Deliver at 30 weeks
Baby Born at 30 Weeks: What to Know
At 30 weeks pregnant, you might have the next 10 weeks of your calendar prepped with lunch dates, nursery decorating, and prenatal classes before the big B-Day arrives. But your baby might have other ideas!
Preterm babies — that’s babies born before becoming full term at 39 weeks — made up only 10% of births in the U.S. in 2019, so it’s pretty rare.
But the idea of having a preemie can be daunting.
Thankfully, modern medicine practices are progressing all the time to provide better care for premature babies, so even the tiniest of preemies can get the best chance of living long and healthy lives.
As with all baby-related info, there is a huge range of “normal” outcomes.
Remember that you and your baby are unique, and use this as a guide to the types of things you might face if your baby decides to arrive early.
So, what complications might we need to consider, and what’s the 30 weeks survival rate?
We’re here to give you the round-up on babies born at 30 weeks.
In this article 📝
- What does a baby born at 30 weeks look like?
- What happens if a baby is born at 30 weeks?
- Do babies born at 30 weeks need NICU?
- Will a baby born at 30 weeks be OK?
- Can babies born at 30 weeks breathe on their own?
What does a baby born at 30 weeks look like?
If you search for “baby born at 30 weeks pictures”, you won’t see the typical chubby-cheeked newborn we all expect at birth.
Instead, a baby born at 30 weeks won’t have much fat stored beneath their skin, so their skin might look translucent, and they will be very, very delicate.
They will be much smaller than a baby born at 40 weeks, though their head may be disproportionately large compared to their body.
The average weight of a baby born at 30 weeks is around 3 pounds, and they may only be about 15.5 inches long.
What happens if a baby is born at 30 weeks?
A baby born at 30 weeks gestation is classed as “very preterm” in the medical world and is likely to need immediate medical attention after birth.
All of their limbs and external body parts will be formed, so any complications they may have will be due to their internal systems being underdeveloped.
They will probably require help breathing, feeding, fighting off infections, and staying warm.
Do babies born at 30 weeks need NICU?
The exact care they require will be individual, but they’ll spend at least a few weeks in a neonatal intensive care unit (NICU) while they grow and get stronger.
It’s common for a baby born at 30 weeks to be discharged from the hospital just before or around their original due date once they’ve met certain health and developmental milestones, as determined by your doctor.
Will a baby born at 30 weeks be OK?
A recent American study records the baby born at 30 weeks survival rate to be as high as 98.5%, so the chances are very good that your little one born at 30 weeks will be OK.
Though their survival rate is excellent, they may have a higher chance of having some developmental delays later down the track, or issues with things like vision or hearing, than babies born closer to their due date.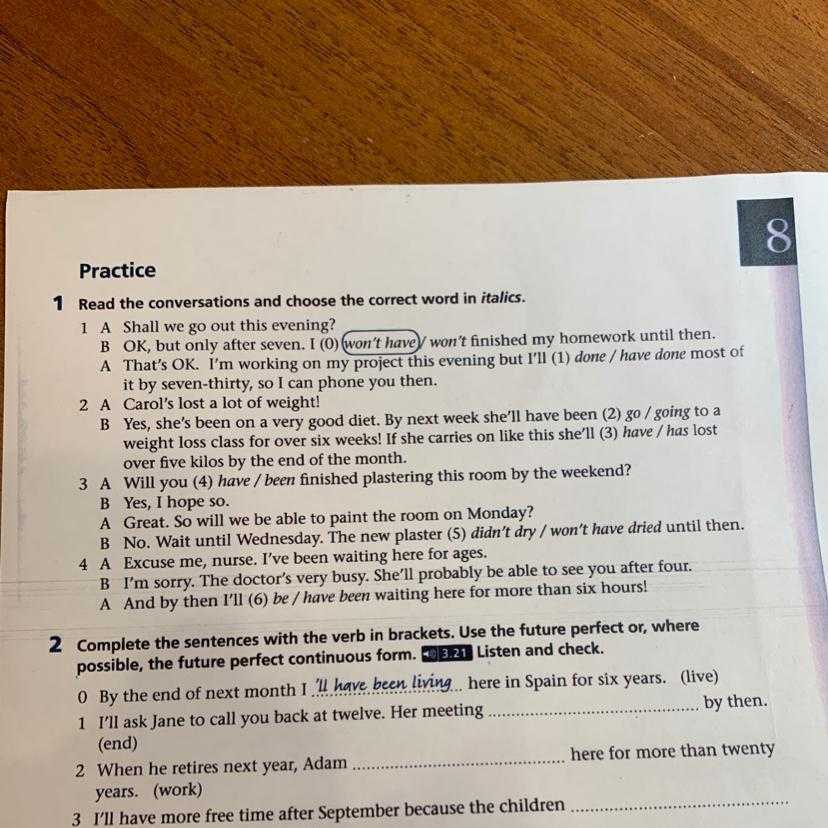
Can babies born at 30 weeks breathe on their own?
In some cases, they can.
But respiratory problems are one of the biggest concerns for doctors of premature babies.
If your baby is struggling to breathe by themselves, they will get the help of a ventilator, which can look scary, but is just what they need to get started in the big wide world.
Are babies’ lungs developed at 30 weeks?
At around 26 weeks gestation, the lower lungs develop and little air sacs called alveoli will form, but they are not fully formed until around week 36.
So, at 30 weeks the lungs may not be big or strong enough to breathe by themselves.
It’s also common for babies born at 30 weeks to be fed by a tube and have various IV lines to give them fluids and medications to fight off infections.
Having a baby in the NICU can be a scary and isolating experience, but chatting with other preemie Peanut Mamas can help.
Your baby born at 30 weeks might be tiny and fragile, and your start to mama-hood might not be the way you planned, but the chances are excellent that your baby will be just fine.
You got this.
You might also be interested in:
Baby Born at 31 Weeks: What to Know
Baby Born at 32 Weeks: What to Know
Baby Born at 33 Weeks: What to Know
Baby Born at 34 Weeks: What to Know
Baby Born at 35 Weeks: What to Know
Baby Born at 36 Weeks: What to Know
Baby Born at 37 Weeks: What to Know
What to Look for in a Preemie Pacifier
Premature baby development: 26-36 weeks
Premature baby development: the basics
A premature baby’s development typically happens in the same order as it would have happened in the womb.
But premature babies might have some health challenges along the way. Sometimes premature babies also have delays in growth and development. Very premature babies and premature babies with medical challenges are more likely to have delays.
For example, a premature baby born at 32 weeks is likely to act differently from a baby born at 26 weeks, who has had many medical challenges by the time they get to 32 weeks. The baby born at 26 weeks might take extra time to put on weight, learn to feed and come out into the social world.
The baby born at 26 weeks might take extra time to put on weight, learn to feed and come out into the social world.
Here are the changes you can expect and watch in your premature baby during their time in hospital.
26 weeks
At 26 weeks, a baby in the womb is about 35 cm long and weighs about 760 gm. But premature babies are often small for their age. A baby born at 26 weeks would probably fit snugly into your hand.
At this age your premature baby’s main job is to grow, sleep and become medically stable.
Your baby might open their eyes occasionally, but they can’t focus. Light or other visual stimuli might stress their body’s systems. Your baby’s nurse might place a cover over your baby’s incubator, and some neonatal intensive care units (NICUs) dim the lights at night.
Your baby’s movements are often jerks, twitches or startles. Your baby doesn’t yet have good muscle tone and can’t curl up. Hospital staff will put your baby in a curled-up position, support their body with bedding and keep them warm. This helps your baby keep up their energy.
This helps your baby keep up their energy.
Your baby might also have apnoea. This is common for very premature babies. The breath triggering part of your baby’s brain hasn’t fully developed yet, so pauses between breaths are common. Your baby will grow out of it.
Your baby’s ears and hearing structures are already fully formed, but your baby might be sensitive to external sounds. Your baby might notice your voice but they can’t respond to you yet.
Your baby won’t be able to feed from your breast yet.
Your baby’s skin is fragile and sensitive, and they might get stressed if they’re handled or touched. The nurses will probably encourage you to ‘comfort hold’ your baby but not stroke them.
Our article on touching, holding and massaging your baby has more information on comfort holding and kangaroo care. And our article on premature baby body language explains what your premature baby’s behaviour is telling you.
26-28 weeks
At 26-28 weeks, babies in the womb continue to put on weight and grow longer. But if your premature baby is sick, their weight gain might not keep up with a baby in the womb. Also, hospitals use careful, staged feeding plans to protect your baby’s immature gut from infection, and this might slow weight gain.
But if your premature baby is sick, their weight gain might not keep up with a baby in the womb. Also, hospitals use careful, staged feeding plans to protect your baby’s immature gut from infection, and this might slow weight gain.
At this age, babies start blinking. They also grow eyelashes and eyebrows.
Your baby still has low muscle tone and is likely to have twitches and tremors.
Your baby’s sleep and wake cycles aren’t clear yet, but your baby might have active and quiet periods and very brief alert times.
Your baby might open their eyes, but they probably still can’t focus or get their eyes moving together.
At this age, your baby’s responses to sound might change from hour to hour or day to day. Or they might respond to your voice but get stressed by other noises. Your baby’s responses will start to give you some clues to what they like and dislike.
Your baby might begin sucking, but they still can’t feed from your breast. To breastfeed, they need to know how to suck, swallow and breathe in the right order.
To breastfeed, they need to know how to suck, swallow and breathe in the right order.
Your baby’s skin is still fragile and sensitive. But if your baby is medically stable, you might be able to start skin-to-skin contact by doing kangaroo care.
28-30 weeks
In the womb a baby keeps getting heavier and longer, starts to move more often, knows the difference between some sounds – for example, voices and music – starts to grasp with their hands, and opens and shuts their eyes.
At this age, your premature baby will still be well supported with bedding and positioning, but they might move and stretch more actively as their muscle tone gets better.
Your baby’s quiet deep sleep (when they don’t move) and light sleep (when they move their limbs and eyes) increase at about 30 weeks. You’ll also start to see short alert, eye-opening periods, but this can be affected by your baby’s health, the environment or the time of day.
Your baby is starting to close their eyelids tightly if it’s bright, but they still can’t move their eyes together very much. Their eyes wouldn’t usually get much stimulation at this age, so it might help to limit what they see.
Your baby keeps responding to pleasant sounds and is still sensitive to other sounds. They might be quiet and attentive to your voice and might even seem to ‘wake up’ when you come in. You can start to talk or sing to your baby during their short alert times. But keep stimulation to one thing at a time – for example, eye contact or talking, but not both at once.
Your baby’s rooting reflex – turning to a touch on the cheek – might start around this time. This means they’re getting ready for breastfeeding. Your baby might even start sucking, but they can’t feed at your breast yet.
Your baby might still be sensitive to touch, but they like steady, gentle, hands-on touch or skin-to-skin contact. You might be able to get involved in caring for your baby about now.
You might be able to get involved in caring for your baby about now.
30-33 weeks
At this age, a baby’s organs are maturing. A baby born now might not need much medical help.
Your premature baby’s movement is smoother and more controlled, and they’ll start to bend their arms and legs for themselves.
Your baby’s deep sleep increases. Their alert periods come more often, especially if the room is dim. When they’re alert, your baby might focus on your face or another interesting object, and they might show an obvious response to your voice. Your baby might shut their eyes tightly if the room is bright.
Your baby might like eye contact, cuddling or talking during these times – but it’s still a good idea to keep it to one thing at a time. And you can also watch your baby’s body language for signs of stress.
Your baby might start to suck rhythmically and might show that they’re ready to suck to feed. Letting your baby smell and taste breastmilk gets their senses ready for breastfeeding. Gently rubbing around your baby’s lips and inside their mouth before feeds helps your baby get ready for the touch sensations of feeding from your breast.
Gently rubbing around your baby’s lips and inside their mouth before feeds helps your baby get ready for the touch sensations of feeding from your breast.
If you see your baby putting their hands to their mouth, this means that they’re starting to soothe themselves.
Your baby might still be very sensitive to touch and handling. It’s helpful to tell them what you’re about to do so they can start associating your voice with what you’re doing. For example, ‘We’re going to change your nappy now’.
33-36 weeks
Your baby is now approaching the date they were due to be born. But even when they’ve reached 37 weeks, they aren’t necessarily like a full-term baby.
Your baby can now move more smoothly and bend their arms and legs. They can also move their head from side to side, and their muscle tone is stronger.
Your baby will be much less likely to experience apnoea.
Your baby’s states are clear – quiet sleep, active sleep, drowsy, quiet and alert, awake and fussy, or crying. Their alert states are still quite short, but they’re getting longer and happening more often. Your baby can have longer social times, and they can now turn away or close their eyes when they’ve had enough.
Their alert states are still quite short, but they’re getting longer and happening more often. Your baby can have longer social times, and they can now turn away or close their eyes when they’ve had enough.
Your baby is more likely to respond to sounds and noises in the same way from day to day. You might even know how they’re going to react when you say something to them.
Your baby probably still doesn’t cry much. But as your baby gets closer to term, they’ll cry more often to let you know what they want.
Your baby can usually start breastfeeding around this time.
Your baby might still be sensitive to touch and handling, although telling your baby what you’re about to do will help them relax over time.
37 weeks and beyond
Your baby might be ready to go home before their expected birth date. But it might take longer if your baby has had surgery or an illness.
The hospital will have health, growth and development goals for your baby to meet before you can take them home.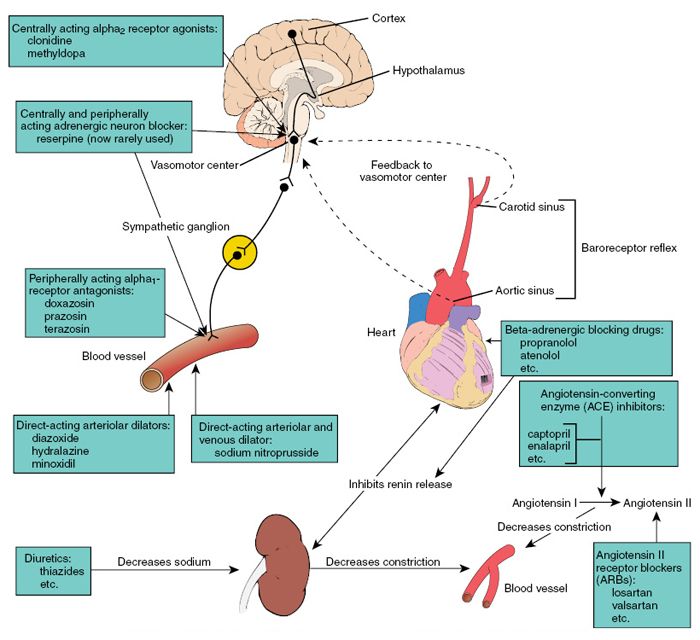 These might include steadily gaining weight, feeding from your breast or a bottle at all feeds, and having no problems with apnoea.
These might include steadily gaining weight, feeding from your breast or a bottle at all feeds, and having no problems with apnoea.
Our article on going home with your premature baby has more information on how to prepare for your baby’s homecoming.
Premature birth - Juno
Premature birth: content of the article
What is preterm birth
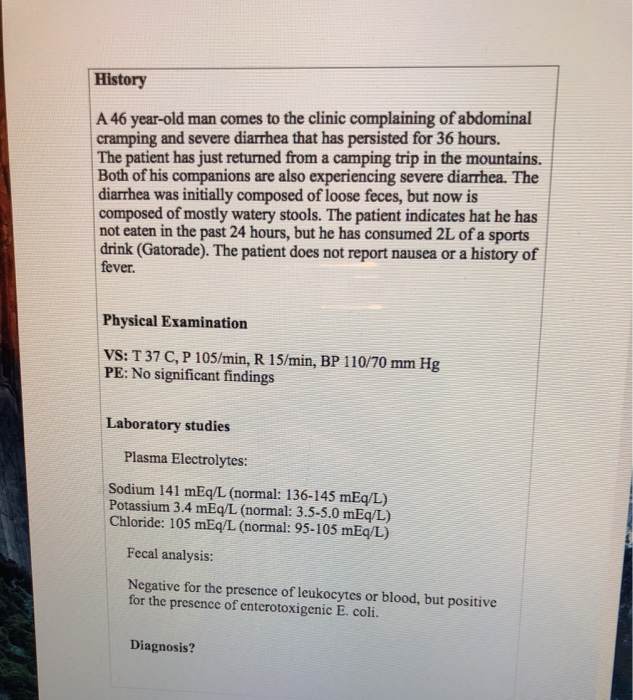
The birth of a baby weighing more than 0.5 kg from 22 to 37 weeks is considered early. According to statistics, 15 million babies are born prematurely around the world.
In our country, until 2012, babies were registered who were born at 28 weeks, and all those born earlier - a week later. The development of obstetrics made it possible to nurse critically premature babies and increased their survival statistics.
Who is at risk
Any pregnant woman can give birth prematurely. Some expectant mothers have a higher chance of preterm birth. The risk zone includes pregnant women:
- under 17 and over 35;
- have more than one fetus;
- have structural features of the uterus or its cervix;
- use harmful substances - drugs, alcohol, smoke;
- have heavy physical activity;
- have a history of preterm birth;
- work in hazardous production;
- are subjected to sexual, emotional abuse, stress, mental stress.

At risk are expectant mothers who are not registered during the gestation period or ignore ultrasound, screenings, laboratory tests.
The threat of early preterm birth is more common with diagnoses: diabetes mellitus, anemia, hypertension, genitourinary infections, hypothyroidism, problems with weight before conception (deficiency or obesity), thrombophilia, vaginal bleeding. There is also a risk when conceiving through IVF, with congenital malformations of the fetus.
If a woman has previously given birth to a child ahead of schedule, the chances of premature birth remain in subsequent pregnancies. The same applies to the weight of the crumbs: if the firstborn was born with a lack of body weight, then his brother or sister may be underweight.
Risk factors
Doctors point to a number of factors that take place long before the conception of a child. These include:
- Gynecological diseases suffered in childhood or adolescence;
- Early initiation of intimate life;
- Hereditary factor;
- Pathologies of previous pregnancy: preeclampsia, fetoplacental insufficiency, premature birth;
- Excessive uterine distension in multiple pregnancies, polyhydramnios;
- Threat of early miscarriage.
Another risk factor is surgery or trauma to the abdominal organs during the gestation period.
Risk of preterm birth at different terms
The birth of a child prematurely has many negative consequences for him. It depends on the trimester in which the pregnancy ended.
The most severe consequence is the death of the infant. With early preterm birth in the period of 22-24 weeks, the threat is the highest - up to 80% of babies die. This occurs against the background of intracranial hemorrhage of 3-4 degrees, cardiopulmonary insufficiency, intrauterine infection of the fetus.
Among those born in the period of 25 - 26 weeks, 40% of babies die, in 27 - 28 - about 20%, in 29 - 32 - no more than 10%, and in 33 - 34 - 2% of newborns are at risk.
Modern medicine is able to provide care for a premature baby and save his life. But no one can guarantee a full healthy life. Such a child can subsequently be given disappointing diagnoses: cerebral palsy, mental retardation, retinopathy of prematurity. He may suffer all his life from problems with the digestive and respiratory systems, impaired vision, hearing, delayed mental and physical development. Diagnosis implies disability.
He may suffer all his life from problems with the digestive and respiratory systems, impaired vision, hearing, delayed mental and physical development. Diagnosis implies disability.
For a woman in labor, preterm labor is usually not dangerous. Without concomitant pathologies, the mother's body does not care how long the child is born. There are only psychological problems: stress, fear and worries about the baby. It is better for a mother to tune in that her child, in case of severe prematurity, will be taken to the intensive care unit for nursing, so she will not see him immediately.
A newly minted mother needs rehabilitation. Therapy is prescribed, depending on the cause of the pathology: a complex of vitamins, antioxidants, hormones.
Why preterm birth is dangerous
Infants are immature: their body is covered with a large amount of cheese-like lubricant, there is a deficiency of subcutaneous fatty tissue, few hairs on the head and fluff on the body, cartilage on the ears and nose are soft, the nails do not go beyond the fingertips, the navel is located closer to the pubis.
Babies are underweight. Depending on the weight of the crumbs, 4 degrees of prematurity are distinguished: at the 1st degree, the baby weighs from 2500 to 2001 g, the 2nd - from 2000 to 1500 g, the 3rd - from 1500 to 1001 g, the 4th - 1000 g and below .
The development of the genital organs has not been completed: the testicles in boys are not lowered into the scrotum, and in girls the large labia do not cover the small and clitoris.
Children have immature lungs. They cannot breathe adequately - often they need help. The cry is weak. There are also problems with digestion. The body cannot absorb all the components from mother's milk.
Extrauterine life for children becomes a strong stress. It's hard to deal with him. They poorly resist infections, quickly lose heat, thermoregulation is impaired. They are subject to hemorrhages against the background of fragile vessels. Especially dangerous are hemorrhages in the cervical spinal cord and ventricles of the brain.
Among the complications of preterm birth are intracranial hemorrhages, asphyxia, intrauterine growth retardation.
Types of preterm birth
Several classifications have been adopted. Let's consider them.
- By term: critically early - up to 28 weeks, significantly early - from 28 to 32 weeks, moderately early or late - from 32 to 37 weeks;
- By the mechanism of attack: induced and spontaneous. Induced cause artificially for medical reasons. Occurs in 40% of cases. Spontaneous in 60% of cases begin with contractions, in 40% - with a rupture of the membranes;
- By the nature of the course: spontaneous, with regular labor activity, without it and artificially provoked. In 80% of cases, preterm labor begins spontaneously. At the same time, the fetal bladder can be intact - and then the contractions are regular, growing. Or amniotic fluid may pour out, labor activity is chaotic. For medical reasons, early delivery can be artificially induced.
 For example, in case of danger to the life of the mother, intrauterine death of the fetus, or defects that are incompatible with life;
For example, in case of danger to the life of the mother, intrauterine death of the fetus, or defects that are incompatible with life; - According to symptoms: threatening, incipient and incipient. With threatening early premature birth, the lower abdomen and lower back hurt, the tone rises. Her neck remains unchanged, the external os is closed. When the process begins, pains appear in the lower abdomen. Regular contractions may begin. The neck is flattened or shortened. The main symptom of the onset of preterm labor is regular labor activity. The cervix opens by 2 - 3 cm, it happens quickly.
In 40% of women in labor, water breaks, 35% gave birth quickly and quickly. The active phase lasts less than when the baby appears on time. The contractions are monotonous, long and painful, the pauses between them are small.
Causes of preterm birth
Doctors indicate the main causes of the pathology:
- Early activity of the fetal endocrine system;
- Infections and inflammatory processes - ureaplasmosis, mycoplasmosis, pyelonephritis, bacterial vaginosis.
 They stimulate the production of prostaglandins. Hormones affect the uterine muscles - cause contractions and premature birth;
They stimulate the production of prostaglandins. Hormones affect the uterine muscles - cause contractions and premature birth; - Placental bleeding. They occur with incorrect presentation or detachment. The situation is serious, there is a threat to the life of the mother. Therefore, with presentation, hospitalization is indicated;
- Neck weakness. In 20% of cases, it leads to preterm birth. This also includes such factors: the interval between the current and previous gestation is less than 2 years, the woman is expecting 4 children or more;
- Isthmic-cervical insufficiency. The cervix opens itself - a miscarriage or premature birth occurs. It is possible to open mechanically - when scraping after a miscarriage, IVF, abortion;
- Pathologies on the part of the baby - intrauterine infection, malformations of internal organs.
Chronic ailments, dental problems, angina, health status during gestation, genetic factors are all common reasons for early delivery. Sometimes it is impossible to determine. Although this is important for the development of effective means of preventing pathology.
Sometimes it is impossible to determine. Although this is important for the development of effective means of preventing pathology.
Symptoms of preterm labor
We list the signs by which you may suspect that the baby is in a hurry to be born ahead of time.
Spasms over the pubis. They are similar to pain during menstruation.
Pain, pressure and discomfort in the genitals, thighs, pelvis. There is a dull pain in the lumbar region.
Feeling of pressure, pressure in the back.
Diarrhea, spasms and pain in the intestines.
Vaginal discharge - they get worse. May be watery, pink, brown, bloody.
Contractions of varying intensity. Touch your stomach with your fingertips - you will feel the contraction and relaxation of the uterus. Counted more than 4 contractions in 60 minutes? Call an ambulance - you need an urgent examination by an obstetrician.
The following symptoms are also dangerous: sudden blurred vision, flashes and “flies” before the eyes, incessant migraine, swelling of the face or hands, temperature of 38º C and above, painful urination, abdominal trauma, decreased fetal activity in the 3rd trimester (less than 10 movements in 12 hours).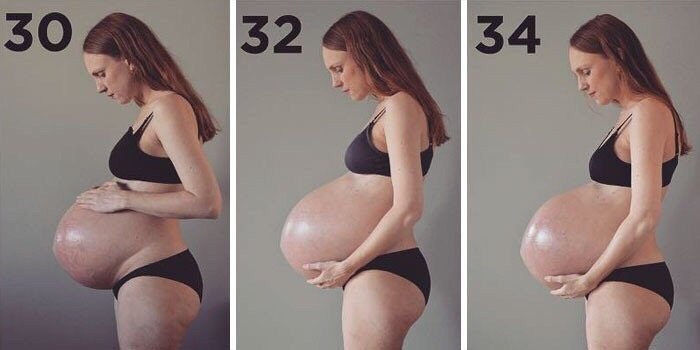
Any of the above symptoms indicate the risk of preterm birth. Seek medical attention.
Diagnosis of preterm birth
Includes several stages.
Transvaginal ultrasound. The length of the cervix is measured, fetal fibronectin is determined - a kind of "biological glue" that binds the fetal sac to the uterine mucosa.
Gynecological examination. Allows you to assess the degree of opening of the neck, its length.
Rapid test for the determination of phosphorylated protein-1. The test determines the possibility of preterm birth. In the future, this helps prevent iatrogenic complications.
When diagnosing, 2 parameters are evaluated:
- Regularity of contractions;
- Neck changes - shortening and smoothing. informative method. For example, with a neck length of 3 cm, the risk of preterm birth in the next week is 1%. The patient is not admitted to the hospital, there is no danger to her and the fetus.

Differential diagnosis
Its goal is to correctly diagnose. The early birth of a baby is accompanied by cramps in the lower abdomen, diarrhea, pain in the lumbar region. These same symptoms are characteristic of other conditions: appendicitis, colitis, cystitis, pyelonephritis.
When complaining of pain in the lower abdomen, the patient is examined for the consistency of the scar after the previous cesarean section, for example. When the temperature rises, flu, sore throat, viral infection are excluded.
Diagnosis
Preterm birth is stated based on the clinical picture. Doctors are guided by such markers.
The first is the length of the neck - less than 2 - 2.5 cm.
The second is the determination of phosphorylated protein-1.
The third is the regularity of contractions. There should be at least 4 in 20 minutes.
Fourth - neck changes in dynamics.
Fifth - assessment of the degree of maturity of the neck. Determined by the level of PSIFR-1 in the cervical canal.
Determined by the level of PSIFR-1 in the cervical canal.
Usually the process begins rapidly, suddenly and intensely.
Treatment for preterm birth
The goal is to reduce the tone of the myometrium, reduce uterine contractions. This is achieved by blocking oxytocin receptors - it is the hormone oxytocin that triggers the birth process.
Such antagonists of oxytocin receptors are tocolytics. One of the modern representatives of this group of drugs is atosiban.
The remedy is effective, but has contraindications. It is forbidden to treat pregnant women for less than 24 and more than 33 weeks, with uterine bleeding, growth retardation, distress or fetal death, severe preeclampsia, with rupture of the fetal membrane after 30 weeks, placenta previa or its detachment.
5 stages of preterm labor
The first stage is forecasting their onset. Depends on the situation: the process is starting, has begun, or it is a threat.
Stage two - prevention of respiratory distress syndrome in a child. Doctors stimulate the maturation of the lungs. Apply funds from the group of glucocorticoids.
Stage three - prolongation of pregnancy. Doctors try to delay preterm labor by giving the baby's lungs and placenta time to mature. For this, tocolytics are used - they inhibit the contractile activity of the uterus. Usually prophylaxis is carried out - tocolysis is carried out before contractions. When started, therapy is ineffective. The duration of treatment is a maximum of 48 hours.
Stage four - preparation for the birth of a premature baby. The woman in labor is transferred to a higher-level hospital. The physiology of preterm labor does not differ from the birth of a child at term. But close attention is required from doctors to minimize complications for mom and baby.
The fifth stage is the prevention of infections and their complications. At risk are women in labor whose waters have broken. If the patient gives birth before 34 weeks, she can be pierced with a course of dexamethasone. It accelerates the maturation of the placenta and internal organs of the baby, reduces the risk of complications.
If the patient gives birth before 34 weeks, she can be pierced with a course of dexamethasone. It accelerates the maturation of the placenta and internal organs of the baby, reduces the risk of complications.
OB sequence
When registering a patient with preterm birth, the doctor gets acquainted with the exchange card, studies the general, gynecological and infectious anamnesis, and the results of examinations. Clarifies complaints and evaluates the condition of the woman in labor. He examines her, measures the pulse and respiration rate, temperature, pressure, abdominal circumference and the height of the uterus.
Clarifies data on the fetus: movements, measures heart rate by auscultation - listening to the heart through the mother's stomach through the device. To assess the condition of the crumbs, the doctor performs cardiotocography. The device records the heart rate.
Ultrasound is performed to assess the condition of the child and mother's organs.
A gynecological examination is carried out: with intact membranes - external, with their rupture - internal. This is necessary to determine the position and position of the child, to assess the degree of disclosure.
Conduct a laboratory examination. They take a smear from the vagina: culture for β-hemolytic streptococcus, bacteriological culture, take blood and urine for a general analysis.
According to the results of the examination, the obstetrician confirms or refutes preterm birth, their stage.
The expectant mother is informed about her condition, forecasts for the child. At the slightest opportunity, they try to prolong the pregnancy. If the child is ready to be born in the near future, the doctor determines the tactics of assistance, coordinates the issue of anesthesia with the woman in labor.
In the absence of indications for a caesarean section, they give birth naturally. This is the best way - it is less traumatic for the baby. A gentle approach is what a weak newborn needs.
A gentle approach is what a weak newborn needs.
Preterm birth care policy
The woman in labor is provided with continuous psychological support. Describe the current obstetric situation.
With head presentation, they give birth naturally.
With pelvic - take into account clinical indications. Caesarean section is not the only effective method in this case. The operation does not improve the prognosis for a premature baby, but it puts an additional burden on the mother's body: it increases infection, morbidity, and complications.
With foot presentation, only a caesarean section is done.
Anesthesia is carefully selected. Avoid opiates - they depress the respiratory center, which is dangerous for premature babies.
At the birth of a baby before 34 weeks, vacuum aspiration is prohibited. It increases the risk of neonatal morbidity. Dosed episiotomy, exit forceps for the birth of the head and epidural anesthesia are performed.
The umbilical cord is clamped at least 1 minute after the baby is born. This tactic reduces the frequency of intraventricular hemorrhage in preterm pregnancies up to 37 weeks of gestation.
Control the state of the crumbs. CTG is done every hour for 40 minutes, auscultation - periodically.
General recommendations for prevention
You need to think about it from the first trimester. If you want to inform the baby, follow the advice of gynecologists.
- Take care of yourself. Rest, avoid nervous overload. Sleep at least 7 hours;
- Eat well. Eat foods rich in vitamins, exclude fast food, fatty, fried, spicy and salty foods from the diet. Give up coffee and strong tea;
- Observe the drinking regimen. Try not to feel thirsty - drink water every 2 hours. If you don't want to - don't force yourself;
- Avoid physical activity. Active training, hard work, general cleaning alone are taboo for a pregnant woman.
 Try not to go outside on ice - you may fall, you will strain your muscles - this can increase your tone and provoke premature birth;
Try not to go outside on ice - you may fall, you will strain your muscles - this can increase your tone and provoke premature birth; - Maintain personal hygiene. Wash your face after a bowel movement. Always wash and dry from front to back. This way you will not bring bacteria from the intestine into the vagina. Infections are provocateurs of premature birth;
- Lead a healthy lifestyle. Alcohol and cigarettes are taboo. Smoking pregnant women are predisposed to preterm labor. If you take medications on a regular basis, tell your gynecologist about it. Walk outdoors. Cancel active workouts in favor of leisurely walks in the park;
- Register at the antenatal clinic in the first trimester - at 6 ‒ 8 weeks. Visit a gynecologist, listen to him, take tests, undergo ultrasound, screenings;
- Be careful with sex. In the first trimester, it is better to limit or abstain from it as much as possible - the embryo must be fixed. With placenta previa and other pathologies, the gynecologist may forbid you to have intimate contacts - listen to him;
- Learn to understand your body.
 In the 2nd trimester, start listening to the baby: his movements, activity. Fix any changes, strange and unpleasant sensations - and talk about them to the doctor. In case of acute pain, contractions, spasms, blood, urgently call an ambulance - this may be a premature birth;
In the 2nd trimester, start listening to the baby: his movements, activity. Fix any changes, strange and unpleasant sensations - and talk about them to the doctor. In case of acute pain, contractions, spasms, blood, urgently call an ambulance - this may be a premature birth; - Maintain bed rest. A gynecologist can advise you to rest. For example, with increased uterine contractions, tone;
- Rest every hour. Sit in a chair, lift your legs up. This will relax the muscles, eliminate swelling;
- Be aware of the signs of preterm labor. In case of their threat, you will not miss a moment and consult a doctor. Perhaps the process can be stopped with the help of drugs. Treatment minimizes complications in the premature baby.
Preterm birth prevention
It is divided into 2 stages: before conception and after.
Preventive measures before conception
It is advisable to carry them out to mothers from the risk zone. The gynecologist limits intrauterine manipulations, such as curettage. During IVF, the number of embryos for transfer is regulated taking into account the age of the expectant mother and her health. Inform about the possibility of premature birth at conception through reproductive technologies.
The gynecologist limits intrauterine manipulations, such as curettage. During IVF, the number of embryos for transfer is regulated taking into account the age of the expectant mother and her health. Inform about the possibility of premature birth at conception through reproductive technologies.
Hydration is shown - enhanced drinking regimen. It improves fetoplacental blood flow and reduces the risk of preterm birth.
Eliminate infections. It is advisable to do this at the planning stage, since antibiotic treatment during gestation harms the fetus.
It is recommended to postpone the conception of a child soon after the birth of an older brother or sister. Mommy's body needs to recover from the previous pregnancy. It takes him at least 2 years to do this. During this time, the uterus will return to its previous state, strength, vitamin reserves and body reserves will be restored.
Vitamin complexes are prescribed for predisposition to preterm birth for planning and expectant mothers. Protein-rich dietary supplements are helpful. They strengthen the immune system, improve blood circulation, protect the pregnant woman from infections - and hence the child.
Protein-rich dietary supplements are helpful. They strengthen the immune system, improve blood circulation, protect the pregnant woman from infections - and hence the child.
Secondary prevention of early delivery
With the threat of premature birth, the condition of the pregnant woman is monitored at critical periods: from 2 to 12 and from 18 to 22 weeks. During these periods, it is better to stay in the hospital of the perinatal center. Doctors prescribe drugs to maintain and prolong pregnancy.
Therapy is selected on an individual basis.
With a short neck from 1 to 2.5 cm, progesterone suppositories are prescribed vaginally. The hormone is also shown in previous preterm births. This tactic reduces their risk by 35%. This is a natural hormone. It is efficient and safe. It is prescribed in the first trimester. Synthetic hormone is harmful: it can provoke gestational diabetes.
If there is a threat of early birth of the crumbs, sutures are placed on the neck. The expectant mother is out of the risk zone in this situation, stitches may not be applied.
The expectant mother is out of the risk zone in this situation, stitches may not be applied.
Another option is to install a pessary on the neck.
These methods reduce the statistics of premature births. But the mortality rate of newborns is not affected.
When carrying twins, circular or U-shaped sutures can be applied. In most cases, such tactics with a short neck in multiple pregnancies can provoke preterm labor. Vaginal progesterone is not prescribed.
For infections (for example, bacteriuria, gonococcus, syphilis, β-hemolytic streptococcus, bacterial vaginosis, chlamydia), antibiotic prophylaxis is prescribed. Depending on the diagnosis, penicillin, ampicillin, metronidazole, erythromycin, ceftriaxone, josamycin may be prescribed.
Terminals
Premature birth is one of the fears of many expectant mothers. Nobody is immune from this. But you can minimize the risks. Follow the recommendations of the gynecologist, take care of yourself, listen to your body, do not refuse to stay in the perinatal center.
Don't think bad. Modern medicine successfully nurses premature babies, reduces the risks of complications and consequences.
▶Preterm birth: what provokes them ✅ ADONIS MC
More than 15 million babies are born prematurely each year. In different countries, they make up from 5 to 18% of the total number of newborns. It is known that preterm birth is a threat to the health of the child due to incomplete intrauterine maturation. Today we asked Alexander Vladimirovich Bogomaz, an obstetrician-gynecologist of the highest category at the ADONIS clinic, to tell us about the causes of preterm birth, their features and methods of pregnancy prolongation.
Alexander Vladimirovich, tell me, which births are considered premature?
– Birth before 37 weeks of gestation is considered premature, but 34 weeks is the critical threshold. Children who are born before this term are extremely immature. They need intensive care and long-term nursing. If a woman has a risk of preterm birth or certain pathologies, it is desirable that the pregnancy is still prolonged to at least 34 weeks, but preferably up to 37.
If a woman has a risk of preterm birth or certain pathologies, it is desirable that the pregnancy is still prolonged to at least 34 weeks, but preferably up to 37.
Tell us about the causes of premature birth. Why do some women give birth on time, while others much earlier?
– There are many reasons for preterm birth, but in some cases they cannot be identified. The main ones include chronic diseases of a woman, hormonal disorders in her body, pregnancy pathologies and injuries. Often, premature births occur due to intrauterine infection of the fetus. If a woman had hidden infections of the genitourinary system even before pregnancy, then during the period of gestation, they can become aggravated and transmitted to him.
Is it possible to detect the risk of preterm birth in advance and prolong the pregnancy?
– Yes, it is now possible to predict preterm labor and prolong pregnancy. To do this, control the hormonal background and measure the cervix. In case of shortening, a suture is applied to it or an obstetric pessary is installed. We use different methods to prolong pregnancy, depending on the reasons that increase the risk of preterm birth. With their help, we try to help a woman bring her baby to at least 37 weeks.
In case of shortening, a suture is applied to it or an obstetric pessary is installed. We use different methods to prolong pregnancy, depending on the reasons that increase the risk of preterm birth. With their help, we try to help a woman bring her baby to at least 37 weeks.
If a woman still had preterm labor, then how do they, from the point of view of an obstetrician-gynecologist, differ from term labor?
- Premature babies are usually very weak, so you need to try to make childbirth as easy and natural as possible. The doctor should use gentle delivery tactics with minimal interference with the natural process.
If delivery occurs before 34 weeks, the pregnant woman is given a course of dexamethasone injections. It is necessary for the prevention of respiratory disorders in a child. The drug helps to accelerate the maturation of the placenta and internal organs of premature babies. This reduces the risk of developing pathologies in newborns.