Diastasis recti what is it
Diastasis Recti (Abdominal Separation): Symptoms & Treatment
Overview
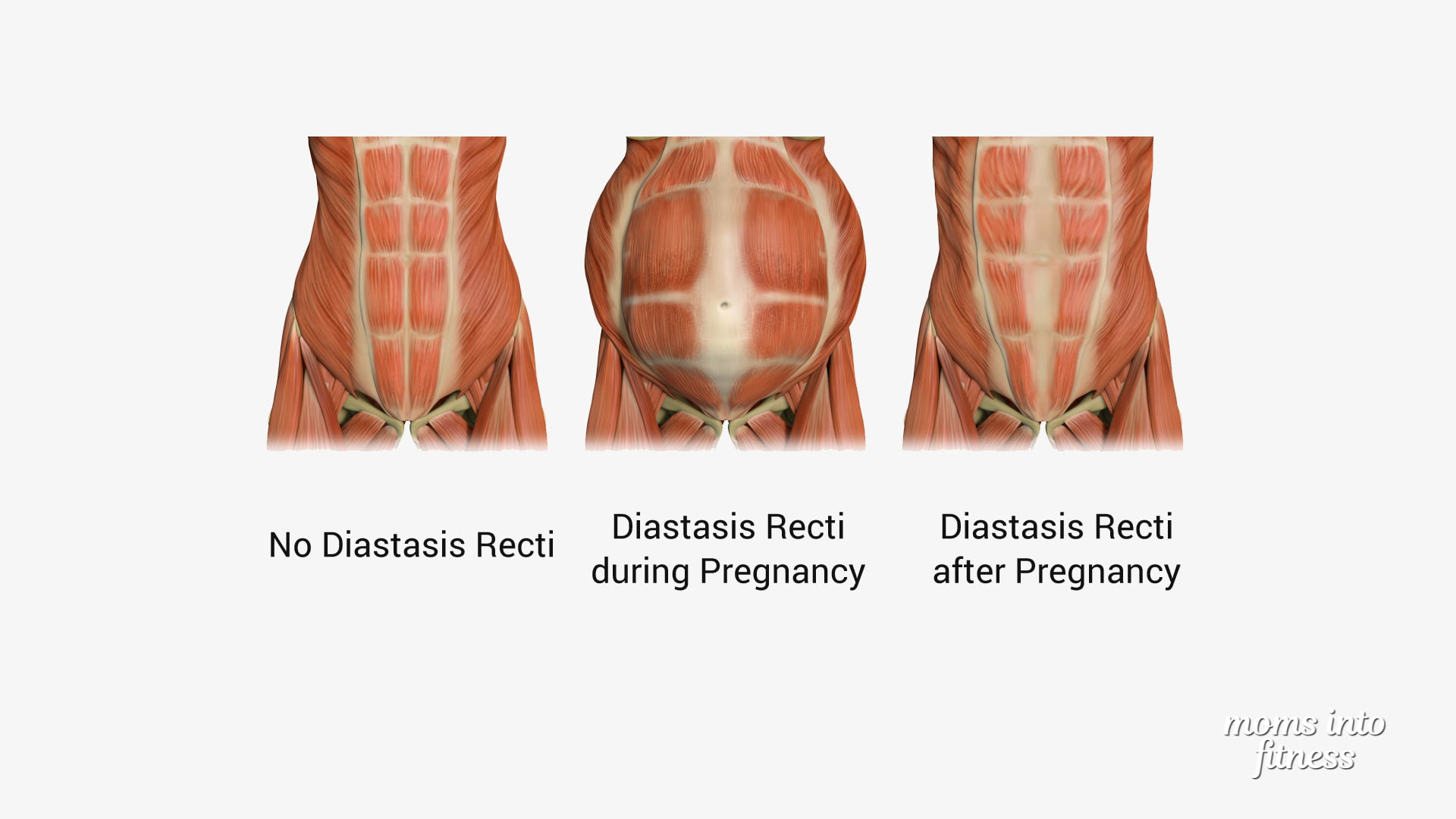
Diastasis recti happens when a person's abdomen stretches during pregnancy and creates a gap in the abdominal muscles.What is diastasis recti?
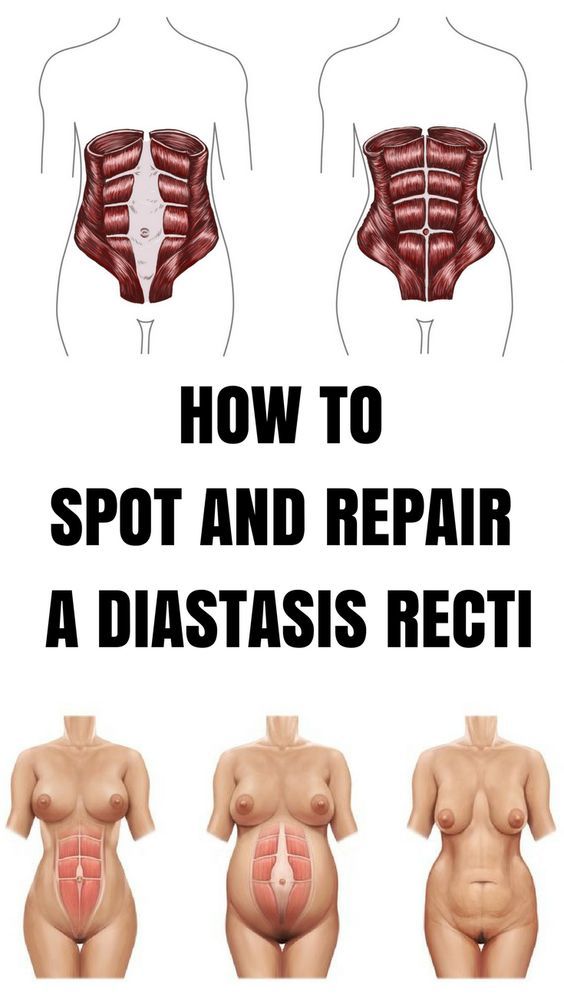
Diastasis recti (diastasis rectus abdominis or diastasis) is the separation of the rectus abdominis muscles during and after pregnancy. The rectus abdominis runs vertically along the front of your stomach. It's frequently referred to as someone's "six-pack abs." It's divided into left and right sides by a band of tissue called the linea alba that runs down the middle. As your uterus expands during pregnancy, the abdominals are stretched and the linea alba thins and pulls apart. This band of tissue gets wider as it's pushed outward.
Once you deliver your baby, the linea alba can heal and come back together. It's highly elastic and retracts backs (like a rubber band). When the tissue loses its elasticity from being overstretched, the gap in the abdominals will not close as much as it should. This is diastasis recti.
If you have diastasis, your belly may appear to stick out just above or below the belly button, making you appear pregnant months or years after giving birth.
Why does diastasis recti happen?
Pregnancy puts a lot of pressure on your abdomen (abs). The abdomen is made up of left and right ab muscles and a thin band of connective tissue (linea alba) in between. They are pushed outward and stretched to make room for the growing baby. Diastasis recti occurs when the linea alba is overstretched and doesn't come back together. The left and right sides of the abdominals stay separated. It's also referred to as an "ab gap" or abdominal separation.
Who gets diastasis recti?
Diastasis recti is most common in pregnant and postpartum women (it can also be seen in men and infants). Diastasis recti usually develops in the third trimester. There is increased pressure on the abdominal wall because the baby is growing quickly during this time. Most people don't notice diastasis recti until the postpartum period.
How common is diastasis recti?
Diastasis recti is extremely common in those who are pregnant and during the postpartum period. It affects 60% of people. It usually resolves itself within eight weeks of delivery. About 40% of those who have diastasis recti still have it by six months postpartum.
Symptoms and Causes
What are the symptoms of diastasis recti?
Most people don't notice signs of diastasis recti until they are postpartum. You can have diastasis recti during pregnancy, but it's hard to distinguish because your abdomen is stretched.
Common signs of diastasis recti during the postpartum period are:
- A visible bulge or "pooch" that protrudes just above or below the belly button.
- Softness or jelly-like feeling around your belly button.
- Coning or doming when you contract your ab muscles.
- Difficulty lifting objects, walking or performing everyday tasks.
- Pain during sex.
- Pelvic or hip pain.
- Low back pain.
- Poor posture.
- Urine leaking when you sneeze or cough.
- Constipation.
- Feeling weak in your abdominals.
What does diastasis recti feel like?
Diastasis recti is not painful. You may feel pain associated with some of the side effects of diastasis, but the ab separation itself doesn't hurt. You may feel weakness in your core when doing once easy tasks, like lifting a laundry basket. Some people feel a jelly-like texture in the space between the left and right abdominals when contracting the ab muscles.
How do I know if I have diastasis recti?
There are some common signs that can signal you have diastasis recti. One of the most common signs of diastasis recti is a bulge in your midsection that doesn't go away, even after exercising or losing weight gained during pregnancy. Another sign is that your belly cones or domes when you lean back on a chair or get up out of bed. You can check for diastasis recti on your own, but it is always a good idea to speak with your healthcare provider about your symptoms.
What are the risk factors for developing diastasis recti?
Several factors can increase your risk for developing diastasis recti:
- Having multiple pregnancies (especially back-to-back).
- Being over 35 years old.
- Having multiples (such as twins or triplets).
- Having a heavy or big baby.
- Being extremely petite.
- Vaginal delivery. Pushing can increase abdominal pressure.
Diagnosis and Tests
How is diastasis recti diagnosed?
Your healthcare provider will evaluate if diastasis is present, where it's located and how severe it is. Diastasis recti can occur above the belly button, below the belly button and at the belly button.
Your provider will use their hands and fingers to feel the abdominal area for gaps and muscle tone. Some providers may use ultrasound, measuring tape or a tool called a caliper for a more accurate measurement. This exam typically occurs at your postpartum appointment before being cleared for exercise.
An abdominal gap wider than 2 centimeters is considered diastasis recti. Diastasis recti is also measured in finger widths, for example, two or three fingers' separation.
Your healthcare provider may recommend movements for diastasis recti or they may refer you to a specialist for additional treatment.
How do I test myself for diastasis recti?
You can test yourself for diastasis recti:
- Lie on your back with your knees bent and feet flat on the floor.
- Lift your shoulders slightly off the ground, keeping one hand behind your head for support. Almost like you are doing a sit-up. Look down at your belly.
- Move your other hand above your belly button area, palms down and fingers towards your toes.
- Use your fingers to feel for a gap between the abs. See how many fingers can fit in the gap between your right and left abdominals.
If you feel a gap of two or more finger widths, discuss your concerns with your healthcare provider. They should confirm diastasis recti with a proper diagnosis and recommend appropriate care.
They should confirm diastasis recti with a proper diagnosis and recommend appropriate care.
Management and Treatment
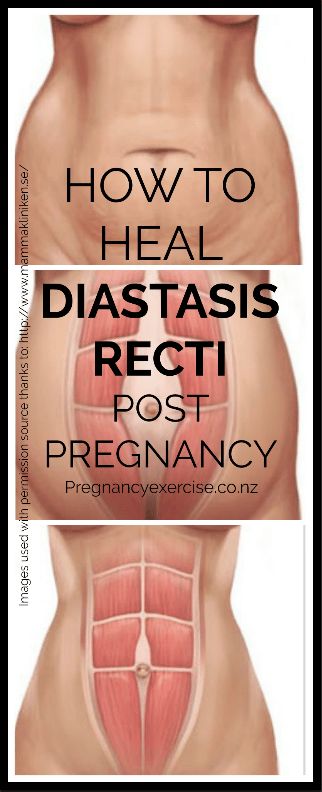
How can I fix diastasis recti?
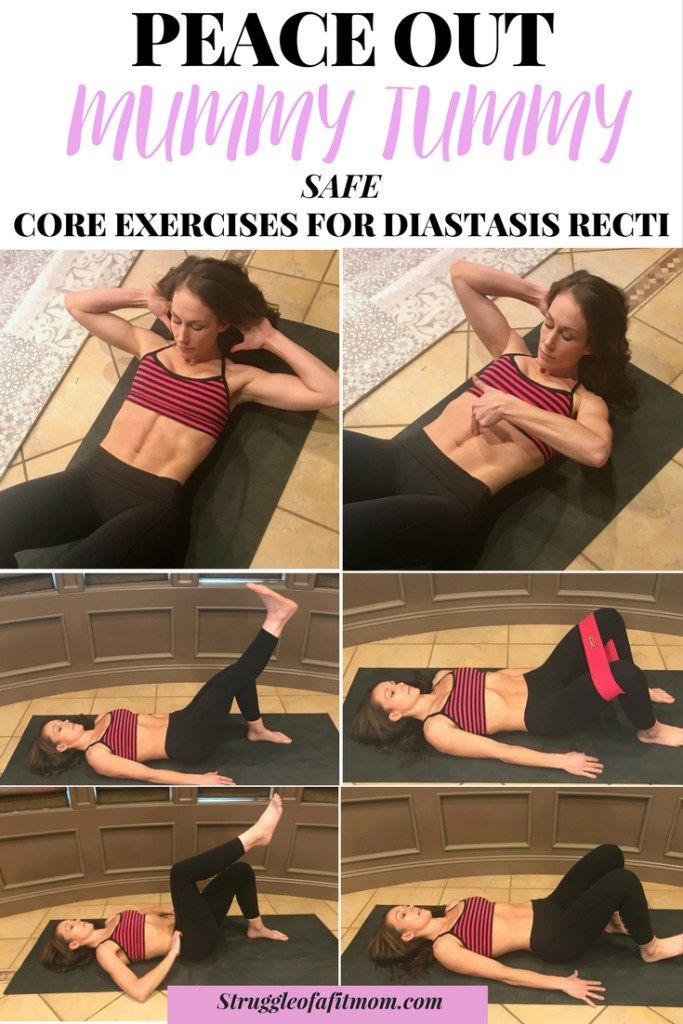
To fix diastasis recti, you'll need to perform gentle movements that engage the abdominal muscles. Before starting an exercise program, be sure it's safe for diastasis recti. Work with a fitness professional or physical therapist who has experience with diastasis recti. They can create a treatment plan to make sure you are performing the movements correctly and progressing to more challenging movements at the right time.
Certain movements will make abdominal separation worse. During the postpartum period, there are some modifications you should make:
- Avoid lifting anything heavier than your baby.
- Roll onto your side when getting out of bed or sitting up. Use your arms to push yourself up.
- Skip activities and movements that push your abdominals outward (like crunches and sit-ups).
Some people use binding devices (elastic belly bands) to help hold their belly in and support the lower back. Wearing binders can't heal diastasis recti and will not strengthen your core muscles. It can be a good reminder of your diastasis recti and promote good posture.
Wearing binders can't heal diastasis recti and will not strengthen your core muscles. It can be a good reminder of your diastasis recti and promote good posture.
Can you fix diastasis recti without surgery?
Yes, it's possible to fix diastasis recti without surgery. Surgery is rarely performed to fix diastasis recti. Healthcare providers will recommend physical therapy or at-home exercises to help heal diastasis before surgical methods. Surgery is performed in cases of hernia (when an organ pushes through the linea alba) or if a woman wants diastasis recti surgery (a tummy tuck).
What are the best exercises for diastasis recti?
The best exercises for diastasis recti are those that engage the deep abdominals. Most diastasis recti exercises involve deep breathing and slow, controlled movements. Unfortunately, many of the most common ab exercises (like crunches) can worsen your diastasis. Before starting abdominal exercises, ask your healthcare provider to check you for diastasis recti.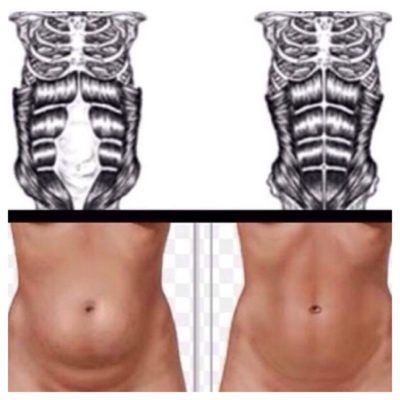
What movements make diastasis recti worse?
Any movement that bulges the abdominal wall forward can cause more damage to your diastasis recti. Everyday movements like getting out of bed or up off a chair can worsen diastasis. Try to be mindful about how you are using your abdominals as you go about your day.
These exercise movements should be avoided if you have diastasis recti:
- Crunches or sit-ups of any kind.
- Planks or push-ups (unless using modifications).
- Downward dog, boat pose and other yoga poses.
- Double leg lifts, scissors and other Pilates moves.
- Any exercise that causes your abdominals to bulge, cone or dome.
Prevention
How do I prevent diastasis recti?
Some abdominal separation is normal and expected with pregnancy. There are some things you can do to lower your risk for developing diastasis recti:
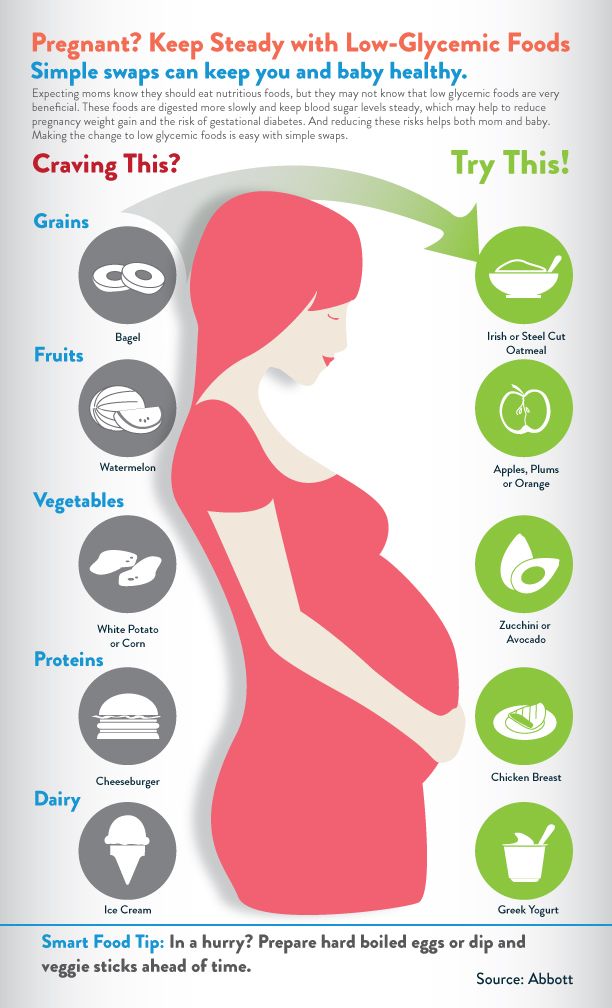
- Healthy weight gain during pregnancy: Exercising and eating healthy foods to keep weight gain within a healthy range.
- Proper posture and deep breathing: Stand up straight with your shoulders back. Take deep breaths that allow your ribs to expand and not just your belly.
- Safe core exercises: Avoid exercises like sit-ups and crunches that put pressure on your abdominals after 12 weeks of pregnancy and postpartum.
- Don't strain while lifting: Certain day-to-day activities like lifting grocery bags or your children can put undue strain on your abdominals.
- Log roll when getting out of bed: If you're pregnant or postpartum, roll to one side and use your arms to push up out of bed.
Outlook / Prognosis
How long will it take to heal my diastasis recti?
The amount of time it takes to heal diastasis recti depends on the amount of ab separation and how consistent you are with strengthening exercises. After several weeks postpartum, this gap will start to close as your muscles regain strength.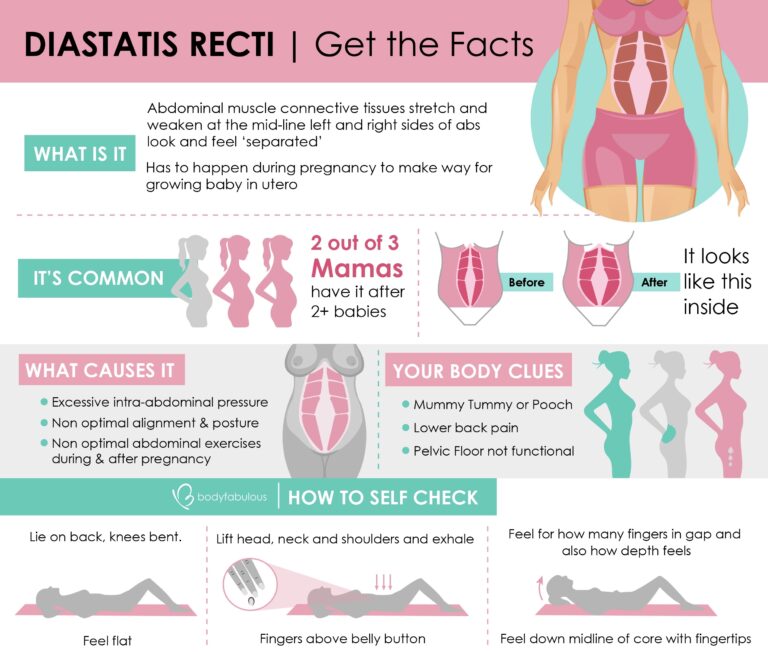 If you're making modifications to your lifestyle and performing exercises with good form, you're more likely to notice progress.
If you're making modifications to your lifestyle and performing exercises with good form, you're more likely to notice progress.
Can I get diastasis recti again?
Yes, you can heal your diastasis recti and get it again. Your risk for diastasis recti increases the more times you are pregnant. Think of the linea alba as a rubber band that is continuously stretched. Over time, the rubber band will lose its elasticity. The linea alba may not regain its original shape or form after being stretched through multiple pregnancies.
Is it too late to fix my diastasis recti?
It's never too late to repair your diastasis recti. With the proper exercises, you can fix your ab separation years after you've delivered your last baby.
Are there complications from diastasis recti?
If left untreated or in severe cases of diastasis recti, complications can include:
- Umbilical hernia.
- Increase in back pain.
- Pain during sex.
- Urinary incontinence.
- Pelvic and hip pain.
Living With
When should I see my healthcare provider?
Diastasis recti is a common and easily treated condition. If you have more than a two-finger gap between your abdominals or are experiencing pain, contact your healthcare provider for a diagnosis. They may want you to see a physical therapist or pelvic floor specialist to help strengthen your abdominal muscles.
A note from Cleveland Clinic:
Diastasis recti can make you appear pregnant years after your last baby. Discuss your concerns with your healthcare provider so they can diagnose and treat you. Getting treatment can help you feel more confident in your body and correct any pain you are experiencing.
Diastasis Recti (Abdominal Separation): Symptoms & Treatment
Overview
Diastasis recti happens when a person's abdomen stretches during pregnancy and creates a gap in the abdominal muscles.What is diastasis recti?
Diastasis recti (diastasis rectus abdominis or diastasis) is the separation of the rectus abdominis muscles during and after pregnancy. The rectus abdominis runs vertically along the front of your stomach. It's frequently referred to as someone's "six-pack abs." It's divided into left and right sides by a band of tissue called the linea alba that runs down the middle. As your uterus expands during pregnancy, the abdominals are stretched and the linea alba thins and pulls apart. This band of tissue gets wider as it's pushed outward.
The rectus abdominis runs vertically along the front of your stomach. It's frequently referred to as someone's "six-pack abs." It's divided into left and right sides by a band of tissue called the linea alba that runs down the middle. As your uterus expands during pregnancy, the abdominals are stretched and the linea alba thins and pulls apart. This band of tissue gets wider as it's pushed outward.
Once you deliver your baby, the linea alba can heal and come back together. It's highly elastic and retracts backs (like a rubber band). When the tissue loses its elasticity from being overstretched, the gap in the abdominals will not close as much as it should. This is diastasis recti.
If you have diastasis, your belly may appear to stick out just above or below the belly button, making you appear pregnant months or years after giving birth.
Why does diastasis recti happen?
Pregnancy puts a lot of pressure on your abdomen (abs). The abdomen is made up of left and right ab muscles and a thin band of connective tissue (linea alba) in between. They are pushed outward and stretched to make room for the growing baby. Diastasis recti occurs when the linea alba is overstretched and doesn't come back together. The left and right sides of the abdominals stay separated. It's also referred to as an "ab gap" or abdominal separation.
They are pushed outward and stretched to make room for the growing baby. Diastasis recti occurs when the linea alba is overstretched and doesn't come back together. The left and right sides of the abdominals stay separated. It's also referred to as an "ab gap" or abdominal separation.
Who gets diastasis recti?
Diastasis recti is most common in pregnant and postpartum women (it can also be seen in men and infants). Diastasis recti usually develops in the third trimester. There is increased pressure on the abdominal wall because the baby is growing quickly during this time. Most people don't notice diastasis recti until the postpartum period.
How common is diastasis recti?
Diastasis recti is extremely common in those who are pregnant and during the postpartum period. It affects 60% of people. It usually resolves itself within eight weeks of delivery. About 40% of those who have diastasis recti still have it by six months postpartum.
Symptoms and Causes
What are the symptoms of diastasis recti?
Most people don't notice signs of diastasis recti until they are postpartum.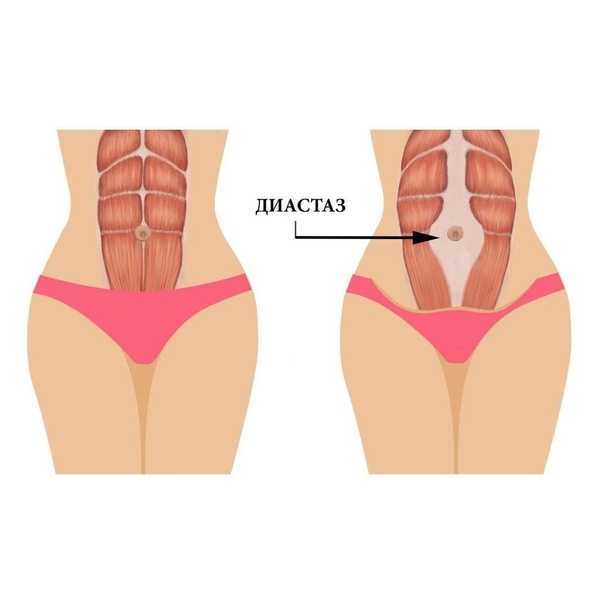 You can have diastasis recti during pregnancy, but it's hard to distinguish because your abdomen is stretched.
You can have diastasis recti during pregnancy, but it's hard to distinguish because your abdomen is stretched.
Common signs of diastasis recti during the postpartum period are:
- A visible bulge or "pooch" that protrudes just above or below the belly button.
- Softness or jelly-like feeling around your belly button.
- Coning or doming when you contract your ab muscles.
- Difficulty lifting objects, walking or performing everyday tasks.
- Pain during sex.
- Pelvic or hip pain.
- Low back pain.
- Poor posture.
- Urine leaking when you sneeze or cough.
- Constipation.
- Feeling weak in your abdominals.
What does diastasis recti feel like?
Diastasis recti is not painful. You may feel pain associated with some of the side effects of diastasis, but the ab separation itself doesn't hurt. You may feel weakness in your core when doing once easy tasks, like lifting a laundry basket. Some people feel a jelly-like texture in the space between the left and right abdominals when contracting the ab muscles.
How do I know if I have diastasis recti?
There are some common signs that can signal you have diastasis recti. One of the most common signs of diastasis recti is a bulge in your midsection that doesn't go away, even after exercising or losing weight gained during pregnancy. Another sign is that your belly cones or domes when you lean back on a chair or get up out of bed. You can check for diastasis recti on your own, but it is always a good idea to speak with your healthcare provider about your symptoms.
What are the risk factors for developing diastasis recti?
Several factors can increase your risk for developing diastasis recti:
- Having multiple pregnancies (especially back-to-back).
- Being over 35 years old.
- Having multiples (such as twins or triplets).
- Having a heavy or big baby.
- Being extremely petite.
- Vaginal delivery. Pushing can increase abdominal pressure.
Diagnosis and Tests
How is diastasis recti diagnosed?
Your healthcare provider will evaluate if diastasis is present, where it's located and how severe it is. Diastasis recti can occur above the belly button, below the belly button and at the belly button.
Diastasis recti can occur above the belly button, below the belly button and at the belly button.
Your provider will use their hands and fingers to feel the abdominal area for gaps and muscle tone. Some providers may use ultrasound, measuring tape or a tool called a caliper for a more accurate measurement. This exam typically occurs at your postpartum appointment before being cleared for exercise.
An abdominal gap wider than 2 centimeters is considered diastasis recti. Diastasis recti is also measured in finger widths, for example, two or three fingers' separation.
Your healthcare provider may recommend movements for diastasis recti or they may refer you to a specialist for additional treatment.
How do I test myself for diastasis recti?
You can test yourself for diastasis recti:
- Lie on your back with your knees bent and feet flat on the floor.
- Lift your shoulders slightly off the ground, keeping one hand behind your head for support. Almost like you are doing a sit-up.
 Look down at your belly.
Look down at your belly. - Move your other hand above your belly button area, palms down and fingers towards your toes.
- Use your fingers to feel for a gap between the abs. See how many fingers can fit in the gap between your right and left abdominals.
If you feel a gap of two or more finger widths, discuss your concerns with your healthcare provider. They should confirm diastasis recti with a proper diagnosis and recommend appropriate care.
Management and Treatment
How can I fix diastasis recti?
To fix diastasis recti, you'll need to perform gentle movements that engage the abdominal muscles. Before starting an exercise program, be sure it's safe for diastasis recti. Work with a fitness professional or physical therapist who has experience with diastasis recti. They can create a treatment plan to make sure you are performing the movements correctly and progressing to more challenging movements at the right time.
Certain movements will make abdominal separation worse.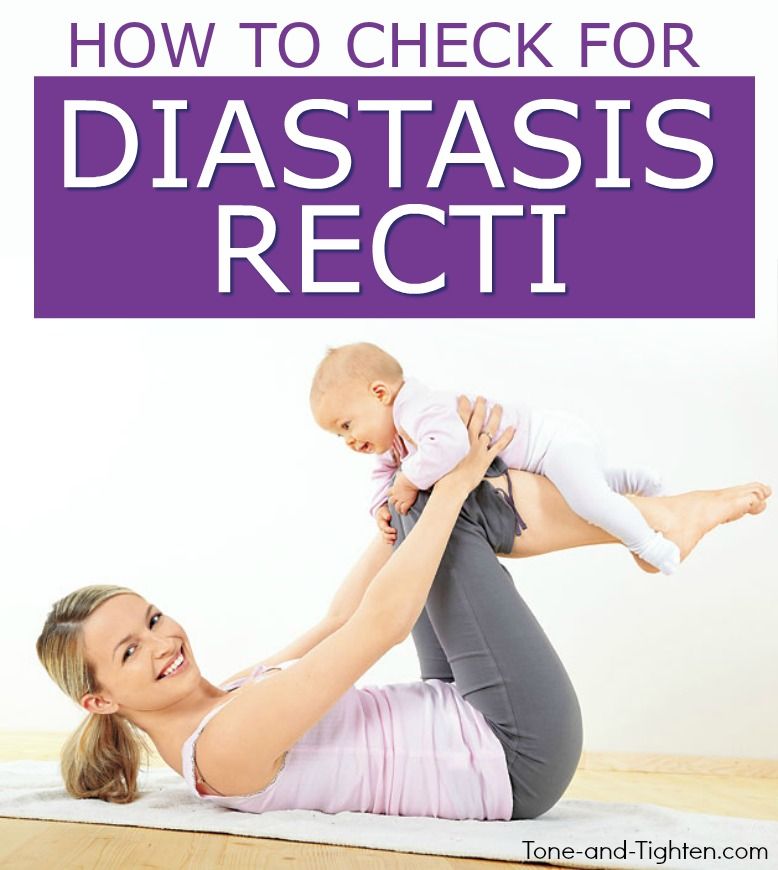 During the postpartum period, there are some modifications you should make:
During the postpartum period, there are some modifications you should make:
- Avoid lifting anything heavier than your baby.
- Roll onto your side when getting out of bed or sitting up. Use your arms to push yourself up.
- Skip activities and movements that push your abdominals outward (like crunches and sit-ups).
Some people use binding devices (elastic belly bands) to help hold their belly in and support the lower back. Wearing binders can't heal diastasis recti and will not strengthen your core muscles. It can be a good reminder of your diastasis recti and promote good posture.
Can you fix diastasis recti without surgery?
Yes, it's possible to fix diastasis recti without surgery. Surgery is rarely performed to fix diastasis recti. Healthcare providers will recommend physical therapy or at-home exercises to help heal diastasis before surgical methods. Surgery is performed in cases of hernia (when an organ pushes through the linea alba) or if a woman wants diastasis recti surgery (a tummy tuck).
What are the best exercises for diastasis recti?
The best exercises for diastasis recti are those that engage the deep abdominals. Most diastasis recti exercises involve deep breathing and slow, controlled movements. Unfortunately, many of the most common ab exercises (like crunches) can worsen your diastasis. Before starting abdominal exercises, ask your healthcare provider to check you for diastasis recti.
What movements make diastasis recti worse?
Any movement that bulges the abdominal wall forward can cause more damage to your diastasis recti. Everyday movements like getting out of bed or up off a chair can worsen diastasis. Try to be mindful about how you are using your abdominals as you go about your day.
These exercise movements should be avoided if you have diastasis recti:
- Crunches or sit-ups of any kind.
- Planks or push-ups (unless using modifications).
- Downward dog, boat pose and other yoga poses.
- Double leg lifts, scissors and other Pilates moves.
- Any exercise that causes your abdominals to bulge, cone or dome.
Prevention
How do I prevent diastasis recti?
Some abdominal separation is normal and expected with pregnancy. There are some things you can do to lower your risk for developing diastasis recti:
- Healthy weight gain during pregnancy: Exercising and eating healthy foods to keep weight gain within a healthy range.
- Proper posture and deep breathing: Stand up straight with your shoulders back. Take deep breaths that allow your ribs to expand and not just your belly.
- Safe core exercises: Avoid exercises like sit-ups and crunches that put pressure on your abdominals after 12 weeks of pregnancy and postpartum.
- Don't strain while lifting: Certain day-to-day activities like lifting grocery bags or your children can put undue strain on your abdominals.
- Log roll when getting out of bed: If you're pregnant or postpartum, roll to one side and use your arms to push up out of bed.

Outlook / Prognosis
How long will it take to heal my diastasis recti?
The amount of time it takes to heal diastasis recti depends on the amount of ab separation and how consistent you are with strengthening exercises. After several weeks postpartum, this gap will start to close as your muscles regain strength. If you're making modifications to your lifestyle and performing exercises with good form, you're more likely to notice progress.
Can I get diastasis recti again?
Yes, you can heal your diastasis recti and get it again. Your risk for diastasis recti increases the more times you are pregnant. Think of the linea alba as a rubber band that is continuously stretched. Over time, the rubber band will lose its elasticity. The linea alba may not regain its original shape or form after being stretched through multiple pregnancies.
Is it too late to fix my diastasis recti?
It's never too late to repair your diastasis recti. With the proper exercises, you can fix your ab separation years after you've delivered your last baby.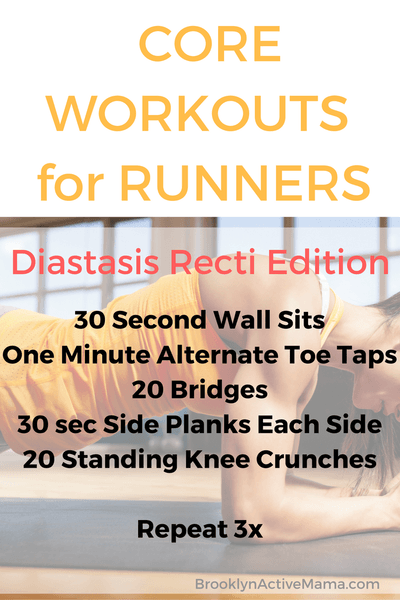
Are there complications from diastasis recti?
If left untreated or in severe cases of diastasis recti, complications can include:
- Umbilical hernia.
- Increase in back pain.
- Pain during sex.
- Urinary incontinence.
- Pelvic and hip pain.
Living With
When should I see my healthcare provider?
Diastasis recti is a common and easily treated condition. If you have more than a two-finger gap between your abdominals or are experiencing pain, contact your healthcare provider for a diagnosis. They may want you to see a physical therapist or pelvic floor specialist to help strengthen your abdominal muscles.
A note from Cleveland Clinic:
Diastasis recti can make you appear pregnant years after your last baby. Discuss your concerns with your healthcare provider so they can diagnose and treat you. Getting treatment can help you feel more confident in your body and correct any pain you are experiencing.
Diastasis of the rectus abdominis muscles - symptoms, signs, degrees, causes and treatment in men and women in Moscow in the "SM-Clinic"
The surgeon deals with the treatment of this disease
Book online Request a call
- What is diastasis rectus abdominis?
- About disease
- Species
- Symptoms of diastasis recti
- Causes of diastasis recti
- Diagnostics of diastasis of the rectus abdominis muscles
- Expert opinion
- Treatment of diastasis recti
- Surgical treatment of diastasis recti
- Prophylaxis
- Rehabilitation after surgery
- Questions and answers
- Sources
About the disease
The disease is based on stretching and expansion of the white line of the abdomen - a tendon that is located between the rectus muscles, connects and holds them. This is a strip of connective tissue, consisting of several layers, located in the middle of the abdomen vertically from the xiphoid process to the pubic joint.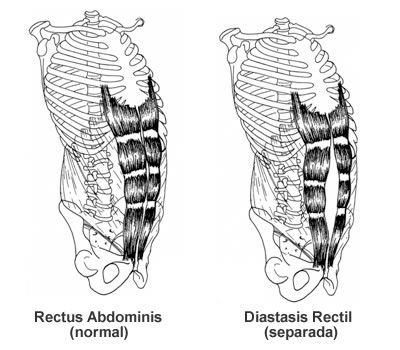 nine0003
nine0003
Due to an increase in intra-abdominal pressure or a violation of the properties of the connective fibers, the structure of the tendon changes, it weakens, becomes thinner and stretches. The trigger mechanism is prolonged pressure on the abdominal wall associated with pregnancy or visceral obesity. An aggravating factor is the loosening of the white line against the background of collagenopathy, the effects of relaxin, the immaturity of cellular structures, etc.
As a result, the white line becomes thinner and stretched. Normally, its dimensions are restored with a gradual decrease in the abdomen or as the properties of the connective tissue normalize. Thus, physiological diastasis is eliminated during the neonatal period or in women after childbirth. nine0003
If abdominal training is started early in the postpartum period, this leads to a contraction of the rectus muscles and a simultaneous increase in intra-abdominal pressure, and the white line is fixed in a stretched position and does not hold the internal organs well. As a result, unaesthetic vertical folds form on the abdomen, a rounded protrusion appears, dysfunction of the digestive tract occurs and the risk of hernia formation increases.
As a result, unaesthetic vertical folds form on the abdomen, a rounded protrusion appears, dysfunction of the digestive tract occurs and the risk of hernia formation increases.
Species
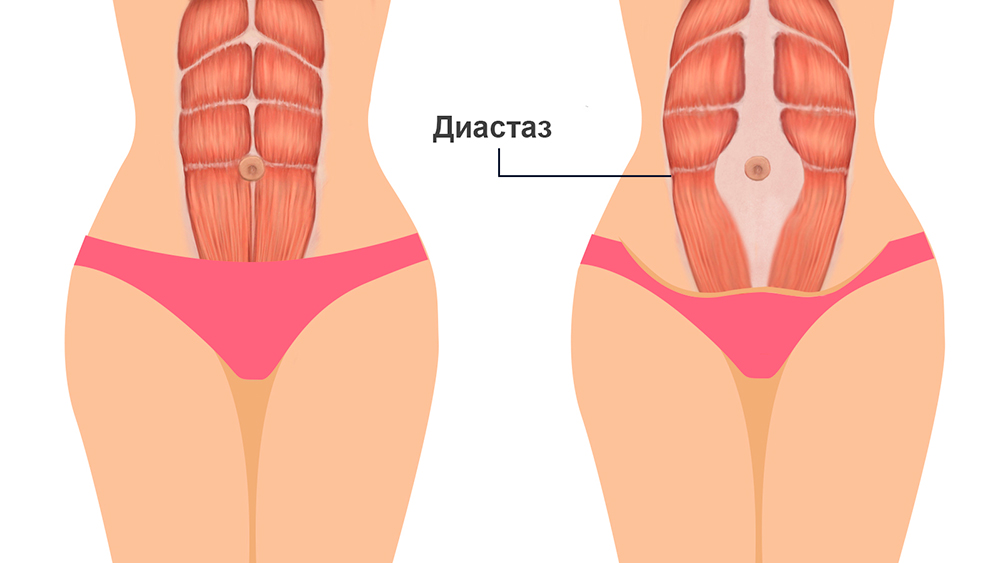
Depending on the magnitude of the stretching of the tendon ligament, there are 3 degrees of diastasis of the rectus abdominis muscles:
- first - the muscles move away from each other by 2.5-5 cm;
- second - ligaments diverge by 5-8 cm;
- third - the line is stretched more than 8 cm.
According to the localization of the place of maximum stretching, supra-umbilical, sub-umbilical and mixed forms of diastasis are distinguished.
According to the degree of involvement of other muscles of the anterior abdominal wall, the pathology is classified into types:
- A - classical divergence of muscles after natural childbirth; nine0008
- B - relaxation of the lower lateral sections of the muscles;
- C - expansion affects the region of the ribs and the xiphoid process;
- D - diastasis is combined with a curvature of the waist line.
Symptoms of diastasis of the rectus abdominis muscles
Manifestations of BPMD increase as the pathology progresses. In women, a vivid clinical picture manifests itself abruptly (shortly after childbirth), while in men the disease develops gradually.
At the onset of the disease, there may be no symptoms at all. The patient then notices a characteristic rounded vertical protrusion in the center of the abdomen. With deliberate tension of the press, the inner edges of the rectus muscles and the groove between them are clearly visible. Due to muscle dysfunction, pain in the spine, lower back, fatigue, and posture disorders are possible.
With the progression of the pathology, manifestations of dysfunction of the gastrointestinal tract join:
- heartburn; nine0007 belching;
- flatulence;
- abdominal pain;
- constipation.
In the third stage of diastasis, patients are faced with the formation of hernias, which are formed due to structural defects in the white line. Possible ptosis (omission) of internal organs and serious disturbances in the work of the intestines (in severe cases, intestinal obstruction develops). Women often experience urinary incontinence, renal colic.
Possible ptosis (omission) of internal organs and serious disturbances in the work of the intestines (in severe cases, intestinal obstruction develops). Women often experience urinary incontinence, renal colic.
Causes of diastasis recti
Increase the risk of diastasis, connective tissue pathology and increased pressure in the abdominal cavity. In different categories of patients, the causes of the development of PMSD are different.
Divergence of muscles in children is due to the failure of the musculature and tendons. After 2-12 months after birth, the muscles come into tone, the ligaments and tendons are strengthened - the process resolves itself. In premature babies and infants with intrauterine developmental pathologies, this may take longer. With Down syndrome, there is a risk of maintaining diastasis for life. nine0003
Pregnancy is the provocateur of diastasis of the rectus abdominis muscles in women. The growing uterus puts considerable pressure on the linea alba, stretching it.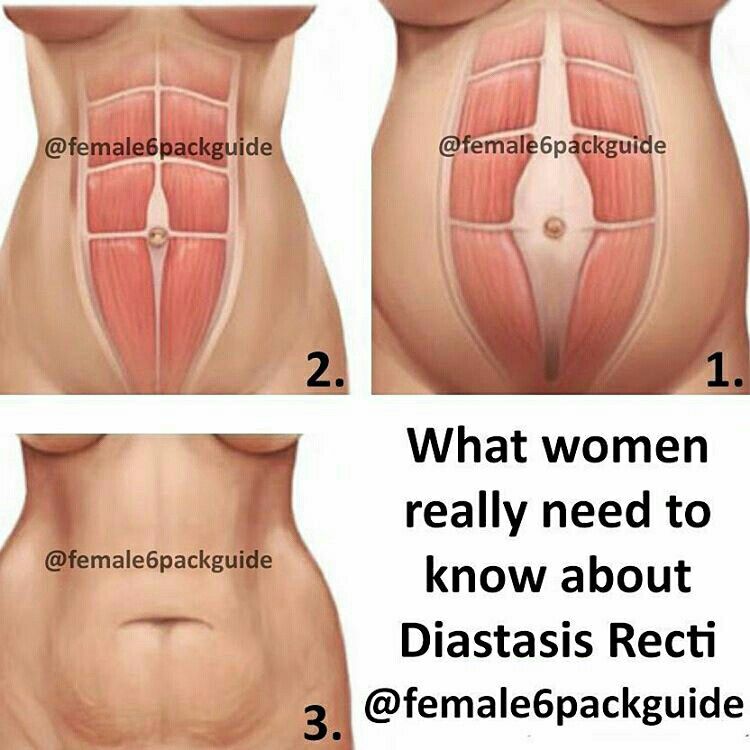 Under the action of hormones, the synthesis of collagen fibers is inhibited, the ligaments become looser. But a few months after the birth, the white line of the abdomen is normally restored.
Under the action of hormones, the synthesis of collagen fibers is inhibited, the ligaments become looser. But a few months after the birth, the white line of the abdomen is normally restored.
In men, BMD is often provoked by obesity, physical activity and hereditary collagenopathies. The risk of diastasis increases with a tendency to constipation, as well as with chronic respiratory diseases accompanied by coughing. nine0003
Treatment of pathology by conservative methods is possible with a small diastasis. At the later stages of development, the pathological divergence of muscles is eliminated with the help of abdominal plastic surgery.
Get advice
If you experience these symptoms, we recommend that you make an appointment with your doctor. Timely consultation will prevent negative consequences for your health.
You can find out more about the disease, prices for treatment and sign up for a consultation with a specialist by phone:
+7 (495) 292-39-72
Request a call back Book online
Why SM-Clinic?
1
Treatment is carried out in accordance with clinical recommendations
2
A comprehensive assessment of the nature of the disease and treatment forecast
3
Modern diagnostic equipment and own laboratory
4
High level of service and weighted pricing policy
Diagnosis of diastasis of the rectus abdominis muscles
Identification of BPMD is not difficult, since the disease has characteristic clinical manifestations.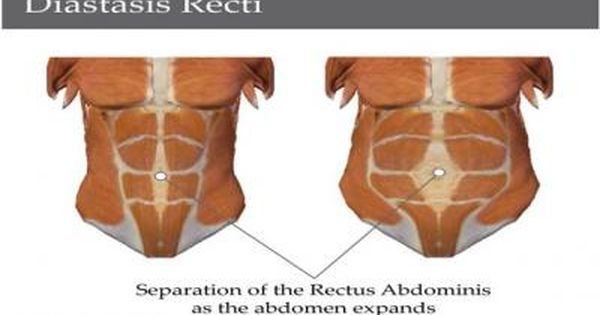 With signs of diastasis, you should contact the surgeon.
With signs of diastasis, you should contact the surgeon.
An increase in the space between the rectus muscles is determined during palpation of the abdomen. To conduct the test, the patient is asked to lie on his back, legs slightly bent at the knees, and then tighten the abdominal muscles, raising his head and shoulder blades. In patients with obesity, the doctor is not always able to fully explore the width of the white line. nine0003
The exact size of the stretch is determined by ultrasound. This diagnostic method also allows you to detect complications (hernia, displacement of internal organs). In order to differentiate the symptoms of diastasis and manifestations of chronic diseases of the gastrointestinal tract or the genitourinary system, consultations of specialized specialists are prescribed.
Expert opinion
Surgeons warn that diastasis of the rectus abdominis muscles is asymptomatic for a long time. Therefore, in the presence of predisposing factors (recent pregnancy and childbirth, chronic constipation, obesity) or non-specific complaints, you should independently feel the white line of the abdomen in the navel. If the distance between the rectus muscles is more than 2.5 cm, contact the surgeon. Also, do not delay the visit in any doubtful cases. Only a doctor can establish the correct diagnosis, self-examination does not exclude the need for an in-person consultation. nine0003
If the distance between the rectus muscles is more than 2.5 cm, contact the surgeon. Also, do not delay the visit in any doubtful cases. Only a doctor can establish the correct diagnosis, self-examination does not exclude the need for an in-person consultation. nine0003
Egiev Valery Nikolaevich, surgeon, oncologist, doctor of medical sciences, professor, head of the Department of Surgery and Oncology, FPC MR MI RUDN University
Treatment of diastasis recti
Functional diastasis in newborns and puerperas does not require treatment. Doctors use expectant tactics, recommend adhering to the principles of rational nutrition, doing massages, and doing gymnastics. The observation period can last up to 12 months. If after this time the problem persists, the surgeon decides on an operative method of correction. nine0003
Conservative treatment
Patients are prescribed a diet to prevent constipation and excessive gas formation, as well as to gradually reduce weight.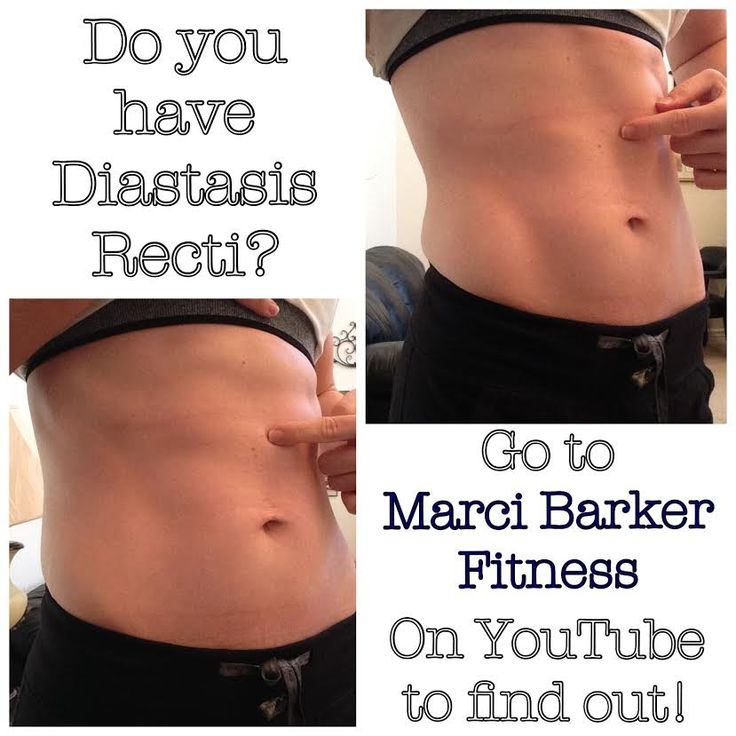 In the postpartum period, incl. after a caesarean section, women are advised to wear a bandage, support the stomach during sneezing and coughing. The general strengthening of the muscles allows you to quickly restore the tone of the anterior abdominal wall, so patients are prescribed exercise therapy, swimming, yoga classes. It is important to exclude any training of the abdominal muscles. You can not perform exercises in the knee-elbow position, as well as in the emphasis (bar). Such loads can be resumed after the restoration of the size of the white line. Conservative treatment is effective only at the 1st stage of BPMD. nine0003
In the postpartum period, incl. after a caesarean section, women are advised to wear a bandage, support the stomach during sneezing and coughing. The general strengthening of the muscles allows you to quickly restore the tone of the anterior abdominal wall, so patients are prescribed exercise therapy, swimming, yoga classes. It is important to exclude any training of the abdominal muscles. You can not perform exercises in the knee-elbow position, as well as in the emphasis (bar). Such loads can be resumed after the restoration of the size of the white line. Conservative treatment is effective only at the 1st stage of BPMD. nine0003
Surgical treatment of diastasis of the rectus abdominis muscles
In case of complicated and uncomplicated diastasis of the rectus abdominis muscles of the 2-3rd degree, surgical treatment is indicated. It is possible to use the following surgical techniques:
- Tension plastic using own tissues. It involves stitching the edges of the muscles with the removal of excess connective tissue.
 To date, it is not used due to the high risk of recurrence.
To date, it is not used due to the high risk of recurrence. - Tension-free repair with a mesh prosthesis. It implies the introduction of an endoprosthesis under the site of stretching. nine0008
- Tension plasty with prosthesis installation. It involves the removal of excess connective tissue, suturing the edges of the muscles and strengthening the zone with a polypropylene mesh.
- Combined technique. Includes muscle suturing, mesh strengthening, removal of excess adipose tissue and stretched skin.
Prevention
To reduce the risk of developing diastasis rectus abdominis, you should keep your body in shape - engage in regular exercise, train your muscles. However, do not overdo it: lifting weights can, on the contrary, become the main cause of muscle divergence. nine0003
It is also important to eat a complete and balanced diet - a lack of nutrients will lead to a decrease in the elasticity of the connective tissue.
It is necessary to control your weight - body mass index should not exceed 26 kg/m3. Obesity, especially of the abdominal type, is an important risk factor for BLV.
Obesity, especially of the abdominal type, is an important risk factor for BLV.
Prevention and timely treatment of chronic lung diseases accompanied by cough, pathologies of the digestive system, occurring with constipation, will reduce the possibility of increasing intra-abdominal pressure and, as a result, the likelihood of diastasis. nine0003
Rehabilitation after surgery
After surgery, the patient is under inpatient observation, receiving analgesic and antibiotic therapy. Full recovery lasts 1-3 months. During this period, the patient is prescribed a diet to normalize defecation, it is recommended to avoid significant physical exertion, weight lifting. To prevent excess tension, it is necessary to wear a bandage.
Questions and answers
A surgeon deals with the treatment of pathology. nine0003
In the stronger sex, obesity and connective tissue dysplasia are considered to be the main cause of BMD. Sharp weight loss or weight gain, excessive passion for power loads are capable of provoking muscle divergence.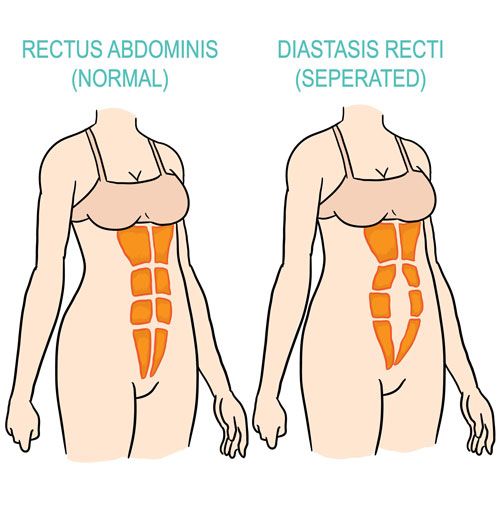 If a man or close relatives have hernias, varicose veins, valgus flat feet, hemorrhoids, this is regarded as an increased tendency to PMSD.
If a man or close relatives have hernias, varicose veins, valgus flat feet, hemorrhoids, this is regarded as an increased tendency to PMSD.
There is no need to rush in this matter. Just the desire to quickly get in shape is the main reason for the progression of diastasis in women. Physical activity can be resumed 1-2 months after delivery. You can start with hiking or yoga. Abdominal exercises can be performed soon after the white line is reduced to 2 cm. It is advisable to pay attention to the diet. A smooth decrease in weight and volume of visceral fat will ensure gradual and timely muscle contraction. Sharp weight loss, on the contrary, can increase diastasis. nine0003
You can lie on a hard surface on your back, tense your abs. With gentle movements of the fingers, you should begin to probe the stomach in the middle in the navel. With a normal width of the white line and with diastasis, a depression will be found - this is the median ligament. If its width is equal to or greater than the width of two fingers, you should contact the surgeon.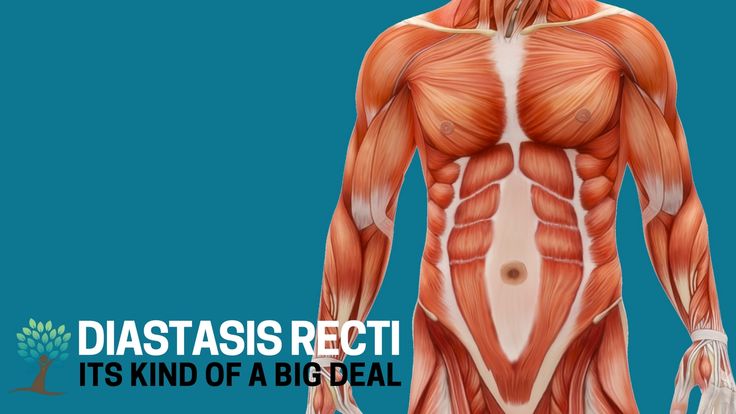 Constipation, bloating and abdominal pain should be alarming. If there are such symptoms, it is necessary to get to the surgeon in the near future.
Constipation, bloating and abdominal pain should be alarming. If there are such symptoms, it is necessary to get to the surgeon in the near future.
Pathogenesis and treatment of ventral hernias and diastasis of the rectus abdominis muscles: Abstract of the thesis / Zagirov U.Z. - nineteen95.
Comparative aspects of methods for eliminating diastasis of the rectus abdominis muscles / Topchiev MA, Bondarev VA, Elderov S.Sh.// Astrakhan medical journal. - 2010.
Jessen M. L., Öberg S., Rosenberg J. Treatment Options for Abdominal Rectus Diastasis // Front Surg. - 2019. - No. 6. - R. 65
>
Surgeon Referral Diseases
Brodie's Abscess soft tissue abscess liver abscess Appendicitis ascites Atheroma femoral hernia Crohn's disease Gangrene soft tissue hematoma Giant cell tumor of bone Hygroma festering wounds Hernia Hernia of the white line of the abdomen hiatal hernia Intestinal diverticulosis Cholelithiasis Keratoma liver cyst pancreatic cyst salivary gland cyst Neck cyst Lipoma Mechanical jaundice Bowel obstruction Oleogranuloma kidney tumor Acute pancreatitis Pancreatic necrosis Inguinal hernia Peritonitis Barrett's esophagus Postoperative hernia Umbilical hernia Cancer of the extrahepatic bile ducts Stomach cancer gallbladder cancer bowel cancer adrenal cancer Parathyroid Cancer Liver cancer Esophageal carcinoma colon cancer thyroid cancer Thyroiditis vein thrombosis Thrombophlebitis Furuncle (boil) Furunculosis cholestasis Cholecystitis Chronic cholecystitis Esophageal ulcer Peptic ulcer of the stomach and duodenum
All doctors
VDNKh metro station
Belorusskaya metro station
Lesnaya, 57, pp. 1
1
Lane Raskova, 14/22
m. Youth
m. Textiles
m. Dynamo
m. Kurskaya
m. Sevastopol
m. Chertanovskaya
Krylatskoye metro station
Voykovskaya metro station
Staropetrovsky proezd, 7A, building 22
Clara Zetkin, 33 bldg. 28
Baltiyskaya metro station
Staropetrovsky proezd, 7A, building 22
st. Clara Zetkin, 33 bldg. 28
m. Maryina grove
m. New birds
m. Water stadium
m. 1905 street
m. South-west
m. Sukharevskaya
All doctors
Loading load
Licenses
Go to the section of licenses Go to the section of legal information
Diastasis of the abdominal muscles after childbirth in women in Moscow
Diastasis is a divergence to the sides of the rectus abdominis muscles. At the same time, the white line of the abdomen becomes thinner and stretched - a connective tissue structure that connects the muscles that form the very desired "press cubes".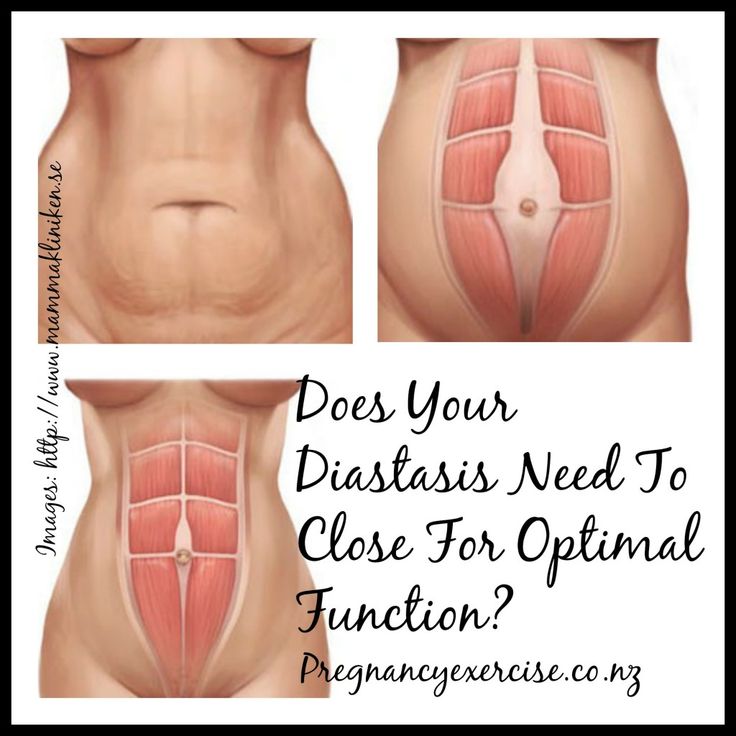 nine0003
nine0003
If its width is more than 20 mm, we are talking about the presence of diastasis of the rectus muscles.
Diastasis itself is not a disease, but rather a physiological condition. This is not a hernia: there is no defect in the white line, so there is no risk of infringement of internal organs. At the same time, the expansion and thinning of the white line increases the potential risk of developing true hernias.
Causes of diastasis
Most often, diastasis appears in the third trimester of pregnancy. This is one of the manifestations of physiological changes in the connective tissue of a woman during this period under the influence of hormones - the anterior abdominal wall is stretched due to connective tissue structures (and primarily the white line) - otherwise the uterus with a growing child would simply not fit in the abdominal cavity. In this case, the center of gravity of the body shifts anteriorly, the bend of the spine increases, the pressure on the anterior abdominal wall increases. The second reason for the appearance and increase in diastasis is an increase in pressure in the abdominal cavity, including during certain physical exercises. nine0003
The second reason for the appearance and increase in diastasis is an increase in pressure in the abdominal cavity, including during certain physical exercises. nine0003
In the postpartum period, the distance between the muscles decreases, but this process takes about a year. A survey of 300 women conducted by our Norwegian colleagues showed that 6 weeks after birth, diastasis persists in 60% of women, and after 12 months - only in 33%. That is why we do not recommend considering the issue of surgical treatment of diastasis earlier than a year after childbirth.
Classification of diastasis
There are several classifications of diastasis. Back at 1990 Ranney proposed to define diastasis as small with a width of up to 3 cm, moderate - 3-5 cm and large - if the distance between the rectus muscles is 5 cm or more.
Today, we most often use the classification of Reinpold et al. (2019), which is similar to the hernia classification of the European Society of Herniology. We also note the number of pregnancies, skin condition, clinical symptoms and a number of other parameters that help us to carefully describe the situation in each case and choose the best way to correct diastasis. nine0003
We also note the number of pregnancies, skin condition, clinical symptoms and a number of other parameters that help us to carefully describe the situation in each case and choose the best way to correct diastasis. nine0003
Symptoms of diastasis
Often diastasis is visible to the naked eye. For its clearer definition, we ask patients in the supine position to raise their heads and shoulders. At the same time, the rectus abdominis muscles contract and a protrusion becomes visible, or vice versa, a deepening along a line running from the sternum to the pubis. Palpation allows you to more accurately identify the presence and degree of diastasis.
Diastasis can also be manifested by clinical symptoms. The loss of a strong “foothold” for the muscles of the anterior abdominal wall leads to a redistribution of the static load, which in turn can lead to pelvic and lumbar pain, and in some, fortunately rare, cases, dysfunction of the pelvic organs. nine0003
Diastasis diagnostics
We routinely use ultrasound to accurately determine the presence, length and width of diastasis, white line defects and hernias. Ultrasound is included in the consultation and is performed by the surgeon, who determines the tactics of treatment. This approach, in our opinion, is optimal and allows you to obtain reliable additional information that affects the adoption of a tactical decision.
Ultrasound is included in the consultation and is performed by the surgeon, who determines the tactics of treatment. This approach, in our opinion, is optimal and allows you to obtain reliable additional information that affects the adoption of a tactical decision.
In some cases, usually with severe diastasis and the presence of a hernia, we perform computed tomography, which gives us an understanding of the state of the anterior abdominal wall and allows us to determine and model the optimal method for diastasis plasty. nine0003
How can diastasis be treated?
As we said above, diastasis is not a disease, but rather a postpartum condition leading to an aesthetic and functional defect of the anterior abdominal wall. Accordingly, we prefer to replace "treatment" with "correction".
A properly selected set of exercises can often correct external manifestations. It must be remembered that not all exercises can be performed with diastasis. All types of exercises that can contribute to an increase in diastasis are prohibited - these are all basic exercises with weights (deadlift, squats), many exercises for the abdominal muscles - twisting, hanging leg raises, etc.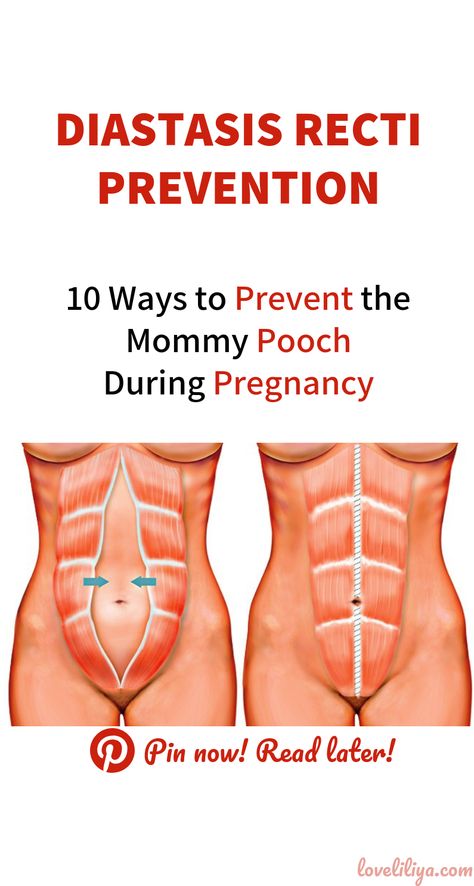 The classic "bar" is also not recommended for patients with diastasis. nine0003
The classic "bar" is also not recommended for patients with diastasis. nine0003
What exercises do we recommend for diastasis? Anything that strengthens the “deep core muscles”: side plank, tummy tuck, cat, Kegel exercises.
They cannot reduce the width of the white line (we remember that this is not a muscle, but a connective tissue that cannot be “pumped up”), but they can often improve the appearance of the abdomen and the quality of life of its owner, as a recent study by Thabet and Alshehri showed, although the level The evidence for this thesis is low. However, we recommend a training program for at least 6 months before considering diastasis surgery. nine0003
NB! This does not apply to situations where diastasis is combined with hernias - umbilical or white line. It is impossible to eliminate hernias with physical exercises, we immediately move on to the surgical treatment option (here, it is the treatment).
Surgical treatment of diastasis
Surgery for diastasis is a rather extensive topic: there are several options for operations: laparoscopic (at least three fundamentally different methods) and open (also at least three), with or without implants, various suture materials, etc.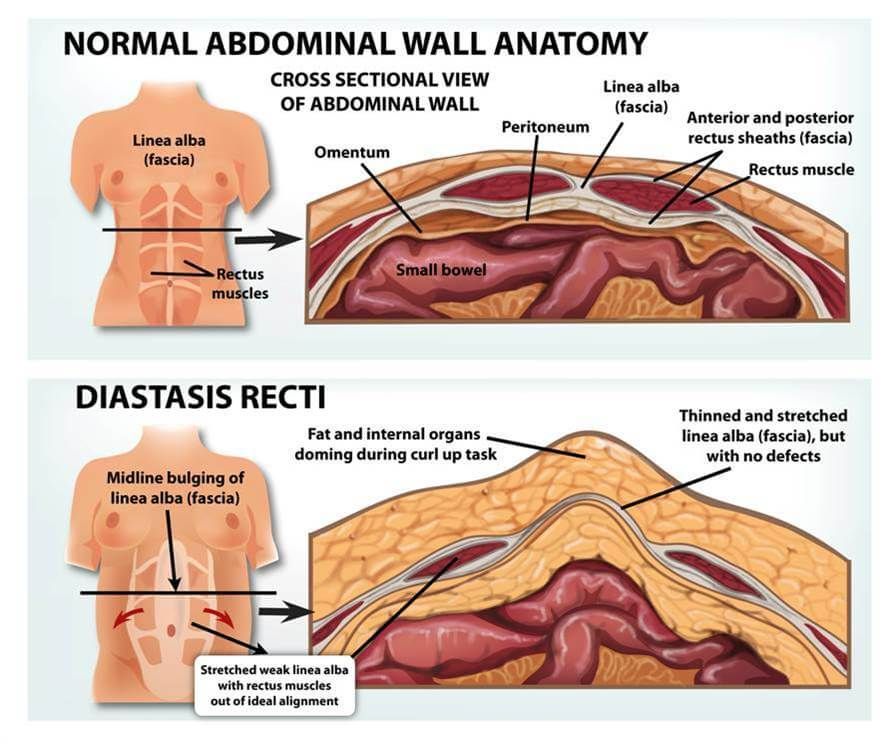 We will devote a separate article to these features, and now we will only briefly dwell on the indications for surgical correction: nine0003
We will devote a separate article to these features, and now we will only briefly dwell on the indications for surgical correction: nine0003
- Any diastasis associated with a hernia of the anterior abdominal wall or severe diastasis with a cosmetic defect and/or clinical symptoms
- Childbirth more than 12 months ago
- No effect after 6 months of training
- No other pregnancy planned
If these four conditions are met, we can plan the surgical treatment of diastasis.
Prevention of diastasis
To date, there are practically no scientifically based measures for the prevention of diastasis. You can reduce pressure on the anterior abdominal wall by following these 5 principles:
- Do not slouch
- Before sitting or getting out of bed, roll over onto your side to engage your lateral abdominal muscles when you get up
- Avoid heavy lifting during pregnancy, and if you have to, use proper lifting technique with a straight back
- A special supporting corset takes on part of the load, and in addition, it physically pulls the rectus abdominis muscles together
- Don't forget about regular exercise during pregnancy to strengthen your core and pelvic floor muscles.