Does early pregnancy cause migraines
Causes, Treatments, When to Worry
Migraine and Pregnancy: Causes, Treatments, When to Worry- Health Conditions
- Featured
- Breast Cancer
- IBD
- Migraine
- Multiple Sclerosis (MS)
- Rheumatoid Arthritis
- Type 2 Diabetes
- Articles
- Acid Reflux
- ADHD
- Allergies
- Alzheimer's & Dementia
- Bipolar Disorder
- Cancer
- Crohn's Disease
- Chronic Pain
- Cold & Flu
- COPD
- Depression
- Fibromyalgia
- Heart Disease
- High Cholesterol
- HIV
- Hypertension
- IPF
- Osteoarthritis
- Psoriasis
- Skin Disorders and Care
- STDs
- Featured
- Discover
- Wellness Topics
- Nutrition
- Fitness
- Skin Care
- Sexual Health
- Women's Health
- Mental Well-Being
- Sleep
- Product Reviews
- Vitamins & Supplements
- Sleep
- Mental Health
- Nutrition
- At-Home Testing
- CBD
- Men’s Health
- Original Series
- Fresh Food Fast
- Diagnosis Diaries
- You’re Not Alone
- Present Tense
- Video Series
- Youth in Focus
- Healthy Harvest
- No More Silence
- Future of Health
- Wellness Topics
- Plan
- Health Challenges
- Mindful Eating
- Sugar Savvy
- Move Your Body
- Gut Health
- Mood Foods
- Align Your Spine
- Find Care
- Primary Care
- Mental Health
- OB-GYN
- Dermatologists
- Neurologists
- Cardiologists
- Orthopedists
- Lifestyle Quizzes
- Weight Management
- Am I Depressed? A Quiz for Teens
- Are You a Workaholic?
- How Well Do You Sleep?
- Tools & Resources
- Health News
- Find a Diet
- Find Healthy Snacks
- Drugs A-Z
- Health A-Z
- Health Challenges
- Connect
- Breast Cancer
- Inflammatory Bowel Disease
- Psoriatic Arthritis
- Migraine
- Multiple Sclerosis
- Psoriasis
Medically reviewed by Debra Rose Wilson, Ph. D., MSN, R.N., IBCLC, AHN-BC, CHT — By Donna Christiano on May 6, 2020
We’re gonna give it to you straight: Pregnancy can mess with your head. And we’re not just talking about brain fog and forgetfulness. We’re also talking about headaches — migraine attacks, in particular.
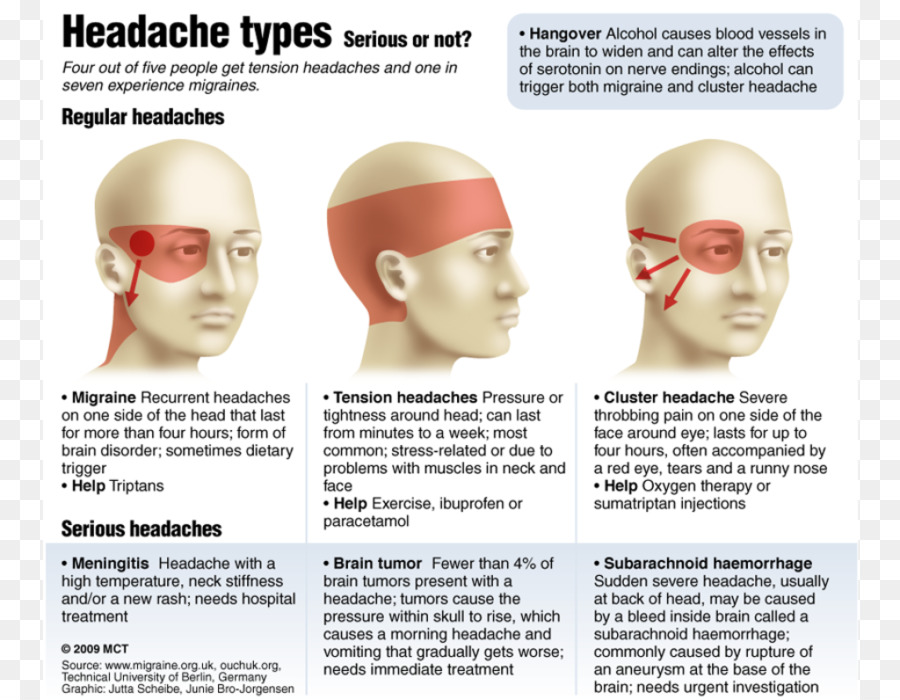
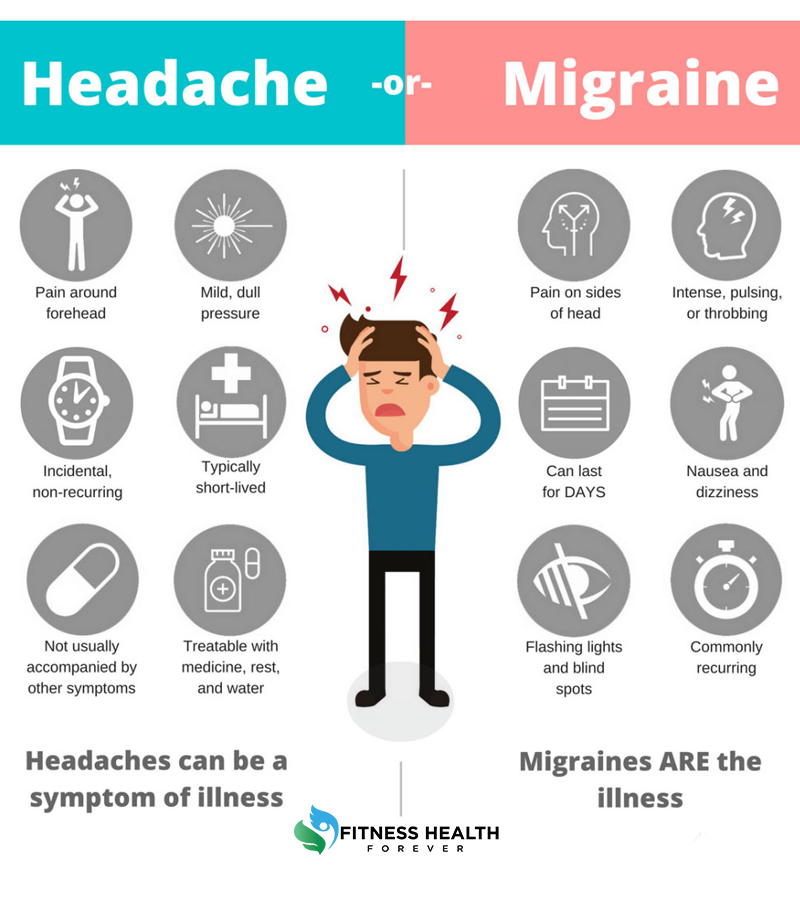
Migraine is a type of headache that can cause intense throbbing, usually on one side of the head. Imagine having a 3-year-old living behind your eye socket and relentlessly pounding a drum. Each beat sends waves of agony through your skull. The pain can make natural childbirth seem like a walk in the park.
Well, almost. Maybe we shouldn’t go that far — but migraine attacks can be very painful.
Migraine affects about 30 million Americans, 75 percent of whom are women. While many women (up to 80 percent) find that their migraine attacks improve with pregnancy, others struggle on.
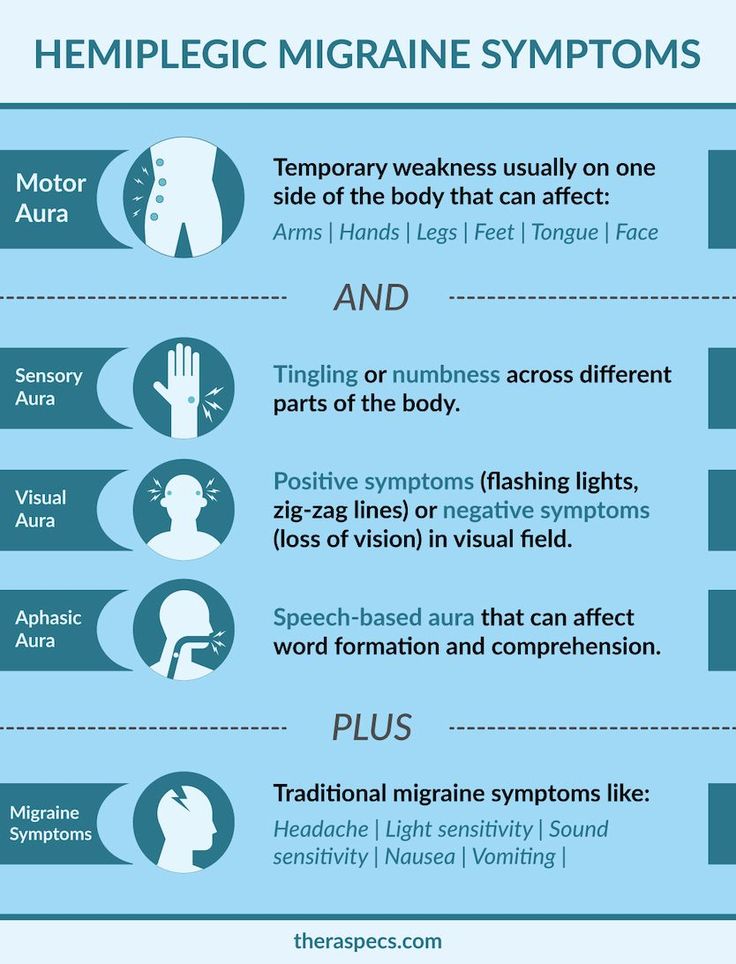
In fact, about 15 to 20 percent of pregnant women experience migraine. Women who have migraine attacks with “aura” — a neurological event that accompanies or proceeds migraine and can manifest as flashing lights, wavy lines, vision loss, and tingling or numbness — generally don’t see their headaches improve during pregnancy, according to experts.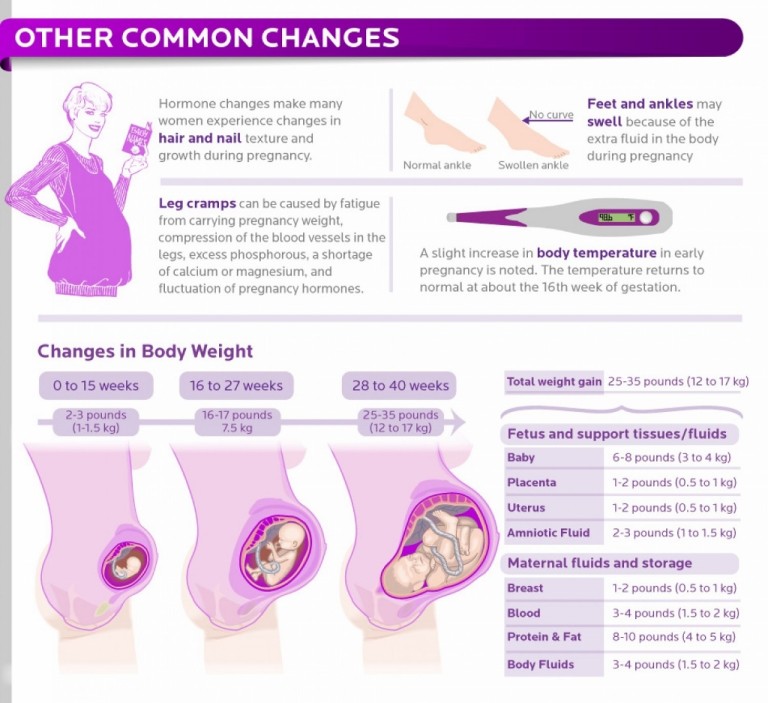
So what’s a mom-to-be to do when a migraine attack strikes? What’s safe to take and what’s not? Is migraine ever dangerous enough that you should seek emergency medical care?
Most headaches during pregnancy — including migraine — are nothing to worry about. But that’s not to say that migraine attacks aren’t incredibly annoying, and, in some cases, dangerous for pregnant women and their babies.
Here’s everything you need to know about migraine during pregnancy so you can tackle the pain — head on.
Migraine headaches seem to have a genetic component, which means they tend to run in families. That said, there’s usually a triggering event that unleashes them. One of the most common triggers — at least for women — is fluctuating hormone levels, particularly the rise and fall of estrogen.
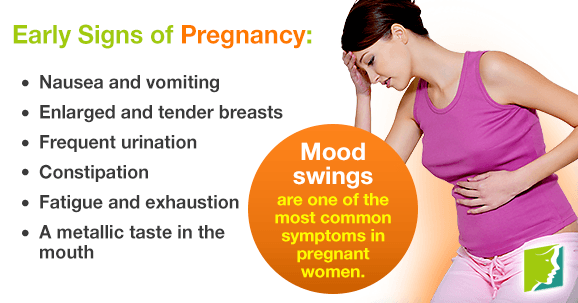
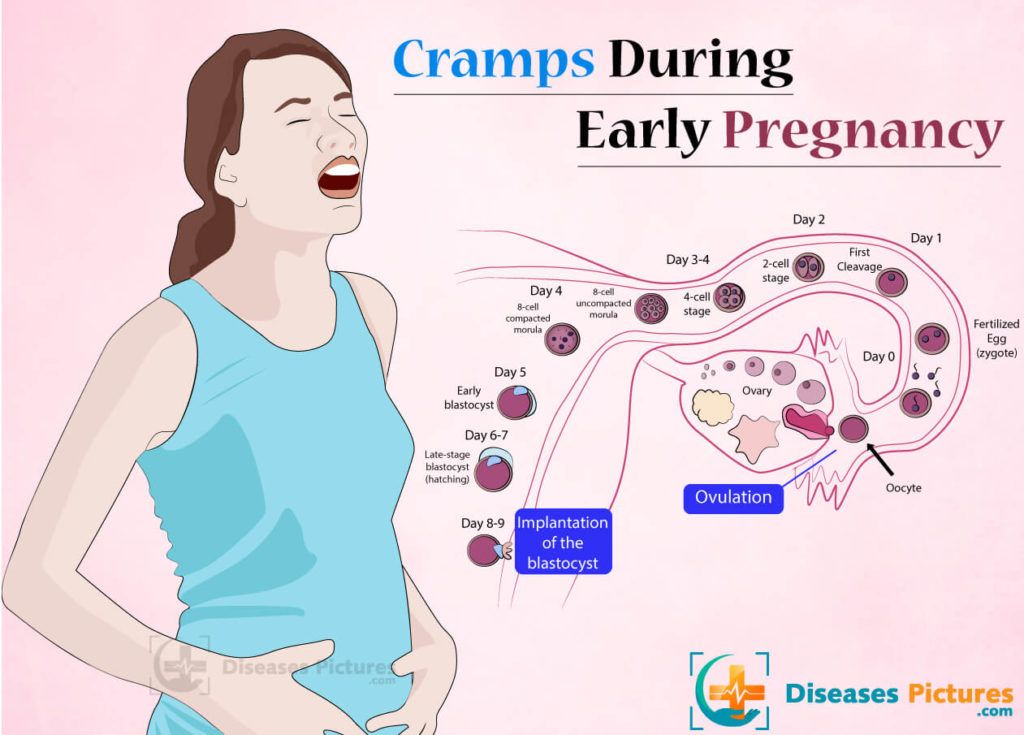
Moms-to-be who get migraine attacks tend to experience them most often in the first trimester of pregnancy, when hormone levels, including estrogen, haven’t yet stabilized. (In fact, headaches in general are an early pregnancy sign for a lot of women. )
)
An increase in blood volume, which is also common in the first trimester, can be an additional factor. As blood vessels in the brain expand to accommodate extra blood flow, they can press against sensitive nerve endings, causing pain.
Other common migraine triggers, whether you’re pregnant or not, include:
- Not getting enough sleep. The American Academy of Family Physicians recommends 8–10 hours per night when you’re pregnant. Sorry, Jimmy Fallon — we’ll catch you on the flip side.
- Stress.
- Not staying hydrated. According to the American Migraine Foundation, one-third of those who get migraine headaches say dehydration is a trigger. Pregnant women should aim for 10 cups (or 2.4 liters) of fluid daily. Try to drink them earlier in the day so sleep isn’t interrupted by nighttime visits to the bathroom.
- Certain foods. These include chocolate, aged cheeses, wines (not that you should be drinking any of those), and foods containing monosodium glutamate (MSG).

- Exposure to bright, intense light. Light-related triggers include sunlight and florescent lighting.
- Exposure to strong smells. Examples include paints, perfumes, and your toddler’s explosive diaper.
- Weather changes.
A migraine attack while you’re pregnant will look a lot like a migraine attack when you’re not pregnant. You’re apt to experience:
- throbbing head pain; usually it’s one-sided — behind one eye, for example — but it can occur all over
- nausea
- sensitivity to light, smells, sounds, and movement
- vomiting
When you’re pregnant, you have to think twice about everything you put into your body. Is it OK to have that second cup of coffee? What about a nibble of Brie? When you’re hit with the mother of all headaches — migraine — you want real relief quickly. But what are your options?
At-home remedies
These should be your first line of defense to avoid and treat migraine:
- Know your triggers.
 Stay hydrated, get your sleep, eat at regular intervals, and steer clear of any foods you know bring on a migraine attack.
Stay hydrated, get your sleep, eat at regular intervals, and steer clear of any foods you know bring on a migraine attack. - Hot/cold compresses. Figure out what eases migraine pain for you. A cold pack (wrapped in a towel) placed over your head can numb the pain; a heating pad around your neck can ease tension in tight muscles.
- Stay in the dark. If you have the luxury, retreat to a dark, quiet room when a migraine attack hits. Light and noise can make your headache worse.
Medications
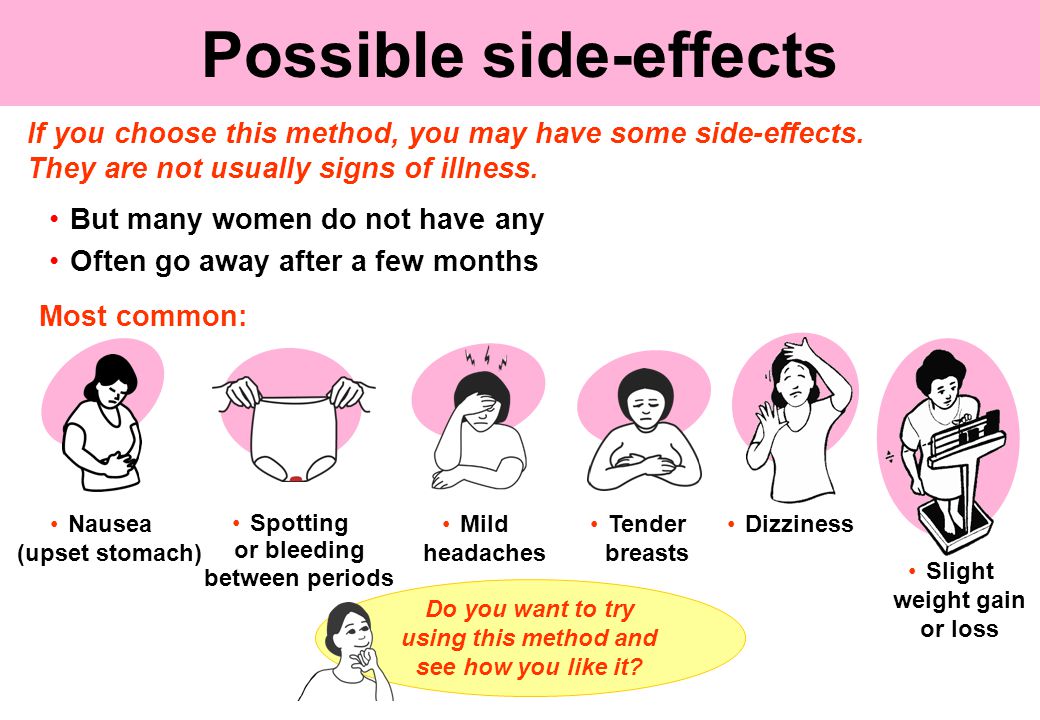
If you’re like a lot of pregnant women, you may loathe the idea of taking medication. Nevertheless, migraine attacks can be intense, and sometimes the only thing that’ll snuff out the pain is medication.
Safe to take
According to the American Academy of Family Physicians (AAFP), drugs safe to use for migraine in pregnancy are:
- Acetaminophen. This is the generic name of the drug in Tylenol.
 It’s also sold under many other brand names.
It’s also sold under many other brand names. - Metoclopramide. This drug is often used to increase the speed of stomach emptying but also sometimes prescribed for migraine, especially when nausea is a side effect.
Possibly safe to take under certain circumstances
- Non-steroidal anti-inflammatory drugs (NSAIDS). These include ibuprofen (Advil) and naproxen (Aleve) and are only OK in the second trimester of pregnancy. Earlier than that there’s an increased chance of miscarriage; later than that there can be complications like bleeding.
- Triptans. These include Imitrex and Amerge. While their use during pregnancy is somewhat controversial — there’s not a lot of well-performed research proving their safety — many doctors think the benefits of their use outweigh any risks.
No-gos
- Full-dose aspirin. If you’re to kick it old school and pop some aspirin, don’t.
 Its use during pregnancy has been linked to many problems, including miscarriage and bleeding in you and your baby. Ask your doctor before taking combination drugs like Excedrin Migraine.
Its use during pregnancy has been linked to many problems, including miscarriage and bleeding in you and your baby. Ask your doctor before taking combination drugs like Excedrin Migraine. - Opioids. According to the Centers for Disease Control and Prevention (CDC), opioid use during pregnancy can lead to preterm birth, stillbirth, and certain birth defects. If an opioid is prescribed, it should be for limited use and carefully monitored by your doctor.
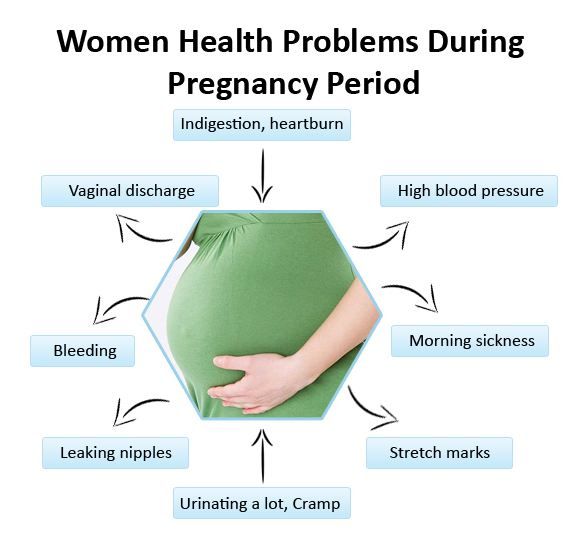
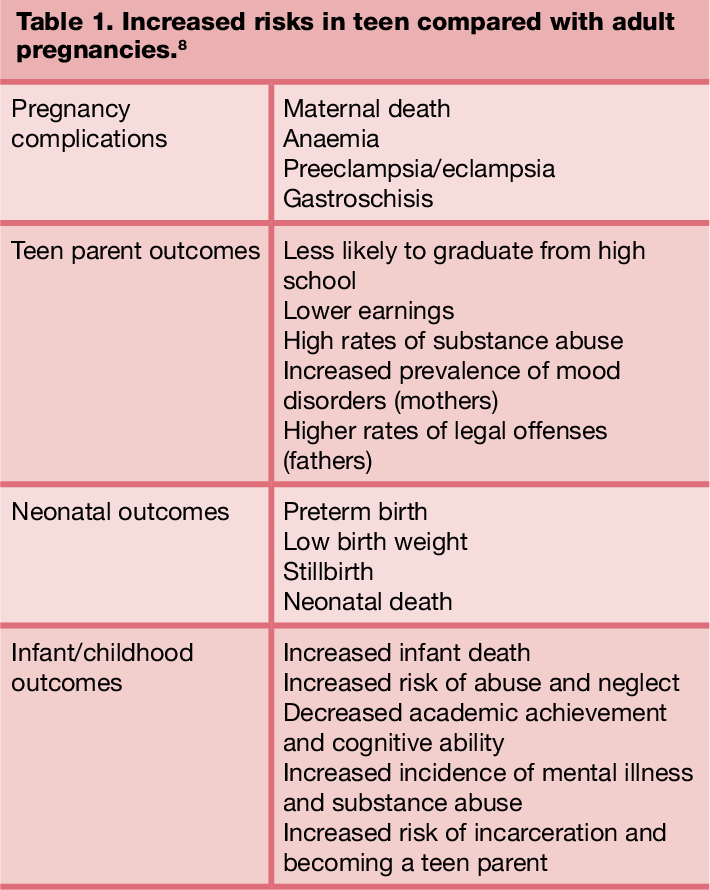
According to a 2019 study, pregnant women with migraine attacks have an increased risk of certain complications, including:
- having high blood pressure while pregnant, which may progress to preeclampsia
- delivering a low birth weight baby
- having a cesarean delivery
Older research shows that pregnant women with migraine have a higher risk of stroke. But — take a deep breath — experts say that the risk is still very low.
That’s the bad news — and it’s important to keep it in perspective.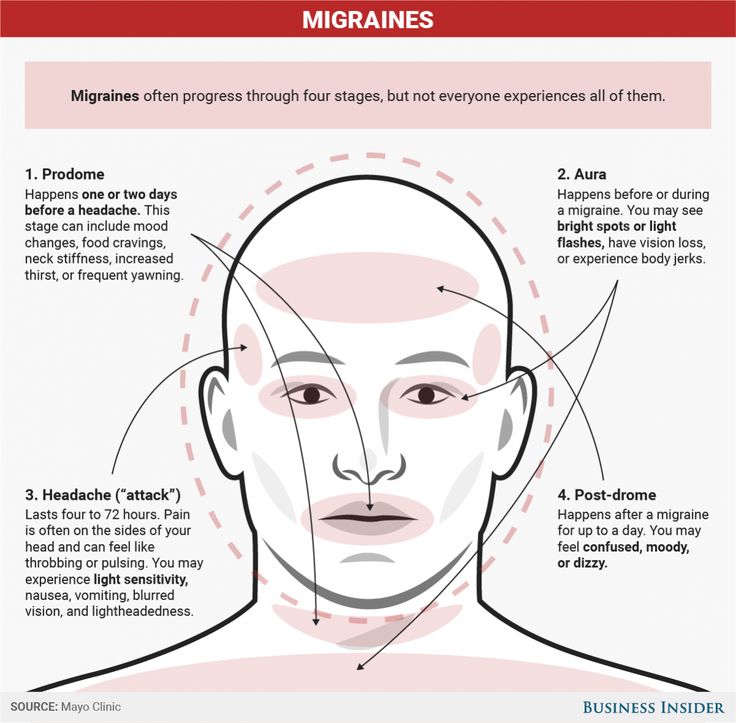 The fact of the matter is, most women with migraine headaches will sail through their pregnancies just fine. You can head off (pun intended) very serious problems when you know what to watch out for. Get immediate medical attention if:
The fact of the matter is, most women with migraine headaches will sail through their pregnancies just fine. You can head off (pun intended) very serious problems when you know what to watch out for. Get immediate medical attention if:
- you have a first-time headache during pregnancy
- you have a severe headache
- you have high blood pressure and a headache
- you have a headache that won’t go away
- you have a headache accompanied by changes in your vision, such as blurry vision or sensitivity to light
Thanks to a more constant supply of hormones, most women get a break from migraine attacks during pregnancy. For an unlucky few, though, their migraine struggles continue. If you’re one of them, you’ll be more limited in what you can take and when you can take it, but treatment options are available.
Make a migraine management plan with your doctor early on in your pregnancy (and ideally, before), so you have tools at the ready.
Last medically reviewed on May 6, 2020
- Parenthood
- Pregnancy
How we reviewed this article:
Healthline has strict sourcing guidelines and relies on peer-reviewed studies, academic research institutions, and medical associations. We avoid using tertiary references. You can learn more about how we ensure our content is accurate and current by reading our editorial policy.
We avoid using tertiary references. You can learn more about how we ensure our content is accurate and current by reading our editorial policy.
- About opioid use during pregnancy. (2020).
cdc.gov/pregnancy/opioids/basics.html - Bushnell CD, et al. (2009). Migraines during pregnancy linked to stroke and vascular diseases: US population based case-control study. DOI:
10.1136/bmj.b664 - Experts comment on research suggesting links between migraine and stroke risk in pregnancy, as published in the BMJ. (2009).
sciencemediacentre.org/experts-comment-on-research-suggesting-links-between-migraine-and-stroke-risk-in-pregnancy-as-published-in-the-bmj-2/ - Mayans L, et al. (2018). Acute migraine headache: Treatment strategies.
aafp.org/afp/2018/0215/p243.html#sec-6 - Mayo Clinic Staff. (2017). Nutrition and healthy eating.
mayoclinic.org/healthy-lifestyle/nutrition-and-healthy-eating/in-depth/water/art-20044256 - Migraine.
 (2019).
(2019).
womenshealth.gov/a-z-topics/migraine - Migraine and pregnancy: What moms-to-be need to know. (2017).
americanmigrainefoundation.org/resource-library/understanding-migrainemigraine-and-pregnancy-what-moms-to-be-need-to-know/ - Migraine headaches during pregnancy. (n.d.).
stanfordchildrens.org/en/topic/default?id=migraine-headache-90-P02476 - Migraine headaches during pregnancy. (n.d.).
chop.edu/conditions-diseases/migraine-headaches-during-pregnancy - Pregnancy and breastfeeding: Key issues for women who have migraine and become pregnant. (n.d.).
migrainetrust.org/living-with-migraine/coping-managing/pregnancy-breastfeeding/ - Skajaa N, et al. (2019). Pregnancy, birth, neonatal, and postnatal neurological outcomes after pregnancy with migraine. DOI:
10.1111/head.13536 - Sleep and pregnancy. (2017).
familydoctor.org/getting-enough-sleep-pregnancy/ - Top 10 migraine triggers and how to deal with them.
 (2017).
(2017).
americanmigrainefoundation.org/resource-library/top-10-migraine-triggers-and-how-to-deal-with-them/
Our experts continually monitor the health and wellness space, and we update our articles when new information becomes available.
Current Version
May 6, 2020
Written By
Donna Christiano
Edited By
Jessica Jondle
Medically Reviewed By
Debra Rose Wilson, PhD, MSN, RN, IBCLC, AHN-BC, CHT
Copy Edited By
Christina Guzik, BA, MBA
Share this article
Medically reviewed by Debra Rose Wilson, Ph.D., MSN, R.N., IBCLC, AHN-BC, CHT — By Donna Christiano on May 6, 2020
related stories
5 Tips for Managing Pregnancy Challenges with Migraine
How Improving Sleep Can Prevent Migraine Attacks
Headache During Pregnancy: What You Need to Know
7 Tips for Making Yourself as Comfortable as Possible During a Migraine Attack
How Symptom Tracking Can Help You Find Relief from Migraine
Read this next
5 Tips for Managing Pregnancy Challenges with Migraine
Medically reviewed by Carolyn Kay, M.
 D.
D.Managing migraine throughout pregnancy can be a challenge, but there are options that can help limit attacks.
READ MORE
How Improving Sleep Can Prevent Migraine Attacks
Medically reviewed by Seunggu Han, M.D.
A lack of rest can trigger migraine attacks. Here are eight ways you can improve the quality of your sleep for migraine relief.
READ MORE
Headache During Pregnancy: What You Need to Know
Medically reviewed by Deborah Weatherspoon, Ph.D., MSN
Headache during pregnancy can be a painful problem. Your doctor can help determine what is causing your headaches and the most effective and safe…
READ MORE
7 Tips for Making Yourself as Comfortable as Possible During a Migraine Attack
Medically reviewed by Deena Kuruvilla, MD
During a migraine attack, sometimes the only thing you can do is make yourself as comfortable as possible while you ride out the neurological storm.
READ MORE
How Symptom Tracking Can Help You Find Relief from Migraine
Medically reviewed by Deena Kuruvilla, MD
Symptom tracking can be a helpful tool to better understand and manage your migraine pain.
READ MORE
Pregnancy Friendly Recipe: Creamy White Chicken Chili with Greek Yogurt
This pregnancy-friendly spin on traditional chili is packed with the nutrients your body needs when you're expecting.
READ MORE
What You Should Know About Consuming Turmeric During Pregnancy
Consuming turmeric in pregnancy is a debated subject. We'll tell you if it's safe.
READ MORE
Pregnancy-Friendly Recipe: Herby Gruyère Frittata with Asparagus and Sweet Potatoes
Medically reviewed by Kathy W.
 Warwick, R.D., CDE
Warwick, R.D., CDESo easy and delicious. This frittata is high in protein and rich in essential nutrients your body needs to support a growing baby. Bonus: You can…
READ MORE
The Best Stretch Mark Creams and Belly Oils for Pregnancy in 2023
Stretch marks are easier to prevent than erase. If you're seeking a preventive, we've gathered a few of the best stretch mark creams for pregnancy.
READ MORE
Why Twins Don’t Have Identical Fingerprints
Medically reviewed by Alana Biggers, M.D., MPH
Identical twins are the same in so many ways, but does that include having the same fingerprints? There's conflicting information out there so we look…
READ MORE
Causes, Treatments, When to Worry
Migraine and Pregnancy: Causes, Treatments, When to Worry- Health Conditions
- Featured
- Breast Cancer
- IBD
- Migraine
- Multiple Sclerosis (MS)
- Rheumatoid Arthritis
- Type 2 Diabetes
- Articles
- Acid Reflux
- ADHD
- Allergies
- Alzheimer's & Dementia
- Bipolar Disorder
- Cancer
- Crohn's Disease
- Chronic Pain
- Cold & Flu
- COPD
- Depression
- Fibromyalgia
- Heart Disease
- High Cholesterol
- HIV
- Hypertension
- IPF
- Osteoarthritis
- Psoriasis
- Skin Disorders and Care
- STDs
- Featured
- Discover
- Wellness Topics
- Nutrition
- Fitness
- Skin Care
- Sexual Health
- Women's Health
- Mental Well-Being
- Sleep
- Product Reviews
- Vitamins & Supplements
- Sleep
- Mental Health
- Nutrition
- At-Home Testing
- CBD
- Men’s Health
- Original Series
- Fresh Food Fast
- Diagnosis Diaries
- You’re Not Alone
- Present Tense
- Video Series
- Youth in Focus
- Healthy Harvest
- No More Silence
- Future of Health
- Wellness Topics
- Plan
- Health Challenges
- Mindful Eating
- Sugar Savvy
- Move Your Body
- Gut Health
- Mood Foods
- Align Your Spine
- Find Care
- Primary Care
- Mental Health
- OB-GYN
- Dermatologists
- Neurologists
- Cardiologists
- Orthopedists
- Lifestyle Quizzes
- Weight Management
- Am I Depressed? A Quiz for Teens
- Are You a Workaholic?
- How Well Do You Sleep?
- Tools & Resources
- Health News
- Find a Diet
- Find Healthy Snacks
- Drugs A-Z
- Health A-Z
- Health Challenges
- Connect
- Breast Cancer
- Inflammatory Bowel Disease
- Psoriatic Arthritis
- Migraine
- Multiple Sclerosis
- Psoriasis
Medically reviewed by Debra Rose Wilson, Ph. D., MSN, R.N., IBCLC, AHN-BC, CHT — By Donna Christiano on May 6, 2020
D., MSN, R.N., IBCLC, AHN-BC, CHT — By Donna Christiano on May 6, 2020
We’re gonna give it to you straight: Pregnancy can mess with your head. And we’re not just talking about brain fog and forgetfulness. We’re also talking about headaches — migraine attacks, in particular.
Migraine is a type of headache that can cause intense throbbing, usually on one side of the head. Imagine having a 3-year-old living behind your eye socket and relentlessly pounding a drum. Each beat sends waves of agony through your skull. The pain can make natural childbirth seem like a walk in the park.
Well, almost. Maybe we shouldn’t go that far — but migraine attacks can be very painful.
Migraine affects about 30 million Americans, 75 percent of whom are women. While many women (up to 80 percent) find that their migraine attacks improve with pregnancy, others struggle on.
In fact, about 15 to 20 percent of pregnant women experience migraine. Women who have migraine attacks with “aura” — a neurological event that accompanies or proceeds migraine and can manifest as flashing lights, wavy lines, vision loss, and tingling or numbness — generally don’t see their headaches improve during pregnancy, according to experts.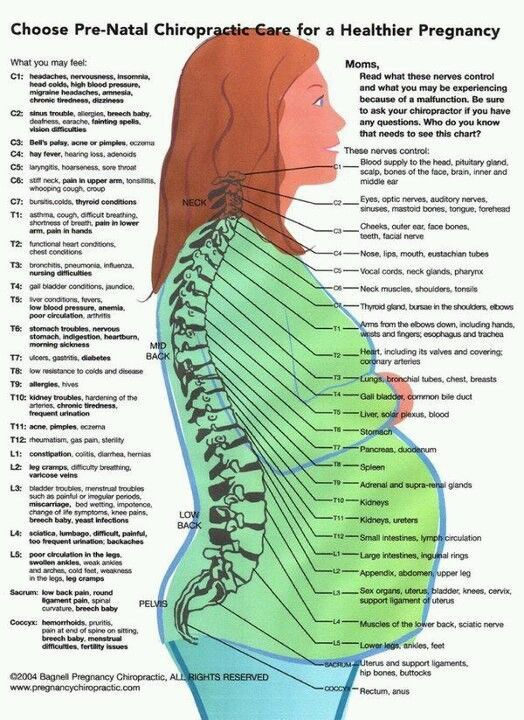
So what’s a mom-to-be to do when a migraine attack strikes? What’s safe to take and what’s not? Is migraine ever dangerous enough that you should seek emergency medical care?
Most headaches during pregnancy — including migraine — are nothing to worry about. But that’s not to say that migraine attacks aren’t incredibly annoying, and, in some cases, dangerous for pregnant women and their babies.
Here’s everything you need to know about migraine during pregnancy so you can tackle the pain — head on.
Migraine headaches seem to have a genetic component, which means they tend to run in families. That said, there’s usually a triggering event that unleashes them. One of the most common triggers — at least for women — is fluctuating hormone levels, particularly the rise and fall of estrogen.
Moms-to-be who get migraine attacks tend to experience them most often in the first trimester of pregnancy, when hormone levels, including estrogen, haven’t yet stabilized. (In fact, headaches in general are an early pregnancy sign for a lot of women.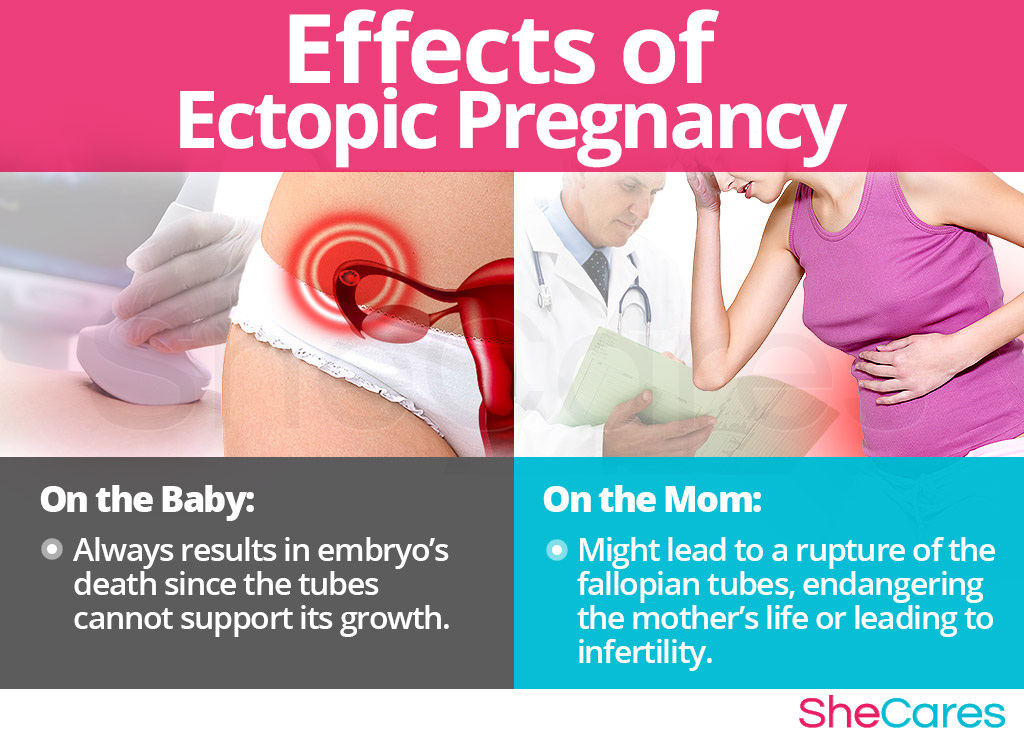 )
)
An increase in blood volume, which is also common in the first trimester, can be an additional factor. As blood vessels in the brain expand to accommodate extra blood flow, they can press against sensitive nerve endings, causing pain.
Other common migraine triggers, whether you’re pregnant or not, include:
- Not getting enough sleep. The American Academy of Family Physicians recommends 8–10 hours per night when you’re pregnant. Sorry, Jimmy Fallon — we’ll catch you on the flip side.
- Stress.
- Not staying hydrated. According to the American Migraine Foundation, one-third of those who get migraine headaches say dehydration is a trigger. Pregnant women should aim for 10 cups (or 2.4 liters) of fluid daily. Try to drink them earlier in the day so sleep isn’t interrupted by nighttime visits to the bathroom.
- Certain foods. These include chocolate, aged cheeses, wines (not that you should be drinking any of those), and foods containing monosodium glutamate (MSG).

- Exposure to bright, intense light. Light-related triggers include sunlight and florescent lighting.
- Exposure to strong smells. Examples include paints, perfumes, and your toddler’s explosive diaper.
- Weather changes.
A migraine attack while you’re pregnant will look a lot like a migraine attack when you’re not pregnant. You’re apt to experience:
- throbbing head pain; usually it’s one-sided — behind one eye, for example — but it can occur all over
- nausea
- sensitivity to light, smells, sounds, and movement
- vomiting
When you’re pregnant, you have to think twice about everything you put into your body. Is it OK to have that second cup of coffee? What about a nibble of Brie? When you’re hit with the mother of all headaches — migraine — you want real relief quickly. But what are your options?
At-home remedies
These should be your first line of defense to avoid and treat migraine:
- Know your triggers.
 Stay hydrated, get your sleep, eat at regular intervals, and steer clear of any foods you know bring on a migraine attack.
Stay hydrated, get your sleep, eat at regular intervals, and steer clear of any foods you know bring on a migraine attack. - Hot/cold compresses. Figure out what eases migraine pain for you. A cold pack (wrapped in a towel) placed over your head can numb the pain; a heating pad around your neck can ease tension in tight muscles.
- Stay in the dark. If you have the luxury, retreat to a dark, quiet room when a migraine attack hits. Light and noise can make your headache worse.
Medications
If you’re like a lot of pregnant women, you may loathe the idea of taking medication. Nevertheless, migraine attacks can be intense, and sometimes the only thing that’ll snuff out the pain is medication.
Safe to take
According to the American Academy of Family Physicians (AAFP), drugs safe to use for migraine in pregnancy are:
- Acetaminophen. This is the generic name of the drug in Tylenol.
 It’s also sold under many other brand names.
It’s also sold under many other brand names. - Metoclopramide. This drug is often used to increase the speed of stomach emptying but also sometimes prescribed for migraine, especially when nausea is a side effect.
Possibly safe to take under certain circumstances
- Non-steroidal anti-inflammatory drugs (NSAIDS). These include ibuprofen (Advil) and naproxen (Aleve) and are only OK in the second trimester of pregnancy. Earlier than that there’s an increased chance of miscarriage; later than that there can be complications like bleeding.
- Triptans. These include Imitrex and Amerge. While their use during pregnancy is somewhat controversial — there’s not a lot of well-performed research proving their safety — many doctors think the benefits of their use outweigh any risks.
No-gos
- Full-dose aspirin. If you’re to kick it old school and pop some aspirin, don’t.
 Its use during pregnancy has been linked to many problems, including miscarriage and bleeding in you and your baby. Ask your doctor before taking combination drugs like Excedrin Migraine.
Its use during pregnancy has been linked to many problems, including miscarriage and bleeding in you and your baby. Ask your doctor before taking combination drugs like Excedrin Migraine. - Opioids. According to the Centers for Disease Control and Prevention (CDC), opioid use during pregnancy can lead to preterm birth, stillbirth, and certain birth defects. If an opioid is prescribed, it should be for limited use and carefully monitored by your doctor.
According to a 2019 study, pregnant women with migraine attacks have an increased risk of certain complications, including:
- having high blood pressure while pregnant, which may progress to preeclampsia
- delivering a low birth weight baby
- having a cesarean delivery
Older research shows that pregnant women with migraine have a higher risk of stroke. But — take a deep breath — experts say that the risk is still very low.
That’s the bad news — and it’s important to keep it in perspective. The fact of the matter is, most women with migraine headaches will sail through their pregnancies just fine. You can head off (pun intended) very serious problems when you know what to watch out for. Get immediate medical attention if:
The fact of the matter is, most women with migraine headaches will sail through their pregnancies just fine. You can head off (pun intended) very serious problems when you know what to watch out for. Get immediate medical attention if:
- you have a first-time headache during pregnancy
- you have a severe headache
- you have high blood pressure and a headache
- you have a headache that won’t go away
- you have a headache accompanied by changes in your vision, such as blurry vision or sensitivity to light
Thanks to a more constant supply of hormones, most women get a break from migraine attacks during pregnancy. For an unlucky few, though, their migraine struggles continue. If you’re one of them, you’ll be more limited in what you can take and when you can take it, but treatment options are available.
Make a migraine management plan with your doctor early on in your pregnancy (and ideally, before), so you have tools at the ready.
Last medically reviewed on May 6, 2020
- Parenthood
- Pregnancy
How we reviewed this article:
Healthline has strict sourcing guidelines and relies on peer-reviewed studies, academic research institutions, and medical associations.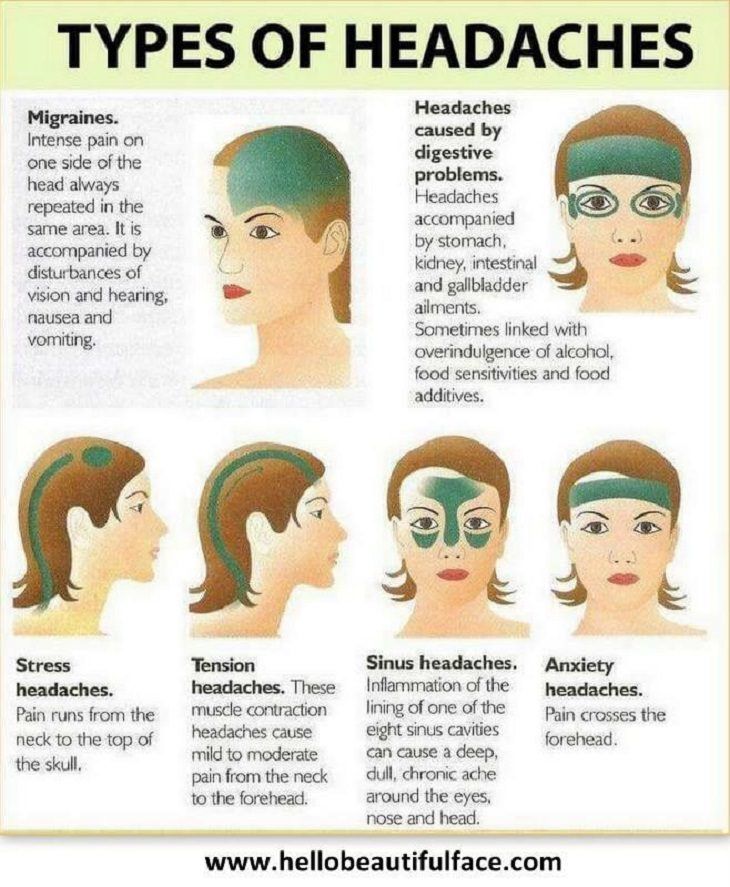 We avoid using tertiary references. You can learn more about how we ensure our content is accurate and current by reading our editorial policy.
We avoid using tertiary references. You can learn more about how we ensure our content is accurate and current by reading our editorial policy.
- About opioid use during pregnancy. (2020).
cdc.gov/pregnancy/opioids/basics.html - Bushnell CD, et al. (2009). Migraines during pregnancy linked to stroke and vascular diseases: US population based case-control study. DOI:
10.1136/bmj.b664 - Experts comment on research suggesting links between migraine and stroke risk in pregnancy, as published in the BMJ. (2009).
sciencemediacentre.org/experts-comment-on-research-suggesting-links-between-migraine-and-stroke-risk-in-pregnancy-as-published-in-the-bmj-2/ - Mayans L, et al. (2018). Acute migraine headache: Treatment strategies.
aafp.org/afp/2018/0215/p243.html#sec-6 - Mayo Clinic Staff. (2017). Nutrition and healthy eating.
mayoclinic.org/healthy-lifestyle/nutrition-and-healthy-eating/in-depth/water/art-20044256 - Migraine.
 (2019).
(2019).
womenshealth.gov/a-z-topics/migraine - Migraine and pregnancy: What moms-to-be need to know. (2017).
americanmigrainefoundation.org/resource-library/understanding-migrainemigraine-and-pregnancy-what-moms-to-be-need-to-know/ - Migraine headaches during pregnancy. (n.d.).
stanfordchildrens.org/en/topic/default?id=migraine-headache-90-P02476 - Migraine headaches during pregnancy. (n.d.).
chop.edu/conditions-diseases/migraine-headaches-during-pregnancy - Pregnancy and breastfeeding: Key issues for women who have migraine and become pregnant. (n.d.).
migrainetrust.org/living-with-migraine/coping-managing/pregnancy-breastfeeding/ - Skajaa N, et al. (2019). Pregnancy, birth, neonatal, and postnatal neurological outcomes after pregnancy with migraine. DOI:
10.1111/head.13536 - Sleep and pregnancy. (2017).
familydoctor.org/getting-enough-sleep-pregnancy/ - Top 10 migraine triggers and how to deal with them.
 (2017).
(2017).
americanmigrainefoundation.org/resource-library/top-10-migraine-triggers-and-how-to-deal-with-them/
Our experts continually monitor the health and wellness space, and we update our articles when new information becomes available.
Current Version
May 6, 2020
Written By
Donna Christiano
Edited By
Jessica Jondle
Medically Reviewed By
Debra Rose Wilson, PhD, MSN, RN, IBCLC, AHN-BC, CHT
Copy Edited By
Christina Guzik, BA, MBA
Share this article
Medically reviewed by Debra Rose Wilson, Ph.D., MSN, R.N., IBCLC, AHN-BC, CHT — By Donna Christiano on May 6, 2020
related stories
5 Tips for Managing Pregnancy Challenges with Migraine
How Improving Sleep Can Prevent Migraine Attacks
Headache During Pregnancy: What You Need to Know
7 Tips for Making Yourself as Comfortable as Possible During a Migraine Attack
How Symptom Tracking Can Help You Find Relief from Migraine
Read this next
5 Tips for Managing Pregnancy Challenges with Migraine
Medically reviewed by Carolyn Kay, M.
 D.
D.Managing migraine throughout pregnancy can be a challenge, but there are options that can help limit attacks.
READ MORE
How Improving Sleep Can Prevent Migraine Attacks
Medically reviewed by Seunggu Han, M.D.
A lack of rest can trigger migraine attacks. Here are eight ways you can improve the quality of your sleep for migraine relief.
READ MORE
Headache During Pregnancy: What You Need to Know
Medically reviewed by Deborah Weatherspoon, Ph.D., MSN
Headache during pregnancy can be a painful problem. Your doctor can help determine what is causing your headaches and the most effective and safe…
READ MORE
7 Tips for Making Yourself as Comfortable as Possible During a Migraine Attack
Medically reviewed by Deena Kuruvilla, MD
During a migraine attack, sometimes the only thing you can do is make yourself as comfortable as possible while you ride out the neurological storm.
READ MORE
How Symptom Tracking Can Help You Find Relief from Migraine
Medically reviewed by Deena Kuruvilla, MD
Symptom tracking can be a helpful tool to better understand and manage your migraine pain.
READ MORE
Pregnancy Friendly Recipe: Creamy White Chicken Chili with Greek Yogurt
This pregnancy-friendly spin on traditional chili is packed with the nutrients your body needs when you're expecting.
READ MORE
What You Should Know About Consuming Turmeric During Pregnancy
Consuming turmeric in pregnancy is a debated subject. We'll tell you if it's safe.
READ MORE
Pregnancy-Friendly Recipe: Herby Gruyère Frittata with Asparagus and Sweet Potatoes
Medically reviewed by Kathy W.
 Warwick, R.D., CDE
Warwick, R.D., CDESo easy and delicious. This frittata is high in protein and rich in essential nutrients your body needs to support a growing baby. Bonus: You can…
READ MORE
The Best Stretch Mark Creams and Belly Oils for Pregnancy in 2023
Stretch marks are easier to prevent than erase. If you're seeking a preventive, we've gathered a few of the best stretch mark creams for pregnancy.
READ MORE
Why Twins Don’t Have Identical Fingerprints
Medically reviewed by Alana Biggers, M.D., MPH
Identical twins are the same in so many ways, but does that include having the same fingerprints? There's conflicting information out there so we look…
READ MORE
Migraine during pregnancy - Juno
Migraine during pregnancy - Junohome
Articles
Migraine during pregnancy
How to recognize an attack and deal with it properly - read on. We will tell you how dangerous migraines are and how to get rid of them safely during pregnancy.
We will tell you how dangerous migraines are and how to get rid of them safely during pregnancy.
Contents of the article
Features and manifestations of migraine during pregnancy
If a woman was worried about migraines before pregnancy, then during the bearing of a child, the attacks are more likely to stop, or become milder and rarer. Improvements come from the 2nd trimester and are due to the fact that fluctuations in estrogen levels stop. In the early stages, the likelihood of migraine is higher. In the 1st trimester, ailments often occur, including headaches. But it's not always a migraine.
Migraine symptoms in pregnant women are similar to those that occur in other people. Approximately the picture looks like this:
- Harbingers. They are not characteristic for everyone and may be absent. They occur 1-3 days before an attack, manifest as irritability, depression, or, conversely, a surge of activity.
- Headache.
 Very intense, more often covers the temporal or frontal region, has a pulsating, arching character. It can be localized in one half of the head, but sometimes it spreads to the entire head. The pain lasts from 2-3 hours to several days, it is difficult to remove.
Very intense, more often covers the temporal or frontal region, has a pulsating, arching character. It can be localized in one half of the head, but sometimes it spreads to the entire head. The pain lasts from 2-3 hours to several days, it is difficult to remove. - Aura. It also doesn't happen to everyone. The phenomenon accompanies headache and lasts 10-40 minutes. Patients note flashes of light, spots, flies before the eyes, sometimes numbness of the extremities worries. With an aura, it is almost impossible to do something around the house or work.
Even after the pain passes, the expectant mother experiences depression, fatigue, irritability. Unpleasant sensations continue for about a day.
Why do pregnant women get migraines
The exact cause of the disease has not been established. However, specialists involved in the management of pregnancy distinguish hormonal changes in the body and an increased load on the body during pregnancy among the provoking factors.
General risk factors:
- sudden change of weather - especially for weather-sensitive women;
- stress and depression have a bad effect on blood vessels and the nervous system;
- violation of the diet - long intervals between meals, overeating, abuse of citrus fruits, smoked products and chocolate;
- overwork - physical fatigue at home and at work, sleep disturbances;
- irritants - unpleasant odors, stuffiness, excessive light or noise;
- fluid deficiency - dehydration due to insufficient water intake;
- concomitant pathologies, for example, hypertension.
The condition of pregnant women is adversely affected by weight gain, hypothermia and overheating. This can also provoke migraine attacks, especially if they have happened before.
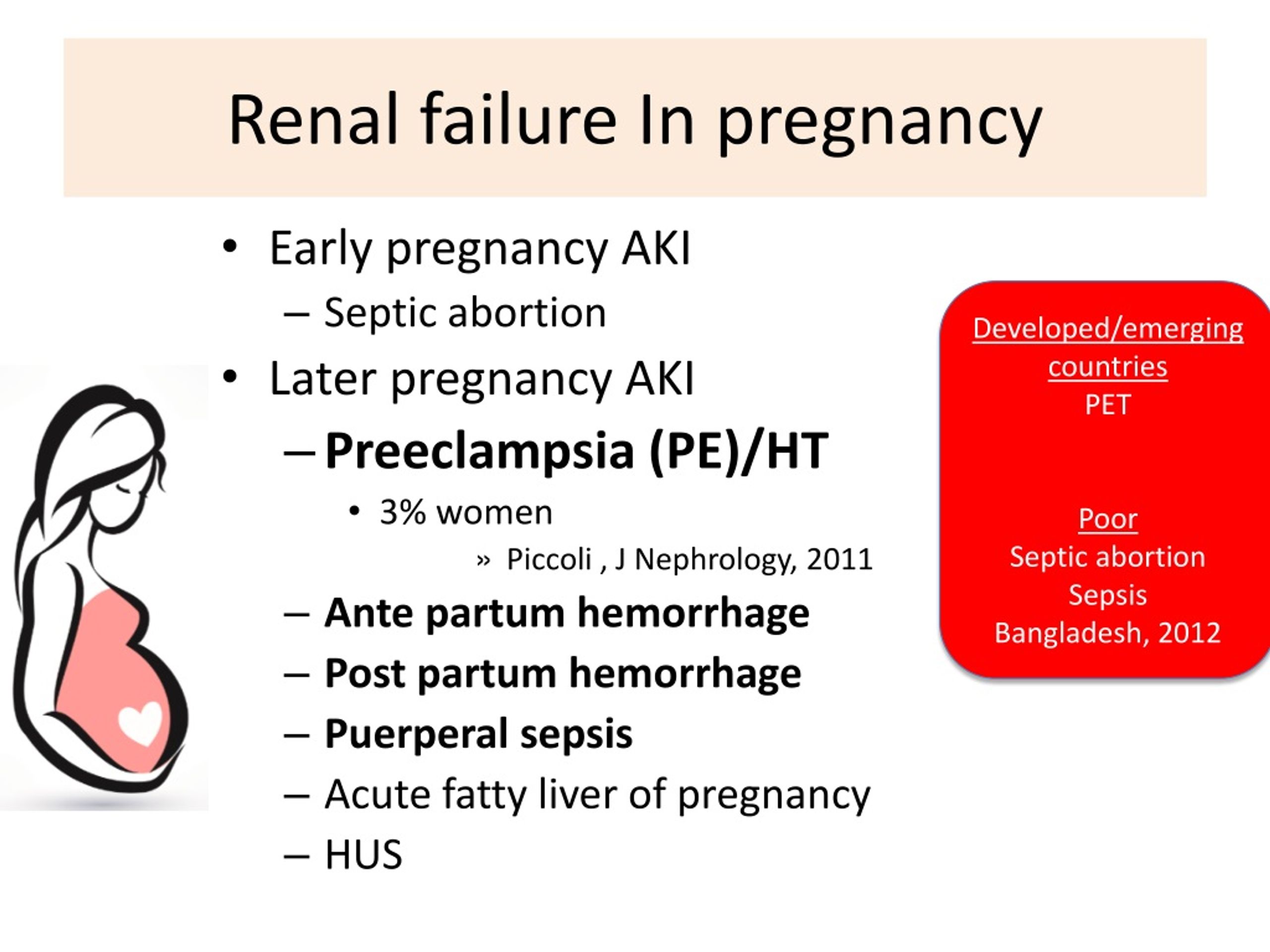
Are seizures dangerous for the fetus
By itself, migraine during pregnancy is not critical. If the seizures are not caused by more serious problems - hypertension, eclampsia, then a woman is highly likely to give birth to a healthy child at term. Migraine does not increase the risk of preterm birth or developmental anomalies in the fetus.
Migraine does not increase the risk of preterm birth or developmental anomalies in the fetus.
But despite the safety for the baby, migraines are debilitating for a pregnant woman. This affects general well-being - worsens sleep, nutrition, causes stress, decreased activity. Therefore, too frequent seizures can result in problems with the nervous system, fetal hypoxia. It is important to help yourself in time.
Treatment of migraine during pregnancy
Tablets should be taken only as a last resort. In the early stages, strong drugs are prohibited. First, try to cope with non-drug methods:
- Drink sweet tea or cola. Caffeine in small doses is harmless and can help relieve headaches.
- Take a walk in the fresh air, do simple exercises. This contributes to the outflow of blood from the vessels of the brain and the elimination of pain.
- Apply a warm or cool compress to the head. It can be a towel moistened with water or a heating pad.
- Take a cool shower (but not too cold). The procedure is useful as a prevention of varicose veins and migraines.
- Relax and sleep in a quiet, dark room.
- Do not hold back the urge to vomit - it can relieve an attack of pain.
- Rub essential oils of lemon, orange, lemon balm into whiskey - a little is enough. Too much oil can make headaches worse. If you have previously noticed such a reaction of your body to odors, you should not apply this method now.
- Drink freshly squeezed juice or clean water. Replenishing fluids often helps get rid of a migraine.
If the above measures do not help, and the seizures are disturbing enough, you need to consult a doctor. The specialist will prescribe treatment, for example, prescribe pills that will help to cope with pain. The safest drug is paracetamol. It can be taken on its own. The doctor may prescribe magnesium for treatment - it has a beneficial effect on blood vessels.
In some cases, ibuprofen and aspirin are acceptable (only in the 2nd trimester). Opioid analgesics and triptans are strictly prohibited. If a migraine is growing or has appeared for the first time, an aura has joined, pressure rises, you should definitely consult a doctor in the near future.
Opioid analgesics and triptans are strictly prohibited. If a migraine is growing or has appeared for the first time, an aura has joined, pressure rises, you should definitely consult a doctor in the near future.
Prophylaxis
Dealing with migraines during pregnancy is not always easy. It is better to follow some rules that will help reduce the risk of seizures:
- Keep a sleep and rest schedule.
- Control sweets and fatty foods.
- Try to walk every day, do light exercises.
- Massage or self-massage the head and collar area. Movements should be light: it is better if the specialist shows what they should be.
Even if an attack has already happened, try not to abruptly get involved in worries and affairs after it. Remember that you are responsible not only for yourself, but also for the child. Do not be shy to turn to your loved ones for help and do not be heroic. Be healthy!
Other articles
01/31/2023
Management of multiple pregnancies
Multiple pregnancy is not only a great joy in the family, but also implies maximum attention to the expectant mother and babies, as it carries an increased risk for everyone. We will tell you more in our article.
We will tell you more in our article.
01/05/2023
Ultrasound folliculometry: how and why is it performed?
Folliculometry is the observation of changes in a woman's genitals during the menstrual cycle using ultrasound. Such an examination is necessary to identify the causes of menstrual irregularities, to monitor the growth and formation of the egg in the case of diagnosis and treatment of infertility.
01/01/2023
Ultrasound of the pelvis: how to prepare correctly?
Ultrasound diagnostics is indispensable in modern medicine! This study is necessary to identify various nuances of women's health, as well as diagnose many diseases and identify pleasant moments in a woman's life - such as pregnancy, tracking the development of the baby in each trimester of pregnancy.
Making an appointment?
Making an appointment?
Request a call
Migraine during pregnancy: description of the disease, causes, symptoms, cost of treatment in Moscow
Migraine during pregnancy is a fairly common phenomenon that should not be ignored and treated. There are many reasons for the appearance of the problem during this period. After childbirth, the disease usually disappears completely. In the next pregnancy, there is a risk of recurrence of the violation, but it will not necessarily appear again. Since the pain negatively affects not only the condition of the woman, but also the child, it is necessary to take drugs to eliminate the attack, but only those that are allowed for pregnant women.
Migraine in pregnant women occurs not infrequently, since, in addition to hormonal changes in the body, there are also changes in the psycho-emotional state, which often also act as a trigger for the development of pathology.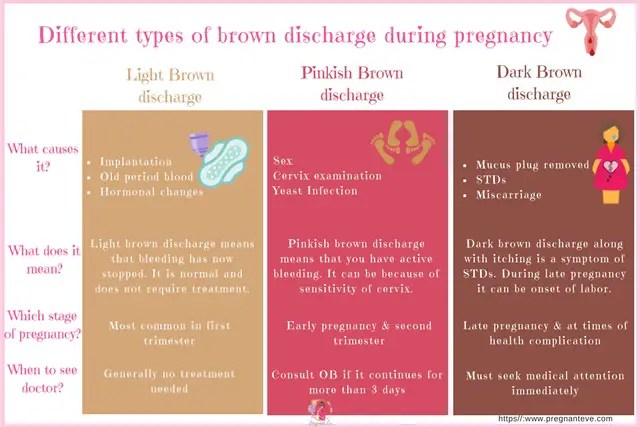 Depending on the duration of pregnancy, a woman's well-being may improve or worsen. The peak of migraines in most cases occurs in the first trimester of pregnancy, when a woman's body undergoes especially rapid hormonal changes. In the later stages, headaches may begin to disturb due to changes in the spine that appear against the background of a shift in the center of gravity.
Depending on the duration of pregnancy, a woman's well-being may improve or worsen. The peak of migraines in most cases occurs in the first trimester of pregnancy, when a woman's body undergoes especially rapid hormonal changes. In the later stages, headaches may begin to disturb due to changes in the spine that appear against the background of a shift in the center of gravity.
Reasons
Migraine attacks during pregnancy are usually triggered by specific factors. Migraines during early pregnancy can be caused by the following reasons:
-
specific stresses for the body, which are associated with the process of implantation of the egg and the beginning of the development of the embryo;
-
a sharp change in hormonal levels;
-
dehydration due to changes in metabolic processes in the body and a woman's lack of attention to herself;
-
emergence of food intolerance against the background of early toxicosis.

Also, a number of women in the first trimester of pregnancy often experience migraine-provoking nervous strain due to constant concern about their condition, the development of the child and the upcoming birth.
In the second trimester, a woman has a significant improvement in her condition. The frequency of seizures is reduced, and because of the ability to use more drugs, they become less painful. The main provocateurs of the appearance of headaches in this period are the following factors:
-
physical overload - it occurs if a woman does not reduce physical activity, continuing to lead the same lifestyle as before pregnancy. As a result, an attack occurs as a protest of the body against what is happening;
-
strong emotional experience;
-
abrupt weather changes - they affect a woman if she suffered from meteorological dependence before pregnancy;
-
inhalation of very sweet heavy odours.

In the third trimester of pregnancy, the intensity of migraine increases. Due to the ongoing changes in the spine, blood circulation begins to deteriorate to a large extent, due to which even a slight vascular spasm is enough for a migraine attack. The main reasons that can cause it are:
-
drinking a large amount of liquid at once - in order not to provoke an attack, you need to drink often, but little by little, thereby not causing a sharp influx of water into the blood;
-
staying in an uncomfortable position, which significantly worsens blood circulation in the lower extremities;
-
prolonged stay in the supine position, which also worsens blood circulation;
-
eating spicy or spicy foods;
-
great excitement or prolonged nervous tension.
For some time after childbirth, migraines may persist due to hormonal changes in the body. However, this phenomenon is not always the case and is considered the exception rather than the rule for migraine during pregnancy.
Is an aura possible
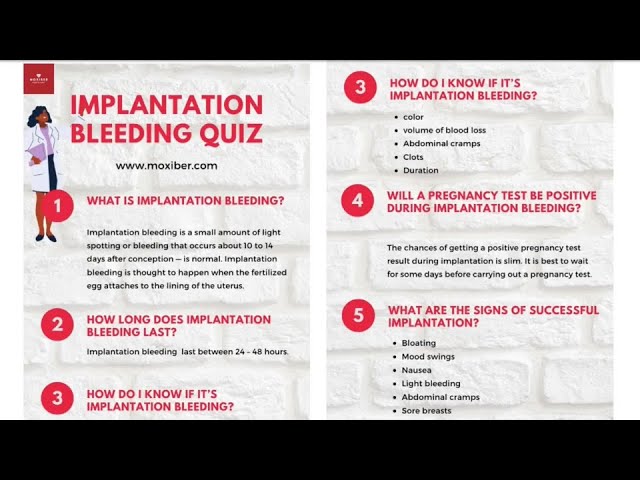
Migraine with aura occurs in pregnant women with the same frequency as the classical one. In a quarter of cases, a few minutes before an attack or a maximum of an hour before it, a woman develops previous neurological disorders. If they do not appear strongly, then the patient has time to take medications, thereby relieving an attack, or to return home. When the symptoms of the aura are strong, they can cause no less torment than the pain attack itself.
You can talk about the presence of an aura in a woman if any of the following symptoms are present before a migraine attack:
-
visual disturbances - with them, loss of visual fields, temporary loss of vision in one or both eyes, flickering flies before the eyes or flashes of light;
-
severe weakness - it can spread to the whole body, but more often it is felt only in the limbs of the side from which the head will hurt in the future. The opposite side of the body suffers much less often;
-
tingling in the limbs and upper half of the body, even affecting the tongue and lips;
-
goosebumps;
-
complete loss or significant reduction in the sensation of limbs;
-
various speech disorders such as confusion or slurring.

Quite often, in pregnant women with migraine with aura, such a phenomenon is noted that if during this period the effect of the negative factor is eliminated, a further attack does not develop, even if medications are not taken. Because of this, in such a situation, a woman needs to fix as accurately as possible what caused the deterioration.
Is an attack dangerous for the fetus
Today, thanks to numerous studies, doctors have been able to find out whether a migraine attack affects the fetus. The unborn child is able to feel the emotions of the mother and her pain, which is why there is a negative change in his condition at the time of the attack. Also, against the background of pain, a spasm of the vessels supplying the placenta often occurs. As a result, the fetus begins to receive significantly less oxygen, which causes hypoxia in it, which, with frequent repetitions of migraine attacks, can cause mental development disorders against the background of brain damage.
Medicines prescribed for pregnant women must be taken during an attack without fail. They will not harm the child, as they do not penetrate the placental barrier and effectively relieve pain, eliminating its negative impact. It is unacceptable to prescribe such funds on your own, since mistakes can be too dangerous for the fetus. All drugs are correctly selected taking into account the duration of pregnancy only by a doctor.
Prophylaxis
Preventive measures against migraine during pregnancy greatly help to reduce the risk of this problem. Additionally, it will help improve well-being and a proper lifestyle. The main preventive measures during pregnancy include:
-
full sleep at least 9 hours a day;
-
taking light sedatives when nervous tension appears;
-
providing a comfortable temperature in the room;
-
drinking frequently and in small amounts;
-
eating food that does not cause a burning sensation in the mouth.