White stuff coming out of eye
White Eye Discharge: Causes, Treatment, and More
Overview
White eye discharge in one or both of your eyes is often an indication of irritation or an eye infection. In other cases, this discharge or “sleep” may just be a buildup of oil and mucus that accumulates while you’re resting. White eye discharge may not be an initial cause for concern in some cases, but medical attention is still recommended to ensure your condition does not cause damaging complications.
Common irritants may be to blame for your white eye discharge. However, there are also a number of conditions that can cause eye irritation, discharge, and general discomfort.
Conjunctivitis
Conjunctivitis, more commonly referred to as pinkeye, is an inflammation of the membrane that lines your eyelid. When blood vessels in this membrane become inflamed, it causes your eye to appear pink or red in color. Conjunctivitis can be a common infection, often caused by bacteria or a virus. In many cases, conjunctivitis can be contagious.
Other than eye redness, symptoms associated with this infection include:
- itchiness
- discharge in one or both eyes
- tearing
- pain
- grittiness or irritation
Treatment for pink eye typically focuses on relieving symptoms. Your doctor may prescribe eye drops and recommend applying cold compresses to help with discomfort. If you experience pink eye as an allergy symptom, your doctor may also recommend anti-inflammatory medication and allergy medication.
Allergies
Eye allergies, or allergic conjunctivitis, is an immune response that occurs when your eye is irritated by allergens such as pollen or dust. This form of conjunctivitis can affect one or both eyes, and may also be accompanied by congestion and eye discharge. Other symptoms associated with eye allergies include:
- itchiness
- burning
- swollen eyelids
- runny nose
- sneezing
Allergy medication and associated shots may be helpful in treating eye allergy symptoms. Your doctor may also prescribe eye drops to relieve inflammation and discomfort. However, the best way to prevent an allergic reaction and eye irritation is to avoid the known allergen, if possible.
Your doctor may also prescribe eye drops to relieve inflammation and discomfort. However, the best way to prevent an allergic reaction and eye irritation is to avoid the known allergen, if possible.
Corneal ulcer
In more extreme cases of dry eye or infection, you may develop a corneal ulcer. The cornea is a clear membrane that covers the iris and the pupil. When it becomes inflamed or infected, an ulcer can form and may cause white eye discharge. Other symptoms associated with corneal ulcers include:
- eye redness
- pain
- excessive tearing
- difficulty opening your eyelid
- sensitivity to light
Most cases of corneal ulcers require treatment. If they are causing significant pain, you may need antibiotic treatment. In severe cases, if a corneal ulcer permanently affects your vision or causes lasting damage, a cornea transplant may be necessary.
You should consult your doctor if your eye discharge becomes excessive or doesn’t improve after a week. In more severe cases, your eye discharge may occur with other symptoms such as pain and impaired vision.
In more severe cases, your eye discharge may occur with other symptoms such as pain and impaired vision.
If you begin to experience adverse symptoms alongside your eye discharge, or if you notice an irregular-colored discharge, seek immediate medical attention. These may be signs of a more serious underlying condition.
White eye discharge can be caused by a number of eye conditions. In some cases, this symptom is no cause for alarm. However, if it becomes excessive or is accompanied by irregular symptoms, you should visit a doctor. There are home treatments to help with symptoms, but antibiotics and other professional medical attention may be necessary to improve your condition.
White Eye Discharge: Causes, Treatment, and More
Overview
White eye discharge in one or both of your eyes is often an indication of irritation or an eye infection. In other cases, this discharge or “sleep” may just be a buildup of oil and mucus that accumulates while you’re resting.![]() White eye discharge may not be an initial cause for concern in some cases, but medical attention is still recommended to ensure your condition does not cause damaging complications.
White eye discharge may not be an initial cause for concern in some cases, but medical attention is still recommended to ensure your condition does not cause damaging complications.
Common irritants may be to blame for your white eye discharge. However, there are also a number of conditions that can cause eye irritation, discharge, and general discomfort.
Conjunctivitis
Conjunctivitis, more commonly referred to as pinkeye, is an inflammation of the membrane that lines your eyelid. When blood vessels in this membrane become inflamed, it causes your eye to appear pink or red in color. Conjunctivitis can be a common infection, often caused by bacteria or a virus. In many cases, conjunctivitis can be contagious.
Other than eye redness, symptoms associated with this infection include:
- itchiness
- discharge in one or both eyes
- tearing
- pain
- grittiness or irritation
Treatment for pink eye typically focuses on relieving symptoms. Your doctor may prescribe eye drops and recommend applying cold compresses to help with discomfort. If you experience pink eye as an allergy symptom, your doctor may also recommend anti-inflammatory medication and allergy medication.
Your doctor may prescribe eye drops and recommend applying cold compresses to help with discomfort. If you experience pink eye as an allergy symptom, your doctor may also recommend anti-inflammatory medication and allergy medication.
Allergies
Eye allergies, or allergic conjunctivitis, is an immune response that occurs when your eye is irritated by allergens such as pollen or dust. This form of conjunctivitis can affect one or both eyes, and may also be accompanied by congestion and eye discharge. Other symptoms associated with eye allergies include:
- itchiness
- burning
- swollen eyelids
- runny nose
- sneezing
Allergy medication and associated shots may be helpful in treating eye allergy symptoms. Your doctor may also prescribe eye drops to relieve inflammation and discomfort. However, the best way to prevent an allergic reaction and eye irritation is to avoid the known allergen, if possible.
Corneal ulcer
In more extreme cases of dry eye or infection, you may develop a corneal ulcer. The cornea is a clear membrane that covers the iris and the pupil. When it becomes inflamed or infected, an ulcer can form and may cause white eye discharge. Other symptoms associated with corneal ulcers include:
The cornea is a clear membrane that covers the iris and the pupil. When it becomes inflamed or infected, an ulcer can form and may cause white eye discharge. Other symptoms associated with corneal ulcers include:
- eye redness
- pain
- excessive tearing
- difficulty opening your eyelid
- sensitivity to light
Most cases of corneal ulcers require treatment. If they are causing significant pain, you may need antibiotic treatment. In severe cases, if a corneal ulcer permanently affects your vision or causes lasting damage, a cornea transplant may be necessary.
You should consult your doctor if your eye discharge becomes excessive or doesn’t improve after a week. In more severe cases, your eye discharge may occur with other symptoms such as pain and impaired vision.
If you begin to experience adverse symptoms alongside your eye discharge, or if you notice an irregular-colored discharge, seek immediate medical attention. These may be signs of a more serious underlying condition.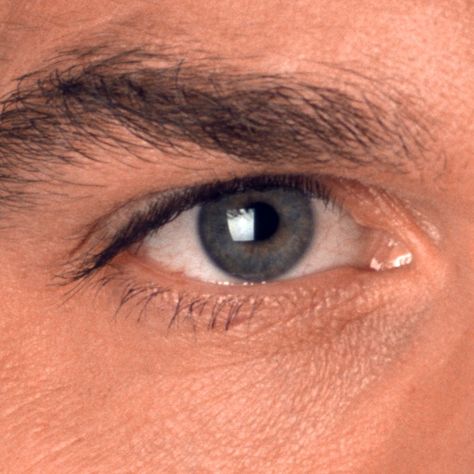
White eye discharge can be caused by a number of eye conditions. In some cases, this symptom is no cause for alarm. However, if it becomes excessive or is accompanied by irregular symptoms, you should visit a doctor. There are home treatments to help with symptoms, but antibiotics and other professional medical attention may be necessary to improve your condition.
“Flying flies” and “glassy worms” in the eyes, or where do the “broken pixels” come from in the vitreous / Habr
Raise your head and look at something evenly colored, at some kind of light background no sun). If something like this suddenly began to slowly float before your eyes:
... Then get acquainted, these are “broken pixels” in your eye formed by the vitreous body (in the figure below it is in all its glory). Many of these “glitches” appear in childhood and multiply or gradually change over the years. For most people, their presence is not a cause for concern, but their sudden appearance or a sharp increase is a reason for an urgent visit to an ophthalmologist. Especially if lightning in front of the eyes, a dark veil or fine “tobacco dust” are added to this.
Especially if lightning in front of the eyes, a dark veil or fine “tobacco dust” are added to this.
But to understand the whole situation, let's talk about what this phenomenon is in general and where it comes from.
Where is the most vitreous
The eye is a ball, most of which is occupied by the vitreous body (as much as 2/3 of the volume). It is clearly visible in the diagram above - this is the space between the lens and the retina in the cavity of the eye. In a normal eye, the vitreous body is so transparent that when viewed through the eye it appears empty.
The vitreous body is a jelly-like, viscous and well-stretching liquid like jelly or jelly. Only transparent. This "jelly" consists of water, colloids and microelements - collagen fibers resembling intertwined ropes impregnated with hyaluronic acid. Unlike the cornea, which consists of the same matrix, the density of threads in the vitreous body is lower, so the cornea is dense and rigid (by the standards of what is in the eye), but here we are waiting for a viscous medium.
This environment is heterogeneous, there are voids and "cisterns" in it, various lacunae. You can inject a special solution into the eye, which will color the vitreous body, and all this beauty will be visible. Here, for example:
The vitreous body is adjacent to the posterior surface of the lens, for the rest of its length it is in contact with the inner limiting membrane of the retina. A special hyaloid canal passes from the optic disc to the lens through the vitreous body, and the framework of the vitreous body forms a thin network of intertwining fibers of various forms of collagen protein. And the gaps are filled with liquid - this structure gives it the appearance of a gelatinous mass.
Thanks to the vitreous body, the eye has a regular spherical shape, it provides incompressibility and eye tone, absorbs shock, nutrients move through the channels. But its light-refracting function is very small.
If we need to deliver a medicinal substance to the deep parts of the eye, then we inject it directly into the vitreous cavity with a microneedle, because the eye is such an organ that is quite isolated from the body as a whole, and not everything that enters the blood reaches the internal contents of the eye. Interferes with the hematoophthalmic barrier.
Interferes with the hematoophthalmic barrier.
It happens like this:
Where do glass worms come from
For the most part, the translucent "ghosts" that appear in the field of view during, for example, a sharp fall or parachute jump, lifting weights or against the background of complete well-being and subsequently distinguishable when carefully examining light objects are natural lacunae in the vitreous body, due to its design. They sometimes close themselves, move, or new ones form by themselves (slowly, over months).
In general, any noticeable "worms" are something in the vitreous that prevents light from reaching the retina normally. In English literature, referred to as "floaters" -
like dust particles on a camera matrix. This condition is called "vitreous destruction" (DST).
The presence of small single fragments in the vitreous cavity is the norm from a medical point of view.
Often there is another story. But now we need to go a little deeper into the anatomy. By itself, the vitreous body is not attached to the retina along the main area, but simply adjoins very closely. However, in the macula (center of the eye, yellow spot), near the optic nerve and along the equator of the retina, there are attachments, and they are quite strong. If in the eye with age, with an injury or the appearance of another disease of the eye and the body as a whole, not just destruction (in general, not dangerous), but some kind of blood cells appears, inflammation is a very dangerous problem. Everything that gets into such a closed cavity is absorbed for a long time, it is difficult and not always completely with a transparent effect. As a rule, stained opacities, coarse adhesions and bands remain, reducing visual acuity. Everything is explained by close, I would even say, intimate contact with such an important tissue as the retina (the retina and vitreous body suffer simultaneously in case of illness).
But now we need to go a little deeper into the anatomy. By itself, the vitreous body is not attached to the retina along the main area, but simply adjoins very closely. However, in the macula (center of the eye, yellow spot), near the optic nerve and along the equator of the retina, there are attachments, and they are quite strong. If in the eye with age, with an injury or the appearance of another disease of the eye and the body as a whole, not just destruction (in general, not dangerous), but some kind of blood cells appears, inflammation is a very dangerous problem. Everything that gets into such a closed cavity is absorbed for a long time, it is difficult and not always completely with a transparent effect. As a rule, stained opacities, coarse adhesions and bands remain, reducing visual acuity. Everything is explained by close, I would even say, intimate contact with such an important tissue as the retina (the retina and vitreous body suffer simultaneously in case of illness).
Such a terrible picture can be seen with a hemorrhage in the vitreous body (it is called hemophthalmos).
And if droplets of cholesterol accumulate in the vitreous, it looks like a "golden rain".
With a blunt impact to the eye, the vitreous body will take on the main deformation as a result of mechanical trauma and begin to change shape. Where it simply adhered to the retina, it will boldly move back and come back. But where there were adhesions, the vitreous body, when deformed, will pull the retina behind it inside the eye. This can lead to a much more serious injury - rupture or detachment of the retina. And this is all the chances of losing vision or deteriorating the optical quality of the eye to a few percent of the norm.
Retinal tear delimited by laser
What happens with myopia?
In myopic people, as a rule, the axial length of the eye is more than 24 mm (the average parameter, the measurement of which tells us about the progression of myopia). The eye transforms from a soccer ball shape into a rugby ball. In this case, the posterior pole of the eye is stretched, but if this is not dangerous for the outer sclera (it is elastic enough), then the middle (choroid) and inner shell (retina) do not stretch. Therefore, the nutrition of the retina worsens in the posterior pole, and dystrophic zones of sprains and ruptures appear along the periphery. The vitreous body plays an important role in this. In places of attachment, it pulls the retina - and holes are formed.
In this case, the posterior pole of the eye is stretched, but if this is not dangerous for the outer sclera (it is elastic enough), then the middle (choroid) and inner shell (retina) do not stretch. Therefore, the nutrition of the retina worsens in the posterior pole, and dystrophic zones of sprains and ruptures appear along the periphery. The vitreous body plays an important role in this. In places of attachment, it pulls the retina - and holes are formed.
What happens with age?
Somewhere after 30 years, new "midges" often begin to appear, and after 40 years hyaluronic acid is gradually lost, the transparency of the vitreous body decreases, visualization of the fibers appears.
Still later, the vitreous body dries out altogether and begins to flake off the retina (it just comes off in places where there is no attachment).
Vitreous detachment is a normal sign of aging, it is caused by thinning of the vitreous body, leads to retinal tension in places of strong attachment, which can lead to retinal rupture. Acute vitreous detachment in 15% of cases leads to retinal breaks.
Acute vitreous detachment in 15% of cases leads to retinal breaks.
Figuratively speaking, a kind of "snot" of gel (this is a very inaccurate description of this type of tissue, but gives a very good understanding) dangles inside the eye. Then this "lump of gel" comes off the optic nerve. As a rule, the separation zone looks like a ring (Weiss ring), that is, when projected onto the retina, what patients call a “spider”, “big midge”, “eight”, “dark spot”, “analemma”, “circle” is obtained. " and so on. The kaleidoscope can change: every day a new shape. If the fastening ring did not come off, but simply stretched out - to hell with it, with a kaleidoscope, you can live. But if it pulled the retina and tore off a piece, then there are retinal breaks, and detachments, and in general a lot of trouble.
This is how an ophthalmologist sees the Weiss ring:
Treatment of breaks before a retinal detachment occurs - laser coagulation of the breaks in several rows along the edge so that the formed adhesions hold the retina in place.
All this is treated with a good prognosis in case of an appeal within the first days to an ophthalmological surgeon, with an average prognosis - in case of an appeal within a month. If detachment has begun and the fluid that has entered through the gap continues to flow under the retina, peeling it off, the problems begin to become irreversible, and the question is about maintaining vision as such, at least with some optical quality.
Therefore, if you suddenly see a lot of new "midges", or they behave in some strange way, or something else incomprehensible is happening in the eye, you should urgently go to an ophthalmologist.
"Blackflies" in the eye: so what to do with them?
If, after examination, the doctor does not find damage to the retina in the fundus and notes only the presence of microinclusions in the vitreous body, then you should not worry - there are no serious risks to vision in this case.
If the patient at the same time sees "garbage and midges" that bother him, but knows that there is no danger in this, the issue of dynamic observation and getting used to minor shortcomings in the quality of vision is most often discussed. In addition, after a couple of months, patients really stop noticing these inclusions and do not fixate their attention on them.
In addition, after a couple of months, patients really stop noticing these inclusions and do not fixate their attention on them.
But in some cases, complaints may be due to reduced vision due to "turbidity" floating in front of the eye. Then, together with an ophthalmologist who specializes in the retina (and not just a doctor in a polyclinic who knows quite a bit about modern ophthalmology), the question of the treatment of this condition can be discussed.
There are two options: the first one involves the destruction of fragments in the vitreous body using a modern YAG laser for laser vitreolysis, the second one is the surgical removal of a part of the vitreous body within the optical axis - vitrectomy surgery.
Treatment without surgery
The whole trick with the problem of "midges" and "spiders" is how to find a doctor who correctly interprets changes in the eye. The difference with incorrect diagnosis is colossal: to distinguish a degenerative calm state of simple destruction of the vitreous body from the pathological appearance in the vitreous of inflammatory cells, blood, the onset of retinal detachment, vascular disorders and other things.
That is, the patient is faced with the task of finding that expert who will calm him down or notice the problem in time.
The difference is in further tactics: the destruction does not need to be treated, it is necessary to get used to it.
In polyclinics, with a clear picture of DST (the usual "garbage" in the eyes without the risk of further complications), they say: "Let's prescribe resolving therapy." And some kind of “placebo” is prescribed: emoxipin, taufon, catachrom. "Holy water" in this case will help better if you believe in it. It’s nice for a person, and the brain builds a map of “broken pixels” in a couple of weeks and removes them on its own (at a high level, if you start looking, they will be visible again). If you start catching the “glitch” on purpose (as you may be doing right now), the distortions will be more noticeable. If you don't think about them, you won't see them. Which is what is required. The brain is very adaptable.
Another thing is to overlook inflammation or the beginning of retinal detachment.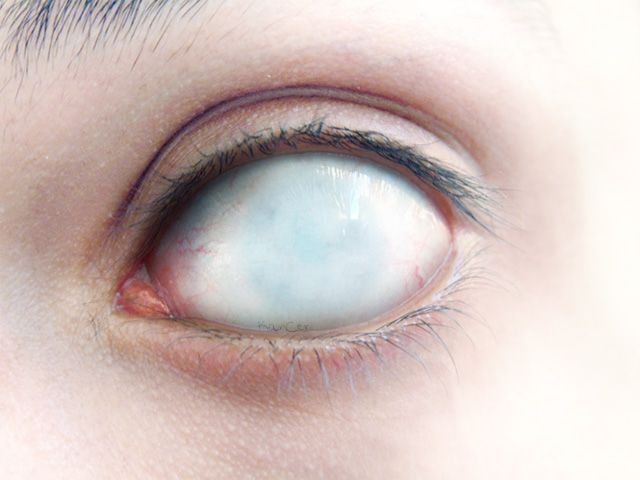 Here, "soothing" methods make the patient lose a week or two, which will then lead to serious complications.
Here, "soothing" methods make the patient lose a week or two, which will then lead to serious complications.
When operation is shown
Let's agree that we are talking about a degenerative change in the vitreous body, and not about the other conditions mentioned above. That is, when it is reliably known that from a medical point of view there are no risks, but something floating in front of the eyes still greatly interferes with seeing.
Option 1. Laser vitreolysis.
Any work in a closed vitreous cavity is potentially dangerous. It must be performed very precisely, since such sensitive structures as the retina (especially its central zone) and the lens are nearby.
Ellex has recently introduced a new minimally invasive treatment for vitreous pathology: Weiss rings, intravitreal opacities and adhesions, vitreous degeneration. This is a YAG laser unit for the treatment of the anterior and posterior sections of the eye using a targeted red diode laser. Since the structures adjacent to the vitreous body are very delicate, they came up with a reduction in the total energy due to the ultra-Gaussian profile of the laser beam. The small spot size and low energy of optical breakdown (less than 1.8 mJ in air) cause photodestruction of inclusions in the vitreous body.
Since the structures adjacent to the vitreous body are very delicate, they came up with a reduction in the total energy due to the ultra-Gaussian profile of the laser beam. The small spot size and low energy of optical breakdown (less than 1.8 mJ in air) cause photodestruction of inclusions in the vitreous body.
Practically 50% effective, because if the opacification is close to the retina or close to the posterior lens capsule, or too dense, etc., then application is not possible. Often one large fragment turns into several smaller ones, they can shift from the optical axis, or they can be added. In general, only after an examination by a specialist with experience in laser surgery at this unit will you be able to find out if this is your method.
Option 2 Vitrectomy.
This is a full-fledged abdominal operation with all the consequences that follow from it. That is, it does not matter whether a small "midge" swims or a "big spider" - the technology involves the work of a vitreoretinal surgeon. Vitrectomy is underway - an operation to remove the vitreous body - like this:
Vitrectomy is underway - an operation to remove the vitreous body - like this:
3 small punctures are made into the cavity of the eyeball in the projection of the plane of the ciliary body, that is, 3.5–4 mm from the limbus - the border of the transparent and opaque parts. The size of the puncture is measured in gages G (imperial unit of radius). The standard 3-port seamless technique is 23 G. Now most of the operations are carried out according to the 25G method - this is 0.445 millimeters. The dependence is as follows: the larger G, the smaller the size of the puncture. The most gentle technique is 27G (0.361 mm). By the way, the smaller the puncture, the more expensive the cost of a set of consumables. Ideal for removing floaters 27 G.
A saline and pH balanced solution is delivered through one port to maintain eye tone and volume during surgery so that the eye does not “collapse” when the vitreous body is removed. The second incision is needed to shine inside this "cave", that is, the cavity inside the eye, where the vitreous body is located. In the third one, in fact, an instrument is inserted - a vitreotome, such a small guillotine with a pipe. It looks like a micromeat grinder, with which the surgeon grinds the vitreous body fibers and sucks them into the tube cavity.
In the third one, in fact, an instrument is inserted - a vitreotome, such a small guillotine with a pipe. It looks like a micromeat grinder, with which the surgeon grinds the vitreous body fibers and sucks them into the tube cavity.
At the end of the operation, a balanced solution remains in the eye, which is then replaced with intraocular fluid. The ports are removed from the self-sealing sutures and a dressing is applied for a couple of hours.
In experienced hands, this operation takes 20 minutes under local anesthesia and the result is no coarse floating flakes in front of the eyes, but any operation that opens the eyeball has a wide range of potential risks, surgery of the posterior segment of the eye doubles these risks.
In any case, I always make it clear to the patient that this is a very serious intervention with a minimal medical problem.
From time to time, with gross opacities that reduce vision, it is necessary to perform such an operation for drivers, pilots, etc.![]() - in the case when even a slight short-term “fogging” can affect safety.
- in the case when even a slight short-term “fogging” can affect safety.
Scarecrow
In my beloved Fedorovsky Center, such patients who are worried over trifles because of the "midge" are told a story about a patient who came to the clinic with a complaint about the "midge". He was told that it was not dangerous, it did not need to be treated. He insisted, the doctor from Fedorov's clinic dissuaded me from the operation in every possible way. He even offered to visit a psychiatrist to find the answer to the question “How to live with such a “midge”?”. The patient did not persuade the doctor from Fedorov's clinic for an operation and flew off to look in the States for someone who would agree to operate on him. Found. After the operation, there was inflammation of the membranes of the eye. The eye went blind, became small, red and began to disturb the patient. Already in Russia, the eye had to be removed. Finale: no eye - no "midge".
Conclusion
It is very difficult to judge how much, in principle, the body needs this structure - the vitreous body. It seems possible without it, but the need for it in the structure of the eye has not yet been fully studied. While it is intuitively clear that it is better to save, if possible.
It seems possible without it, but the need for it in the structure of the eye has not yet been fully studied. While it is intuitively clear that it is better to save, if possible.
A large number of doctors of the last century and the present one are studying the structure of the vitreous body - this can be seen from the number of surnames with which its structures (channels, ligaments, etc.) are named.
With age, the vitreous body ages, shrinks and can cause certain problems. You need to monitor your eyes, if you have symptoms of visual impairment in any form and age, seek help from specialists.
Eye discharge - is it dangerous?
Discharge from the eyes - is it dangerous? - OCOMEDICASMon-Fri 9:00 - 17:00
Mon-Fri 9:00 - 17:00
Sat - Sun: day off
+38 (050) 840 00 44
+38 (068) 840 00 44
Normally, in an adult, the mucous membrane produces a mucous film that covers the eye and performs a protective function. And a small amount of whitish mucus in the morning (after sleep) should not cause concern and fear. But with infectious lesions, the picture changes: the discharge becomes more abundant, they can change color and become yellow, the eyes turn red and fester. In this case, it is necessary to identify the cause of purulent discharge and be sure to consult a doctor.
And a small amount of whitish mucus in the morning (after sleep) should not cause concern and fear. But with infectious lesions, the picture changes: the discharge becomes more abundant, they can change color and become yellow, the eyes turn red and fester. In this case, it is necessary to identify the cause of purulent discharge and be sure to consult a doctor.
Diseases that cause purulent discharge from the eyes:
- Conjunctivitis. Eye inflammation can be caused by bacteria, viruses, or be allergic in nature. Discharge from the eyes can be very profuse. In bacterial conjunctivitis, the discharge from the eyes can be very thick, yellow-green in color, and cause the eyes to stick very tightly. With allergic inflammation - discharge from the eyes is more watery, yellowish in color.
- In addition to conjunctivitis, there may be other conditions in the eye that cause purulent discharge from the eyes. These include ocular herpes, fungal keratitis
- Corneal ulcer also causes active suppuration from the eyes.
 It is usually the result of an untreated eye injury and can lead to complete loss of vision.
It is usually the result of an untreated eye injury and can lead to complete loss of vision. - Dacryocystitis (inflammation of the lacrimal sac) causes swelling and redness of the inner corner of the eye. When pressing on the area of the lacrimal sac, abundant yellow discharge appears.
- With blepharitis (acute or chronic inflammation of the eyelids), there is swelling and itching of the eyelids, the eyes fester - usually in the morning. Discharge from the eyes is frothy, yellow-green in color.
- Barley or chalazion. May be accompanied by profuse purulent discharge. In this case, the affected eyelid is swollen, red.
- Dry eye syndrome. Dry eye symptoms include eye redness, burning sensation, blurry vision, and foreign body sensation. Very often, people with dry eye syndrome complain that their eyes fester in the morning, after sleep, but this is not pus, but accumulated mucous secretions.
A slight discharge from the eyes of a mucous nature is harmless.