Do you get tested for chlamydia when pregnant
Chlamydia and pregnancy | Pregnancy Birth and Baby
Chlamydia and pregnancy | Pregnancy Birth and Baby beginning of content3-minute read
Listen
Chlamydia is a bacterial sexually transmitted infection (STI) that affects both men and women. Chlamydia can also cause a number of issues during pregnancy.
Most people with chlamydia are unaware that they have the infection. Left untreated, chlamydia can cause serious complications including infertility and chronic pain. Chlamydia is fairly easy to treat if you know you have it — one course of antibiotics is usually enough.
Causes of chlamydia
Chlamydia is caused by an infection with the bacterium Chlamydia trachomatis. It is spread by unprotected (unsafe) vaginal or anal sex with an infected person.
Chlamydia is the most commonly reported STI in Australia.
What are the symptoms of chlamydia?
Most men and women with chlamydia have no signs or symptoms, which makes it very easy to spread. Some people have the infection for many months or years without knowing it.
Women who get symptoms may have:
- vaginal discharge
- bleeding between periods or after sex
- burning or pain when urinating
- abdominal or pelvic pain
- pain during sex
Men who get symptoms may have some clear discharge from the penis or pain during urination.
In rare cases, people with chlamydia have sore joints (arthritis) or inflammation of the eye (uveitis).
Diagnosing chlamydia
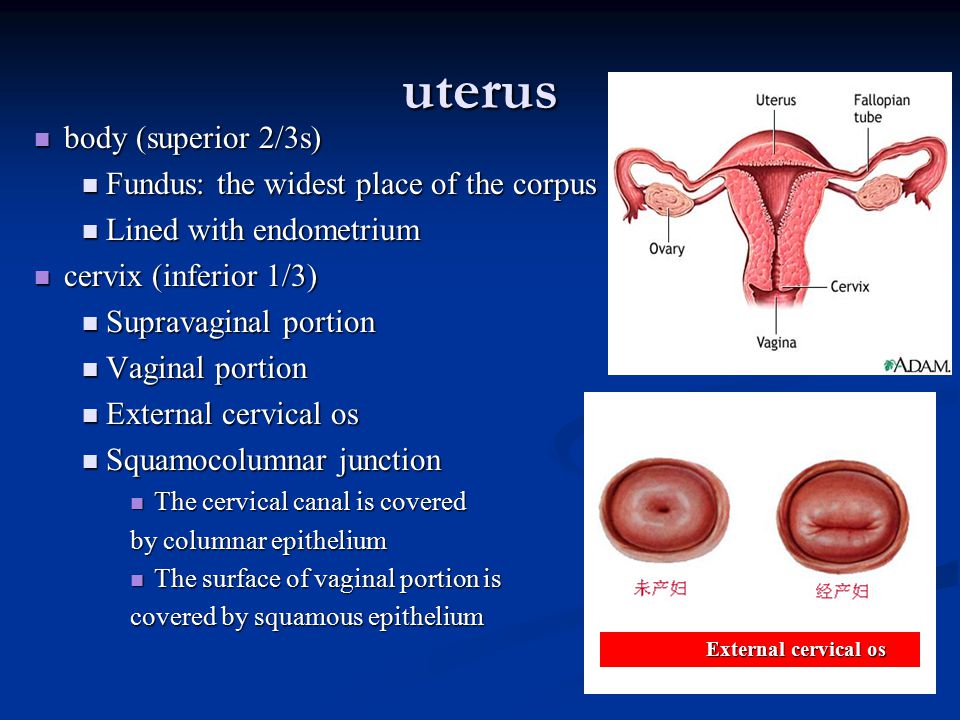
Chlamydia is easily diagnosed. Your doctor may take a sample from the vagina, cervix, anus or penis, and may ask for a urine test. These are sent to a laboratory for testing.
If you think you or your partner have chlamydia, see your doctor or sexual health clinic so you can both be tested. It is important that any sexual partners of people with chlamydia are tested, even if they don’t have symptoms.
It is important that any sexual partners of people with chlamydia are tested, even if they don’t have symptoms.
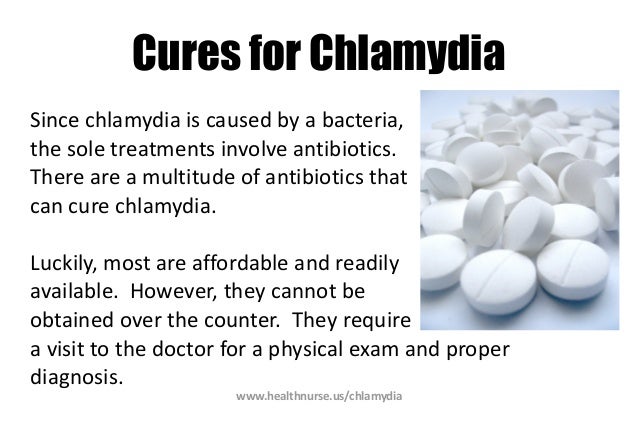
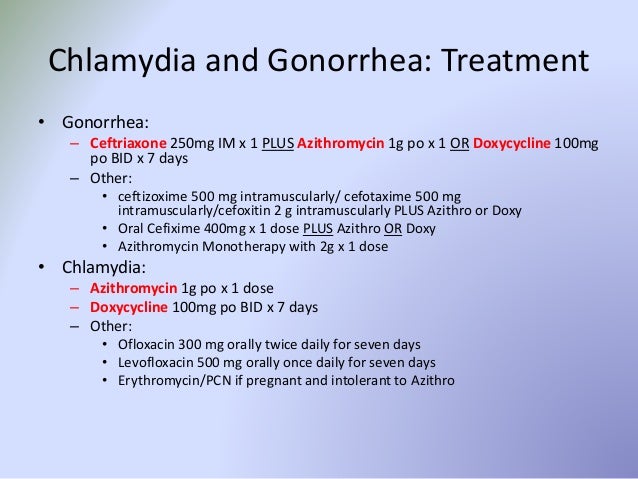
Treating chlamydia
Treatment for chlamydia is a course of antibiotics. It is important to avoid sex until the full course of treatment is finished, and for at least a week following. You should have another test 3 months after you are treated.
If you have chlamydia, all of your sexual partners should be informed, tested and treated, as they may be infected and can infect you, and others, again after treatment.
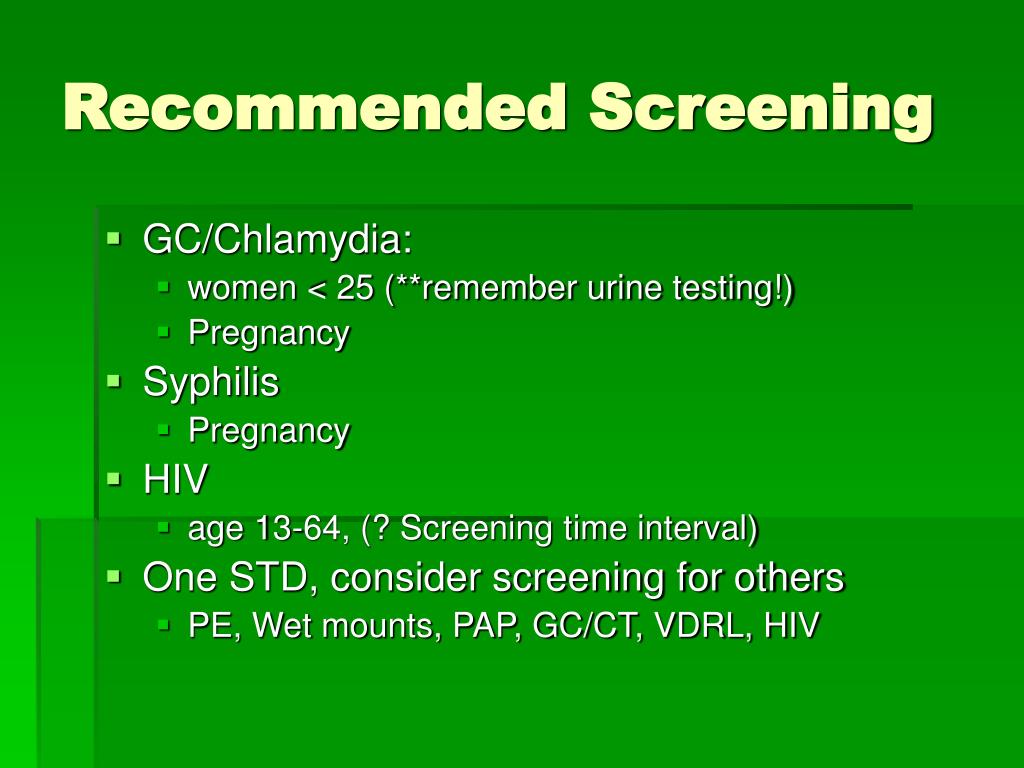
If your partner has had a positive test for chlamydia, you should be treated even if you have had a negative test result. As chlamydia infection increases the possibility of contracting other infections, it is important to be tested for other STIs such as gonorrhoea, hepatitis, HIV and syphilis. Using latex condoms and a water-based lubricant is the most effective way to prevent STIs. People who have chlamydia for long periods without treatment risk becoming infertile or developing arthritis.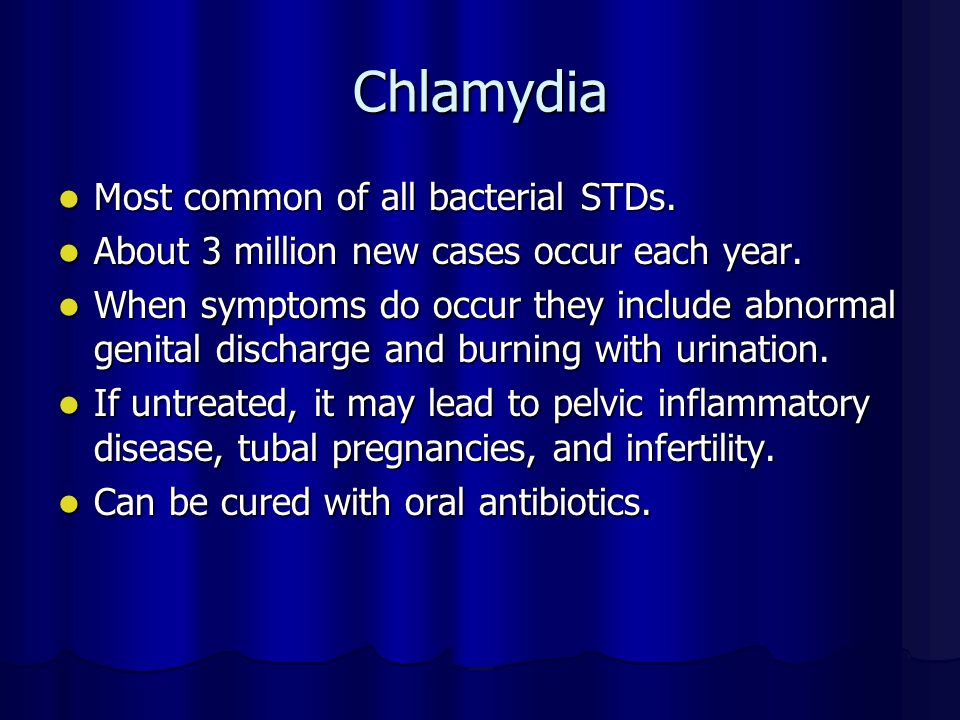 Women can get pelvic inflammatory disease, and men can get epididymitis (a painful infection near the testicle).
Women can get pelvic inflammatory disease, and men can get epididymitis (a painful infection near the testicle).
Chlamydia complications
If chlamydia isn't treated properly, it can cause serious complications. People who have chlamydia for long periods without treatment risk becoming infertile or developing arthritis.
For women, chlamydia can spread into the uterus and fallopian tubes, causing pelvic inflammatory disease. Pelvic inflammatory disease can lead to ectopic pregnancies, chronic pelvic pain and infertility.
In men, chlamydia can cause epididymitis (a painful infection near the testicle) or spread to the prostate gland, and the tubes that carry sperm, which may result in chronic pain and/or fertility problems.
Both men and women can develop arthritis, eye inflammation and inflammation of the rectum.
Chlamydia and pregnancy
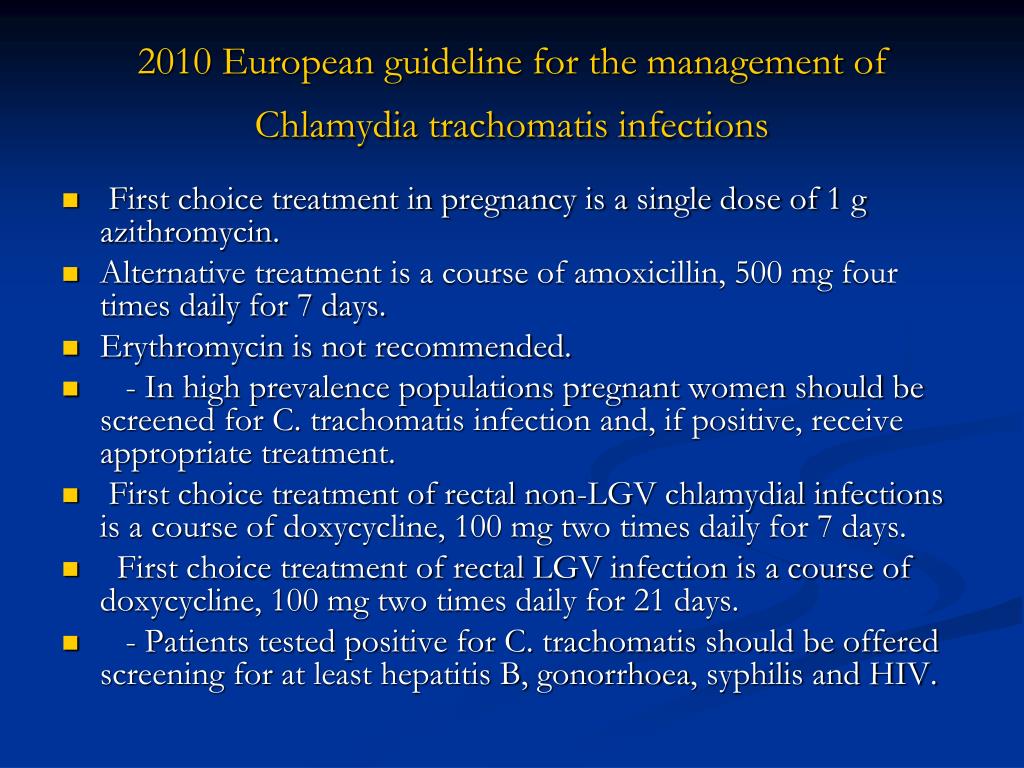
Because of this, doctors recommend that pregnant women under the age of 30 should be screened for chlamydia.
Pregnant women who are infected with chlamydia have an increased risk of their waters breaking prematurely, causing the baby to be born early.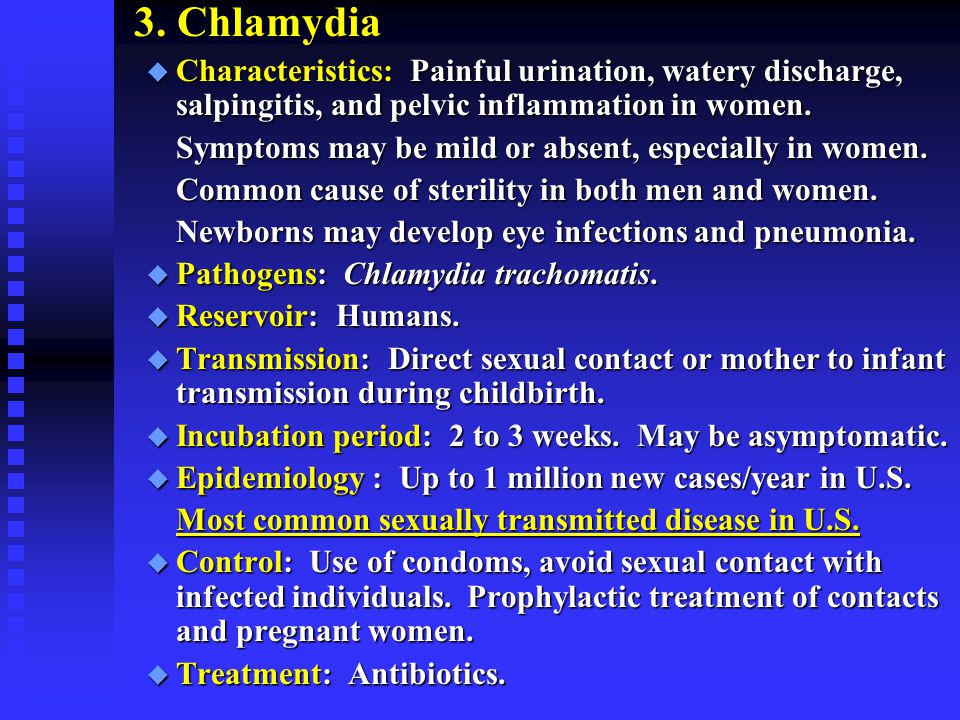
If a woman has chlamydia when giving birth, the baby might become infected during delivery. These babies can develop an eye infection (conjunctivitis) or pneumonia, and might need antibiotics. Chlamydia has also been associated with low birthweight.
The antibiotics used to treat chlamydia are safe in pregnancy and are used in pregnant women for many other types of infections.
Sources:
Australian Sexual Health Alliance (STI Management Guidelines for use in primary care; Chlamydia), King Edward Memorial Hospital Women and Newborn Health Service (Chlamydia clinical practice guideline), Lab Tests Online AU (Chlamydia), Melbourne Sexual Health Centre (National Management Guidelines for Sexually Transmissible Infections - Chlamydia), NSW Health (Chlamydia fact sheet)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: November 2020
Back To Top
Related pages
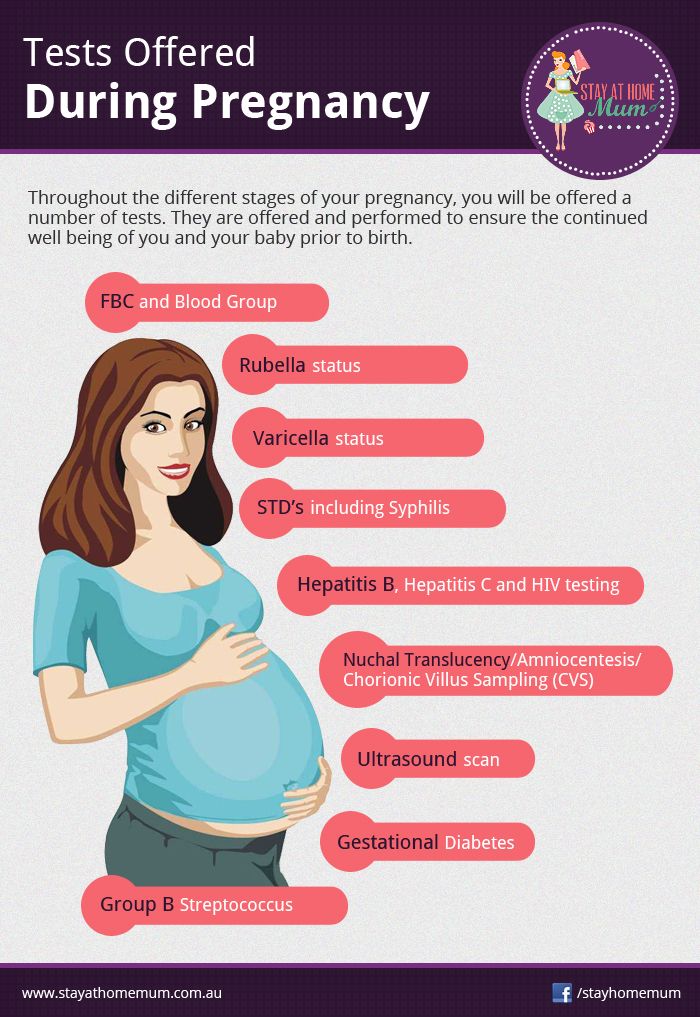
- Routine antenatal tests
- Antenatal care during your pregnancy
Need more information?
Chlamydia - MyDr.com.au
Chlamydia is a sexually transmitted infection (STI). It affects both men and women, and it's spread by having sex with a person who has the infection.
Read more on myDr website
Chlamydia - Better Health Channel
Chlamydia is often called the 'silent infection' because most people do not realise they have it.
Read more on Better Health Channel website
Chlamydia fact sheet - Fact sheets
Chlamydia is a sexually transmissible infection. Many people who are infected do not have symptoms of infection but can still spread the disease. Chlamydia can lead to infertility, and other complications if not treated.
Many people who are infected do not have symptoms of infection but can still spread the disease. Chlamydia can lead to infertility, and other complications if not treated.
Read more on NSW Health website
Chlamydia | Family Planning NSW
Chlamydia is a common sexually transmitted infection (STI) caused by a bacteria. It affects both men and women. Most people with chlamydia do not have symptoms. This means you can pass the infection to a partner without knowing it. Having a regular sexual health check-up can help you find out if you have chlamydia.
Read more on Family Planning NSW website
Chlamydia treatment for your partner - Play Safe
Did you know it’s possible for your partner to get treated for Chlamydia without ever having to see a GP or go to a sexual health clinic? This is known as Patient Delivered Partner Therapy (PDPT)
Read more on NSW Health website
The facts about Chlamydia, what it is, how to prevent it, and how to treat it
Chlamydia is on the rise in Australia and it’s the most important thing for young people to test for.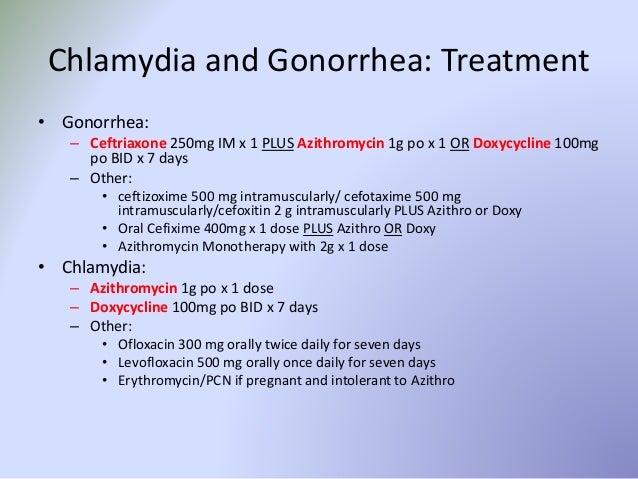 It often doesn’t have any symptoms which means that it’s easy to miss without regular STI testing.
It often doesn’t have any symptoms which means that it’s easy to miss without regular STI testing.
Read more on NSW Health website
Trachoma - Eye Infection
Trachoma is a preventable eye condition caused by repeated infections with eye strains of the bacterium Chlamydia trachomatis that lead to a roughening of the inner surface of the eyelid.
Read more on Queensland Health website
Gonorrhoea | Family Planning NSW
Gonorrhoea is a bacterial sexually transmitted infection (STI). It is spread through vaginal, anal or oral sex, or by the fingers and hands from the genitals to the eyes. It is less common in the general community than other STIs such as chlamydia.
Read more on Family Planning NSW website
Sexually transmitted infections (STIs) | Healthy Male
A sexually transmitted infection (STI) is an infection you get or give during sexual activity. STIs can be caused by viruses (e.g., human immunodeficiency virus, herpes), bacteria (e.g., gonorrhea, syphilis), or parasites (e.g., pubic lice).
STIs can be caused by viruses (e.g., human immunodeficiency virus, herpes), bacteria (e.g., gonorrhea, syphilis), or parasites (e.g., pubic lice).
Read more on Healthy Male - Andrology Australia website
STIs and pregnancy
Sexually transmitted infections (STIs), if left untreated, can cause serious problems for both mother and child.
Read more on Pregnancy, Birth & Baby website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.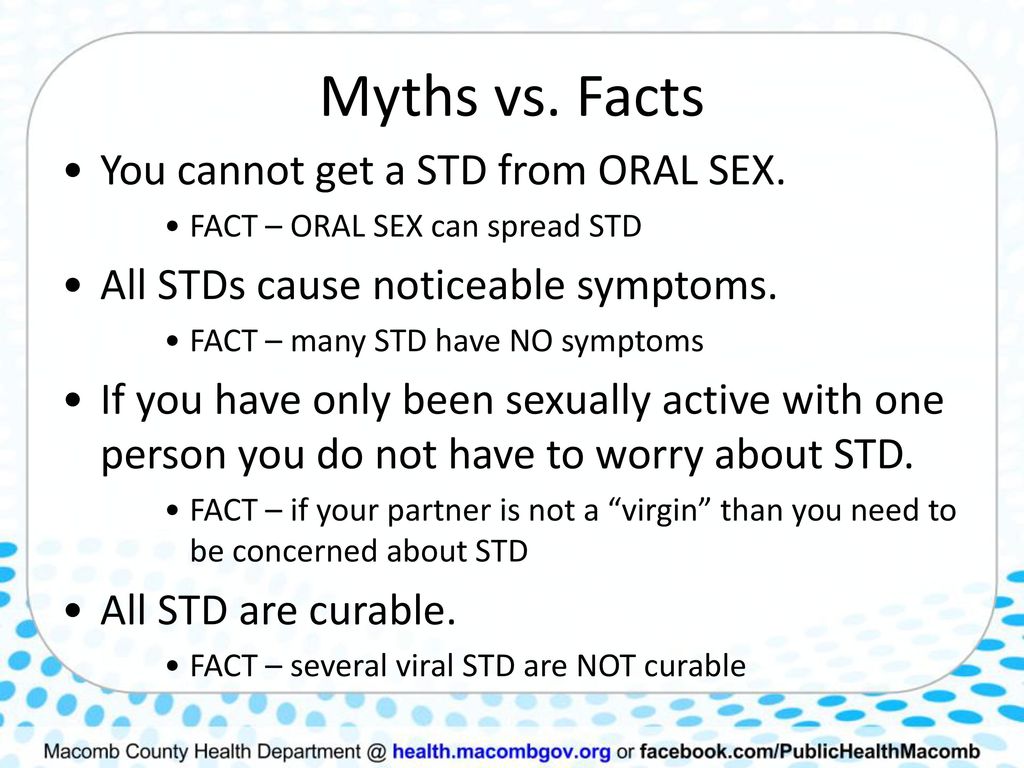
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
STD Facts - STDs & Pregnancy
If you are pregnant, you can become infected with the same sexually transmitted diseases (STDs) as women who are not pregnant. Pregnant women should ask their doctors about getting tested for STDs, since some doctors do not routinely perform these tests. This fact sheet answers basic questions about STDs during pregnancy.

I’m pregnant. Can I get an STD?
Yes, you can. Women who are pregnant can become infected with the same STDs as women who are not pregnant. Pregnancy does not provide women or their babies any additional protection against STDs. Many STDs are ‘silent,’ or have no symptoms, so you may not know if you are infected. If you are pregnant, you should be tested for STDs, including HIV (the virus that causes AIDS), as a part of your medical care during pregnancy. The results of an STD can be more serious, even life-threatening, for you and your baby if you become infected while pregnant. It is important that you are aware of the harmful effects of STDs and how to protect yourself and your unborn baby against infection. If you are diagnosed with an STD while pregnant, your sex partner(s) should also be tested and treated.
How can STDs affect me and my unborn baby?
STDs can complicate your pregnancy and may have serious effects on both you and your developing baby. Some of these problems may be seen at birth; others may not be discovered until months or years later. In addition, it is well known that infection with an STD can make it easier for a person to get infected with HIV. Most of these problems can be prevented if you receive regular medical care during pregnancy. This includes tests for STDs starting early in pregnancy and repeated close to delivery, as needed.
In addition, it is well known that infection with an STD can make it easier for a person to get infected with HIV. Most of these problems can be prevented if you receive regular medical care during pregnancy. This includes tests for STDs starting early in pregnancy and repeated close to delivery, as needed.
Should I be tested for STDs during my pregnancy?
Yes. Testing and treating pregnant women for STDs is a vital way to prevent serious health complications to both mother and baby that may otherwise happen with infection. The sooner you begin receiving medical care during pregnancy, the better the health outcomes will be for you and your unborn baby. The Centers for Disease Control and Prevention’s 2015 STD Treatment Guidelines recommend screening pregnant women for STDs. The CDC screening recommendations that your health care provider should follow are incorporated into the table on the STDs during Pregnancy – Detailed CDC Fact Sheet.
Be sure to ask your doctor about getting tested for STDs. It is also important that you have an open, honest conversation with your provider and discuss any symptoms you are experiencing and any high-risk sexual behavior that you engage in, since some doctors do not routinely perform these tests. Even if you have been tested in the past, you should be tested again when you become pregnant.
It is also important that you have an open, honest conversation with your provider and discuss any symptoms you are experiencing and any high-risk sexual behavior that you engage in, since some doctors do not routinely perform these tests. Even if you have been tested in the past, you should be tested again when you become pregnant.
Can I get treated for an STD while I’m pregnant?
It depends. STDs, such as chlamydia, gonorrhea, syphilis, trichomoniasis and BV can all be treated and cured with antibiotics that are safe to take during pregnancy. STDs that are caused by viruses, like genital herpes, hepatitis B, or HIV cannot be cured. However, in some cases these infections can be treated with antiviral medications or other preventive measures to reduce the risk of passing the infection to your baby. If you are pregnant or considering pregnancy, you should be tested so you can take steps to protect yourself and your baby.
How can I reduce my risk of getting an STD while pregnant?
The only way to avoid STDs is to not have vaginal, anal, or oral sex.
If you are sexually active, you can do the following things to lower your chances of getting chlamydia:
- Being in a long-term mutually monogamous relationship with a partner who has been tested and has negative STD test results;
- Using latex condoms the right way every time you have sex.
You can add this content to your website by syndicating.
STDs during Pregnancy - CDC Detailed Fact Sheet
Detailed fact sheets are intended for physicians and individuals with specific questions about sexually transmitted diseases. Detailed fact sheets include specific testing and treatment recommendations as well as citations so the reader can research the topic more in depth.
Pregnancy screening not STD
If you are planning a pregnancy, you should know that you need to be screened for sexually transmitted infections before pregnancy. How to correctly pass all the tests, what kind of treatment is needed if the infection is still detected?
In this article, only those infections that often become the subject of controversy will be consecrated - how best to identify them, whether they always need to be treated, what treatment is better to prescribe to a woman. Very often, patients engage in self-deception, completely trusting the results of a single analysis. Five infections will be consecrated - chlamydia, mycoplasmosis, urepaplasmosis, herpes, cytomegalovirus.
Very often, patients engage in self-deception, completely trusting the results of a single analysis. Five infections will be consecrated - chlamydia, mycoplasmosis, urepaplasmosis, herpes, cytomegalovirus.
If you have been diagnosed with chlamydia
Chlamydia is a sexually transmitted infection through unprotected intercourse. Chlamydia bacteria can be the cause of chlamydia. The likelihood that you will become infected with them in the household way - after sitting on the toilet, swimming in the pool - is very low, since chlamydia quickly die outside the human body.
Chlamydia symptoms
The incubation period is 7 to 30 days. In a woman: white, yellow, clear discharge from the vagina, pain during urination, during sexual intercourse, pain in the lower abdomen, in the lumbar region. In a man: discharge from the urethra - transparent, scanty, pain during urination and coitus.
Chlamydia is often asymptomatic and can be detected by testing. A chlamydial infection can be a complication. For women, it is fraught with inflammatory diseases of the uterus and appendages, which can lead to infertility. For men, it is fraught with inflammation of the epididymis - epididymitis. In order to identify this infection, you need to pass an analysis for chlamydia using the PCR method - DNA diagnostics. If the doctor detects chlamydia, he will prescribe a course of treatment that must be completed by both partners.
A chlamydial infection can be a complication. For women, it is fraught with inflammatory diseases of the uterus and appendages, which can lead to infertility. For men, it is fraught with inflammation of the epididymis - epididymitis. In order to identify this infection, you need to pass an analysis for chlamydia using the PCR method - DNA diagnostics. If the doctor detects chlamydia, he will prescribe a course of treatment that must be completed by both partners.
Treatment for chlamydia: a course of antibiotics for 21 days. If chlamydia is detected during pregnancy, then the woman is also prescribed antibiotics that are allowed during pregnancy - a course of 2 weeks, but this can only be done after the 20th week of pregnancy.
Why chlamydia is dangerous during pregnancy
Chlamydia increases the risk of miscarriage. If the fetus becomes infected, this will lead to chlamydial pneumonia in the newborn, to the fact that he will develop inflammatory eye diseases.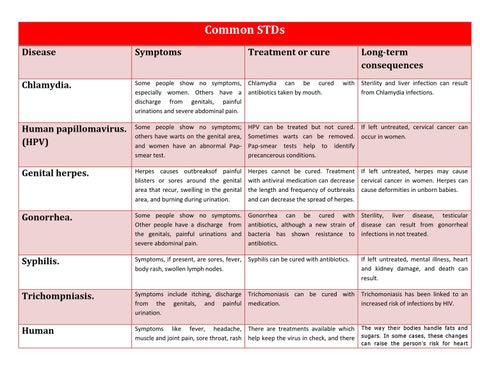 Treatment of chlamydial infection during pregnancy is a must!
Treatment of chlamydial infection during pregnancy is a must!
If ureplasmosis, mycoplasmosis is detected
Ureaplasmas are bacteria that live in the human body, on the mucous membranes of the genital organs, urinary tract. These microorganisms can be classified as conditionally pathogenic, which means that every person has them. If the number of bacteria increases sharply, then it begins to exceed the permissible limits, a person develops painful symptoms. This happens when the immune system is weakened.
Mycoplasmosis and ureaplasmosis are sexually transmitted. Also, another way of transmission is from a child to a mother, while a person may grow up to a certain point without even suspecting that this disease is the cause of a weakened immune system. Symptoms of ureplasmosis: inflammatory diseases of the uterus and appendages, cystitis, pyelonephritis, kidney stones, bacterial vaginosis. In men, these bacteria most often multiply rapidly with urethritis, pyelonephritis, kidney stones.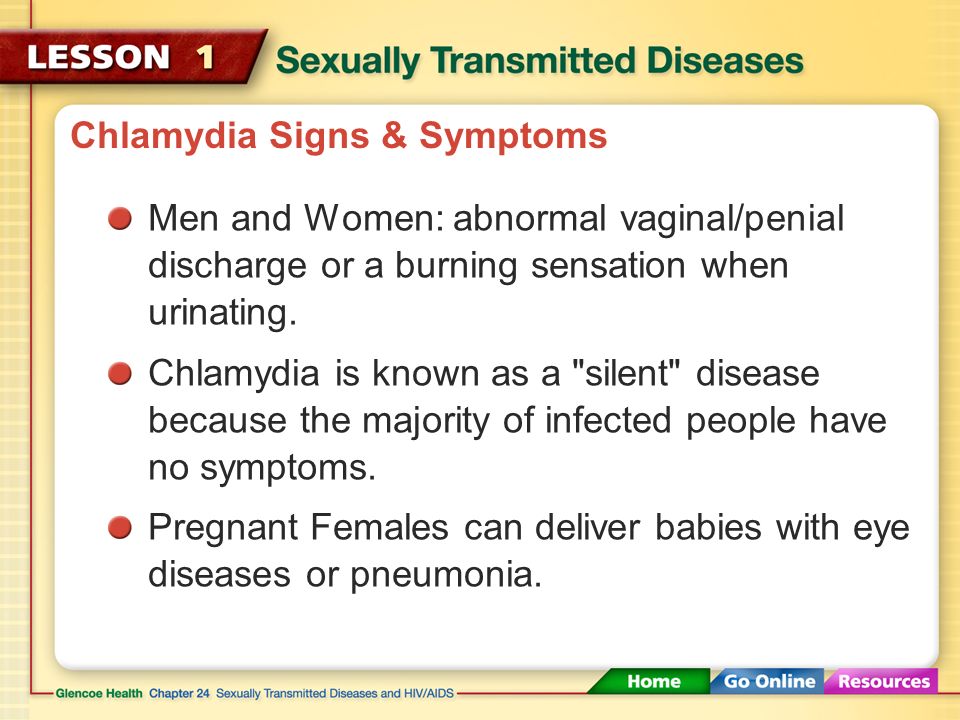
Diagnosis of ureplasmosis
In order to identify ureplasmosis, it is necessary to take tests using PCR or culture.
The culture method shows a more objective picture - the number of bacteria. PCR provides information that these microorganisms are in the genitourinary tract, but does not establish their number. If a woman is found to have mycoplasmas or ureaplasmas in the amount of 102, then treatment is not needed, but if in the amount of 104, then treatment is necessary. Culture can also determine which antibiotic is needed to make treatment more effective. When detecting ureaplasmas and mycoplasmas in a blood test, there are often false positive results.
Treatment of ureaplasmosis. They are usually treated when a woman has health problems - inflammation of the uterus, appendages, cystitis, pyelonephritis. If women do not experience pain, then these infections do not need to be treated. Unmotivated use of antibiotics will only lead to a violation of the microflora of the vagina.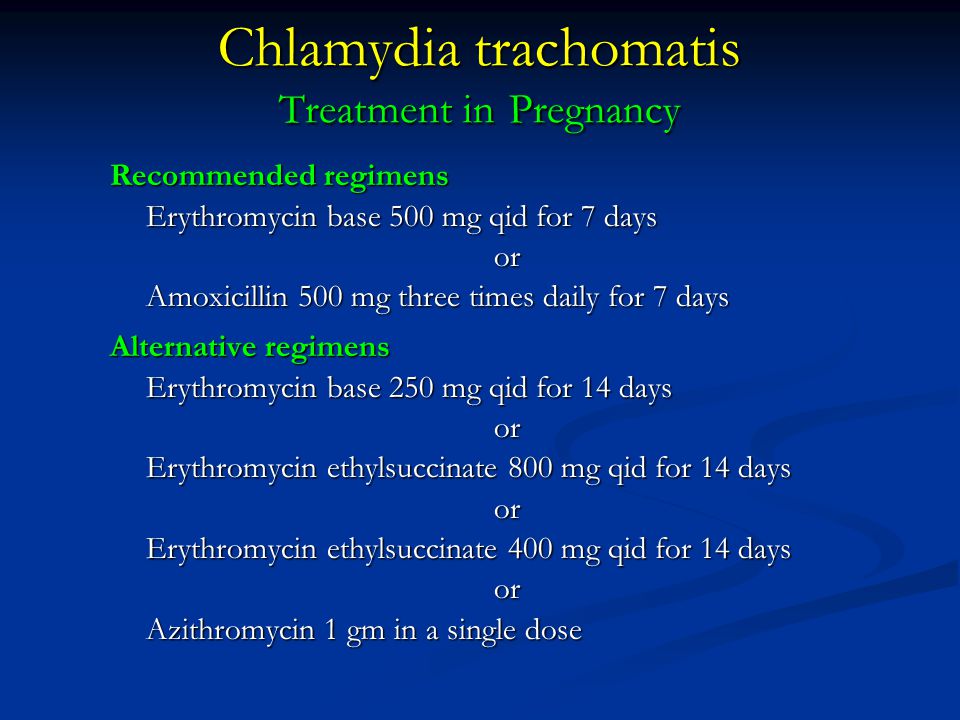
If we are talking about planning a pregnancy, then it is necessary to treat it, even if the woman does not have symptoms of the disease. Treatment consists of taking antibiotics for a course of 10 days. In order to start taking, you need to do a seeding for sensitivity to antibiotics in order to determine the choice of the desired drug. Both husband and wife must take the course.
If ureaplasma is detected during pregnancy, then the woman is also prescribed an antibiotic. Treatment is carried out only after the 20th week of pregnancy. Prior to this, the woman is prescribed immunoglobulin therapy (from the 10th week of pregnancy).
Why ureaplasma and mycoplasma are dangerous
Ureaplasma and mycoplasma can lead to abortion or premature birth, and the child can also be infected. Also, children can develop pathologies of the urinary tract, cystitis, pyelitis.
If you have found genital herpes
The herpes simplex virus is dangerous for your unborn baby.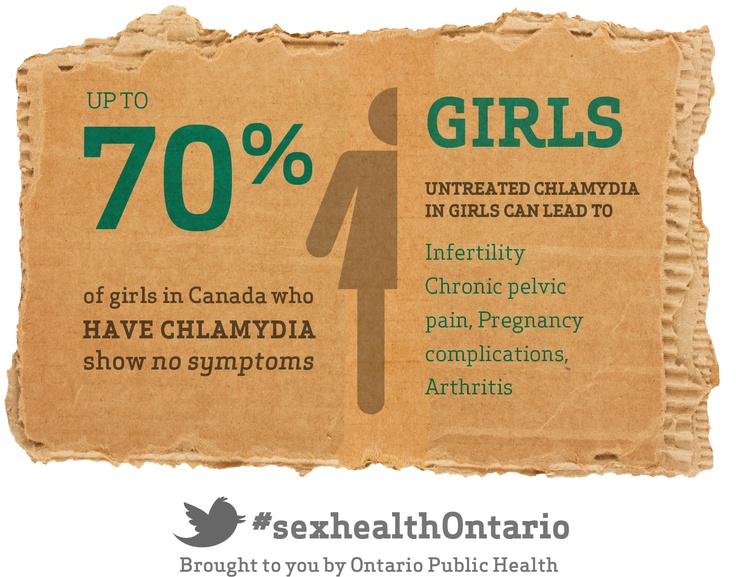 The genital child is sexually transmitted, may be passed on by the mother to the child. A person lives and does not know that an infection lives in him, and when immunity is weakened, herpes suddenly manifests itself.
The genital child is sexually transmitted, may be passed on by the mother to the child. A person lives and does not know that an infection lives in him, and when immunity is weakened, herpes suddenly manifests itself.
Symptoms of genital herpes - when infected with herpes, there is pain, burning, swelling in the genital area. These symptoms are accompanied by general malaise, fever, headache. Small bubbles appear on the genitals, which are filled with liquid. The blisters burst and painful red sores form. Heal within two weeks.
If a relapse of the disease occurs, then it is accompanied by a rise in temperature, hypothermia and stress can lead to relapses. Genital herpes is asymptomatic, it is possible for a husband to be infected by his wife, or vice versa.
Diagnosis of genital herpes : if you are planning a pregnancy, you need to take a blood test from a vein for IgM and IgG antibodies to herpes simplex viruses.
If, according to the results of the analysis, class G antibodies are detected, the organism has already encountered genital herpes. If antibodies to class M immunoglobulins are present, genital herpes is in an acute stage.
If antibodies to class M immunoglobulins are present, genital herpes is in an acute stage.
Genital herpes treatment : treatment with antiviral drugs, partner should also be tested - he may not be infected. During pregnancy, antiviral drugs should not be taken, but it is necessary to undergo immunoglobulin therapy.
Why genital herpes is dangerous during pregnancy
Primary herpes infection during pregnancy is the most dangerous. It leads to termination of pregnancy, as well as to serious damage to the fetus. If a pregnant woman becomes infected with this virus shortly before the expected birth of a child, then the doctor refuses to give birth naturally, the woman is given a caesarean section. In natural childbirth, the risk of infection of the child when passing through the mother's birth canal is high. If the disease is in the acute phase, then the child is highly likely to become infected, so you need to treat it in a timely manner.
If cytomegalovirus is detected
Cytomegalovirus is sexually transmitted, it can also be transmitted from mother to fetus, it is possible to transmit the virus through kissing, through blood.
Cytomegalovirus is asymptomatic, in a month or two a mononucleosis-like syndrome. It is similar to ARVI and flu, accompanied by high fever, chills, a person gets very tired, feels unwell, and has a headache.
If the immune system is weakened, then cytomegalovirus can cause serious diseases - damage to the eyes, lungs, digestive system and brain.
Diagnosis of cytomegalovirus : it can be detected by the results of a blood test from a vein for antibodies of the IgM and IgG classes to cytomegalovirus. If antibodies to class M immunoglobulins are fixed, then the disease is in the acute stage, if antibodies to class G immunoglobulins are detected, then the body has already met with this infection.
Treatment of cytomegalovirus : a woman is prescribed immune drugs, during pregnancy immunotherapy is carried out using approved drugs.
Why cytomegalovirus is dangerous during pregnancy: primary infection with cytomegalovirus during pregnancy is dangerous, it can lead to infection of the fetus, abortion, and fetal malformations. Treatment of cytomegalovirus before pregnancy and during pregnancy is mandatory.
Treatment of cytomegalovirus before pregnancy and during pregnancy is mandatory.
How to get tested for sexually transmitted diseases
Do this before your period, right after it. On such days, the woman's immunity is reduced. 20 days before the test, you need to stop taking antibiotics, stop putting candles, etc. Before visiting the doctor, you do not need to wash yourself, take a shower.
When are tests taken?
For the first time - before pregnancy. If an infection is found, then you need to undergo treatment, then re-take tests. Within 3 weeks, sexual activity must be carried out with condoms. One of the partners may not be cured.
After the onset of pregnancy, you will be registered with an obstetrician-gynecologist, the doctor will once again offer to take tests. New surges are possible during pregnancy, as the woman's immunity is greatly weakened.
If a doctor prescribes several courses of antibiotics in a row to treat the same infection, then it is worth considering whether to continue treatment with him, it is worth looking for another clinic.
Obstetrician-gynecologist Kurylenko Elena Georgievna
Get tested for chlamydia. PCR smear for chlamydia during pregnancy
print version
Biomaterial
For this study, the laboratory accepts the following biomaterial:
- Urine
- Prostate secret
- Scraping / vaginal discharge
- Scraping / discharge from the urethra
- Scraping / discharge from the cervical canal
Study preparation
You can make an appointment with a urologist to take a secret of the prostate for research.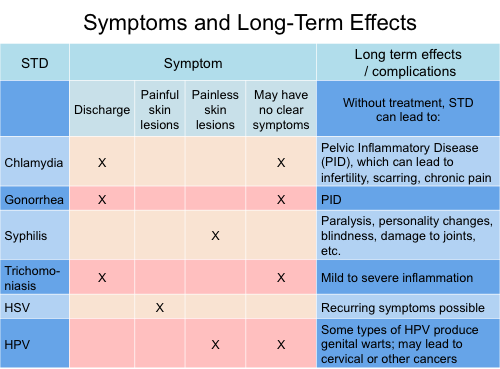
Preparation conditions are determined by the attending physician.
Recommended sampling:
- not earlier than the 5th day of the menstrual cycle (outside spotting) and not later than 5 days before the expected start of menstruation;
- not earlier than 48 hours after sexual intercourse, after colposcopy, ultrasound with the use of a vaginal probe, the use of lubricants, tampons, spermicides, the introduction of medicines, creams into the vagina, douching;
- not earlier than 2 weeks after antimicrobial treatment;
- taking a swab from the urethra is carried out no earlier than 2 hours after the last urination.
Attention! For women, the detection of STI pathogens by PCR in the urine is not informative!
Urine collection in men is carried out after careful toileting of the external genitalia. It is necessary to free the external opening of the urethra by pulling the skin fold. Collect the first portion of morning urine in the amount of 10-15 ml in a universal plastic container.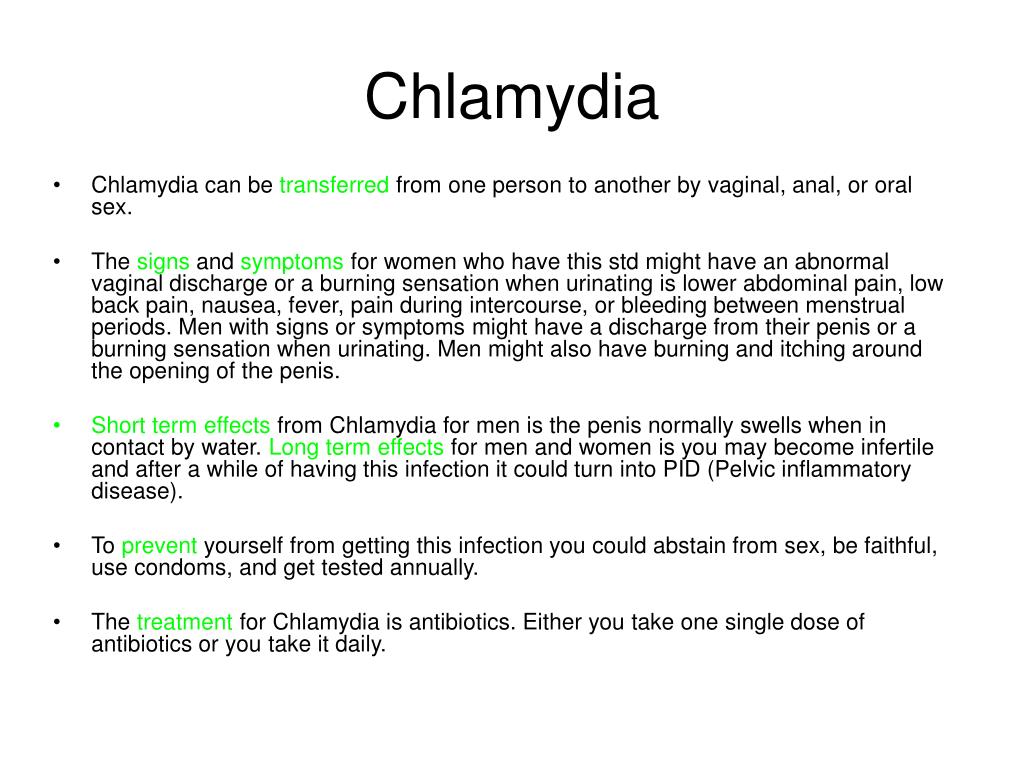
Attention! Calling a nurse at home is possible only if urine is selected as a biomaterial for men. In other cases, this service cannot be ordered with a house call!
Genital scrapings are NOT performed at the following offices.
Biomaterial is taken only by a gynecologist in the following patients:
- pregnant women;
- girls who are not sexually active.
Therefore, before visiting the CMD office/clinic, please check the doctor's appointment schedule by calling the helpline.
Test method
- PCR
Chlamydia infection is caused by the gram-negative bacterium Chlamydia trachomatis. Chlamydia trachomatis DNA is a direct marker of the presence of the pathogen.
Urogenital chlamydial infection (urogenital chlamydia) is the most common sexually transmitted infection (STI).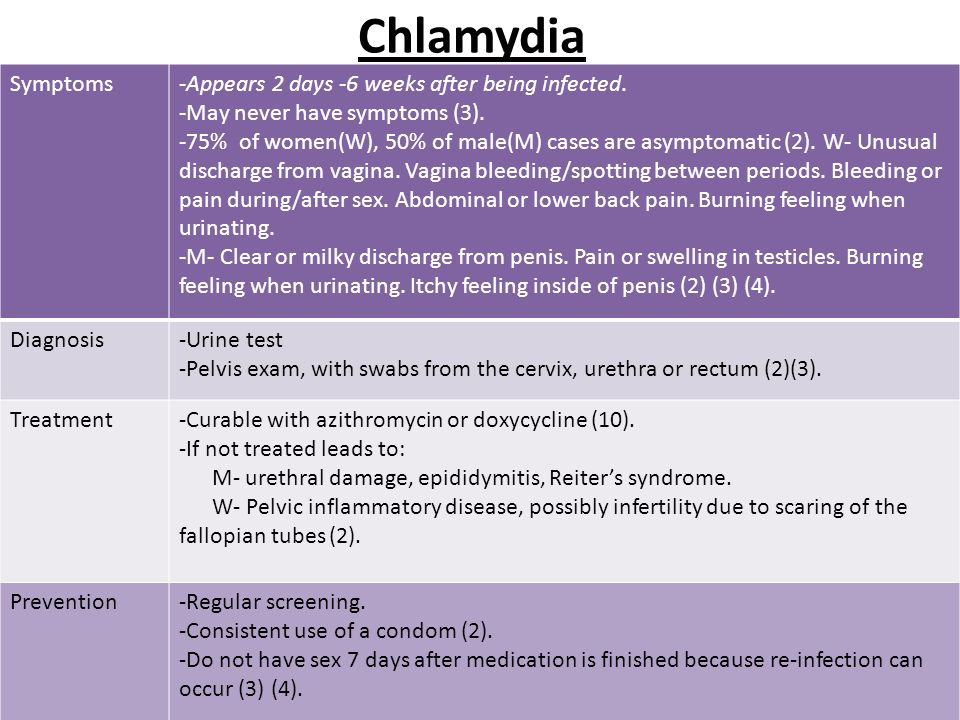 Uncomplicated chlamydial infection occurs in men most often in the form of urethritis, in women - in the form of mucopurulent cervicitis. A significant part of cases of urogenital chlamydial infection occurs in an asymptomatic or oligosymptomatic form and manifests itself already at the stage of complications. The main complications are: epididymitis, endometritis, salpingitis, salpingoophoritis, ectopic pregnancy, tubal infertility, Reiter's disease.
Uncomplicated chlamydial infection occurs in men most often in the form of urethritis, in women - in the form of mucopurulent cervicitis. A significant part of cases of urogenital chlamydial infection occurs in an asymptomatic or oligosymptomatic form and manifests itself already at the stage of complications. The main complications are: epididymitis, endometritis, salpingitis, salpingoophoritis, ectopic pregnancy, tubal infertility, Reiter's disease.
Early detection of chlamydial infection makes it possible not only to prevent its further spread and transmission to offspring, but also significantly reduces the risk of complications.
Any suspicion of a chlamydial infection should be tested for chlamydia.
Indications for testing:
- Screening for people at high risk (persons under 25 years of age and with a non-regular sexual partner)
- Examination in the presence of complaints and clinical manifestations of inflammation of the urogenital tract
- Planning for pregnancy and during pregnancy
- Examination of persons whose sexual partners have complaints or are diagnosed with STIs
Reference values (standard version):
| Parameter | Reference values |
|---|---|
| Chlamydia trachomatis DNA | Not detected |
Detection of Chlamydia trachomatis DNA indicates infection with chlamydia.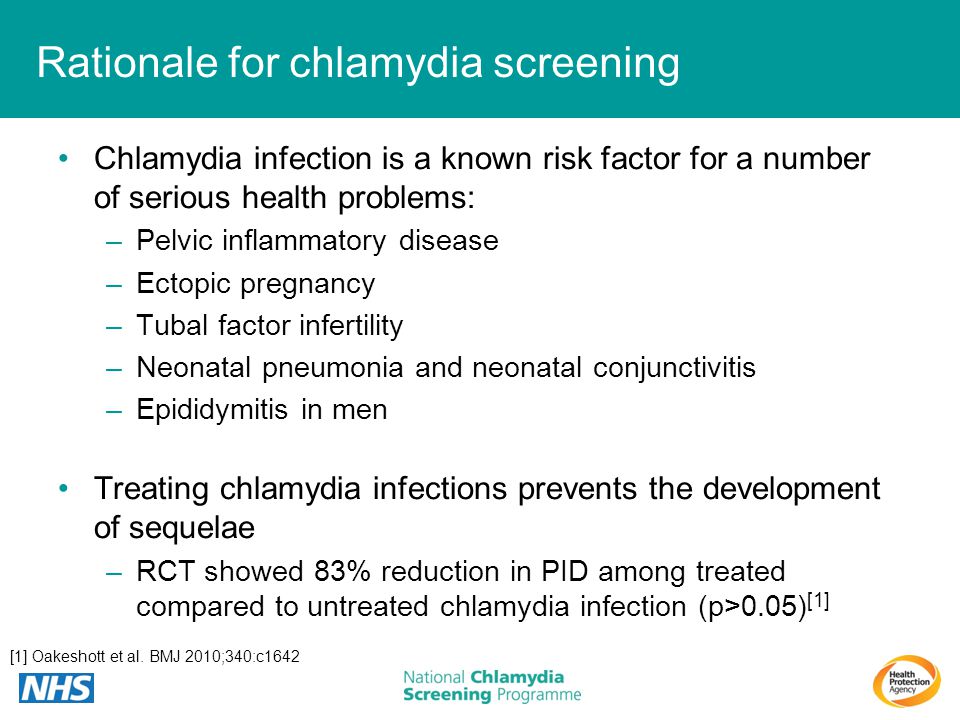
We draw your attention to the fact that the interpretation of the results of studies, the establishment of a diagnosis, as well as the appointment of treatment, in accordance with the Federal Law No. 323-FZ "On the Fundamentals of Protecting the Health of Citizens in the Russian Federation" dated November 21, 2011, must be carried out by a doctor of the appropriate specialization.
- The code:
-
010001
can be taken at home
- Price:
-
When ordering several services at a time, the service for collecting biomaterial is paid only once.
374 R.
- + 1 350 rubles. Collection of prostate secretion
- + 390 rubles Taking a scraping/smear
cheaper as part of a complex
- Deadline:
-
The specified period does not include the day of taking the biomaterial.
1 k.d.
As part of the complex is cheaper than
Program Minimum (7)
- Code:
- 300055
- Deadline:
- 1 k.d.
Price: 2 140 rubles
Medium program (9)
- Code:
- 300056
- Deadline:
- 1 k.
 d.
d.
Price: 2 730 rubles
Program Maximum (12)
- Code:
- 300057
- Deadline:
- 1 k.d.
Price: 3 305 r.
Premium Program (15)
- Code:
- 300058
- Deadline:
- 1 k.
 d.
d.
Price: $3,895
With this analysis order
The causative agent of candidiasis (Candida albicans), qualitative determination of DNA
- Code:
- 020001
- Deadline:
- 1 k.d.
Price: 374 r.
Microscopic examination of a smear from the vagina and cervical canal
- Code:
- 110310
- Deadline:
- 1 k.d.
Price: 495 r.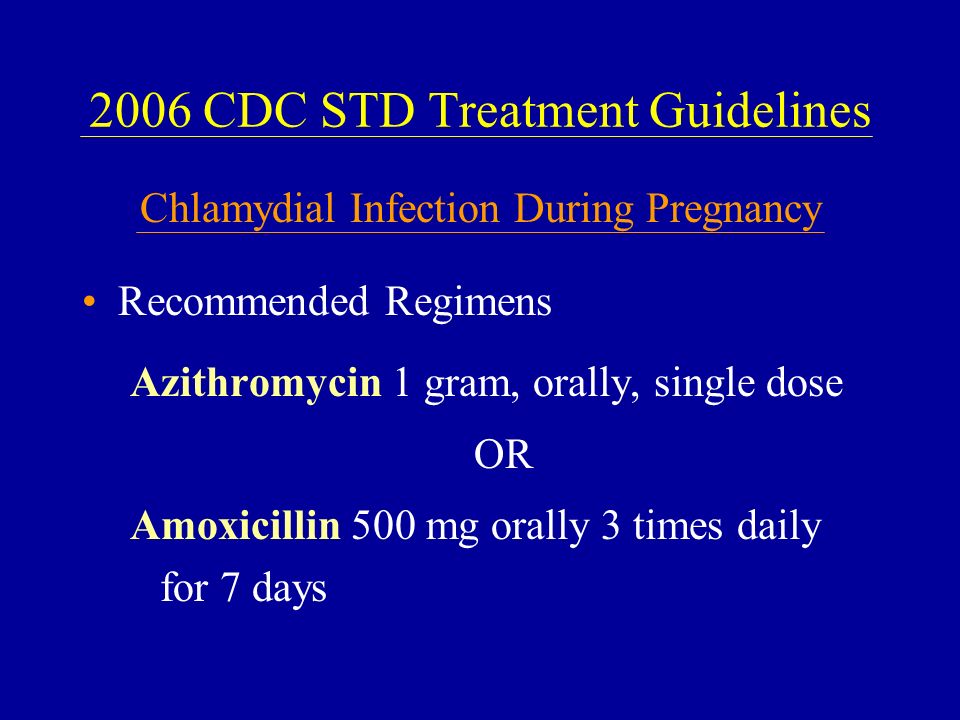
Mycoplasma (Mycoplasma genitalium), qualitative determination of DNA
- Code:
- 010102
- Deadline:
- 1 k.d.
Price: 374 r.
Ureaplasma (U.urealyticum / U.parvum), qualitative determination of DNA
- Code:
- 010107
- Deadline:
- 1 k.d.
Price: 380 r.
Gardnerella (Gardnerella vaginalis), qualitative determination of DNA
- Code:
- 010201
- Deadline:
- 1 k.d.
Price: 374 r.