Are babies immune systems stronger than adults
Infant Immune Systems Are Stronger Than You Think
New study may help explain why infants are less affected by COVID than adults
December 10, 2021
Share this page
As any parent knows, infants are prone to getting respiratory infections.
But a new study shows that the infant immune system is stronger than most people think and beats adults at fighting off new pathogens.
The infant immune system has a reputation for being weak and underdeveloped when compared to the adult immune system, but the comparison isn’t quite fair, says Donna Farber, PhD, professor of microbiology & immunology and the George H. Humphreys II Professor of Surgical Sciences at Columbia University Vagelos College of Physicians and Surgeons.
Watching T cells react to flu antigens helped the researchers identify why naive T cells from infant mice (shown above) responded faster and more robustly to the pathogen than the same cells from adult mice. The colors in the images represent different molecules involved in T cell activation.Babies do get a lot of respiratory illnesses from viruses, like influenza and respiratory syncytial virus, compared to adults. But unlike adults, babies are seeing these viruses for the first time. “Adults don’t get sick as often because we’ve recorded memories of these viruse, and the memories protect us,” Farber says, “whereas everything the baby encounters is new to them.”
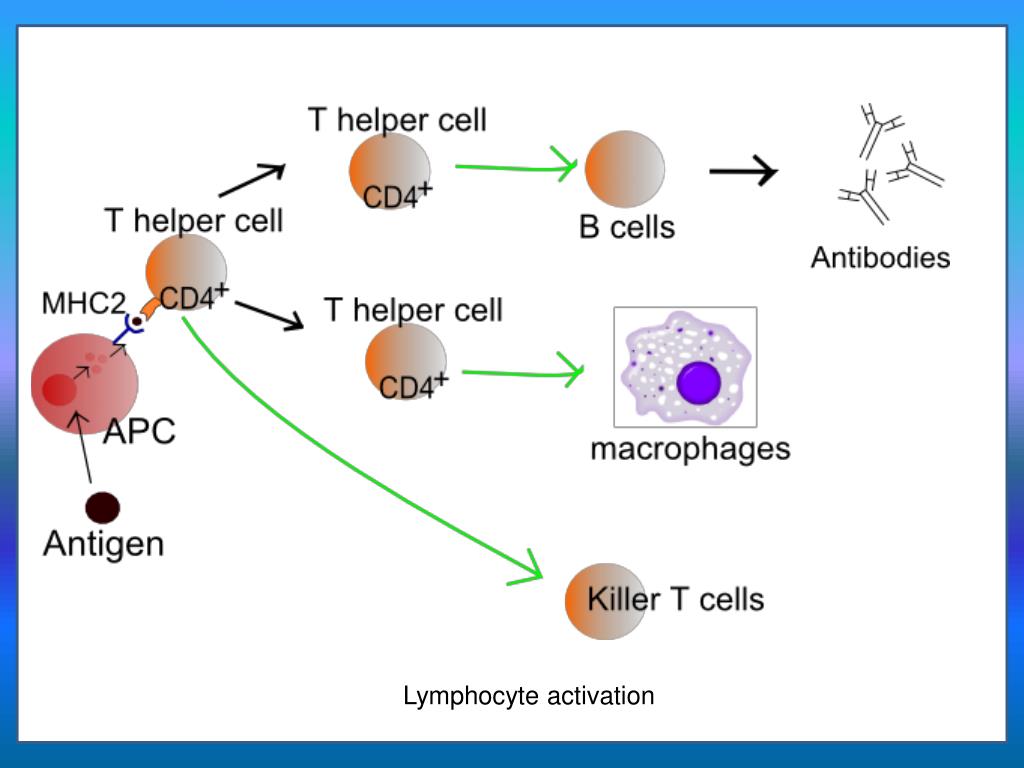
In the new study, Farber and colleagues leveled the playing field and only tested the immune system’s ability to respond to a new pathogen, essentially eliminating any contribution from immunological memories.
For the head-to-head comparison, the researchers collected naïve T cells—immune cells that have never encountered a pathogen—from both infant and adult mice. The cells were placed into an adult mouse infected with a virus.
In the competition to eradicate the virus, the infant T cells won handily: Naïve T cells from infant mice detect lower levels of the virus than adult cells and the infant cells proliferated faster and traveled in greater numbers to the site of infection, rapidly building a strong defense against the virus.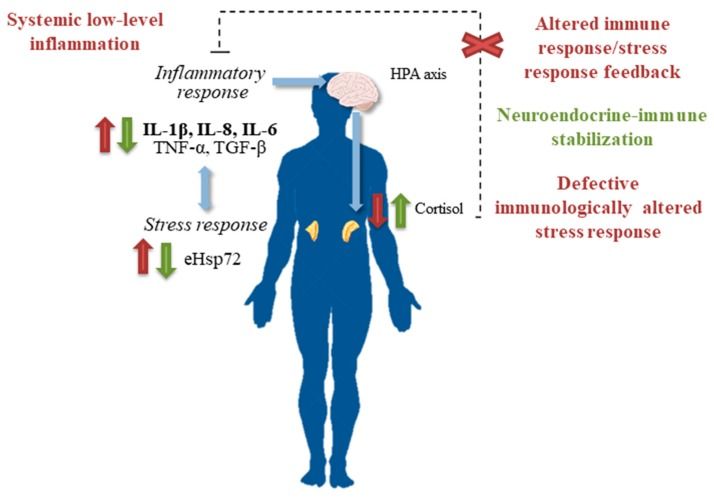 A laboratory comparison found similar enhancements among human infant compared to adult T cells.
A laboratory comparison found similar enhancements among human infant compared to adult T cells.
“We were looking at naïve T cells that have never been activated, so it was a surprise that they behaved differently based on age,” Farber says. “What this is saying is that the infant’s immune system is robust, it's efficient, and it can get rid of pathogens in early life. In some ways, it may be even better than the adult immune system, since it’s designed to respond to a multitude of new pathogens.”
That appears to be playing out in the case of COVID. “SARS-CoV-2 is new to absolutely everybody, so we’re now seeing a natural, side-by-side comparison of the adult and infant immune system,” Farber says. “And the kids are doing much better. Adults faced with a novel pathogen are slower to react. That gives the virus a chance to replicate more, and that’s when you get sick.”
The findings also help explain why vaccines are particularly effective in childhood, when T cells are very robust. “That is the time to get vaccines and you shouldn't worry about getting multiple vaccines in that window,” Farber says. “Any child living in the world, particularly before we started wearing masks, is exposed to a huge number of new antigens every day. They’re already handling multiple exposures.”
“That is the time to get vaccines and you shouldn't worry about getting multiple vaccines in that window,” Farber says. “Any child living in the world, particularly before we started wearing masks, is exposed to a huge number of new antigens every day. They’re already handling multiple exposures.”
The study could lead to better vaccine designs for children.
“Most vaccine formulations and doses are the same for all ages, but understanding the distinct immune responses in childhood suggests we can use lower doses for children and could help us design vaccines that are more effective for this age group,” Farber says.
References
More information
The paper, titled "Infant T cells are developmentally adapted for robust lung immune responses through enhanced T cell receptor signaling," was published Dec. 10 in Science Immunology.
Donna Farber also is chief of the Division of Surgical Sciences in the Department of Surgery, Columbia University Vagelos College of Physicians and Surgeons, and principal investigator at the Columbia Center for Translational Immunology.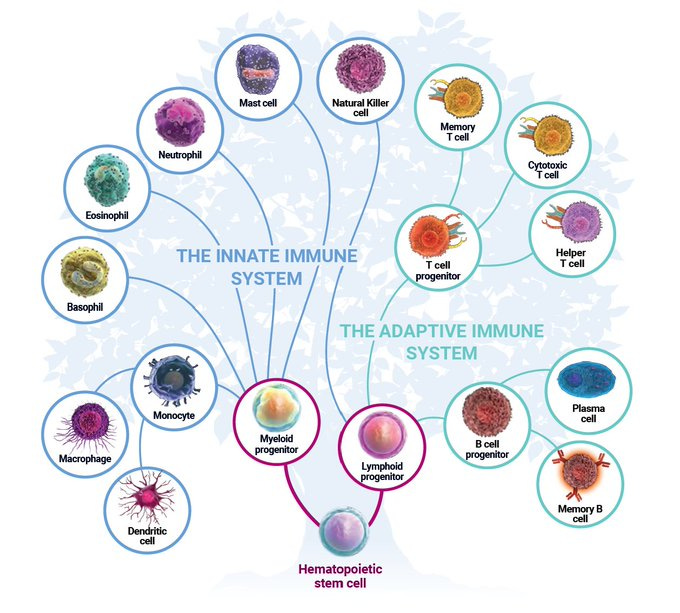
All authors (all from Columbia University unless noted): Puspa Thapa, Rebecca S. Guyer, Alexander Y. Yang, Christopher A. Parks, Todd M. Brusko (University of Florida), Maigan Brusko (University of Florida), Thomas J. Connors, and Donna L. Farber.
This work was supported by the U.S. National Institutes of Health (NIH grants AI100119, AI106697, K23 AI141686, and AI42288) and the Helmsley Charitable Trust. Studies were performed in the Columbia Center for Translational Immunology’s Flow Cytometry Core, supported by NIH grants S10RR027050 and S10OD020056, and the Columbia Stem Cell Initiative’s Flow Core, supported in part by NIH grant S10OD026845.
The authors declared no competing interests.
Study Finds Infant Immune Systems Stronger Than Commonly Perceived
The researchers collected naïve T cells, defined as immune cells that have never encountered a pathogen, from both infant and adult mice and placed the cells into adult mice infected with a virus.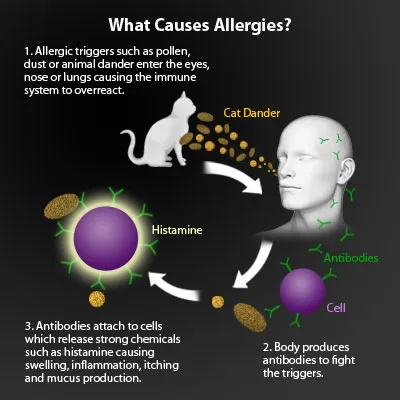
A new study shows that the infant immune system is stronger than most people think and can outdo adults in fighting off new pathogens, according to a Columbia University press release.
The immune systems of infants have a reputation for being weak and underdeveloped compared to the adult immune system; however, Donna Farber, PhD, professor of microbiology & immunology and the George H. Humphreys II Professor of Surgical Sciences at Columbia University Vagelos College of Physicians and Surgeons, said that unlike adults, babies are seeing viruses such as influenza for the first time.
“Adults don’t get sick as often because we’ve recorded memories of these viruses, and the memories protect us, whereas everything the baby encounters is new to them,” Farber said in the press release.
The new study only tested the immune system’s ability to respond to a new pathogen, essentially eliminating any contribution from immunological memories. The researchers collected naïve T cells, defined as immune cells that have never encountered a pathogen, from both infant and adult mice and placed the cells into adult mice infected with a virus.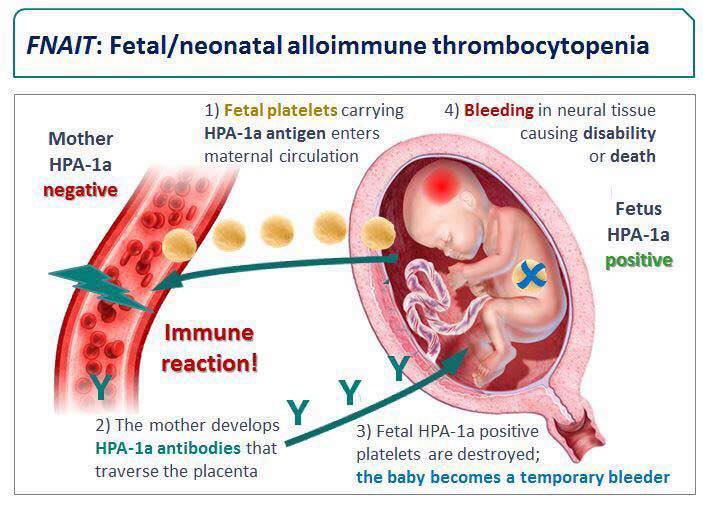
In the experiment, the naïve T cells from infant mice detected lower levels of the virus than adult cells and the infant cells proliferated faster and traveled in greater numbers to the site of the infection, rapidly building a strong defense against the virus. Further, a laboratory comparison found similar enhancements among human infant T cells compared to adults, according to the study authors.
“We were looking at naïve T cells that have never been activated, so it was a surprise that they behaved differently based on age,” Farber said in the press release. “What this is saying is that the infant’s immune system is robust, it's efficient, and it can get rid of pathogens in early life. In some ways, it may be even better than the adult immune system, since it’s designed to respond to a multitude of new pathogens.”
The new findings also help explain why vaccines are particularly effective in childhood, when T cells are very robust, according to Farber.
“That is the time to get vaccines and you shouldn't worry about getting multiple vaccines in that window,” Farber said in the press release.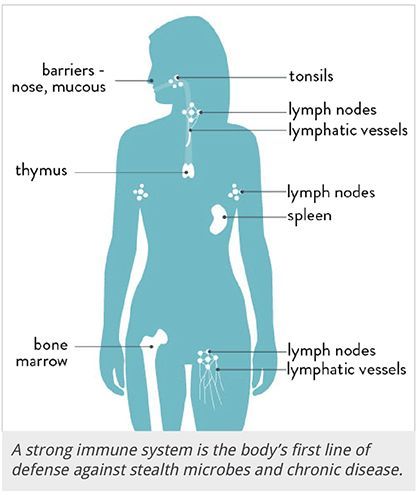 “Any child living in the world, particularly before we started wearing masks, is exposed to a huge number of new antigens every day. They’re already handling multiple exposures.”
“Any child living in the world, particularly before we started wearing masks, is exposed to a huge number of new antigens every day. They’re already handling multiple exposures.”
According to Farber, the study could lead to better vaccine designs for children.
“Most vaccine formulations and doses are the same for all ages, but understanding the distinct immune responses in childhood suggests we can use lower doses for children and could help us design vaccines that are more effective for this age group,” Farber said in the press release.
REFERENCE
Infant immune systems are stronger than you think. Columbia University Irving Medical Center. December 10, 2021. Accessed December 15, 2021. https://www.cuimc.columbia.edu/news/infant-immune-systems-are-stronger-you-think
Features of immunity in children of different ages
Irina Solomonovna Freidlin, Doctor of Medical Sciences, Professor in Microbiology, Virology and Immunology, Honored Scientist of the Russian Federation, Corresponding Member of the Russian Academy of Medical Sciences. Head of the Immunology Department of the Institute of Experimental Medicine, editor-in-chief of the Medical Immunology journal.
Head of the Immunology Department of the Institute of Experimental Medicine, editor-in-chief of the Medical Immunology journal.
The development of the body's immune system continues throughout childhood. In the process of development of the child's immune system, "critical" periods are distinguished, i.e. periods of maximum risk of developing infectious diseases associated with insufficiency of the immune system.
1. First critical period e
neonatal period (up to 29 days of life), when the child's body is protected almost exclusively by maternal antibodies obtained through the placenta and breast milk. The sensitivity of a newborn child to bacterial and viral infections during this period is very high. The group of increased risk of developing infections among newborns is made up of premature babies, and among them are small babies suffering from the most pronounced and persistent immunological defects.
2.
 Second critical period
Second critical period 4-6 months. life) is characterized by the loss of antibodies received from the mother. The ability to produce own antibodies during this period is limited by the weak synthesis of only immunoglobulins M, while immunoglobulins G are the main protective antibodies. Insufficiency of local mucosal protection is associated with a later accumulation of secretory immunoglobulin A. In this regard, the child's sensitivity to many airborne and intestinal infections during this period is very high.
3. The third critical period
(the 2nd year of life), when the child's contacts with the outside world and with infectious agents are significantly expanded. The child's immune response to infectious antigens remains defective. Local mucosal protection is still imperfect due to low levels of secretory IgA. The child's susceptibility to respiratory and intestinal infections is still high.
4. The fourth critical period
(6-7th years of life), when the absolute and relative number of lymphocytes in the child's blood decreases. During this period, the levels of immunoglobulins M and G in the blood of the child approach the levels of adults, but the level of immunoglobulin A still remains lower, which is associated with weak local mucosal protection. The content of immunoglobulin E, on the contrary, reaches its maximum level due to the high level of helminthic invasions, which explains the increased sensitivity to allergic reactions in children of this age group. The sensitivity of children of this age to infections is still high.
During this period, the levels of immunoglobulins M and G in the blood of the child approach the levels of adults, but the level of immunoglobulin A still remains lower, which is associated with weak local mucosal protection. The content of immunoglobulin E, on the contrary, reaches its maximum level due to the high level of helminthic invasions, which explains the increased sensitivity to allergic reactions in children of this age group. The sensitivity of children of this age to infections is still high.
5. Fifth critical period
adolescence (in girls from 12-13 years old, in boys from 14-15 years old), when a growth spurt is combined with a relative decrease in the mass of lymphoid organs, and the onset of secretion of sex hormones causes depression cellular mechanisms of immunity. At this age, external, often adverse, effects on the immune system increase sharply. Children of this age are characterized by high sensitivity to viral infections.
In each of these periods, the child's immune system is characterized by a number of features
At birth, neutrophils predominate in the child's blood. By the end of the first week of life, the number of neutrophils and lymphocytes levels off - the so-called "first cross" - with a subsequent increase in the number of lymphocytes, which in the next 4-5 years of life remain the predominant cells among the child's blood leukocytes. The "second crossover" occurs in a child aged 6-7 years, when the absolute and relative number of lymphocytes decreases and the leukocyte formula takes on the form characteristic of adults. When evaluating the data of a clinical blood test in children, these "crosses" must be taken into account.
By the end of the first week of life, the number of neutrophils and lymphocytes levels off - the so-called "first cross" - with a subsequent increase in the number of lymphocytes, which in the next 4-5 years of life remain the predominant cells among the child's blood leukocytes. The "second crossover" occurs in a child aged 6-7 years, when the absolute and relative number of lymphocytes decreases and the leukocyte formula takes on the form characteristic of adults. When evaluating the data of a clinical blood test in children, these "crosses" must be taken into account.
An increased number of granulocytes in the blood of newborns to some extent compensates for the insufficient activity of their protective functions. The absolute number of blood monocytes in newborns is higher than in older children, but they also have a low protective activity.
The content of the antibacterial enzyme lysozyme in the blood serum of a newborn exceeds the level of maternal blood already at birth, it increases during the first days of life, and by the 7-8th day of life it somewhat decreases and reaches the level of adults.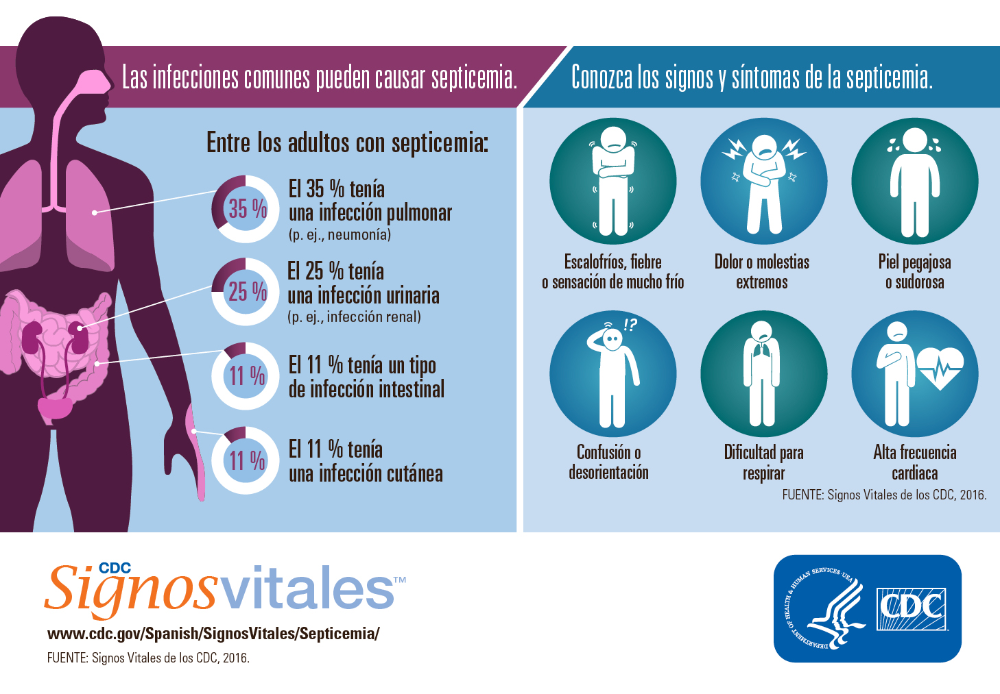 And in the lacrimal fluid of newborns, the content of lysozyme is lower than in adults, which is the reason for the increased frequency of conjunctivitis in newborns.
And in the lacrimal fluid of newborns, the content of lysozyme is lower than in adults, which is the reason for the increased frequency of conjunctivitis in newborns.
The low content of the main components of the complement system in the blood of newborns is the reason for the insufficient auxiliary activity of blood serum during phagocytosis. Only by the second year of life, the production of the components of the complement system finally matures.
In the blood of newborns, the content of natural killers is significantly lower than in adults. Natural killers of children's blood are characterized by reduced cytotoxic and secretory activity.
As can be seen from the above, in newborns, all the main mechanisms of nonspecific defense of the body against pathogenic bacteria and viruses are sharply weakened, which explains the high sensitivity of newborns and children of the first year of life to bacterial and viral infections.
Defects in phagocytic cells are most pronounced in premature newborns and children with intrauterine growth retardation.

These children are characterized by prolonged infections (eg, pneumonia) and poor response to antibiotic therapy. In recent years, attempts have been made to use combined treatment with an immunomodulator 9 in these children.0009 Likopid® showed that clinical signs of improvement in the condition of children, reduction in the duration of the disease are combined with the correction of defective functions of phagocytic cells.
After birth, the child's immune system receives the strongest stimulus for rapid development in the form of a stream of foreign (microbial) antigens entering the child's body through the skin, mucous membranes of the respiratory tract, gastrointestinal tract, actively populated by microflora in the first hours after birth.
Microorganisms entering through the gastrointestinal tract are the main engines of the maturation of the entire immune system of the child.
The rapid development of the immune system is manifested by an increase in the mass of lymph nodes, which are populated by T- and B-lymphocytes. After the birth of a child, the absolute number of lymphocytes in the blood rises sharply already at the 1st week of life (the first cross in the white blood formula). Physiological age-related lymphocytosis persists for 5-6 years of life and can be considered as compensatory.
After the birth of a child, the absolute number of lymphocytes in the blood rises sharply already at the 1st week of life (the first cross in the white blood formula). Physiological age-related lymphocytosis persists for 5-6 years of life and can be considered as compensatory.
The relative number of T-lymphocytes in newborns is lower than in adults, but due to age-related lymphocytosis, the absolute number of T-lymphocytes in the blood of newborns is even higher than in adults. Features of T-lymphocytes of newborns are associated with the release of immature precursors into the bloodstream. It is precisely in connection with the defectiveness of cellular defense mechanisms that a high degree of risk of tuberculosis remains throughout the entire period of childhood due to the widespread circulation of the causative agent of tuberculosis.
The weakness of cellular defense mechanisms makes children particularly susceptible to viral and fungal infections, protection against which requires the participation of functionally complete T-lymphocytes.
Among children aged 1 to 6 years, a group of "frequently and long-term ill" acute respiratory viral infections (ARVI) is often distinguished. When immunological examination of such children, they usually reveal defects in the main protective mechanisms. Such findings were the basis for preventive immunocorrection, in which children received the immunomodulator Likopid® outside the period of exacerbation of the disease. The effectiveness of this method of immunocorrection was monitored by the frequency and duration of ARVI episodes and by changes in immunological parameters.
The frequency of diseases in the group of children who received Licopid® without exacerbation decreased by half.
At the same time, a significant increase in the content of secretory immunoglobulin A in the saliva of children of this group, which is the most important factor in protecting mucous membranes from bacteria and viruses, was noted.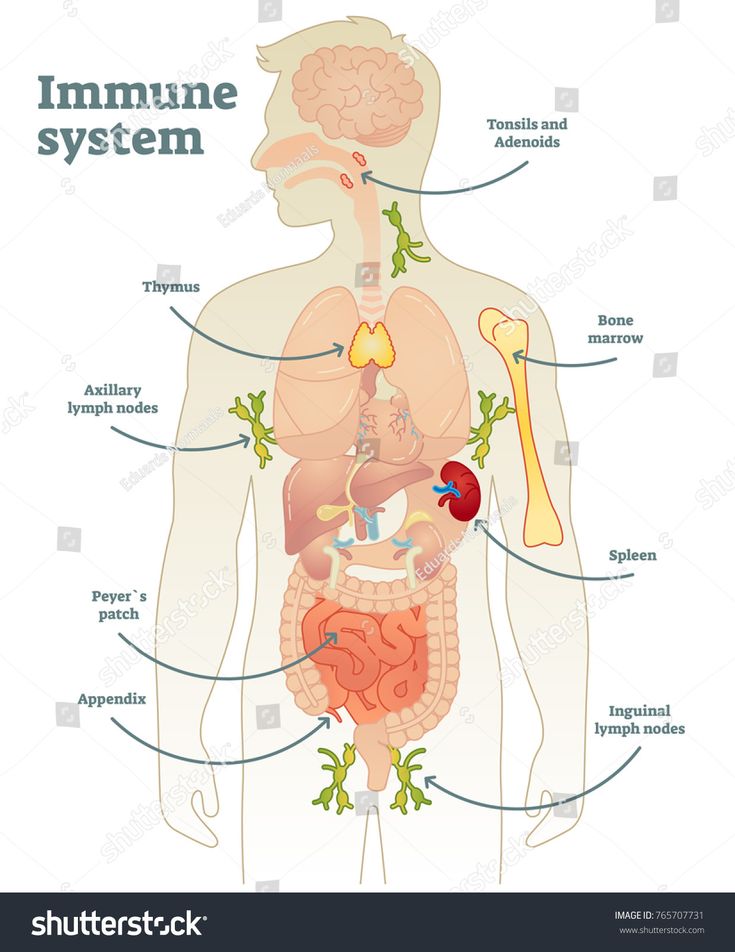
In a newborn, the thymus is fully developed and reaches its maximum size during the first year of life. The intense functioning of the thymus, in which all T-lymphocytes mature, is maintained during the first 2-3 years of life. The rapid increase in thymus mass in the first 3 months of life continues at a slower pace until the age of 6, after which the thymus mass begins to decline. From the age of two, the production of T-lymphocytes also begins to decrease. The process of age-related involution of the thymus accelerates in adolescence. During the first half of life, true thymic tissue is gradually replaced by adipose and connective tissue. From this it follows that the thymus manages to carry out its main function of the formation of T-lymphocytes in the first years of life.
Therefore, during the first three years of life, children are routinely vaccinated against all the most dangerous and frequent infectious diseases: tuberculosis, poliomyelitis, diphtheria, tetanus, whooping cough, measles, and viral hepatitis.

At this age, the body's immune system responds to vaccination (with killed or weakened pathogens, their antigens, their neutralized toxins) by the formation of long-lived memory T-cells, which provide a quick and effective protective response when infected with an infectious agent. It is in childhood, during the flowering of thymus functions, that specific antimicrobial immunity and the corresponding immunological memory are formed, which should be enough for the rest of life.
Absolute and relative lymphocytosis in the blood of children reflects the process of accumulation of lymphocytes that have specific receptors for recognition of various foreign antigens. This process is completed, mainly by the age of 5-7, which is manifested by a change in the blood formula: lymphocytes cease to dominate and neutrophils begin to predominate.
The lymph nodes of a young child respond to any infection, to any inflammatory process with a pronounced increase in size (swelling).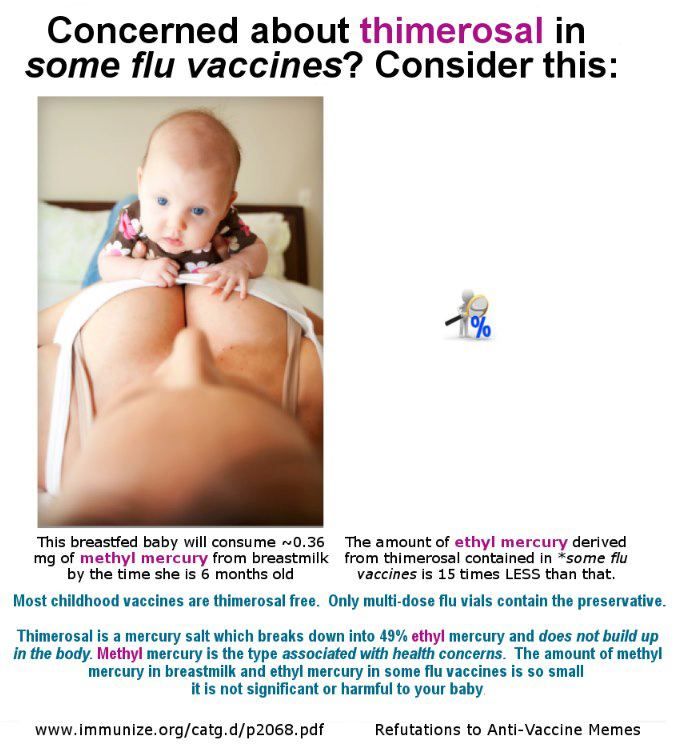 For children of the first years of life, a similar response to infections is characterized by an increase in the volume of lymphoid tissue associated with mucous membranes, for example, the larynx, which is associated with an increased frequency and risk of rapid development of edema in the larynx in children with infections and allergic reactions. The lymphoid tissue associated with the gastrointestinal tract remains immature in children of the first years of life, which is associated with a high risk of intestinal infections.
For children of the first years of life, a similar response to infections is characterized by an increase in the volume of lymphoid tissue associated with mucous membranes, for example, the larynx, which is associated with an increased frequency and risk of rapid development of edema in the larynx in children with infections and allergic reactions. The lymphoid tissue associated with the gastrointestinal tract remains immature in children of the first years of life, which is associated with a high risk of intestinal infections.
Immunoglobulin A in the blood of newborns is either absent or present in a small amount (0.01 g/l), and only at a much older age reaches the level of adults (after 10-12 years). Secretory immunoglobulins A are absent in newborns, and appear in secrets after the 3rd month of life. Adult levels of secretory immunoglobulin A in mucosal secretions are reached by the age of 2-4 years. Until this age, the local protection of mucous membranes in children remains sharply weakened.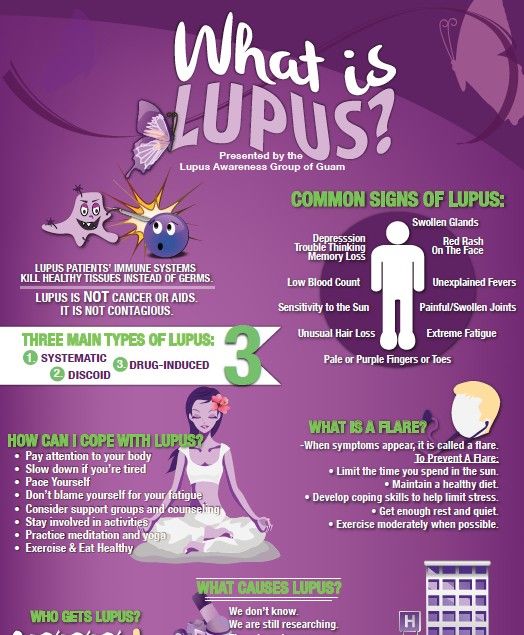 When breastfeeding, the lack of local mucosal immunity is partially compensated by the intake of secretory immunoglobulin A with mother's milk.
When breastfeeding, the lack of local mucosal immunity is partially compensated by the intake of secretory immunoglobulin A with mother's milk.
Newborn's body defense reserve is associated with breastfeeding.
With mother's milk, ready-made antibacterial and antiviral antibodies, secretory immunoglobulins A and G, enter the child's body. Secretory antibodies go directly to the mucous membranes of the gastrointestinal and respiratory tracts and protect these mucous membranes of the child from infections. Due to the presence of special receptors on the mucosa of the gastrointestinal tract of the newborn, immunoglobulins G penetrate from the gastrointestinal tract of the child into his bloodstream, where they replenish the supply of maternal antibodies that previously entered through the placenta.
An increase in the reserves of the immune system and the prevention of infections in newborns is achieved by breastfeeding.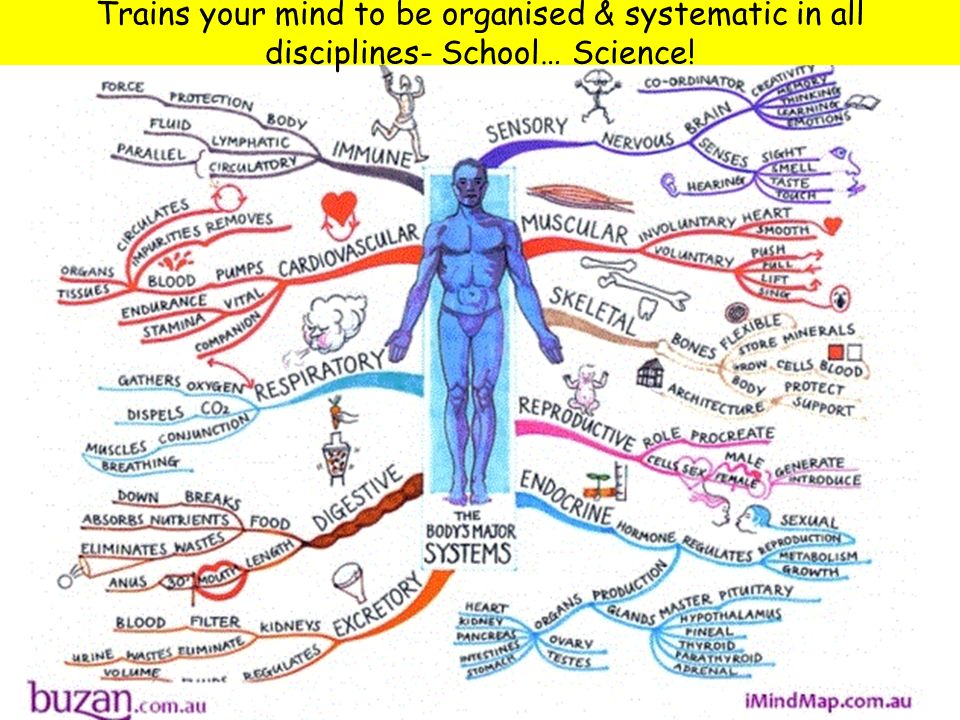 Human milk contains not only a complex of nutritional components necessary for a child, but also the most important factors of nonspecific protection and products of a specific immune response in the form of class A secretory immunoglobulins. Secretory IgA supplied with breast milk improves local protection of the mucous membranes of the gastrointestinal, respiratory and even urinary tract of the child.
Human milk contains not only a complex of nutritional components necessary for a child, but also the most important factors of nonspecific protection and products of a specific immune response in the form of class A secretory immunoglobulins. Secretory IgA supplied with breast milk improves local protection of the mucous membranes of the gastrointestinal, respiratory and even urinary tract of the child.
Breastfeeding through the introduction of ready-made antibacterial and antiviral antibodies of the SIgA class significantly increases the resistance of children to intestinal infections, respiratory infections, and otitis media. The mother's immunoglobulins and lymphocytes, which come with breast milk, stimulate the child's immune system, providing long-term antibacterial and antiviral immunity.
Breastfeeding increases the immune response of children to vaccines.
Breastfeeding prevents the development of allergic diseases and the autoimmune disease celiac disease.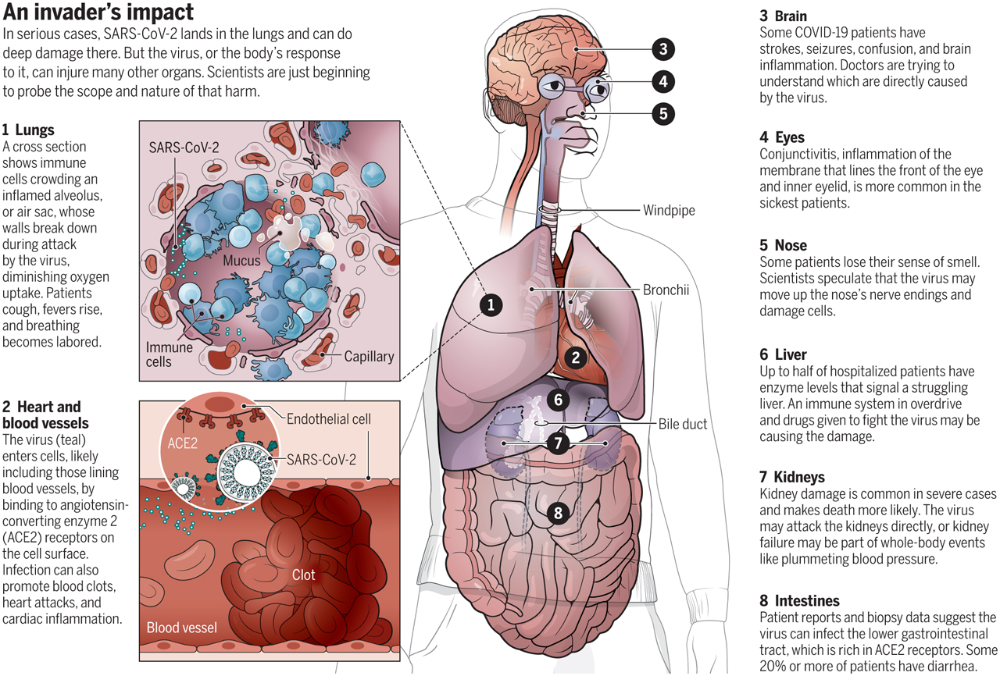 One of the components of breast milk - lactoferrin is involved in the stimulation of immunological functions, being able to penetrate into immunocompetent cells, bind to DNA, inducing transcription of cytokine genes. Such components of breast milk as specific antibodies, bacteriocidins, inhibitors of bacterial adhesion have direct antibacterial activity.
One of the components of breast milk - lactoferrin is involved in the stimulation of immunological functions, being able to penetrate into immunocompetent cells, bind to DNA, inducing transcription of cytokine genes. Such components of breast milk as specific antibodies, bacteriocidins, inhibitors of bacterial adhesion have direct antibacterial activity.
All of the above requires great attention in preventive work with pregnant women to explain the benefits of breastfeeding. Special educational programs are useful, involving not only women, but also their husbands, parents and other persons who can influence a woman's decision to breastfeed a child.
As the child's immune system matures, the mechanisms of a specific immune response improve, the risk of an overreaction of his immune system to contact with environmental antigens and the development of allergic reactions increases. Even intrauterine contact of the fetus with pollen allergens inhaled by the mother leads to the subsequent development of atopic reactions and diseases in the newborn.
A high risk of developing atopic reactions in children of the first years of life is associated with the predominance of their differentiation of T-helper 2, which controls the synthesis of immunoglobulin E and increased secretion of histamine by basophils and mast cells. A low level of secretory IgA on mucous membranes in children contributes to the unhindered penetration of allergens through the mucous membranes of the respiratory and gastrointestinal tract.
A feature of atopic reactions in children of the first years of life can be considered a higher frequency of food and a lower frequency of dust/pollen allergy compared to adults.
Children are often allergic to cow's milk (2-3% of children in industrialized countries). Cow's milk contains more than 20 protein components, and many of them are capable of causing the synthesis of immunoglobulin E. The widespread occurrence of such an allergy makes it difficult to artificially feed children, forcing them to look for adequate substitutes (for example, soy products).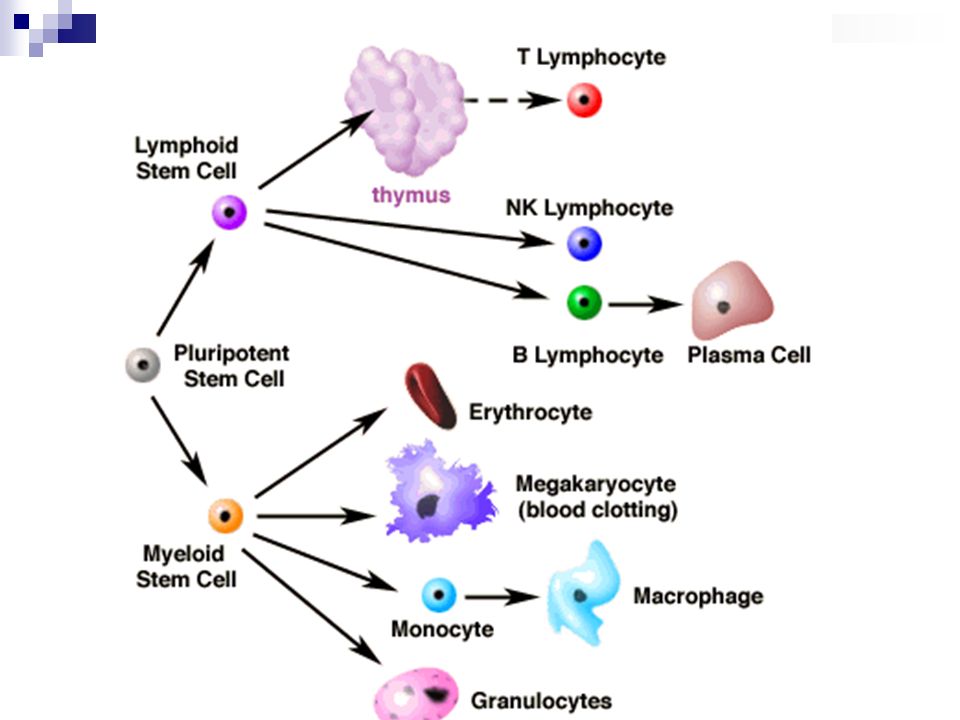
The described manifestations of immunodeficiency in children of the first years of life are usually assessed as "physiological", i.e. beyond the age limits. However, the increased sensitivity to infections caused by these age-related immunological defects forces us to look for ways of immunocorrection.
Immunomodulator Likopid® 1 mg
Above we have considered examples of the use of the immunomodulator Likopid® 1 mg , including for the purpose of immunocorrection. The immunocorrective effect of a balanced diet for a child, measures to harden the body, and dosed physical activity have been repeatedly proven.
A CHILD'S IMMUNITY BEGINS IN THE Maternity Hospital!
What affects the development of a child's immunity and what measures should parents take to increase the body's defenses? Andrey Petrovich Prodeus — pediatrician-immunologist, doctor of medical sciences, professor, chief pediatrician of Children's City Clinical Hospital No. 9 tellsthem. G.N. Speransky, chief freelance pediatric allergist-immunologist of the Ministry of Health of the Moscow Region, head of the Department of Clinical Immunology and Allergology of the Higher Medical School.
What does high immunity in a child depend on?
I would single out four main factors responsible for strong immunity.
The first is a full-term pregnancy. If a child is born on time, it means that his immune system has formed sufficiently to meet the world of viruses and bacteria. The more premature a baby is born, the more immature its protective cells will be and the more difficult it will be for his body to adapt to the characteristics of the environment.
The second factor is the type of delivery. If the birth ends with a caesarean section, then the child will receive a completely different microbiota: he will not pass through the woman's birth canal and will not "pick up" the mother's bacteria, which form the initial interaction between him and the environment.
The third factor is breastfeeding. The longer the baby receives mother's milk, the better will be his immune response to infections from the outside world.
The fourth factor is timely vaccination. Properly done and with a personal approach to the child, it will form the normal development of the immune response.
Babies born by caesarean section are several times more likely to suffer from allergies, be overweight and respond less well to vaccinations.
Do all children need to boost their immunity?
Definitely not for everyone. Children have another interesting feature: they do not always show an active aggressive response to some kind of infection. Imagine that a virus or bacterium enters the nasopharyngeal mucosa and an adult develops nasal congestion, snot, and a red throat. Is it good or bad? In principle, it’s good, because it says that our immunity has begun a war against infection.
On the other hand, this is nothing but a manifestation of a disease.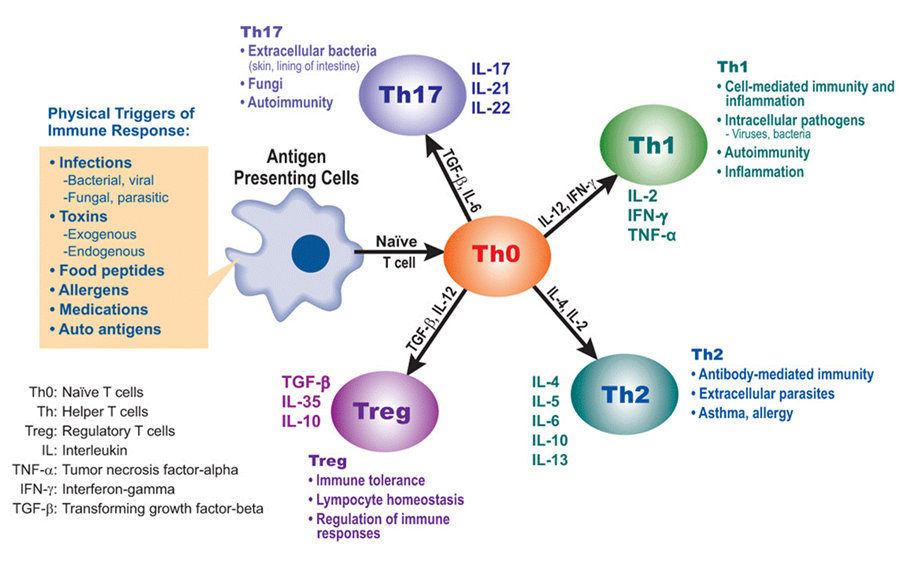 Ideally, the picture looks like this: a virus or bacterium got on the mucous membrane, but the immune system dealt with it so quickly and effectively that we did not notice it. Conclusion: do we want to increase the strength of the immune response indefinitely? Probably not always.
Ideally, the picture looks like this: a virus or bacterium got on the mucous membrane, but the immune system dealt with it so quickly and effectively that we did not notice it. Conclusion: do we want to increase the strength of the immune response indefinitely? Probably not always.
Because if we actively strengthen the response of, say, a child of the 1st year of life, then instead of calmly reacting to some virus or bacterium that comes to him from outside, he will begin to suck badly, not sleep and put on a little weight, and parents will start to worry a lot. But if, in response to the invasion of a viral agent, nasal congestion appears in a 14-year-old teenager, then nothing terrible will happen: he will blow his nose and still go to play football.
That is, the same problem can be perceived differently and have different consequences for children of different ages. The difference in adaptive immune response is designed in such a way by nature that it limits the strength of the response in the child until he adapts to the environment. And you should not interfere in this process.
And you should not interfere in this process.
Hardening can help in strengthening the immune system?
I wouldn't use that wording. Any kind of hardening, as well as playing sports, is not a little about immunity. Here we are talking about general physical processes. We, pediatricians, only welcome them, because it instills healthy lifestyle skills in a child.
However, to date, there is no direct clinically proven link between these activities and the strengthening of the immune response anywhere in the world. Yes, indeed, sports and hardening can theoretically increase the adaptive abilities of the body, but the question is exclusively individual: it will help someone, but not so much for someone. Therefore, I would recommend that all parents treat these things without fanaticism and do not tyrannize children with sports clubs or cold showers "in the name of immunity."
How can parents strengthen their child's immunity at home?
There are two cornerstones: a daily routine and a balanced diet.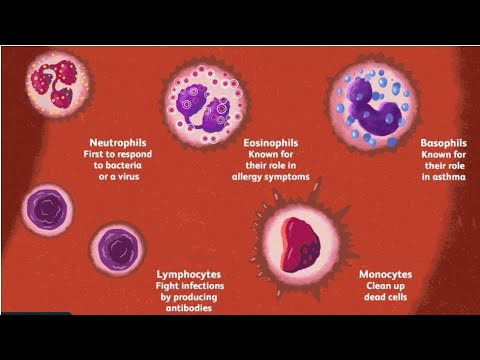 The daily routine for a child is absolutely essential for strengthening the immune response. Why? Because all organs and systems of the body, including immune cells and bone marrow, are most active from ten in the evening until about three in the morning. Therefore, if a child goes to bed at eleven or twelve, his immune system (especially its "officers" - T-cells) will not be able to recover normally. Therefore, a systematic "torn" regime for a child is absolutely contraindicated precisely from the standpoint of immunity, and not just his mental health.
The daily routine for a child is absolutely essential for strengthening the immune response. Why? Because all organs and systems of the body, including immune cells and bone marrow, are most active from ten in the evening until about three in the morning. Therefore, if a child goes to bed at eleven or twelve, his immune system (especially its "officers" - T-cells) will not be able to recover normally. Therefore, a systematic "torn" regime for a child is absolutely contraindicated precisely from the standpoint of immunity, and not just his mental health.
As for normal baby food, you need to pay attention to the constant presence of two components in food: vitamin D and iron. It is vitamin D that helps our cells fight viral infection. If earlier its prophylactic dose was considered to be 400 units per day, now at least 1000 units are prescribed. Statistics show that approximately two-thirds of children who live north of 42nd latitude have a decrease in vitamin D levels, and some of them are completely deficient.
An equally important component for immunity is iron. Its assistance in the efficient functioning of the immune system's T-cells is considered one of its main functions, in addition to the formation of hemoglobin. The ability of the body to respond with the “correct” inflammation to a bacterial or viral infection is impossible without a sufficient amount of iron in the blood. Therefore, it is necessary to raise the question not only of getting more of this element with food (the so-called heme iron in the form of meat, poultry and fish), but also about prescribing courses of iron preparations that are easily absorbed by the doctor.
There is a dangerous myth in Russia: drink pomegranate juice, eat beets, buckwheat and green apples, and you will have happiness in the form of iron. Will not be! Because the absorption of iron from plant sources is approximately 5% of its total amount in them.
Today even doctors often argue about the importance of vaccination for children. What is your opinion on this matter?
What is your opinion on this matter?
Vaccinations are not meant to please doctors or drug companies. By and large, healthy immunity begins precisely in the maternity hospital, when a newborn receives his first vaccinations, and comes into this world already protected.
Vaccination was invented either for those diseases whose consequences are fatal, that is, from them there is a high risk of death (for example, with meningitis, rabies, tetanus). Or for those for whom there is no therapy (hepatitis B, mumps, measles, rubella, or the same covid). Yes, a person can easily get sick with them, but no one guarantees this.
Case in point: 10% of boys who recover from mumps become infertile. In this regard, I always have a question for “refusenik” parents: who gave you the right to doom a child to such a fate?!
There is a popular belief that only healthy people should be vaccinated. No! Immune-compromised children, who have peculiarities in the development of the immune response, need it more.