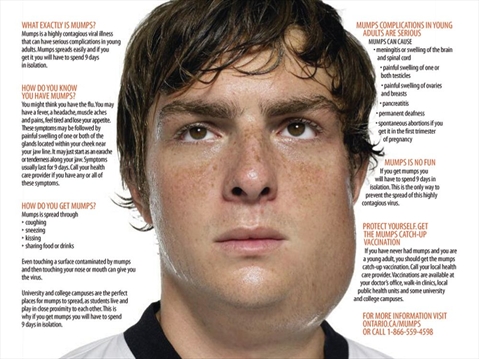
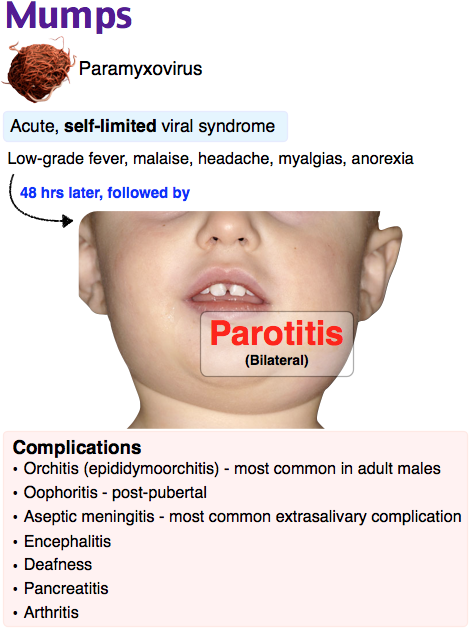
Complications of mumps
Mumps - Complications - NHS
There are several problems that often occur with mumps. These can be worrying, but they're rarely serious and usually improve as the infection passes.
Common complications
Swollen testicle
Pain and swelling of the testicle (orchitis) affects up to 1 in 3 males who get mumps after puberty. The swelling is usually sudden and affects only one testicle. The testicle may also feel warm and tender.
In affected boys and men, swelling of the testicle normally begins 4 to 8 days after the swelling of the parotid gland. Occasionally, swelling can occur up to 6 weeks after the swelling of the glands.
Any testicle pain can be eased using painkillers such as paracetamol or ibuprofen you buy from the pharmacy or supermarket. If the pain is particularly severe, contact your GP, who may prescribe you a stronger painkiller.
Applying cold or warm compresses to your testicle and wearing supportive underwear may also reduce any pain.
Just under half of all males who get mumps-related orchitis notice some shrinkage of their testicles and an estimated 1 in 10 men experience a drop in their sperm count (the amount of healthy sperm their body can produce). However, this is very rarely large enough to cause infertility.
Swollen ovaries
About 1 in 15 females who get mumps after puberty experience swelling of the ovaries (oophoritis), which can cause:
- lower abdominal pain
- high temperature
- being sick
The symptoms of oophoritis usually pass once the body has fought off the underlying mumps infection.
Viral meningitis
Viral meningitis can occur if the mumps virus spreads into the outer protective layer of the brain (the meninges).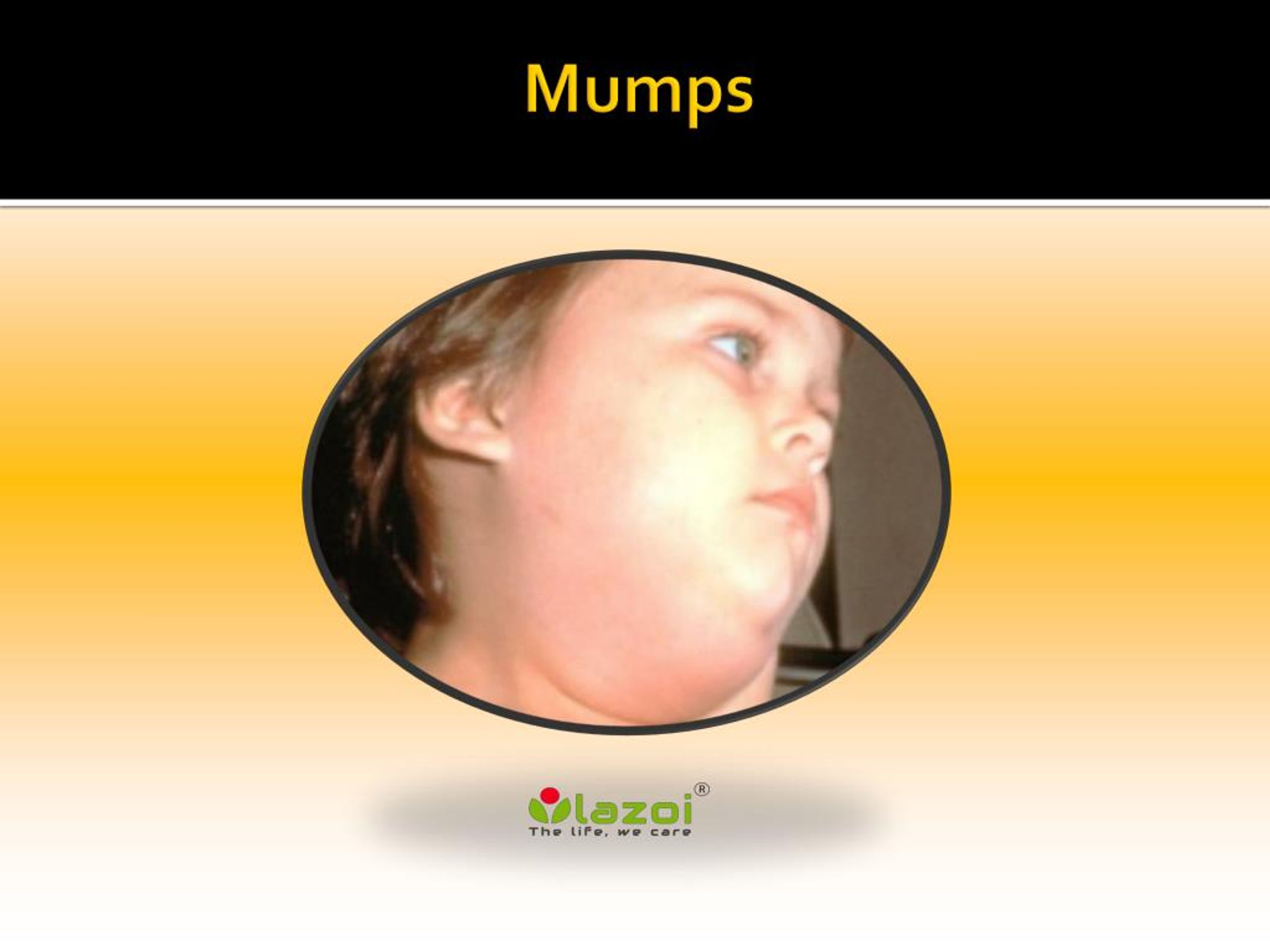 It occurs in up to 1 in 4 cases of mumps.
It occurs in up to 1 in 4 cases of mumps.
Unlike bacterial meningitis, which is regarded as a potentially life-threatening medical emergency, viral meningitis causes milder, flu-like symptoms, and the risk of serious complications is low.
Sensitivity to light, neck stiffness and headaches are common symptoms of viral meningitis. These usually pass within 14 days.
Pancreatitis
About 1 in 25 cases of mumps lead to short-term inflammation of the pancreas (acute pancreatitis). The most common symptom is sudden pain in the centre of your belly.
Other symptoms of acute pancreatitis can include:
- feeling or being sick
- diarrhoea
- loss of appetite
- high temperature
- tenderness of the belly
- less commonly, yellowing of the whites of the eyes and the skin (jaundice), although this may be less noticeable on black or brown skin
Although pancreatitis associated with mumps is usually mild, you may be admitted to hospital so your body functions can be supported until your pancreas recovers.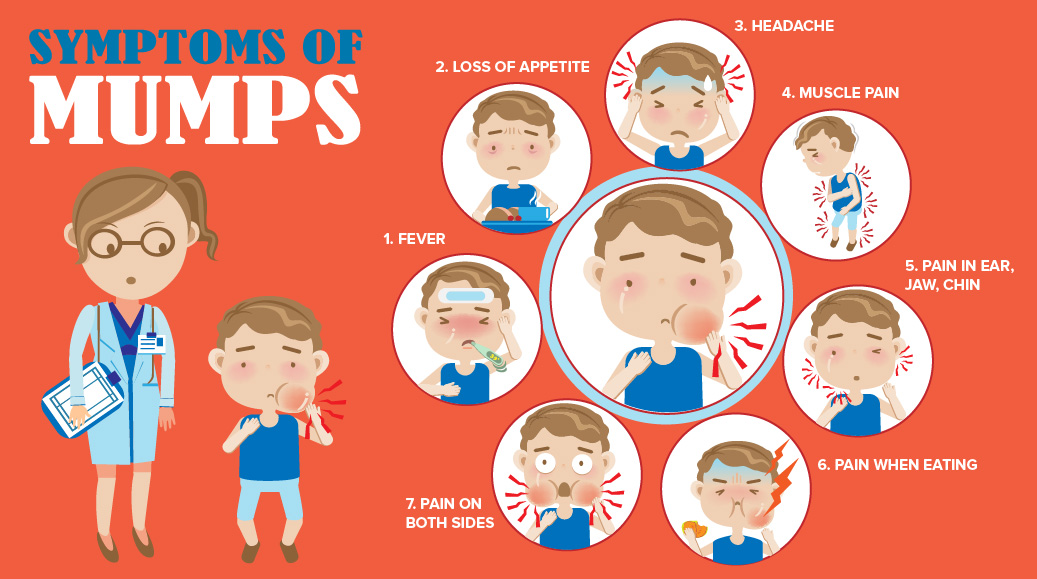
Rare complications of mumps
Rare but potentially serious complications of mumps include an infection of the brain itself, known as encephalitis. This is thought to occur in around 1 in 1,000 cases of mumps. Encephalitis is a potentially fatal condition that requires admission to a hospital intensive care unit.
About 1 in 25 people with mumps experience some temporary hearing loss, but permanent loss of hearing is rare. It's estimated this occurs in around 1 in 20,000 cases of mumps.
Mumps and pregnancy
In the past it was thought developing mumps during pregnancy increased the risk of miscarriage, but there's little evidence to support this.
But, as a general precaution it's recommended pregnant women avoid close contact with people known to have an active mumps infection (or any other type of infection).
If you're pregnant and you think you've come into contact with someone with mumps but you haven't been vaccinated, contact your GP or midwife for advice.
Page last reviewed: 24 September 2021
Next review due: 24 September 2024
Mumps - Symptoms and causes
Overview
Salivary glands
Salivary glands
You have three pairs of major salivary glands — parotid, sublingual and submandibular. Each gland has its own tube (duct) leading from the gland to the mouth.
Mumps is a viral infection that primarily affects saliva-producing (salivary) glands that are located near your ears. Mumps can cause swelling in one or both of these glands.
Mumps was common in the United States until mumps vaccination became routine. Since then, the number of cases has dropped dramatically.
However, mumps outbreaks still occur in the United States, and the number of cases has crept up in recent years. These outbreaks generally affect people who aren't vaccinated, and occur in close-contact settings such as schools or college campuses.
These outbreaks generally affect people who aren't vaccinated, and occur in close-contact settings such as schools or college campuses.
Complications of mumps, such as hearing loss, are potentially serious but rare. There's no specific treatment for mumps.
Products & Services
- Book: Mayo Clinic Guide to Raising a Healthy Child
Symptoms
Mumps
Mumps
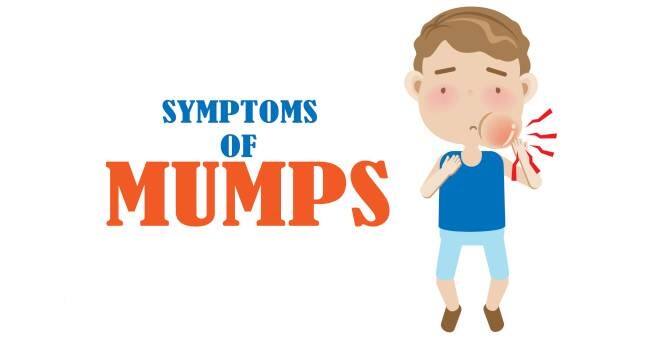
Mumps is characterized by swollen, painful salivary glands in the face, causing the cheeks to puff out.
Some people infected with the mumps virus have either no signs or symptoms or very mild ones. When signs and symptoms do develop, they usually appear about two to three weeks after exposure to the virus.
The primary sign of mumps is swollen salivary glands that cause the cheeks to puff out. Other signs and symptoms may include:
- Pain in the swollen salivary glands on one or both sides of your face
- Pain while chewing or swallowing
- Fever
- Headache
- Muscle aches
- Weakness and fatigue
- Loss of appetite
When to see a doctor
See your doctor if you or your child has signs and symptoms of mumps. Mumps is highly contagious for about nine days after symptoms appear. Tell your doctor's office before you go in that you suspect mumps so arrangements can be made to avoid spreading the virus to others in the waiting room.
Mumps is highly contagious for about nine days after symptoms appear. Tell your doctor's office before you go in that you suspect mumps so arrangements can be made to avoid spreading the virus to others in the waiting room.
In the meantime:
- Rest as much as possible
- Try to ease symptoms with cold compresses and over-the-counter pain relievers such as ibuprofen (Advil, Motrin IB, others) and acetaminophen (Tylenol, others)
Mumps has become uncommon, so it's possible that another condition is causing your signs and symptoms. Swollen salivary glands and a fever could indicate:
- A blocked salivary gland
- A different viral infection
Request an Appointment at Mayo Clinic
From Mayo Clinic to your inbox
Sign up for free, and stay up to date on research advancements, health tips and current health topics, like COVID-19, plus expertise on managing health.
To provide you with the most relevant and helpful information, and understand which
information is beneficial, we may combine your email and website usage information with
other information we have about you.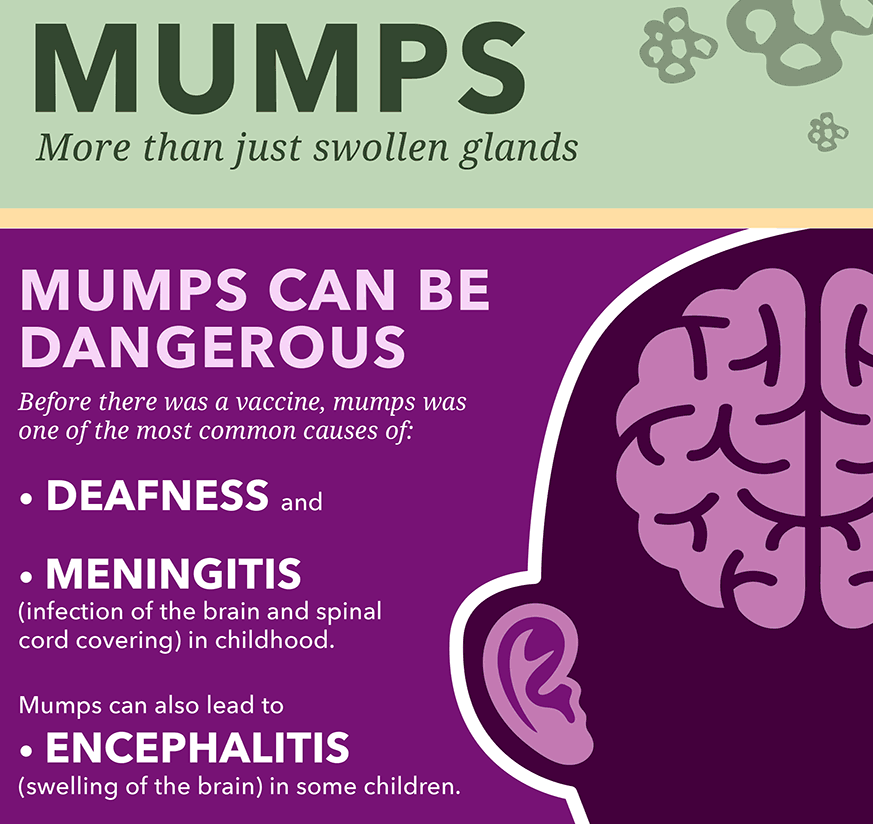 If you are a Mayo Clinic patient, this could
include protected health information. If we combine this information with your protected
health information, we will treat all of that information as protected health
information and will only use or disclose that information as set forth in our notice of
privacy practices. You may opt-out of email communications at any time by clicking on
the unsubscribe link in the e-mail.
If you are a Mayo Clinic patient, this could
include protected health information. If we combine this information with your protected
health information, we will treat all of that information as protected health
information and will only use or disclose that information as set forth in our notice of
privacy practices. You may opt-out of email communications at any time by clicking on
the unsubscribe link in the e-mail.
Causes
Mumps is caused by a virus that spreads easily from person to person through infected saliva. If you're not immune, you can contract mumps by breathing in saliva droplets from an infected person who has just sneezed or coughed. You can also contract mumps from sharing utensils or cups with someone who has mumps.
Complications
Complications of mumps are rare, but some are potentially serious.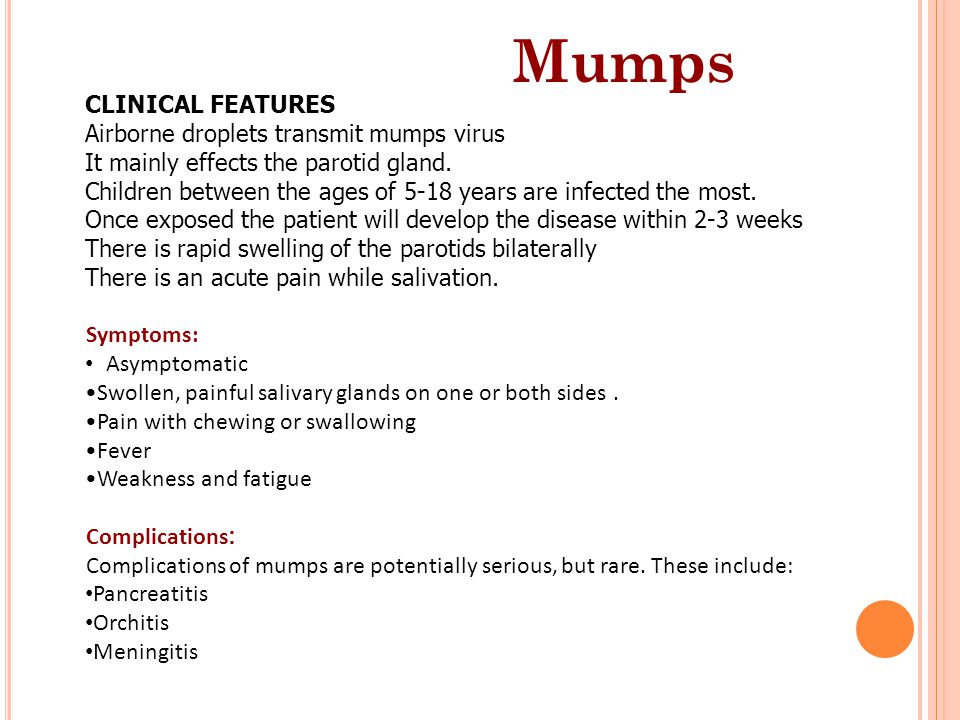
Most mumps complications involve inflammation and swelling in some part of the body, such as:
- Testicles. This condition, known as orchitis, causes one or both testicles to swell in males who've reached puberty. Orchitis is painful, but it rarely leads to the inability to father a child (sterility).
- Brain. Viral infections such as mumps can lead to inflammation of the brain (encephalitis). Encephalitis can cause neurological problems and become life-threatening.
- Membranes and fluid around the brain and spinal cord. This condition, known as meningitis, can occur if the mumps virus spreads through your bloodstream to infect your central nervous system.
- Pancreas. The signs and symptoms of this condition, known as pancreatitis, include pain in the upper abdomen, nausea and vomiting.
Other complications of mumps include:
- Hearing loss. Hearing loss can occur in one or both ears.
 Although rare, the hearing loss is sometimes permanent.
Although rare, the hearing loss is sometimes permanent. - Heart problems. Rarely, mumps has been associated with abnormal heartbeat and diseases of the heart muscle.
- Miscarriage. Contracting mumps while you're pregnant, especially early in your pregnancy, may lead to miscarriage.
Prevention
The best way to prevent mumps is to be vaccinated against the disease. Most people have immunity to mumps once they're fully vaccinated.
The mumps vaccine is usually given as a combined measles-mumps-rubella (MMR) inoculation, which contains the safest and most effective form of each vaccine. Two doses of the MMR vaccine are recommended before a child enters school. Those vaccines should be given when the child is:
- Between the ages of 12 and 15 months
- Between the ages of 4 and 6 years
College students, international travelers and health care workers in particular are encouraged to make sure they've had two doses of the MMR vaccine. A single dose is not completely effective at preventing mumps.
A single dose is not completely effective at preventing mumps.
A third dose of vaccine isn't routinely recommended. But your doctor might recommend a third dose if you are in an area that is experiencing an outbreak. A study of a recent mumps outbreak on a college campus showed that students who received a third dose of MMR vaccine had a much lower risk of contracting the disease.
Those who don't need the MMR vaccine
You don't need a vaccination if you:
- Had two doses of the MMR vaccine after 12 months of age
- Had one dose of MMR after 12 months of age and you're a preschool child or an adult who isn't at high risk of measles or mumps exposure
- Have blood tests that demonstrate your immunity to measles, mumps and rubella
- Were born before 1957 — most people in that age group were likely infected by the virus naturally and have immunity
Also, the vaccine isn't recommended for:
- People who have had a life-threatening allergic reaction to the antibiotic neomycin or any other component of the MMR vaccine
- Pregnant women or women who plan to get pregnant within the next four weeks
- People with severely compromised immune systems
Those who should get the MMR vaccine
You should get vaccinated if you don't fit the criteria listed above and if you:
- Are a nonpregnant woman of childbearing age
- Attend college or another postsecondary school
- Work in a hospital, medical facility, child care center or school
- Plan to travel overseas or take a cruise
Those who should wait to get the MMR vaccine
Consider waiting if:
- You're moderately or severely ill.
 Wait until you recover.
Wait until you recover. - You're pregnant. Wait until after you give birth.
Those who should check with their doctors
Talk to your doctor before getting vaccinated for mumps if you:
- Have cancer
- Have a blood disorder
- Have a disease that affects your immune system, such as HIV/AIDS
- Are being treated with drugs, such as steroids, that affect your immune system
- Have received another vaccine within the past four weeks
Side effects of the vaccine
The MMR vaccine is very safe and effective. Getting the MMR vaccine is much safer than getting mumps.
Most people experience no side effects from the vaccine. Some people experience a mild fever or rash or achy joints for a short time.
Rarely, children who get the MMR vaccine might experience a seizure caused by fever. But these seizures haven't been associated with any long-term problems.
Extensive reports — from the American Academy of Pediatrics, the Institute of Medicine and the Centers for Disease Control and Prevention — conclude that there's no link between the MMR vaccine and autism.
By Mayo Clinic Staff
Parotitis in children: recommendations, treatment, complications
Share
Authors: doctor, Ph.D. doctor, candidate of medical sciences, Tolmacheva E. A., [email protected]
doctor, scientific director of JSC "Vidal Rus", Zhuchkova T.V., [email protected]
Table of contents:
- General information
- Causes of disease
- Symptoms of mumps (mumps)
- Complications
- What can you do
- Treatment
- Prophylaxis
General information
Mumps (often referred to as mumps) is an acute viral disease in which inflammation of the salivary glands occurs. Most often, mumps affects children aged 5-15 years, but adults can also get sick.
As a rule, the disease is not very severe. However, parotitis has a number of dangerous complications. To insure against an unfavorable course of the disease, it is necessary to prevent the very possibility of developing mumps.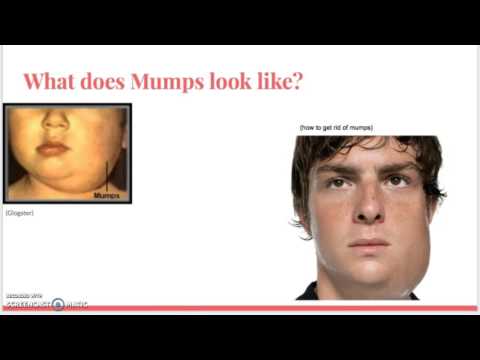 For this, there is a mumps vaccine, which is included in the list of mandatory vaccinations in all countries of the world.
For this, there is a mumps vaccine, which is included in the list of mandatory vaccinations in all countries of the world.
Causes of disease
Infection occurs by airborne droplets (when coughing, sneezing, talking) from a sick person. A sick mumps is contagious 1-2 days before the onset of the first signs of the disease and within 9 days after its onset (the maximum isolation of the virus is from the third to the fifth day). After entering the body, the virus multiplies in the glandular tissue and can affect almost all glands of the body - genital, salivary, pancreas, thyroid. Changes in the work of most glands rarely reach the level at which specific complaints and symptoms begin to arise, but the salivary glands are affected first and most severely.
Symptoms of mumps (mumps)
The disease usually has an acute onset. The temperature can rise to 40 degrees, there is pain in the ear or in front of it, especially when chewing and swallowing, increased salivation. Especially sharp pain occurs when food is ingested, causing profuse salivation (for example, sour). Inflammation of the parotid salivary gland causes an increase in the cheek - a rapidly spreading swelling appears in front of the auricle, which increases to the maximum by the 5-6th day. The earlobe protrudes upwards and anteriorly, which gives the patient a characteristic appearance. Feeling this place is painful. Elevated body temperature persists for 5-7 days.
Especially sharp pain occurs when food is ingested, causing profuse salivation (for example, sour). Inflammation of the parotid salivary gland causes an increase in the cheek - a rapidly spreading swelling appears in front of the auricle, which increases to the maximum by the 5-6th day. The earlobe protrudes upwards and anteriorly, which gives the patient a characteristic appearance. Feeling this place is painful. Elevated body temperature persists for 5-7 days.
Complications
The most common complications of mumps are inflammation of the pancreas (pancreatitis) and gonads. Perhaps inflammation of the thyroid and other internal glands of the body, as well as damage to the nervous system in the form of meningitis or encephalitis.
Pancreatitis begins with severe pain in the abdomen (often girdle), vomiting, loss of appetite, stool disorders. If you notice the appearance of such symptoms, you should immediately consult a doctor.
Sex glands can be affected in both boys and girls. If in boys the inflammation of the testicles is quite noticeable, due to their anatomical location and a rather vivid clinical picture (a new rise in temperature, soreness of the testicle, discoloration of the skin above it), then in girls the diagnosis of ovarian damage is difficult. The consequence of such inflammation may subsequently be testicular atrophy and infertility in men, ovarian atrophy, infertility, menstrual dysfunction in women.
If in boys the inflammation of the testicles is quite noticeable, due to their anatomical location and a rather vivid clinical picture (a new rise in temperature, soreness of the testicle, discoloration of the skin above it), then in girls the diagnosis of ovarian damage is difficult. The consequence of such inflammation may subsequently be testicular atrophy and infertility in men, ovarian atrophy, infertility, menstrual dysfunction in women.
What can you do
There is no specific therapy for mumps. The disease is most dangerous in boys during puberty, due to possible damage to the testicles. Treatment is aimed at preventing the development of complications. Do not self-medicate. Only a doctor can correctly diagnose and check whether other glands are affected.
Treatment
What a doctor can do
In typical cases, the diagnosis does not cause difficulties and the doctor immediately prescribes treatment. In doubtful cases, the doctor may prescribe additional diagnostic methods. Patients are advised to stay in bed for 7-10 days. It is known that in boys who did not comply with bed rest during the 1st week, orchitis (inflammation of the testicles) develops about 3 times more often. It is necessary to monitor the cleanliness of the oral cavity. To do this, prescribe daily rinsing with a 2% solution of soda or other disinfectants.
Patients are advised to stay in bed for 7-10 days. It is known that in boys who did not comply with bed rest during the 1st week, orchitis (inflammation of the testicles) develops about 3 times more often. It is necessary to monitor the cleanliness of the oral cavity. To do this, prescribe daily rinsing with a 2% solution of soda or other disinfectants.
A dry, warm dressing is applied to the affected salivary gland. Patients are prescribed liquid or crushed food. To prevent inflammation of the pancreas, in addition, it is necessary to follow a certain diet: avoid overeating, reduce the amount of white bread, pasta, fats, cabbage. The diet should be dairy-vegetarian. From cereals it is better to use rice, brown bread, potatoes are allowed.
Prevention of mumps (mumps)
The danger of complications of mumps is beyond doubt. That is why methods of preventing this disease are so common in the form of quarantine in children's groups and preventive vaccinations.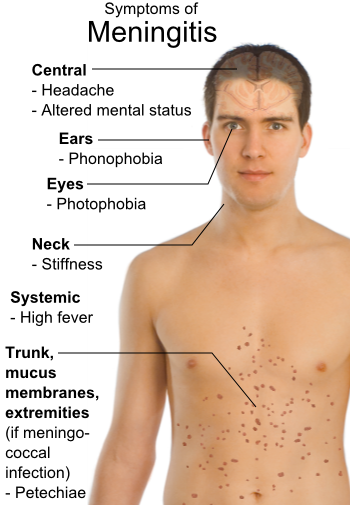 The patient is isolated until the 9th day of illness; children who have been in contact with the patient are not allowed to visit children's institutions (nurseries, kindergartens, schools) for 21 days. However, the problem is that in 30-40% of those infected with the virus, no signs of the disease occur (asymptomatic forms). Therefore, avoiding mumps, hiding from patients, is not always possible. Accordingly, the only acceptable way of prevention is vaccination. According to the preventive vaccination calendar in Russia, vaccination against mumps is carried out at 12 months and at 6 years.
The patient is isolated until the 9th day of illness; children who have been in contact with the patient are not allowed to visit children's institutions (nurseries, kindergartens, schools) for 21 days. However, the problem is that in 30-40% of those infected with the virus, no signs of the disease occur (asymptomatic forms). Therefore, avoiding mumps, hiding from patients, is not always possible. Accordingly, the only acceptable way of prevention is vaccination. According to the preventive vaccination calendar in Russia, vaccination against mumps is carried out at 12 months and at 6 years.
Before using any drug, consult a specialist and read the instructions for use.
References
- Infectious diseases. National leadership. / Ed. N.D. Yushchuk, Yu.Ya. Vengerov. - M.: GEOTAR-Media, 2019. - 848 p.
- Children's infectious diseases: a textbook. / L.G. Kuzmenko. - Academia, 2009. - 528 p.
- Emergency pediatrics. National leadership. / under the reaction of B.
 M. Blokhin. - M.: GEOTAR-Media, 2017. - 832 p.
M. Blokhin. - M.: GEOTAR-Media, 2017. - 832 p.
← Previous article
Read more
You may be interested in
- Increased body temperature in children
- birth trauma
- Hardening a child
- Where to get vaccinated
- Allergy in newborns
Mumps (epidemic)
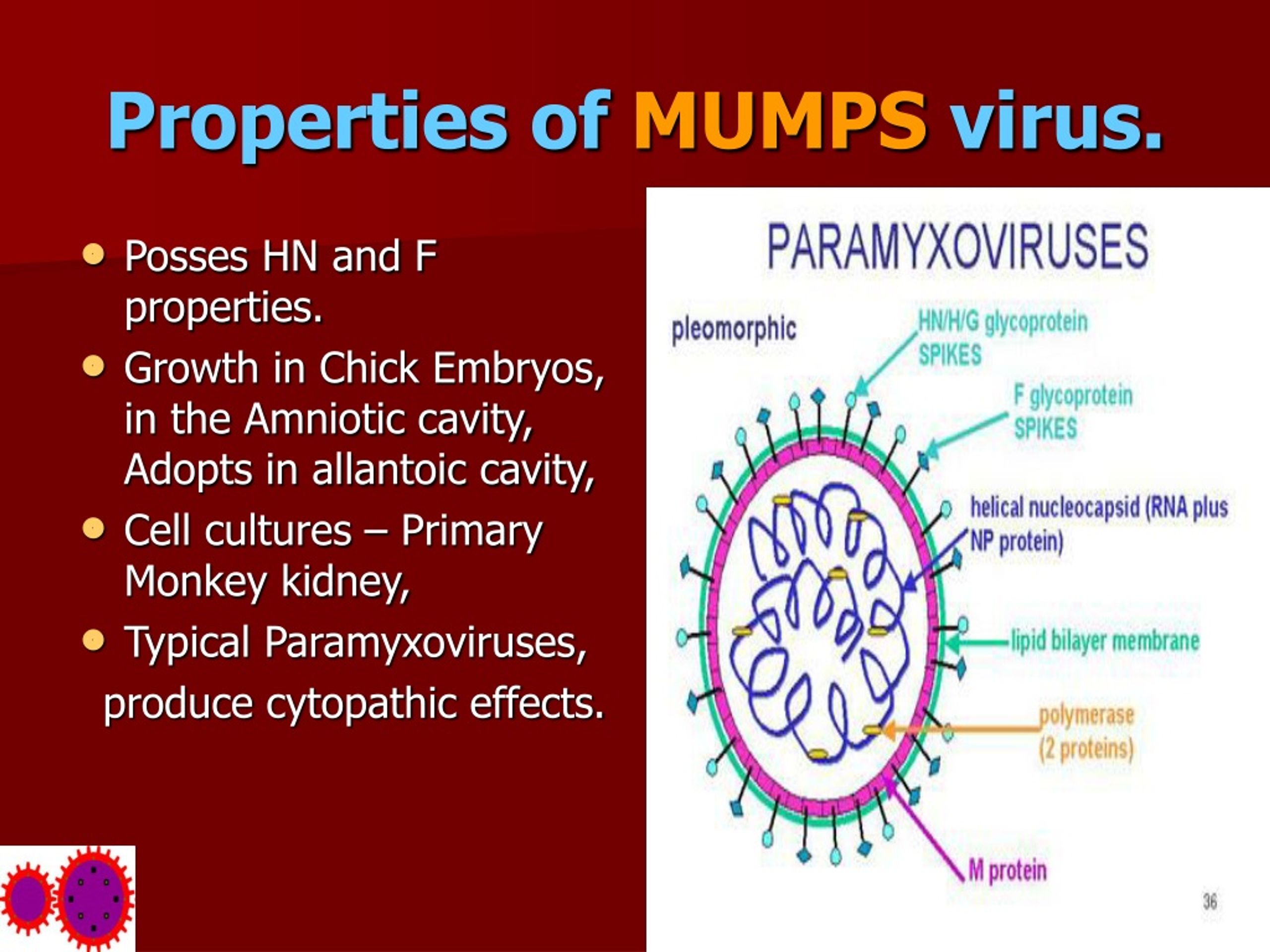
Mumps is an acute infectious disease caused by a virus of the paramyxovirus family. The main signs of the disease are intoxication and inflammation of the parotid salivary glands.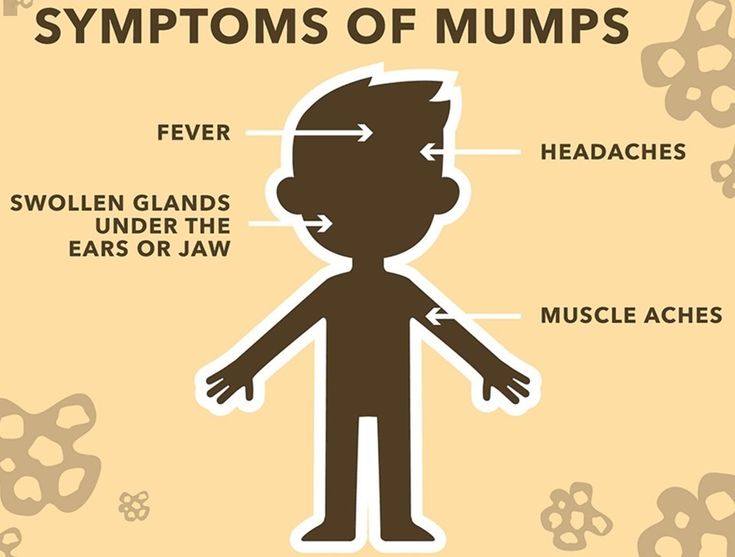 In some cases, other organs may be involved in the pathological process: the nervous system, testicles, pancreas. After the disease, in almost all cases, stable lifelong immunity is formed.
In some cases, other organs may be involved in the pathological process: the nervous system, testicles, pancreas. After the disease, in almost all cases, stable lifelong immunity is formed.
There is a vaccine against mumps that can significantly reduce the risk of infection, and before the introduction of mass vaccination it was widely available. Now outbreaks of infection are rare in developed countries. Most often, children aged 2-12 years get sick, although recently the percentage of adults has increased among the sick - those who were not vaccinated in a timely manner and who did not develop a sufficiently strong immunity as a result of vaccination.
The prognosis for parotitis is generally favorable. Complications are quite rare and in most cases do not lead to irreversible pathological changes. However, mumps can sometimes cause infertility, deafness, and neurological problems.
Russian synonyms
Mumps, mumps, mumps.
English synonyms
Parotitis, mumps.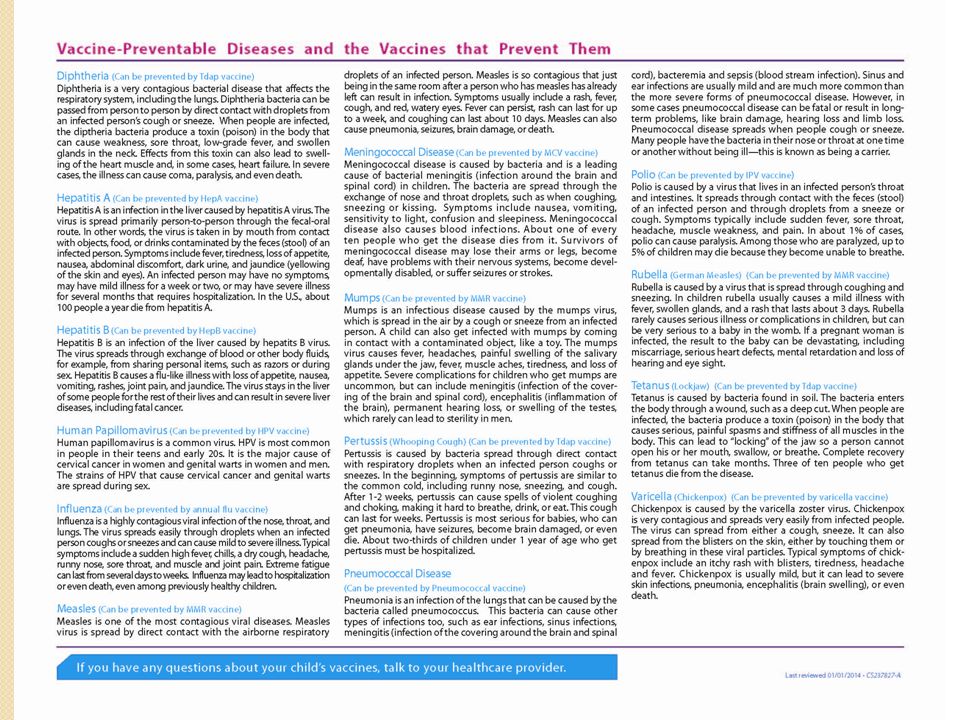
Symptoms
The initial stages of the disease are characterized by non-specific symptoms of general intoxication. About 20% of patients experience almost no discomfort - the disease can proceed unnoticed. The most characteristic sign of mumps - inflammation of the parotid salivary glands - develops only on the third day of the disease or may be completely absent.
The main symptoms of mumps are:
- fever,
- malaise,
- loss of appetite,
- swelling, soreness in the parotid salivary gland on one or both sides, which is aggravated by chewing, drinking acidic drinks, talking.
General information about the disease
The mumps virus belongs to the paromyxovirus family and resembles the influenza virus in structure. It consists of a single-stranded RNA surrounded by a glycoprotein envelope.
You can become infected from an infected person through airborne droplets. The virus is unstable in the external environment. The incubation period, that is, the time between contact with the source of infection and the onset of symptoms, is 2-3 weeks. A sick person is contagious already two days before the first symptoms and about a week after they appear. Uncomplicated parotitis usually lasts about seven days, rarely up to ten.
The virus is unstable in the external environment. The incubation period, that is, the time between contact with the source of infection and the onset of symptoms, is 2-3 weeks. A sick person is contagious already two days before the first symptoms and about a week after they appear. Uncomplicated parotitis usually lasts about seven days, rarely up to ten.
Children aged 2-12 are most affected by mumps. During the first year of life, the child's body is usually protected by maternal antibodies. At the same time, the disease is more severe in adults.
The onset of mumps is usually accompanied by non-specific symptoms: fever, muscle pain, weakness, loss of appetite. The temperature is highest on the second day of illness. On the third day, 95% of patients experience swelling, pain in the parotid salivary glands, after which the manifestations of general intoxication begin to subside. Swelling of the salivary glands persists for up to 10 days. Inflammation of the parotid salivary glands can be one- or two-sided, the pain is aggravated by chewing, swallowing. The skin over the glands is tense. Soreness is especially pronounced with pressure in front of the earlobe and behind it, as well as in the region of the mastoid process. There is also a symptom of Mursu - inflammation in the area of the excretory duct of the gland. The swelling can also spread to the neck area.
The skin over the glands is tense. Soreness is especially pronounced with pressure in front of the earlobe and behind it, as well as in the region of the mastoid process. There is also a symptom of Mursu - inflammation in the area of the excretory duct of the gland. The swelling can also spread to the neck area.
Complications of mumps are rare. Most often, the following violations occur.
- Damage to the nervous system - encephalitis and meningitis. Mild forms of neurological disorders are observed in 10% of patients with parotitis, but in the vast majority of cases they are completely curable and do not lead to severe consequences.
- Sensorineural deafness. Reversible hearing impairment develops in 4% of patients, but irreversible deafness is much less common and more often unilateral.
- Orchitis is an inflammation of the testicles that affects 20-50% of patients with mumps. Atrophic changes of varying degrees in testicular tissue occur in a third of patients, and fertility (the ability to conceive) may decrease, but infertility as a result of mumps is rare.

- Oophoritis - inflammation of the ovaries. It is very rare and does not lead to a decrease in fertility.
- Pancreatitis - inflammation of the pancreas. It affects 5% of patients with mumps. Changes in the pancreas are rarely irreversible, but a few cases of diabetes mellitus have been identified against the background of damage to the cells of the pancreas by the virus.
In addition to the mumps virus, inflammation of the parotid salivary glands can be caused by cytomegalovirus, influenza and parainfluenza viruses, HIV infection, various bacteria, in addition, it can be associated with metabolic disorders, neoplasms, salivary stone disease, and taking a number of medications.
Who is at risk?
- Children from 2 to 12 years old.
- Elderly people.
- Immunocompromised patients.
- Those who have not been vaccinated or who have not developed a sufficient level of immunity after vaccination.
Diagnosis
Diagnosis of mumps is based primarily on the history and symptoms present. Additional diagnostic measures may be required to exclude other diseases with a similar clinical picture.
Laboratory diagnostics
- Complete blood count (without leukocyte formula and ESR). Leukocyte formula. In mumps, leukopenia with relative lymphocytosis can be detected.
- Erythrocyte sedimentation rate (ESR). This is a non-specific sign of inflammation. With parotitis, it is increased.
- C-reactive protein. With parotitis, it is sometimes elevated.
- Total amylase in daily urine and total amylase in serum. Amylase is an enzyme produced by the pancreas and salivary glands. It is necessary for the digestion of carbohydrates contained in food. With pathology of the salivary glands or pancreas, the level of amylase in the blood and urine may be increased.
- Pancreatic amylase. Increased with damage to the pancreas.
- Determination of antibodies to the mumps virus in the blood. Class M immunoglobulins and class G immunoglobulins to the mumps virus are detected. IgM are responsible for the primary immune response and appear in the blood in the first days of illness. IgG begin to be produced a little later.
Other research methods
- Radiography (sialography), computed tomography, magnetic resonance imaging of the salivary glands. These methods allow assessing the state of the glands, identifying neoplasms, salivary stones, violations of the secretion outflow, pathological changes in the tissues of the salivary gland or surrounding areas.
- Testicular ultrasound. May be required for orchitis.
In case of complications, the doctor may prescribe a number of additional tests.
Treatment
There is no specific treatment for mumps, therapy is prescribed depending on the symptoms. Of great importance is bed rest, which reduces the risk of complications several times.