Dry red patch on baby face
Managing Eczema in Winter and Year Round: A Parents Guide
Cold, dry outdoor air and indoor heating can rob skin of its natural moisture in the winter. Red, crusty, dry patches can be common on a baby's skin, particularly in winter, and cause concern for parents. Such symptoms can be treated, however, and many babies and children do outgrow the dry, itchy skin of atopic dermatitis, also known as eczema.
We spoke with pediatric dermatologist Katherine Puttgen to learn more.
What is eczema?Broadly speaking, eczema describes dry, rashy and itchy skin. It is a hereditary and chronic skin disorder most commonly seen in infants or very young children, often beginning in the first year of life and most commonly seen before age 5. Eczema is not contagious.
While many children outgrow eczema, for some it might last into adolescence or adulthood. The American Academy of Dermatology estimates that 10-to-20 percent of children in the world have eczema, and it affects up to 20 percent of infants.
What causes eczema in infants and children?
Eczema is brought about by the complex interplay of a genetic predisposition and the child’s environment. Many things – from the climate to possible allergens – can cause eczema to flare. We know that eczema tends to run in the families with a predisposition to other atopic diseases, such as food allergies, asthma and hay fever. Individuals with atopic dermatitis may lack certain proteins in the skin, which leads to greater sensitivity. Parents with eczema are more likely to have children with eczema. However, the exact way it passes from parents to children is still not known. Most children who have eczema will show signs of the condition in the first year of life. It tends to wax and wane in severity.
What causes eczema to wax, to flare?Different "triggers" can make eczema worse. For infants, these can be irritants such as wool, certain detergents or extreme temperatures, or other immune triggers, such as food allergies and asthma, and even pet dander.
Most kids with the condition have the hardest time in winter, when the air is cold and dry. A small percentage has a harder time in the summer, when it is hot and humid.
What does it look like?The signs of eczema in infants include itchy, dry and scaly skin, redness and swelling of the skin and small bumps that open and weep when scratched. In infants and young children, eczema is usually found on the face, outside of the elbows, and on the knees.
In older children and adults, eczema tends to be on the hands and feet, the arms, and on the back of the knees.Keep in mind that all patches of dry skin are not eczema. The cold, dry outdoor air and indoor heating can dry all babies’ skin in winter, causing dry patches. In children prone to dry skin, so can the sun, air conditioning, and pool and salt water.
We dermatologists usually say “if it’s not itchy, it’s not eczema”; you can’t make a diagnosis of eczema unless there is an itchiness that goes with the rash. Babies with cradle cap, also known as seborrheic dermatitis, can also have a wide-spread rash, which is not eczema in itself. But it is common for cradle cap and eczema to co-exist in the first several months of life.
Babies with cradle cap, also known as seborrheic dermatitis, can also have a wide-spread rash, which is not eczema in itself. But it is common for cradle cap and eczema to co-exist in the first several months of life.
Eczema symptoms may resemble other skin conditions, so always consult your child’s pediatrician. A diagnosis includes a complete medical history and a physical examination.
How is it treated?Because there is not yet a cure for eczema, our treatment goals are to reduce itching and skin inflammation, and to prevent infection. The best treatment for eczema is a proactive one, using gentle skin care and moisturizers to re-establish the skin barrier.
Infants’ and older children’s skin should be kept well moisturized, and washed with fragrance-free non-soap cleansers. We also recommend a fragrance-free ointment-based moisturizer, with petrolatum as either the only or the first ingredient. In young children and infants, it is reasonable to use an over-the-counter topical hydrocortisone ointment, which is a mild topical steroid, for up to a week.
In young children and infants, it is reasonable to use an over-the-counter topical hydrocortisone ointment, which is a mild topical steroid, for up to a week.
But if the rash either persists or you find that you need to use the hydrocortisone more than one week out of the month, you should discuss further use with your child’s pediatrician. You can apply the ointment, as prescribed, then a coat of petrolatum-based moisturizer, to help keep in the moisture.
For school-age children, who don’t want to be so greasy, we usually talk about creams. As for infants, though, when their skin gets very dry, we still recommend a petroleum-based ointment as a top coat. In addition to providing the best barrier protection, ointments don’t sting or burn when applied; creams and lotions sometimes can when the skin is inflamed and very dry. Moisturizers should be applied at least two to three times a day; for children in diapers, each diaper change can present an easy opportunity to moisturize the skin. More frequent use of moisturizers results in better control of itching and less frequent need for topical steroids, and it helps to restore the skin’s natural barrier function.
More frequent use of moisturizers results in better control of itching and less frequent need for topical steroids, and it helps to restore the skin’s natural barrier function.
For all ages of kids with eczema, or prone to eczema, baths should be brief (less than 15 minutes) in warm water, to avoid over-drying of the skin. Children should be protected against scratching their skin (little mitts can help infants) and from irritants that contact their skin, such as harsh detergents and certain fabrics (including bedding). To reduce potential skin irritation, babies and children with eczema should wear only cotton or other natural fiber clothing next to the skin, with the exception of wool, of course. And they should be protected against cold (or very hot) environments to help prevent a skin reaction.
If your child’s skin does not respond well to any of these measures or becomes infected, contact your pediatrician, who can diagnose the condition and then prescribe another topical cream or antihistamine.
Without a cure on the near horizon, we here at Johns Hopkins are creating an Eczema Day Treatment Unit to help our patients with moderate to severe eczema keep their symptoms under control and prevent flare-ups. We anticipate that this novel, multidisciplinary program will include experts from Child Life, behavioral psychology, allergy, dermatology and infectious diseases to provide the comprehensive care these children need – care that cannot be provided in an average clinic visit.
A primary goal of the day treatment unit will be education; children and their families will learn techniques such as wet-wrap therapy, to help deeply moisturize the skin. This therapy involves coating the skin with a topical ointment, followed by a greasy ointment like petroleum jelly, then dressing in wet pajamas, followed by dry pajamas, allowing the skin to soak in the moisture.
In partnering with our colleagues in behavioral psychology, we have seen many of our patients with severe eczema improve significantly with help in finding ways to avoid scratching, which inflames their skin condition, and by helping older children talk about the social difficulties in coping with a chronic condition or going to school with a visible disorder. Child Life specialists are an integral part of the Johns Hopkins Children’s Center and their ability to engage children in age-appropriate play and conversation is an important cornerstone of building a successful program. Because food and environmental allergies and skin infections are more frequent in children with moderate to severe eczema, strong partnerships with our experts in pediatric allergy and infectious diseases are key, as well.
Child Life specialists are an integral part of the Johns Hopkins Children’s Center and their ability to engage children in age-appropriate play and conversation is an important cornerstone of building a successful program. Because food and environmental allergies and skin infections are more frequent in children with moderate to severe eczema, strong partnerships with our experts in pediatric allergy and infectious diseases are key, as well.
At Johns Hopkins, a lot of us in pediatric dermatology, pediatric infectious disease and pediatric allergy and immunology are looking at better ways to prevent or manage eczema. We’re studying the optimal management of bacterial colonization and infection in atopic skin and the role of food allergy in eczema. Our specialties collaborate; each brings a different approach to eczema management. Our goal is to work together to harness the best approaches to better understand eczema and, in doing so, to treat it more effectively.
We go out of our way to provide the comprehensive care our patients with eczema need. On a case-by-case basis, we communicate with one another – whether in allergy, dermatology, psychology or infectious disease – to put together the best course of treatment for each child.We are optimistic that future therapies and approaches to care for those with even severe eczema are going to be greatly improved with more research and that the creation of the Eczema Day Treatment Unit will help us conduct cutting edge research and answer questions we face every day seeing and treating patients.
Like other atopic diseases, such as food allergies, is the incident of eczema in children increasing?Yes. We don’t really know why. But we’re on the case to find answers.
Scarlet fever - NHS
Scarlet fever is a contagious infection that mostly affects young children. It's easily treated with antibiotics.
It's easily treated with antibiotics.
Check if you have scarlet fever
The first signs of scarlet fever can be flu-like symptoms, including a high temperature, a sore throat and swollen neck glands (a large lump on the side of your neck).
A rash appears 12 to 48 hours later. It looks looks like small, raised bumps and starts on the chest and tummy, then spreads. The rash makes your skin feel rough, like sandpaper.
On white skin the rash looks pink or red. It may be harder to see on brown and black skin, but you can still feel it.Credit:
BIOPHOTO ASSOCIATES/SCIENCE PHOTO LIBRARY https://www.sciencephoto.com/media/262529/view
A white coating also appears on the tongue. This peels, leaving the tongue red, swollen and covered in little bumps (called "strawberry tongue").
Credit:
SCIENCE PHOTO LIBRARY https://www.sciencephoto.com/media/262413/view
The rash does not appear on the face, but the cheeks can look red. The redness may be harder to see on brown and black skin.Credit:
ISM/SCIENCE PHOTO LIBRARY https://www.sciencephoto.com/media/101463/view
The symptoms are the same for children and adults, although scarlet fever is less common in adults.
Non-urgent advice: See a GP if you or your child:
- have scarlet fever symptoms
- do not get better in a week (after seeing a GP)
- have scarlet fever and chickenpox at the same time
- are ill again, weeks after scarlet fever got better – this can be a sign of a complication, such as rheumatic fever
- are feeling unwell and have been in contact with someone who has scarlet fever
Scarlet fever is very easily spread. Check with a GP before you go in. They may suggest a phone consultation.
Check with a GP before you go in. They may suggest a phone consultation.
What happens at your appointment
GPs can often diagnose scarlet fever by looking at your tongue and rash.
Sometimes they may:
- wipe a cotton bud around the back of your throat to test for bacteria
- arrange a blood test
Treating scarlet fever
A GP will prescribe antibiotics. These will:
- help you get better quicker
- reduce the chance of a serious illnesses, such as pneumonia
- make it less likely that you'll pass the infection on to someone else
Taking antibiotics
Keep taking the antibiotics until they're finished, even if you feel better.
Things you can do yourself
You can relieve symptoms of scarlet fever by:
- drinking cool fluids
- eating soft foods if you have a sore throat
- taking painkillers like paracetamol to bring down a high temperature (do not give aspirin to children under 16)
- using calamine lotion or antihistamine tablets to ease itching
How long scarlet fever lasts
Scarlet fever lasts for around 1 week.
You can spread scarlet fever to other people up to 6 days before you get symptoms until 24 hours after you take your 1st dose of antibiotics.
If you do not take antibiotics, you can spread the infection for 2 to 3 weeks after your symptoms start.
Important: Important
If you or your child has scarlet fever, stay away from nursery, school or work for 24 hours after you take the 1st dose of antibiotics.
Is scarlet fever dangerous?
Scarlet fever can be a serious illness, but thanks to antibiotics, it's less common than it used to be and easier to treat.
But cases of scarlet fever have increased in recent years. For more information see GOV.UK: Scarlet fever guidance and data.
Complications from scarlet fever are rare. They can happen during or in the weeks after the infection, and can include:
- ear infection
- throat abscess
- sinusitis
- pneumonia
- meningitis
- rheumatic fever
Pregnancy advice
There's no evidence to suggest that getting scarlet fever during pregnancy will harm your baby.
But it can make you feel unwell, so it's best to avoid close contact with anyone who has it.
Contact a GP if you get symptoms.
Many of the antibiotics used for scarlet fever are considered to be safe to take during pregnancy.
How to avoid spreading scarlet fever
Scarlet fever is very infectious and can easily spread to other people.
To reduce the chance of spreading scarlet fever:
Do
-
wash your hands often with soap and water
-
use tissues to trap germs from coughs or sneezes
-
bin used tissues as quickly as possible
Don’t
-
do not share cutlery, cups, towels, clothes, bedding or baths with anyone who has symptoms of scarlet fever
Page last reviewed: 29 June 2021
Next review due: 29 June 2024
Plaques on the skin - causes, diseases, diagnosis and treatment
- INVITRO
- Library
- Symptoms
- Plaques on the skin
Fungus
Allergy
Psoriasis
Keratoma
Mycosis
Nevus
Melanoma
9675 November 16
IMPORTANT!
The information in this section should not be used for self-diagnosis or self-treatment. In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests.
 For diagnosis and proper treatment, you should contact your doctor.
For diagnosis and proper treatment, you should contact your doctor.
For a correct assessment of the results of your analyzes in dynamics, it is preferable to do studies in the same laboratory, since different laboratories may use different research methods and units of measurement to perform the same analyzes.Plaques on the skin: the causes of occurrence, in what diseases they occur, diagnosis and methods of treatment.
Definition
A plaque is a pathological element with clear edges that rises above the skin surface or merges with it, more than 5 mm in size.In dermatology, many types of plaques are distinguished - about 70 diseases occur with the formation of these elements, which makes the plaque one of the most common rashes.
Plaque varieties
The shape of the plaques are round, oval and irregular in shape. Over time, the shape, surface and appearance of this element may change.
Due to the occurrence of plaques, they can be both a manifestation of skin diseases and a symptom of diseases of internal organs and systems (autoimmune reactions, liver diseases, oncological processes, allergic reactions).
Plaques are dry, smooth, red, brown, gray-white, etc.
Possible causes of plaques
Dry plaques on the skin in adults may be a manifestation of the following diseases: plaques with severe itching.
- Allergic reactions are characterized by the appearance on the skin of smooth dry plaques, pink spots, blisters, which are very itchy and cause severe discomfort. They can develop both when the skin comes into contact with the allergen, and when it gets on the mucous membranes (for example, with urticaria, hay fever, food and contact allergies).
- Psoriasis is a chronic non-infectious skin disease in which scaly dry plaques form on the elbows, knees, scalp, prone to fusion and accompanied by mild itching.
- Dry plaques form on the skin if it is exposed to stress for a long time with the loss of its protective functions.
- Diseases of the digestive tract, accompanied by malabsorption syndrome (impaired absorption of vitamins and trace elements in the small intestine), chronic diseases of the liver and other organs, in which substances that are not normally present in the dermis accumulate, also lead to the appearance of dry plaques.
- Solar keratoma is a precancerous condition, which is characterized by the presence of many light grayish plaques on the skin.
- Drug toxidermia is an allergic reaction accompanied by the appearance of elements in the form of plaques on the skin. In severe cases, Lyell's syndrome or Stevens-Johnson syndrome, toxic epidermal necrolysis, may develop.

- Dühring's dermatitis (herpetiform) is a chronic skin disease with no established etiology, which is characterized by recurrent appearance of a rash of various morphologies on the skin, accompanied by severe skin itching and burning.
- Mycosis fungoides is a primary T-cell lymphoma of the skin, a malignant lymphoid lesion, primarily of the skin. Itchy red plaques appear on the skin, resembling eczema. In the initial stages, they respond well to treatment with hormonal ointments, but the disease itself requires more complex therapy.
- In children, the appearance of red spots and plaques on the skin is most often associated with an allergic reaction to food.
- Becker's nevus is an anomaly in the development of the dermis, when dark plaques with an uneven surface appear on the skin, on which hair can begin to grow over time.
- Pigmentary nevus - "birthmark", may rise above the skin, has a brown or dark color.
- Melanoma is the most malignant skin tumor characterized by rapid metastasis. It develops mainly from nevi and moles. If the nature of the surface, the boundaries of the mole change, its size increases, bleeding occurs, you should immediately contact a dermatologist or oncologist to exclude the development of melanoma.
- Basal cell skin cancer is more often localized on the head, face, neck, does not metastasize, is characterized by slow growth.
- Senile keratoma occurs in elderly people, most likely due to a lack of vitamins, an abundance of animal fats consumed, skin sensitivity to ultraviolet radiation due to a violation of its protective functions. Typical localization - face, neck, open areas of the body.
- Seborrheic keratoma is a yellowish plaque on the skin that eventually transforms into a dark brown growth that tends to flake off, itch severely, crack, bleed, and can serve as an entryway for infection.
- change in the shape of the plaque - the edges have become uneven;
- change in the surface of the plaque - cracks, ulcerations appeared;
- change in the size of the plaque - it began to grow rapidly above the surface of the skin or actively spread through it;
- discoloration of the plaque - in cases of malignancy, an uneven color of the formation is usually observed with areas of darker and lighter shades;
- the appearance of bleeding - both contact and spontaneous;
- enlargement of regional (nearby) lymph nodes.
- Clinical guidelines.
 Dermatitis herpetiformis // Russian Society of Dermatovenerologists and Cosmetologists. 2016.
Dermatitis herpetiformis // Russian Society of Dermatovenerologists and Cosmetologists. 2016. - Clinical guidelines. Urticaria in children // Union of Pediatricians of Russia; Russian Association of Allergists and Clinical Immunologists. 2018.
- Clinical guidelines. Toxidermia // Russian Society of Dermatovenerologists and Cosmetologists. 2016.
- Clinical guidelines. Familial hypercholesterolemia // National Society for the Study of Atherosclerosis. 2018.
-
Gastrointestinal bleeding
639 29 September
-
Intestinal colic
4670 28 September
-
Exanthema
5015 12-th of September
- Photo
- Getty
- Atopic or allergic. The spots are single, appear on the body or limbs.
- Seborrheic. The reddened areas are covered with a yellowish crust on top. Most often, a fungal infection occurs in the first month after birth. Without treatment, this condition drags on for several years.
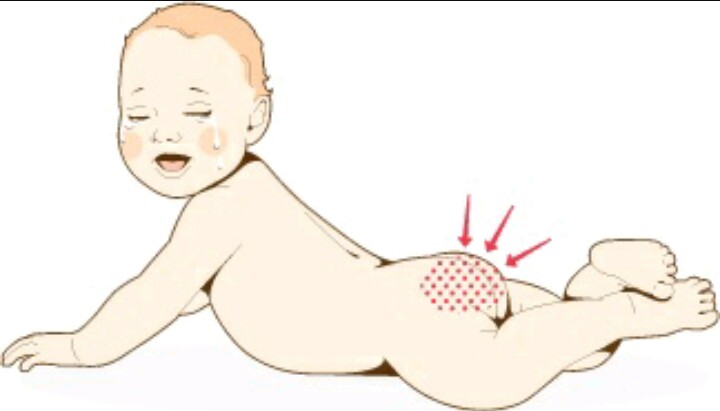
- Diaper. Redness is localized in the buttocks and genitals. They can flake and cause itching. A grayish coating indicates a concomitant fungal infection.
- Contact. Red spots and streaks appear in places where the rough seams of clothing are rubbed. Treatment is needed here if the affected areas are inflamed.
- Change diapers more often and use special baby powders and creams.
- For the little ones, choose clothes with outward facing seams.
- Use hypoallergenic baby powder for washing. Mom's clothes should also be washed using such products.
- Humidify the air in the children's room regularly, especially in winter when the heating is on.

The appearance of red plaques on the skin indicates their good blood supply. Possible causes of this condition may be the following nosologies:
Brown plaques occur when melanin is deposited in the affected area of the dermis, which causes a brown (dark) color. Possible causes may be the following diseases:
Which doctors to contact
With the formation of plaques on the skin, it is necessary to contact a dermatologist to determine the causes of the appearance of this element of the rash.
Plaque diagnostics and examinations
For the diagnosis of fungal skin lesions, scraping from the affected area is used for subsequent microscopic examination.
The development of an allergic reaction requires seeking medical help to identify the allergen, prescribing antihistamines, and sometimes hormonal drugs. In clinical cases of allergy, along with skin tests, analyzes are performed using various sets of common allergens and triggers: a panel for respiratory allergens, for food allergens, and for a combination of both.
Respiratory Panel
Synonyms: Comprehensive Respiratory Allergen Test Panel; Respiratory allergens panel, Allergen respiratory profile, Allergy testing. Brief description of the study "Panel respira...
Brief description of the study "Panel respira...
Up to 5 business days
Available with house call
5 515 RUB
Add to cart
Food Panel, IgE
Food Allergen Panel: hazelnut, peanut, Walnut, almond, cow's milk, egg white, egg ...
Up to 5 working days
Available with house call
5 515 RUB
Add to cart
Food and Respiratory Panel
Panel different allergens: A mixture of grass allergens: fragrant spikelet; perennial rye; timothy; rye cultivated; Woolly buckthorn (GP3) IgE . ..
..
Up to 5 business days
Available with house call
5 515 RUB
Add to cart
In psoriasis, seeing a dermatologist and a rheumatologist can help reduce the symptoms of the disease if appropriate therapy is prescribed. For the diagnosis, it is usually sufficient to examine, determine, the skin manifestations of psoriasis are so characteristic, but if necessary, a differential diagnosis is carried out, including a clinical blood test, feces for the presence of worm eggs and protozoa, and a histological examination of the skin.
Clinical blood test: general analysis, leukoformula, ESR (with microscopy of a blood smear in the presence of pathological changes)
Synonyms: Complete blood count, UAC. Full blood count, FBC, Complete blood count (CBC) with differential white blood cell count (CBC with diff), Hemogram. Brief description of the study CBC: general...
Full blood count, FBC, Complete blood count (CBC) with differential white blood cell count (CBC with diff), Hemogram. Brief description of the study CBC: general...
Up to 1 business day
Available with house call
RUB 810
Add to cart
Fecal test for helminth eggs
Synonyms: Feces on worm eggs; Analysis of feces for eggs of worms. Ova and Parasite Exam; O&P; Stool O&P test. Brief description of the study "Analysis of feces for eggs of helminths&ra...
Up to 1 business day
Available with house call
RUB 570
Add to cart
Fecal analysis for protozoa (PRO stool)
Synonyms: Analysis of faeces for protozoa. Parasite Exam, feces; Parasitic Examination, fecal. Brief description of the study "Analysis of feces for protozoa" Fecal analysis for ...
Parasite Exam, feces; Parasitic Examination, fecal. Brief description of the study "Analysis of feces for protozoa" Fecal analysis for ...
Up to 1 business day
Available with house call
RUB 570
Add to cart
Histological examination of biopsy material and material obtained during surgical interventions (endoscopic material; tissues of the female reproductive system; skin, soft tissues; hematopoietic and lymphoid tissue; bone and cartilage tissue)
Taking biomaterial is paid separately. According to the requirements of clause 17 of the Rules for conducting pathological and anatomical studies, approved. Order of the Ministry of Health of Russia. ..
..
Up to 5 business days
Available with house call
2 880 RUB
Add to cart
Diseases of the stomach and intestines can also lead to plaque formation on the skin. To identify the pathology of the gastrointestinal tract, it is enough to refer to therapist or gastroenterologist, conduct a number of endoscopic examinations (gastroscopy, and, if necessary, colonoscopy), ultrasound of the abdominal organs, perform some screening blood tests for diseases of the liver, intestines, stomach.
Gastroscopy
Examination of the mucosa of the upper gastrointestinal tract with the possibility of biopsy or endoscopic removal of small pathological ...
RUB 4,440 Sign up
Colonoscopy
Endoscopic examination of the colon to look for abnormalities, perform biopsies, and remove small polyps and tumors.
RUB 5,740 Sign up
Comprehensive ultrasound examination of the abdominal organs (liver, gallbladder, pancreas, spleen)
Scanning of the internal organs of the abdominal cavity to assess its functional state and the presence of pathology.
RUB 2,890 Sign up
Liver function tests: screening
Up to 1 business day
Available with house call
RUB 1,935
Add to cart
Diagnosis of celiac disease: intolerance to cereal proteins (gluten)
Up to 8 working days
Available with house call
7 520 RUB
Add to cart
Gastropanel
Up to 9 working days
Available with house call
RUB 4,760
Add to cart
To clarify the diagnosis of keratoma, a skin biopsy is performed and epithelium scraping is performed, followed by microscopic and histochemical examination.
Histological examination of biopsy material and material obtained during surgical interventions (endoscopic material; tissues of the female reproductive system; skin, soft tissues; hematopoietic and lymphoid tissue; bone and cartilage tissue)
Taking biomaterial is paid separately. According to the requirements of clause 17 of the Rules for conducting pathological and anatomical studies, approved. Order of the Ministry of Health of Russia...
Up to 5 working days
Available with house call
2 880 RUB
Add to cart
Examination of scrapings and impressions of tumors and tumor-like formations
Material for research. Imprints and scrapings are obtained from pathological lesions of the skin and mucous membranes (except for the cervix and cervical canal). Relative to test...
Imprints and scrapings are obtained from pathological lesions of the skin and mucous membranes (except for the cervix and cervical canal). Relative to test...
Up to 2 working days
Available with house call
RUB 1,030
Add to cart
If atypical cells are detected in scrapings or biopsies, immediately contact oncologist.
If xanthoma appears on the skin, it is recommended to consult a cardiologist, take blood tests for lipid profile and blood glucose levels, and screen for diabetes.
Lipid profile screening
Up to 1 business day
Available with house call
1 355 RUB
Add to cart
Glucose (in the blood) (Glucose)
Research material Serum or blood plasma. If it is not possible to centrifuge the sample 30 minutes after collection for serum/plasma separation...
If it is not possible to centrifuge the sample 30 minutes after collection for serum/plasma separation...
Up to 1 business day
Available with house call
335 RUB
Add to cart
Diabetes management: advanced
Up to 1 business day
Available with house call
RUB 5 820
Add to cart
What should I do if plaque appears on the skin?
Any newly appeared neoplasms should be shown to a dermatologist. Their cosmetic removal without prior consultation with a specialist is fraught with serious consequences.
Their cosmetic removal without prior consultation with a specialist is fraught with serious consequences.
In addition, there are symptoms that require immediate medical attention:
Plaque treatment
When plaques of an allergic nature appear on the skin, antihistamines are prescribed, in cases of a severe course of the disease, glucocorticosteroids. In addition, it is important to follow a hypoallergenic diet.
In addition, it is important to follow a hypoallergenic diet.
Mycotic plaques require antifungal drugs, both local (ointments, creams) and systemic (tablets). Taking these drugs is associated with a high risk of side effects, and therefore it is possible only after consulting a doctor, accurate verification of the diagnosis and confirmation of the etiology of the disease.
Treatment of psoriasis is multi-stage and complex, it involves constant monitoring by a rheumatologist, taking cytostatics and other drugs, using ointments and shampoos to improve skin condition, using antihistamines to reduce itching, including physiotherapy and a hypoallergenic diet in the treatment regimen.
When confirming the presence of diseases of the gastrointestinal tract, properly selected therapy can stop the appearance of new plaques on the skin, as well as prevent the development of complications of the underlying disease.
Sources:
IMPORTANT!
The information in this section should not be used for self-diagnosis or self-treatment. In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
For a correct assessment of the results of your analyzes in dynamics, it is preferable to do studies in the same laboratory, since different laboratories may use different research methods and units of measurement to perform the same analyzes.
Recommendations
Show more
Fungus
Cystitis
Urethritis
Trauma
Prostatitis
Tumor
Pain in the urethra
Pain in the urethra: causes, diseases in which it develops, methods of diagnosis and treatment.
More
Thyrotoxicosis
Bronchitis
Pulmonary edema
Bronchial asthma
Influenza
Diffuse goiter
Allergy
Tumor
Wheezing
The appearance of wheezing occurs when there is a violation of the passage of air through the bronchial tree. Whistling when breathing can be a sign of serious illness.
Whistling when breathing can be a sign of serious illness.
More
Thyrotoxicosis
Lentigo
Xeroderma
Melanoma
Nevus
Mole
Freckles
Hyperpigmentation of the skin
Hyperpigmentation of the skin: causes, in which diseases it occurs, diagnosis and methods of treatment.
More
Gastritis
Diarrhea
Flatulence
Dysbacteriosis
Allergy
Worms
Ascites
Bloating
In most cases, bloating is associated with flatulence - excessive accumulation of gases in the intestines. Bloating (enlargement) of the abdomen can be due to various reasons.
Bloating (enlargement) of the abdomen can be due to various reasons.
More
Allergy
Adenoids
Nasal polyps
Apnea
Tumor
Rhinitis
Acromegaly
Snoring
Snoring: causes, diseases, diagnosis and treatment.
More
Nothing found
Try editing your query or select a doctor or service from the list.
Doctor not found
Try changing your query or select doctor from the list
Medical office not found
Try changing the query or select medical office from the list
Therapist Traumatologist-orthopedist Endocrinologist Urologist Gynecologist Ultrasound doctor Cardiologist Pediatrician
Nothing found
Please try editing your query
Thank you!
You have successfully made an appointment
Detailed information has been sent to your e-mail
Red dry spots on the skin of a child, on the face, hands
Tips for mothers
Causes of redness on the skin of a child
In newborns, the skin is sensitive due to the fact that the sebaceous glands have not yet adapted to produce protective substances.
Red dry spots on the skin of a child may be a reaction to weather conditions
Red spots on the face of a baby and on other parts of the body may appear due to the aggressive effects of the environment: dry or cold air, exposure to sun or frost
This can be a reaction to hard water, unsuitable bathing products or washing clothes.
The cause of redness on the skin of the baby may be the mother's menu: excessively spicy or allergenic food.
With the elimination of aggressive factors and good care, unpleasant symptoms will disappear by themselves.
But sometimes red spots signal dermatitis that needs treatment:
Red spots on a child's arms or legs are not only caused by allergic dermatitis. Often they are a reaction to insect bites.
Often they are a reaction to insect bites.
In addition to dermatitis, rounded redness on the body of the crumbs may appear due to pink lichen. This fungal infection is transmitted from person to person. Children attending nurseries and kindergartens are more likely to suffer from it.
Reddish spots are due to dysbacteriosis. Also, different types of skin redness can indicate various infectious diseases: rubella, measles, scarlet fever, chickenpox. Usually they are accompanied by poor health and fever.
What to do if the child is covered with red spots
First of all, it is necessary to exclude unfavorable factors: