Diastasis recti in child
Diastasis recti: MedlinePlus Medical Encyclopedia
URL of this page: //medlineplus.gov/ency/article/001602.htm
To use the sharing features on this page, please enable JavaScript.
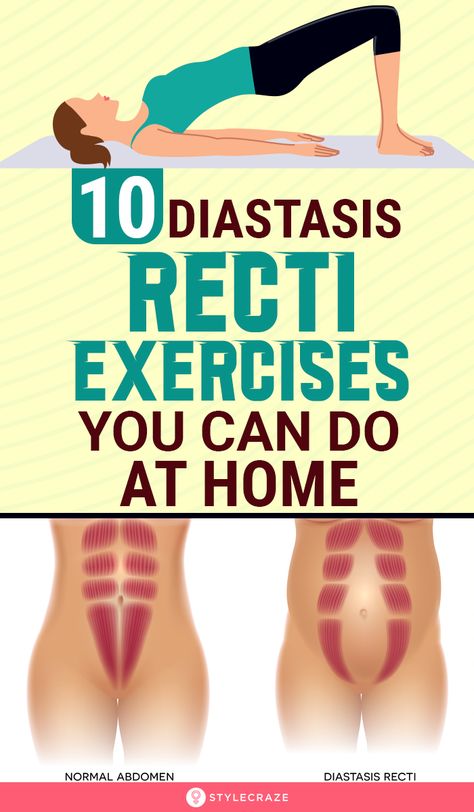
Diastasis recti is a separation between the left and right side of the rectus abdominis muscle. This muscle covers the front surface of the belly area.
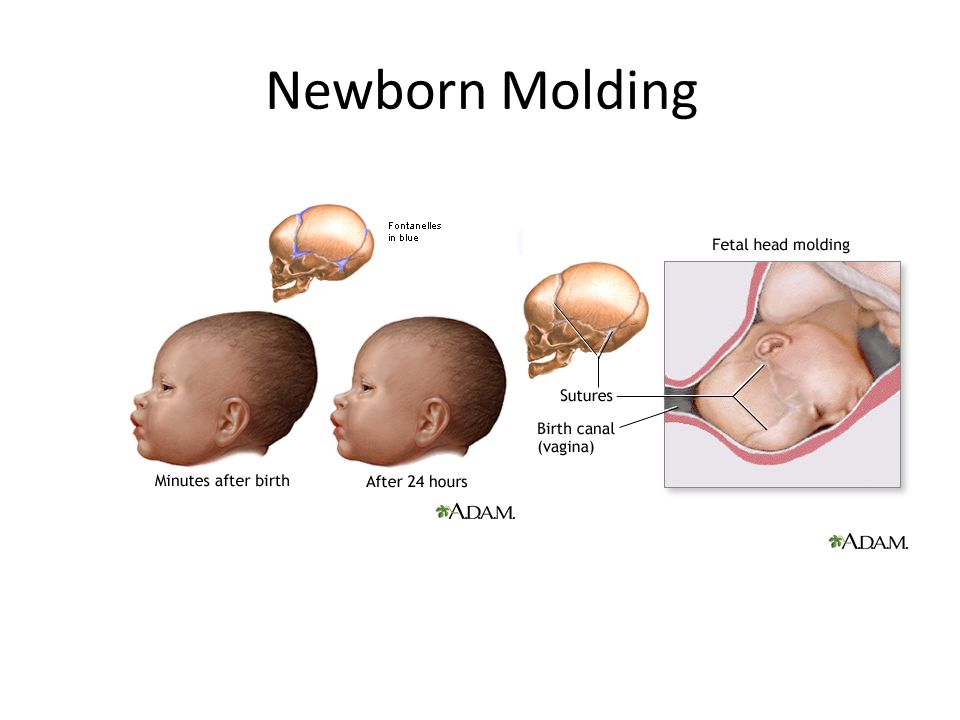
Diastasis recti is common in newborns. It is seen most often in premature and African American infants.
Pregnant women may develop the condition because of increased tension on the abdominal wall. The risk is higher with multiple births or many pregnancies.
A diastasis recti looks like a ridge, which runs down the middle of the belly area. It stretches from the bottom of the breastbone to the belly button. It increases with muscle straining.
In infants, the condition is most easily seen when the baby tries to sit up. When the infant is relaxed, you can often feel the edges of the rectus muscles.
Diastasis recti is commonly seen in women who have multiple pregnancies. This is because the muscles have been stretched many times. Extra skin and soft tissue in the front of the abdominal wall may be the only signs of this condition in early pregnancy. In the later part of pregnancy, the top of the pregnant uterus can be seen bulging out of the abdominal wall. An outline of parts of the unborn baby may be seen in some severe cases.
The health care provider can diagnose this condition with a physical exam.
No treatment is needed for pregnant women with this condition.
In infants, diastasis recti will disappear over time. Surgery may be needed if the baby develops a hernia that becomes trapped in the space between the muscles.
In some cases, diastasis recti heals on its own.
Pregnancy-related diastasis recti often lasts long after the woman gives birth. Exercise may help improve the condition. Umbilical hernia may occur in some cases. Surgery is rarely performed for diastasis recti.
Umbilical hernia may occur in some cases. Surgery is rarely performed for diastasis recti.
In general, complications only result when a hernia develops.
Contact your provider right away if a child with diastasis recti:
- Develops redness or pain in the abdomen
- Has vomiting that does not stop
- Cries all the time
- Diastasis recti
Ledbetter DJ, Chabra S, Javid PJ. Abdominal wall defects. In: Gleason CA, Juul SE, eds. Avery's Diseases of the Newborn. 10th ed. Philadelphia, PA: Elsevier; 2018:chap 73.
Privratsky AM, Barreto JC, Turnage RH. Abdominal wall, umbilicus, peritoneum, mesenteries, omentum, and retroperitoneum. In: Townsend CM Jr, Beauchamp RD, Evers BM, Mattox KL, eds. Sabiston Textbook of Surgery. 21st ed. St Louis, MO: Elsevier; 2022:chap 44.
Updated by: Debra G. Wechter, MD, FACS, General Surgery Practice Specializing in Breast Cancer, Virginia Mason Medical Center, Seattle, WA. Also reviewed by David Zieve, MD, MHA, Medical Director, Brenda Conaway, Editorial Director, and the A. D.A.M. Editorial team.
D.A.M. Editorial team.
Diastasis Recti in Children | The Tummy Team
Did you just learn that your child may have Diastasis Recti and want answers?
You are in the right place. The Tummy Team specializes in the treatment of Diastasis Recti in men, women and children.
What most people do not know is that everyone is actually born with some form of diastasis recti to allow the umbilical cord exit the body. This separation typically closes in the first few weeks after delivery but can take up to 3-4 years or longer to fully close in some children. Lack of closure of the diastasis can contribute to functional core weakness, muscle imbalance, intestinal issues and several complications in normal physical development.
Explore Our Children’s Online Rehab Course
First, let’s define Diastasis Recti
Diastasis Recti (DR): a separation of the abdominal muscles caused by excessive stretching of the connective tissue that runs down the midline of the abdominal wall.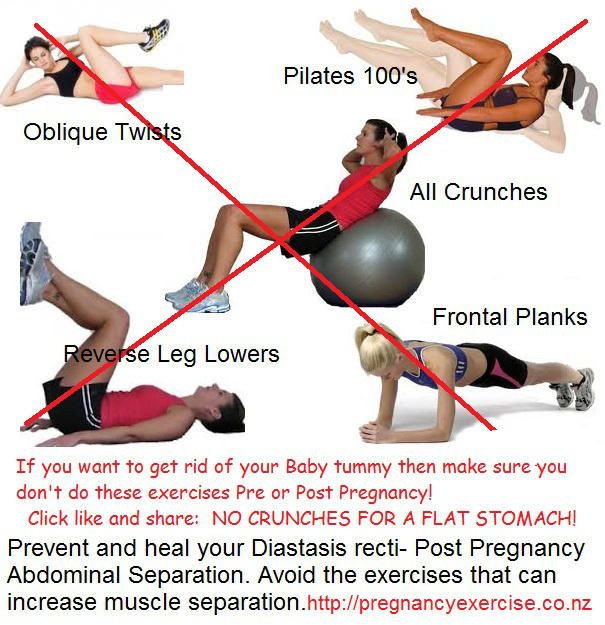
What does Diastasis look like?
(*diastasis recti can present differently depending on the age of your child and not all children have all of these symptoms)
- A trench or football shaped bulge down the midline of the tummy when they do crunch like movements, cough or cry.
- Bulging tummy that gets worse with activity, throughout the day or with eating.
- Overall weakness in the core – affecting posture, developmental delays, ability to balance, walk, run, lift, reach.
- Sluggish intestinal function, bloating, gas, constipation, and the need to bear down to have a bowel movements.
- Flared rib cage or barrel chest
Diastasis Recti or Umbilical Hernia or both?
Often babies, children and toddlers are diagnosed with both diastasis and an umbilical hernia or there is some confusion between the two. Let’s clarify the difference and help you understand what might be going on with your child. It is possible to have a diastasis and not have a hernia, and have a hernia and not have a diastasis and to have both conditions at once.
It is possible to have a diastasis and not have a hernia, and have a hernia and not have a diastasis and to have both conditions at once.
What is the difference?
Diastasis Recti: a separation of the abdominals down the midline as the linea albea stretches
Umbilical Hernia: a tear in the connective tissue that allows the umbilicus to pop out.
Detached Umbilicus: a bulging umbilicus (outie or partially outie belly button) without a tear in the connective tissue.
So how did this happen?
When we are born our abdominal wall is slightly separated to allow for the umbilical cord to pass from the placenta into our tummy. After delivery, the cord is cut and gradually retracts into the body and eventually scar tissue tethers the umbilicus and creates an anchor that looks in most cases like and “innie” belly button. In some cases, babies experience chronic forward pressure (intra-abdominal pressure) that presses out on the abdominal wall and keep the umbilical cord from fully retracting and tethering down(detached umbilicus). This pressure keeps the connective tissue from closing and can redirect pressure out on the tummy causing a bulge or trench down the midline (diastasis recti) or creating a tear in the connective tissue that pushes the umbilical cord through the navel (umbilical hernia). Chronic forward pressure on the tummy is most often caused from colic, painful gas, bloating, constipation, straining, respiratory issues, chronic coughing, conditions that cause a lot of vomiting or a muscle tone imbalance.
This pressure keeps the connective tissue from closing and can redirect pressure out on the tummy causing a bulge or trench down the midline (diastasis recti) or creating a tear in the connective tissue that pushes the umbilical cord through the navel (umbilical hernia). Chronic forward pressure on the tummy is most often caused from colic, painful gas, bloating, constipation, straining, respiratory issues, chronic coughing, conditions that cause a lot of vomiting or a muscle tone imbalance.
Diastasis recti can be misdiagnosed as an umbilical hernia in young children. But it is possible to have a diastasis and an umbilical hernia or have a diastasis with a detached umbilicus. Both diastasis recti and umbilical hernias in young children are typically caused by chronic intra abdominal pressure that pushes out on the tummy and keeps the umbilical root from fully retracting and tethering down to create an “innie belly button”. In both cases, we treat the cause to correct the presenting condition.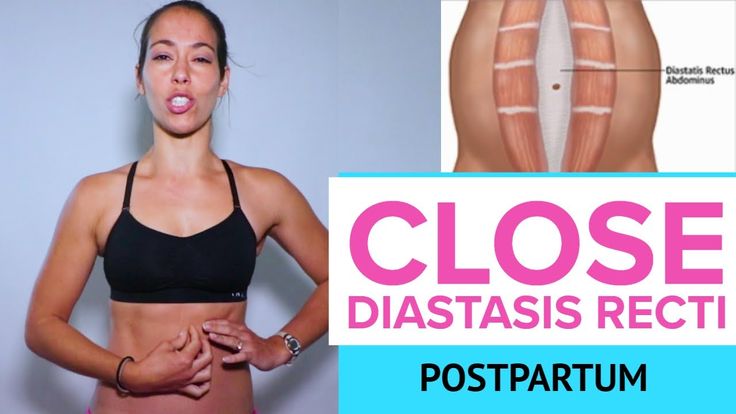 The Tummy Team uses functional core rehab to retrain that forward pushing compensation pattern and improve both of these conditions.
The Tummy Team uses functional core rehab to retrain that forward pushing compensation pattern and improve both of these conditions.
The Tummy Team’s approach to core rehab in children can encourage the diastasis to close, minimize the risk of a tear and even promote the retraction of the umbilicus in some cases. Even if surgery is recommended, we encourage parents to educate themselves and develop tools to promote the healthy functional strength of their child’s core moving forward. Surgery will patch the hole but will not retrain the muscle patterns. And all children need a strong core to meet their developmental milestones.
How do we fix this?
Diastasis Recti is treatable and should be addressed in young children when it does not appear to be closing on its own. Typical compensation patterns in children are holding the breath, tensing when straining, bracing the muscles and recruiting upper and lower body muscles to stabilize the core. All of these strategies actually push out on the abdominal wall (even slightly) instead of drawing in and elongating the core. This habitual outward pressure keeps the connective tissue of the abdominal wall (the linea alba) from closing and can make it get bigger, but also can be retrained with the right approach.
This habitual outward pressure keeps the connective tissue of the abdominal wall (the linea alba) from closing and can make it get bigger, but also can be retrained with the right approach.
The Tummy Team offers a Toddler Course geared to parents of children ages 1-5 years old to help you understand the diastasis and the conditions contributing to it as well as providing tools to help your child close the diastasis and improve their functional core strength. If your child is older or younger than this age range then please reach out to our specialist to see what the best course of action is for you and your child.
Want to talk to our specialist first?
Book a FREE 15-Minute Phone Consult with Kelly Here
Check out our children’s functional core rehab course or book a 1:1 eSession with Kelly Dean, MPT:
Diastasis of the rectus abdominis muscles - symptoms, signs, degrees, causes and treatment in men and women in Moscow in the "SM-Clinic"
The surgeon deals with the treatment of this disease
Book online Request a call
- What is diastasis rectus abdominis?
- About disease
- Species
- Symptoms of diastasis recti
- Causes of diastasis recti
- Diagnostics of diastasis of the rectus abdominis muscles
- Expert opinion
- Treatment of diastasis recti
- Surgical treatment of diastasis recti
- Prophylaxis
- Rehabilitation after surgery
- Questions and answers
- Sources
About the disease
The disease is based on stretching and expansion of the white line of the abdomen - a tendon that is located between the rectus muscles, connects and holds them. This is a strip of connective tissue, consisting of several layers, located in the middle of the abdomen vertically from the xiphoid process to the pubic joint.
This is a strip of connective tissue, consisting of several layers, located in the middle of the abdomen vertically from the xiphoid process to the pubic joint.
Due to an increase in intra-abdominal pressure or a violation of the properties of the connective fibers, the structure of the tendon changes, it weakens, becomes thinner and stretches. The trigger mechanism is prolonged pressure on the abdominal wall associated with pregnancy or visceral obesity. An aggravating factor is the loosening of the white line against the background of collagenopathy, the effects of relaxin, the immaturity of cellular structures, etc.
As a result, the white line becomes thinner and stretched. Normally, its dimensions are restored with a gradual decrease in the abdomen or as the properties of the connective tissue normalize. Thus, physiological diastasis is eliminated during the neonatal period or in women after childbirth.
If abdominal training is started early in the postpartum period, this leads to a contraction of the rectus muscles and a simultaneous increase in intra-abdominal pressure, and the white line is fixed in a stretched position and does not hold the internal organs well. As a result, unaesthetic vertical folds form on the abdomen, a rounded protrusion appears, dysfunction of the digestive tract occurs and the risk of hernia formation increases.
As a result, unaesthetic vertical folds form on the abdomen, a rounded protrusion appears, dysfunction of the digestive tract occurs and the risk of hernia formation increases.
Species
Depending on the magnitude of the stretching of the tendon ligament, there are 3 degrees of diastasis of the rectus abdominis muscles:
- first - the muscles move away from each other by 2.5-5 cm;
- second - ligaments diverge by 5-8 cm;
- third - the line is stretched more than 8 cm.
According to the localization of the place of maximum stretching, supra-umbilical, sub-umbilical and mixed forms of diastasis are distinguished.
According to the degree of involvement of other muscles of the anterior abdominal wall, the pathology is classified into types:
- A - classical divergence of muscles after natural childbirth;
- B - relaxation of the lower lateral sections of the muscles;
- C - expansion affects the region of the ribs and the xiphoid process;
- D - diastasis is combined with a curvature of the waistline.
Symptoms of diastasis of the rectus abdominis muscles
Manifestations of BPMD increase as the pathology progresses. In women, a vivid clinical picture manifests itself abruptly (shortly after childbirth), while in men the disease develops gradually.
At the onset of the disease, there may be no symptoms at all. The patient then notices a characteristic rounded vertical protrusion in the center of the abdomen. With deliberate tension of the press, the inner edges of the rectus muscles and the groove between them are clearly visible. Due to muscle dysfunction, pain in the spine, lower back, fatigue, and posture disorders are possible.
With the progression of the pathology, manifestations of dysfunction of the gastrointestinal tract join:
- heartburn;
- belching;
- flatulence;
- abdominal pain;
- constipation.
In the third stage of diastasis, patients are faced with the formation of hernias, which are formed due to structural defects in the white line. Possible ptosis (omission) of internal organs and serious disturbances in the work of the intestines (in severe cases, intestinal obstruction develops). Women often experience urinary incontinence, renal colic.
Possible ptosis (omission) of internal organs and serious disturbances in the work of the intestines (in severe cases, intestinal obstruction develops). Women often experience urinary incontinence, renal colic.
Causes of diastasis recti
Increase the risk of diastasis, connective tissue pathology and increased pressure in the abdominal cavity. In different categories of patients, the causes of the development of PMSD are different.
Divergence of muscles in children is due to the failure of the musculature and tendons. After 2-12 months after birth, the muscles come into tone, the ligaments and tendons are strengthened - the process resolves itself. In premature babies and infants with intrauterine developmental pathologies, this may take longer. With Down syndrome, there is a risk of maintaining diastasis for life.
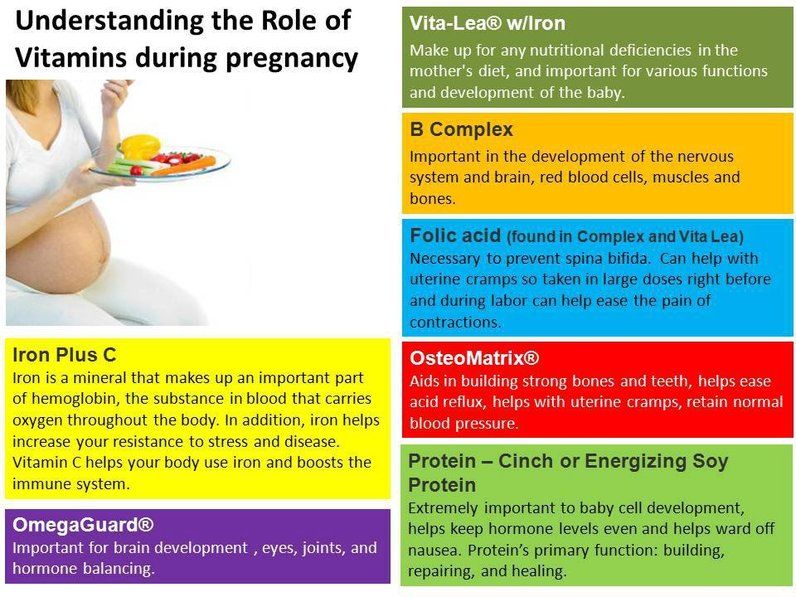
Pregnancy is the provocateur of diastasis of the rectus abdominis muscles in women. The growing uterus puts considerable pressure on the linea alba, stretching it.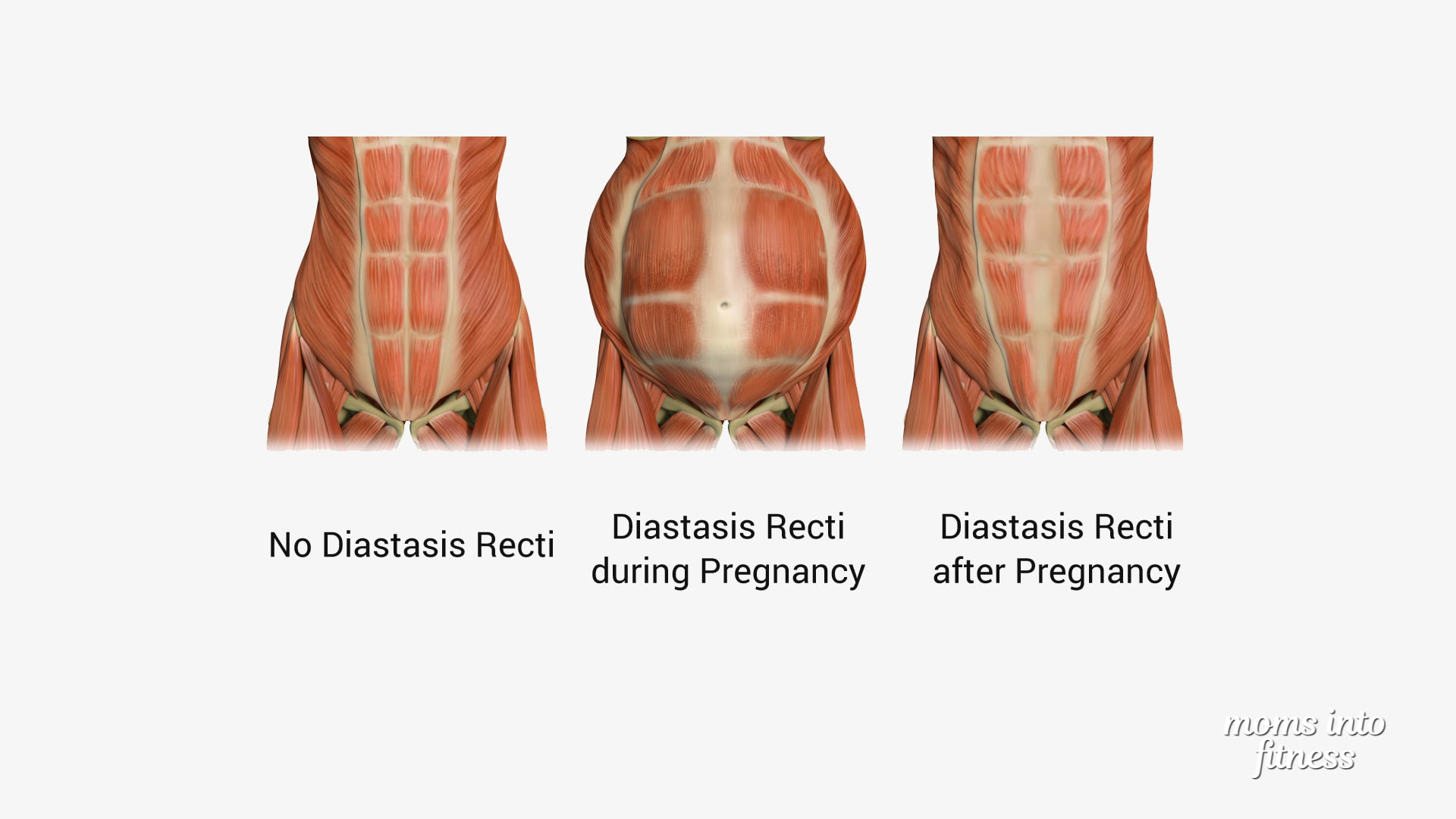 Under the action of hormones, the synthesis of collagen fibers is inhibited, the ligaments become looser. But a few months after the birth, the white line of the abdomen is normally restored.
Under the action of hormones, the synthesis of collagen fibers is inhibited, the ligaments become looser. But a few months after the birth, the white line of the abdomen is normally restored.
In men, BMD is often provoked by obesity, physical activity and hereditary collagenopathies. The risk of diastasis increases with a tendency to constipation, as well as with chronic respiratory diseases accompanied by coughing.
Treatment of pathology by conservative methods is possible with a small diastasis. At the later stages of development, the pathological divergence of muscles is eliminated with the help of abdominal plastic surgery.
Get advice
If you experience these symptoms, we recommend that you make an appointment with your doctor. Timely consultation will prevent negative consequences for your health.
You can find out more about the disease, prices for treatment and sign up for a consultation with a specialist by phone:
+7 (495) 292-39-72
Request a call back Book online
Why SM-Clinic?
1
Treatment is carried out in accordance with clinical recommendations
2
A comprehensive assessment of the nature of the disease and treatment forecast
3
Modern diagnostic equipment and own laboratory
4
High level of service and balanced price policy
Diagnosis of diastasis of the rectus abdominis muscles
Identification of BPMD is not difficult, since the disease has characteristic clinical manifestations.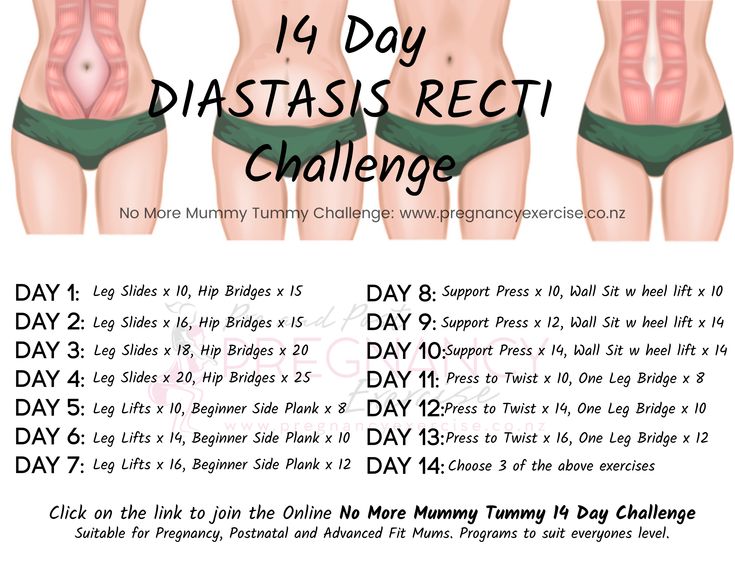 With signs of diastasis, you should contact the surgeon.
With signs of diastasis, you should contact the surgeon.
An increase in the space between the rectus muscles is determined during palpation of the abdomen. To conduct the test, the patient is asked to lie on his back, legs slightly bent at the knees, and then tighten the abdominal muscles, raising his head and shoulder blades. In patients with obesity, the doctor is not always able to fully explore the width of the white line.
The exact size of the stretch is determined by ultrasound. This diagnostic method also allows you to detect complications (hernia, displacement of internal organs). In order to differentiate the symptoms of diastasis and manifestations of chronic diseases of the gastrointestinal tract or the genitourinary system, consultations of specialized specialists are prescribed.
Expert opinion
Surgeons warn that diastasis of the rectus abdominis muscles is asymptomatic for a long time. Therefore, in the presence of predisposing factors (recent pregnancy and childbirth, chronic constipation, obesity) or non-specific complaints, you should independently feel the white line of the abdomen in the navel. If the distance between the rectus muscles is more than 2.5 cm, contact the surgeon. Also, do not delay the visit in any doubtful cases. Only a doctor can establish the correct diagnosis, self-examination does not exclude the need for an in-person consultation.
If the distance between the rectus muscles is more than 2.5 cm, contact the surgeon. Also, do not delay the visit in any doubtful cases. Only a doctor can establish the correct diagnosis, self-examination does not exclude the need for an in-person consultation.
Egiev Valery Nikolaevich, surgeon, oncologist, doctor of medical sciences, professor, head of the Department of Surgery and Oncology, FPC MR MI RUDN University
Treatment of diastasis recti
Functional diastasis in newborns and puerperas does not require treatment. Doctors use expectant tactics, recommend adhering to the principles of rational nutrition, doing massages, and doing gymnastics. The observation period can last up to 12 months. If after this time the problem persists, the surgeon decides on an operative method of correction.
Conservative treatment
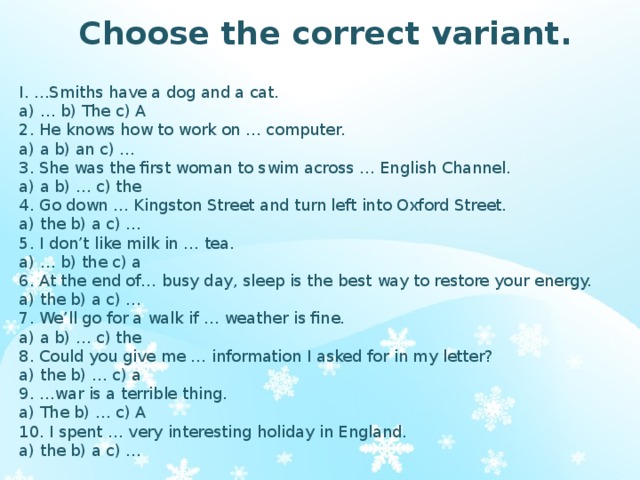
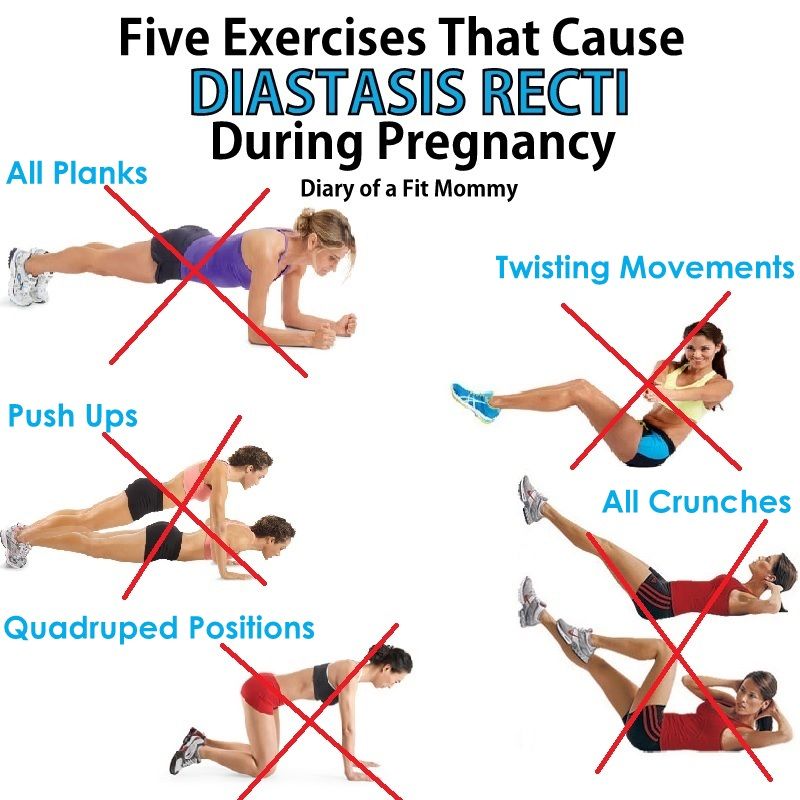
Patients are prescribed a diet to prevent constipation and excessive gas formation, as well as to gradually reduce weight. In the postpartum period, incl.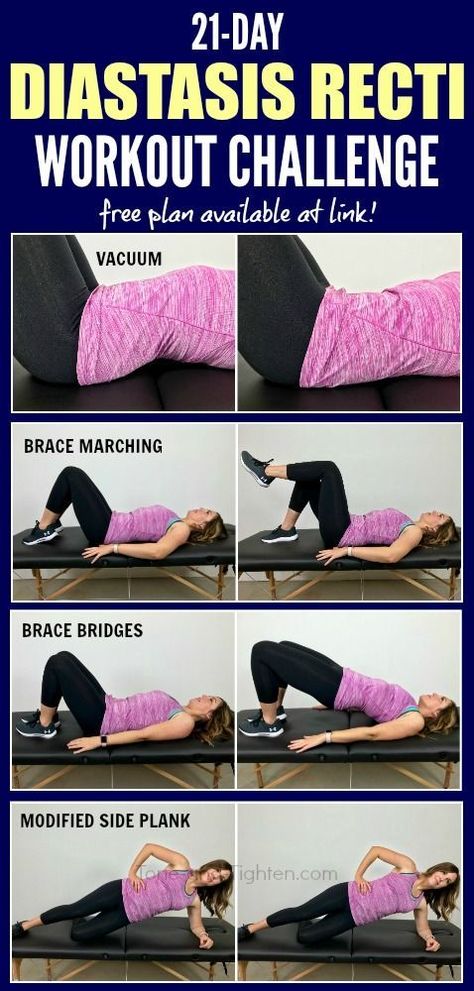 after a caesarean section, women are advised to wear a bandage, support the stomach during sneezing and coughing. The general strengthening of the muscles allows you to quickly restore the tone of the anterior abdominal wall, so patients are prescribed exercise therapy, swimming, yoga classes. It is important to exclude any training of the abdominal muscles. You can not perform exercises in the knee-elbow position, as well as in the emphasis (bar). Such loads can be resumed after the restoration of the size of the white line. Conservative treatment is effective only at the 1st stage of BPMD.
after a caesarean section, women are advised to wear a bandage, support the stomach during sneezing and coughing. The general strengthening of the muscles allows you to quickly restore the tone of the anterior abdominal wall, so patients are prescribed exercise therapy, swimming, yoga classes. It is important to exclude any training of the abdominal muscles. You can not perform exercises in the knee-elbow position, as well as in the emphasis (bar). Such loads can be resumed after the restoration of the size of the white line. Conservative treatment is effective only at the 1st stage of BPMD.
Surgical treatment of diastasis of the rectus abdominis muscles
In case of complicated and uncomplicated diastasis of the rectus abdominis muscles of the 2-3rd degree, surgical treatment is indicated. It is possible to use the following surgical techniques:
- Tension plastic using own tissues. It involves stitching the edges of the muscles with the removal of excess connective tissue.
 To date, it is not used due to the high risk of recurrence.
To date, it is not used due to the high risk of recurrence. - Tension-free repair with a mesh prosthesis. It implies the introduction of an endoprosthesis under the site of stretching.
- Tension plasty with prosthesis installation. It involves the removal of excess connective tissue, suturing the edges of the muscles and strengthening the zone with a polypropylene mesh.
- Combined technique. Includes muscle suturing, mesh strengthening, removal of excess adipose tissue and stretched skin.
Prevention
To reduce the risk of developing diastasis rectus abdominis, you should keep your body in shape - engage in regular exercise, train your muscles. However, do not overdo it: lifting weights can, on the contrary, become the main cause of muscle divergence.
It is also important to eat a complete and balanced diet - a lack of nutrients will lead to a decrease in the elasticity of the connective tissue.
It is necessary to control your weight - body mass index should not exceed 26 kg/m3. Obesity, especially of the abdominal type, is an important risk factor for BLV.
Obesity, especially of the abdominal type, is an important risk factor for BLV.
Prevention and timely treatment of chronic lung diseases accompanied by cough, pathologies of the digestive system, occurring with constipation, will reduce the possibility of increasing intra-abdominal pressure and, as a result, the likelihood of diastasis.
Rehabilitation after surgery
After surgery, the patient is under inpatient observation, receiving analgesic and antibiotic therapy. Full recovery lasts 1-3 months. During this period, the patient is prescribed a diet to normalize defecation, it is recommended to avoid significant physical exertion, weight lifting. To prevent excess tension, it is necessary to wear a bandage.
Questions and answers
A surgeon deals with the treatment of pathology.
In the stronger sex, obesity and connective tissue dysplasia are considered to be the main cause of BMD. Sharp weight loss or weight gain, excessive passion for power loads are capable of provoking muscle divergence. If a man or close relatives have hernias, varicose veins, valgus flat feet, hemorrhoids, this is regarded as an increased tendency to PMSD.
If a man or close relatives have hernias, varicose veins, valgus flat feet, hemorrhoids, this is regarded as an increased tendency to PMSD.
There is no need to rush in this matter. Just the desire to quickly get in shape is the main reason for the progression of diastasis in women. Physical activity can be resumed 1-2 months after delivery. You can start with hiking or yoga. Abdominal exercises can be performed soon after the white line is reduced to 2 cm. It is advisable to pay attention to the diet. A smooth decrease in weight and volume of visceral fat will ensure gradual and timely muscle contraction. Sharp weight loss, on the contrary, can increase diastasis.
You can lie on a hard surface on your back, tense your abs. With gentle movements of the fingers, you should begin to probe the stomach in the middle in the navel. With a normal width of the white line and with diastasis, a depression will be found - this is the median ligament. If its width is equal to or greater than the width of two fingers, you should contact the surgeon. Constipation, bloating and abdominal pain should be alarming. If there are such symptoms, it is necessary to get to the surgeon in the near future.
Constipation, bloating and abdominal pain should be alarming. If there are such symptoms, it is necessary to get to the surgeon in the near future.
Pathogenesis and treatment of ventral hernias and diastasis of the rectus abdominis muscles: Abstract of the thesis / Zagirov U.Z. - 1995.
Comparative aspects of methods for eliminating diastasis of the rectus abdominis muscles / Topchiev MA, Bondarev VA, Elderov S.Sh.// Astrakhan medical journal. - 2010.
Jessen M. L., Öberg S., Rosenberg J. Treatment Options for Abdominal Rectus Diastasis // Front Surg. - 2019. - No. 6. - R. 65
>
Diseases referred by the Surgeon
Soft tissue abscess liver abscess Appendicitis Ascites Atheroma femoral hernia Crohn's disease Ingrown toenail (onychocryptosis) Gangrene soft tissue hematoma Giant cell tumor of bone Hygroma festering wounds Hernia Hernia of the white line of the abdomen hiatal hernia Intestinal diverticulosis Cholelithiasis Keratoma liver cyst pancreatic cyst salivary gland cyst Neck cyst Lipoma Mechanical jaundice Bowel obstruction Oleogranuloma kidney tumor Acute pancreatitis Pancreatic necrosis Inguinal hernia Peritonitis Barrett's esophagus Postoperative hernia Umbilical hernia Cancer of the extrahepatic bile ducts Stomach cancer gallbladder cancer bowel cancer adrenal cancer Parathyroid Cancer Liver cancer Esophageal carcinoma colon cancer thyroid cancer Fistula of the gallbladder Thyroiditis Intestinal injury vein thrombosis Thrombophlebitis Furuncle (boil) Furunculosis cholestasis Cholecystitis Chronic cholecystitis Esophageal ulcer Peptic ulcer of the stomach and duodenum
All doctors
VDNKh metro station
Belorusskaya metro station
Lesnaya, 57, pp.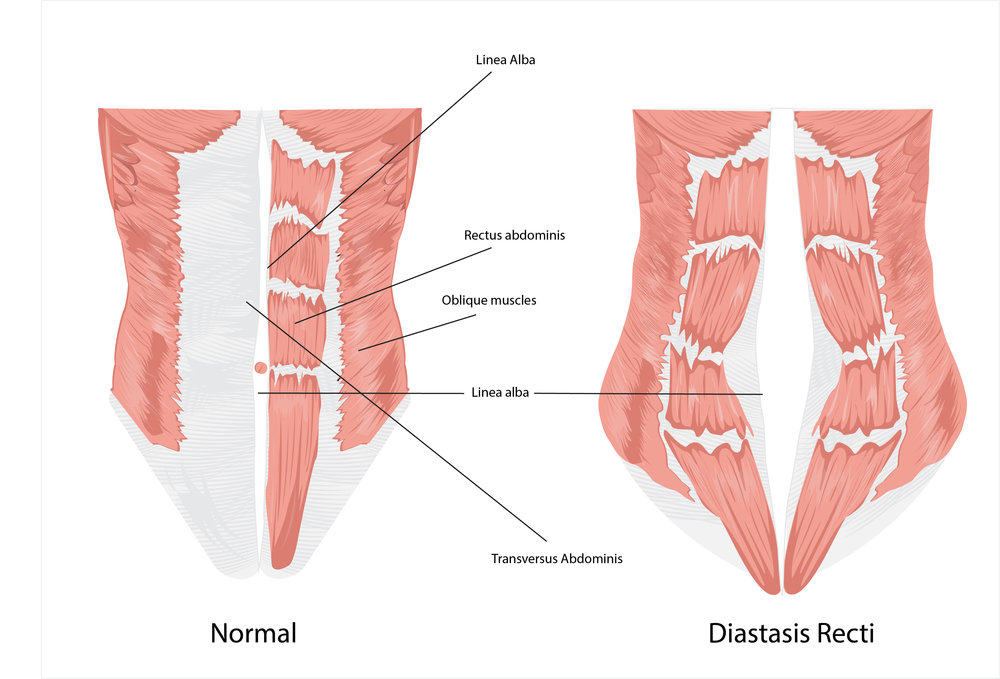 1
1
Raskova Lane, 14/22
m. Youth
m. Textiles
m. Dynamo
m. Kurskaya
m. Sevastopol
m. Chertanovskaya
Krylatskoye metro station
Voykovskaya metro station
Staropetrovsky proezd, 7A, building 22
Clara Zetkin, 33 bldg. 28
Baltiyskaya metro station
Staropetrovsky proezd, 7A, building 22
st. Clara Zetkin, 33 bldg. 28
m. Maryina grove
m. New birds
m. Water stadium
m. 1905 street
m. South-west
m. Sukharevskaya
All doctors
Loading
Licenses
Go to the section of licenses Go to the section of legal information
Diastasis rectus abdominis and diastasis pubis. Solvable problems of pregnancy. Interview with Doctor of Medical Sciences, Professor M.A. Chechnyova
— What is muscle diastasis and what is pubic diastasis?
— Pregnancy is an amazing and wonderful time, but it is also a period of additional loads, which undoubtedly becomes a test of strength for the female body.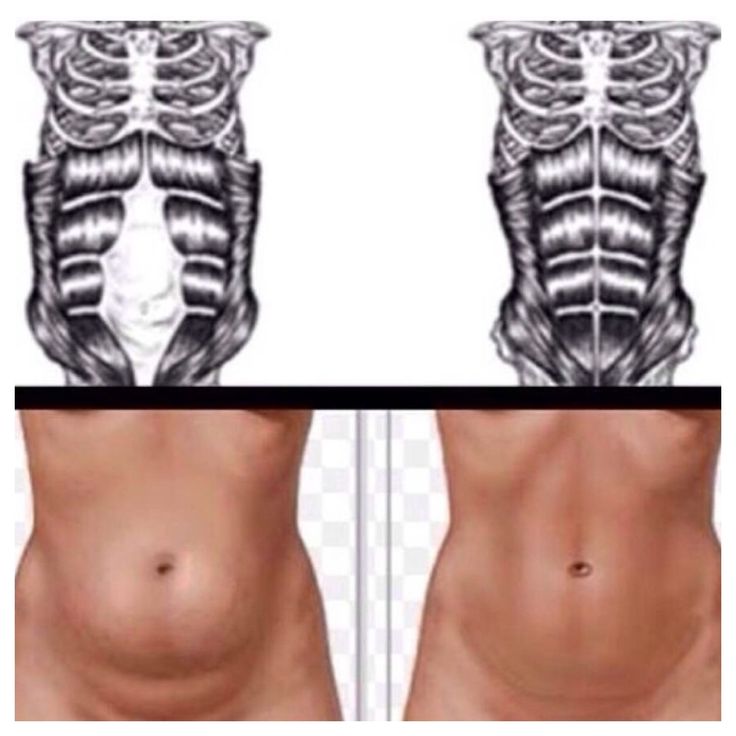
The previously existing everyday point of view that pregnancy rejuvenates and gives strength is not confirmed by anything. During the bearing of a child, significant additional loads are placed on the mother's body, which often lead to the manifestation of problems that were invisible before pregnancy.
Diastasis of the rectus abdominis muscles is a divergence of the inner edges of the muscles along the white line of the abdomen (connective tissue structure) at a distance of more than 27 mm. Pubic diastasis is one of the manifestations of pregnancy-associated pelvic girdle pain. This pathology affects the entire pelvic ring, sacroiliac joints and symphysis. And they certainly have common causes for the appearance.
The formation of such problems is facilitated by a decrease in the strength of collagen in the connective tissue. One of the reasons is an innate predisposition, the so-called connective tissue dysplasia, when the tissues are very elastic, extensible.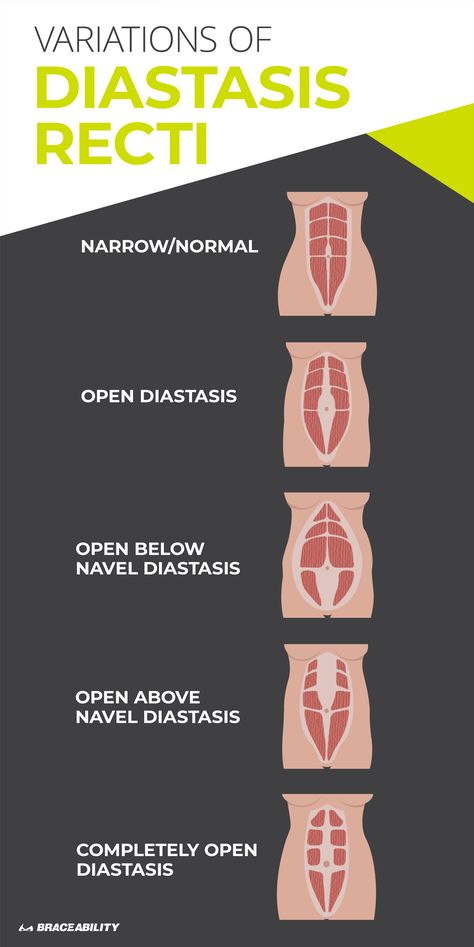 During pregnancy, the body of a woman increases the production of the hormone relaxin, which reduces the synthesis of collagen and enhances its breakdown. This is provided by nature to create maximum elasticity of the birth canal. However, other structures, such as the anterior abdominal wall and the pubic symphysis, also fall under the action of relaxin.
During pregnancy, the body of a woman increases the production of the hormone relaxin, which reduces the synthesis of collagen and enhances its breakdown. This is provided by nature to create maximum elasticity of the birth canal. However, other structures, such as the anterior abdominal wall and the pubic symphysis, also fall under the action of relaxin.
— How does diastasis of the muscles and diastasis of the pubis affect pregnancy and childbirth?
— Divergence of the rectus abdominis occurs in about 40% of pregnant women. During pregnancy, it does not give serious complications that threaten the life of the mother or the condition of the fetus. However, the inferiority of the work of the rectus abdominis muscles forces the redistribution of the load on the back muscles, which can lead to lumbar-pelvic pain and, accordingly, discomfort in the back. During childbirth, the abdominal muscles are involved in attempts, and the violation of their anatomy and function can affect the birth act.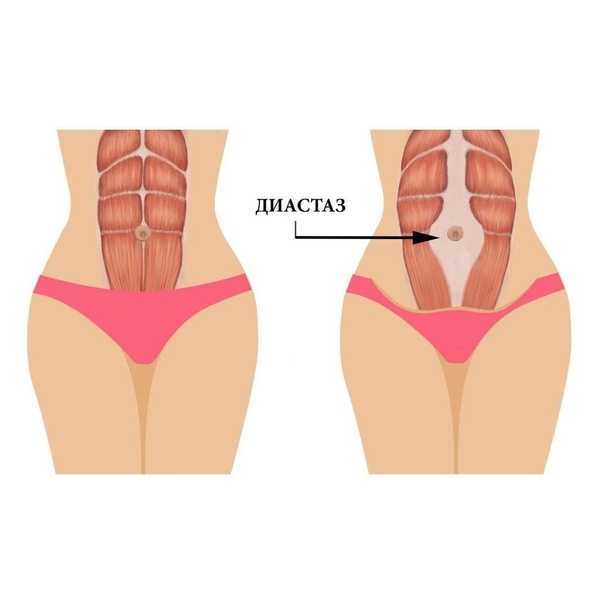
With diastasis of the pubis, things are more complicated. As already mentioned, this is only one of the manifestations of a violation of the structure and function of the pubic joint (symphysiopathy) during pregnancy. It occurs in about 50% of pregnant women in varying degrees of severity: in 25% of cases it leads to restriction of the mobility of the pregnant woman, in 8% - to severe disorders up to disability.
With symphysiopathy, the ligaments of the pubic articulation and cartilage that connect the pubic bones suffer. All this leads to severe pain in the pubic joint, pelvic bones, lower back, as well as to a violation of gait and the inability to stand up or lie down without outside help. Women with pelvic girdle pain syndrome experience significant levels of discomfort, disability, and depression, with associated social and economic problems. These include impaired sexual activity during pregnancy, chronic pain syndrome, risk of venous thromboembolism due to prolonged immobility, and even seeking early induction of labor or caesarean section to stop pain.
During childbirth, such a patient may have a rupture of the pubic symphysis, may require surgery to restore it.
— How to prevent the development of muscle and pelvic diastasis during pregnancy and childbirth? What factors increase the likelihood of its development?
- There is no recipe that will be one hundred percent. There is a wonderful term in the medical literature called "lifestyle modification". Whatever diseases we study, be it symphysiopathy, diabetes mellitus or preeclampsia, the risk group for pathology is always overweight women. You need to prepare for pregnancy, you need to be in good physical shape. During pregnancy, weight gain should be monitored. The recommendation to "eat for two" is not just wrong, but extremely harmful. Pregnant women should maintain reasonable physical activity. Weak and flabby abdominal muscles, combined with the large size of the fetus, undoubtedly increase the risk of diastasis.
The risk factors for symphysiopathy in numerous studies are hard physical labor and previous injuries of the pelvic bones.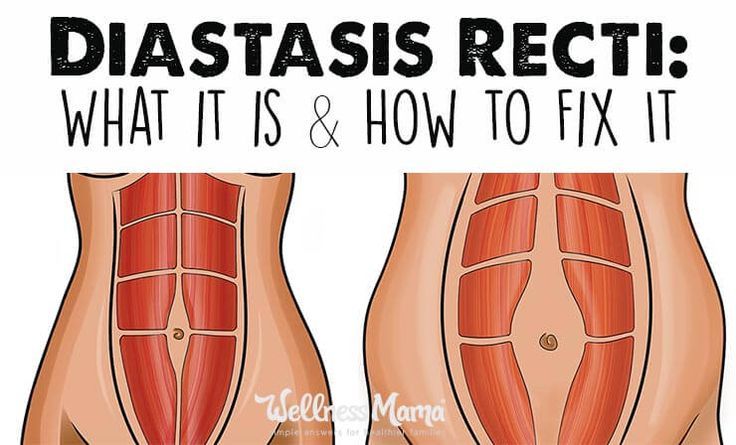 Factors such as time elapsed from previous pregnancies, smoking, use of hormonal contraception, epidural anesthesia, mother's ethnicity, number of previous pregnancies, bone density, weight and gestational age of the fetus (post-term fetus) are not associated with an increased risk of symphysiopathy.
Factors such as time elapsed from previous pregnancies, smoking, use of hormonal contraception, epidural anesthesia, mother's ethnicity, number of previous pregnancies, bone density, weight and gestational age of the fetus (post-term fetus) are not associated with an increased risk of symphysiopathy.
- How to diagnose diastasis of the rectus muscles and diastasis of the pubic symphysis?
— In most cases, diastasis rectus abdominis can be diagnosed clinically. It happens that inspection, palpation and simple measurements are enough.
In the standing position, you can see the divergence of the muscles when the woman does not have subcutaneous fat. In this case, diastasis is defined as a vertical defect between the rectus muscles.
With tension of the abdominal press, a longitudinal protrusion is observed in the diastasis zone. Such a protrusion is especially noticeable if the patient in the supine position is asked to raise her head and legs. If necessary, you can measure the width of the defect simply with a ruler.
Ultrasound may be the most accurate diagnostic method. With ultrasound, the inner edges of the rectus muscles are clearly visible and the distance between them at different levels can be measured.
Computed tomography is used in the diagnosis of diastasis extremely rarely, mainly in scientific research.
For the diagnosis of symphysiopathy and diastasis pubis there is no one test as a "gold standard".
The first place, of course, is the questioning and examination of the patient. We pay attention to the gait of the pregnant woman, to how she sits down, lies down and how she gets up. Symphysiopathy is characterized by a “duck gait”, when a pregnant woman rolls from foot to foot. On palpation in the area of the womb, pain and swelling are noted. The so-called pain provocative tests are used, for example, a mat-test (pulling up an imaginary rug, mat with your foot towards you).
The following questionnaires are used to assess quality of life, pain and disability: Health-Related Quality of Life (HRQL), Oswestry Disability Index (ODI), Disability Rating Index (DRI), Edinburgh Postpartum Depression Scale (EPDS), Pregnancy Mobility Index (PMI), and Pelvic Ring Score (PGQ).
Of the instrumental methods, ultrasound is the most widely used, less often computed or magnetic resonance imaging. Ultrasound allows you to assess the condition of the ligaments of the pubic joint and the interpubic disc, the severity of the changes and the risk of natural childbirth.
— What is the treatment for diastasis recti or pubis?
— Primary prevention: when planning and during pregnancy, it is necessary to strengthen all muscle groups of the pelvic girdle, as well as the pelvic diaphragm.
More often, diastasis of the rectus muscles disappears on its own during the first months after childbirth. Special physical exercises to correct the work of muscles, to tone them and restore their basic functions should be performed under the guidance of a competent instructor. There are types of physical exercises that can, on the contrary, worsen the situation with diastasis of the rectus abdominis muscles. In some cases, when there is no effect from physiotherapy exercises, it is necessary to resort to surgical correction of the defect.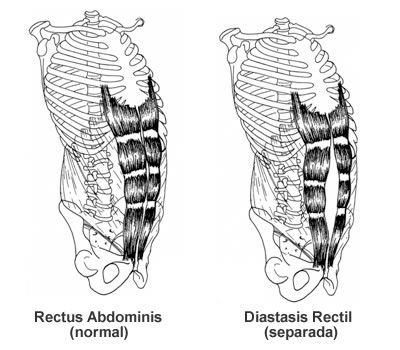 Currently, both endoscopic and open surgery are practiced. The choice of method depends on the size and localization of the defect.
Currently, both endoscopic and open surgery are practiced. The choice of method depends on the size and localization of the defect.
In case of symphysiopathy, therapeutic exercises reduce back and pelvic pain. Acupuncture and wearing a pelvic bandage have a positive effect on symphysiopathy.
Initial treatment for pubic symphysis should be conservative even if symptoms are severe. Treatment includes bed rest and the use of a pelvic brace or corset that tightens the pelvis. Early appointment of physiotherapy with dosed therapeutic exercises will help to avoid complications associated with prolonged immobilization. Walking should be done with assistive devices such as walkers.
In most cases (up to 93%), the symptoms of dysfunction of the pelvic ring, including the pubic joint, progressively subside and completely disappear six months after birth. In other cases, it persists, becoming chronic. However, if the diastasis exceeds 40 mm, then surgical treatment may be required.