Deep cough while pregnant
Bronchitis While Pregnant: Prevent and Treat
When you’re expecting, your growing belly can make it difficult to take in full, deep breaths. And bronchitis, an inflammation of the lower respiratory tract, can make taking in deep breaths even harder.
Bronchitis is inflammation of the airways that causes you to develop extra mucus. Acute bronchitis is most often caused by infection. It results in lots of coughing. You might also have a fever, sore throat, shortness of breath, chest pain, chills, and body aches.
While you may not normally call your doctor for these symptoms, you have to be more careful during pregnancy. Now you’re living for two (or more).
Bronchitis is fairly common, especially during the winter months. Taking preventive steps is important to help you and your baby-to-be stay well.
Bronchitis can be the result of a bacterial or viral infection. Both are unfortunately easy to catch. One of the best ways to protect against bronchitis is to wash your hands often.
Avoiding exposure to people that have bronchitis or other respiratory conditions is also important. If a loved one has an infection, try to stay away as much as you can. This is especially true if they have a fever.
The flu virus can cause bronchitis, so be sure to get an annual flu shot. You can also encourage those around you to get the shot. The flu shot doesn’t contain live viruses, so it shouldn’t make you sick.
Getting the flu shot can also boost your baby’s immune system for about six months after birth. That means your little one will be less likely to experience the flu virus.
Avoiding cigarette smoke is also important in preventing bronchitis. Smoking irritates the airway linings, hindering the body’s natural defense system against infections.
Unfortunately, for some expectant moms, bronchitis can quickly progress to a more severe respiratory disorder. One example could be pneumonia. Seek emergency medical treatment if you experience the following symptoms:
- chest pain
- coughing up blood
- fever greater than 100.
 4°F, or 38°C
4°F, or 38°C - shortness of breath that doesn’t get better with rest
While a large portion of bronchitis-related cases are due to a virus, sometimes bacteria can lead to bronchitis.
Bacteria-caused bronchitis can be treated with antibiotics if symptoms become severe or don’t seem to be getting better after a week. Check with your doctor to see if you’ll need antibiotics.
If your doctor suspects your bronchitis is due to a bacterial infection, they may prescribe antibiotics. While not all antibiotics are considered safe during pregnancy, some are.
The following antibiotics are typically considered safe during pregnancy:
- amoxicillin
- ampicillin
- clindamycin
- erythromycin
- penicillin
- nitrofurantoin
You shouldn’t take a class of antibiotics called tetracycline antibiotics. Examples include doxycycline and minocycline. These are associated with potentially causing discoloration to a baby’s teeth.
The antibiotics trimethoprim and sulfamethoxazole also are pregnancy no-no’s. They’ve been known to cause birth defects.
Antibiotics aren’t always necessary to treat bronchitis. A virus usually causes the condition and antibiotics won’t kill a virus. But if your symptoms aren’t getting better after a few days, see your doctor. They will evaluate you further and look for bacterial causes of infection.
Always check with your doctor before trying any at-home treatments. You’ll want to make sure they’re safe for you and your growing little one. While these treatments won’t cure bronchitis, they can help you feel better as your body heals.
Try irrigating your nasal passages using a mixture of 8 ounces warm water, 1/2 teaspoon of salt, and 1/2 teaspoon of baking soda. This can help you feel less stuffy.
Lean forward over a sink with your head at a 45-degree angle so that one nostril is pointed toward the sink. Using a syringe or squeeze bottle, pour the water into your nostril as you breathe through your mouth. The water should come out on the other side of your nose.
The water should come out on the other side of your nose.
Repeat this process about three to four times per day.
Other at-home treatment options include:
- Vicks vapor rub
- using a humidifier
- rest and fluids
- steamy shower
- pregnancy-safe hot tea
While you should always check with your doctor first, you may be able to take some over-the-counter antihistamines after the first trimester.
You can take the following medications to help dry up the extra mucus that has built up in your lungs after your first trimester:
- chlorpheniramine (Chlor-Trimeton)
- loratadine (Claritin)
- Novahistine
- pseudoephedrine (Sudafed)
- Tylenol Cold & Sinus
Most respiratory infections like bronchitis are not associated with a high risk for pregnancy complications or birth defects. But that doesn’t address the discomfort you experience while you are recovering from bronchitis. Take preventive measures and check in with your doctor for treatment options.
Bronchitis While Pregnant: Prevent and Treat
When you’re expecting, your growing belly can make it difficult to take in full, deep breaths. And bronchitis, an inflammation of the lower respiratory tract, can make taking in deep breaths even harder.
Bronchitis is inflammation of the airways that causes you to develop extra mucus. Acute bronchitis is most often caused by infection. It results in lots of coughing. You might also have a fever, sore throat, shortness of breath, chest pain, chills, and body aches.
While you may not normally call your doctor for these symptoms, you have to be more careful during pregnancy. Now you’re living for two (or more).
Bronchitis is fairly common, especially during the winter months. Taking preventive steps is important to help you and your baby-to-be stay well.
Bronchitis can be the result of a bacterial or viral infection. Both are unfortunately easy to catch. One of the best ways to protect against bronchitis is to wash your hands often.
Avoiding exposure to people that have bronchitis or other respiratory conditions is also important. If a loved one has an infection, try to stay away as much as you can. This is especially true if they have a fever.
The flu virus can cause bronchitis, so be sure to get an annual flu shot. You can also encourage those around you to get the shot. The flu shot doesn’t contain live viruses, so it shouldn’t make you sick.
Getting the flu shot can also boost your baby’s immune system for about six months after birth. That means your little one will be less likely to experience the flu virus.
Avoiding cigarette smoke is also important in preventing bronchitis. Smoking irritates the airway linings, hindering the body’s natural defense system against infections.
Unfortunately, for some expectant moms, bronchitis can quickly progress to a more severe respiratory disorder. One example could be pneumonia. Seek emergency medical treatment if you experience the following symptoms:
- chest pain
- coughing up blood
- fever greater than 100.
 4°F, or 38°C
4°F, or 38°C - shortness of breath that doesn’t get better with rest
While a large portion of bronchitis-related cases are due to a virus, sometimes bacteria can lead to bronchitis.
Bacteria-caused bronchitis can be treated with antibiotics if symptoms become severe or don’t seem to be getting better after a week. Check with your doctor to see if you’ll need antibiotics.
If your doctor suspects your bronchitis is due to a bacterial infection, they may prescribe antibiotics. While not all antibiotics are considered safe during pregnancy, some are.
The following antibiotics are typically considered safe during pregnancy:
- amoxicillin
- ampicillin
- clindamycin
- erythromycin
- penicillin
- nitrofurantoin
You shouldn’t take a class of antibiotics called tetracycline antibiotics. Examples include doxycycline and minocycline. These are associated with potentially causing discoloration to a baby’s teeth.
The antibiotics trimethoprim and sulfamethoxazole also are pregnancy no-no’s. They’ve been known to cause birth defects.
Antibiotics aren’t always necessary to treat bronchitis. A virus usually causes the condition and antibiotics won’t kill a virus. But if your symptoms aren’t getting better after a few days, see your doctor. They will evaluate you further and look for bacterial causes of infection.
Always check with your doctor before trying any at-home treatments. You’ll want to make sure they’re safe for you and your growing little one. While these treatments won’t cure bronchitis, they can help you feel better as your body heals.
Try irrigating your nasal passages using a mixture of 8 ounces warm water, 1/2 teaspoon of salt, and 1/2 teaspoon of baking soda. This can help you feel less stuffy.
Lean forward over a sink with your head at a 45-degree angle so that one nostril is pointed toward the sink. Using a syringe or squeeze bottle, pour the water into your nostril as you breathe through your mouth. The water should come out on the other side of your nose.
The water should come out on the other side of your nose.
Repeat this process about three to four times per day.
Other at-home treatment options include:
- Vicks vapor rub
- using a humidifier
- rest and fluids
- steamy shower
- pregnancy-safe hot tea
While you should always check with your doctor first, you may be able to take some over-the-counter antihistamines after the first trimester.
You can take the following medications to help dry up the extra mucus that has built up in your lungs after your first trimester:
- chlorpheniramine (Chlor-Trimeton)
- loratadine (Claritin)
- Novahistine
- pseudoephedrine (Sudafed)
- Tylenol Cold & Sinus
Most respiratory infections like bronchitis are not associated with a high risk for pregnancy complications or birth defects. But that doesn’t address the discomfort you experience while you are recovering from bronchitis. Take preventive measures and check in with your doctor for treatment options.
causes, risks, recommendations for treatment and prevention
- General information
- What is dangerous cough during pregnancy
- Causes and symptoms
- Common causes of cough in pregnant women
- Treatment of cough in pregnant women
- General recommendations
- Prophylaxis
Pregnant women, due to the load on the body and a weakened immune system, endure colds and SARS more difficult. This is due to the inability to take certain medications to quickly relieve symptoms, as well as the effect of the symptoms themselves on the body of a pregnant woman.
Cough as a concomitant symptom of colds provokes contraction of the abdominal, pectoral and spinal muscles. This increases the likelihood of developing uterine tone. If a pregnant woman is diagnosed with a cough with sputum that is difficult to separate, only a doctor can prescribe a drug for treatment. Most often, these are expectorants of plant origin.
General
Cold viruses mainly infect the mucous membranes of the nose and throat, as well as the upper respiratory tract. Cough that occurs when the upper respiratory tract is affected is divided into productive and unproductive.
- A productive cough is due to a cold (flu-like infection), bronchitis or an allergic disease. Accompanied by the formation of a large amount of separated mucus.
- Unproductive cough (dry cough) occurs as a result of inflammation of the larynx, trachea or bronchial mucosa, as well as irritation by foreign particles (dust or pollen). During coughing, mucus and phlegm do not calve.
The form of cough is divided into acute and chronic. An acute cough lasts less than 4 weeks and is usually caused by infection or exposure to cold. Chronic cough lasts more than 4 weeks and can be caused by recurrent respiratory infections.
What is dangerous cough during pregnancy
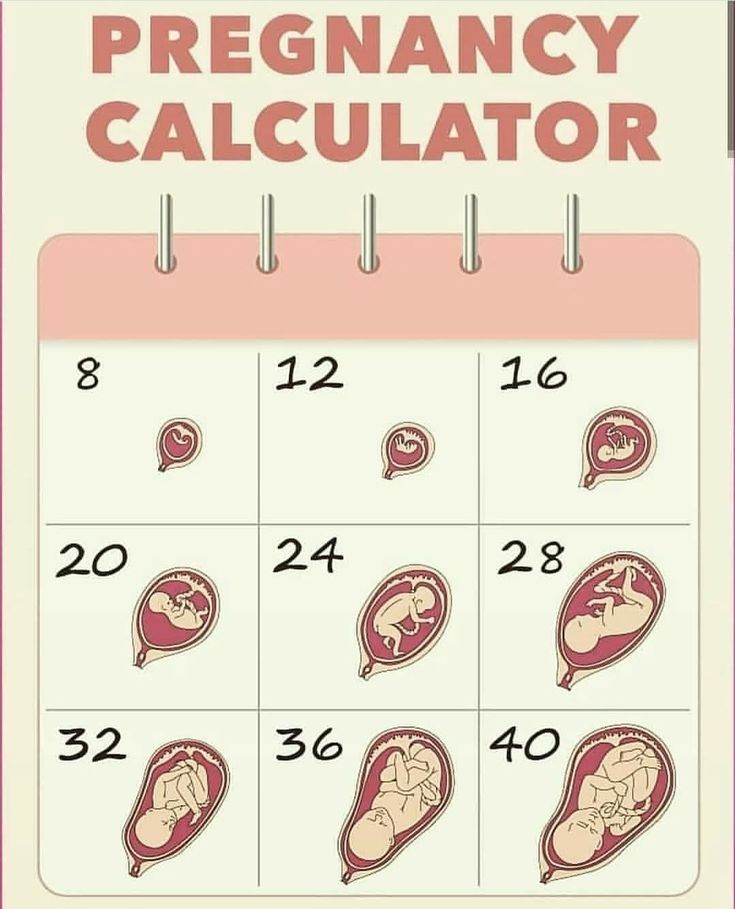
- 1st trimester.
 The nervous and vascular systems are formed in the fetus, the natural barrier in the form of the placenta has not yet formed, so the defeat of intrauterine infection is fraught with fetal pathologies.
The nervous and vascular systems are formed in the fetus, the natural barrier in the form of the placenta has not yet formed, so the defeat of intrauterine infection is fraught with fetal pathologies. - 2nd trimester. The placenta is forming, and SARS can slow down this process. Cough causes a strong load on the pelvic organs, which provokes placental abruption. Characteristic signs - pulling pain in the lower abdomen, bleeding. The supply of oxygen and nutrients stops, this leads to hypoxia. At the same time, short-term hypoxia (5-10 seconds) does no harm.
- 3rd trimester. A productive cough can lead to rupture of the amniotic sac, premature birth, bleeding. Cough, accompanied by high fever, provokes the aging of the placenta.
In addition, any symptom of SARS is an additional stress for the expectant mother. A constant feeling of discomfort, fears for the health of the child contribute to the production of cortisol. The stress hormone, in turn, activates the work of the heart, provokes vasospasm, which, with prolonged exposure to the body, increases the risk of fetal hypoxia.
Against the background of a catarrhal disease suffered by the mother, the child may have weak immunity, nervousness, and low weight. According to medical observations, during the gestation period, viral diseases are most common - up to 85% of cases. Bacterial diseases account for up to 15% of cases. Common pathogens are adenoviruses, streptococci, coronaviruses, enteroviruses, rhinoviruses.
Causes and symptoms
The nature of the cough helps the specialist to establish its cause and make a preliminary diagnosis.
- Influenza - dry cough, sometimes purulent mucous discharge appears after a few days. Cough is accompanied by severe headache and muscle pain, high fever and general weakness.
- Bronchitis - a sharp spasmodic cough with contraction of the abdominal muscles. A strong cough can trigger a gag reflex. There is pain in the chest area. Cough worse in cold or dry air.
- Allergic cough is a problem faced by pregnant women due to hormonal changes.
 Contact with an allergen provokes attacks of suffocation. Discharges of a mucous nature and are practically absent.
Contact with an allergen provokes attacks of suffocation. Discharges of a mucous nature and are practically absent. - Rhinitis and pharyngitis accompanied by nocturnal dry cough. In rare cases, the head and the area under the eyes hurt.
- Pleurisy - acute chest pain, shortness of breath, high temperature, which practically does not go astray, frequent dry cough.
- Measles - debilitating cough and skin rash.
Causes of cough typical of pregnant women
- Dryness in the room, which increases the sensitivity of mucous membranes. This leads to an increased urge to cough. This problem is more common during the winter months in heavily heated rooms.
- Vasomotor rhinitis during pregnancy is a runny nose caused not by viruses, but by hormonal changes. With a stuffy nose, patients breathe more often through the mouth, which leads to overdrying of the mucous membrane, which, in turn, leads to irritation of the throat.
- Heartburn is a typical complaint.
 Coughing fits occur when lying down, when acid flows from the stomach back into the esophagus, irritating the sensitive mucous membrane of the throat, and then there is an urge to cough.
Coughing fits occur when lying down, when acid flows from the stomach back into the esophagus, irritating the sensitive mucous membrane of the throat, and then there is an urge to cough. - Cardiac cough occurs after excessive exercise and as a consequence of heart failure. The blood stagnates, edema forms in the lungs, which irritates the respiratory receptors and provokes a cough.
Treatment of cough in pregnant women
Due to the sensitivity of the situation and the risk of complications, most drugs and preventive measures are not recommended for pregnant women. If the disease is mild and does not require antibiotics, then you can limit yourself to general recommendations, after consulting with your doctor.
Consultation with the attending physician is required as a preventive measure before starting treatment to identify the causative agent of cough. The selection of drugs takes place taking into account their teratogenicity - the degree of toxicity of the drug in relation to the embryo.
Cough remedies are divided into two main groups - antitussive and expectorant. Their simultaneous reception is not allowed. Antitussives, peripherally or centrally act on the receptors and the cough center, blocking the urge to cough. Expectorants are divided into:
- mucolytics, which thin the sputum and help to expel it;
- drugs that activate the cough and vomiting centers in the brain by irritating the nerve endings and thereby stimulate the expectoration process;
- drugs that increase the amount of pulmonary surfactant (prescribed for dry cough and wheezing in the bronchi).
In addition to drugs, pregnant women are recommended to rinse the nasopharynx. They are designed for local action, they are not absorbed into the blood and do not cause complications in the fetus.
Pregnant women can take cough and sore throat lozenges, topical sprays with anti-inflammatory or antimicrobial effects. Even at high concentrations, only a small dose enters the digestive system.
Inhalations with a nebulizer help to improve secretion and sputum output. The device must not be used at high temperatures.
General recommendations
- Room humidity should be 65-70%. This level of humidity is comfortable for the body, prevents the mucous membrane from drying out, and reduces the rate of development of pathogens. Wet cleaning reduces the risk of contact with allergens (pollen, dust, pet hair).
- The room must be regularly ventilated, at least 2 times a day. Fresh air reduces the concentration of the virus in the air. The temperature in the room is recommended to be maintained at 22 degrees.
- Sufficient fluids must be drunk to allow sputum to thin naturally.
- Bed rest, especially in the first 3-4 days after the onset of the first symptoms.
Prevention
- It is not recommended to visit crowded places, especially during seasonal influenza epidemics.
- Contact with sick people should be limited.
- Nasal moisturizers should be used regularly.
- After visiting public places, it is important to thoroughly clean hands with antibacterial agents.
- Must wear a gauze bandage when visiting health facilities and public facilities.
- Use only personal household appliances and hygiene products to avoid household transmission of microbes.
Dry cough during pregnancy: causes and treatment
Diagnosis of cough during pregnancy
As a rule, the examination is carried out by a general practitioner who, after the examination, can refer you to another specialist. Diagnosis of cough during pregnancy without fail begins with a physical examination, which includes:
- measurement of body temperature;
- heart rate check;
- blood pressure measurement;
- palpation of the lymph nodes.
The data obtained at this stage of the examination are very important for determining the cause of the cough as accurately as possible. No less significant is the analysis of anamnesis and complaints.
No less significant is the analysis of anamnesis and complaints.
An initial examination is often sufficient to determine the cause of a cough in pregnant women. If there is not enough data to establish an accurate diagnosis, the doctor may order an ultrasound scan or the following tests:
| Diagnostic procedure | Time |
|---|---|
| Sputum examination | 15-30 minutes |
| Complete blood count | 10 minutes |
| Blood chemistry | 10 minutes |
| Allergy test | 20 minutes |
In difficult cases, chest x-rays may be used for pregnant women. However, this is permissible only when the risk of developing pathology is more serious than the harm that the study brings. Before visiting a doctor, take a self-diagnosis on our website. It is worth noting that passing this test does not replace going to the doctor. Its results are only approximate and help to navigate what to look for when visiting a doctor. That is why they cannot be used to make a diagnosis and prescribe therapy.
Its results are only approximate and help to navigate what to look for when visiting a doctor. That is why they cannot be used to make a diagnosis and prescribe therapy.
Which doctor should I contact?
If you have a dry cough, see a doctor in the following specialty:
Our specialists
Suvan-ool Marina Anatolyevna
Where the doctor takes:
m. Street 1905
Make an appointment for an appointment
Vlasova Svetlana Sergeevna
Where the doctor takes:
m. Prospekt Mira
m. at reception
Abramova Irina Petrovna
Where the doctor sees:
m. Street 1905
Make an appointment for an appointment
Goncharova Ekaterina Olegovna
Where the doctor takes:
m. Street 1905
m. Street 1905
for an appointment
Cheremisina Anna Yurievna
Where does the doctor:
m. Street 1905 goda
Sign up for an appointment
Myasnikova Natalia Petrovna
Where the doctor takes:
m. Street 1905
Make an appointment for an appointment
Buchina Anaida Valerievna
Where the doctor takes:
m. Street 1905
Make an appointment for an appointment
After the examination, the doctor will prescribe the necessary diagnostics in your case. Some diseases are difficult to diagnose as they say "by eye". Therefore, you need to trust the doctor when prescribing research. After all the tests, the doctor will be able to draw up the correct course of treatment. Remember: accurate diagnosis and correct diagnosis are already 50% of success in treatment!
Remember: accurate diagnosis and correct diagnosis are already 50% of success in treatment!
Dry cough during pregnancy
Any changes in a woman's condition during pregnancy require attention. In particular, dry cough during pregnancy can harm the unborn baby. It can appear due to an acute respiratory illness or influenza virus. To treat such a cough, expectorants (syrups, lozenges) or special procedures that provoke sputum production, for example, inhalation, are used. It is important to note that the use of folk or over-the-counter remedies without the advice of a doctor can be dangerous for the fetus.
Cough in early pregnancy
In the first trimester, due to a sharp restructuring of the body, a woman's immunity decreases. That is why coughing in early pregnancy occurs quite often. It can be provoked by:
- a cold;
- influenza;
- stress;
- gastric disorders.
One of the causes of cough is allergy. As a rule, during this period, it weakens, which is associated with the production of a large amount of cortisol, which has anti-allergic activity. However, some observe an exacerbation of diseases.
As a rule, during this period, it weakens, which is associated with the production of a large amount of cortisol, which has anti-allergic activity. However, some observe an exacerbation of diseases.
In early pregnancy, a cough, no matter what causes it, can cause significant harm to the baby. Therefore, the treatment of diseases must be carried out as early as possible. The negative effect is explained by the fact that during coughing, tension of the uterus occurs, which in turn impairs the blood supply to the fetus and reduces the amount of nutrients it receives. In the first trimester, such a symptom can lead to:
- the development of hypoxia in the baby;
- placental abruption;
- I will miscarry.
In order to understand how to get rid of a cough during pregnancy and not harm the health of the fetus, you should seek the help of a doctor.
Cough in the second and third trimesters
In later periods, such manifestations are less dangerous. In the second trimester, the fetus is already protected by the placenta, so uterine contractions practically do not affect the supply of nutrients to its body. However, this does not mean that the diseases that provoke coughing can not be treated. The symptom itself is not dangerous, but the pathology that it signals can cause:
In the second trimester, the fetus is already protected by the placenta, so uterine contractions practically do not affect the supply of nutrients to its body. However, this does not mean that the diseases that provoke coughing can not be treated. The symptom itself is not dangerous, but the pathology that it signals can cause:
- abnormal development of the endocrine system;
- miscarriages;
- abnormal formation of bone tissue.
It is also worth noting that in the third trimester the placenta becomes more permeable and can pass a large number of viruses, which leads to congenital pathologies.
Cough during pregnancy: treatment
Depending on why an unpleasant symptom appeared, the doctor will prescribe the necessary therapy. Cough during pregnancy, which appeared due to allergies, is treated by taking antihistamines and eliminating the irritant. They can be plant pollen, animal hair, dust, food. For the treatment of colds and viral respiratory diseases, drugs are used that restore immunity, relieve spasm.