What are the causes of miscarriage in early pregnancy
Miscarriage - Causes - NHS
There are many reasons why a miscarriage may happen, although the cause is often not identified.
If a miscarriage happens during the first trimester of pregnancy (the first 3 months), it's usually caused by problems with the unborn baby (foetus). About 3 in every 4 miscarriages happen during this period.
If a miscarriage happens after the first trimester of pregnancy, it may be the result of things like an underlying health condition in the mother.
These late miscarriages may also be caused by an infection around the baby, which leads to the bag of waters breaking before any pain or bleeding. Sometimes they can be caused by the neck of the womb opening too soon.
First trimester miscarriages
First trimester miscarriages are often caused by problems with the chromosomes of the foetus.
Chromosome problems
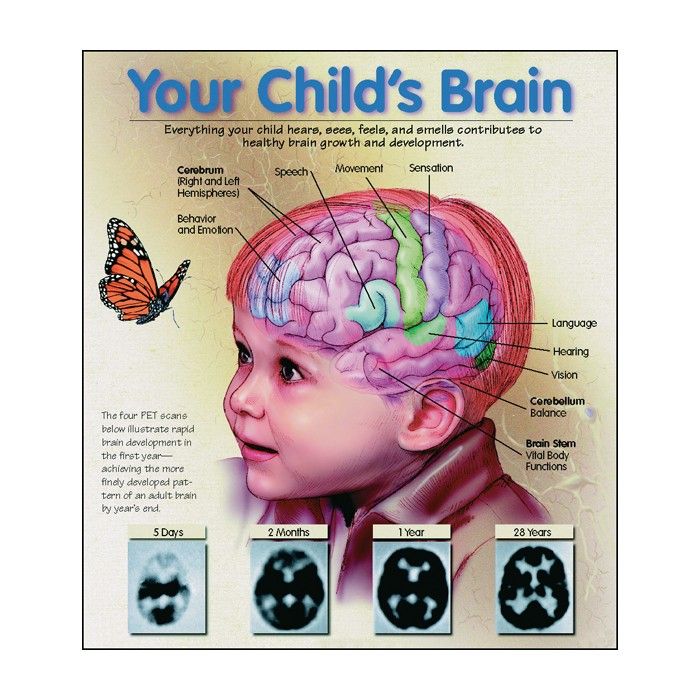
Chromosomes are blocks of DNA. They contain a detailed set of instructions that control a wide range of factors, from how the cells of the body develop to what colour eyes a baby will have.
Sometimes something can go wrong at the point of conception and the foetus receives too many or not enough chromosomes. The reasons for this are often unclear, but it means the foetus will not be able to develop normally, resulting in a miscarriage.
This is very unlikely to recur. It does not necessarily mean there's any problem with you or your partner.
Placenta problems
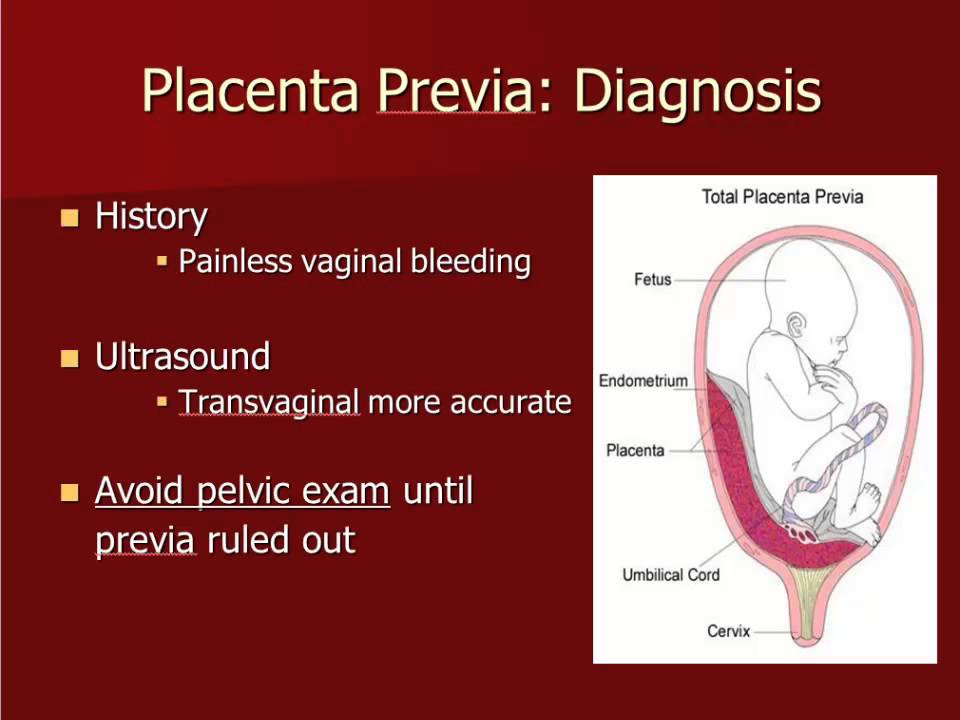
The placenta is the organ linking your blood supply to your baby's. If there's a problem with the development of the placenta, it can also lead to a miscarriage.
Things that increase your risk
An early miscarriage may happen by chance. But there are several things known to increase your risk of problems happening.
But there are several things known to increase your risk of problems happening.
Your age can also have an influence:
- in women under 30, 1 in 10 pregnancies will end in miscarriage
- in women aged 35 to 39, up to 2 in 10 pregnancies will end in miscarriage
- in women over 45, more than 5 in 10 pregnancies will end in miscarriage
A pregnancy may also be more likely to end in miscarriage if you:
- are obese
- smoke
- use drugs
- drink lots of caffeine
- drink alcohol
Second trimester miscarriages
Long-term health conditions
Several long-term (chronic) health conditions can increase your risk of having a miscarriage in the second trimester, especially if they're not treated or well controlled.
These include:
- diabetes (if it's poorly controlled)
- severe high blood pressure
- lupus
- kidney disease
- an overactive thyroid gland (hyperthyroidism)
- an underactive thyroid gland (hypothyroidism)
- antiphospholipid syndrome (APS)
Infections
The following infections may also increase your risk:
- rubella (german measles)
- cytomegalovirus (CMV)
- bacterial vaginosis
- HIV
- chlamydia
- gonorrhoea
- syphilis
- malaria
Food poisoning
Food poisoning, caused by eating contaminated food, can also increase the risk of miscarriage. For example:
For example:
- listeriosis – most commonly found in unpasteurised dairy products, such as blue cheese
- toxoplasmosis – which can be caught by eating raw or undercooked infected meat
- salmonella – most often caused by eating raw or partly cooked eggs
Read more about foods to avoid in pregnancy.
Medicines
Medicines that increase your risk include:
- misoprostol – used for stomach ulcers
- retinoids – used for eczema and acne
- methotrexate – used for conditions such as rheumatoid arthritis
- non-steroidal anti-inflammatory drugs (NSAIDs) – such as ibuprofen; these are used for pain and inflammation
To be sure a medicine is safe in pregnancy, always check with your doctor, midwife or pharmacist before taking it.
Read more about medicines during pregnancy.
Womb structure
Problems and abnormalities with your womb can also lead to second trimester miscarriages. Possible problems include:
- non-cancerous growths in the womb called fibroids
- an abnormally shaped womb
Weakened cervix
In some cases, the muscles of the cervix (neck of the womb) are weaker than usual. This is known as a weakened cervix or cervical incompetence.
A weakened cervix may be caused by a previous injury to this area, usually after a surgical procedure. The muscle weakness can cause the cervix to open too early during pregnancy, leading to a miscarriage.
Polycystic ovary syndrome (PCOS)
Polycystic ovary syndrome (PCOS) is a condition where the ovaries are larger than normal. It's caused by hormonal changes in the ovaries.
It's caused by hormonal changes in the ovaries.
PCOS is known to be a leading cause of infertility as it can prevent the release of an egg (ovulation). There's some evidence to suggest it may also be linked to an increased risk of miscarriage.
Misconceptions about miscarriage
An increased risk of miscarriage is not linked to:
- your emotional state during pregnancy, such as being stressed or depressed
- having a shock or fright during pregnancy
- exercise during pregnancy – but discuss with your GP or midwife what type and amount of exercise is suitable for you during pregnancy
- lifting or straining during pregnancy
- working during pregnancy – or work that involves sitting or standing for long periods
- having sex during pregnancy
- travelling by air
- eating spicy food
Recurrent miscarriages
If you have had a miscarriage, it's natural to worry that you'll have another if you get pregnant again. But most miscarriages are a one-off event.
But most miscarriages are a one-off event.
About 1 in 100 women experience recurrent miscarriages (3 or more in a row) and many of these women go on to have a successful pregnancy.
Page last reviewed: 09 March 2022
Next review due: 09 March 2025
Causes, Symptoms, Risks, Treatment & Prevention
Overview
What is a miscarriage?
A miscarriage (also called a spontaneous abortion) is the unexpected ending of a pregnancy in the first 20 weeks of gestation. Just because it’s called a “miscarriage” doesn’t mean you did something wrong in carrying the pregnancy. Most miscarriages are beyond your control and occur because the fetus stops growing.
Types of miscarriage
Your pregnancy care provider may diagnose you with the following types of miscarriage:
- Missed miscarriage: You’ve lost the pregnancy but are unaware it’s happened. There are no symptoms of miscarriage, but an ultrasound confirms the fetus has no heartbeat.

- Complete miscarriage: You’ve lost the pregnancy and your uterus is empty. You’ve experienced bleeding and passed fetal tissue. Your provider can confirm a complete miscarriage with an ultrasound.
- Recurrent miscarriage: Three consecutive miscarriages. It affects about 1% of couples.
- Threatened miscarriage: Your cervix stays closed, but you’re bleeding and experiencing pelvic cramping. The pregnancy typically continues with no further issues. Your pregnancy care provider may monitor you more closely for the rest of your pregnancy.
- Inevitable miscarriage: You’re bleeding, cramping and your cervix has started to open (dilate). You may leak amniotic fluid. A complete miscarriage is likely.
How do I know if I’m having a miscarriage?
You may not be aware you’re having a miscarriage. In people who have symptoms of a miscarriage, the most common signs are:
- Bleeding that progresses from light to heavy.
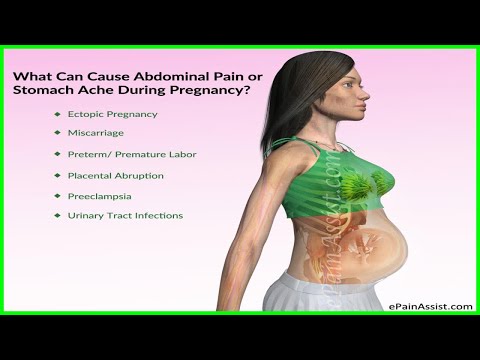 You may also pass grayish tissue or blood clots.
You may also pass grayish tissue or blood clots. - Cramps and abdominal pain (usually worse than menstrual cramps).
- Low back ache that may range from mild to severe.
- A decrease in pregnancy symptoms.
Contact your pregnancy care provider right away if you’re experiencing any of these symptoms. They will tell you to come into the office or go to the emergency room.
Symptoms and Causes
What causes miscarriage?
Chromosomal abnormalities cause about 50% of all miscarriages in the first trimester (up to 13 weeks) of pregnancy. Chromosomes are tiny structures inside the cells of your body that carry your genes. Genes determine all of a person’s physical attributes, such as assigned sex, hair and eye color and blood type.
During fertilization, when the egg and sperm join, two sets of chromosomes come together. If an egg or sperm has more or fewer chromosomes than normal, the fetus will have an abnormal number. As a fertilized egg grows into a fetus, its cells divide and multiply several times. Abnormalities during this process also leads to miscarriage.
Abnormalities during this process also leads to miscarriage.
Most chromosomal problems occur by chance. It’s not completely known why this happens.
Several factors may cause miscarriage:
- Infection.
- Exposure to TORCH diseases.
- Hormonal imbalances.
- Improper implantation of fertilized egg in your uterine lining.
- How old you are.
- Uterine abnormalities.
- Incompetent cervix (your cervix begins to open too early in pregnancy).
- Lifestyle factors such as smoking, drinking alcohol or using recreational drugs.
- Disorders of the immune system like lupus.
- Severe kidney disease.
- Congenital heart disease.
- Diabetes that is not controlled.
- Thyroid disease.
- Radiation.
- Certain medicines, such as the acne drug isotretinoin (Accutane®).
- Severe malnutrition.
There is no scientific proof that stress, exercise, sexual activity or prolonged use of birth control pills cause miscarriage. Whatever your situation is, it’s important to not blame yourself for having a miscarriage. Most miscarriages have nothing to do with something you did or didn’t do.
Whatever your situation is, it’s important to not blame yourself for having a miscarriage. Most miscarriages have nothing to do with something you did or didn’t do.
How painful is a miscarriage?
Miscarriages are different for every person. Some people have painful cramping, while other people have cramps similar to their menstrual period. The type of miscarriage you have may also affect your pain level. For example, if you have a complete miscarriage at home, you may have more pain than a person who has a missed miscarriage and has a surgical procedure to remove the pregnancy.
What happens first during a miscarriage?
It’s hard to say what happens first during a miscarriage because everyone’s symptoms are different. Sometimes there are no signs of miscarriage, and you find out at a prenatal ultrasound that you’ve lost the pregnancy. Most people will experience some degree of cramping and bleeding, but what happens first varies.
How long does a miscarriage take?
It depends. Some people have painful cramping and heavy bleeding longer than others. Your pregnancy care provider can tell you what to expect and give you advice on how to manage pain and cramps during your miscarriage.
Some people have painful cramping and heavy bleeding longer than others. Your pregnancy care provider can tell you what to expect and give you advice on how to manage pain and cramps during your miscarriage.
What are the risk factors for a miscarriage?
A risk factor is a trait or behavior that increases a person’s chance of developing a disease or condition. Risk factors for miscarriage include:
- Your age: Studies show that the risk of miscarriage is 12% to 15% for people in their 20s and rises to about 25% for people by age 40. Most age-related miscarriages happen because of a chromosomal abnormality (the fetus has missing or extra chromosomes).
- Previous miscarriage: You have a 25% chance of having another miscarriage (only slightly higher than someone who hasn’t had a miscarriage) if you’ve already had one.
- Health conditions: Certain health conditions like unmanaged diabetes, infections or issues with your uterus or cervix increase your chance of miscarriage.

Talk to your pregnancy care provider about the risk factors for miscarriage. They can discuss your risk after they’ve reviewed your medical history.
How many people have miscarriages?
Between 10% and 20% of all known pregnancies end in miscarriage. Most miscarriages (80%) happen within the first three months of pregnancy (up to 13 weeks of pregnancy). Less than 5% of miscarriages occur after 20 weeks’ gestation.The rate of miscarriage may be higher if you consider miscarriages that happen shortly after implantation. A person may not realize they’re pregnant because bleeding happens around the time of their menstrual period. This is called a chemical pregnancy.
What is my risk of miscarriage by week?
Your risk of pregnancy loss declines each week you’re pregnant. Around 15% of pregnancies end in miscarriage. Miscarriage risk in the second trimester (13 to 19 weeks) is between 1% and 5%. Many factors affect your risk of miscarriage such as your age and health. However, everyone’s risk of miscarriage declines each week of pregnancy if the pregnant person has no other health conditions.
However, everyone’s risk of miscarriage declines each week of pregnancy if the pregnant person has no other health conditions.
Diagnosis and Tests
How is a miscarriage diagnosed?
Your pregnancy care provider will perform an ultrasound test to confirm a miscarriage. These tests check for fetal heartbeat or the presence of a yolk sac (one of the first fetal structures your provider can see on ultrasound).
You may also have a blood test to measure human chorionic gonadotropin (hCG), a hormone produced by the placenta. A low hCG level can confirm a miscarriage.
Finally, your provider may perform a pelvic exam to check if your cervix has opened.
Management and Treatment
What are the treatments for a miscarriage?
If you experience the loss of a pregnancy, the fetus must be removed from your uterus. If any parts of the pregnancy are left inside your body, you could experience infection, bleeding or other complications.
If the miscarriage is complete and your uterus expels all the fetal tissue, then no further treatment is usually needed. Your pregnancy care provider will conduct an ultrasound to make sure there’s nothing left in your uterus.
Your pregnancy care provider will conduct an ultrasound to make sure there’s nothing left in your uterus.
If your body doesn’t remove all the tissue on its own or you haven’t started to bleed, your pregnancy care provider will recommend removing the tissue with medication or surgery.
Nonsurgical treatment
Your pregnancy care provider may recommend waiting to see if you pass the pregnancy on your own. This may be the case if you have a missed miscarriage. Waiting for a miscarriage to start could take several days. If waiting to pass the tissue isn’t safe or you wish to remove the tissue as soon as possible, they may recommend taking a medication that helps your uterus pass the pregnancy. These options are typically only available if you’ve miscarried before 10 weeks of pregnancy.
If a miscarriage wasn’t confirmed, but you had symptoms of a miscarriage, your provider may prescribe bed rest for several days. You might be admitted to the hospital overnight for observation. When the bleeding stops, you may be able to continue with your normal activities. If your cervix is dilated, they may diagnose you with an incompetent cervix, and they may perform a procedure to close your cervix (cervical cerclage).
When the bleeding stops, you may be able to continue with your normal activities. If your cervix is dilated, they may diagnose you with an incompetent cervix, and they may perform a procedure to close your cervix (cervical cerclage).
Surgical treatment
Your provider may perform a dilation and curettage (D&C) or dilation and evacuation (D&E) if your uterus hasn’t passed the pregnancy or if you’re bleeding heavily. Surgery may also be the only option if your pregnancy is beyond 10 weeks’ gestation. During these procedures, your cervix is dilated, and any remaining pregnancy-related tissue is gently scraped or suctioned out of your uterus. Your provider performs these surgeries in a hospital, and you’ll be under anesthesia.
What are some of the symptoms after a miscarriage?
Spotting and mild discomfort are common symptoms after a miscarriage.
Contact your healthcare provider immediately if you have any of these symptoms as it could be signs of an infection:
- Heavy bleeding or worsening bleeding.

- Fever.
- Chills.
- Intense pain.
Don’t put anything inside your vagina for at least two weeks after a miscarriage. This includes tampons, sexual intercourse and fingers or sex toys. Your provider will schedule a follow-up appointment with you to discuss your recovery and any complications.
What tests should I have after repeat miscarriages?
Blood tests or genetic tests might be necessary if you’ve more than three miscarriages in a row (called repeated miscarriage). These include:
- Genetic tests: You and your partner can have blood tests, like karyotyping, to check for chromosome abnormalities. If tissue from the miscarriage is available, your provider may be able to test it for chromosome irregularities.
- Blood tests: You may have a blood test to check for autoimmune or hormone conditions that could be causing miscarriages.
Your provider may also look at your uterus using one of the following procedures:
- Hysterosalpingogram (an X-ray dye test of your uterus and fallopian tubes).
- Hysteroscopy (a test during which your provider views the inside of your uterus with a thin, telescope-like device).
- Laparoscopy (a procedure during which your provider views the pelvic organs with a lighted device).
Prevention
How can I prevent another miscarriage?
It’s usually not possible to prevent a miscarriage. If you have a miscarriage, it’s not because you did something to cause it. Taking care of your body is the best thing you can do. Some examples of ways to care for yourself include:
- Attending all your prenatal care appointments.
- Maintaining a weight that's healthy for you.
- Avoiding risk factors for miscarriage like drinking alcohol and smoking cigarettes.
- Taking a prenatal vitamin.
- Getting regular exercise and eating a healthy diet.
Outlook / Prognosis
Can I get pregnant after I’ve had a miscarriage?
Yes. Most people (87%) who have miscarriages have subsequent normal pregnancies and births. Having a miscarriage doesn’t necessarily mean you have a fertility problem. Remember, most miscarriages occur because of a chromosomal abnormality, not because of something you did.
Having a miscarriage doesn’t necessarily mean you have a fertility problem. Remember, most miscarriages occur because of a chromosomal abnormality, not because of something you did.
How soon can I get pregnant after a miscarriage?
The decision on when you should begin trying to get pregnant again is between you and your pregnancy care provider. Most people can get pregnant again after they’ve had one “normal” menstrual period.
Taking time to heal both physically and emotionally after a miscarriage is important. Counseling is available to help you cope with your loss. A pregnancy loss support group might also be a valuable resource to you and your partner. Ask your healthcare provider for more information about counseling and support groups. Above all, don’t blame yourself for the miscarriage. Take the time you need to grieve.
If you’ve had three miscarriages in a row, ask your provider about performing tests to figure out an underlying cause. You should use birth control until you receive the results. After your provider reviews the test results, they may suggest going off birth control and trying to conceive again.
After your provider reviews the test results, they may suggest going off birth control and trying to conceive again.
Living With
How can I cope with my miscarriage?
Losing a pregnancy can be devastating and leave you with a range of emotions and lots of questions. Healing emotionally from a miscarriage is often harder and longer than the physical healing. Take the time you need to grieve your loss. Talk to your partner, friends and family about your feelings or find a pregnancy loss support group online. Surround yourself with supportive people or seek professional counseling to help you cope with the loss.
A note from Cleveland Clinic
A miscarriage is a very emotional moment for expectant parents and it’s natural to grieve the loss. Remember that a miscarriage can’t be prevented, and it’s not caused by something you did wrong. It doesn’t mean that you can’t have children or that you’ll have another miscarriage. If you’re planning to become pregnant, reach out to your healthcare provider to discuss the timing of your next pregnancy and ask any questions you have. It’s OK to be sad. Find support from family, friends online support groups or a licensed counselor.
It’s OK to be sad. Find support from family, friends online support groups or a licensed counselor.
What are the main causes of miscarriage
Miscarriage is called spontaneous termination of pregnancy in the period from conception to the 37th week. With a term of termination of pregnancy up to 12 weeks, a spontaneous abortion of an early term is diagnosed; from the 13th to the 21st week - late spontaneous abortion; from the 22nd week, this is a preterm birth (up to a period of 36 weeks + 6 days, when an immature viable baby weighing 500 grams or more is born).
Habitual miscarriage is considered spontaneous abortion 2 times or more.
The frequency of miscarriage ranges from 10 to 25%; in the first trimester it can reach 50%, in the second trimester - 20%, in the third trimester - 30%.
Any questions?
Leave the phone -
and we will call you back
Reasons for miscarriage
The causes of miscarriage are many and varied. Conventionally, they can be divided into the following main groups: anatomical and functional changes in the genital organs; immunological factors; gene and chromosomal disorders; environmental factors; infectious factors; hereditary and acquired defects of hemostasis.
Conventionally, they can be divided into the following main groups: anatomical and functional changes in the genital organs; immunological factors; gene and chromosomal disorders; environmental factors; infectious factors; hereditary and acquired defects of hemostasis.
The development of functional changes can be facilitated by infectious diseases, especially in childhood and puberty, artificial abortions, inflammatory diseases of the genital organs, impaired functional state of the endocrine glands (neuroendocrine disorders, functional changes in the adrenal glands, thyroid gland) after pathological childbirth, stressful situations, general diseases. In 64-74% of cases, the cause of abortion is hormonal insufficiency of the ovaries and placenta. Anatomical changes in the genital organs include infantilism (underdevelopment) of the uterus, uterine malformations (bicornuate or unicornuate, intrauterine septum), isthmic-cervical insufficiency (ICN), traumatic damage to the uterus during artificial abortion and childbirth, various tumors (uterine fibroids, ovarian tumors and etc. ), intrauterine synechia.
), intrauterine synechia.
Genital infantilism is characterized by a combination of such unfavorable factors as a deficiency of sex hormones, underdevelopment of the uterus, inferiority of its muscular layer, increased excitability, etc.
For isthmic-cervical insufficiency, the inferiority of the circular muscles in the area of the internal pharynx is characteristic, which contributes to the development of insufficiency of the isthmus and cervix. Organic failure develops as a result of trauma to the cervix during induced abortion, childbirth with a large fetus, operative delivery (obstetric forceps, vacuum aspiration of the fetus, etc.), inflammatory diseases of the cervix and vagina. Functional isthmic-cervical insufficiency is caused by infantilism and hormonal insufficiency, develops during pregnancy with hyperandrogenism and is observed more often than organic. Surgical correction of CI is carried out at the beginning of the second trimester of pregnancy in the conditions of hospitalization in a hospital, with the appearance of clinical signs - softening and shortening of the cervix.
Particularly noteworthy are infections whose pathogens penetrate the hematoplacental barrier, damaging the placenta and causing intrauterine infection of the fetus (toxoplasmosis, listeriosis, ricketenosis, chlamydia, rubella, cytomegalovirus, herpes, influenza, adenovirus infection, mumps, etc.)
Severe extragenital diseases (decompensated heart defects, hypertension, anemia, pyelonephritis, etc.)
Severe complications of the course of pregnancy lead to miscarriage - severe toxicosis of the first and second half of pregnancy, placenta previa and premature abruption, polyhydramnios and multiple pregnancies, and abnormal position of the fetus.
Among the causes of miscarriage, the histocompatibility system is of particular importance, which, even in the absence of autoimmune diseases, affects conception, implantation (implantation of the embryo) and the course of pregnancy. Recently, it has been established that the more HLA-gene allele matches in a married couple, the higher the probability of abortion.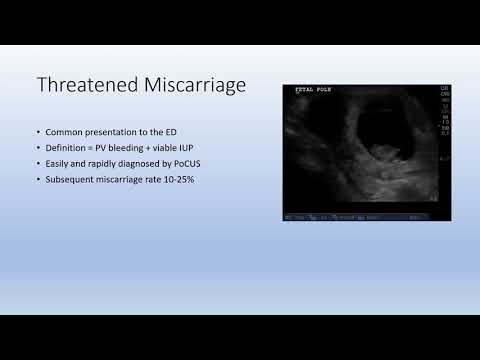 A large number of matching HLA class II antigens leads to a lack of a sufficient immune response in the mother, does not trigger special immune reactions in the mother's body aimed at maintaining pregnancy: special NK-killer cells (killers) that can provoke a miscarriage are blocked. The embryo is not recognized as a fetus, but is perceived as an accumulation of its own altered cells, against which the immune system begins to work for destruction. Currently, when immunological incompatibility of HLA gene partners is detected in spouses with habitual miscarriage and unsuccessful IVF attempts, active immunization of a woman (“vaccination”) with husband’s lymphocytes – lymphocytoimmunotherapy (LIT) is used as the main method of therapy.
A large number of matching HLA class II antigens leads to a lack of a sufficient immune response in the mother, does not trigger special immune reactions in the mother's body aimed at maintaining pregnancy: special NK-killer cells (killers) that can provoke a miscarriage are blocked. The embryo is not recognized as a fetus, but is perceived as an accumulation of its own altered cells, against which the immune system begins to work for destruction. Currently, when immunological incompatibility of HLA gene partners is detected in spouses with habitual miscarriage and unsuccessful IVF attempts, active immunization of a woman (“vaccination”) with husband’s lymphocytes – lymphocytoimmunotherapy (LIT) is used as the main method of therapy.
An important role in the etiology of spontaneous abortion in early pregnancy is played by chromosomal abnormalities leading to the death of the embryo, both due to hereditary factors and arising in the gametogenesis of the parents or in the early stages of zygote division.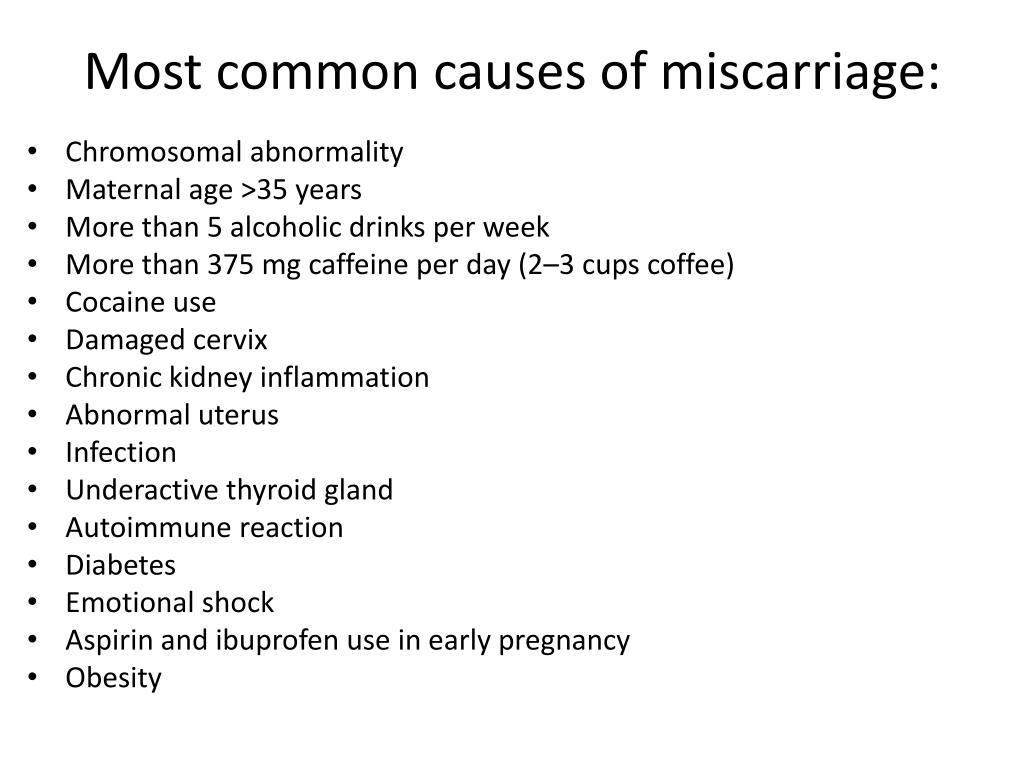 Cytogenetic study and molecular karyotyping of abortive material, carried out after vacuum aspiration or curettage of a missed pregnancy or anembryony, as well as a non-invasive prenatal DNA test (a high-tech method for studying fetal pathologies, which is based on the study of fragments of extracellular fetal DNA circulating in maternal blood and about 5-10% of the total amount of DNA in the blood) can detect major aneuploidies and other genetic abnormalities with an accuracy of 99%.
Cytogenetic study and molecular karyotyping of abortive material, carried out after vacuum aspiration or curettage of a missed pregnancy or anembryony, as well as a non-invasive prenatal DNA test (a high-tech method for studying fetal pathologies, which is based on the study of fragments of extracellular fetal DNA circulating in maternal blood and about 5-10% of the total amount of DNA in the blood) can detect major aneuploidies and other genetic abnormalities with an accuracy of 99%.
A significant role in miscarriage is occupied by thrombophilic conditions. Antiphospholipid syndrome is the cause of recurrent miscarriage in 40-60% of cases. In the first weeks of pregnancy, hemostasiogram monitoring is carried out every 7-10 days to select the dose of glucocorticoids and anticoagulants (heparin, fraxiparin, etc.).
Environmental factors include mechanical, physical, biological, chemical. As a result of their damaging action, the death of the embryo occurs or anomalies in its development occur, leading to spontaneous abortion. One of the main reasons is objectively smoking (in proportion to the number of cigarettes smoked), alcoholism and abuse of coffee and caffeinated drinks.
One of the main reasons is objectively smoking (in proportion to the number of cigarettes smoked), alcoholism and abuse of coffee and caffeinated drinks.
Examination for miscarriage
Examination of women who have suffered miscarriage and their treatment should be carried out before pregnancy. Treatment should be carried out taking into account the identified risk factors for miscarriage and must be combined with symptomatic therapy.
The doctor must study the hereditary history, working conditions, adverse social factors, previous diseases, chronic infections, extragenital pathology, find out the health of the husband, the harmfulness of working conditions, bad habits, carefully study the features of menstrual function. When studying the generative function in the presence of a history of abortion, the period at which it occurred, the nature of the treatment, the duration of primary infertility, the intervals in the onset of pregnancy between miscarriages, after induced abortion are specified.
During a general examination, it is important to assess the physique, the development of secondary genital organs, a gynecological examination reveals signs of genital infantilism, developmental anomalies, etc.
According to ultrasound, it is possible to identify signs of infantilism of the genital organs, tumors of the uterus and appendages, signs of anatomical pathology of the endocrine glands (thyroid gland, adrenal glands), preclinical signs of a threatened abortion (areas of hypertonicity of the uterine myometrium, chorion detachment), allows us to assess the size of the fetal egg, embryo , the fetus, to identify its cardiac activity and motor activity, the state of the internal pharynx of the cervix.
With hysteroscopy, pathological changes in the endometrium, the presence of submucosal uterine fibroids, internal endometriosis of the uterine body, septum and synechia in the uterine cavity and other pathologies can be detected.
Therapeutic and diagnostic laparoscopy allows you to find out the condition of the uterus, ovaries, fallopian tubes, adhesions in the pelvis, to perform surgical interventions to correct the identified pathology.
Hysterosalpingography, ultrasonohysteroscopy, MRI of the pelvic organs, hydrotubation, pertrubation, pneumopelpiography and radioisotope scanning allow us to assess the condition of the fallopian tubes, anomalies in the development of the uterus, genital infantilism, synechia in the uterine cavity, the state of the isthmic-cervical region, the presence of uterine fibroids, internal endometriosis of the uterine body, pathology of the endometrium.
To study the endocrine function of the ovaries, both functional diagnostic tests and a study of blood serum are used, which allows ovarian hypofunction, imbalance of hormonal homeostasis, as well as signs of hyperandrogenism of ovarian or adrenal genesis.
Methods of miscarriage treatment
Estradiol and progesterone preparations are used to correct ovarian hypofunction, and glucocorticoid preparations up to 16 weeks of pregnancy in case of hyperandrogenism, under the control of the concentration of 17-hydroxyprogesterone, dehydroepiandrosterone in the blood. For the correct choice of the dose of the prescribed drug, the content of sex hormones in the peripheral blood is determined in dynamics.
For the correct choice of the dose of the prescribed drug, the content of sex hormones in the peripheral blood is determined in dynamics.
The appointment of hormonal therapy with the threat of miscarriage in the early stages of pregnancy is carried out according to the basic principles:
-
a strict justification for the need for hormone therapy;
-
hormonal preparations are prescribed in the minimum effective doses during the first 14-18 weeks of pregnancy, progesterone preparations up to 36 weeks;
-
complex use of sex steroid hormones (estrogens are prescribed in combination with gestagens).
Women with miscarriage have a number of functional changes in the nervous system, which leads to the development of feelings of anxiety, tension, up to neurasthenia and psychasthenia. In such cases, the help of a psychologist, psychotherapy, and the appointment of sedatives are necessary.
In the complex of measures for the treatment of miscarriage, physiotherapeutic methods are widely used: endonasal electrophoresis of vitamin B1 in the first trimester of pregnancy, electrophoresis of magnesium with sinusoidal currents on the lower abdomen in the second half of pregnancy, central electronalgesia, acupuncture, hirudotherapy with an increase in blood clotting.
Rehabilitation in case of miscarriage
The complex of measures for the rehabilitation of women with habitual miscarriage includes several stages. At the first stage, a complex anti-inflammatory and restorative treatment is carried out. At the second stage, special research methods are used to identify the causes of miscarriage both on an outpatient basis and in a hospital. At the third stage, pathogenetic therapy is carried out. At the fourth stage, a complex of preventive and therapeutic measures is carried out at critical and individual critical periods aimed at maintaining pregnancy.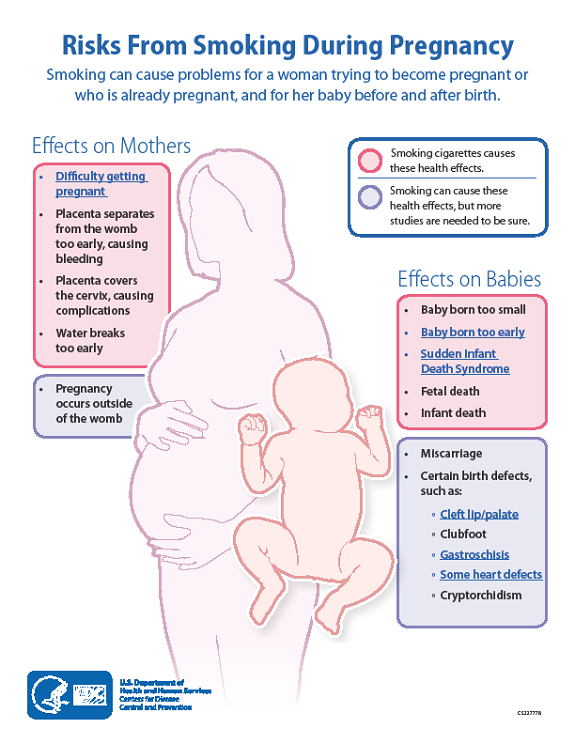
Regardless of the causative factors of miscarriage during pregnancy, placental insufficiency and chronic fetal hypoxia are prevented, which are usually observed in this pathology.
Thus, only an integrated approach to the formation of an individual plan for the treatment and rehabilitation of patients with miscarriage can prolong pregnancy in order to ensure the birth of a child.
Do not self-medicate. Contact our specialists who will correctly diagnose and prescribe treatment.
Rate how useful the material was
Thank you for rating
Miscarriage: primary and habitual, why miscarriage occurs
Miscarriage is a pathological condition that consists in the termination of (spontaneous) pregnancy for up to 37 weeks. If after the first miscarriage, appropriate treatment was not carried out, the risk of a second one increases. That is why it is important to consult a doctor in a timely manner. This will reduce the risks of recurrent miscarriage, eliminate existing pathologies and become pregnant.
It should be understood that there is nothing shameful in the diagnosis of "miscarriage", treatment should be carried out in a timely manner and by professionals!
Miscarriage is a problem that today has affected a huge number of women around the world. It negatively affects the birth rate and is important from the point of view of socio-economic development. Miscarriage, the causes of which are constantly being studied, depending on the time of occurrence, can be classified as spontaneous abortion (early: before 12 weeks, late: before 22 weeks) or preterm birth (early: from 22 to 28 weeks, late: from 28 to 37 weeks ).
Reasons
Miscarriage, the causes and treatment of which are being investigated by specialists, is a complex pathology.
Usually it is provoked by pathological conditions of the woman's body, immunological disorders in the "mother-placenta-fetus", chromosomal and gene disorders, socio-biological (physiological, chemical and other factors).
The causes of the pathological condition include:
- Induced abortions
- Metabolic disorders
- Anomalies in the structure of internal organs (mainly uterus)
- Immune system disorders
- Inflammation of the pelvic organs: gonorrhea, trichomoniasis, etc.
- Disturbance of blood flow in the uterus or placenta
Often, specialists diagnose not one, but several causes of miscarriage at once.
Early miscarriage
Early termination of pregnancy usually occurs due to pathologies of the endocrine system, genetic factors or inflammatory processes. Miscarriages in the second trimester are rare. If pathology occurs, it is usually under the influence of factors such as violations of blood clotting processes.
Provoke abortion in the early stages can and reasons such as:
- Myoma
- Anomalies in the structure of the uterus
- Placenta previa
Important! The threat of miscarriage exists constantly, not only in the early stages.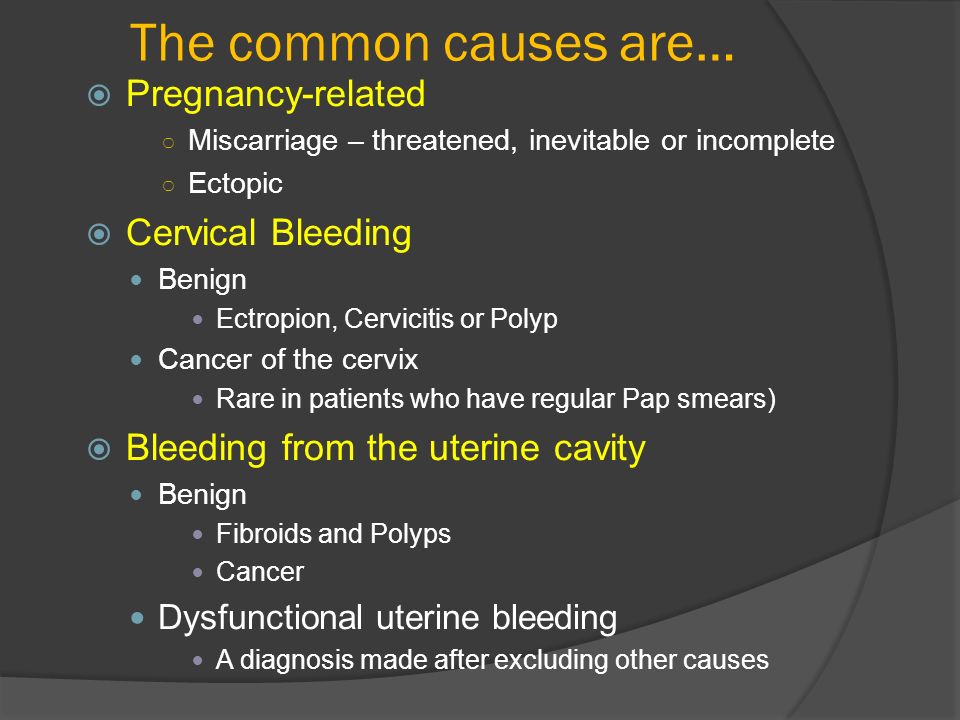 That is why you should be regularly examined in a antenatal clinic or a doctor in a large clinic. Only timely diagnosis will help to avoid a pathological condition and prevent miscarriage in the early or late stages. For any unusual sensations or signs, you should consult a doctor! So you can keep the pregnancy and bear a healthy baby, even if there is a predisposition to abortion.
That is why you should be regularly examined in a antenatal clinic or a doctor in a large clinic. Only timely diagnosis will help to avoid a pathological condition and prevent miscarriage in the early or late stages. For any unusual sensations or signs, you should consult a doctor! So you can keep the pregnancy and bear a healthy baby, even if there is a predisposition to abortion.
Recurrent miscarriage
The diagnosis of "recurrent miscarriage" is made if the interruption occurred more than 2-3 times in a row. A woman needs not only the supervision of a doctor, but also a thorough examination. All therapy is based on the factors and causes of miscarriage. If necessary, the patient is observed not only by a gynecologist, but also by an endocrinologist, geneticist, and other specialists. Particular attention is paid to finding out the main and additional reasons that provoked a miscarriage.
Risk of miscarriage
Miscarriage is a pathological condition that can occur today in almost every woman.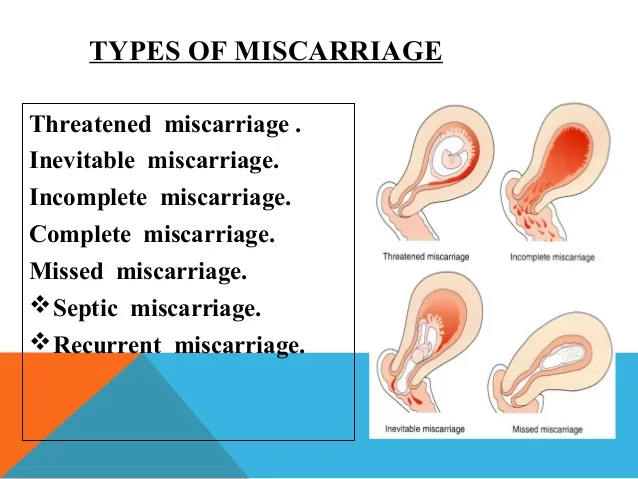
This is due to the fact that it is provoked by factors such as:
- Regular strenuous exercise
- Night shift work
- Exposure to stressors
- Smoking and drinking
- Abortion
- Caesarean section and other pelvic surgeries
- Genetics: miscarriage in mother or grandmother
- Age: under 16 and over 35
- Cardiovascular pathologies
- Diabetes mellitus
- Diseases of the kidneys
- Obesity 2-3 degrees
- Diseases of the thyroid gland
- Increased blood clotting, etc.
The cause of abortion (especially in the early stages) in some cases is even a common viral infection.
Pathology diagnostics
Diagnosis of pathology is carried out in the presence of clinical signs of miscarriage (persistent miscarriages, fetal growth retardation, stillbirths) and symptoms of a threatened abortion, which include bloody discharge from the genital tract and pulling pains in the lower abdomen at any stage of pregnancy.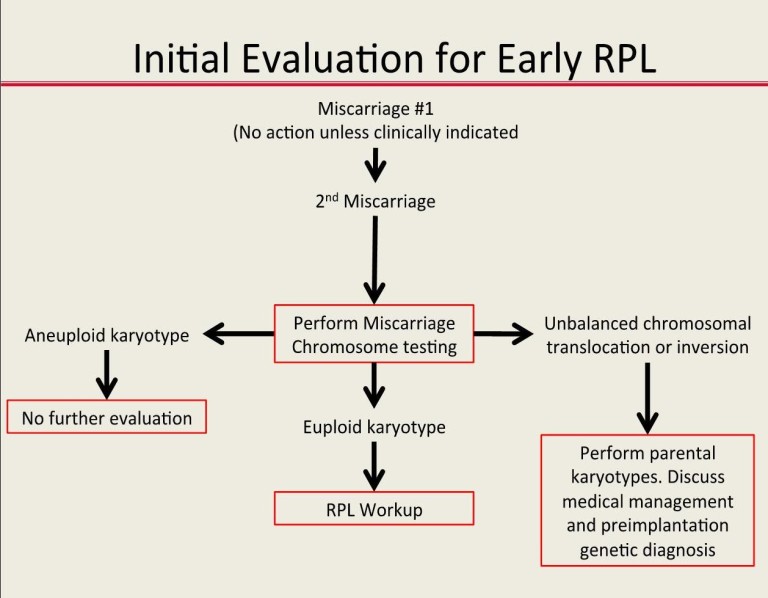
For the diagnosis of pathology are carried out:
General examination of the patient
The doctor performs it comprehensively, paying attention to:
- Body type
- Height to weight ratio
- Blood pressure readings
- Presence of skin striae
- Status of the liver
- Features of the cardiovascular system
- Expression of secondary sexual characteristics
The increased risk of miscarriage may be indicated by such signs as:
- Psycho-emotional instability of the patient
- Excessive sweating
- Paleness or blueness of the skin
- Rapid pulse
Gynecological examination
It consists in:
- Detection of scars on the cervix
- Determination of the dimensions of the external os of the cervical canal
- Neck fixings
- Identification of hair type
During a gynecological examination, a specialist can detect the presence of genital warts and other formations, as well as tumor processes, determine the size of the ovaries, detect inflammation and malformations of internal organs.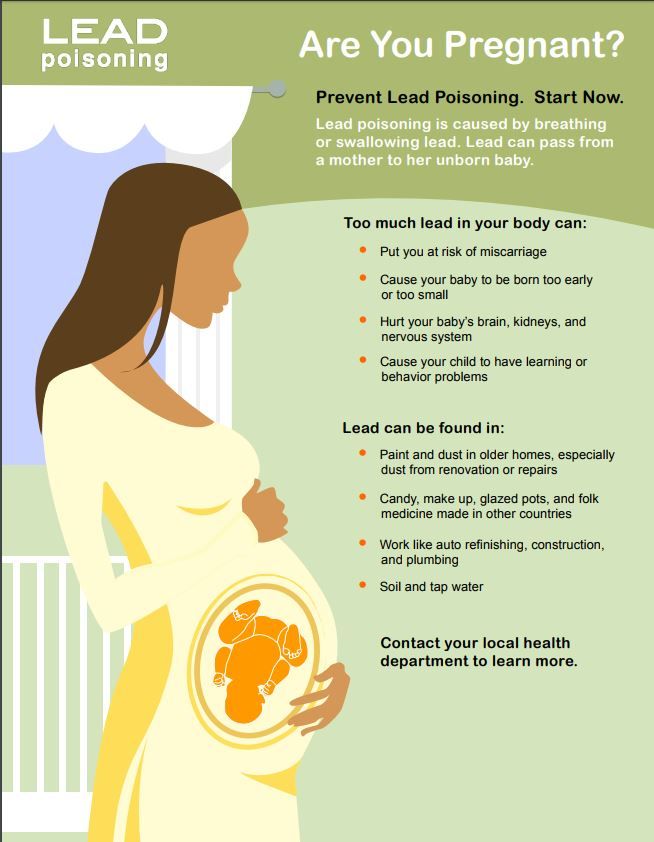
Special examinations
Diagnostics is carried out in two stages. At the first, the general condition of the reproductive system of the couple is assessed, at the second, the causes of the pathological condition (if it is detected) are specified.
Hormonal studies
When diagnosing, the causes of hormonal imbalance in the body are determined. Thanks to this study, doctors are able to quickly select the necessary means of therapy.
Analyzes are aimed at studying hormones such as:
- Progesterone
- Testosterone
- Thyroid-stimulating hormone, etc.
The full range of studies is voiced by a specialist.
Immunological testing
With such a diagnosis, indicators of immunoglobulins, growth hormone, thyroid hormones and other parameters are determined that determine the ability of a woman's body to bear a child.
Bacteriological tests
Such a diagnosis consists in the study:
- Vaginal, cervical and uterine materials
- Urine
- Blood
Experts determine not only the causative agents of the infection, but also the presence of antibodies to them.
Genetic research
Diagnostics is carried out at:
- Early termination of pregnancy
- History of stillbirth
- Couple over 35
The geneticist necessarily studies the pedigree of the couple, receives information that allows us to understand the regularity or randomness of the miscarriage factors.
Important! Diagnosis with suspicion of pathology is not only a woman, but also a man.
What tests and examinations are needed?
Women with suspicions of miscarriage and for an accurate diagnosis pass the following tests:
- Clinical analysis of urine and blood
- Biochemical blood test
- Rh factor and blood group determination
- Hormone profiling
- Virological testing
- Genetic diagnostics
- Immunological study
A pelvic ultrasound is also performed to determine ovulation.
The man will:
- Complete virological and genetic testing
- Take a spermogram
- Visit a urologist-andrologist for a comprehensive examination and consultation
Important! Only a comprehensive examination allows you to find out all the main and concomitant causes of miscarriage, after which you can develop an individual treatment plan, even with a combination of a number of factors that provoke miscarriages.
Examination: features of conducting
With such a pathology as miscarriage, tests are given by the patient and her partner all the time.
At the first visit to a pregnant gynecologist and registration, the following are carried out:
- History taking
- Gynecological examination
- ultrasound
- Laboratory tests (blood and urine tests)
When diagnosing thrombopholia (blood clotting disorders), the causes of the pathology are identified. Immediately after this, the necessary therapy is carried out. Be sure to study the indicator of TBG (marker of placental insufficiency). If the rate is reduced in the first trimester, the doctor may judge the risk of miscarriage.
At 15-20 weeks of pregnancy are carried out:
- Cervical examination
- ultrasound
- Vaginal and cervical swabs (for elevated leukocyte counts)
- Specialized tests to rule out Down's disease and other genetic abnormalities
At the 24th week of pregnancy, the following are performed:
- Glucose tolerance tests
- Transviganile ultrasound
- Manual examination of the cervix
- Cervical swabs
- Doppler study to determine placental and uterine blood flow
At week 32, the following are evaluated:
- Fetal activity
- Absence of antibodies in the blood (with negative Rh)
- Uterine contraction
- Bacteriological status (presence of infections in the vagina)
- Preterm Labor Markers
If necessary, the woman is hospitalized. It is aimed at the prevention of miscarriage and treatment in case of detection of pathological processes.
It is aimed at the prevention of miscarriage and treatment in case of detection of pathological processes.
At 37 weeks:
- Blood sugar test is taken
- WBC and total protein are assessed
- Determine the contractile function of the uterus
- Fetal assessment
- Smears being examined
- Hepatitis, HIV and AIDS tests are taken
Preparation for pregnancy in case of miscarriage and treatment
Preparation for pregnancy with a diagnosis of "miscarriage" is always carried out according to an individual scheme, which is developed in accordance with the patient's condition and the results of the diagnosis.
Preparation may include:
- Elimination of inflammatory processes
- Restoration of the immune status
- Correction of comorbidities
- Restoration of hormonal status
- Elimination of metabolic disorders, etc.
It usually takes at least 2-3 months to prepare for pregnancy.
The psychological support of the woman becomes obligatory.
It is important for specialists:
- Remove all psychological barriers
- Teach a woman to talk about a problem
- Set up the patient for a successful pregnancy
Preparation is impossible without the support of loved ones. In no case should you brush aside the problems of a woman who cannot bear a child. You should devote time to her problem, talk to her, tune in to a positive outcome of the upcoming pregnancy. Do not forget that one of the causes of the pathological condition is stress.
The treatment of miscarriage largely depends on the causes that provoked the difficulties.
Patients may be given:
- Herbal sedatives
- Antispasmodics
- Hormonal preparations
- Immunoglobulins
Treatment is possible with placental insufficiency, premature rupture of amniotic fluid, inflammatory and other negative and aggressive processes.
In some cases, partner treatment is also carried out.
Today, special attention is paid to the prevention of pathological conditions.
It is aimed at:
- Determination of factors provoking miscarriage
- Comprehensive couple examination
- Preparing for a successful pregnancy
- Mandatory control over the occurrence of complications during childbearing
- Taking special drugs
Prevention in a condition such as miscarriage can reduce complications (risks of their occurrence) by several times.
With the right approach, you can:
- Reduce the chances of miscarriage
- Prevent purulent infections, heavy bleeding, spread of infection during miscarriage
- Reduce the risk of preterm birth and neonatal death
Of course, in such a condition as miscarriage, rehabilitation after a miscarriage should be carried out only under the supervision of experienced professionals. A woman can undergo recovery both in a hospital and at home. The decision on hospitalization is made by the patient together with the doctor.
A woman can undergo recovery both in a hospital and at home. The decision on hospitalization is made by the patient together with the doctor.
Factors such as:
- Need for ongoing medical support
- Psychological status of the patient
- Presence of comorbidities
Benefits of treatment in MEDSI clinics
- Assistance to patients with primary and recurrent miscarriage at various times. Support is provided by experienced professionals who improve their skills
- Availability of facilities for comprehensive diagnostics of a woman and her partner. For examinations, modern installations of well-known manufacturers are used. Availability of own laboratory allows to carry out analyzes in the CITO mode (urgently)
- Use in diagnosis, treatment, prevention and rehabilitation of classical and modern methods
- Expert gynecological consultations providing a second opinion on your situation
- Opportunities for conservative and surgical treatment using modern drugs and innovative techniques and equipment
- Reproductive hemostasiologist appointment for bleeding disorders, which in some cases is the cause of miscarriage
- Full service provision to the woman and her partner
- Pre-pregnancy programs to reduce the risk of miscarriage
- Comfortable conditions and pleasant psychological atmosphere in clinics
- Opportunities for psychotherapeutic support
- Involvement of several doctors in the work with a patient
Make an appointment by calling +7 (495) 7-800-500.