Baby 6 week rash
Common childhood rashes | Pregnancy Birth and Baby
If your child has a seizure, call triple zero (000) immediately and ask for an ambulance.
If you think your child might have meningococcal rash, go to the nearest emergency department immediately.
Key facts
- There are many different types of childhood rashes. Many are not serious.
- If your child has a rash and fever, they should see their doctor.
- If your child has a meningococcal rash, go immediately to the emergency department.
Meningococcal rash
If you think your child might have meningococcal rash, go to the nearest emergency department immediately.
You can read more about serious childhood rashes here.
Rashes with no fever or itching
Milia (blocked oil glands)
Up to 1 in every 2 newborn babies develop small white spots called milia on their face, especially on the nose. These are just blocked pores, and they’re not itchy or contagious. They usually clear up without treatment within a few weeks.
Erythema toxicum
Many newborns develop a blotchy red skin reaction called erythema toxicum, which can appear between 2 days and 2 weeks after birth. Flat, red patches or small bumps often first appear on the face and spread to the body and limbs. The rash is harmless, not contagious, and will clear after a few days or a week.
Baby acne
Some babies get pimples on their cheeks and nose in the first three months of life. These pimples normally disappear without any treatment, usually within a few months.
Nappy rash
Nappy rash is inflammation of the skin in the nappy area. It can look red, sore and inflamed. Nappy rash is usually caused by urine (wee) or faeces (poo) irritating the skin.
To avoid nappy rash, keep the nappy area clean and dry with frequent nappy changes and nappy-free time. You can help protect the skin by putting on a barrier cream such as zinc or soft white paraffin at each nappy change.
Persistent nappy rash can be treated with a medicated cream. Don’t use talcum powder or antiseptics to treat nappy rash. If your baby develops a fungal infection, you’ll need to use an antifungal ointment. Ask your doctor or pharmacist for advice.
Erythema multiforme (minor)
Erythema multiforme is a rash triggered by an infection (most commonly herpes simplex virus), medicine or an illness. Your baby might feel unwell or have a mild fever before the rash appears. Red spots develop on the hands, feet, arms and legs and spread symmetrically across both sides of the body. The spots often become raised or blistered and then develop into classic target-like lesions.
Erythema multiforme is not contagious, and usually resolves without treatment in 3 to 6 weeks.
Keratosis pilaris (‘chicken skin’)
Keratosis pilaris is a harmless condition where the skin becomes rough and bumpy, as if permanently covered in goose pimples. These bumps most commonly occur on the upper arms and thighs. You can try several things to help the rash to clear up, including moisturising regularly.
You can try several things to help the rash to clear up, including moisturising regularly.
Rashes that might be itchy
Eczema (Atopic dermatitis)
Eczema is a very common skin condition affecting 1 in 3 Australians. It causes the skin to become itchy, red, dry and cracked, often in the creases at the knees and elbows.
Eczema commonly starts before a baby is 12 months old. Eczema follows a relapsing-remitting course. This means that there are flare-ups of the rash, followed by periods where there is no rash or a minimal rash.
Eczema management includes preventative treatment such as avoiding skin irritants, moisturising regularly and using bath oil. Treatment of flare-ups includes using steroid and anti-inflammatory creams.
Ringworm (tinea)
Ringworm is a common, contagious skin infection that causes a ring-like red rash with a clear centre. It commonly occurs on the scalp, feet and groin, but it can appear almost anywhere on the body.
Ringworm is caused by a fungus, not a worm, and is usually treated with over-the-counter antifungal creams. You should keep your child home from childcare or school until a day after you have started treatment to prevent spreading the infection.
You should keep your child home from childcare or school until a day after you have started treatment to prevent spreading the infection.
Prickly heat (heat rash)
Heat rash might appear if your baby gets hot in a humid environment. The rash shows as tiny red bumps or blisters on the skin, which can be very itchy. Cooling your baby down and avoiding humidity is the best way to prevent heat rash, which usually clears within 2 to 3 days without treatment.
Impetigo (school sores)
Impetigo is a highly contagious bacterial infection of the skin. It causes red sores and blisters that form a yellow crust. It is very common in children aged 2 to 6, and it is not usually serious in this age group, but it can be dangerous for newborn babies.
If your child has impetigo, you should see your doctor, who might prescribe an antibiotic cream, ointment or tablet. This should clear the infection within 7 to 10 days. Keep your child home from childcare or school and away from young babies until the sores have dried up, usually a few days after treatment starts.
Hives (urticaria)
Hives is a raised, red, itchy rash. It is common on the chest, stomach and back, as well as the throat and limbs, but it can appear on any part of the body. Hives usually disappears within a few days without any treatment. Antihistamines can be given to relieve itching. If the rash doesn't go away, you should see your doctor.
Hives isn’t usually serious, but it can be a sign of a more serious allergic reaction (anaphylaxis). If your child develops hives after eating, or together with other symptoms such as vomiting, dizziness or trouble breathing, you should seek urgent medical attention.
If your child has symptoms of a serious allergic reaction (anaphylaxis), call triple zero (000) immediately and ask for an ambulance.
Pityriasis rosea
Pityriasis rosea is a mild skin rash that sometimes appears after a sore throat, cold or fever. It begins with a single pink or tan-coloured patch on the chest or back. Red, oval-shaped patches, which may be itchy, then appear on the chest or back and limbs over the next weeks.
The exact cause of pityriasis rosea is unclear, and it is not thought to be contagious. The rash usually clears up within a couple of months without treatment.
If you are pregnant, pityriasis rosea can in rare cases lead to complications. See your doctor if you are pregnant and have contact with a child who has pityriasis rosea.
Molluscum contagiosum
Molluscum contagiosum is a viral skin infection that is spread by skin-to-skin contact or by sharing swimming pool water, bath water or towels.
Molluscum contagiosum spots look like pimples and grow into round pearly white lumps, usually 2 to 5 millimetres in size. They can be itchy. They usually heal without treatment within 6 months, but sometimes longer.
Rashes with fever
Slapped cheek disease (fifth disease)
Slapped cheek disease is a viral infection that mainly affects pre-school and school-age children. It typically causes a bright red rash on both cheeks that spreads as a ‘lacy’ rash on the body and limbs. Occasionally, it causes a fever.
Occasionally, it causes a fever.
Slapped cheek disease is usually mild and clears up in a few days without treatment. The child is contagious before the rash appears, but not once it has appeared.
If you are pregnant and catch the virus, it may cause a type of anaemia in your unborn baby. It can also cause miscarriage. If you suspect you or your child has slapped cheek disease, you should avoid contact with people who might be pregnant.
Hand, foot and mouth disease
Hand, foot and mouth disease is a mild but highly contagious viral illness. It causes a rash on the palms of the hands and soles of the feet and blisters in the mouth. It is not the same as the foot-and-mouth disease that affects farm animals.
The disease is common in childcare and kindergartens. Your child might feel unwell and have a fever and blisters on the hands and feet and in the mouth and in the nappy area. The illness usually lasts about 7 to 10 days. Children with hand, foot and mouth disease should stay away from childcare or school until all the blisters have dried up.
Hand, foot and mouth disease usually resolves on its own without complications. In rare cases, it can be more serious, especially if you have a weakened immune system or are pregnant. Complications can include infections of the brain and heart muscle and miscarriage.
Roseola infantum
Roseola infantum is a contagious viral infection that can cause cold-like symptoms and a high fever. The high fever may last for a few days. Roseola infantum can also cause some children to have a febrile convulsion (seizure).
Children with roseola infantum develop a rash after the fever has resolved. The rash looks like raised pink spots that start on the chest, stomach and back and spread to the limbs. The child is contagious before the rash appears, but not after. The rash usually lasts 3 to 5 days.
Febrile convulsions can look scary but are generally not harmful.
If your child has a seizure, call triple zero (000) immediately and ask for an ambulance.
When to seek help
Many babies develop a skin rash in their first days or weeks of life as their sensitive skin adapts to a new environment. Most rashes are harmless and go away on their own, but if your baby seems unwell, or if you’re worried, you should see your doctor. They can advise about the cause and whether treatment is necessary.
Most rashes are harmless and go away on their own, but if your baby seems unwell, or if you’re worried, you should see your doctor. They can advise about the cause and whether treatment is necessary.
Whatever their age, you should take your child to the doctor if they have a rash and persistent high temperature, cold or cough symptoms or swollen neck glands.
Treatment of common childhood rashes
If you think your child might be contagious, they should stay at home. Keep them away from school, childcare and other children. You should also keep them away from people who are pregnant, or who might be pregnant, since some childhood infections can cause serious problems in unborn babies.
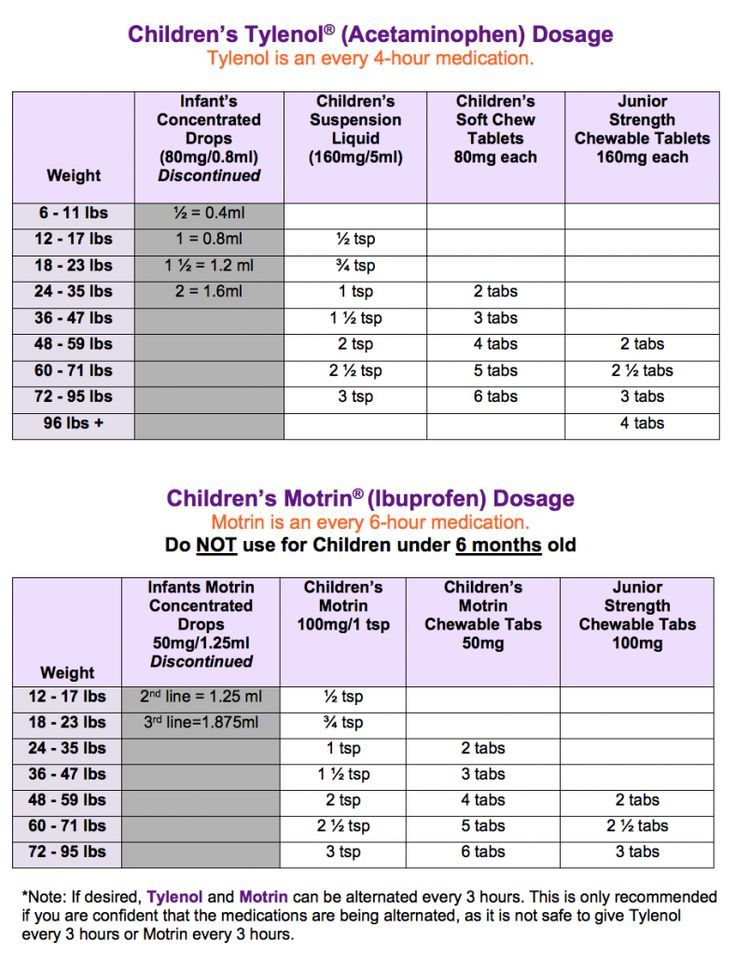
You can use paracetamol or ibuprofen (in babies aged over 3 months) to reduce fever — read the packet instructions carefully to ensure your child receives the right amount for their age and weight.
Your pharmacist can advise you on treating the symptoms of common rashes. For example, you can use over-the-counter creams to prevent itchiness.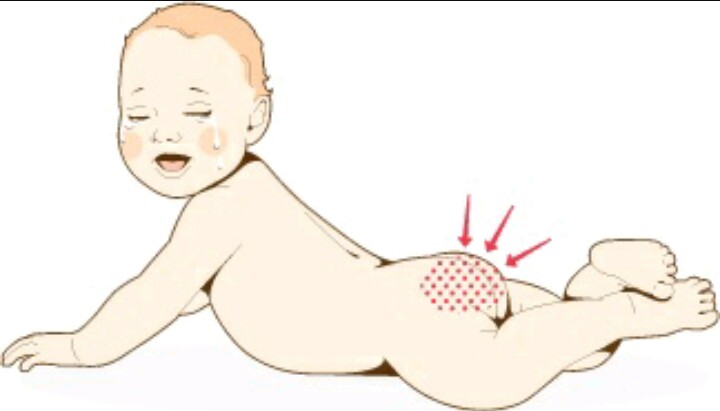
If you are concerned about your child’s rash, call Pregnancy, Birth and Baby on 1800 882 436 to talk to a maternal child health nurse, or call Healthdirect on 1800 022 022 to talk to a registered nurse. Alternatively, contact your doctor.
Speak to a maternal child health nurse
Call Pregnancy, Birth and Baby to speak to a maternal child health nurse on 1800 882 436 or video call. Available 7am to midnight (AET), 7 days a week.
Learn more here about the development and quality assurance of healthdirect content.
Newborn Rashes and Birthmarks
Is this your child's symptom?
- Normal skin rashes and birthmark questions about newborns
Newborn Rashes - Topics Covered
If your baby is healthy, skip the "What to Do" section. Go directly to the topic number that relates to your question for advice.
- Acne. Small red bumps on the face (onset 2-4 weeks).
- Drooling or Spit-Up Rash. Rash around the mouth and on the chin (onset anytime).

- Erythema Toxicum. Red blotches with small white "pimple" in the center (onset 2-3 days).
- Skin Injury from Birth Process. From forceps, scalp electrode or birth canal (present at birth).
- Milia. Tiny white bumps on the nose and cheeks (present at birth).
- Mongolian Spots. Bluish-green birthmark, often on buttock (present at birth).
- Stork Bites (Pink Birthmarks). On back of neck or bridge of nose (present at birth).
- Strawberry Hemangiomas. Raised red birthmarks (onset 2-4 weeks).
- Port-wine Stains. Dark red or purple flat birthmarks (present at birth).
Newborn Face Rashes: Most Common Ones
- Erythema Toxicum 50% (onset day 2 or 3)
- Milia 40% (present at birth)
- Baby Acne 30% (onset week 2 to 4)
- Drooling or Spit-up Rash (common and onset any time)
- Heat Rash (common and onset any time)
Heat Rash
- Many newborn rashes that have no clear cause are heat rashes.
- Heat rashes are a pink blotchy area with tiny bumps.

- They mainly occur on the face, neck and chest.
- During hot weather, most temporary newborn rashes are heat rashes.
- Cause: blocked off sweat glands. The openings are so tiny in newborns, that any irritation can block them. Examples are getting any ointment on the skin, friction from clothing or being overheated. Being held against the mother's skin while nursing causes many face rashes.
Herpes Simplex: Serious Newborn Rash
- Appearance. Several water blisters or pimples grouped in a cluster. They look like the cold sores (fever blisters) that adults get on their lip. After several days, they crust over.
- Location. Just one part of the body, usually the scalp or face.
- Redness. The base can be pink. The pinkness does not extend beyond the cluster of vesicles.
- Onset. Within the first 2 weeks of life.
- Importance. Early treatment with anti-viral drugs can prevent serious problems.
 If you think your newborn's rash looks like herpes, call your child's doctor now.
If you think your newborn's rash looks like herpes, call your child's doctor now. - Imitator. Although herpes can be confused with erythema toxicum, they look very different.
When to Call for Newborn Rashes and Birthmarks
Call 911 Now
- Not moving or very weak
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Age less than 1 month old and looks or acts abnormal in any way
- Fever in baby less than 12 weeks old. Caution: do NOT give your baby any fever medicine before being seen.
- Purple or blood-colored spots or dots not present at birth
- Tiny blisters (little bumps that contain clear fluid)
- Pimples (little bumps that contain pus). Exception: looks like erythema toxicum which occurs in half of newborns.
- Skin looks infected (such as spreading redness, sores or pus)
- Rash is painful to touch
- You think your child needs to be seen, and the problem is urgent
Contact Doctor Within 24 Hours
- You think your child needs to be seen, but the problem is not urgent
Contact Doctor During Office Hours
- Mild newborn rash, but cause is not clear
- You have other questions or concerns
Self Care at Home
- Normal newborn rashes or birthmarks
Seattle Children's Urgent Care Locations
If your child’s illness or injury is life-threatening, call 911.
- Bellevue
- Everett
- Federal Way
- Seattle
Care Advice for Newborn Rashes and Birthmarks
- Acne:
- More than 30 percent of newborns develop baby acne of the face. Acne consists of small red bumps.
- This baby acne begins at 2 to 4 weeks of age. It lasts until 4 to 6 months of age.
- The cause appears to be the transfer of maternal hormones just prior to birth.
- Since it goes away on its own, no treatment is needed.
 Baby oil or ointments make it worse.
Baby oil or ointments make it worse.
- Drooling or Spit-up Rash:
- Many babies have a rash on the chin or cheeks that comes and goes. This is often due to contact with food. It's more common after starting baby foods. In newborns, it can also be from stomach acid that has been spit up. Prolonged contact with spit-up during sleep can cause the rash to get worse.
- Other temporary rashes on the face are heat rashes. These can occur in areas held against the mother's skin during nursing. Heat rashes are more common in the summertime.
- Rinse the face with water after all feedings or spitting up. During hot weather, change the baby's position more often. Also, put a cool wet washcloth on the rash. Do this for 10 minutes.
- Erythema Toxicum:
- More than 50 percent of babies get a rash called erythema toxicum. It starts on the second or third day of life.
- It's a harmless baby rash that doesn't need to be seen.

- The rash is made up red blotches. They are ½ inch to 1 inch (1 to 2.5 cm). The blotches have a small white or yellow "pimple" in the center.
- They look like insect bites, but are not. Red blotches are the main feature.
- They can be numerous, keep occurring, and look terrible. They can occur anywhere on the body surface, except the palms and soles.
- Their cause is unknown, but they are not an infection.
- They go away by 1-2 weeks of age.
- No treatment is needed. Ointments or baby oil make it worse.
- Skin Injury from Forceps, Scalp Electrode or Birth Canal:
- The pressure of a forceps on the skin can leave marks. You may see bruises or scrapes anywhere on the head or face.
- During birth, skin overlying bony prominences can become damaged. You might see this on the sides of the skull bone. This is from pressure from the birth canal. Even without a forceps delivery, you may see bruises or scrapes.
- Scalp electrodes can also cause scalp scrapes and scabs.

- The bruises and scrapes will be noted at birth. They will be more noticeable by day 2. They heal over or go away by 1 - 2 weeks of age.
- A fat tissue injury won't appear until day 5 to 10. Look for a firm coin-shaped lump. It will be under the skin and sometimes with a scab. This lump may take 3 or 4 weeks to go away.
- For any breaks in the skin, apply an antibiotic ointment (such as Polysporin). No prescription is needed. Use 3 times per day until healed.
- Call Your Doctor If:
- It becomes tender to the touch
- Becomes soft in the center
- Starts to looks infected
- Milia:
- Milia are tiny white bumps that occur on the face. The nose and cheeks are most often involved. Milia can also be seen on the forehead and chin.
- Milia occur in 40 percent of newborn babies. Present at birth.
- Milia are many in number. They occur equally on both sides of the face.
- Although they look like pimples, they are much smaller (pinhead size).
 They are not infected.
They are not infected. - They do not look like water blisters.
- They are blocked-off skin pores. They will open up.
- Milia will go away by 1 to 2 months of age.
- No treatment is needed. Ointments or creams can make them worse.
- Mongolian Spots:
- A Mongolian spot is a normal bluish-green or bluish-gray flat birthmark. They occur in over 90 percent of Native American, Asian, Hispanic, and African American babies. They are also seen in 10 percent of Caucasians, especially those of Mediterranean descent.
- They are present at birth.
- They occur most commonly over the back and buttocks. However, they can be present on any part of the body.
- They vary greatly in size and shape.
- They do not indicate illness or any disease.
- Most fade away by 2 or 3 years of age. A trace may last into adult life.
- Stork Bites (Pink Birthmarks):
- Flat pink birthmarks that occur over the bridge of the nose or the eyelids.
 You can also find them on the back of the neck ("stork bites"). The ones in front are often referred to as "an angel's kiss".
You can also find them on the back of the neck ("stork bites"). The ones in front are often referred to as "an angel's kiss". - They occur in more than 50 percent of newborns. They are present at birth.
- All the birthmarks on the bridge of the nose and eyelids clear completely. Those on the eyelids clear by 1 year of age. Those on the bridge of the nose may last for a few more years. Those on the forehead from the nose up to the hairline usually last into adulthood. Laser treatment during infancy should be considered. Most birthmarks on the nape of the neck also clear. But, 25 percent can last into adult life.
- Flat pink birthmarks that occur over the bridge of the nose or the eyelids.
- Strawberry Hemangiomas:
- Strawberry hemangiomas are red birthmarks that are raised or increasing in size.
- Onset usually between 2-4 weeks of age. Most often, start after 3 weeks of age. Sometimes (although rare), they don't appear until the second month of life.
- They become larger for 1 year. Then, they fade away over 6 to 8 years without any treatment.
- They run a small risk of bleeding with trauma. Any bleeding should stop with 10 minutes of direct pressure.
- Discuss with your child's doctor on the next regular visit. Call sooner if you are concerned.
- Port-Wine Stain Birthmarks:
- Present at birth in 1 out of 200 newborns
- Deeper in color (dark red or purple) than stork bites (salmon patches)
- Flat, smooth surface
- Natural course: Do not fade or disappear like stork bites. May become darker.
- Grow with the child, but cover the same area
- Treatment: May refer to dermatologist for laser treatments early in infancy
- Call Your Doctor If:
- Your baby starts to look or act abnormal in any way
- You think your child needs to be seen
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
You, the reader, assume full responsibility for how you choose to use it.
Last Reviewed: 11/06/2022
Last Revised: 01/13/2022
Copyright 2000-2022. Schmitt Pediatric Guidelines LLC.
Rashes in infants | Rassvet Clinic
Babies are generous with various rashes. According to the "good" tradition, most of them are considered allergic with all the consequences - a strict diet for a nursing mother, transfer to artificial feeding, prescription of therapeutic mixtures, etc. In fact, true allergic rashes in infants are not so common. Allergic diseases affecting the skin in infants include: atopic dermatitis, acute urticaria and angioedema. Acute urticaria is extremely rare in infants - this is an acute allergic reaction in the form of peculiar rashes like blisters (as with a nettle burn, hence the name), which suddenly appear on the skin and just as suddenly disappear without leaving any trace, usually do not exist on the skin for longer than a day and are accompanied by severe itching, which manifests itself in the general anxiety of the child. The most common causes are dietary proteins (such as cow's milk), viral infections, insect bites, and drugs (such as antibiotics). In severe cases, it may be accompanied by swelling and redness of the soft tissues of the face, neck, larynx, arms, legs, genitals or abdominal cavity - Quincke's edema, which requires immediate medical attention.
The most common causes are dietary proteins (such as cow's milk), viral infections, insect bites, and drugs (such as antibiotics). In severe cases, it may be accompanied by swelling and redness of the soft tissues of the face, neck, larynx, arms, legs, genitals or abdominal cavity - Quincke's edema, which requires immediate medical attention.
Let's look at what is most often undeservedly called an allergy:
Toxic erythema newborns - a transient benign rash, the exact cause of the appearance is unknown (possibly due to skin irritation by environmental factors).
Appears at birth or in the first 24-48 hours of life. Localization - face, trunk, limbs, except for the palms and soles. Disappears on its own within 5-7 days, sometimes 3 weeks. Does not require treatment.
Neonatal acne (acne infancy, neonatal pustulosis) is caused by androgen stimulation of the baby's sebaceous glands.
Peak rash falls on the 3rd week of life. It is localized more often on the face, sometimes spreads to the scalp, less often to the collar zone. They resolve spontaneously. The skin needs cleansing and moisturizing, in some cases, the application of
It is localized more often on the face, sometimes spreads to the scalp, less often to the collar zone. They resolve spontaneously. The skin needs cleansing and moisturizing, in some cases, the application of
treatment creams may be required.
Sweating rash , which occurs in poorly "ventilated" areas as a result of blockage of the sweat glands. May occur at any age.
Localization - skin folds, buttocks and back surface of the body, sometimes the face (after sleep). Depending on the depth of the lesion, it happens - crystal prickly heat, prickly heat, deep prickly heat (superficial).
The duration of the rash is from several hours to several days.
Treatment - cool water baths, air baths, prevention of overheating. Lotions containing calamine and creams with corticosteroids and antibiotics may be used to treat some cases of red and deep prickly heat.
Seborrheic dermatitis is a skin disorder that develops in areas rich in sebum. The exact cause is unknown (a certain role is assigned to the skin saprophyte - the Malassezia fungus, which grows well and multiplies in the sebaceous secretion).
The exact cause is unknown (a certain role is assigned to the skin saprophyte - the Malassezia fungus, which grows well and multiplies in the sebaceous secretion).
It can be foci or widespread, dermatitis with bran-like scales, which can form a crust (“bonnet”, gneiss) on the scalp.
Favorite localization - scalp, face, folds (!).
May begin at 1-2 weeks of age or later, resolve spontaneously within weeks or months.
Treatment consists of softening the crusts with oil or cream and then removing them, moisturizing the skin and, in some cases, applying antifungal and anti-inflammatory creams.
Simple contact dermatitis is a non-specific skin injury due to prolonged or repeated exposure to a variety of substances - saliva, fruit juices, foaming bath products, detergents (their residues on the walls of the bath), etc. In infants, saliva is often causes dermatitis in the area of contact with the nipple and in the folds of the neck.
As a rule, removal of the damaging agent and short-term use of anti-inflammatory creams leads to a quick recovery, but some children are so sensitive that it is almost impossible to identify the causative factor.
Diaper dermatitis (prototype of contact dermatitis) is a skin lesion that occurs under the influence of physical (overheating), chemical, enzymatic (contact with sweat, urine and feces) and microbial factors. Localization - the area of the diaper or diaper fit.
Treatment is carried out using the abbreviation ABCDE (air, barrier, cleansing, diaper, education) - air, barrier, cleansing, diaper and parent education. Frequent diaper changes, washing the skin and drying it thoroughly help. Dermatitis is effectively prevented by the application to clean skin of products that completely cover it (Vaseline, zinc paste). In stubborn cases, medicated creams containing corticosteroids, antibiotics, or antifungals may be recommended.
And now a few words about AD:
Atopic dermatitis is a chronic allergic inflammation of the skin, genetically determined, associated with the loss of the skin barrier and, therefore, accompanied by dryness, itching and various rashes. In a third (!) of cases, it is combined with food allergies (the most common "culprits" are cow's milk, chicken eggs, wheat, fish, soy, nuts).
Starts more often not earlier than 3 months of life.
The most common localization up to 2-3 years is the face (cheeks, forehead, chin), convex parts of the limbs (extensor surfaces) and trunk, never in babies in folds (!).
Exacerbations are provoked by various factors - stress, dry air, sweat, food (histamine liberators), infections, contact with tobacco smoke, animal hair, coarse fabrics, detergent residues on clothing, etc.
Treated with careful skin care and using anti-inflammatory creams.
There are also:
Pseudo-allergic reactions are reactions that look similar to allergic reactions (for example, various rashes), but are not such, due to the non-immune mechanism of their development.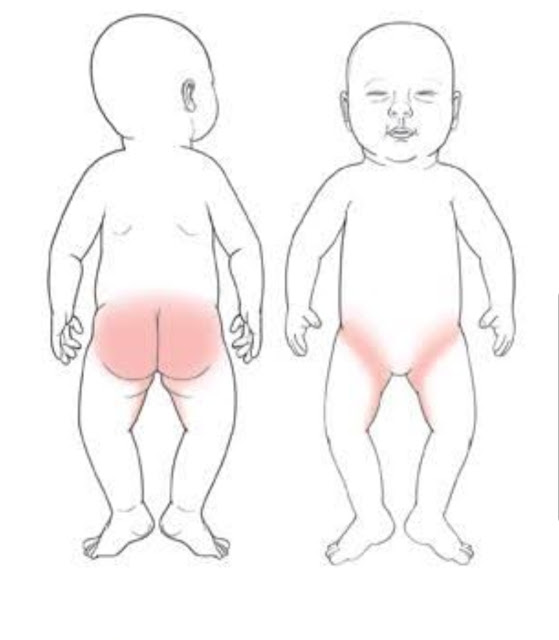
The reason is an increased content of histamine (tyramine, serotonin) in foods, or the ability of foods to increase the release of these substances in the body, or their increased absorption, due to the pathology of the gastrointestinal tract (fermentopathy, inflammation in the intestinal wall, etc.). ). Such products include chocolate, cocoa, strawberries, citrus fruits, honey, sauerkraut, marinades and spices, seafood, fish, caviar, pork, mushrooms, cheeses, nuts, smoked meats, preservatives, dyes and flavor enhancers.
Treatment includes dietary advice, skin care, and in some cases, antihistamines and anti-inflammatory creams.
Clinical manifestations of atopic dermatitis, simple contact dermatitis in highly sensitive children and the manifestation of pseudo-allergic reactions are very similar to each other, so the main task remains to create a "skin barrier" by constantly moisturizing the skin with the help of emollients, stopping exacerbation with anti-inflammatory creams and eliminating exacerbation-provoking factors .
And the last:
Skin infections - herpesvirus, staphylococcal pemphigus, candidiasis also occurs in infants, do not forget about them. It is worth contacting a doctor immediately if the child is lethargic, has a fever, refuses to breast or bottle, skin rashes are accompanied by pus or are covered with purulent crusts, there are blisters or a group of bubbles, erosion (violation of the integrity of the skin), severe swelling and redness of the skin.
Author:
Eroshkina Maria Sergeevna
pediatrician
Rash in a child on body, legs, back
We treat children according to the principles of evidence-based medicine: we choose only those diagnostic and treatment methods that have proven their effectiveness. We will never prescribe unnecessary examinations and medicines!
Make an appointment via WhatsApp
Prices Doctors
The first children's clinic of evidence-based medicine in Moscow
No unnecessary examinations and drugs! We will prescribe only what has proven effective and will help your child.