear space in the tissue at the back of the baby's neck (nuchal translucency)
Typically, first trimester screening is done between weeks 11 and 14 of pregnancy.
Using your age and the results of the blood test and the ultrasound, your health care provider can gauge your risk of carrying a baby with Down syndrome or trisomy 18.
If results show that your risk level is moderate or high, you might choose to follow first trimester screening with another test that's more definitive.
Products & Services
- Book: Mayo Clinic Guide to a Healthy Pregnancy
- Book: Obstetricks
Why it's done
First trimester screening is done to evaluate your risk of carrying a baby with Down syndrome. The test also provides information about the risk of trisomy 18.
The test also provides information about the risk of trisomy 18.
Down syndrome causes lifelong impairments in mental and social development, as well as various physical concerns. Trisomy 18 causes more severe delays and is often fatal by age 1.
First trimester screening doesn't evaluate the risk of neural tube defects, such as spina bifida.
Because first trimester screening can be done earlier than most other prenatal screening tests, you'll have the results early in your pregnancy. This will give you more time to make decisions about further diagnostic tests, the course of the pregnancy, medical treatment and management during and after delivery. If your baby has a higher risk of Down syndrome, you'll also have more time to prepare for the possibility of caring for a child who has special needs.
Other screening tests can be done later in pregnancy. An example is the quad screen, a blood test that's typically done between weeks 15 and 20 of pregnancy. The quad screen can evaluate your risk of carrying a baby with Down syndrome or trisomy 18, as well as neural tube defects, such as spina bifida. Some health care providers choose to combine the results of first trimester screening with the quad screen. This is called integrated screening. This can improve the detection rate of Down syndrome.
Some health care providers choose to combine the results of first trimester screening with the quad screen. This is called integrated screening. This can improve the detection rate of Down syndrome.
First trimester screening is optional. Test results indicate only whether you have an increased risk of carrying a baby with Down syndrome or trisomy 18, not whether your baby actually has one of these conditions.
Before the screening, think about what the results will mean to you. Consider whether the screening will be worth any anxiety it might cause, or whether you'll manage your pregnancy differently depending on the results. You might also consider what level of risk would be enough for you to choose a more invasive follow-up test.
More Information
- Prenatal testing: Quick guide to common tests
Request an Appointment at Mayo Clinic
Risks
First trimester screening is a routine prenatal screening test. The screening poses no risk of miscarriage or other pregnancy complications.
How you prepare
You don't need to do anything special to prepare for first trimester screening. You can eat and drink normally before both the blood test and the ultrasound exam.
What you can expect
First trimester screening includes a blood draw and an ultrasound exam.
During the blood test, a member of your health care team takes a sample of blood by inserting a needle into a vein in your arm. The blood sample is sent to a lab for analysis. You can return to your usual activities immediately.
For the ultrasound exam, you'll lie on your back on an exam table. Your health care provider or an ultrasound technician will place a transducer — a small plastic device that sends and receives sound waves — over your abdomen. The reflected sound waves will be digitally converted into images on a monitor. Your health care provider or the technician will use these images to measure the size of the clear space in the tissue at the back of your baby's neck.
The ultrasound doesn't hurt, and you can return to your usual activities immediately.
Results
Your health care provider will use your age and the results of the blood test and ultrasound exam to gauge your risk of carrying a baby with Down syndrome or trisomy 18. Other factors — such as a prior Down syndrome pregnancy — also might affect your risk.
First trimester screening results are given as positive or negative and also as a probability, such as a 1 in 250 risk of carrying a baby with Down syndrome.
First trimester screening correctly identifies about 85 percent of women who are carrying a baby with Down syndrome. About 5 percent of women have a false-positive result, meaning that the test result is positive but the baby doesn't actually have Down syndrome.
When you consider your test results, remember that first trimester screening indicates only your overall risk of carrying a baby with Down syndrome or trisomy 18. A low-risk result doesn't guarantee that your baby won't have one of these conditions. Likewise, a high-risk result doesn't guarantee that your baby will be born with one of these conditions.
If you have a positive test result, your health care provider and a genetics professional will discuss your options, including additional testing. For example:
- Prenatal cell-free DNA (cfDNA) screening. This is a sophisticated blood test that examines fetal DNA in the maternal bloodstream to determine whether your baby is at risk of Down syndrome, extra sequences of chromosome 13 (trisomy 13) or extra sequences of chromosome 18 (trisomy 18). Some forms of cfDNA screening also screen for other chromosome problems and provide information about fetal sex. A normal result might eliminate the need for a more invasive prenatal diagnostic test.
- Chorionic villus sampling (CVS). CVS can be used to diagnose chromosomal conditions, such as Down syndrome. During CVS, which is usually done during the first trimester, a sample of tissue from the placenta is removed for testing.
 CVS poses a small risk of miscarriage.
CVS poses a small risk of miscarriage. - Amniocentesis. Amniocentesis can be used to diagnose both chromosomal conditions, such as Down syndrome, and neural tube defects, such as spina bifida. During amniocentesis, which is usually done during the second trimester, a sample of amniotic fluid is removed from the uterus for testing. Like CVS, amniocentesis poses a small risk of miscarriage.
Your health care provider or a genetic counselor will help you understand your test results and what the results mean for your pregnancy.
By Mayo Clinic Staff
Related
Products & Services
Screening for Down Syndrome - Bahçeci IVF Clinic
The desire of every future parent is to have a healthy child. During pregnancy, various tests are used to assess the health of the unborn baby. Tests such as ultrasounds and blood tests are used during pregnancy for screening purposes.
What is Screening?
Tests called screening tests are used to detect a specific disease in healthy people. Thanks to these tests, it is possible to intervene during the course of the disease, either before it occurs or at an early stage. The main screening tests for women's health are breast ultrasound for breast cancer and the PAP smear test for cervical cancer. But screening is not a diagnostic test. Additional tests are needed to confirm the diagnosis in patients at high risk of developing the disease. For example, taking a tissue sample (biopsy) from a suspicious area. These tests are called "diagnostic" tests.
Why Are Diagnostic Tests Not Used Right Away?
Screening tests are tests that can be applied to all people, are inexpensive, and cause the least discomfort to patients. Diagnostic tests are expensive operations that require special interventions, knowledge and equipment. For example, to diagnose Down's syndrome, it is necessary to perform an amniocentesis (analysis of the amniotic fluid in which the baby is located). This procedure requires an experienced doctor, ultrasound, as well as a genetic laboratory and a specialist geneticist for chromosome analysis. Because of the risks and costs associated with them, diagnostic tests are only performed on pregnant women who have been identified as “high risk” of the disease.
This procedure requires an experienced doctor, ultrasound, as well as a genetic laboratory and a specialist geneticist for chromosome analysis. Because of the risks and costs associated with them, diagnostic tests are only performed on pregnant women who have been identified as “high risk” of the disease.
What is a Chromosome?
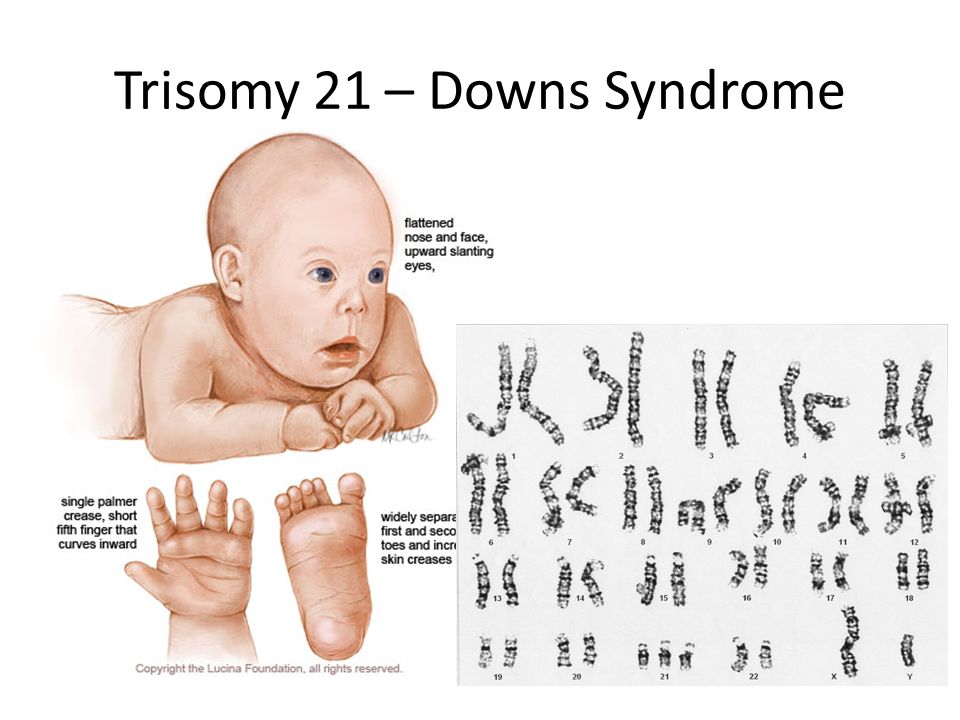
Chromosomal cells are the building blocks that contain the genetic information that makes us who we are and passes that information on to our children. Humans have 23 pairs of chromosomes. The pair of these chromosomes are the sex chromosomes (XY in males; XX in females).
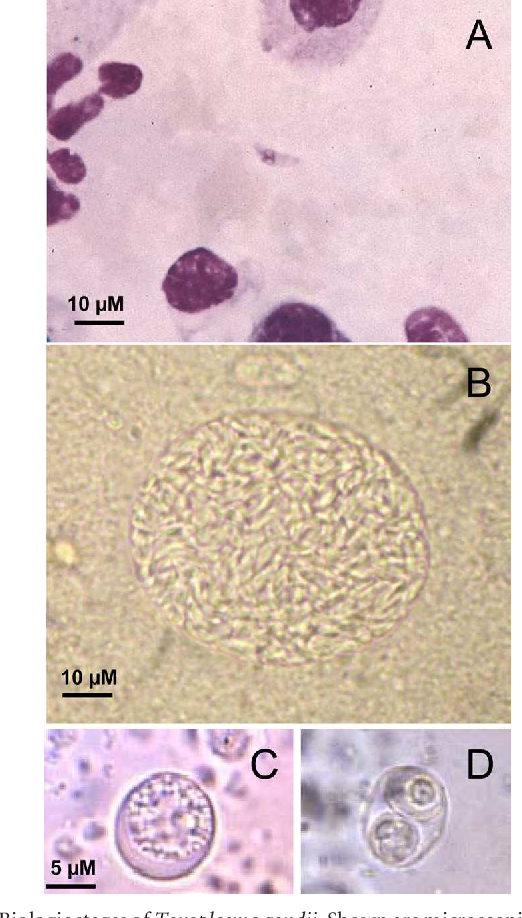
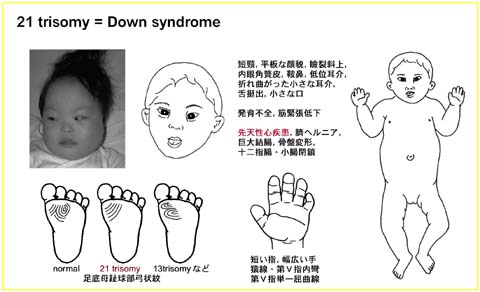
What is Down Syndrome?
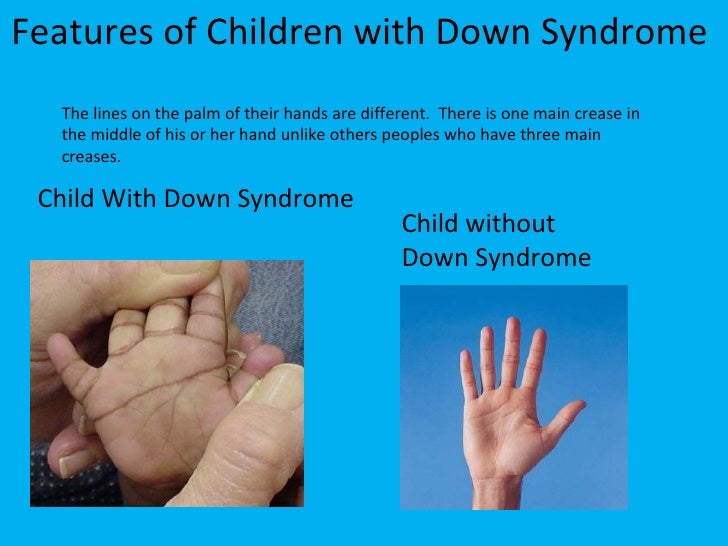
Down syndrome (trisomy 21) is a genetic disorder caused by an excess of part or all of chromosome 21. Children with Down syndrome have mild or severe mental retardation, learning difficulties, and physical retardation. They are also at high risk for heart abnormalities, reflux, recurrent ear infections, sleep disturbances, and thyroid disease. One child with Down syndrome is born in 800-1000 children.
One child with Down syndrome is born in 800-1000 children.
How is Down Syndrome screened during pregnancy?
At 10-14 and 16-18 weeks of pregnancy, biochemical analyzes of the mother's blood are performed. At weeks 10-14, free beta hCG and PAPP-A tests are done, and at weeks 16-18, alpha-fetoprotein, beta-hCG and estriol levels are checked. These tests are not "intelligence tests". As you know, IQ tests are written and oral exams, not blood tests. Therefore, the definition of "intellectual test" is used incorrectly.
First Trimester Screening
Obstetricians describe the pregnancy process by dividing it into three periods (trimesters). The first 14 weeks are called the first trimester. Between 10 and 14 weeks of pregnancy, your doctor will use ultrasound to measure your baby's age, heart rate, and nasal bone. Also at this time, the child's collar zone (NT) is measured.
Second Trimester Screening
In the second trimester of pregnancy, between 16 and 18 weeks, the next screening is done. A blood sample is taken from the expectant mother and examined for alpha-fetoprotein, beta hCG and estriol. The risk is calculated from the results of these tests.
A blood sample is taken from the expectant mother and examined for alpha-fetoprotein, beta hCG and estriol. The risk is calculated from the results of these tests.
What are the Risks?
So what does high risk and low risk mean?
The screening test is not a diagnostic test. Its goal is to refer only pregnant women at high risk of having a baby with Down's syndrome for further, more serious investigations (chromosomal analysis and amniocentesis).
A “high risk” or “positive” result does not mean your child has Down syndrome. On the other hand, "low risk" or "negative" does not mean that your child will not have Down syndrome either. According to statistics, out of 10 children with Down syndrome, screening reveals 9, but one baby with this diagnosis is born into the world.
Is screening done for multiple pregnancies?
In multiple pregnancies, maternal blood counts are not used for screening purposes. Between 10 and 14 weeks of pregnancy, measurements of the collar zone and nasal bone are taken, and ultrasound is done in the second trimester. However, it should be remembered that ultrasound evaluation is less accurate than maternal blood tests. Measurement of the collar zone in the first trimester allows you to correctly diagnose 7 out of 10 cases with Down syndrome.
However, it should be remembered that ultrasound evaluation is less accurate than maternal blood tests. Measurement of the collar zone in the first trimester allows you to correctly diagnose 7 out of 10 cases with Down syndrome.
Suggestions:
Please talk to your doctor about the need for the above tests. We wish you an easy pregnancy!
Screening tests for Down syndrome in the first 24 weeks of pregnancy
Relevance
Down's syndrome (also known as Down's disease or Trisomy 21) is an incurable genetic disorder that causes significant physical and mental health problems and disability. However, Down syndrome affects people in completely different ways. Some have significant symptoms, while others have minor health problems and are able to lead relatively normal lives. There is no way to predict how badly a child might be affected.
Parents-to-be during pregnancy are given the opportunity to have a screening test for Down's Syndrome in their baby to help them make a decision. If a mother is carrying a child with Down syndrome, then a decision should be made whether to terminate the pregnancy or keep it. The information gives parents the opportunity to plan life with a child with Down syndrome.
If a mother is carrying a child with Down syndrome, then a decision should be made whether to terminate the pregnancy or keep it. The information gives parents the opportunity to plan life with a child with Down syndrome.
The most accurate screening tests for Down syndrome include amniotic fluid (amniocentesis) or placental tissue (chorionic villus biopsy (CVS)) to look for abnormal chromosomes associated with Down syndrome. Both of these tests involve inserting a needle into the mother's abdomen, which is known to increase the risk of miscarriage. Thus, screening tests are not suitable for all pregnant women. Therefore, more often take blood and urine tests of the mother, and also conduct an ultrasound examination of the child. These screening tests are not perfect because they can miss cases of Down syndrome and are also at high risk of being positive when the child does not have Down syndrome. Thus, if a high risk is identified using these screening tests, further amniocentesis or CVS is required to confirm the diagnosis of Down syndrome.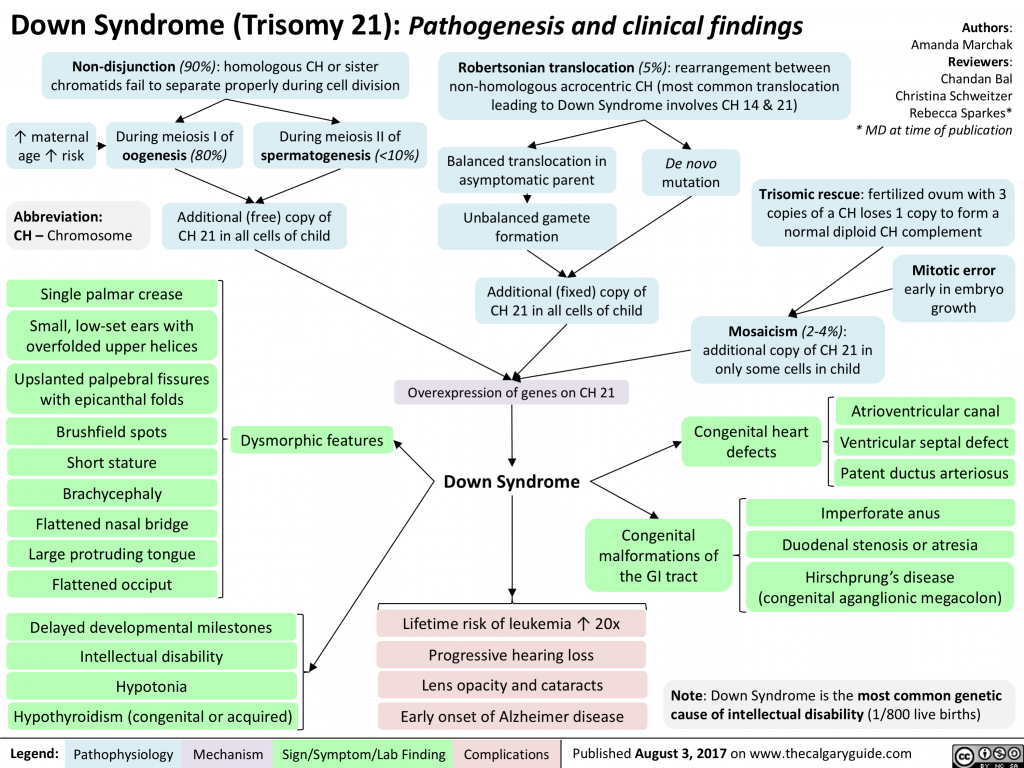
What we did
We analyzed combinations of serum screening tests in the first (up to 14 weeks) and second (up to 24 weeks) trimesters of pregnancy with or without ultrasound screening in the first trimester. Our goal was to identify the most accurate tests for predicting the risk of Down syndrome during pregnancy. One ultrasound index (neckfold thickness) and seven different serological indexes (PAPP-A, total hCG, free beta-hCG, unbound estriol, alpha-fetoprotein, inhibin A, ADAM 12) were studied, which can be used separately, in ratios or in combination with each other, obtained before 24 weeks of gestation, thereby obtaining 32 screening tests for the detection of Down's syndrome. We found 22 studies involving 228615 pregnant women (including 1067 fetuses with Down syndrome).
What we found
During Down Syndrome screening, which included tests during the first and second trimesters that combined to determine overall risk, we found that a test that included neckfold measurement and PAPP- A in the first trimester, as well as the determination of total hCG, unbound estriol, alpha-fetoprotein and inhibin A in the second trimester, turned out to be the most sensitive, as it allowed to determine 9out of 10 pregnancies associated with Down syndrome.