How to have a miscarriages
Causes, Symptoms, Risks, Treatment & Prevention
Overview
What is a miscarriage?
A miscarriage (also called a spontaneous abortion) is the unexpected ending of a pregnancy in the first 20 weeks of gestation. Just because it’s called a “miscarriage” doesn’t mean you did something wrong in carrying the pregnancy. Most miscarriages are beyond your control and occur because the fetus stops growing.
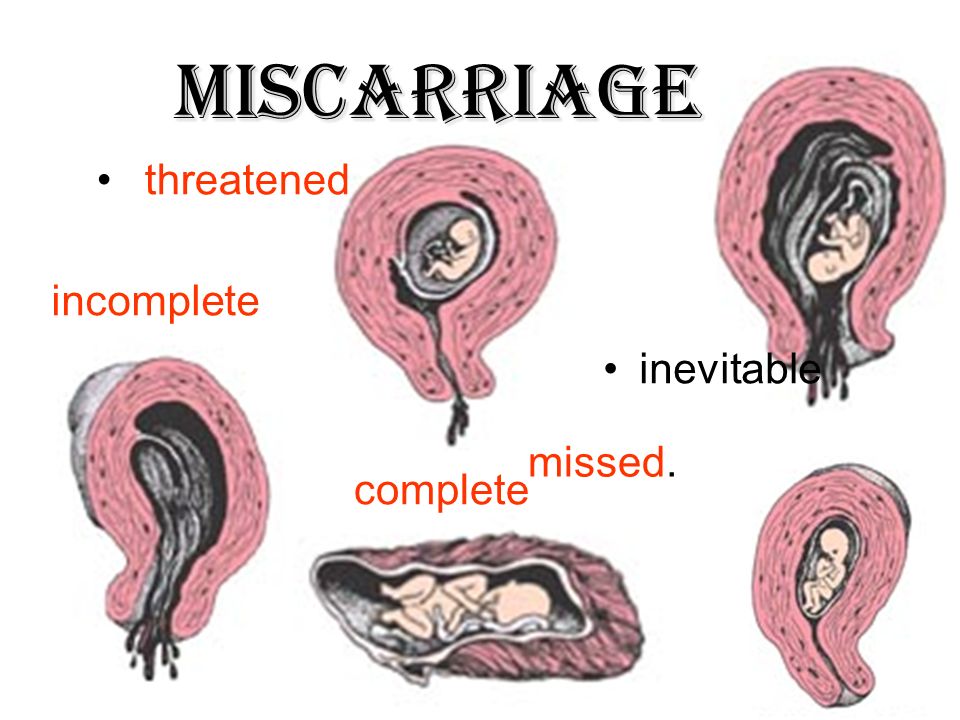
Types of miscarriage
Your pregnancy care provider may diagnose you with the following types of miscarriage:
- Missed miscarriage: You’ve lost the pregnancy but are unaware it’s happened. There are no symptoms of miscarriage, but an ultrasound confirms the fetus has no heartbeat.
- Complete miscarriage: You’ve lost the pregnancy and your uterus is empty. You’ve experienced bleeding and passed fetal tissue. Your provider can confirm a complete miscarriage with an ultrasound.
- Recurrent miscarriage: Three consecutive miscarriages.
It affects about 1% of couples.
- Threatened miscarriage: Your cervix stays closed, but you’re bleeding and experiencing pelvic cramping. The pregnancy typically continues with no further issues. Your pregnancy care provider may monitor you more closely for the rest of your pregnancy.
- Inevitable miscarriage: You’re bleeding, cramping and your cervix has started to open (dilate). You may leak amniotic fluid. A complete miscarriage is likely.
How do I know if I’m having a miscarriage?
You may not be aware you’re having a miscarriage. In people who have symptoms of a miscarriage, the most common signs are:
- Bleeding that progresses from light to heavy. You may also pass grayish tissue or blood clots.
- Cramps and abdominal pain (usually worse than menstrual cramps).
- Low back ache that may range from mild to severe.
- A decrease in pregnancy symptoms.
Contact your pregnancy care provider right away if you’re experiencing any of these symptoms. They will tell you to come into the office or go to the emergency room.
They will tell you to come into the office or go to the emergency room.
Symptoms and Causes
What causes miscarriage?
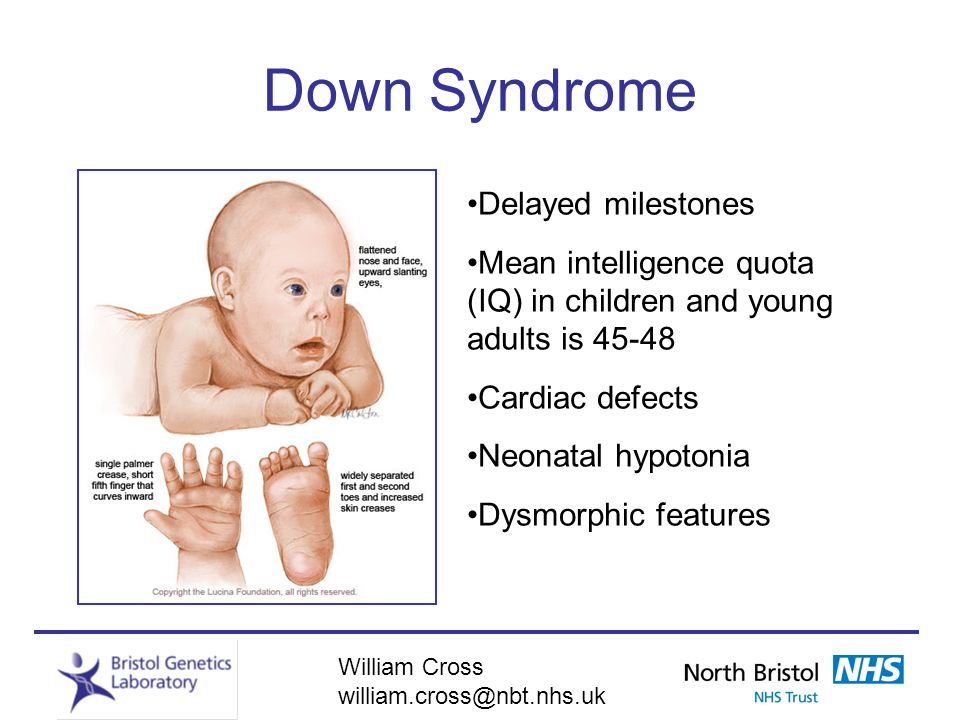
Chromosomal abnormalities cause about 50% of all miscarriages in the first trimester (up to 13 weeks) of pregnancy. Chromosomes are tiny structures inside the cells of your body that carry your genes. Genes determine all of a person’s physical attributes, such as assigned sex, hair and eye color and blood type.
During fertilization, when the egg and sperm join, two sets of chromosomes come together. If an egg or sperm has more or fewer chromosomes than normal, the fetus will have an abnormal number. As a fertilized egg grows into a fetus, its cells divide and multiply several times. Abnormalities during this process also leads to miscarriage.
Most chromosomal problems occur by chance. It’s not completely known why this happens.
Several factors may cause miscarriage:
- Infection.
- Exposure to TORCH diseases.
- Hormonal imbalances.
- Improper implantation of fertilized egg in your uterine lining.
- How old you are.
- Uterine abnormalities.
- Incompetent cervix (your cervix begins to open too early in pregnancy).
- Lifestyle factors such as smoking, drinking alcohol or using recreational drugs.
- Disorders of the immune system like lupus.
- Severe kidney disease.
- Congenital heart disease.
- Diabetes that isn't managed.
- Thyroid disease.
- Radiation.
- Certain medicines, such as the acne drug isotretinoin (Accutane®).
- Severe malnutrition.
There is no scientific proof that stress, exercise, sexual activity or prolonged use of birth control pills cause miscarriage. Whatever your situation is, it’s important to not blame yourself for having a miscarriage. Most miscarriages have nothing to do with something you did or didn’t do.
How painful is a miscarriage?
Miscarriages are different for every person. Some people have painful cramping, while other people have cramps similar to their menstrual period. The type of miscarriage you have may also affect your pain level. For example, if you have a complete miscarriage at home, you may have more pain than a person who has a missed miscarriage and has a surgical procedure to remove the pregnancy.
Some people have painful cramping, while other people have cramps similar to their menstrual period. The type of miscarriage you have may also affect your pain level. For example, if you have a complete miscarriage at home, you may have more pain than a person who has a missed miscarriage and has a surgical procedure to remove the pregnancy.
What happens first during a miscarriage?
It’s hard to say what happens first during a miscarriage because everyone’s symptoms are different. Sometimes there are no signs of miscarriage, and you find out at a prenatal ultrasound that you’ve lost the pregnancy. Most people will experience some degree of cramping and bleeding, but what happens first varies.
How long does a miscarriage take?
It depends. Some people have painful cramping and heavy bleeding longer than others. Your pregnancy care provider can tell you what to expect and give you advice on how to manage pain and cramps during your miscarriage.
What are the risk factors for a miscarriage?
A risk factor is a trait or behavior that increases a person’s chance of developing a disease or condition. Risk factors for miscarriage include:
Risk factors for miscarriage include:
- Your age: Studies show that the risk of miscarriage is 12% to 15% for people in their 20s and rises to about 25% for people by age 40. Most age-related miscarriages happen because of a chromosomal abnormality (the fetus has missing or extra chromosomes).
- Previous miscarriage: You have a 25% chance of having another miscarriage (only slightly higher than someone who hasn’t had a miscarriage) if you’ve already had one.
- Health conditions: Certain health conditions like unmanaged diabetes, infections or issues with your uterus or cervix increase your chance of miscarriage.
Talk to your pregnancy care provider about the risk factors for miscarriage. They can discuss your risk after they’ve reviewed your medical history.
How many people have miscarriages?
Between 10% and 20% of all known pregnancies end in miscarriage. Most miscarriages (80%) happen within the first three months of pregnancy (up to 13 weeks of pregnancy). Less than 5% of miscarriages occur after 20 weeks’ gestation.The rate of miscarriage may be higher if you consider miscarriages that happen shortly after implantation. A person may not realize they’re pregnant because bleeding happens around the time of their menstrual period. This is called a chemical pregnancy.
Less than 5% of miscarriages occur after 20 weeks’ gestation.The rate of miscarriage may be higher if you consider miscarriages that happen shortly after implantation. A person may not realize they’re pregnant because bleeding happens around the time of their menstrual period. This is called a chemical pregnancy.
What is my risk of miscarriage by week?
Your risk of pregnancy loss declines each week you’re pregnant. Around 15% of pregnancies end in miscarriage. Miscarriage risk in the second trimester (13 to 19 weeks) is between 1% and 5%. Many factors affect your risk of miscarriage such as your age and health. However, everyone’s risk of miscarriage declines each week of pregnancy if the pregnant person has no other health conditions.
Diagnosis and Tests
How is a miscarriage diagnosed?
Your pregnancy care provider will perform an ultrasound test to confirm a miscarriage. These tests check for fetal heartbeat or the presence of a yolk sac (one of the first fetal structures your provider can see on ultrasound).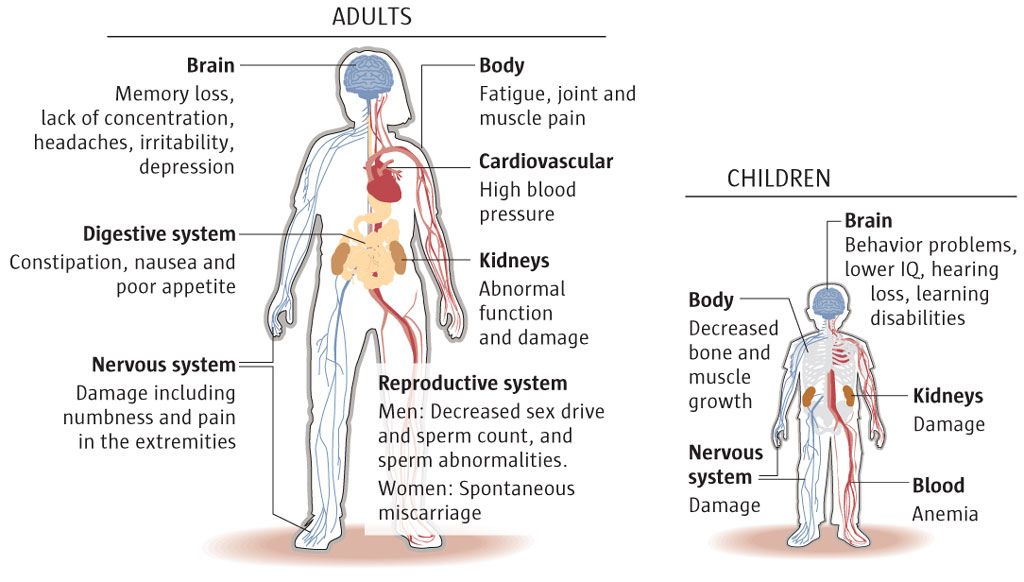
You may also have a blood test to measure human chorionic gonadotropin (hCG), a hormone produced by the placenta. A low hCG level can confirm a miscarriage.
Finally, your provider may perform a pelvic exam to check if your cervix has opened.
Management and Treatment
What are the treatments for a miscarriage?
If you experience the loss of a pregnancy, the fetus must be removed from your uterus. If any parts of the pregnancy are left inside your body, you could experience infection, bleeding or other complications.
If the miscarriage is complete and your uterus expels all the fetal tissue, then no further treatment is usually needed. Your pregnancy care provider will conduct an ultrasound to make sure there’s nothing left in your uterus.
If your body doesn’t remove all the tissue on its own or you haven’t started to bleed, your pregnancy care provider will recommend removing the tissue with medication or surgery.
Nonsurgical treatment
Your pregnancy care provider may recommend waiting to see if you pass the pregnancy on your own. This may be the case if you have a missed miscarriage. Waiting for a miscarriage to start could take several days. If waiting to pass the tissue isn’t safe or you wish to remove the tissue as soon as possible, they may recommend taking a medication that helps your uterus pass the pregnancy. These options are typically only available if you’ve miscarried before 10 weeks of pregnancy.
This may be the case if you have a missed miscarriage. Waiting for a miscarriage to start could take several days. If waiting to pass the tissue isn’t safe or you wish to remove the tissue as soon as possible, they may recommend taking a medication that helps your uterus pass the pregnancy. These options are typically only available if you’ve miscarried before 10 weeks of pregnancy.
If a miscarriage wasn’t confirmed, but you had symptoms of a miscarriage, your provider may prescribe bed rest for several days. You might be admitted to the hospital overnight for observation. When the bleeding stops, you may be able to continue with your normal activities. If your cervix is dilated, they may diagnose you with an incompetent cervix, and they may perform a procedure to close your cervix (cervical cerclage).
Surgical treatment
Your provider may perform a dilation and curettage (D&C) or dilation and evacuation (D&E) if your uterus hasn’t passed the pregnancy or if you’re bleeding heavily. Surgery may also be the only option if your pregnancy is beyond 10 weeks’ gestation. During these procedures, your cervix is dilated, and any remaining pregnancy-related tissue is gently scraped or suctioned out of your uterus. Your provider performs these surgeries in a hospital, and you’ll be under anesthesia.
Surgery may also be the only option if your pregnancy is beyond 10 weeks’ gestation. During these procedures, your cervix is dilated, and any remaining pregnancy-related tissue is gently scraped or suctioned out of your uterus. Your provider performs these surgeries in a hospital, and you’ll be under anesthesia.
What are some of the symptoms after a miscarriage?
Spotting and mild discomfort are common symptoms after a miscarriage.
Contact your healthcare provider immediately if you have any of these symptoms as it could be signs of an infection:
- Heavy bleeding or worsening bleeding.
- Fever.
- Chills.
- Intense pain.
Don’t put anything inside your vagina for at least two weeks after a miscarriage. This includes tampons, sexual intercourse and fingers or sex toys. Your provider will schedule a follow-up appointment with you to discuss your recovery and any complications.
What tests should I have after repeat miscarriages?
Blood tests or genetic tests might be necessary if you’ve more than three miscarriages in a row (called repeated miscarriage). These include:
These include:
- Genetic tests: You and your partner can have blood tests, like karyotyping, to check for chromosome abnormalities. If tissue from the miscarriage is available, your provider may be able to test it for chromosome irregularities.
- Blood tests: You may have a blood test to check for autoimmune or hormone conditions that could be causing miscarriages.
Your provider may also look at your uterus using one of the following procedures:
- Hysterosalpingogram (an X-ray dye test of your uterus and fallopian tubes).
- Hysteroscopy (a test during which your provider views the inside of your uterus with a thin, telescope-like device).
- Laparoscopy (a procedure during which your provider views the pelvic organs with a lighted device).
Prevention
How can I prevent another miscarriage?
It’s usually not possible to prevent a miscarriage. If you have a miscarriage, it’s not because you did something to cause it. Taking care of your body is the best thing you can do. Some examples of ways to care for yourself include:
Taking care of your body is the best thing you can do. Some examples of ways to care for yourself include:
- Attending all your prenatal care appointments.
- Maintaining a weight that's healthy for you.
- Avoiding risk factors for miscarriage like drinking alcohol and smoking cigarettes.
- Taking a prenatal vitamin.
- Getting regular exercise and eating a healthy diet.
Outlook / Prognosis
Can I get pregnant after I’ve had a miscarriage?
Yes. Most people (87%) who have miscarriages have subsequent normal pregnancies and births. Having a miscarriage doesn’t necessarily mean you have a fertility problem. Remember, most miscarriages occur because of a chromosomal abnormality, not because of something you did.
How soon can I get pregnant after a miscarriage?
The decision on when you should begin trying to get pregnant again is between you and your pregnancy care provider. Most people can get pregnant again after they’ve had one “normal” menstrual period.
Taking time to heal both physically and emotionally after a miscarriage is important. Counseling is available to help you cope with your loss. A pregnancy loss support group might also be a valuable resource to you and your partner. Ask your healthcare provider for more information about counseling and support groups. Above all, don’t blame yourself for the miscarriage. Take the time you need to grieve.
If you’ve had three miscarriages in a row, ask your provider about performing tests to figure out an underlying cause. You should use birth control until you receive the results. After your provider reviews the test results, they may suggest going off birth control and trying to conceive again.
Living With
How can I cope with my miscarriage?
Losing a pregnancy can be devastating and leave you with a range of emotions and lots of questions. Healing emotionally from a miscarriage is often harder and longer than the physical healing. Take the time you need to grieve your loss.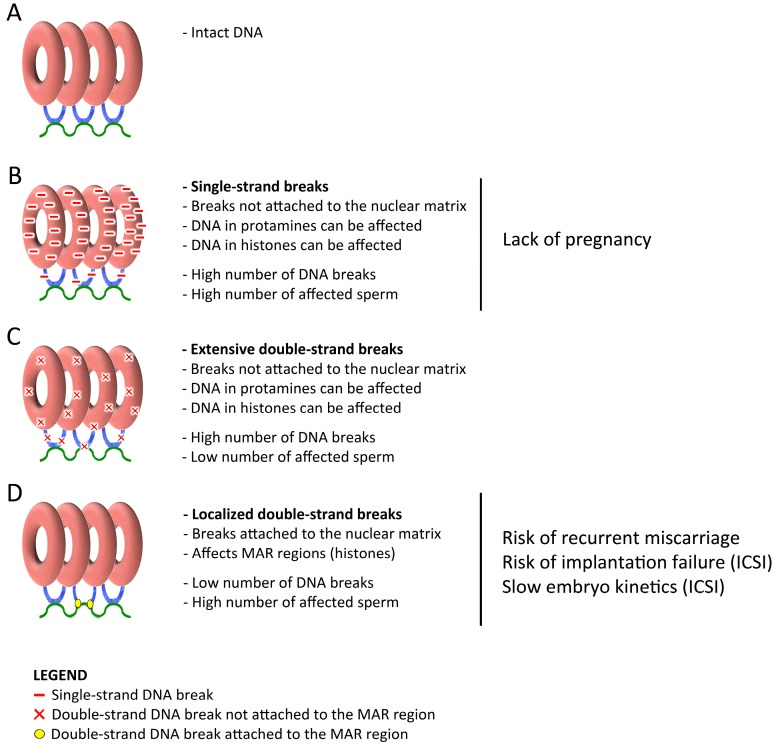 Talk to your partner, friends and family about your feelings or find a pregnancy loss support group online. Surround yourself with supportive people or seek professional counseling to help you cope with the loss.
Talk to your partner, friends and family about your feelings or find a pregnancy loss support group online. Surround yourself with supportive people or seek professional counseling to help you cope with the loss.
A note from Cleveland Clinic
A miscarriage is a very emotional moment for expectant parents and it’s natural to grieve the loss. Remember that a miscarriage can’t be prevented, and it’s not caused by something you did wrong. It doesn’t mean that you can’t have children or that you’ll have another miscarriage. If you’re planning to become pregnant, reach out to your healthcare provider to discuss the timing of your next pregnancy and ask any questions you have. It’s OK to be sad. Find support from family, friends online support groups or a licensed counselor.
Causes, Symptoms, Risks, Treatment & Prevention
Overview
What is a miscarriage?
A miscarriage (also called a spontaneous abortion) is the unexpected ending of a pregnancy in the first 20 weeks of gestation. Just because it’s called a “miscarriage” doesn’t mean you did something wrong in carrying the pregnancy. Most miscarriages are beyond your control and occur because the fetus stops growing.
Just because it’s called a “miscarriage” doesn’t mean you did something wrong in carrying the pregnancy. Most miscarriages are beyond your control and occur because the fetus stops growing.
Types of miscarriage
Your pregnancy care provider may diagnose you with the following types of miscarriage:
- Missed miscarriage: You’ve lost the pregnancy but are unaware it’s happened. There are no symptoms of miscarriage, but an ultrasound confirms the fetus has no heartbeat.
- Complete miscarriage: You’ve lost the pregnancy and your uterus is empty. You’ve experienced bleeding and passed fetal tissue. Your provider can confirm a complete miscarriage with an ultrasound.
- Recurrent miscarriage: Three consecutive miscarriages. It affects about 1% of couples.
- Threatened miscarriage: Your cervix stays closed, but you’re bleeding and experiencing pelvic cramping. The pregnancy typically continues with no further issues.
 Your pregnancy care provider may monitor you more closely for the rest of your pregnancy.
Your pregnancy care provider may monitor you more closely for the rest of your pregnancy. - Inevitable miscarriage: You’re bleeding, cramping and your cervix has started to open (dilate). You may leak amniotic fluid. A complete miscarriage is likely.
How do I know if I’m having a miscarriage?
You may not be aware you’re having a miscarriage. In people who have symptoms of a miscarriage, the most common signs are:
- Bleeding that progresses from light to heavy. You may also pass grayish tissue or blood clots.
- Cramps and abdominal pain (usually worse than menstrual cramps).
- Low back ache that may range from mild to severe.
- A decrease in pregnancy symptoms.
Contact your pregnancy care provider right away if you’re experiencing any of these symptoms. They will tell you to come into the office or go to the emergency room.
Symptoms and Causes
What causes miscarriage?
Chromosomal abnormalities cause about 50% of all miscarriages in the first trimester (up to 13 weeks) of pregnancy. Chromosomes are tiny structures inside the cells of your body that carry your genes. Genes determine all of a person’s physical attributes, such as assigned sex, hair and eye color and blood type.
Chromosomes are tiny structures inside the cells of your body that carry your genes. Genes determine all of a person’s physical attributes, such as assigned sex, hair and eye color and blood type.
During fertilization, when the egg and sperm join, two sets of chromosomes come together. If an egg or sperm has more or fewer chromosomes than normal, the fetus will have an abnormal number. As a fertilized egg grows into a fetus, its cells divide and multiply several times. Abnormalities during this process also leads to miscarriage.
Most chromosomal problems occur by chance. It’s not completely known why this happens.
Several factors may cause miscarriage:
- Infection.
- Exposure to TORCH diseases.
- Hormonal imbalances.
- Improper implantation of fertilized egg in your uterine lining.
- How old you are.
- Uterine abnormalities.
- Incompetent cervix (your cervix begins to open too early in pregnancy).
- Lifestyle factors such as smoking, drinking alcohol or using recreational drugs.

- Disorders of the immune system like lupus.
- Severe kidney disease.
- Congenital heart disease.
- Diabetes that isn't managed.
- Thyroid disease.
- Radiation.
- Certain medicines, such as the acne drug isotretinoin (Accutane®).
- Severe malnutrition.
There is no scientific proof that stress, exercise, sexual activity or prolonged use of birth control pills cause miscarriage. Whatever your situation is, it’s important to not blame yourself for having a miscarriage. Most miscarriages have nothing to do with something you did or didn’t do.
How painful is a miscarriage?
Miscarriages are different for every person. Some people have painful cramping, while other people have cramps similar to their menstrual period. The type of miscarriage you have may also affect your pain level. For example, if you have a complete miscarriage at home, you may have more pain than a person who has a missed miscarriage and has a surgical procedure to remove the pregnancy.
What happens first during a miscarriage?
It’s hard to say what happens first during a miscarriage because everyone’s symptoms are different. Sometimes there are no signs of miscarriage, and you find out at a prenatal ultrasound that you’ve lost the pregnancy. Most people will experience some degree of cramping and bleeding, but what happens first varies.
How long does a miscarriage take?
It depends. Some people have painful cramping and heavy bleeding longer than others. Your pregnancy care provider can tell you what to expect and give you advice on how to manage pain and cramps during your miscarriage.
What are the risk factors for a miscarriage?
A risk factor is a trait or behavior that increases a person’s chance of developing a disease or condition. Risk factors for miscarriage include:
- Your age: Studies show that the risk of miscarriage is 12% to 15% for people in their 20s and rises to about 25% for people by age 40.
 Most age-related miscarriages happen because of a chromosomal abnormality (the fetus has missing or extra chromosomes).
Most age-related miscarriages happen because of a chromosomal abnormality (the fetus has missing or extra chromosomes). - Previous miscarriage: You have a 25% chance of having another miscarriage (only slightly higher than someone who hasn’t had a miscarriage) if you’ve already had one.
- Health conditions: Certain health conditions like unmanaged diabetes, infections or issues with your uterus or cervix increase your chance of miscarriage.
Talk to your pregnancy care provider about the risk factors for miscarriage. They can discuss your risk after they’ve reviewed your medical history.
How many people have miscarriages?
Between 10% and 20% of all known pregnancies end in miscarriage. Most miscarriages (80%) happen within the first three months of pregnancy (up to 13 weeks of pregnancy). Less than 5% of miscarriages occur after 20 weeks’ gestation.The rate of miscarriage may be higher if you consider miscarriages that happen shortly after implantation. A person may not realize they’re pregnant because bleeding happens around the time of their menstrual period. This is called a chemical pregnancy.
A person may not realize they’re pregnant because bleeding happens around the time of their menstrual period. This is called a chemical pregnancy.
What is my risk of miscarriage by week?
Your risk of pregnancy loss declines each week you’re pregnant. Around 15% of pregnancies end in miscarriage. Miscarriage risk in the second trimester (13 to 19 weeks) is between 1% and 5%. Many factors affect your risk of miscarriage such as your age and health. However, everyone’s risk of miscarriage declines each week of pregnancy if the pregnant person has no other health conditions.
Diagnosis and Tests
How is a miscarriage diagnosed?
Your pregnancy care provider will perform an ultrasound test to confirm a miscarriage. These tests check for fetal heartbeat or the presence of a yolk sac (one of the first fetal structures your provider can see on ultrasound).
You may also have a blood test to measure human chorionic gonadotropin (hCG), a hormone produced by the placenta. A low hCG level can confirm a miscarriage.
A low hCG level can confirm a miscarriage.
Finally, your provider may perform a pelvic exam to check if your cervix has opened.
Management and Treatment
What are the treatments for a miscarriage?
If you experience the loss of a pregnancy, the fetus must be removed from your uterus. If any parts of the pregnancy are left inside your body, you could experience infection, bleeding or other complications.
If the miscarriage is complete and your uterus expels all the fetal tissue, then no further treatment is usually needed. Your pregnancy care provider will conduct an ultrasound to make sure there’s nothing left in your uterus.
If your body doesn’t remove all the tissue on its own or you haven’t started to bleed, your pregnancy care provider will recommend removing the tissue with medication or surgery.
Nonsurgical treatment
Your pregnancy care provider may recommend waiting to see if you pass the pregnancy on your own. This may be the case if you have a missed miscarriage. Waiting for a miscarriage to start could take several days. If waiting to pass the tissue isn’t safe or you wish to remove the tissue as soon as possible, they may recommend taking a medication that helps your uterus pass the pregnancy. These options are typically only available if you’ve miscarried before 10 weeks of pregnancy.
Waiting for a miscarriage to start could take several days. If waiting to pass the tissue isn’t safe or you wish to remove the tissue as soon as possible, they may recommend taking a medication that helps your uterus pass the pregnancy. These options are typically only available if you’ve miscarried before 10 weeks of pregnancy.
If a miscarriage wasn’t confirmed, but you had symptoms of a miscarriage, your provider may prescribe bed rest for several days. You might be admitted to the hospital overnight for observation. When the bleeding stops, you may be able to continue with your normal activities. If your cervix is dilated, they may diagnose you with an incompetent cervix, and they may perform a procedure to close your cervix (cervical cerclage).
Surgical treatment
Your provider may perform a dilation and curettage (D&C) or dilation and evacuation (D&E) if your uterus hasn’t passed the pregnancy or if you’re bleeding heavily. Surgery may also be the only option if your pregnancy is beyond 10 weeks’ gestation. During these procedures, your cervix is dilated, and any remaining pregnancy-related tissue is gently scraped or suctioned out of your uterus. Your provider performs these surgeries in a hospital, and you’ll be under anesthesia.
During these procedures, your cervix is dilated, and any remaining pregnancy-related tissue is gently scraped or suctioned out of your uterus. Your provider performs these surgeries in a hospital, and you’ll be under anesthesia.
What are some of the symptoms after a miscarriage?
Spotting and mild discomfort are common symptoms after a miscarriage.
Contact your healthcare provider immediately if you have any of these symptoms as it could be signs of an infection:
- Heavy bleeding or worsening bleeding.
- Fever.
- Chills.
- Intense pain.
Don’t put anything inside your vagina for at least two weeks after a miscarriage. This includes tampons, sexual intercourse and fingers or sex toys. Your provider will schedule a follow-up appointment with you to discuss your recovery and any complications.
What tests should I have after repeat miscarriages?
Blood tests or genetic tests might be necessary if you’ve more than three miscarriages in a row (called repeated miscarriage). These include:
- Genetic tests: You and your partner can have blood tests, like karyotyping, to check for chromosome abnormalities. If tissue from the miscarriage is available, your provider may be able to test it for chromosome irregularities.
- Blood tests: You may have a blood test to check for autoimmune or hormone conditions that could be causing miscarriages.
Your provider may also look at your uterus using one of the following procedures:
- Hysterosalpingogram (an X-ray dye test of your uterus and fallopian tubes).
- Hysteroscopy (a test during which your provider views the inside of your uterus with a thin, telescope-like device).
- Laparoscopy (a procedure during which your provider views the pelvic organs with a lighted device).
Prevention
How can I prevent another miscarriage?
It’s usually not possible to prevent a miscarriage. If you have a miscarriage, it’s not because you did something to cause it. Taking care of your body is the best thing you can do. Some examples of ways to care for yourself include:
Taking care of your body is the best thing you can do. Some examples of ways to care for yourself include:
- Attending all your prenatal care appointments.
- Maintaining a weight that's healthy for you.
- Avoiding risk factors for miscarriage like drinking alcohol and smoking cigarettes.
- Taking a prenatal vitamin.
- Getting regular exercise and eating a healthy diet.
Outlook / Prognosis
Can I get pregnant after I’ve had a miscarriage?
Yes. Most people (87%) who have miscarriages have subsequent normal pregnancies and births. Having a miscarriage doesn’t necessarily mean you have a fertility problem. Remember, most miscarriages occur because of a chromosomal abnormality, not because of something you did.
How soon can I get pregnant after a miscarriage?
The decision on when you should begin trying to get pregnant again is between you and your pregnancy care provider. Most people can get pregnant again after they’ve had one “normal” menstrual period.
Taking time to heal both physically and emotionally after a miscarriage is important. Counseling is available to help you cope with your loss. A pregnancy loss support group might also be a valuable resource to you and your partner. Ask your healthcare provider for more information about counseling and support groups. Above all, don’t blame yourself for the miscarriage. Take the time you need to grieve.
If you’ve had three miscarriages in a row, ask your provider about performing tests to figure out an underlying cause. You should use birth control until you receive the results. After your provider reviews the test results, they may suggest going off birth control and trying to conceive again.
Living With
How can I cope with my miscarriage?
Losing a pregnancy can be devastating and leave you with a range of emotions and lots of questions. Healing emotionally from a miscarriage is often harder and longer than the physical healing. Take the time you need to grieve your loss.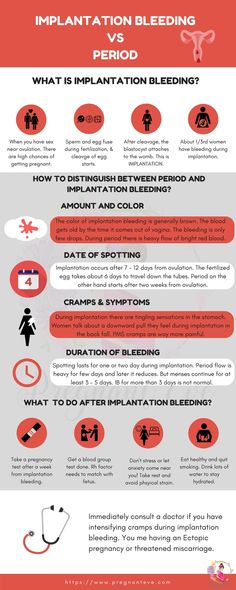 Talk to your partner, friends and family about your feelings or find a pregnancy loss support group online. Surround yourself with supportive people or seek professional counseling to help you cope with the loss.
Talk to your partner, friends and family about your feelings or find a pregnancy loss support group online. Surround yourself with supportive people or seek professional counseling to help you cope with the loss.
A note from Cleveland Clinic
A miscarriage is a very emotional moment for expectant parents and it’s natural to grieve the loss. Remember that a miscarriage can’t be prevented, and it’s not caused by something you did wrong. It doesn’t mean that you can’t have children or that you’ll have another miscarriage. If you’re planning to become pregnant, reach out to your healthcare provider to discuss the timing of your next pregnancy and ask any questions you have. It’s OK to be sad. Find support from family, friends online support groups or a licensed counselor.
Medical termination of pregnancy in the early stages in Nizhny Novgorod at the Tonus clinic, medical abortion, mini abortion
Termination of pregnancy is an important step in the life of a woman who is going to do this. It is important to think carefully about everything, and also, to choose a clinic where you would like to have an abortion. After you have made up your mind, the question arises, where to have an abortion? Not all clinics are licensed to perform abortions, so if you want to do abortion, clinic , in which it will be performed, must have the appropriate permission.
It is important to think carefully about everything, and also, to choose a clinic where you would like to have an abortion. After you have made up your mind, the question arises, where to have an abortion? Not all clinics are licensed to perform abortions, so if you want to do abortion, clinic , in which it will be performed, must have the appropriate permission.
In our country, at her own request, a woman can have an abortion for up to 12 weeks. There are also various indications for termination of pregnancy. Abortion for social reasons a woman can do up to 22 weeks, for medical - at any stage of pregnancy.
Abortion in this case is performed after determining the indications for it by a gynecologist and related specialists. The reason for termination of pregnancy for medical reasons can be both a serious pathology on the part of the woman and on the part of the fetus. Only a competent and experienced gynecologist will help you decide on the choice of the method of abortion - medical, mini-abortion or surgical.
The best is early termination of pregnancy . Early termination of pregnancy reduces the risk of complications in the future and can be carried out without the use of invasive techniques.
Early termination of pregnancy. Medical abortion
Medical abortion is one of the safest methods and an excellent alternative to surgical abortion. Medical abortion is performed up to 6 weeks of pregnancy. When holding medical termination of pregnancy in the early stages, drugs are used that, by their mechanism of action, inhibit the synthesis of progesterone.
Medical abortion is performed only under the strict supervision of a gynecologist. After medical termination of pregnancy, an ultrasound scan is required to examine the uterine cavity.
Early termination of pregnancy by medical abortion method does not impair the woman's reproductive function. According to many studies, after medical termination of pregnancy, ovulation is restored in the shortest possible time. An additional positive quality of medical abortion is the possibility of its implementation directly on the day of treatment.
An additional positive quality of medical abortion is the possibility of its implementation directly on the day of treatment.
Early termination of pregnancy - mini-abortion
Mini-abortion as a method of early termination of pregnancy can be performed from 6 to 12 weeks. The main technique for mini-abortion is vacuum aspiration. The fertilized egg is removed from the uterine cavity using a special electric suction. This option for early termination of pregnancy is more gentle than the standard options for surgical abortion.
We must not forget that the sooner have an abortion , the lower the risk of complications.
The procedure takes about 5 minutes and the woman can go home within a few hours after the procedure. The uterine mucosa, unlike curettage, is slightly injured. A contraindication to abortion in this way is the presence of infection in the acute period. After the mini-abortion, a control ultrasound examination of the uterine cavity is performed.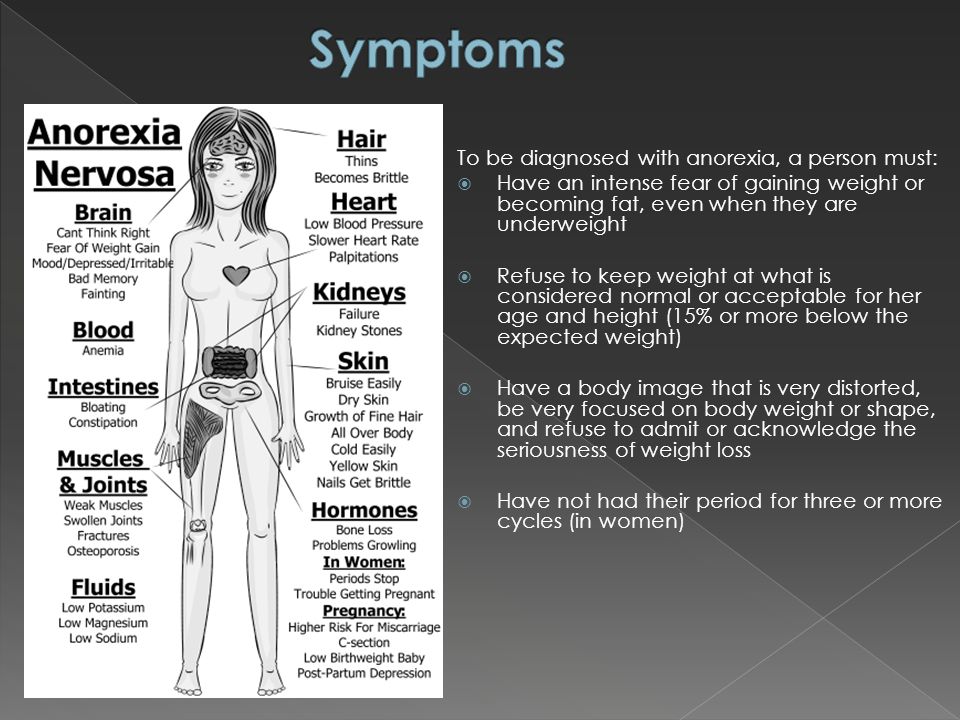
Where to have an abortion?
Many women (especially young women), in order not to advertise their pregnancy, start looking for options, where to have an abortion . It must be remembered that it is most correct to have an abortion in a clinic, under the supervision of specialists, and not with the help of folk remedies.
An abortion made outside the walls of a medical institution that has the right to perform this manipulation is called criminal. A self-performed abortion by untested means can lead to serious consequences. In this case, a woman risks not only the possibility of having children in the future, but also her health.
Medical abortion
Termination of pregnancy by indications or at the request of a woman for a period of 6 to 12 weeks can be performed by curettage of the uterine cavity. This procedure is a surgical procedure and requires preparation. As with any other operation, all the necessary tests are given. Termination of pregnancy is carried out on an empty stomach, as the woman is given anesthesia.
Termination of pregnancy is carried out on an empty stomach, as the woman is given anesthesia.
In the postoperative period during the month you need to refrain from sexual intercourse, do not go to the sauna, bath, bathing in water, it is not recommended to take a bath. All these measures are aimed at preventing infection.
It is also not advisable to overcool, be subjected to excessive stress and physical exertion for some time. It is necessary to give the body a rest, so that in the future there will be no problems with conception.
After the abortion, it is necessary to visit a gynecologist. During the appointment, the doctor will conduct a comprehensive examination with obligatory ultrasound control, as well as select the optimal method of contraception, which will help to avoid unwanted pregnancies in the future, and therefore new abortions. A large number of abortions brings with it a large number of complications that can affect the reproductive potential of a woman.
Psychological support for a woman is also important, both before and after an abortion. The doctor in this case should be not only a competent specialist, but also a sensitive psychologist who can encourage the patient.
A great role is given to conversations with a woman, since she must understand that the doctor is on her side and in no case condemns the perfect act.
Within a month after the abortion, women should monitor their well-being.
If you experience pain, bleeding, fever or other unusual phenomena, you should definitely visit a gynecologist for a comprehensive examination and identify the cause of the symptoms.
Where to have an abortion in Nizhny Novgorod?
Termination of pregnancy in Nizhny Novgorod is performed by experienced specialists at Tonus Medical Center. It is possible to carry out manipulations at various stages of pregnancy. An abortion performed at Tonus Medical Center is a safe procedure carried out by highly qualified doctors who choose an individual approach to each woman and provide reliable medical care.
You can make an appointment at the Center for Obstetrics and Gynecology by calling 8 (831) 411-11-22
Self-administered medical abortion versus provider-led medical abortion (review)
Cochrane Evidence Synthesis and Methods ►
Review question
The purpose of this review was to compare whether self-administered abortion medications without the supervision of a healthcare professional can be as effective and safe as taking these medications in the presence of trained healthcare professionals.
Relevance
Medical abortion to terminate pregnancy has been shown to be successful and safe when women have access to the necessary information and resources. In a provider-led medical abortion, medications are taken in the presence of trained health professionals. Medical abortion drugs became more widely available, allowing women to self-administer the drugs and giving them more control over the abortion procedure.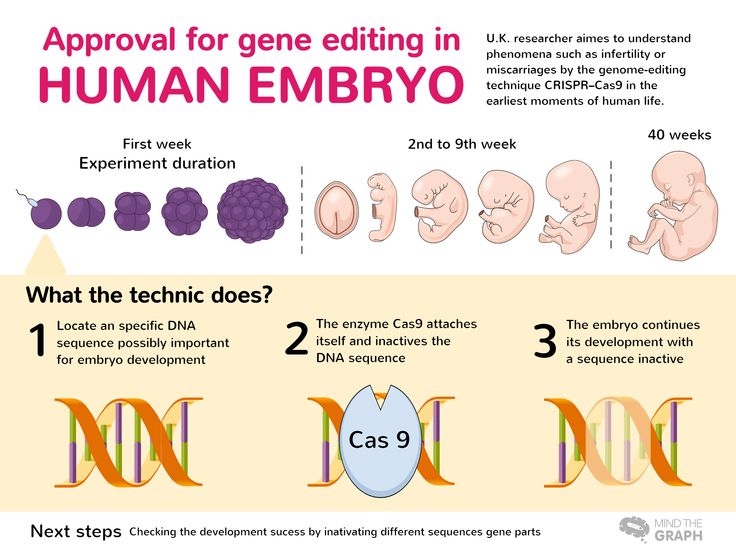 In a self-administered medical abortion, the woman takes the drug(s) without the supervision of a healthcare professional after receiving the necessary information and resources. This is the first review of published evidence on whether self-administration of medical abortion drugs is a safe and successful way to terminate a pregnancy. We compared the success and safety of self-administered medical abortion versus provider-led medical abortion.
In a self-administered medical abortion, the woman takes the drug(s) without the supervision of a healthcare professional after receiving the necessary information and resources. This is the first review of published evidence on whether self-administration of medical abortion drugs is a safe and successful way to terminate a pregnancy. We compared the success and safety of self-administered medical abortion versus provider-led medical abortion.
Study profile
We included 18 studies (two randomized controlled trials and 16 prospective cohort studies) involving 11043 women who had medical abortion in early pregnancy (before nine weeks of pregnancy) in 10 countries. These studies compared self-administered medical abortion with provider-led medical abortion. In both cases, the abortion was performed after the initial visit to the clinic. Most of the studies (16) were conducted in low- or moderate-resource settings, and two studies were conducted in high-resource settings.