Do u poop more when pregnant
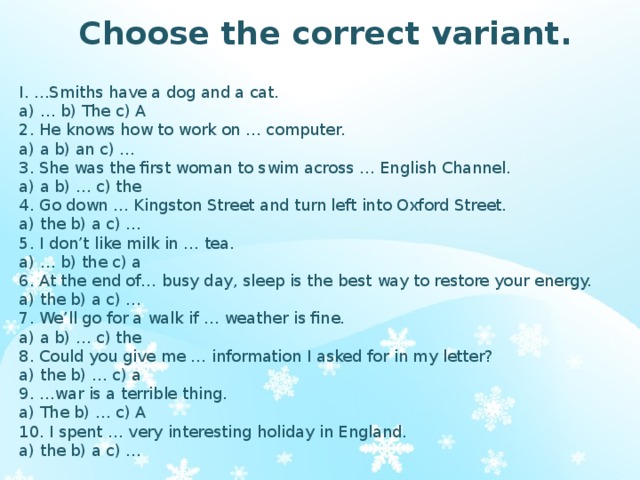
Is Pooping A Lot A Sign Of Pregnancy?
You've heard all about morning sickness and tender boobs as early signs of pregnancy, but what about your uh...bathroom habits? Whether you’re newly pregnant or wondering if you could be, there are some digestive changes that come along with pregnancy that you should know about, particularly if you're suddenly running to the toilet for number twos all the time. (Not fun!)
Sooo...is pooping a lot one of the signs of early pregnancy?Actually, this is a bit of a myth, says Temeka Zore, MD, a board-certified ob-gyn and reproductive endocrinologist at Spring Fertility. Pooping a lot isn't linked to the beginning of most pregnancies. In fact, constipation is more likely.
Hormonal changes, particularly during the menstrual cycle, can have an affect on bowels, especially for people with IBS, research has found. But without a regular cycle during pregnancy, you may not notice the same digestive patterns (a. k.a. period poops) that you might have during menstruation. (Still, that's not to say *no one* experiences an increase in poops during early pregnancy, it's just not super common.)
During the early stages of pregnancy, the first thing you’ll probably notice is your period dropping off. Then, it’s common to experience nausea or vomiting, breast tenderness, fatigue, and increased urination, says Dr. Zore. Bloating and cramping, particularly of the uterus, are also some things you should be prepared for. It’s important to note that most of these unpleasant symptoms won’t last for too long in your pregnancy (thankfully!).
What if I *am* pregnant and pooping more frequently—normal?If your stomach issues go beyond occasional cramping, bloating, and fullness—these are signs that the uterus is expanding and compressing your bowels, says Dr. Zore—there might be something else going on. Of course, if you’re already aware that you have a form of inflammatory bowel disease, just note that the symptoms may flare up during pregnancy, according to a study published in Gastroenterology and Hematology.
Related Story
- 7 IBS Symptoms Every Woman Should Know About
If you’ve never been diagnosed with any gastroenterological conditions and are experiencing frequent bouts of diarrhea throughout your pregnancy, for example, this is worth getting checked out, since it could be a sign of a more serious inflammatory bowel condition, like ulcerative colitis or Crohn’s disease. "These include multiple episodes of diarrhea per day, bloody stools, fever, and abdominal pain,” Dr. Zore explains. It’s important to pay attention to any of these symptoms, whether they’re mild, moderate, or severe, she says.
What can you do if you have pregnancy diarrhea?Again, diarrhea throughout pregnancy is actually less typical than constipation, but if you do experience it, it's more likely to happen closer to the time of delivery. “At that time, your uterus starts producing hormones known as prostaglandins, which help soften the cervix and prepare the uterus to contract in labor,” explains Dr. Zore.
Zore.
The prostaglandins also get the smooth muscles of the digestive tract moving, so stool will pass more quickly, Dr. Zore says. You may just experience increased frequency or urgency to go to the bathroom, or you may even get diarrhea in some cases.
If you do have diarrhea, hydration is super important. Basically, loading up on water is your best defense mechanism. Eating a diet rich in fiber while pregnant is also key to make sure you don’t end up with loose stools, says Dr. Zore.
What other poop changes can happen during pregnancy?You’re likely to have constipation at any point of your pregnancy due to the hormonal changes going on. “The elevated progesterone levels in pregnancy lead to smooth muscle relaxation in the uterus (to prevent uterine contractions early on) but can also lead to the relaxation of the smooth muscle in the colon, leading to reduced bowel activity and constipation,” says Dr. Zore.
Zore.
Related Story
- 12 Foods to Eat When You’re Constipated
The other unpleasant symptom you may experience during pregnancy is hemorrhoids, which can affect 30 to 40 percent of people during pregnancy and the postpartum stage, according to Dr. Zore. They can make constipation worse, first of all, but can also cause pain and even bleeding. This makes your hydration and high-fiber diet even more of a priority, Dr. Zore says.
If you’re experiencing persistent bleeding or bloody stools, that is a red flag of a potentially more serious condition.
When should you see a doctor?Any time you notice blood in your stools while pregnant, contact your ob-gyn to check in on what could be wrong, Dr. Zore says. If you have persistent diarrhea that’s causing you to lose weight during pregnancy or is accompanied by a fever greater than 100.4 degrees, alert your doc, she adds. And, if you find yourself not making it to the bathroom, or having extreme stomach pains or cramping, you should bring these symptoms up to your gyno, too.
And, if you find yourself not making it to the bathroom, or having extreme stomach pains or cramping, you should bring these symptoms up to your gyno, too.
In some cases, it might benefit you to see a G.I. doctor as well as your ob-gyn. “If you have a known history of inflammatory bowel disease and notice you are having a flare of your symptoms, you should contact your ob-gyn as well as your gastroenterologist,” says Dr. Zore. Or, if your pregnancy is causing stomach issues beyond the scope of what seems normal, it wouldn’t hurt to have a check up with a gastroenterologist to make sure your digestion is healthy.
The bottom line: Pooping more and having diarrhea usually isn't an early sign of pregnancy. Most pregnant women deal with constipation. If you are having diarrhea, check in with your ob-gyn.
Mara Santilli
Mara is a freelance writer and editor specializing in culture, politics, wellness, and the intersection between them, whose print and digital work has appeared in Marie Claire, Women’s Health, Cosmopolitan, Airbnb Mag, Prevention, and more. She’s a Fordham University graduate who also has a degree in Italian Studies, so naturally she’s always daydreaming about focaccia.
She’s a Fordham University graduate who also has a degree in Italian Studies, so naturally she’s always daydreaming about focaccia.
What you need to know
What’s going on in our guts when we fall pregnant and are growing a baby? A LOT, it turns out. In fact, pregnancy brings with it some shifts that directly impact our gut health … and our poop!
The amazing gut
Did you know that digestion begins in your mouth well before any food reaches your gut? The food then winds its way to your bottom as part of this truly remarkable process. What happens along the way when you are pregnant, however, can be a bit mystifying and quite different to pre-pregnant days.
The gut’s microbiome – which provides a range of beneficial properties – is primarily located in the gastrointestinal tract. The microbiome can affect how we feel, so looking after your gut is obviously important.
Pregnancy poop 101
So, how else can you keep your gut healthy and happy as you grow a little human? Tweaking your diet to consider nutrition is a great place to start, especially when you consider the host of digestive and poopy complaints pregnant ladies often report.
And look, while we’re talking about poop, let us count the ways that gut health and pregnancy might change things up in that department. If you’re going through these things you are NOT ALONE!
1. Constipation
Hormones, changes in physical activity levels, physiological shifts and changes in diet can all contribute to constipation in expectant mums. Pregnancy vitamins also often contain an iron supplement that can be constipating. A diet high in fibre, drinking plenty of water and daily exercise can help shift things.
2. Uncomfortable pooping
Pooping can sometimes be uncomfortable during pregnancy due to a common side-effect – haemorrhoids. Haemorrhoids are swollen veins inside the back passage that can become enlarged when carrying a baby. If you’re enduring this uncomfy condition, there are many different treatments that can relieve discomfort and make pooping easier. But remember, it’s always best to visit your doctor for guidance and advice.
3.
 Diarrhoea
DiarrhoeaDiarrhoea is characterised by the passing of three or more stools per day, usually with a loose consistency. Some women find they experience diarrhoea in early pregnancy, though it’s less common than constipation. Sometimes, shifting to a more nutritious diet – as many women do when they have a baby on board – can change their bowel movements temporarily. Hormones, drinking more water or changing the way they exercise can change things up too. If you’re experiencing diarrhoea, check in with your doctor to discuss relevant treatment.
4. Frequent pooping
Frequent bowel movements during early pregnancy, much like frequent peeing, are related to hormonal changes. It’s worth noting that many prenatal vitamin supplements contain docusate sodium, which acts as a stool softener, while some foods can also contribute to more frequent pooping. Avoid spicy, fried and fatty foods. This should right itself as you move into the second trimester.
Unsurprisingly, great nutrition, daily exercise, getting enough sleep and avoiding stress will also contribute to a healthier gut and may assist with your pregnancy poop problems. Fortunately, it’s short-term pain for a long-term gain!
Fortunately, it’s short-term pain for a long-term gain!
This is a sponsored post for Life-Space Probiotics
Posted on by Babyology
Get more babyology straight to your inbox
Join now
Treatment of constipation in pregnant women in a private clinic
This is one of the most common, but at the same time the most delicate problems that occur in at least 50% of pregnant women. In a normal state, bowel movements should be daily and in sufficient volume. Any deviations in this process require attention and adjustment of the diet, lifestyle and even psychological attitude. From a physiological point of view, problems in the work of the gastrointestinal tract are explained by hormonal changes and the physiological characteristics of the body of a pregnant woman (under the influence of various processes in different phases of pregnancy, the contraction of the smooth muscles of the intestine is weakened, in addition, the enlarged uterus compresses the intestines, etc. ).
).
Among other - non-medical reasons - the most common are the features of a woman's lifestyle: systematic stress; lack of mobility; lack of fiber; low water intake (not liquids!) and/or high intake of refined foods and foods with a high composition of sugar, homogenized fats and salt (fast food). “Refined foods are refined oils, polished rice, white flour and all the familiar white refined sugar, plus fast food with a high composition of sugar, homogenized fats and salt, which slow down the absorption of nutrients by the body and the passage of food in the intestines” (Laima Lankmane, naturopath, herbalist).
Homeopaths say that constipation is not only a “problem” of the rectum, “it is a problem of the whole organism as a whole and it must be solved in a complex way” (D.V. Arkhipova, Ph.D., homeopath): for example, this may be an allergic reaction to certain foods. Therefore, constipation is, in principle, an individual problem, and an individual approach will be the most effective solution to the problem: “Even equally pregnant women do not have 2 identical constipations: some had them before pregnancy, others did not eat properly, others did not move. All good wishes for real constipation will work only in 10% of cases. The only right decision is a full-fledged visit to a homeopath, who will approach the solution of the disharmony that has arisen, taking into account all the individual characteristics of a woman, looking at her as an integral unique system ”(A.S. Gavrilenko, obstetrician-gynecologist, Ph.D., homeopath , reflexologist).
All good wishes for real constipation will work only in 10% of cases. The only right decision is a full-fledged visit to a homeopath, who will approach the solution of the disharmony that has arisen, taking into account all the individual characteristics of a woman, looking at her as an integral unique system ”(A.S. Gavrilenko, obstetrician-gynecologist, Ph.D., homeopath , reflexologist).
First, about how NOT to solve the problem of constipation: classic laxatives such as hay, aloe vera and castor oil are contraindicated for pregnant women - they can cause premature contractions.
Now about what is POSSIBLE and NEEDED.
DIET
- Need to temporarily eliminate dairy products. “The main milk protein, casein, is one of the most difficult to digest proteins and is also a strong allergen. The fact that cottage cheese itself is capable of causing constipation is probably known to everyone. If you solve the problem with constipation in this way, then carefully introduce natural fermented milk products into the diet (preferably without flavorings and sugar) ”(D.
 V. Arkhipova, Ph.D., homeopath). It’s not worth worrying that the baby won’t get enough of something - he will take everything he needs from “mother’s reserves”, and the question is not in the amount eaten, but in the amount absorbed by the mother’s body. From the point of view of homeopathy, if you want - eat, no - you don’t need to force yourself, because. food likes and aversions are in accordance with our constitution, and therefore our needs (naturally, this applies to healthy and healthy eating habits).
V. Arkhipova, Ph.D., homeopath). It’s not worth worrying that the baby won’t get enough of something - he will take everything he needs from “mother’s reserves”, and the question is not in the amount eaten, but in the amount absorbed by the mother’s body. From the point of view of homeopathy, if you want - eat, no - you don’t need to force yourself, because. food likes and aversions are in accordance with our constitution, and therefore our needs (naturally, this applies to healthy and healthy eating habits). - It is necessary to monitor the fluid used - or rather, drink enough clean water. Volume - from one to three liters per day, if desired, but not less than a liter. “If you don’t feel like drinking water, you need to remove sweet drinks and teas from the diet and compensate for this with clean water (preferably raw, of artesian origin, pleasant to the taste, and even better thawed).” (T.G. Sadovaya, obstetrician, author of the lecture “Nutrition during pregnancy”).
- “Dried fruits are required (you can pour prunes with water at night and drink an infusion in the morning), and / or drink a glass of water in the morning on an empty stomach (you can add a little lemon juice there) and a glass of water with honey at night” (I.
 S. Arefyeva, obstetrician gynecologist).
S. Arefyeva, obstetrician gynecologist). - The diet should have a sufficient amount of fiber: at least 50% of the diet of natural plant foods in raw and processed form (fiber stimulates peristalsis). It can be whole grain cereals, products made from wholemeal flour, fruits before meals or in between, vegetables, berries (the same cranberries help with constipation).
- A daily intake of 1 to 3 tablespoons of unrefined oils has a good effect on the body. “Sweet almond oil (food) has a pronounced laxative effect and does not irritate the intestinal wall. Olive and linseed oils, as well as walnut oil, also have a mild laxative effect. Do not forget that unrefined oils should be stored in the refrigerator (with the exception of olive oil), and flaxseed should be eaten within a month after opening the bottle. (O.L. Bannikova, obstetrician).
- Add magnesium-rich foods to your diet, such as green leafy vegetables, walnuts and almonds, sunflower seeds (unroasted and preferably pre-soaked for 5-7 hours), green buckwheat and spinach.
 “You can try this recipe - soak 1 teaspoon of flax seeds in ½ cup of warm water and leave for several hours. Then eat it just like that or add it to porridge, soup” (L. Lankmane, naturopath, phytotherapeutist).
“You can try this recipe - soak 1 teaspoon of flax seeds in ½ cup of warm water and leave for several hours. Then eat it just like that or add it to porridge, soup” (L. Lankmane, naturopath, phytotherapeutist). - You can try to consume more foods that normalize the balance of intestinal flora - such as kefir (preferably homemade), miso soup, sauerkraut.
- You should not get carried away with strong tea, black coffee, cocoa, chocolate, white bread, flour and slimy soups, semolina, blueberries. All these products, like dry food, have a fixing effect. For the time of problems with the gastrointestinal tract, it is better to observe separate fractional meals, drink liquid 15 minutes before meals or some time later, etc. - that is, to facilitate the assimilation of the food consumed as much as possible. Make sure that there are no distortions - the daily diet should be balanced.
HOW TO HELP
- Enzymatic preparations can be drunk for a short time.
 If these are preparations of animal origin - no more than 7 days, plant enzymes can be taken longer. You can take probiotics, beneficial gut bacteria that aid digestion. Long-term use of these biological products not only normalizes the intestinal flora, but also contributes to a less pronounced manifestation of dysbacteriosis in a newborn child. (D.V. Arkhipova, homeopath, PhD, pediatrician)
If these are preparations of animal origin - no more than 7 days, plant enzymes can be taken longer. You can take probiotics, beneficial gut bacteria that aid digestion. Long-term use of these biological products not only normalizes the intestinal flora, but also contributes to a less pronounced manifestation of dysbacteriosis in a newborn child. (D.V. Arkhipova, homeopath, PhD, pediatrician) - Check the level of iron with a doctor - against the background of its deficiency, intestinal disorders are also possible. “But keep in mind that some iron-containing dietary supplements, unfortunately, can only worsen this condition (not to mention dosage forms). It is better to add foods rich in iron, such as almonds, pine nuts, apricots, avocados, sunflower and pumpkin seeds, wheat germ ”(L. Lankmane, naturopath, herbalist).
- Freshly squeezed juices, diluted 1 to 1 with water 15 minutes before meals, stimulate the production of pancreatic enzymes and aid digestion in the most natural way.
 (D.V. Arkhipova, homeopath, PhD, pediatrician)
(D.V. Arkhipova, homeopath, PhD, pediatrician) - Drink hot - as far as possible - water on an empty stomach, a little later, eat half a banana, chewing it for a long time and macerating it with saliva to a liquid slurry (the banana must be ripe!). (O.L. Bannikova, obstetrician).
- Starting from the second trimester, you can use essential oils: exotic basil (Ocimum basilicum in Latin), seaside pine (Pinus Pinaster), saro (Cinnamosma fragrans, Saro), rosewood (Aniba rosaeodora). “Oils should be only edible, of good quality! It is not recommended to use essential oils during the first 3 months of pregnancy. 1st composition - take 1 drop of basil, 2 drops of pine on a small piece of sugar or honey and suck under the tongue in the morning on an empty stomach. 2nd composition - basil 30 drops, rosewood 20 drops, saro 10 drops and 40 drops of apricot kernel oil or any other unrefined food oil. Mix. Take 3 drops of this mixture under the tongue on sugar or honey morning and evening before meals for 5-7 days or as needed.
 When buying aroma oils, be sure to check whether there is information on the packaging that this oil can be eaten. (O.L. Bannikova, obstetrician)
When buying aroma oils, be sure to check whether there is information on the packaging that this oil can be eaten. (O.L. Bannikova, obstetrician) - If this does not help, you can try to use "Duphalac" for a short time.
LIFESTYLE
Enough physical activity, swimming in the pool. Walking for at least one hour. But the load should be increased gradually. To begin with, one lesson should be no more than 30 minutes. The step should be slow, the shoes are comfortable, and the route should be laid away from the roads. Gymnastics for pregnant women for at least 30 minutes daily. As gymnastics, our yoga instructor for pregnant women Svetlana Shnyrova recommends a few simple exercises:
- backbends in cat pose (standing on all fours),
- alternating leg raises from a sitting position on the floor with support on the hands,
- certain types of soft twists of the spine from a sitting or lying position,
- Breathing exercises such as a few deep belly breaths can also help.

During class, you should carefully monitor your well-being and, if any discomfort occurs, immediately leave the pose. And watch how your baby reacts to the exercises.
These exercises stimulate the intestines, improve blood circulation in the abdominal cavity, and help to establish a regular bowel movement. In general, the problem of constipation should be approached comprehensively, drink more water in the morning, adjust nutrition, move more, walk, swim, do yoga.
Signs, symptoms and causes of hemorrhoids in pregnant women - NEARMEDIC network of clinics
The main causes of hemorrhoids in pregnant women can be as follows:
- Chronic constipation. In this case, the stretching and tension of the walls of the rectum increases during defecation, which leads to the formation of hemorrhoids. In pregnant women, constipation occurs much more often due to a decrease in intestinal tone.
- Inactive lifestyle. With hypodynamia, blood stagnation occurs in the venous plexus of the rectum, which eventually leads to vein thrombosis and the formation of hemorrhoids.
 Features of the condition do not always allow pregnant women to be mobile, therefore they have a high risk of developing this disease.
Features of the condition do not always allow pregnant women to be mobile, therefore they have a high risk of developing this disease. - Violation of blood circulation in the lower half of the body. During pregnancy, the uterus grows and compresses the inferior vena cava. This leads to stagnation of blood in the veins of the legs and rectum. During childbirth, a woman's intra-abdominal pressure rises greatly - this can cause hemorrhoids after pregnancy.
Signs of hemorrhoids in pregnant women
The longer the period, the higher the likelihood of developing the disease. Most often, hemorrhoids appear in the 3rd trimester or after childbirth.
The blood vessels of the hemorrhoidal plexus of the rectum gradually dilate. Over longer periods, the stretching of the veins becomes even stronger. With the expansion of the walls of the veins of the rectum, they lose their elasticity. This provokes protrusion of the veins under the mucous membrane.
If hemorrhoids protrude only into the lumen of the rectum and do not come out of the anus, then we are talking about the treatment of hemorrhoids of the 1st stage. The farther, the larger the knots become and the more they sag from the anus. In the second stage of hemorrhoids, the nodes sag from the anus, but are easily set back on their own. The third stage occurs when the nodes can no longer cope back.
The symptoms of the disease depend on its stage.
- Internal hemorrhoids. Symptoms are mild, there is no sagging of hemorrhoids from the anus. At this stage, women may experience pain during bowel movements, slight bleeding or fresh blood in the stool, and itching and discomfort in the anus.
- External hemorrhoids. The main symptom is the sagging of one or more purple-red nodes from the anus. This manifestation is the main sign of what is required, and not of another disease, such as anal fissure. Walking, sitting and defecation in this case become extremely painful.

Urgent medical attention is required in case of infringement of the hemorrhoid - a pregnant woman experiences very severe pain in the anus with fever.
Treatment of hemorrhoids during pregnancy
If a woman already has any symptoms of hemorrhoids - itching, pain in the anus, bleeding from the anus, etc. - professional treatment is required.
At NEARMEDIC, the first stage of treatment is the preventive measures described above, which stop the progression of the disease. Then the woman is prescribed drugs, both local and systemic. But due to pregnancy, local therapy is preferable, as this reduces the risk of side effects, increases the effectiveness of treatment and reduces the negative effects of drugs on the child. In any case, the medicine is prescribed only by the attending physician who observes the woman during pregnancy.
In the case when a woman already has prolapsed nodes that cannot be set, an operation is prescribed. Other indications for surgical intervention are infringement or necrosis of the hemorrhoid, as well as acute inflammation. Most often, in NEARMEDIC surgery is postponed until the postpartum period, and during pregnancy they are limited to conservative treatment.
Most often, in NEARMEDIC surgery is postponed until the postpartum period, and during pregnancy they are limited to conservative treatment.
Prevention of hemorrhoids during pregnancy
Due to the fact that all pregnant women are at high risk of developing hemorrhoids, NEARMEDIC clinic doctors strongly recommend that preventive measures be taken throughout pregnancy, without waiting for symptoms to appear.
- Relief of constipation. To do this, you need to adjust your diet: eat more foods that contain coarse vegetable fiber - vegetables, fruits, cereals, cereals, prunes. Dairy products also have a beneficial effect on digestion. On the contrary, it is better to refuse meat and other foods rich in protein. As well as from an excess of fat, coffee and hot spices.
- Hygiene. It is recommended to wash the perineum and anus after each act of defecation. In addition, once a day you can take sitz baths with antiseptics: chamomile infusion, a weak solution of potassium permanganate, etc.