Placenta on top of baby
Is Placenta on Top a Problem?
The placenta is normally expelled or removed from the body after delivery. This occurs during the third stage of labor in vaginal births. People who have a retained placenta (when the placenta is not delivered within 30 minutes after birth) may experience certain post-delivery complications like bleeding or infection.
The placenta develops wherever the fertilized egg embeds in your uterus. This leads to a range of possible locations:
- Anterior position (on the front wall of your uterus, closest to the belly)
- Posterior position (on the back wall of your uterus, closest to the spine)
- Fundal position (on the top wall of your uterus)
- Lateral position (on the right or left side of your uterus)
- Low-lying placenta (low in the uterus, near to or partially covering the internal cervical os)
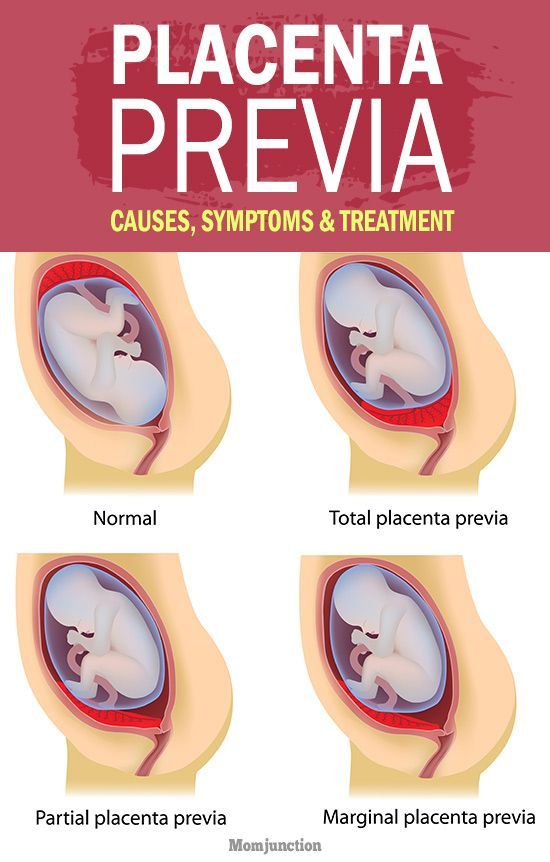
- Placenta previa (extending over the internal cervical os)
Take a quiz
Find out what you can do with our Health Assistant
Placental development stages
Since it can change over time, placenta positioning should be monitored throughout your pregnancy. It could move toward the upper region of the uterus as the uterus enlarges and the placenta’s attachment area stretches upward. During growth, the baby’s head starts to descend into the pelvis in preparation for labor and delivery. This movement adds pressure to the lower uterus, which causes its walls to stretch and become thinner. As a result, the placenta will usually ascend by the third trimester. In nine out of 10 cases, the placenta moves up by about 32 weeks of pregnancy.
What is a fundal placenta?
A fundal placenta appears in the fundus, or top region, of the uterus. Some people experience a combination of fundal-anterior or fundal-posterior positioning. Placental positioning is often checked between 18 and 21 weeks of pregnancy using an ultrasound.
Is it OK for the placenta to be on top?
Wherever the placenta grows, it can sufficiently nourish your baby throughout the pregnancy. As the pregnancy progresses, the placenta tends to migrate toward the upper region of the uterus.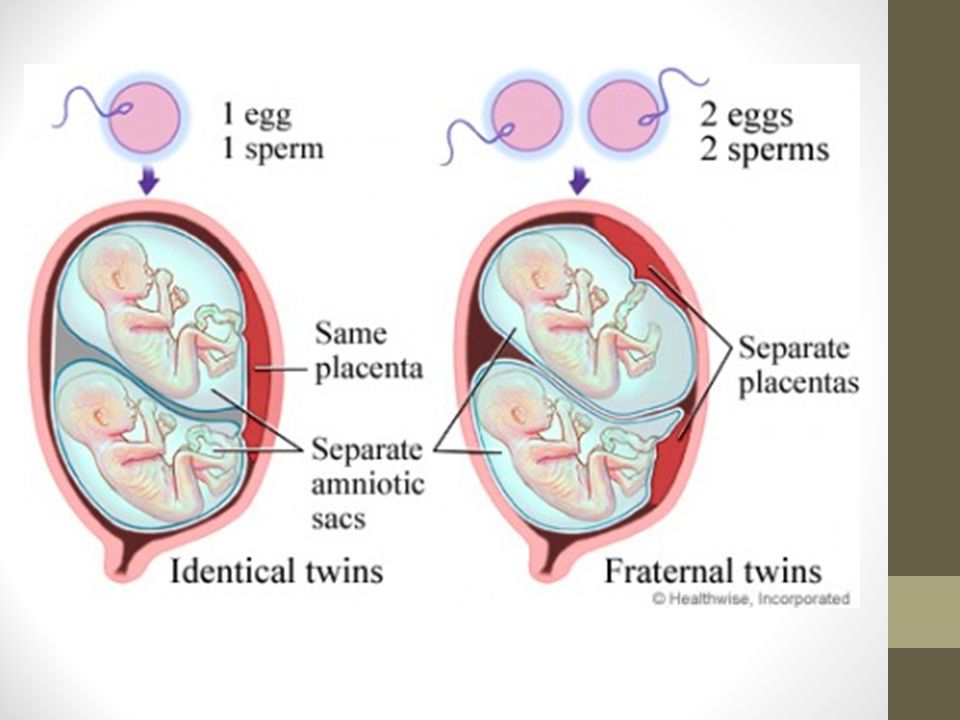 This is rarely a cause for concern unless it’s accompanied by other signs or symptoms.
This is rarely a cause for concern unless it’s accompanied by other signs or symptoms.
Fundal-anterior placenta
A fundal-anterior placenta is located mostly at the top of the uterus but also extends slightly toward the front (belly side).
Fundal-posterior placenta
A fundal-posterior placenta still appears mostly at the top of the uterus but extends slightly toward the back (spine side).
Fundal placenta complications
The most complex placental position is called placenta previa. In this condition, the cervix is covered during the third trimester of pregnancy. It can lead to severe bleeding and requires careful medical attention.
The main risk factors for placenta previa are:
- Previous placenta previa
- Previous cesarean delivery
- Multiple gestation
If the placenta covers the cervix during the third trimester, certain complications like bleeding can happen. According to researchers, placenta previa affects approximately four per 1000 births, but cases vary worldwide.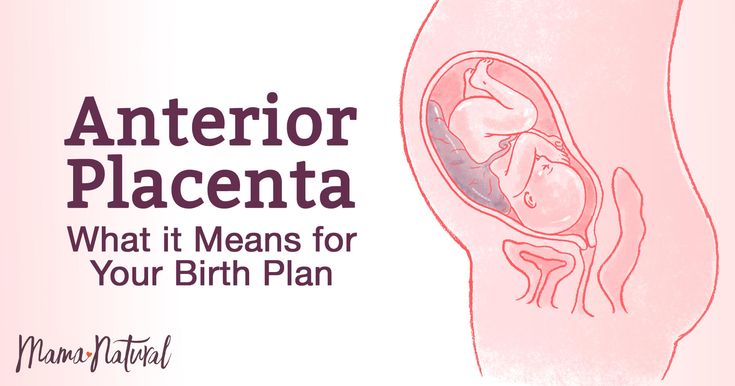
If the placenta is located anteriorly and the mother needs a cesarean section, the placenta may affect where the health care provider makes the incision.
Finally, if you’ve experienced an injury due to a fall or any other accident, it is important to undergo a physical examination. A health care provider can determine whether the health of your baby or placenta has been compromised. They may recommend extra monitoring of the position of your fetus and placenta, as well as your vital signs, to ensure a healthy pregnancy.
Anterior placenta | Tommy's
What is the placenta?
The placenta is an organ that helps your baby grow and develop. It’s attached to the lining of the womb and is connected to your baby by the umbilical cord. The placenta passes oxygen, nutrients and antibodies from your blood supply to your baby. It also carries waste products from your baby to your blood supply, so your body can get rid of them.
What is an anterior placenta?
The placenta develops in the first few weeks of pregnancy, wherever the fertilised egg embeds itself. This could be along the top, sides, front or back wall of the uterus. If the placenta attaches to the front, this is called an anterior placenta.
This could be along the top, sides, front or back wall of the uterus. If the placenta attaches to the front, this is called an anterior placenta.
People sometimes think that having an anterior placenta is linked to having a low-lying placenta but it is not. A low-lying placenta (also known as placenta praevia) is when the placenta attaches lower down and may cover a part of or all of the cervix (the entrance to the womb).
How will I know if I have an anterior placenta?
You’ll find out whether you have an anterior placenta during your second ultrasound scan when you are 18 to 21 weeks pregnant.
Can an anterior placenta cause complications?
This is very unlikely. The front wall of the uterus is a normal place for the placenta to implant and develop. An anterior placenta will still do its job of nourishing your baby, but there are some things to be aware of if you are diagnosed.
Feeling your baby’s movements
Most women usually feel their baby move between 18 and 24 weeks. If this is your first pregnancy, you may not notice your baby’s movements until you are more than 20 weeks pregnant.
If this is your first pregnancy, you may not notice your baby’s movements until you are more than 20 weeks pregnant.
Having an anterior placenta can make it a bit harder to feel your baby move because your baby is cushioned by the placenta lying at the front of your stomach. However, it’s very important that you never assume that having an anterior placenta is a reason why you can’t feel your baby move.
Get to know your baby’s movements and be aware of them throughout your pregnancy. Contact your midwife or maternity unit immediately if you think your baby’s movements have slowed down, stopped or changed. It’s always best to get checked.
Some women may feel particularly anxious about their baby’s movements, especially if they’ve had difficult experiences in previous pregnancies. Talk to your midwife about how you feel. They may be able to reassure you or help you get more help and support, if you need it.
Find out more about your baby's movements.
Lower back pain
You may have lower back pain if you have an anterior placenta.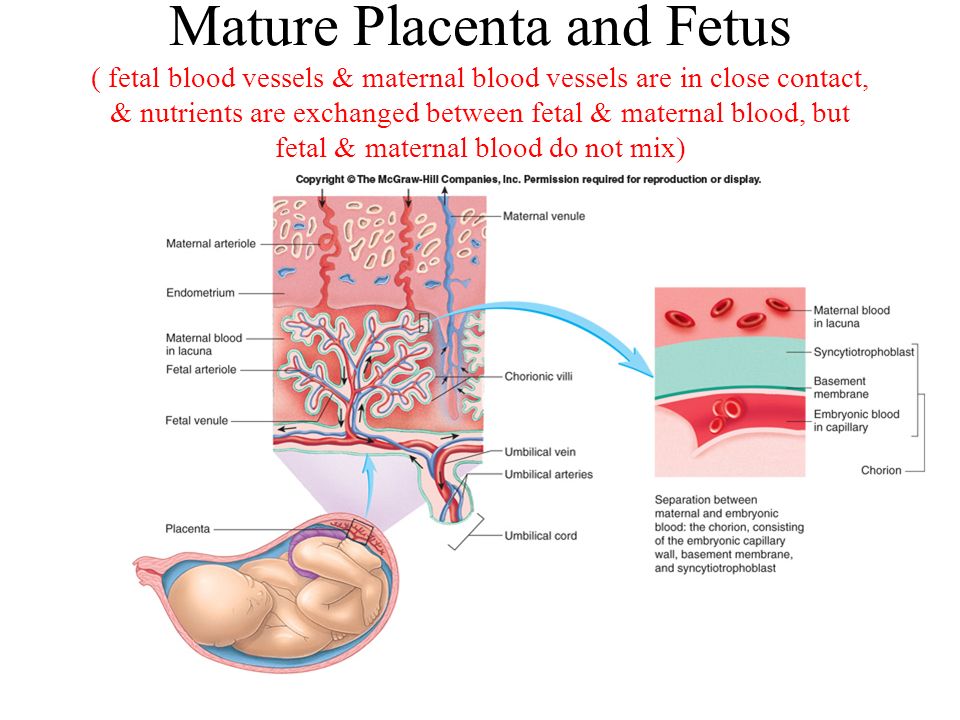 Irritable back pain can be common in pregnancy and there are things you can do to try to ease it.
Irritable back pain can be common in pregnancy and there are things you can do to try to ease it.
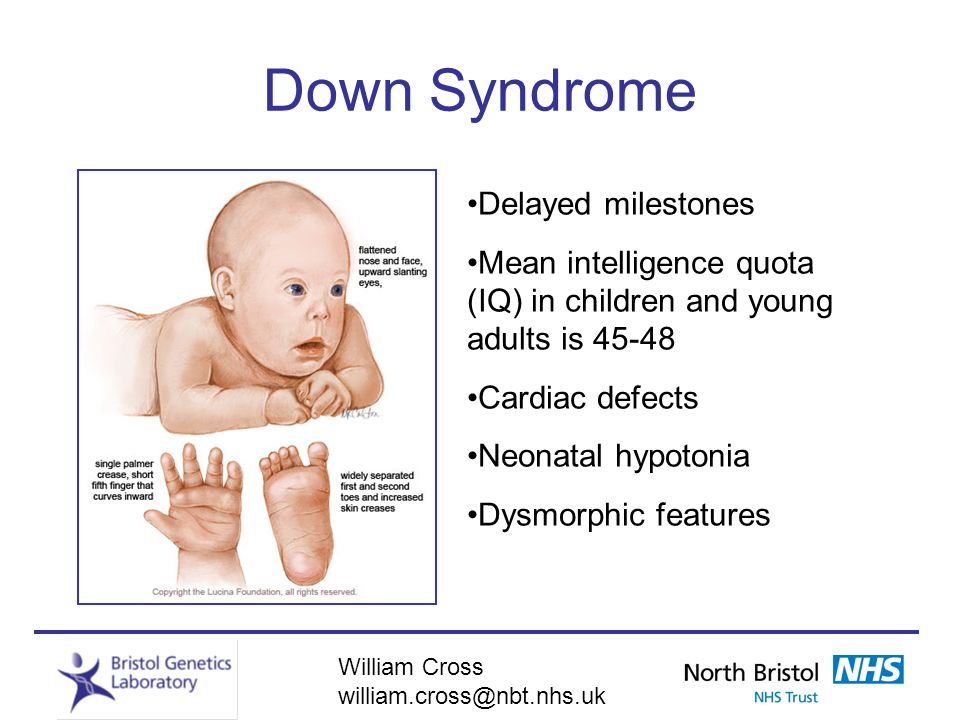
Screening and diagnostic tests
An anterior placenta can make it more difficult to perform certain tests, such as amniocentesis. Not all women are offered this test during pregnancy. You’ll only be offered this test if the results of your screening tests show that your baby has a high risk of certain conditions, such as Down’s syndrome.
The test involves inserting a long, thin needle through the stomach into the amniotic sac to remove a sample of cells so doctors can test for health conditions. Having an anterior placenta can make this more difficult, but doctors will use an ultrasound scanner to guide the needle and avoid the placenta. An ultrasound scanner is used to guide the needle, which significantly reduces the risk of injury.
There is a small risk of miscarriage after an amniocentesis test, regardless of where the placenta is. Having an anterior placenta does not increase this risk.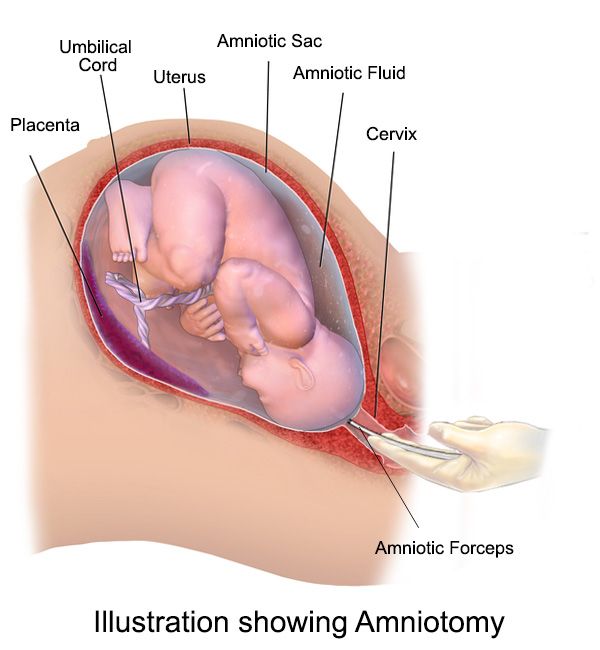
Your baby’s position in the womb
Having an anterior placenta increases the chances of the baby being in a back-to-back (occipitoposterior) position. This is when the baby’s head is down, but the back of their head and their back is against your spine.
If your baby is in a back-to-back position when you go into labour, it’s likely that your baby will turn into the best position for birth and you will have a normal vaginal delivery. But having a baby in a back-to-back position during labour does increase the chances of:
- a longer labour
- a more painful labour
- a caesarean section
- assisted birth.
Talk to your midwife or doctor if you have any concerns about having an anterior placenta.
Artificial Placenta to Increase Survival of Extremely Premature Babies
The device will place a premature newborn in an environment similar to that of a mother's womb connected to an artificial umbilical cord and reduce neurological consequences.
The BCNatal (Hospital Sant Joan de Deu - Barcelona Clinical Hospital) team presented a unique project in Europe to create artificial placenta . Its goal is to improve survival of extremely preterm newborns , minimize the severe neurological consequences that most of them suffer from, and improve their quality of life and that of their families.
Despite the fact that more than 90% of pregnancies reach a normal term of delivery, intrauterine life continues to be one of the phases of greatest risk to humans. One of the main problems that has yet to be addressed is extreme prematurity (six months or less), which affects 9 children every year.0005 25,000 families in Europe only.
"Despite great advances in medicine , recent important studies in Sweden and the USA show that no clear improvement has been achieved in the last twenty years.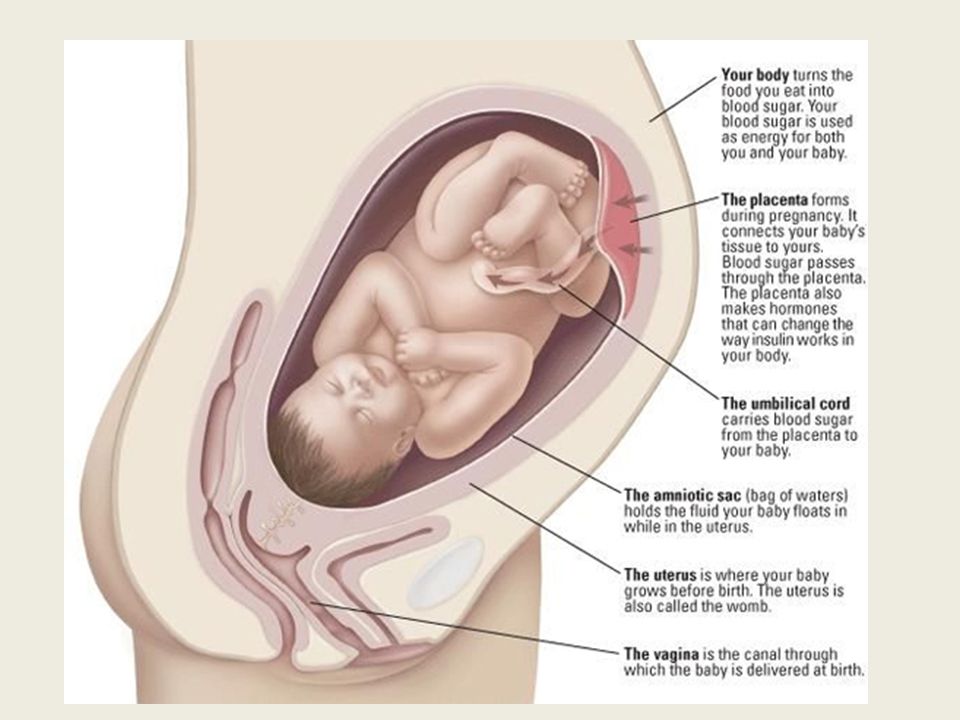 At present, results can be improved, even in exemplary hospital wards, who use best practices, such as the Department of Neonatology of the Hospital Sant Joan de Deu Barcelona In our center for extreme prematurity survival rates are 26% to 70% if gestational age at birth is between 23 and 26 weeks and 90% and 93% at birth at 27 and 28 weeks, respectively. In more severe cases, prematurity, up to 50% of survivors may have neurological complications (this applies to infants born at 23 weeks), and this figure decreases with increasing gestational age. "
At present, results can be improved, even in exemplary hospital wards, who use best practices, such as the Department of Neonatology of the Hospital Sant Joan de Deu Barcelona In our center for extreme prematurity survival rates are 26% to 70% if gestational age at birth is between 23 and 26 weeks and 90% and 93% at birth at 27 and 28 weeks, respectively. In more severe cases, prematurity, up to 50% of survivors may have neurological complications (this applies to infants born at 23 weeks), and this figure decreases with increasing gestational age. "
This low survival rate is due to the fact that up to six months of pregnancy - the lungs, intestines and brain of the fetus are underdeveloped . In fact, Extremely Premature Newborn -- is a fetus that must survive in a very unnatural environment. With a weight of less than 1 kilogram, the child must cope with temperature changes, mechanical breathing and tube feeding , so that his nervous system, lungs, heart, intestines and kidneys suffer from severe stress, which can cause serious consequences for a child in children and adults .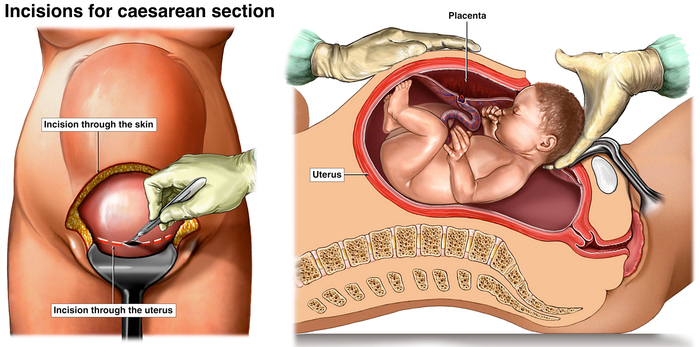
One of the most unique research projects that can be done today in the field of fetal medicine.
The idea of the artificial placenta originated more than 60 years ago, although its clinical application is only now considered possible, thanks to the technical and scientific advances that have developed over the past 10 years.
The artificial placenta project, supported by the La Caixa Foundation, is a major medical and technological challenge that requires many cutting-edge research areas as it requires the successful transport of a fetus weighing 500 to 1000 grams from the mother's uterus into an artificial womb where, while in liquid, his umbilical cord must continue to receive oxygen and food.
According to Eduard Gratakos, director of BCNatal, "this is one of the most revolutionary and unique research projects that can be done today in the field of fetal medicine. There is only an experimental platform like the one that will be built and will allow conduct parallel studies that are important for understanding normal and abnormal fetal development . This will increase the opportunities for attracting investment in research and innovation in Barcelona, Catalonia and Spain, and will also enable a new generation of methods and procedures that will revolutionize fetal medicine. with biocompatible materials.0005 in the womb, inside a soft container made of biocompatible materials and protected from sound and light, although sounds similar to those of womb will be played.
There is only an experimental platform like the one that will be built and will allow conduct parallel studies that are important for understanding normal and abnormal fetal development . This will increase the opportunities for attracting investment in research and innovation in Barcelona, Catalonia and Spain, and will also enable a new generation of methods and procedures that will revolutionize fetal medicine. with biocompatible materials.0005 in the womb, inside a soft container made of biocompatible materials and protected from sound and light, although sounds similar to those of womb will be played.
It will be connected via the umbilical cord to an oxygenator designed and adapted specifically for the fetus, which will provide the necessary amount of oxygen to the fetus. Through this umbilical cord, he will also receive nutrition, hormones and other substances which are the fetus receives from the mother or which are directly produced by the placenta and which are necessary for its proper development.
The baby will be continuously monitored using ultrasound of blood flow, blood pressure and heart rate, and microsensors located in the amniotic fluid or umbilical cord .
Results from experiments will be integrated and evaluated using artificial intelligence to make improvements to the system.
The BCNatal research team has been working on a project for two years now, which has already developed the main components of the placenta. Dozens of professionals from the Hospital Sant Joan de Deu Barcelona and the Clinical Hospital, , as well as several technology centers in Barcelona , will collaborate to implement the initiative, such as the Institut Químic de Sarrià (biomaterials), the Polytechnic University of Catalonia (robotics and artificial intelligence) and the Bioengineering Institute of Catalonia (IBEC) (microsensors).
In addition, the project will have several steering committees, which will include non-medical experts (including in the field of reproductive rights and bioethics), as well as mothers and fathers of premature babies.
The evaluation of the artificial placenta project is carried out at the international level by a committee of experts, which is guided by the strictest standards for this type of initiative. Globally recognized leading experts come from five countries: Australia, Spain, Israel, Portugal and the UK. They all agreed on the excellence of the scientific strategy developed, the magnitude of the problem, the need for alternative solutions such as the artificial placenta , and the importance of new ambitious projects to advance progress in this area. They also emphasized that BCNatal is one of the few organizations in the world and certainly the only in Europe capable of implementing a project of this level.
A pioneering and unique project in Europe to be implemented in two phases.
For project BCNatal (Hospital Sant Joan de Deu - Clinical Hospital), the La Caixa Foundation will allocate about 7 million euros in two phases over five years.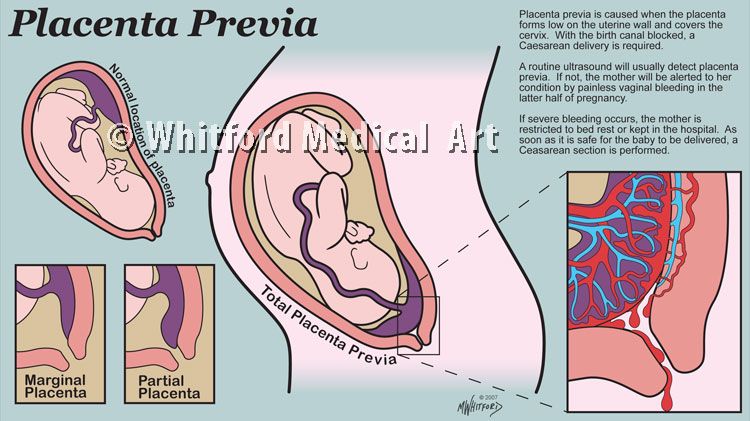 The first phase focuses on development and experimental validation using an animal (sheep) model, with a view to subsequently transferring it to clinical practice if success rates are achieved. At the end of the first phase, the expert group will evaluate the progress made and decide whether to start the preparatory phase for clinical use.
The first phase focuses on development and experimental validation using an animal (sheep) model, with a view to subsequently transferring it to clinical practice if success rates are achieved. At the end of the first phase, the expert group will evaluate the progress made and decide whether to start the preparatory phase for clinical use.
The second phase will assess the long-term effects on the brain, heart, lungs and metabolism and make environmental and nutritional improvements to achieve the best possible system. Once these assessments have been completed, steps will begin to translate the system into clinical use, including an assessment of all ethical aspects and taking into account the opinions and experiences of families who have given birth to a premature baby.
Artificial placenta is a major problem due to its great complexity. On the one hand, this requires a large critical mass, which is possible only in large hospitals operating in a powerful biotechnological environment .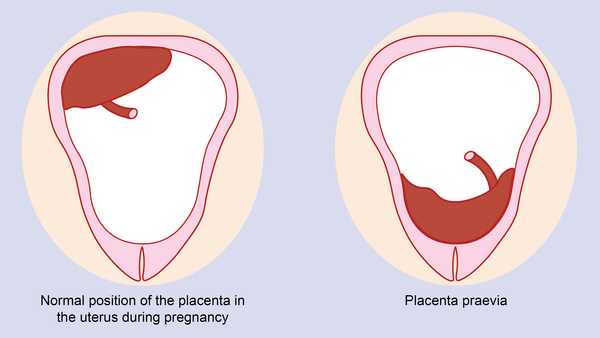 These are projects that may require more than 100 people and many experts in a wide variety of fields . On the other hand, this is a very expensive project, so it is very difficult to obtain the necessary funding for its implementation.
These are projects that may require more than 100 people and many experts in a wide variety of fields . On the other hand, this is a very expensive project, so it is very difficult to obtain the necessary funding for its implementation.
At present, there are only three groups in the world: the United States, Australia and Japan, who have developed similar experimental models, having made significant progress in recent years.
Marginal placenta previa. What is marginal placenta previa?
IMPORTANT
The information in this section should not be used for self-diagnosis or self-treatment. In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
Marginal placenta previa is a pathological attachment of an embryonic organ that provides a connection between the mother and the fetus, in which there is a partial overlap of the internal os of the uterus (no more than a third of it).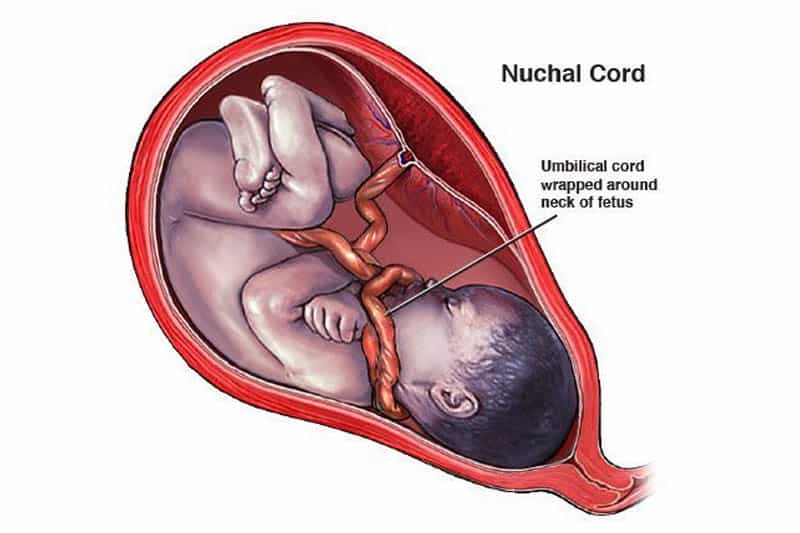 Clinically, the disease is manifested by bleeding of varying intensity, not accompanied by discomfort. It is possible to identify marginal placenta previa with the help of a planned ultrasound in the second trimester or when pathological signs occur. Treatment involves hospitalization, bed rest, symptomatic therapy. Expectant management is indicated before the term of the expected birth, subject to the normal condition of the woman and the fetus.
Clinically, the disease is manifested by bleeding of varying intensity, not accompanied by discomfort. It is possible to identify marginal placenta previa with the help of a planned ultrasound in the second trimester or when pathological signs occur. Treatment involves hospitalization, bed rest, symptomatic therapy. Expectant management is indicated before the term of the expected birth, subject to the normal condition of the woman and the fetus.
- Causes of marginal placenta previa
- Classification of marginal placenta previa
- Symptoms and diagnosis of marginal placenta previa
- Treatment of marginal placenta previa
- Prognosis and prevention of marginal placenta previa
- Prices for treatment
General
Marginal placenta previa is a pathology of pregnancy, accompanied by abnormal attachment of the placenta and partial overlap of the internal os of the uterus. This condition is dangerous for both the woman herself and the fetus. Marginal placenta previa in the early stages is associated with less risk, since with the subsequent growth of the baby and stretching of the myometrium, it can shift and acquire the correct location. Otherwise, there is a possibility of squeezing the supply vessels, partially blocking the access of oxygen and nutrients to the fetus, which can cause its hypoxia and even antenatal death.
Marginal placenta previa in the early stages is associated with less risk, since with the subsequent growth of the baby and stretching of the myometrium, it can shift and acquire the correct location. Otherwise, there is a possibility of squeezing the supply vessels, partially blocking the access of oxygen and nutrients to the fetus, which can cause its hypoxia and even antenatal death.
Marginal placenta previa can lead to placental abruption. This is due to the fact that the lower segment of the uterus has less ability to stretch. Also, marginal placenta previa often provokes massive bleeding during childbirth. Such an outcome is possible during natural childbirth, if there was a sharp separation of the membranes as a result of the passage of the fetus through the birth canal. In obstetrics, placenta previa occurs predominantly in repeated pregnancies. Pathology requires careful monitoring, since in about 25% of cases it is accompanied by stillbirth.
Marginal placenta previa
Causes of marginal placenta previa
Marginal placenta previa may be due to abnormal attachment of the trophoblast during implantation or anatomical features of the myometrium.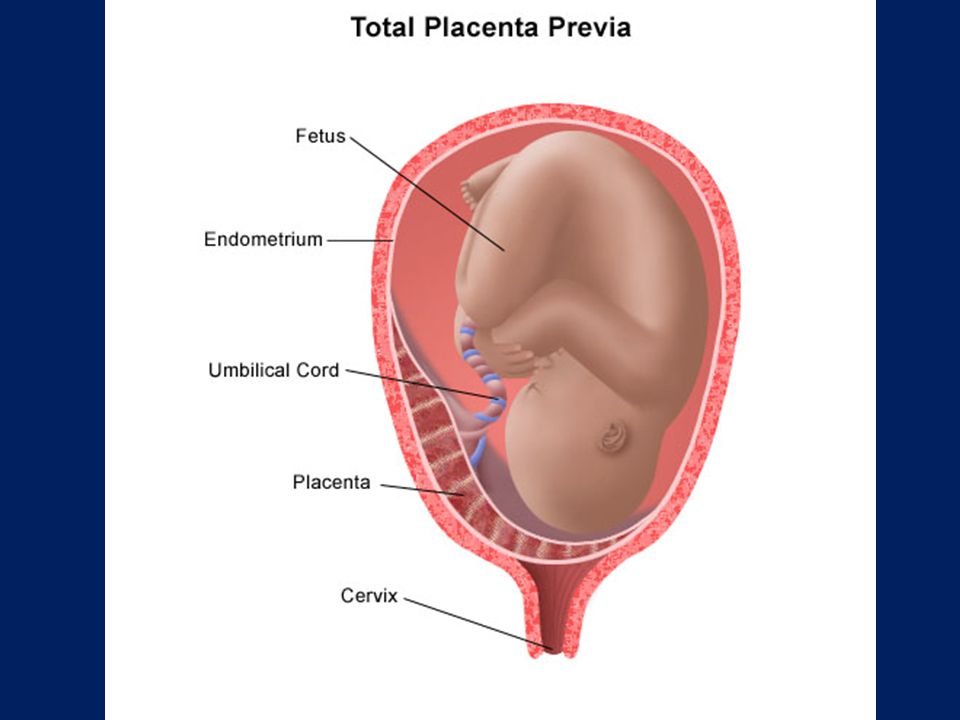 In the latter case, a violation of the structure of muscle fibers in the wall of the uterus occurs against the background of inflammatory changes, the consequences of genital infections. Marginal placenta previa is more often diagnosed with thinning of the myometrium, provoked by frequent curettage and abortion. Also, the cause of abnormal attachment of the trophoblast can be uterine deformities caused by benign tumors or resulting from congenital pathologies.
In the latter case, a violation of the structure of muscle fibers in the wall of the uterus occurs against the background of inflammatory changes, the consequences of genital infections. Marginal placenta previa is more often diagnosed with thinning of the myometrium, provoked by frequent curettage and abortion. Also, the cause of abnormal attachment of the trophoblast can be uterine deformities caused by benign tumors or resulting from congenital pathologies.
Marginal placenta previa often develops in women with concomitant diseases of the internal organs, in particular, in the pathology of the cardiovascular system. Due to insufficient blood circulation and congestion in the pelvis, the placenta cannot fully attach. In addition, marginal placenta previa is possible against the background of abnormal development of the embryo immediately after fertilization. A similar outcome is observed with a belated appearance of the enzymatic functions of the trophoblast.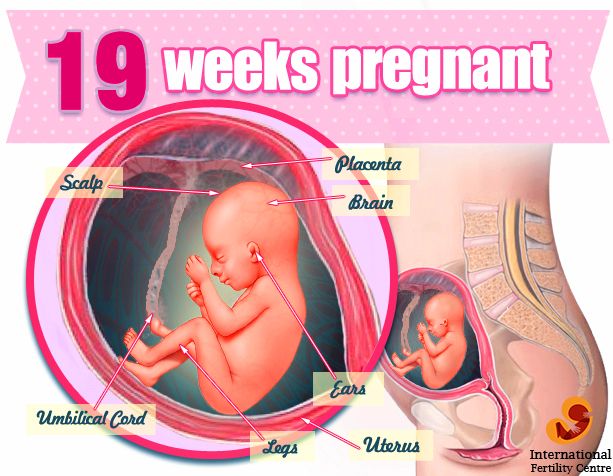 As a result, it attaches to the myometrium later than it normally does, staying in the lower part of the uterus.
As a result, it attaches to the myometrium later than it normally does, staying in the lower part of the uterus.
Classification of marginal placenta previa
Marginal placenta previa can be of two types, depending on the place of its attachment:
- Localization along the anterior wall is the most dangerous variant of the pathology. With marginal placenta previa of this type, there is a high risk of mechanical damage to it, followed by detachment due to the physical activity of the woman, the movements of the baby, against the background of a strong stretching of the uterus in the third trimester of pregnancy. Despite this, when placing the embryonic organ on the anterior wall of the uterus, there is a possibility of its movement upwards.
- Attachment along the back wall is a more favorable variant of the marginal placenta previa. It is accompanied by a lower risk of complications in the process of gestation and childbirth for the mother and baby.

Both types of anomalies are a pathology of pregnancy and require mandatory monitoring by an obstetrician-gynecologist.
Symptoms and diagnosis of marginal placenta previa
Marginal placenta previa has a characteristic symptomatology - the appearance of spotting without worsening overall well-being. Often this pathological symptom occurs at rest or at night. As for the timing of embryogenesis, the marginal placenta previa manifests itself mainly at 28-32 weeks. It is during this period that the uterus is characterized by increased activity due to the preparation of the myometrium for the upcoming birth. Somewhat less often, abnormal discharge is observed already at the beginning of the second trimester. The volume of bleeding can be different and depends on the degree of damage to the vessels.
With marginal placenta previa in the third trimester of pregnancy, bleeding can be triggered by physical activity, sexual intercourse, fetal movement and other factors that provoke rupture of nutrient vessels.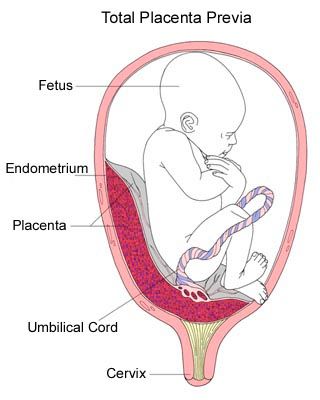 The appearance of this symptom is possible even during a gynecological examination. Sometimes marginal placenta previa is combined with the threat of miscarriage. With this combination, there is discomfort in the lower abdomen, hypertonicity of the uterus. With systematic bleeding in pregnant women with such a diagnosis, iron deficiency anemia develops. In such cases, there is increased fatigue, weakness. On the part of the fetus, growth and development may be slowed down, hypoxia due to insufficient intake of nutrients. Marginal placenta previa is often combined with an abnormal position of the fetus, which can be oblique or transverse.
The appearance of this symptom is possible even during a gynecological examination. Sometimes marginal placenta previa is combined with the threat of miscarriage. With this combination, there is discomfort in the lower abdomen, hypertonicity of the uterus. With systematic bleeding in pregnant women with such a diagnosis, iron deficiency anemia develops. In such cases, there is increased fatigue, weakness. On the part of the fetus, growth and development may be slowed down, hypoxia due to insufficient intake of nutrients. Marginal placenta previa is often combined with an abnormal position of the fetus, which can be oblique or transverse.
A preliminary diagnosis is established on the basis of the patient's complaints of spotting in the absence of pain. Another characteristic sign of the abnormal location of the embryonic organ is the high standing of the uterine fundus, which does not correspond to the period of embryogenesis. It is possible to confirm the marginal presentation of the placenta with the help of ultrasound. During the scanning process, a specialist can accurately visualize the location of the placenta and the degree of overlap of the uterine os, determine the condition of the child and assess the possible risks to the woman and the fetus.
During the scanning process, a specialist can accurately visualize the location of the placenta and the degree of overlap of the uterine os, determine the condition of the child and assess the possible risks to the woman and the fetus.
Treatment of marginal placenta previa
Treatment of marginal placenta previa depends on the identified symptoms, the period of embryogenesis, as well as the condition of the expectant mother and fetus. If the diagnosis is established only on the basis of ultrasound scanning and bleeding is not observed, it is possible to control the patient's condition on an outpatient basis. Hospitalization is indicated if marginal placenta previa is accompanied by secretions of any volume of blood. In this case, careful monitoring in the hospital is required. Women with such a diagnosis are assigned complete rest, it is recommended to exclude sexual intercourse and stress. You must wear a bandage. In the second trimester, a special exercise therapy for pregnant women sometimes helps to correct the location of the placenta.
With marginal placenta previa, anemia often develops due to systematic blood loss. Therefore, pregnant women are shown a diet enriched with foods high in iron. The diet should contain red fish, offal, buckwheat, beef, apples. Pregnancy management with marginal placenta previa involves a protective regime in order to achieve the expected date of birth and the birth of a full-term baby. Also, patients with a similar diagnosis are prescribed medications, taking into account the general condition and comorbidities.
With marginal placenta previa, symptomatic drug therapy is carried out. With uterine hypertonicity, tocolytics and antispasmodics are used, and preparations containing iron are prescribed to eliminate anemia. To maintain the general condition of the patient and the fetus, vitamin complexes can be used. Sometimes, with marginal placenta previa, it is advisable to use sedatives. According to indications, antiplatelet agents are introduced, the doctor calculates the dosage of drugs in order to avoid a negative impact on the baby.
If marginal placenta previa is accompanied by massive bleeding, delivery is carried out regardless of the period of embryogenesis by emergency caesarean section. In the case of a full-term pregnancy, vaginal delivery is acceptable provided that the cervix is ripe, active labor activity, and the patient and fetus are in good condition. When opening the cervix by 3 cm, an amniotomy is performed. Oxytocin is administered to prevent bleeding. If, with marginal presentation, the placenta significantly overlaps the uterine os or childbirth through the natural canal is impossible, a caesarean section is indicated.
Prognosis and prevention of marginal placenta previa
The prognosis for marginal placenta previa is favorable. With timely diagnosis and compliance with medical recommendations, patients manage to carry the fetus up to 38 weeks and give birth to a completely healthy baby. Marginal placenta previa can provoke the development of bleeding in the postpartum period.